Abstract
Introduction:
“Primum non nocere” (first do no harm): Hippocrates (c. 460 BC-377 BC). Wrong site surgery is the fourth commonest sentinel event after patient suicide, operative and post-operative complications, and medication errors. Misinterpretation of the clinic letters or radiology reports is the commonest reason for the wrong site being marked before surgery.
Materials and Methods:
We analyzed 50 cases each of operations carried out on the kidney, ureter, and the testis. The side mentioned on clinic letters, the consent form, and radiology reports lists were also studied. The results were analyzed in detail to determine where the potential pitfalls were likely to arise.
Results:
A total of 803 clinic letters from 150 cases were reviewed. The side of disease was not documented in 8.71% and five patients had the wrong side mentioned in one of their clinic letters. In the radiology reports, the side was not mentioned in three cases and it was reported wrongly in two patients. No wrong side was ever consented for and no wrong side surgery was performed.
Conclusion:
The side of surgery was not always indicated in clinic letter, theatre list, or the consent form despite the procedure being carried on a bilateral organ. As misinterpretation is a major cause of wrong side surgery, it is prudent that the side is mentioned every time in every clinic letter, consent form, and on the theatre list. The WHO surgical safety checklist has already been very effective in minimizing the wrong site surgery in the National Health Service.
Keywords: Safety, universal protocol, urology, WHO checklist, wrong site surgery
INTRODUCTION
Wrong site surgery is a broad term that encompasses surgery performed on the wrong body part, wrong side of the body, wrong patient, or at the wrong level of the correctly identified anatomical side. In 2001, Joint Commission on Accreditation of Healthcare Organisation (JCAHO) Sentinel Event Alert Issue 24 cited 126 wrong site surgery cases. Although no specialty predominates, no specialty is immune from performing wrong side operations. 41% in orthopedics and podiatric surgery; 20% to general surgery; 14% to neurosurgery; 11% to urology surgery; and the rest to specialties including dental/oral maxillofacial; cardiovascular/thoracic; ear, nose, and throat; and ophthalmologic surgery.[1] The deformity of a broken long bone is obvious from outside but the diseases that affect the paired urological organs are concealed in body cavities, escalating the risk of wrong side surgery that necessitates the need of strict protocols to prevent this mishap from occurring. The event that resulted in wrong kidney being removed has once again caught the world's attention on wrong side surgery.[2,3]
In 2008, WHO launched mandatory Global Patient Safety Challenge, “Safe Surgery Saves Lives.” The checklist has three components: Sign in (before induction of anesthesia), time-out (after induction and before surgical incision), and sign out (during or immediately after wound closure but before removing the patient from the operating room) [Figure 1].[4] In England and Wales, 129,419 incidents relating to surgical specialties were reported to the National Reporting and Learning Service with a range of degrees of harm, including 271 deaths. In-line with WHO safety checklist, National Patient Safety Agency introduced a safety checklist alert in 2009. The organizations are required to: (a) ensure an executive and a clinical lead to implement the surgical safety checklist within the organization. (b) ensure the checklist is completed for every patient undergoing a surgical procedure (including local anesthesia). (c) ensure that the use of the checklist is entered in the clinical notes or electronic record by a registered member of the team.[5]
Figure 1.

The WHO surgical safety checklist
We aimed to find from our study whether the side of the disease process is always mentioned in all notes, any mistakes of side mentioning, and its impact on patient management.
MATERIALS AND METHODS
A retrospective review of 150 case records of patients who have had surgery on their kidney, ureter, and testis (50 cases each). Basic demographics data and following details were collected from the case file.
Which side was the primary disease?
Was the side mentioned every time the organ was mentioned?
At any time was the wrong side mentioned?
If there was a wrong side mentioned, was it rectified?
Did mentioning of the wrong side affect the patient safety?
Did not mentioning the side affect the patient safety?
Did the imaging study mention the correct side?
RESULTS
A total of 150 case files were reviewed. Of the 385 clinic letters belonging to 50 patients who had undergone investigations and operations for renal problems, 6.23% of the letters did not mention the side of the pathology [Table 1]. In three patients, wrong side was mentioned in the clinic letters. Out of these three, in one patient, the wrong side was continued to the next clinic letter. In two of the radiology reports, the side of the pathology or intervention was not mentioned, but it is important to note that the radiologists did not report the wrong side of renal pathology. No wrong side surgery was performed.
Table 1.
Interventions on kidney, ureter and testis
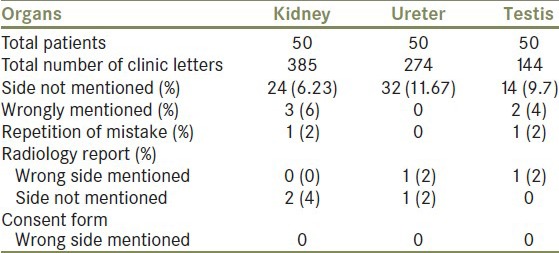
In 50 patients (274 clinic letters) who had undergone interventions on their ureter, 11.67% did not mention the side [Table 1]. However, no wrong side was mentioned in any of the clinic letters. A patient with bilateral ureteric stent placement had only one stent removed after 6 weeks. The other stent was overlooked for 1 year before removal. Root cause analysis revealed that the admission card for this patient mentioned “flexible cystoscopy and removal of ureteric double J stent.” In one radiological report, side of intervention was not mentioned and in another, wrong side of the disease was mentioned. No wrong side surgery was performed on any of these patients.
Of the 144 clinic letters belonging to patients who have had testicular procedures, 9.7% of the clinic letters did not mention the side [Table 1]. Of the two clinic letters that mentioned the procedure wrongly, it was repeated in one letter. In one radiological report, the side of pathology was reported wrongly. No wrong side surgery was performed in the reviewed case files.
A total of 803 clinic letters were reviewed from 150 patients, of which 8.71% of the clinic letters did not mention the side of the disease [Table 2]. A total of five patients had the wrong side mentioned in one of their clinic letters. Out of these, it was repeated twice. In three patients, the side of pathology was not mentioned by the radiologist and it was reported wrongly in two patients. No wrong side was ever consented for and was operated on.
Table 2.
Interventions in all cases

DISCUSSION
Wrong side surgery is probably the most dramatic, visible, and devastating of all surgical errors. It is arguably the error that is feared by most surgeons. If we study the events that led to removal of wrong kidney in the UK, it is evident that multiple factors led to the confusion, and these factors could have been prevented. This started with the house-officer indicated, the wrong side on the admission slip. This misinformation was then transferred on to the surgeon's diary. Though the patient was consented correctly by another junior doctor at the time of pre-assessment, no one rechecked the consent form or marked the side of surgery on the day of procedure. The imaging studies were also not reviewed in the ward. The X-rays were misinterpreted by the operating team. There were two instances which were again not seriously considered. The operating surgeon entered the theatre room with the intention of removing the correct kidney (right side) but was misled by the scrub nurse that the theatre list indicated the contralateral kidney (left side). The surgeon proceeded to operate on the left kidney having no reason to doubt details mentioned on the theatre list. A medical student had warned the surgeon that the wrong side was being operated upon on reviewing the X-rays. Taking some “time-out” to seriously looking into both these instances could have avoided the mistake of wrong side surgery.[3,6]
Another finding of our study was that even though the wrong side operation was not performed, there are many instances wherein the side was not mentioned at all. This practice of omission of the side could potentially be the start of chain of events that may lead to a catastrophic event. With each mistake in a clinic letter or radiology report, there is a potential chance that it could happen in subsequent documentation and could be perpetuated to theatre, leading to wrong side surgery. Failure of removal of both ureteric stents in our series highlights the fact that mentioning “bilateral” on the admission card could have avoided the error. Zhao et al. and Rooney et al. reviewed the available evidence and concluded that surgical site marking does not affect the sterility of the surgical field.[7,8]
Wrong side surgery. Is it being reported?
There are surprisingly few peer-reviewed papers on the subject of wrong-sided surgery in the medical literature. In this era of “universal protocol,” Stahel et al. analyzed the physician insurance database for self-reported adverse events and identified 25 wrong patient and 107 wrong site procedures. One patient died secondary to a wrong site procedure and significant harm was inflicted in 20% wrong patient procedures and 35% wrong site procedures. Common causes for wrong site procedures were errors in judgment (85.0%) and the lack of performing a “time-out” (72.0%). They recommend strict adherence to the universal protocol and this must be expanded to non-surgical specialties.[9]
Why is there under-reporting of such incidents?
The most likely reason would be the “Culture of blame.” The society, media, and the medical society have always tended to name, blame, and shame the person at fault. Healthcare personnel have, therefore, been quite understandably concerned about personal consequences. There is a natural reluctance in junior member of the staff to openly question their senior's actions. Factors that are involved may be respect and fear. Respect for the seniors authority and experience can be excessive or on the other hand fear of unleashing the senior's wrath. Personality conflicts either between junior staff and consultants or between consultants greatly increase the risk of error.
The second reason is such incidences are “Tedious to report” and the belief that no action will be taken even if it were to be reported. In the National Health Service in the United Kingdom, every hospital has a “Critical incidence report” book where in misses and near misses can be entered without the fear of being named. These data are collected and analyzed to find out a solution for a particular problem rather than to blame a particular person.
The JCAHO which collects the sentinel events of medical errors has shown that majority of the information comes from self-reporting by the responsible institution. However, significant numbers do come from media and other sources such as law firms and court hearings.[10]
What are the factors that can contribute to medical errors?
Environmental factors
Distractions, noise, ergonomics, precautions, clutter, and interruptions are the major environmental factors identified in contributing to medical errors in general. In an elegant study, Undre et al. showed that the operating theatre environment is not as cohesive as it is previously assumed.[11] Further studies from the same group on observational teamwork assessment for surgery when applied to Urological surgery revealed interesting results. They found that a number of communication and equipment/provision tasks were not routinely performed during the operations. Anesthetists and nurses obtained the lowest score on communication when they assessed teamwork-related behavior.[12] They have also elaborated on the distraction that is often present in the urology operating theatre.[13]
Cima et al. reported 759 (1.38%) listing errors from surgical listing data. No wrong site surgeries occurred but the common adverse events were missing laterality (66%) and incorrect side (14%); common areas of identification/correction of the listing error were pre-operative nursing review (68%), pre-operative admission unit (17%), operating room (12%), recovery room (0.8%), and other (0.8%). So they recommended an electronic listing system using standardized case descriptions with required laterality to reduce these adverse events.[14]
Human factors
Human error is an inherent part of human behavior and cannot be completely eliminated. Certain factors may pre-dispose to increased frequency of human error in surgery, such as fatigue, which is common in surgeons and has been shown to increase error. Time pressures, especially in an emergency setting, may be another important factor for wrong side surgery. Dealing with multiple patients and working in a multi-surgical team may also contribute to errors.[15,16] Another major factor that has been seen more than often is the imperfect communication between the team members especially in the operating room.[17]
A literature review over 20 year period by Braaf et al. concluded that effective communication among healthcare professionals is vital to the delivery of safe patient care and failure in communication contributes to the cascade of events that result in compromised patient safety and potentially adverse patient outcomes.[18] More effective communication between different members of the operating theatre could be improved by multi-disciplinary crisis simulation.[12] Similarly, Medical Misadventure Unit investigating the causes of wrong site surgery (25 cases) in New Zealand found that 20% were due to a surgeon misinterpreting a referral letter or radiology report. 16% of errors were due to a surgeon identifying the wrong site during surgery, with a further 16% due to the wrong site of a patient being marked before surgery. There are suggestions that the personality of certain individuals with the framework of a team may be the responsible element.[19]
Patient factors
It is being increasingly recognized that involvement of the patient in marking the side of surgery can decrease the incidence of wrong side, wrong person, and wrong operations being performed. However, many factors of the patient such as behavioral issues, language barrier, compliance, knowledge deficit, fear, and disease acuity have been responsible for medical errors to occur. Improper communication tops the list of JCAHO reported factors for wrong side surgery.[20,21]
How do we approach this problem?
The modern approach to patient safety and prevention of error focuses on a systems approach as opposed to human error.[22] If systems are in place that make it impossible for human error to reach the patient and cause harm, patient safety will be markedly improved.[23]
How can we manage errors?
Avoid errors
Stop errors from happening. Stringent following of protocols and guidelines with no exceptions of deviation can prevent from errors being committed.
Trap errors
Identify errors when they do happen. This is the most important process of learning to avoid making an error. Learn from the mistake that has taken place and reinforce safety guidelines to prevent further repetition of such errors.
Manage errors
Reduce the effect of errors that are not caught. Incident reporting of near misses and analyzing the pitfalls in the system will also prevent a future catastrophe. The no blame culture may encourage more reporting of these adverse events or near misses.
As shown by our study, minor errors such as omitting to mention the side in the patient's documentation early in a patient's management can compound and potentially lead to a disaster. The essential points in risk reduction are good protocols, good notes, and good communication. Good teamwork and the deletion of unnecessary paperwork may also be of added benefit.
How can we prevent wrong side surgery?
Develop protocols and guidelines
The first priority in a clinical setting is to develop and implement a mandatory protocol and guidelines for the identification and verification of the correct surgical side. Development of a protocol should be a collaborative effort including surgical, anesthesia, nursing staff, theatre staff, and patient support group members. Correct side protocols and guidelines must include clear and specific instructions that leave no room for varied interpretations. Knight et al. showed that use of an anatomic marking form over 4.5 years as an alternative to the universal protocol can be effective in preventing wrong site, wrong procedure, and wrong person surgery.[24]
As a physician, it is our responsibility that we mention the side whenever a bilateral organ in every clinic letter or documentation that is written. Before a patient is taken to theatre, in the ward, the operating surgeon or the consultant in-charge should be the only person marking the side of the surgery. The surgeon should confirm the correct side with the clinic letter, consent form, theatre list, imaging studies, and also most importantly with the patient. The mark should be made by an indelible, hypoallergenic, latex-free skin marker and mark may be the initials of the surgeon. In 1997, the American Academy of Orthopaedic Surgeons (AAOS) appointed a task force on wrong site surgery to develop recommendations regarding methods for its prevention. The report of the task force on wrong site surgery was approved by the Academy's Board of Directors, and the AAOS issued an advisory statement entitled “Sign Your Site” in 1997. They recommended that the operating surgeon is responsible to put their initials on the respective site and side.[25] The surgeon should again confirm the side to be operated upon in the theatre before positioning the patient.
In the UK, both The Royal College of Surgeons of England and The Royal College of Surgeons of Edinburgh have provided guidelines reminding surgeons that they are operating on the correct patient, for the correct diagnosis, correct side, and the consent form is correct.[26] As a patient, they should actively take part in the every decision of their health care. They should verify the information on the identity bracelet and alert a member of the health care team if the information is incorrect and insist that it should be replaced immediately. They should ensure that the correct side is mentioned on the consent form. On the day of surgery, they should ensure that the operating surgeon rechecks the side of the surgery and puts his initials on the side of the surgery. They should not hesitate to ask questions and speak up if you have any concerns. The policy that “if verification does not occur, the procedure should not occur” should be implemented to foolproof the system. There are many protocols developed by institutions and organizations for verification of the side of surgery like American College of Surgeons Board's “Correct patient, correct site and correct procedure surgery” and JCAHO's universal protocol.[27]
CONCLUSION
Wrong side surgery is a devastating catastrophe not only for the patient and their family but also for the physician and the institution. It is totally preventable and performing operation on the wrong side is both legally and ethically indefensible. Prevention cannot be the responsibility of one single individual and has to be a collective responsibility of the entire team looking after the patient. Emphasis should also be placed on patient involvement. Physicians have to mention the side correctly whenever a bilateral organ is involved. It is prudent for us to use such simple measures as small mistakes or series of omissions lead to a major disaster.
A sentinel, catastrophic event that could be detrimental to both the patient's life and the surgeon's career, occurs due to a series of “fateful chain of events.” The cause of failure to operate on the correct side is often multi-factorial and should be prevented by a stringent “foolproof” checklist that should be made mandatory. The WHO surgical safety checklist is mandatory in majority of hospitals around the globe and this has been very effective in minimizing the wrong site surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.A follow-up review of wrong site surgery. Jt Comm Perspect. 2002;22:10–1. [PubMed] [Google Scholar]
- 2.Dobson R. College begins inquiry into removal of wrong kidney. BMJ. 2000;320:332. [PubMed] [Google Scholar]
- 3.Crumlin: 2008. [Last accessed on 2011 Jan 26]. Investigation into the removal of the wrong kidney from a patient (October 2008) Available from: https://docs.google.com/viewer?url=http%3A%2F%2Fwww.stateclaims.ie%2FClinicalIndemnityScheme%2Fpublications%2F2009%2FOLHSC.pdf . [Google Scholar]
- 4.Mahajan RP. The WHO surgical checklist. Best Pract Res Clin Anaesthesiol. 2011;25:161–8. doi: 10.1016/j.bpa.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Panesar SS, Cleary K, Sheikh A, Donaldson L. The WHO checklist: A global tool to prevent errors in surgery. Patient Saf Surg. 2009;3:9. doi: 10.1186/1754-9493-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dyer O. Doctors suspended for removing wrong kidney. BMJ. 2004;328:246. doi: 10.1136/bmj.328.7434.246-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao X, Chen J, Fang XQ, Fan SW. Surgical site marking will not affect sterility of the surgical field. Med Hypotheses. 2009;73:319–20. doi: 10.1016/j.mehy.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 8.Rooney J, Khoo OK, Higgs AR, Small TJ, Bell S. Surgical site marking does not affect sterility. ANZ J Surg. 2008;78:688–9. doi: 10.1111/j.1445-2197.2008.04618.x. [DOI] [PubMed] [Google Scholar]
- 9.Stahel PF, Sabel AL, Victoroff MS, Varnell J, Lembitz A, Boyle DJ, et al. Wrong-site and wrong-patient procedures in the universal protocol era: Analysis of a prospective database of physician self-reported occurrences. Arch Surg. 2010;145:978–84. doi: 10.1001/archsurg.2010.185. [DOI] [PubMed] [Google Scholar]
- 10.New Joint Commission center to take on wrong-site surgery. OR Manager. 2009;25:1–6. [PubMed] [Google Scholar]
- 11.Undre S, Sevdalis N, Healey AN, Darzi S, Vincent CA. Teamwork in the operating theatre: Cohesion or confusion? J Eval Clin Pract. 2006;12:182–9. doi: 10.1111/j.1365-2753.2006.00614.x. [DOI] [PubMed] [Google Scholar]
- 12.Undre S, Koutantji M, Sevdalis N, Gautama S, Selvapatt N, Williams S, et al. Multidisciplinary crisis simulations: The way forward for training surgical teams. World J Surg. 2007;31:1843–53. doi: 10.1007/s00268-007-9128-x. [DOI] [PubMed] [Google Scholar]
- 13.Primus CP, Healey AN, Undre S. Distraction in the urology operating theatre. BJU Int. 2007;99:493–4. doi: 10.1111/j.1464-410X.2007.06573.x. [DOI] [PubMed] [Google Scholar]
- 14.Cima RR, Hale C, Kollengode A, Rogers JC, Cassivi SD, Deschamps C. Surgical case listing accuracy: Failure analysis at a high-volume academic medical center. Arch Surg. 2010;145:641–6. doi: 10.1001/archsurg.2010.112. [DOI] [PubMed] [Google Scholar]
- 15.Boutros F, Redelmeier DA. Effects of trauma cases on the care of patients who have chest pain in an emergency department. J Trauma. 2000;48:649–53. doi: 10.1097/00005373-200004000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Flynn EA, Barker KN, Gibson JT, Pearson RE, Berger BA, Smith LA. Impact of interruptions and distractions on dispensing errors in an ambulatory care pharmacy. Am J Health Syst Pharm. 1999;56:1319–25. doi: 10.1093/ajhp/56.13.1319. [DOI] [PubMed] [Google Scholar]
- 17.Lingard L, Reznick R, Espin S, Regehr G, DeVito I. Team communications in the operating room: Talk patterns, sites of tension, and implications for novices. Acad Med. 2002;77:232–7. doi: 10.1097/00001888-200203000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Braaf S, Manias E, Riley R. The role of documents and documentation in communication failure across the perioperative pathway. A literature review. Int J Nurs Stud. 2011;48:1024–38. doi: 10.1016/j.ijnurstu.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 19.Senders JW, Kanzki R. The egocentric surgeon or the roots of wrong side surgery. Qual Saf Health Care. 2008;17:396–400. doi: 10.1136/qshc.2007.023564. [DOI] [PubMed] [Google Scholar]
- 20.JCAHO protocol to prevent wrong-site surgery is endorsed. Qual Lett Healthc Lead. 2004;16:13. [PubMed] [Google Scholar]
- 21.Mulloy DF, Hughes RG. Wrong-site surgery: A preventable medical error. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville: Agency for Healthcare Research and Quality; 2008. p. 381. [PubMed] [Google Scholar]
- 22.Bernstein M. Surgical teaching: How should neurosurgeons handle the conflict of duty to today's patients with the duty to tomorrow's? Br J Neurosurg. 2003;17:121–3. doi: 10.1080/0268869031000108981. [DOI] [PubMed] [Google Scholar]
- 23.Bernstein M. Wrong-side surgery: Systems for prevention. Can J Surg. 2003;46:144–6. [PMC free article] [PubMed] [Google Scholar]
- 24.Knight N, Aucar J. Use of an anatomic marking form as an alternative to the universal protocol for preventing wrong site, wrong procedure and wrong person surgery. Am J Surg. 2010;200:803–7. doi: 10.1016/j.amjsurg.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 25.Cowell HR. Wrong-site surgery. J Bone Joint Surg Am. 1998;80:463. doi: 10.2106/00004623-199804000-00001. [DOI] [PubMed] [Google Scholar]
- 26. [Last accessed on 2012 Mar 10]. Available from: http://www.rcseng.ac.uk/publications/docs/good-surgical-practice-1 .
- 27.Statement on ensuring correct patient, correct site, and correct procedure surgery. Bull Am Coll Surg. 2002;87:26. [PubMed] [Google Scholar]


