Abstract
Circumcision is one of the oldest and most commonly performed surgical procedures. Unfortunately, various complications may occur during circumcision, ranging from trivial to tragic such as penile amputation which is a serious complication and a challenging injury to treat. We describe two cases of non-microsurgical successful reattachment of a distal penile glans which were amputated during circumcision. In the first case, a 5-year-old child underwent circumcision by an urologist under local anesthesia. In the second one, a 3-year-old child underwent circumcision by a general practitioner who used to make circumcision. In this article, the literature is reviewed; results and potential complications of this surgery are also discussed. Glans sensation was present, early morning erection was maintained, and there was an erectile response during penile manipulation in both cases. Although circumcision is not technically difficult, it should be taken seriously. The use of microsurgical reattachment is not always possible, especially in pediatric cases; it also requires special equipment and training.
Keywords: Circumcision, penile amputation, reconstructive surgical procedures, wounds and injuries
INTRODUCTION
Traumatic amputation of the penis is an uncommon emergency and requires immediate replantation.[1] In pediatric population, penile trauma has been reported infrequently after circumcision and has shown high rate of success.[2]
In this article, we describe two cases of successful reattachment of a distal penile glans, which were amputated during ritual circumcision, with review of the literature.
MATERIALS AND METHODS
Between 2009 and 2011, we observed two pediatric cases of penile amputation which followed a ritual circumcision. In the first case, a 5-year-old child underwent circumcision by an urologist under local anesthesia. In the second one, a 3-year-old child underwent circumcision by a general practitioner who used to make circumcision. The same technique for circumcision is used: The foreskin is pulled and clamped just distal to the tip of the glans and is excised between the glans and the clamp. In our cases, the glans was inadvertently caught in the clamp.
It was immediately recognized that half of the penile glans had been amputated in the first case [Figure 1a] and in the second one, the entire glans had been amputated and the corpora cavernosa were sectioned at their distal part [Figure 1b]. In both cases, the urethra was sectioned as well. To stop the bleeding, a compressive dressing was applied on the proximal part of the penis and the excised tissue was placed in a plastic bag and stored on an ice saline solution bath to be transported to our medical center. Approximate time from amputation to surgical reattachment was half an hour in the first case and about 2 hours in the second one. Examination in the operation room revealed a viable penis with partial shaft skin loss, and clean excision of the foreskin in both cases.
Figure 1.
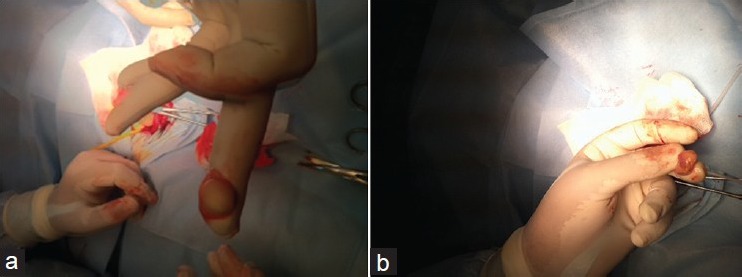
(a) Case 1 at presentation: Clean excision of the foreskin and distal third of the glans. (b) Case 2 at presentation: Clean excision of all the glans
The same technique of reattachment was applied in both cases: The cut surfaces were cleaned with sterile saline, an 8-Fr Foley catheter was inserted through the urethra of the amputated part and the proximal urethral stump; the urethra and the underlying corpus spongiosum were anastomosed with a single layer of interrupted sutures Vicryl 4/0 over the Foley catheter [Figure 2a and b]. In the first case, the corpus cavernosum was not affected, while in the second one, the tunica albuginea of the corpus cavernosum was reanastomosed using interrupted sutures Vicryl 5/0. The fascial layer and skin were reapproximated with interrupted 4-0 Vicryl sutures. The graft returned to normal pink color in a few minutes [Figure 3a and b]. A dressing was placed around the glans to keep the penis immobilized.
Figure 2.
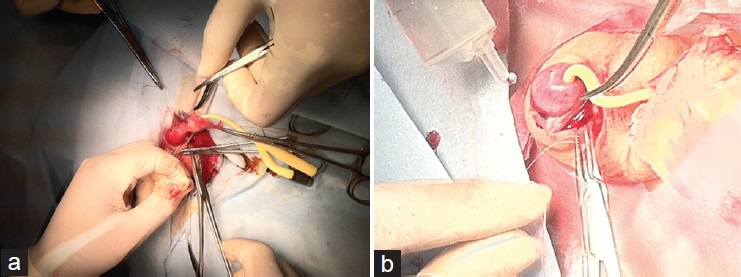
Steps of the procedure. (a, b) Urethral mucosa anastomosis formed end-to-end with interrupted sutures over the Foley catheter
Figure 3.
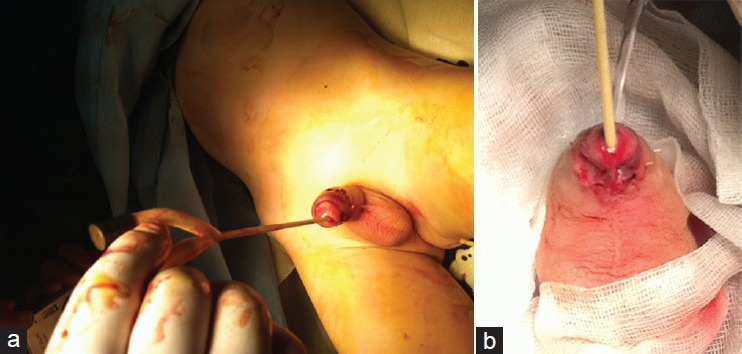
Immediate result after surgery: (a) case 1 (b) case 2
Prophylactic low-molecular-weight heparins, intravenous gentamicin and cefotaxime were given for 10 days.
RESULTS
In the first case, a thin eschar was formed around the meatus on the glans penis after 3 days, which required debridement and was peeled off after 2 weeks, leaving appropriate glans tissue.
In the second case, eschar around the meatus remained for 3 weeks postoperatively.
In both cases, the urethral stent was removed after 3 weeks.
After 2 years for the first case and 13 months for the second one, we noticed that penile cosmesis was good, glans sensation was present, and early morning erection was maintained for both cases. No stricture or fistula has been noted until now [Figure 4a and b].
Figure 4.
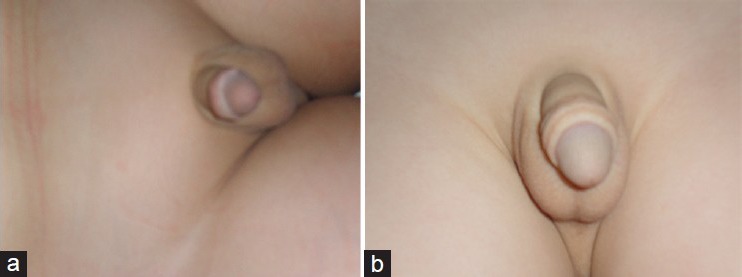
Result of the surgery: (a) after 2 years of follow-up and (b) after 16 months of follow-up
DISCUSSION
Penile trauma during circumcision has been reported more frequently, with varying degrees of severity ranging from skin or meatal injury, partial glanular amputation to total penile amputation.[3]
Witswell and Geschke reviewed the records of 136,086 circumcised boys and reported an overall complication rate of 0.19%.[4]
The fairly high rate (1.5-15%), with more serious complications, is reported when the procedure is often performed by an inexperienced individual without attention to basic surgical principles often in a traditional setting or when poor surgical technique is used.[5] Partial glans removal has been reported to occur with the use of clamp techniques.[6] With this technique, amputation can occur if the operator inadvertently catches the glans in the clamp, as in our case. Carrying out circumcision under local anesthesia as in our case or without anesthesia or by unqualified village barbers like in many Muslim countries is very dangerous and can cause many serious complications such as penile amputation. In these countries, we suggest to devote some days in every hospitals for free circumcisions to encourage people to do it in a more secure way.
Bahnasawy and El-Sherbiny[3] reported the largest series of penile trauma in the pediatric population; 64 boys with penile trauma were hospitalized over 20 years and 43 (67%) were caused by circumcision.
Ehrich reported the first case of replantation of an amputated penis in 1929.[7] The initial form of replantation was based on approximation of major penile structures without attention to nerve or blood vessel anastomosis.
Replantation of a severed penis without reestablishing the arterial blood site is a form of graft. As a graft, it should first survive by imbibitions, obtaining nutrients from the adjacent graft bed by diffusion.[8] Because the dorsal and urethral arteries represent an excellent source of vascularity to the glans and corpora spongiosum,[9] we anastomosed the urethra and tunica albuginea. The immobilization with a bulky dressing is important to allow imbibition and inosculation.[5] The goal of our technique was to position the amputated part of the glans on its proximal part over a urethral catheter and to try to keep the graft immobilized with dressings.
The development of microsurgical techniques has improved the rate of success with regard to penile replantation.[5] The first cases were independently reported in 1977 by Cohen et al.[10] In pediatric cases, it is not always possible to identify deep dorsal arteries, veins, or nerves to anastomose.[8] However, such techniques require special equipment, instruments, and training, which are not always available.
Efforts have been made therefore to develop a simple and standard technique of management that could be performed by any urologist.
CONCLUSION
Multiple complications can occur after circumcision, ranging from the insignificant to the tragic. Virtually all of these complications are preventable with only a modicum of care.
The use of microsurgical reattachment is not always possible, especially in pediatric cases; it also requires special equipment and training.
ACKNOWLEDGMENTS
We are grateful to Dr. Ben Sorba Nebil, Dr. Jaidane Mehdi, and Pr Mosbah Faouzi for their comments on the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None
REFERENCES
- 1.Charlesworth P, Campbell A, Kamaledeen S, Joshi A. Surgical repair of traumatic amputation of the glans. Urology. 2011;77(Suppl 6):1472–3. doi: 10.1016/j.urology.2010.08.034. [DOI] [PubMed] [Google Scholar]
- 2.Roche NA, Vermeulen BT, Blondeel PN, Stillaert FB. Technical recommendations for penile replantation based on lessons learned from penile reconstruction. J Reconstr Microsurg. 2012;28:247–50. doi: 10.1055/s-0032-1306373. [DOI] [PubMed] [Google Scholar]
- 3.El-Bahnasawy MS, El-Sherbiny MT. Paediatric penile trauma. BJU Int. 2002;90(Suppl 1):92–6. doi: 10.1046/j.1464-410x.2002.02741.x. [DOI] [PubMed] [Google Scholar]
- 4.Wiswell TE, Geschke DW. Risks from circumcision during the first month of life compared with those for uncircumcised boys. Pediatrics. 1989;83(Suppl 6):1011–5. [PubMed] [Google Scholar]
- 5.Hashem FK, Ahmed S, al-Malaq AA, Abu Daia JM. Successful replantation of penile amputation (post-circumcision) complicated by prolonged ischaemia. Br J Plast Surg. 1999;52(Suppl 4):308–10. doi: 10.1054/bjps.1999.3097. [DOI] [PubMed] [Google Scholar]
- 6.Faydaci G, Uğur K, Osman C, Sermin S, Bilal E. Amputation of glans penis: A rare circumcision complication and successful management with primary anastomosis and hyperbaric oxygen therapy. Korean J Urol. 2011;52(Suppl 2):147–9. doi: 10.4111/kju.2011.52.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ehrich WS. Two unusual penile injuries. J Urol. 1929;21:239. [Google Scholar]
- 8.Jezior JR, Brady JD, Schlossberg SM. Management of penile amputation injuries. World J Surg. 2001;12:1602–9. doi: 10.1007/s00268-001-0157-6. [DOI] [PubMed] [Google Scholar]
- 9.Jong KP, Jun KKM, Hyung JK. Reimplantation of an amputated penis in prepubertal boys. J Urol. 2001;165:586–7. doi: 10.1097/00005392-200102000-00076. [DOI] [PubMed] [Google Scholar]
- 10.Cohen BE, May JW, Daly JS, Young HH. Successful clinical replantation of an amputated penis by microneurovascular repair. Plast Reconstr Surg. 1977;59:276–80. [PubMed] [Google Scholar]


