Abstract
Background:
Urinary catheterization might have catheter-related bladder discomfort (CRBD). We evaluated the efficacy of different doses of ketamine in comparison to placebo as a treatment of CRBD.
Materials and Methods:
One hundred twenty patients who were candidate for urological surgery requiring catheterization of the urinary bladder were randomly divided into four groups including 30 patients in each. Group I received normal saline, Group II received ketamine 150 μg/kg/iv, Group III received ketamine 200 μg/kg/iv, and Group IV received 250 μg/kg/iv in the equal volume of 2 mL. The patients were observed for each 15 min in the recovery room and in the 1 h, 2 h, 6 h, 12 h, and 24 h after discharging from it for severity of CRBD and pain, levels of sedation, and post-operative nausea and vomiting.
Results:
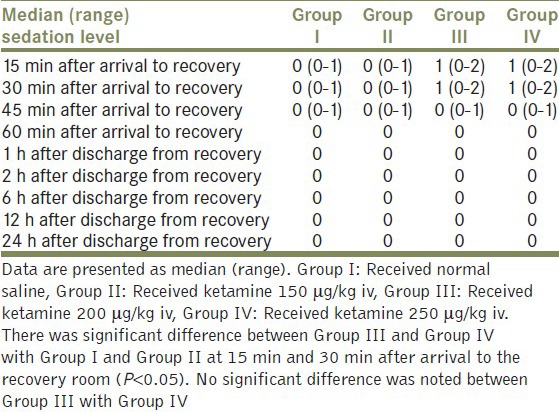
The severity of CRBD at the recovery room was significantly reduced in Group III and Group IV after 24 h compared with Group I and Group II (P < 0.05). There was no significant difference between Group III and Group IV in this respect. The median sedation level was significantly lower in 15 min and 30 min after arrival to the recovery in Group III and Group IV compared with Group I and Group II (P < 0.05). There was no significant difference between Group III and Group IV in this regard.
Conclusions:
Ketamine 200 μg/kg/iv had similar efficacy with ketamine 250 μg/kg/iv in reducing the severity of CRBD without occurring significant side effect.
Keywords: Anesthesia, catheter-related bladder discomfort, ketamine, urologic surgery
INTRODUCTION
Urinary tract catheterization during surgery can cause discomfort after operation because of the catheter that is localized in the bladder. We describe it as catheter-related bladder discomfort (CRBD). The definition of CRBD was as an urgent to void or discomfort in the supra-pubic region observed after operation in patients who are emerge from anesthesia and have had a urinary catheterization during operation.[1]
This is not unusual that patients who have been catheterized during anesthesia complain of an urgency to void in the post-operative period because of catheter-related bladder irritation. The symptoms of CRBD were secondary to an indwelling urinary catheter and mimic those of an overactive bladder (OAB) such as urgency, urinary frequency with or without urgency incontinence.[1,2]
The CRBD can be very unpleasant or badly for the patients and is similar to those who have hyperactive bladder, i.e., urinary frequency with or without urgent incontinence.[2,3] These symptoms can have effect on satisfaction of personnel of hospital. On the other hand, urine catheter and the discomfort of that cause inability to void and increase the impatience of the patients. Another consequence of CRBD is the pain of the urine catheter that causes more oxygen to use. This increase the duration of the recovery stay and in older people increases the severity of coronary artery disease.[4,5,6] So if we decrease this discomfort in anyway, we reduce the side effects also. To reduce this discomfort, different type of drugs had been used. Most of these drugs have significant side effects especially in old age people. The tolterodine and oxybutynin were muscarinic receptor antagonists that have been reported to be effective in preventing CRBD.[1,7,8] In the treatment of resistant cases of OAB, gabapentin has been reported to be very effective.[9] Ketamine in sub-hypnotic dose has been used for treatment of post-operative shivering.[10] Incidentally, ketamine was observed to be effective in the treatment of CRBD, while it was administered for treatment of post-operative shivering.[11] This study was therefore designed to evaluate the efficacy of different dosage of ketamine as a treatment modality for CRBD during the post-operative period.
MATERIALS AND METHODS
After obtaining institutional approval from Ethic Committee of university and taking written informed consent from the patients, 120 American Society of Anesthesiologist (ASA) class I and II patients, aged 18-65 years, who were candidate for elective urologic surgery requiring catheterization of the urinary bladder were enrolled in this prospective randomized, double-blind placebo-controlled study. Patients who were chronic opioid user, had bladder outflow obstruction, neurogenic bladder, Parkinson's disease, diabetes mellitus, OAB (frequency more than 3 times in the night or more than 8 times in 24 h), transurethral resection of the prostate for benign prostatic hyperplasia, end-stage renal disease (urine output less than 50 mL per 24 h), or urinary tract infection were excluded from the study.
All the patients received midazolam (0.05 mg/kg/iv) 20 min before induction of anesthesia. All the patients take similar general anesthesia including fentanyl 2 μg/kg/iv, thiopental sodium 5 mg/kg/iv, and atracurium 0.5 mg/kg/iv. Then, all the patients were intubated and urine catheter was placed with 16 French Foley's catheter and fixed with 10 cc unsterile water. To lubricate the catheter, K-Y jelly was used. For maintaining anesthesia, nitrous oxide 70%, oxygen 30%, and isoflurane 1-1.25% were used. During anesthesia, monitoring of five lead ECG, non-invasive blood pressure, pulse oximetry, and capnography were done. As analgesic, morphine 0.1 mg/kg/iv was used. At the end of the surgery, residual neuromuscular blockade was reversed by combination of neostigmine (0.04 mg/kg/iv) and atropine (0.02 mg/kg/iv). Then the patients were sent to the recovery room.
In the recovery room, the patients who complained of CRBD were randomly divided into the four groups included 30 patients in each. The randomizations of patients were done with the help of a computer-generated table of random numbers into four similar equal groups (n = 30).
In the first group (Group I), the patients received normal saline intravenously; in the second group (Group II), the patients received ketamine 150 μg/kg/iv; in the third group (Group III), the patients received ketamine 200 μg/kg/iv; and in the four group (Group IV), they received ketamine 250 μg/kg/iv in the equal volume of 2 mL. The syringes were coded. The person who injected the drug had no information about the type of the drug injections. After surgery, the severity of CRBD, the level of sedation score, post-operative nausea and vomiting (PONV), respiratory depression, hallucinations, unpleasant dreams, and diplopia were recorded each 15 min in the recovery room, and continued until 24 h after discharge from it at the 1st h, 2nd h, 6th h, 12th h, and 24th h. CRBD score was graded as: No complain, patients did not complain about CRBD even when we asked; mild-complain of CRBD only when we asked from the patients; moderate complain of CRBD was reported by the patients on their own without asking; and severe complain was reported by the patients followed by behavioral responses.[1] The behavioral responses were accompanied with strong vocal response, flailing limbs, and attempts to pull out the catheter. ASA classification divided patients into the four groups, I: Without underline disease, II: With controlled underlined disease, III: Without uncontrolled underlying disease, and IV: Poor prognostic patients. Sedation score was divided into the four category: 0 = fully awake, I = the patient is sleepy but response to verbal orders; II = the patient is sleepy and response only to the touch stimulations; and III = the patient is sleepy and only response to painful stimulations.[12] Nausea and vomiting were evaluated as presence or absence of them. Visual analogue scale (VAS) is a score to classify the pain varied from 0 (no pain) to 10 (the worst) including: 0-3 = mild pain; 3-6 = moderate pain, and 6-10 = severe pain. If patients had VAS > 4, meperidine 0.5 mg/kg was administered. Any possible side effects of the drugs that used in the study were recorded each 15 min in the recovery room and in the 1st, 2nd, 6th, 12th, and 24th h after leaving the recovery room.
Duration of surgery and total consumption of fentanyl were also noted. The adverse effects of drug used in the study including respiratory depression, PONV, level of sedation, hallucinations, diplopia, and unpleasant dreams were assessed every 15 min in the recovery and every 1st h, 2nd h, 6th h, 12th h, and 24th h after recovery. The hallucination and unpleasant dreams were evaluated as presence or absence of them.
For estimation of sample size, it was shown that 30 patients per each group were necessary to achieve 90% power with a significant level of 0.05 to detect difference at proportion of CRBD in a range of 0.1 to 0.6 between four groups. Incidence of CRBD between the groups and fentanyl requirement was analyzed by Pearson Chi-square test, whereas severity of CRBD was analyzed by Fisher's Exact test. The one-way analysis of variance (ANOVA) was used to analyze the demographic data and hemodynamic variables between four groups. Also, the repeated measure ANOVA was used for intergroup comparison of hemodynamic parameters over time in study. Bonferroni correction was applied for multiple comparisons in four groups. SPSS 17.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. P <0.05 was considered as significant.
RESULTS
A total of 127 consecutive patients were evaluated during 1 year. Seven patients were excluded from the study. Therefore, 120 patients were included in the study and received study medication after randomization. The flow diagram of randomized patients is shown in Figure 1.
Figure 1.
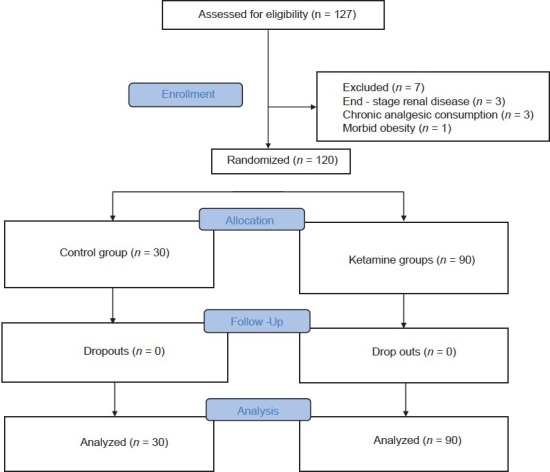
Flow chart of randomized patients
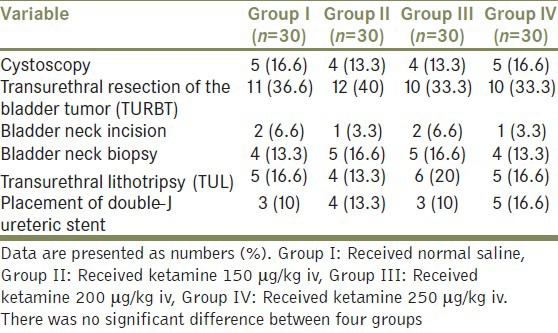
There was no substantial difference among four groups with regard to age, sex, weight, height, ASA, duration of surgery, duration of anesthesia, and duration of recovery stay (P > 0.05) [Table 1]. There was no significant difference between four groups with respect to type of urologic surgery [Table 2]. The mean ± SD of duration of surgery for cystoscopy, transurethral resection of the bladder tumor, bladder neck incision, bladder neck biopsy, transurethral lithotripsy, and placement of double-J ureteric stent was 16 ± 6.3, 65 ± 5.1, 15 ± 4.3, 13 ± 3.8, 36 ± 10.8, and 19 ± 5.1, respectively.
Table 1.
Demographic and clinical data of patients in four groups
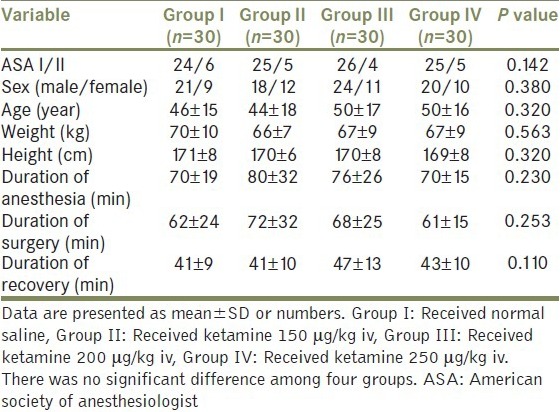
Table 2.
Frequency distribution of different urologic surgeries in four groups
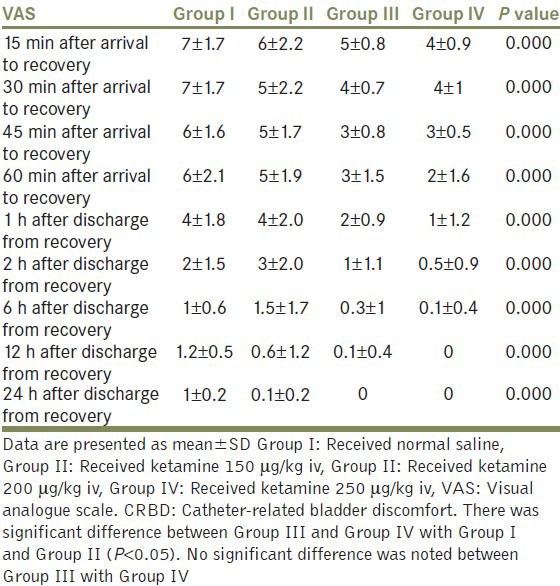
There was no difference between systolic blood pressure, diastolic blood pressure, heart rate, and respiratory rate at different time intervals between four groups (P > 0.05). The severity of CRBD was significantly less in Group III and Group IV compared with Group I and Group II till 24 h after operation (P < 0.05) [Table 3]. There was no significant difference between Group III and Group IV (P > 0.05).
Table 3.
Comparison of severity of catheter-related bladder discomfort at different time intervals in four groups
The median sedation level was significantly lower in 15 min and 30 min after arrival to the recovery in Group III and Group IV compared with Group I and Group II (P < 0.05) [Table 4]. There was no significant difference between Group III and Group IV in this regard [Table 4].
Table 4.
Comparison of median sedation score in different time intervals in four groups
The dosage of rescue analgesic used to control CRBD was significantly less in Group III and Group IV compared with Group I and Group II (P < 0.05) [Table 5]. No significant difference was noted between Group III and Group IV (P > 0.05) [Tables 5 and 6].
Table 5.
Comparison of the rescue analgesic used at different time intervals in four groups
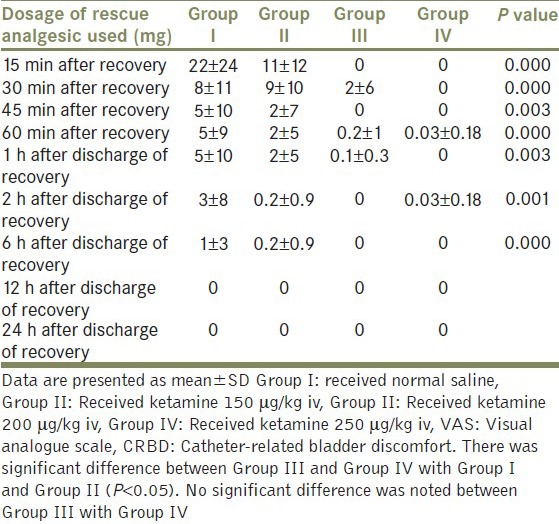
Table 6.
The incidence of adverse effects in four groups
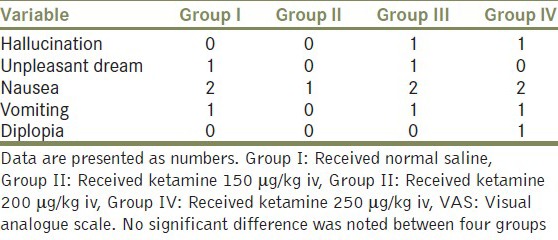
There was no significant difference between four groups in incidence of side effects such as nausea, vomiting, hallucination, unpleasant dreams, and diplopia (P > 0.05). [Table 6]
DISCUSSION
We showed that using low dose of ketamine (200 μg/kg i.v.) compare with higher dose of ketamine (250 μg/kg) significantly reduce the severity of CRBD post-operatively. Effective control of the pain at post-operative period is one of the most important points that must be considered. Acute pain after surgery is a complex physiological reaction to the tissue damage and diseases. Most of the time, patients remember this pain as the most terrible aspect of an operation. This pain has undesirable physiological effect on multi-systems. Better perception of the pain and pathophysiology of it leads to have better control of the patients, decreases morbidity, and reduces the cost of hospitalization in the recovery room and intensive care unit.
There are different kinds of techniques for control of post-operation pain such as using patient-controlled analgesia, central neuraxial blockade, peripheral neural blockade, and oral or intravenous analgesics. Perception of the mechanism of pain and the way to control it by drugs is an obligatory act if we want to have the best treatment. The stimulations produced by chemical, mechanical, and thermal injuries can activate pain receptors which are free end of the afferent myelinated neurons (A-Delta) and demyelinated fiber C. These peripheral afferent neurons send axonal branches to the posterior horn of spine column where they synapse to the primary afferent neurons.
Axonal branches of the second neuronal series change their pathway to the other side of the spinal column and go up to the thalamus (Spinothalamic area) as a secondary afferent way. During this tract, these neurons divide and send axonal branches to the reticular plexus and gray matter. In thalamus, the neurons of the second series synapse to the neurons of the third series and send axonal branches to the sensory cortex.
Catheterization during surgery may cause restlessness of patients after surgery which is because of the CRBD. This restlessness can be mild, moderate, or severe and cause unsatisfaction of patients in the recovery room. Another side effect of CRBD is the pain which happens after catheterization that increases the use of oxygen and hospitalization in the recovery room.[4,6,13] Therefore, if we reduce this discomfort, then the side effects also decrease. To reduce these discomfort, different kinds of drugs had been used: Oxybutynin[1], tolterodin[7], and gamma-aminobutyric acid agonists like gabapentin[14,15] that have their own side effects especially in old people.
Ketamine in sub-hypnotic doses can be used as a treatment for post-operative shivering.[10] Accidently, researchers observed that ketamine can be used as a treatment for CRBD also.[11] In the new study that has been done by Agarwal et al.[16] intravenous (IV) ketamine in 250 μg/kg dose has been used to treat CRBD in the groups having moderate to severe discomfort in the recovery room. The limitation of Agarwal et al. study was that the effect of the lower doses of ketamine for treatment of CRBD was not investigated. So we design this study to evaluate the effectiveness of different dosages of ketamine in treatment of CRBD.
Ketamine is an antagonist of N-methyl-d-aspartate (NMDA) and interacts with multiple binding sites including non-NMDA glutamine receptors, opioid, and mono-aminogenic receptorsnic, nicotinic, and muscarinic cholinergic receptors.[17] Ketamine by effect on the pre-ganglionic fibers, nicotinic receptors in the post-synaptic membrane of intramural ganglion, the muscarinic receptors, and the post-synaptic fibers can decrease the contractile response of the smooth muscles.[18] As Durieux showed, ketamine can inhibit muscarinic receptor signaling significantly.[19] Furthermore, ketamine by effect on the receptors of NMDA in the cortex of the brain can have analgesic effect.[20] The analgesic effect of ketamine might be additive or synergistic with its anti-muscarinic effect causing decrease in the severity of CRBD observed in our study.
Ketamine is partly water soluble and extremely fat soluble. The high solubility of it in fatty tissues causes fast effect of the drug. Most of the ketamine metabolism occur in liver and facilitated by N-demethylation in cytochrome P450 system. The most active metabolite of ketamine is norketamine that has the less efficiency (about 1/3-1/5 of ketamine) and change to inactive-water soluble metabolites that excrete in the urine. Ketamine is the only intravenous anesthetic drug that binds to few proteins (12%). When we use ketamine, most of the reflexes remain but we cannot be sure of the safety of respiratory tract. At the time of its usage, the eyes are open and pupils are in mid-size with nystagmus. Most of its complications are at the time of awaking including hallucinations, visual and auditory illusions, and unpleasant dreams. There is no evidence showing ketamine causing respiratory depression. Ketamine relaxes the soft tissue of bronchus. It has bronchus-dilating effect.[18,19,20,21]
The dosage of ketamine that used in our study was in the range of analgesic dosage not anesthetic dosage. So, its administration does not require full anesthetic coverage. Also, due to low dosage of ketamine used, there was no problem regarding smooth recovery of ketamine.
CONCLUSIONS
Our study showed that i.v. ketamine 200 μg/kg similar to i.vi. ketamine 250 μg/kg significantly reduced the severity of CRBD without causing significant adverse effects. We recommend using sub-hypnotic dosage of ketamine for treatment of CRBD in the post-operative periods.
ACKNOWLEDGMENT
The authors wish to sincerely thank the support of all the colleagues in Nor Hospital Medical Center affiliated to Isfahan University of Medical Sciences in Isfahan, Iran. Furthermore, our special thanks go to the patients, who wholeheartedly and actively assisted us to carry out this research. No conflict of interest existed. This prospective randomized observational study was approved by the Ethics Committee of our university, (Anesthesiology and Critical Care Research Center, Isfahan University of Medical Sciences, Isfahan, Iran) and all patients gave written, informed consent.
Footnotes
Source of Support: Anesthesiology and Critical Care Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
Conflict of Interest: None
REFERENCES
- 1.Agarwal A, Raza M, Singhal V, Dhiraaj S, Kapoor R, Srivastava A, et al. The efficacy of tolterodine for prevention of catheter-related bladder discomfort: A prospective, randomized, placebo-controlled, double-blind study. Anesth Analg. 2005;101:1065–7. doi: 10.1213/01.ane.0000167775.46192.e9. [DOI] [PubMed] [Google Scholar]
- 2.de Groat WC. Anatomy and physiology of the lower urinary tract. Urol Clin North Am. 1993;20:383–401. [PubMed] [Google Scholar]
- 3.Yoshimura N, Chancellor MB. Current and future pharmacological treatment for overactive bladder. J Urol. 2002;168:1897–913. doi: 10.1016/S0022-5347(05)64261-9. [DOI] [PubMed] [Google Scholar]
- 4.Singh P, Dimitriou V, Mahajan RP, Crossley AW. Double-blind comparison between doxapram and pethidine in the treatment of postanaesthetic shivering. Br J Anaesth. 1993;71:685–8. doi: 10.1093/bja/71.5.685. [DOI] [PubMed] [Google Scholar]
- 5.Mathews S, Al Mulla A, Varghese PK, Radim K, Mumtaz S. Postanaesthetic shivering - A new look at tramadol. Anaesthesia. 2002;57:394–8. doi: 10.1046/j.1365-2044.2002.2457_3.x. [DOI] [PubMed] [Google Scholar]
- 6.Piper SN, Suttner SW, Schmidt CC, Maleck WH, Kumle B, Boldt J. Nefopam and clonidine in the prevention of postanaesthetic shivering. Anaesthesia. 1999;54:695–9. doi: 10.1046/j.1365-2044.1999.00849.x. [DOI] [PubMed] [Google Scholar]
- 7.Tauzin-Fin P, Sesay M, Svartz L, Krol-Houdek MC, Maurette P. Sublingual oxybutynin reduces postoperative pain related to indwelling bladder catheter after radical retropubic prostatectomy. Br J Anaesth. 2007;99:572–5. doi: 10.1093/bja/aem232. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal A, Dhiraaj S, Singhal V, Kapoor R, Tandon M. Comparison of efficacy of oxybutynin and tolterodine for prevention of catheter related bladder discomfort: A prospective, randomized, placebo-controlled, double-blind study. Br J Anaesth. 2006;96:377–80. doi: 10.1093/bja/ael003. [DOI] [PubMed] [Google Scholar]
- 9.Yoshimura N, Chancellor MB. Current and future pharmacological treatment for overactive bladder. J Urol. 2002;168:1897–913. doi: 10.1016/S0022-5347(05)64261-9. [DOI] [PubMed] [Google Scholar]
- 10.Dal D, Kose A, Honca M, Akinci SB, Basgul E, Aypar U. Efficacy of prophylactic ketamine in preventing postoperative shivering. Br J Anaesth. 2005;95:189–92. doi: 10.1093/bja/aei148. [DOI] [PubMed] [Google Scholar]
- 11.Gupta D, Agarwal A, Dhiraaj S. Ketamine for treatment of catheter-related bladder discomfort. Br J Anaesth. 2005;95:720. doi: 10.1093/bja/aei609. [DOI] [PubMed] [Google Scholar]
- 12.Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2:656–9. doi: 10.1136/bmj.2.5920.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mathews S, Al Mulla A, Varghese PK, Radim K, Mumtaz S. Postanaesthetic shivering - A new look at tramadol. Anaesthesia. 2002;57:394–8. doi: 10.1046/j.1365-2044.2002.2457_3.x. [DOI] [PubMed] [Google Scholar]
- 14.Agarwal A, Dhiraaj S, Pawar S, Kapoor R, Gupta D, Singh PK. An evaluation of the efficacy of gabapentin for prevention of catheter-related bladder discomfort: A prospective, randomized, placebo-controlled, double-blind study. Anesth Analg. 2007;105:1454–7. doi: 10.1213/01.ane.0000281154.03887.2b. [DOI] [PubMed] [Google Scholar]
- 15.Peter S, David AL, Matthew DM. Intravenouse anesthetics. In: Miller RD, editor. Miller's Anesthesia. 7th ed. Philadelphia, PA: Churchill Livingstone; 2010. pp. 742–7. [Google Scholar]
- 16.Agarwal A, Gupta D, Kumar M, Dhiraaj S, Tandon M, Singh PK. Ketamine for treatment of catheter related bladder discomfort: A prospective, randomized, placebo controlled and double blind study. Br J Anaesth. 2006;96:587–9. doi: 10.1093/bja/ael048. [DOI] [PubMed] [Google Scholar]
- 17.Kohrs R, Durieux ME. Ketamine: Teaching an old drug new tricks. Anesth Analg. 1998;87:1186–93. doi: 10.1097/00000539-199811000-00039. [DOI] [PubMed] [Google Scholar]
- 18.Wilson LE, Hatch DJ, Rehder K. Mechanisms of the relaxant action of ketamine on isolated porcine trachealis muscle. Br J Anaesth. 1993;71:544–50. doi: 10.1093/bja/71.4.544. [DOI] [PubMed] [Google Scholar]
- 19.Durieux ME. Inhibition by ketamine of muscarinic acetylcholine receptor function. Anesth Analg. 1995;81:57–62. doi: 10.1097/00000539-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Park JM, Houck CS, Sethna NF, Sullivan LJ, Atala A, Borer JG, et al. Ketorolac suppresses postoperative bladder spasms after pediatric ureteral reimplantation. Anesth Analg. 2000;91:11–5. doi: 10.1097/00000539-200007000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Weinbroum AA. A single small dose of postoperative ketamine provides rapid and sustained improvement in morphine analgesia in the presence of morphine-resistant pain. Anesth Analg. 2003;96:789–95. doi: 10.1213/01.ANE.0000048088.17761.B4. [DOI] [PubMed] [Google Scholar]


