Abstract
Many projects on developing Electronic Health Record (EHR) systems have been carried out in many countries. The current study was conducted to review the published data on the utilization of open source EHR systems in different countries all over the world. Using free text and keyword search techniques, six bibliographic databases were searched for related articles. The identified papers were screened and reviewed during a string of stages for the irrelevancy and validity. The findings showed that open source EHRs have been wildly used by source limited regions in all continents, especially in Sub-Saharan Africa and South America. It would create opportunities to improve national healthcare level especially in developing countries with minimal financial resources. Open source technology is a solution to overcome the problems of high-costs and inflexibility associated with the proprietary health information systems.
Keywords: Electronic health record, electronic medical record, healthcare, health information system, open source software
INTRODUCTION
Today with the vast development of technology in the world responding to the variable and complex needs for interchanging clinical information among health-care providers to improve the quality of health-care services seems more practical than any time before. Efficacy of healthcare services and medical interventions are highly dependent on a trust worthy and integrated history of individual medical and health status. Electronic health record (EHR) is one such response that covers the need of all engaged parties including patients, doctors, clinical staff, insurance companies, health care providers and policy makers. It provides a platform on which individual health information is stored and accessed only by authorized people. EHR is defined as digitally stored health-care information about an individual's life with the purpose of supporting continuity of care, education and research. Lack of the required health information causes a lot of delay and expenses in health-care delivery.[1] EHR is a new way of storing and processing health information. A wide range of terms and phrases have been used to describe health and medical records. Health Insurance Portability and Accountability Act (HIPAA) defines EHR as “an electronic record of health-related information on an individual that is created, gathered, managed and consulted by authorized health-care clinicians and staff.”[2] The terms “Electronic Medical Record,” (EMR) Computer-based Patient Record (CPR), Electronic Patient Record (EPR), Personal Health Record (PHR), Computerized Medical Record (CMR) may also be treated synonymously with EHR.
OPEN SOURCE SOFTWARE (OSS)
In terms of software development and licensing, OSS and proprietary software are two main categories of software.[3] “The promise of opensource is better quality, higher reliability, more flexibility, lower cost and an end to predatory vendor lock-in.”[4] OSS encourages having access to the source code — the code computer programmers write-with the freedom of usage, modification and redistribution. On the contrary, he source code in proprietary software is confidential. The end user of such products can access and execute only the machine code.[3] The source code of proprietary software is closed and belongs only to the developer. The intention of developing this kind of software is to make a profit from licensing, rental or sale of the software and maintain full control of the product.[5]
Although OSS and “free software” describe almost the same category of software, they stand for views based on different values. Free software respects freedom to run the software to study and change it and also to redistribute copies with or without changes. The free software movement begins in 1983. In 1984, the free operating system GNU was developed.[6] GNU General Public License (GPL) is a free, copy left license for software, which is intended to guarantee the freedom to share and change all versions of software to make sure it remains free for all its users.[7] As some of the users and developers of free software were not agreed with the goals of the free software movement, a part of the free software community separated in 1998 and began to campaign in the name of “open source” afterward. Open source is based only on practical values, such as making or having powerful and reliable software.[6] Open Source Software (OSS), Free and Open Source Software (FOSS) and Free, Libre and Open Source Software (FLOSS)- although are not exactly the same- are alternative terms for free software.
In the health sector, open source products have been designed to improve health-care while reducing the cost of similar proprietary products. According to Reynolds and Wyatt, it creates “a key opportunity for the promotion of effective systems by enhancing clinical engagement in software development, fostering innovation, improving system usability and reducing costs and should therefore be central to a rational HIS [Healthcare Information System] procurement strategy.”[3] A handful of projects on developing EHR systems have been carried out in many countries.
EHR in USA
In the United States of America, approximately 23.9% of physicians used EHR in the ambulatory setting and only 5%of hospitals used Computerized Physician Order Entry (CPOE) through 2005.[8] A study on the levels of EHR adoption in USA revealed that only few US hospitals had a comprehensive electronic clinical information system and many others only had parts of an electronic records system. It seems that financial support, interoperability and training of information technology support staff by policy makers is necessary for increasing the application of EHR in US hospitals.[9] Since the late 1970s, U.S. Department of Veterans Affairs (VA) as a governmental sector advanced their efforts to develop an extensive organizational health information system named veterans’ health information systems and technology architecture (VistA). VistA uses Massachusetts general hospital utility multi-programming system (MUMPS) a program that can be used for disease case registries.[10] Only a few major organizations in the private sector worked on the implementation of EHRs in USA.[11]
EHR in Canada
Canada is another country, which seeks technological solutions to expand high quality health-care services across the country. These solutions also create new challenges, especially in acceptable standards, choice of technologies, overcoming traditional jurisdictional boundaries, privacy and confidentiality.[12] Many projects were planned to develop an efficient EHR in Canada. Health Infoway is among such efforts. Canada Health Infoway is a non-profit corporation founded by the federal government of Canadian 2000. The initial aim of this organization was to accelerate the development of EHR on a pan-Canadian basis by 2007. It tries to connect organizations, which are working on EHR projects and encourage them to produce and share “knowledge objects,” which can be reused by other organizations. Canada Health Infoway is a major investment for Canadians with 1.1 billion dollar budget.[13] This would support more efficient health-care delivery, patient confidentiality, immediate access to complete and accurate patient information while enabling better decisions about diagnosis and treatment. The final result would be a sustainable health-care system with higher quality, accessibility, productivity and cost savings.[6]
EHR in England
In England, National Program for Information Technology, which is directed by the National Health Service (NHS) is responsible for delivering England's EHR.[14] NHS established an EHR system in 2005. The aim was to provide all 50 million NHS patients with an individual electronic NHS Care Record Service (NHSCRS) by 2010. The NHSCRS would securely share the detailed records of each person between different parts of the local NHS sites. The system uses a unique identifier for each patient. Patients would be able to have a summary of their important health information, known as their Summary Care Record (SCR), available to authorized NHS staff anywhere in the NHS in England. They also would access their SCR using a secure website named as “HealthSpace.” The budget of this project was estimated 12.6 billion Pounds in 2006. This was almost 2 times more than what was estimated since the project was first launched. It was assumed that the project may finally cost more than 20 billion pounds.[15]
EHR in Australia
Many regional and national EHR projects and systems have been developed in the Asia-Pacific region.[16] In Australia as the pioneer of EHRs, Health Information Technology (HIT) is considered the basis for improving the quality of healthcare, safety and efficiency by the government. General practices were encouraged to install clinical software packages for prescribing and transmission of clinical data in the late 1990s.[17] HealthConnect is a joint Australian, State and Territory Governments’ initiative for revolving paper-based health records to EHRs for the benefit of consumers and also health-care providers. Through which, health information would be more quickly available and transferred among healthcare professionals under more secure condition. The main aims of this program was the accessibility of life-saving information in emergencies and also the improvement of safety and quality of health information through a shared electronic health record (SEHR).[18] The National E-Health Transition Authority (NEHTA) is responsible for developing a design for SEHR. NEHTA was funded jointly by the Australian, state and territory governments in 2005 to develop national standards and infrastructure for EHR across Australia.[19]
Many studies focused on the benefits of using the OSS in the health sector.[20,21,22,23,24,25,26,27,28,29,30] In a number of researches, the characteristics of OSS systems have been compared with each other.[31,32] During the recent years, utilization of OSS in national health systems has been welcomed by many countries to respond to the necessity of EHR systems for improving the health-care services and the problems of implementing proprietary EHR systems.
The present study was conducted to review the published data on the utilization of open source EHR systems in different countries all over the world and the primary reasons for utilization of those systems highlighted by published studies.
METHODS
A systematic review of studies on the utilization of open source EHR was developed through the following stages:
Eligibility criteria
All indexed original and review articles, short communications, case reports and scientific letters by selected bibliographic databases on the utilization of open source EHR in any country were eligible in this study.
Data sources
Six bibliographic databases including Ovid Medline, ISI Web of Science, Scopus, Excerpta Medica Database (EMBASE), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Library Information Science and Technology Abstracts (LISTA) were searched for relevant articles.
Search strategy
We searched all six databases using free-text and subject-keyword search techniques for relevant studies according to the search tools of each database. The selected keywords were “electronic health record,” “electronic medical record,” “computerized medical record”,” “computer based medical record,” “computerized patient record” “computer based patient record,” “electronic patient record,” “personal health record” and “open source.” We limited the search results to original and review articles, short communications, case reports and scientific letters published from 1990 up to 2012.
Screening and selection
Primary selection of studies was based on the inclusion criteria, which were original and review articles, short communications, case reports and scientific letters on the utilization of open source EHR in any country. The duplicated publications were excluded. At the first screening stage, two reviewers (FA andFS) independently screened title and abstract of retrieved documents to determine those which met the eligibility criteria. Full citations of those documents considered eligible at least by one reviewer were imported into an EndNote database. In the next stage, the full text of the imported papers were provided and reviewed for subject relevancy individually by each of the two reviewers. A critical appraisal check list was used to evaluate the validity of the selected studies and to criticize them.[33] Finally, the two reviewers made a face-to-face meeting, discussing on papers selections. Discrepancies were resolved through discussion. In the cases, which consensus did not happen, a third reviewer (MA) made the final decision on the eligibility of a particular paper. Consequently, those papers, which have been considered as valid by both reviewers, selected for data extraction.
Data extraction
A list of eligible studies was produced. Also, a specific questionnaire for data extraction was designed for recording data from the selected studies. The extracted data were the author`s name, year of publication, the source title, the open source EHR system/systems, country/countries of utilization and the primary reasons for open source EHR utilization in selected studies.
RESULTS
A total of 183 papers were identified by searching six bibliographic databases. The 99 duplicated publications were excluded. After screening, the title and abstract of the retrieved documents, 51 irrelevant papers were excluded and 33 studies were considered for full text evaluation. Then the full texts of selected papers were obtained and evaluated from which 17 papers were selected for inclusion in the review.[32,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49] The flow chart of the process of study selection is shown in Figure 1.
Figure 1.
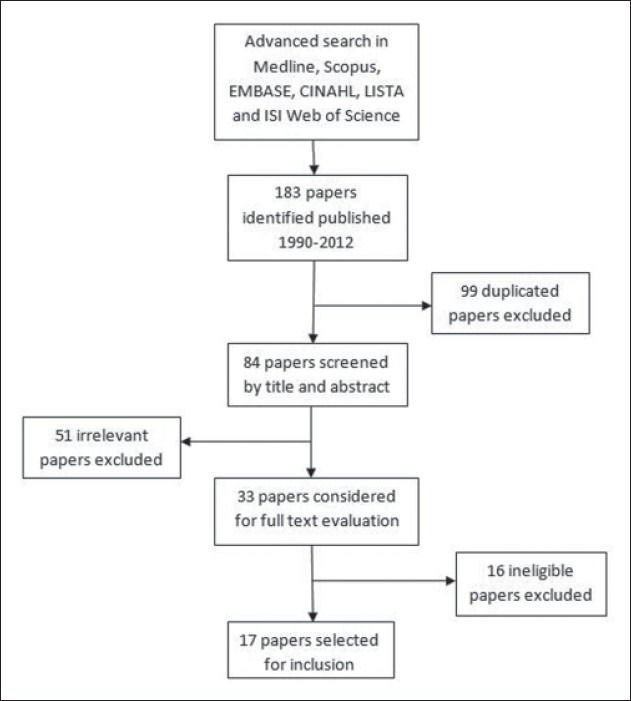
Flow chart of study selection
The excluded studies were not original article, review, case report or scientific letter or did not related to the utilization of a specific open source EHR in a specific country. The included studies are introduced in Table 1.
Table 1.
Included studies
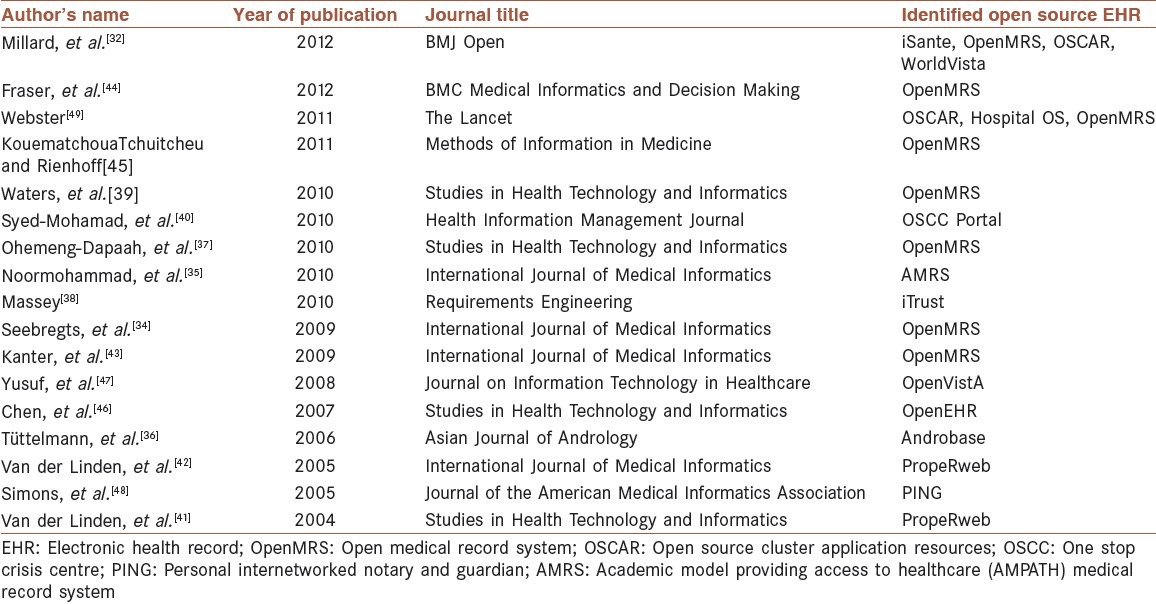
The Academic Model Providing Access to Healthcare (AMPATH) Medical Record System (AMRS), Androbase, HospitalOS, iSante, iTrust, OpenEHR, OpenMRS, OpenVistA, Oopen Source Cluster Application Resources (OSCAR), One Stop Crisis Centre (OSCC) portal, Personal Internetworked Notary and Guardian (PING), PropeRWeb and WorldVistA. Table 2 shows the characteristics of the 13 identified open source EHRs. It represents the country/countries of utilization and the primary reason/reasons for utilization of systems identified by reviewing the selected documents.
Table 2.
Characteristics of identified open source electronic health record systems

AMRS
AMRS is an implementation of Open MRS. AMRS is an open source medical record system developed by the AMPATH informatics team at the AMPATH center in Eldoret, to manage clinical care of human immunodeficiency virus (HIV) infected patients. AMRS is composed of paper-based records as well as EMRs because most clinicians in resource limited settings cannot use computers directly during patient visits. The system collects discrete data from clinical encounters at AMPATH including demographic data, symptoms, vital signs, physical exam findings, test results, diagnoses and treatments. All data are stored as coded concepts to allow easy retrieval and analysis. The system strongly emphasizes on data reuses to support patient care. AMRS is securely accessible via the internet with proper authorization
Androbase
Androbase is a new EPR and database based on open source technology (MySQL database and PHP language), which is established in a university clinic in Germany. Androbase was developed mainly because the lack of adaptability and extensibility of the previous commercially protected system to specific needs and its poor response times during daily work made it unacceptable by users. Utilization of Androbase reduced workload and increased performance through eliminating transcription steps and decreasing time for data entry.
Hospital OS
Hospital OS is an open source EMR system developed by Open Source Technology Co., Ltd. located in Phuket, Thailand. Hospital OS is user-friendly software released under a GNU GPL in 2001. The system developed by a team of programmers, software engineers, healthcare professionals and hospital experts to improve the quality of healthcare services in Thailand`s hospitals at no cost. Hospitals can use and customize the software to suit their particular needs and also share the software to other hospitals. Hospital data reporting and filing is streamlined in Hospital OS. It can save time and cost in health-care management. Nowadays, the system is demanded by many countries around the world.
iSante
iSanté is free open source EMR system developed to improve clinical care of HIV-infected patients in Haiti. The system is available in French and English. iSanté can provide and send aggregated data for national reporting.
iTrust
iTrust is an open source EHR system, which was founded as a project in a software engineering course at North Carolina State University to teach various automatic testing techniques. The system enjoyed the consultation of a practicing physician and a professional from the North Carolina Healthcare Information and Communications Alliance (NCHICA). iTrust is a patient-centered system. Patients can login to the system and do a variety of tasks. It allows patients to access to their own medical records, select their care giver and also communicate with their doctors. Any access and change into a specific medical record can be reported to patient through e-mail alerts. Some of functionalities of iTrust include appointment scheduling, physician order entry, prescribing medication, billing, ordering laboratory tests and viewing lab results.
OpenEHR
OpenEHR is founded by the OpenEHR Foundation, which is a not-for-profit company. It is initiated as a mutual project by University College London, UK and Ocean Informatics Pty Ltd, Australia. The main focus of the openEHR Foundation is EPRs. OpenEHR is about life-long interoperable EHRs to improve the quality of health-care and research. One of the features of openEHR is developing publicly available structures and terminologies in a repository known as the Clinical Knowledge Manager (CKM). As an online clinical knowledge resource, the OpenEHR CKM allows users to participate in the creation an international set of archetypes, which could enhance interoperability of the whole system. OpenEHR enables clinicians to manage clinical content separately from the software through the archetype formalism. Now, it is used in a number of countries around the world.
OpenMRS
OpenMRS is an open source EMR system developed by a large network of open source developers coordinated by the Regenstrief Institutein 2004. The system was implemented initially in Kenya and then was rapidly adopted by health-care organizations in resource poor countries. OpenMRS has a concept dictionary in its core, which stores total diagnosis, tests, drugs and also general questions and potential answers. It has been used in several African countries including South Africa, Ethiopia, Mali, Ghana, Nigeria, Kenya, Rwanda, Malawi, Senegal, Tanzania, Uganda, Lesotho, Zimbabwe, Mozambique, Sierra Leone and Haiti. Nowadays, it is wildly used throughout the world.
OpenVistA
OpenVistA is a non-proprietary, open source EHR system based on the VA VistA software. OpenVistA reduces the expenses by allowing VistA to run on the Linux operating system, which is open source and free. It also enables the client organizations to run the system also on Windows. They can choose either InterSystems Caché or Fidelity GT.Ml. OpenVistA allows multiple clinicians to simultaneously access to various patient data in real-time. The system provides progress note, various templates, ordering and reporting tools, audit capabilities, electronic signature. Document management, data integration tools and CPOE are among other features of OpenVistA.
OSCAR
OSCAR is an open source EHR system developed by Department of Family Medicine at McMaster University, Canada. OSCAR is based on Linux and MySQL database and uses the GPL. The system allows users to install a high performance computing cluster. Multiple message passing interface implementations could be install on one cluster. OSCAR`s functionalities include various services such as registration, scheduling, medical record and billing. Moreover, it includes a powerful testing architecture for ensuring the readiness of the cluster set up for production.
OSCC Portal
The OSCC Portal is an open source web-based EPR system, which is developed for OSCC, Hospital University Sains Malaysia (HUSM) in Kelantan, Malaysia. Utilization of OSCC Portal improved data confidentiality; data integration; communication, coordination between disciplines; standardization of data; quality assessment; and research in HUSM, which are all necessary for quality of care.
PING
PING is a free and open source health information system. It is designed and implemented as an interoperable, personally controlled health record, which enables patients to have control accessibility to their medical information by others. PING architecture is based on replaceable modular pieces so that collaborators can add to or substitute in PING components. PING compiles lifelong patient history and allows patients to store encrypted copies of their records in selective storage sites. PING is adopted by the Canadian National Research as a model for regional, provincial and national personally controlled health records.
PropeRWeb
PropeRWeb is a multidisciplinary EHR system, which is built based on open standards in Netherlands. As a web based application, the system uses servlets and Java Server Pages with CORBA connection to the database servers. In PropeRWeb, patients and care givers are separated into two different Person Identification Specification (PIDS) servers to enhance security and privacy. Auditing as a functionality that provides info at a specific moment is implemented in PropeRWeb by distinguishing between versions of archetypes and forms. Although some aspects such as user friendliness need more improvements; however, the system is flexible enough to be readily customized for use in a variety of clinical domains.
WorldVistA
WorldVistA is an open source EHR system that evolved from VistA project to make it widely available outside of its original setting within the United States and around the world. The system developed additional modules such as pediatrics, obstetrics and patient billing not normally used in the veteran's health-care setting. WorldVistA is able to run on proprietary intersystem cache database. Web-based and client-server configurations can be established on the system depending on the environment. Although it is a primary care system, but other templates for specialties can be created by users. WorldVistA has various functionalities including patient registration, drug allergy and interaction checking, creating health maintenance remainders, clinical order entry, templates for obstetrics/gynecology and pediatrics care, viewing lab and imaging results and generating reports of demographics, medications and problems.
DISCUSSION
EHR provides brilliant chance of readily retrieving the required information for conducting a faster and a much more accurate decision for action. Decline in medical errors is another important advantage of applying EHR that should seriously be taken into account.[1] Open source EHRs have been designed to improve health-care while reducing the cost of similar proprietary systems. Those who developed OSS actually encourage it and rely on this philosophy to see the software spread and grow beyond its original creators.[4] According to the findings, open source EHR systems have been wildly welcomed by source limited regions around the world, especially in Sub-Saharan Africa and South America. Argentina, Australia, Chile, Ecuador, Ethiopia, Germany, Ghana, Haiti, Jordan, Kenya, Lesotho, Malawi, Malaysia, Mali, Mexico, Mozambique, Netherlands, Nigeria, Pakistan, Peru, Rwanda, Senegal, Sierra Leone, South Africa, Sweden, Tanzania, Thailand, Turkey, Uganda, USA and Zimbabwe are among countries, which used open source EHRs to enhance the health care quality. The results indicated that many countries especially developing countries- demand to use an interoperable and cost-efficient EHR system, which is flexible enough to modify and improve.
Commercial software companies and some people claim that open source systems cannot fulfil medicolegal and security requirements required for a health-care system and may allow hackers to know the software bugs more easily than proprietary software.[50] However, some experts believe that open source systems are more secure from external attack than closed source systems because the independent assessment of system security, which happens in OSS “makes bug patching easier and more likely and forces developers to spend more effort on the quality of their code.”[49] Active assessment of software codes by their users makes them more stable than proprietary systems. On the other hand, because of commercial pressures customers’ requirements are more important for proprietary software developers than security requirements, which are invisible to customers.[51]
Open source systems make opportunities for advanced innovation in the health information sector of low income countries.[49] However, cost- efficiency seems to be the most important reason for utilization of open source systems in many countries. Despite the enormous financial investment to Canada Health Infoway, some believes that the reduction in duplicated efforts will reduce the total expenses of a pan-Canadian EHR.[13] Some critics said that spending billions of dollars in purchasing health software would lead to enormous overpayments to technology companies and consultants. Such a huge investment on a national health information structure encourages a competition between companies for profitable deals to sell their electronic health systems promising to connect patients, doctors and hospitals. They believe that OSS would be a better solution instead of spending too much money on expensive proprietary products.[52] The open three (O3) consortium project launched in 2004 is an example of utilization of OSS, which was based on the agreements on the impact of open solutions in facilitating fast integration of health systems in Europe and the world.[22] Even, in the USA some of the current EHR systems are not fully desirable because of being expensive and inflexible and proprietary. Open source systems with the potentiality for local customization could be a possible solution to solve these problems and to improve health-care services in the United States as they have done in many other countries around the world.[28] The evidences indicated that utilization of OSS in the health sector is more welcomed in developing countries with financial limitations. Although various open source EHR programs may not fully encompass the functionality requirements for an ideal EHR system, they create opportunities to improve national health-care level in countries with minimal financial resources.[31] Developing countries use open source EHRs to lower cost and to improve the efficiency and quality of health-care services. The overall results indicated that open source EHR is a solution to overcome the problems of high costs and inflexibility associated with proprietary systems.
CONCLUSION
Several projects on utilizing open source EHR in the world, especially in developing countries confirm the effective role of open source EHR systems in improving the healthcare level in countries with minimal financial resources.
ACKNOWLEDGMENT
This study was part of a PhD thesis supported by Iran University of Medical Sciences.
Footnotes
Source of Support: Iran university of medical sciences
Conflict of Interest: None declared
REFERENCES
- 1.Rezae P, Ahmadi M, Sadughi F. Comparative study on EHR content, structure, and terminology standards in selected organizations and design a model for Iran. J Health Adm. 2007;10:55–64. [Google Scholar]
- 2.HIPPA. The Definition of Electronic Health Record. [Accessed on 2012 Sep 20]. Available from: http://www.hipaa.com/2009/05/the-definition-of-electronic-health-record .
- 3.Reynolds CJ, Wyatt JC. Open source, open standards, and healthcare information systems. J Med Internet Res. 2011;13:e24. doi: 10.2196/jmir.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Open Source initiatives. [Accessed on 2012 Dec 6]. Available from: http://www.Opensource.org/docs/osd .
- 5.Khelifi Adel AT, editor. Abu Dhabi, UAE: European and Mediterranean Conference on Information Systems (EMCIS2010); 2010 April 12-13; A preliminary open source software infrastructure for the health sector in the UAE. [Google Scholar]
- 6.Stallman R. Why open source misses the point of free software. [Accessed on 2012 Sep 20]. Available from: http://www.gnu.org/philosophy/open-source-misses-the-point.html .
- 7.GNU General Public License. [Accessed on 2012 Sep 20]. Available from: http://www.gnu.org/licenses/gpl.html .
- 8.Jha AK, Ferris TG, Donelan K, DesRoches C, Shields A, Rosenbaum S, et al. How common are electronic health records in the United States? A summary of the evidence. Health Aff (Millwood) 2006;25:w496–507. doi: 10.1377/hlthaff.25.w496. [DOI] [PubMed] [Google Scholar]
- 9.Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;360:1628–38. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 10.Greenbaum D, Sboner A, Mu XJ, Gerstein M. Genomics and privacy: Implications of the new reality of closed data for the field. PLoS Comput Biol. 2011;7:e1002278. doi: 10.1371/journal.pcbi.1002278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berner ES, Detmer DE, Simborg D. Will the wave finally break? A brief view of the adoption of electronic medical records in the United States. J Am Med Inform Assoc. 2005;12:3–7. doi: 10.1197/jamia.M1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alvarez RC. The promise of e-health – A Canadian perspective. World Hosp Health Serv. 2004;40:31–5. [PubMed] [Google Scholar]
- 13.Catz M, Bayne J. Canada health infoway – A pan-Canadian approach. AMIA Annu Symp Proc. 2003:807. [PMC free article] [PubMed] [Google Scholar]
- 14.Huston JL. EHR in the UK: Shedding some light from a manager's perspective. Health Care Manag (Frederick) 2006;25:335–40. doi: 10.1097/00126450-200610000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Nicholson L. Amsterdam: EHR Conference; 2008. Electronic Health Records in the United Kingdom of Great Britain Northern Ireland. [Google Scholar]
- 16.Kimura M, Croll P, Li B, Wong CP, Gogia S, Faud A, et al. Survey on medical records and EHR in Asia-Pacific region: Languages, purposes, IDs and regulations. Methods Inf Med. 2011;50:386–91. doi: 10.3414/ME11-02-0002. [DOI] [PubMed] [Google Scholar]
- 17.McInnes DK, Saltman DC, Kidd MR. General practitioners’ use of computers for prescribing and electronic health records: Results from a national survey. Med J Aust. 2006;185:88–91. doi: 10.5694/j.1326-5377.2006.tb00479.x. [DOI] [PubMed] [Google Scholar]
- 18.Health Connect. [Cited on 2012 Sep 09]. Available from: http://www.health.gov.au/healthconnect .
- 19.NEHTA- National E-Health Transition Authority. [Accessed on 2012 Sep 20]. Available from: http://www.nehta.gov.au .
- 20.Bush J. Open-source software: Just what the doctor ordered? Fam Pract Manag. 2003;10:65. 69. [PubMed] [Google Scholar]
- 21.De Lusignan S, Kumarapeli P, Debar S, Kushniruk AW, Pearce C. Using an open source observational tool to measure the influence of the doctor's consulting style and the computer system on the outcomes of the clinical consultation. Stud Health Technol Inform. 2009;150:1017–21. [PubMed] [Google Scholar]
- 22.Dinevski D, Poli A, Krajnc I, Sustersic O, Arh T. E-health integration and interoperability based on open-source information technology. Wien Klin Wochenschr. 2010;122(Suppl2):3–10. doi: 10.1007/s00508-010-1354-9. [DOI] [PubMed] [Google Scholar]
- 23.Dove ES, Ozdemir V, Joly Y. Harnessing omics sciences, population databases, and open innovation models for theranostics-guided drug discovery and development. Drug Dev Res. 2012;73:439–46. [Google Scholar]
- 24.Gatta R, Abeni F, Buglione M, Peveri A, Barbera F, Tonoli S, et al. Open-source, low-cost, high-reliability solutions for digital imaging systems: Example of a “dicom router”. Radiol Med. 2007;112:1252–9. doi: 10.1007/s11547-007-0216-7. [DOI] [PubMed] [Google Scholar]
- 25.Good T, DiTommaso M. SQL Clinic: The open-source alternative for electronic medical records. Psychiatr Serv. 2005;56:269–71. doi: 10.1176/appi.ps.56.3.269. [DOI] [PubMed] [Google Scholar]
- 26.Lee YH. Efficient radiologic reading environment by using an open-source macro programas connection software. Eur J Radiol. 2012;81:100–3. doi: 10.1016/j.ejrad.2010.11.019. [DOI] [PubMed] [Google Scholar]
- 27.Marques ET, Jr, Maciel FilhoR, August PN. Overcoming health inequity: Potential benefits of apatient-centered open-source public health infostructure. Cad Saude Publica. 2008;24:547–57. doi: 10.1590/s0102-311x2008000300008. [DOI] [PubMed] [Google Scholar]
- 28.Yellowlees PM, Marks SL, Hogarth M, Turner S. Standards-based, open source electronic health record systems: A desirable future for the U.S. health industry. Telemed J E Health. 2008;14:284–8. doi: 10.1089/tmj.2007.0052. [DOI] [PubMed] [Google Scholar]
- 29.Kantor GS, Wilson WD, Midgley A. Open-source software and the primary care EMR. J Am Med Inform Assoc. 2003;10:616–7. doi: 10.1197/jamia.M1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Los RK, vanGinneken AM, svanderLei J. Open SDE: Astrategy for expressive and flexible structured data entry. Int J Med Inform. 2005;74:481–90. doi: 10.1016/j.ijmedinf.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 31.Flores Zuniga AE, Win KT, Susilo W. Functionalities of free and open electronic health record systems. Int J Technol Assess Health Care. 2010;26:382–9. doi: 10.1017/S0266462310001121. [DOI] [PubMed] [Google Scholar]
- 32.Millard PS, Bru J, Berger CA. Open-source point-of-care electronic medical records foruse inresource-limited settings: Systematic review and questionnaire surveys. BMJ Open. 2012;2:e000690. doi: 10.1136/bmjopen-2011-000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Critical Appraisal Skills Programme (CASP) [Accessed on 2012 Dec 21]. Available from: http://www.casp-uk.net .
- 34.Seebregts CJ, Mamlin BW, Biondich PG, Fraser HS, Wolfe BA, Jazayeri D, et al. The OpenMRS implementers network. Int J Med Inform. 2009;78:711–20. doi: 10.1016/j.ijmedinf.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 35.Noormohammad SF, Mamlin BW, Biondich PG, McKown B, Kimaiyo SN, Were MC. Changing course to make clinical decision support work in an HIV clinic in Kenya. Int J Med Inform. 2010;79:204–10. doi: 10.1016/j.ijmedinf.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 36.Tüttelmann F, Luetjens CM, Nieschlag E. Optimising workflow in andrology: A new electronic patient record and database. Asian J Androl. 2006;8:235–41. doi: 10.1111/j.1745-7262.2006.00131.x. [DOI] [PubMed] [Google Scholar]
- 37.Ohemeng-Dapaah S, Pronyk P, Akosa E, Nemser B, Kanter AS. Combining vital events registration, verbal autopsy and electronic medical records in rural Ghana for improved health services delivery. Stud Health Technol Inform. 2010;160:416–20. [PubMed] [Google Scholar]
- 38.Massey AK, Otto PN, Hayward LJ, Antón AI. Evaluating existing security and privacy requirements for legal compliance. Requir Eng. 2010;15:119–37. [Google Scholar]
- 39.Waters E, Rafter J, Douglas GP, Bwanali M, Jazayeri D, Fraser HS. Experience implementing a point-of-care electronic medical record system for primary care in Malawi. Stud Health Technol Inform. 2010;160:96–100. [PubMed] [Google Scholar]
- 40.Syed-Mohamad SM, Ali SH, Mat-Husin MN. The development and design of an electronic patient record using opens ource web-based technology. HIMJ. 2010;39:30–5. [PubMed] [Google Scholar]
- 41.Van der Linden H, Tange H, Talmon J. PropeR and archetypes. Stud Health Technol Inform. 2004;110:49–53. [PubMed] [Google Scholar]
- 42.Van der Linden H, Talmon J, Tange H, Grimson J, Hasman A. PropeRrevisited. Int J Med Inform. 2005;74:235–44. doi: 10.1016/j.ijmedinf.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 43.Kanter AS, Negin J, Olayo B, Bukachi F, Johnson E, Sachs SE. Millennium global village-net: Bringing together millennium villages throughout sub-Saharan Africa. Int J Med Inform. 2009;78:802–7. doi: 10.1016/j.ijmedinf.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 44.Fraser HS, Thomas D, Tomaylla J, Garcia N, Lecca L, Murray M, et al. Adaptation of a web-based, open source electronic medical record system platform to support a large study of tuberculosis epidemiology. BMC Med Inform Decis Mak. 2012;12:125. doi: 10.1186/1472-6947-12-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kouematchoua Tchuitcheu G, Rienhoff O. Options for diabetes management in sub-Saharan Africa with an electronic medical record system. Methods Inf Med. 2011;50:11–22. doi: 10.3414/ME09-01-0021. [DOI] [PubMed] [Google Scholar]
- 46.Chen R, Klein G. The openEHR Java reference implementation project. Stud Health Technol Inform. 2007;129:58–62. [PubMed] [Google Scholar]
- 47.Yusuf EM. Implementation of OpenVistA in hospitals in Turkey. J Inf Technol Healthc. 2008;6:212–20. [Google Scholar]
- 48.Simons WW, Mandl KD, Kohane IS. The PING personally controlled electronic medical record system: Technical architecture. J Am Med Inform Assoc. 2005;12:47–54. doi: 10.1197/jamia.M1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Webster PC. The rise of open-source electronic health records. Lancet. 2011;377:1641–2. doi: 10.1016/s0140-6736(11)60659-4. [DOI] [PubMed] [Google Scholar]
- 50.Gallivan MJ. Striking a balance between trust and control in a virtual organization: A content analysis of open source software case studies. Inf Syst J. 2001;11:277–304. [Google Scholar]
- 51.Payne C. On the security of open source software. Inf Syst J. 2002;12:61–78. [Google Scholar]
- 52.Webster PC. Canada's ehealth software “Tower of Babel”. CMAJ. 2010;182:1945–6. doi: 10.1503/cmaj.109-3717. [DOI] [PMC free article] [PubMed] [Google Scholar]


