Abstract
Introduction
Inequalities are evident in early childhood caries rates with the socially disadvantaged experiencing greater burden of disease. This study builds on formative qualitative research, conducted in the Moreland/Hume local government areas of Melbourne, Victoria 2006–2009, in response to community concerns for oral health of children from refugee and migrant backgrounds. Development of the community-based intervention described here extends the partnership approach to cogeneration of contemporary evidence with continued and meaningful involvement of investigators, community, cultural and government partners. This trial aims to establish a model for child oral health promotion for culturally diverse communities in Australia.
Methods and analysis
This is an exploratory trial implementing a community-based child oral health promotion intervention for Australian families from refugee and migrant backgrounds. Families from an Iraqi, Lebanese or Pakistani background with children aged 1–4 years, residing in metropolitan Melbourne, were invited to participate in the trial by peer educators from their respective communities using snowball and purposive sampling techniques. Target sample size was 600. Moreland, a culturally diverse, inner-urban metropolitan area of Melbourne, was chosen as the intervention site. The intervention comprised peer educator led community oral health education sessions and reorienting of dental health and family services through cultural Competency Organisational Review (CORe).
Ethics and dissemination
Ethics approval for this trial was granted by the University of Melbourne Human Research Ethics Committee and the Department of Education and Early Childhood Development Research Committee. Study progress and output will be disseminated via periodic newsletters, peer-reviewed research papers, reports, community seminars and at National and International conferences.
Trial registration number
Australian New Zealand Clinical Trials Registry (ACTRN12611000532909).
Keywords: PUBLIC HEALTH, ORAL HEALTH, CULTURAL COMPETENCY, INEQUALITIES, CHILD, COMMUNITY-BASED PARTICIPATORY RESEARCH
Strengths and limitations of this study.
A culturally competent community-based participatory research process adopted to help build a relationship of trust and partnership between the researchers and communities involved and to maximise the acceptability of the programme and the uptake of research findings.
Study design and methods developed from initial community research and then piloted in a similar community context.
Study design adapted to ensure relevance and applicability to cultural networks and service delivery considerations.
Use of peer educators to increase the cultural appropriateness and accessibility of the intervention.
Non-random allocation of participants to the intervention introduces a potential source of bias.
Background
Early childhood caries (ECC) is a particularly aggressive form of the disease and is characterised by rampant decay in the teeth of infants and young children. In 2006, 41% of Australian 4-year-olds had dental caries, with two teeth per child, on average, having caries to the point of cavitation (dmft=1.94).1 ECC left untreated can lead to pain, infection, abscesses and hospitalisation.2 Recent Australian data indicate that among preschool children, dental caries is the primary cause of hospitalisation for oral healthcare.3 Adverse effects of dental caries include: poor self-image and self-esteem, reduced social interaction, problems in developing permanent dentition and chronic stress and depression.4 ECC can also impair the quality of life of children by interfering with vital functions of daily living such as food selection, eating, swallowing, speaking and social interactions, as well as incurring great financial cost.4 5
Social inequalities are evident in ECC rates with the socially and economically disadvantaged having the greater burden of disease.6 7 A recent report on the oral health of Australian children aged 2–3 years indicated that those children experiencing social disadvantage were 3.29 times more likely to have an oral health problem compared to the least disadvantaged children.8 This highlights ECC as a potential risk for children from refugee and migrant backgrounds as their families are documented, in most cases, to be more socially disadvantaged and have poorer oral health compared to the parent population of the country they migrate to, assuming migration is to a more developed country.9–11 Such a scenario has been observed in Australia among children who are non-English speaking refugees.12 In Victoria, refugee and asylum seekers are considered a priority group and publically funded dental services are made more accessible to these communities by reducing costs and wait times. However, many of these communities still do not access services.
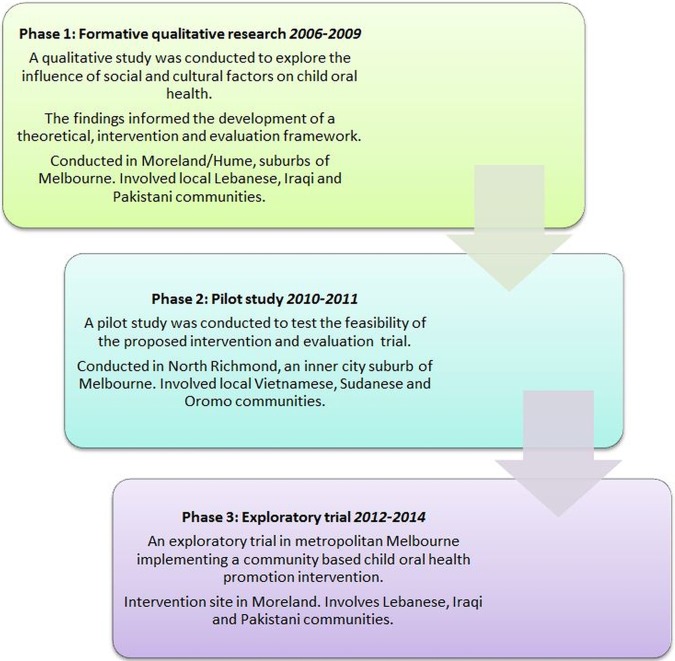
This paper presents the study protocol for the third phase of Teeth Tales, an exploratory trial implementing a community-based child oral health promotion intervention for Australian families from refugee and migrant backgrounds. The trial builds on the formative qualitative research conducted in the first phase of Teeth Tales from 2006 to 2009 in response to community concerns for the oral health of children from refugee and migrant backgrounds residing in the Moreland and Hume local government areas (LGAs) of Melbourne (figure 1). The qualitative research involved people from Iraqi, Lebanese and Pakistani communities, identified as migrant and refugee groups with a high representation of young families in the LGA of Moreland, an urban area of Melbourne, Australia.13 They also represent a mix of migration histories and time since arrival including predominantly humanitarian and family reconnection migration (Lebanese—first, second and third generation and Iraqi—first and second generation) versus skilled migration (Pakistani—first generation). This formative research was undertaken by the University of Melbourne and Merri Community Health Services in partnership with Dental Health Services Victoria (DHSV), Arabic Welfare, Victorian Arabic Social Services and representatives of the Pakistani community, and Moreland City Council. Community leaders, parents, grandparents and representatives from cultural organisations representing the Iraqi, Lebanese and Pakistani communities, participated in a series of semistructured focus groups and interviews to explore the social, cultural and environmental influences of poor child oral health in these communities. The findings identified cultural impacts on oral health beliefs, behaviours and knowledge such as avoidance of tap water due to experience of unsafe drinking water in home countries, lack of knowledge of water fluoridation; and frequent consumption of high sugar, high fat foods and drinks which were considered ‘luxury items’ in their homeland and therefore were not a regular part of the diet. Use of traditional oral health practices including the miswak chewing stick by the Muslim community was found to be a common practice to prevent poor dental health14; but miswak use did not begin until children started school meaning there was little or no oral hygiene in the preschool years. In Victoria, early oral health prevention, support and treatment programmes and services are available such as, The Smiles4Miles programme, an oral health promotion programme for young children. However, this programme was not reaching the targeted communities because of their low involvement in the preschool settings where the programme is delivered. Similarly, the Early Childhood Oral Health Program is a dental care programme available for children which was not being utilised by the target communities because of significant barriers to accessing dental services and experiences of discrimination, highlighting the need for culturally appropriate services. There was strong interest in support for child oral health expressed by the participating communities. A need for parenting support was also identified due to the social isolation of many mothers of young children.15 The piloting of this study, conducted in the second phase of Teeth Tales, also highlighted the critical importance of working collaboratively and flexibly with community-based cultural organisations in order to engage meaningfully with migrant families.16
Figure 1.
Teeth tales phases.
Results from this formative qualitative and pilot research informed the development of a community-based intervention through a collaborative process with investigators, community, cultural and government partners. The intervention framework was designed to be multisite and multilevel consistent with the Fisher-Owens Model and informed by the limited evidence of effective oral health promotion community-based interventions.17–24
Phase 3 of Teeth Tales is an exploratory trial implementing the community based child oral health promotion intervention for Australian families from refugee and migrant backgrounds. See table 1 for the trial aims and objectives.
Table 1.
Trial aims, objectives and measures
| Aim: Establish a model for feasible, replicable and affordable child oral health promotion for culturally diverse LGAs in Australia | |
|---|---|
| Objectives—assessment of effectiveness | Measures |
| 1a. Assess the impact of the intervention on frequency of child tooth brushing | Child dental examination
|
| 1b. Assess the impact of the intervention on parent's knowledge of child oral hygiene needs | Parent questionnaire
|
| Objectives—process evaluation | |
| 2a. Determine the costs of the intervention | Measured by records of resources invested in the intervention by participating organisations |
| 2b. Identify facilitators and barriers to implementing both components of the intervention | Project documentation, formal reflexive practice discussions and observation activities, and focus group discussions with cultural partner organisations CORe staff survey |
| 2c. Assess intervention, fidelity, dose and reach | Project documentation, focus groups and interviews, researcher observations CORe staff survey and document review |
| Objectives—descriptive analyses | |
| 3a. Measure change in child oral health over time for target cultural groups | Child dental examination
How would you rate the oral health of this child? |
| 3b. Measure change in child and parent oral health-related behaviours over time for target cultural groups | Parent questionnaire
Do you add sugar or sweet flavourings to your child's (a) food and (b) drinks?
|
| 3c. Measure change in parent/care-giver oral health-related knowledge, confidence and attitudes over time for target cultural groups | Parent Questionnaire
|
| 4a. Assess access to dental and other services over time for target cultural groups | MCHS service use reports Parent questionnaire ▸ Has your child ever visited a dentist? ▸ Where was your child's last dental visit? ▸ How long since you last saw a dentist? ▸ Where was your last dental visit? |
| 4b. Assess change in cultural competency of local health and dental services over time | Measured by CORe follow-up staff survey and document review |
CORe, Cultural Competency Organisational Review; ICDAS, International Caries Detection and Assessment System; LGA, local government area; MCHS, Merri Community Health Services.
Methods
Study design
Phase 3 of Teeth Tales is an exploratory trial implementing a community-based child oral health promotion intervention for Australian families from refugee and migrant backgrounds. The intervention includes peer educator led community oral health education sessions and a reorienting of dental health and family services through a Cultural Competency Organisational Review (CORe; see below). The planned intervention trial was piloted at North Richmond Community Health (NRCH) in 2010–2011. This led to several changes being made to the original study design.16
Study location
LGAs in Australia are the third and lowest tier of government, administered by State and Territory governments. Moreland LGA in Melbourne, Victoria was chosen as the intervention site for this study as it was the location of the earlier formative qualitative study. Moreland is a culturally diverse, inner-urban metropolitan LGA of Melbourne, Australia. Moreland has one of the most diverse populations in Melbourne with just over one-third of residents born overseas and approximately 40% speaking a language other than English at home.25
Theoretical frameworks and principles
The theoretical framework underpinning the overall approach is the socioenvironmental model of health26 which recognises the range of interacting sociocultural and environmental influences on health beliefs and behaviours. This framework was applied within this trial through use of the Fisher-Owens et al24 conceptual model of interacting biological, child-level, family-level and community-level influences on child oral health over time. The model guided the development of a range of community-based intervention strategies designed to achieve positive oral health knowledge, behaviour and environmental change outcomes. The cultural competence framework for systems and programmes27–31 provided guidance for conducting research focusing on sociocultural differences in culturally diverse community contexts. Cultural competence is defined as ‘a set of congruent behaviours, attitudes and policies that come together in a system, agency or among professionals and enable that system, agency or those professions to work effectively in cross-cultural situations’.31 32 It is strongly aligned with community-based participatory research (CBPR) which is an orientation to research which focuses on the relationship between research partners and is one that involves an equitable partnership between researchers and members of the community.33–36
The peer education component of the intervention is informed by social learning theory in which people learn by observing and modelling the social behaviours of others with whom the person identifies, and through training in skills that lead to confidence in being able to carry out behaviours.37
Recruitment—peer educators
Bilingual peer educators were identified and recruited into the trial by community and cultural partners based on their communication and leadership skills and cultural affinity with the targeted cultural groups. These peer educators were trained by Teeth Tales staff to assist with family recruitment and data collection, and to coordinate and conduct the community oral health education sessions. Reimbursement was provided for peer educator attendance at the peer educator training course, for assistance at recruitment sessions and for conducting the oral health community education sessions. Peer educators in some cases were employed as casual staff specifically for the role and in others selected from existing staff within the partner cultural organisations. The Teeth Tales budget also included appropriate remuneration for the role of the cultural organisations in supporting the intervention and research components of the trial.
Recruitment—trial participants
Families from an Iraqi, Lebanese or Pakistani background with children aged 1–4 years and residing in metropolitan Melbourne were invited to participate in the study by peer educators from their respective communities using snowball and purposive sampling techniques. This non-probability sampling technique is useful in reaching socially isolated populations.38 Participants were recruited by peer educators through cultural networks, community centres, schools, kindergartens, maternal and child health clinics, playgroups and other relevant settings. Potential participants were given dates and locations for the recruitment session and invited to attend. Baseline data collection also took place at recruitment sessions. Recruitment into the trial entailed written parent/care-giver consent for self and children.
All staff from organisations (ie, Merri Community Health Services, Moreland City Council and the University of Melbourne research centre) participating in CORe (further details about CORe provided below) were invited via an email, from the Chief Executive Officer, to complete a staff survey and reminded to participate through staff meetings and reminder emails to increase response rate. The online and hard copy versions of the survey were available to accommodate staff preferences. Key informants from each organisation were also asked to assist with the CORe document review. Organisations then nominate their own group of managers and staff to take responsibility for the development and implementation of the CORe action plan.
Intervention
The Teeth Tales intervention aims to prevent early childhood child dental caries and promote positive oral health behaviour among migrant and refugee children aged 1–4 years and their parents/care-givers in Moreland, Victoria, Australia (see box 1).
Box 1. Intervention aims and objectives.
Specific aims
Achieve substantive and sustained improvements in oral health and healthy behaviours of children and parents of migrant and refugee background.
Reduce the strong social gradient evident in child oral health.
Intervention objectives
1a. Improve child oral health.
1b. Improve child and parent/care-giver oral health-related behaviours.
1c. Improve parent/care-giver oral health-related knowledge, confidence and attitudes.
2a. Increase access to dental and other family services.
2b. Improve cultural competency of local health and dental services.
The intervention will achieve this through implementation of two intervention components: (1) a peer educator-led community oral health education programme and (2) a cultural competence organisational review (see figure 2). Details of each intervention component are provided below.
Figure 2.
Logic model.
Community oral health education
The community oral health education programme was underpinned by the employment of cultural peer educators and conducted in culturally appropriate and accessible community settings. A two stage model of peer education was applied in Teeth Tales.39 The first stage involved training people who are members of a community (in this case determined by language spoken, ethnicity and cultural affinity) in the topic of choice (in this case oral health). The second stage was application of information about the topic to educate people in their own community, via either informal or formal information sessions with methods depending on the goals of the project and the context of the target group (in this case via community oral health education sessions).
Peer educators were trained by Teeth Tales staff in a series of sessions (5 h/week for 4 weeks) to deliver community oral health education sessions for their respective communities in a culturally appropriate setting. The topics covered in the training were based on evidence informed key oral health messages of Eat Well, Drink Well, Clean Well and Stay Well and informed by the phase 1 findings from Teeth Tales. The training also included a dental clinic visit at the community health service, a teeth cleaning demonstration and practice, practice in the use of plaque disclosing agents, as well as an introduction to other family services provided by Merri Community Health Services and Moreland City Council. During the interactive peer educator training, their cultural expertise was sought to make any final adjustments to the content and delivery of the community education sessions to suit particular cultural groups. This was incorporated into the opportunities during training for the peer educators to develop and practice their skills. A refresher course was provided for peer educators if there was a 6-month gap or more of time between training and the planned start of community education sessions. Further support was provided to the peer educators through the provision of a training manual, resources and reading material. Teeth Tales staff were available to support the peer educators in the organisation and delivery of training sessions as needed.
The community education sessions for parents/care-givers (see below) were conducted by the trained peer educators and included two 3 h sessions of oral health education followed by a site visit hosted by the community health dental service and including local council staff. The two oral health education sessions were conducted either on the same day or on different days, to suit the participants. The site visit was conducted a week after the last education session. Participants began the course with an introduction to dental services in Victoria, Australia, the structure of teeth, dental caries and what causes decay, and a discussion about their own oral health beliefs, values and practices and strategies for managing change. The topic areas of Eat Well and Drink Well, adapted from the DHSV Smiles 4 Miles programme (http://www.dhsv.org.au/smiles4miles/), focused on promoting healthy food and drink consumption, suitable foods for children, the benefits of fluoridated water consumption, limiting high sugar foods and drinks in the diet and linking these behaviours to tooth decay. Clean Well focused on the benefit of fluoridated toothpaste to prevent tooth decay, correct tooth brushing techniques, and promoted brushing teeth twice a day. Participants were provided with family oral health packs that included toothbrushes and toothpastes provided free for family members. Participants (parents/caregivers) were given an opportunity to practice brushing their own teeth using plaque disclosing agents to identify areas of plaque stagnation. This was intended to help them to identify how to improve their brushing effectiveness. Stay Well promotes the benefits of regular visits to the dentist and included a group visit to Merri Community Health Services to increase familiarity with the site, the staff, appointment booking processes, the fee structure and the dental clinic experience. Participants joined in a teeth cleaning demonstration, and were introduced to a range of family services provided by the health service and local government. Reminders of the key oral health messages were sent by peer educators to community education participants at regular intervals following completion of the programme (one message per month for 4 months). The language of the reminder messages and method of delivery were determined by participant preference for text message, email, phone call or mailed reminders.
Cultural Competence Organisational Review
CORe provided an opportunity for organisations to conduct a guided evidence-informed internal review of cultural competence in terms of staff perceptions of organisational practice and documented policies and systems. The CORe staff survey, implementation guide and results report were organised according to the following six domains identified as critical for organisational cultural competence: governance; planning, monitoring and evaluation; communication; staff development; partnerships and services and interventions.40 The results of the baseline CORe assessment, described below under data collection and data analysis, were provided to the respective organisations, with resources and templates providing best practice examples, to help direct their action planning process. This was directed by a working group, including senior staff, within the organisation. Partner organisation, Centre for Culture, Ethnicity and Health (CEH) supported organisations participating in CORe as this is consistent with their standard services.
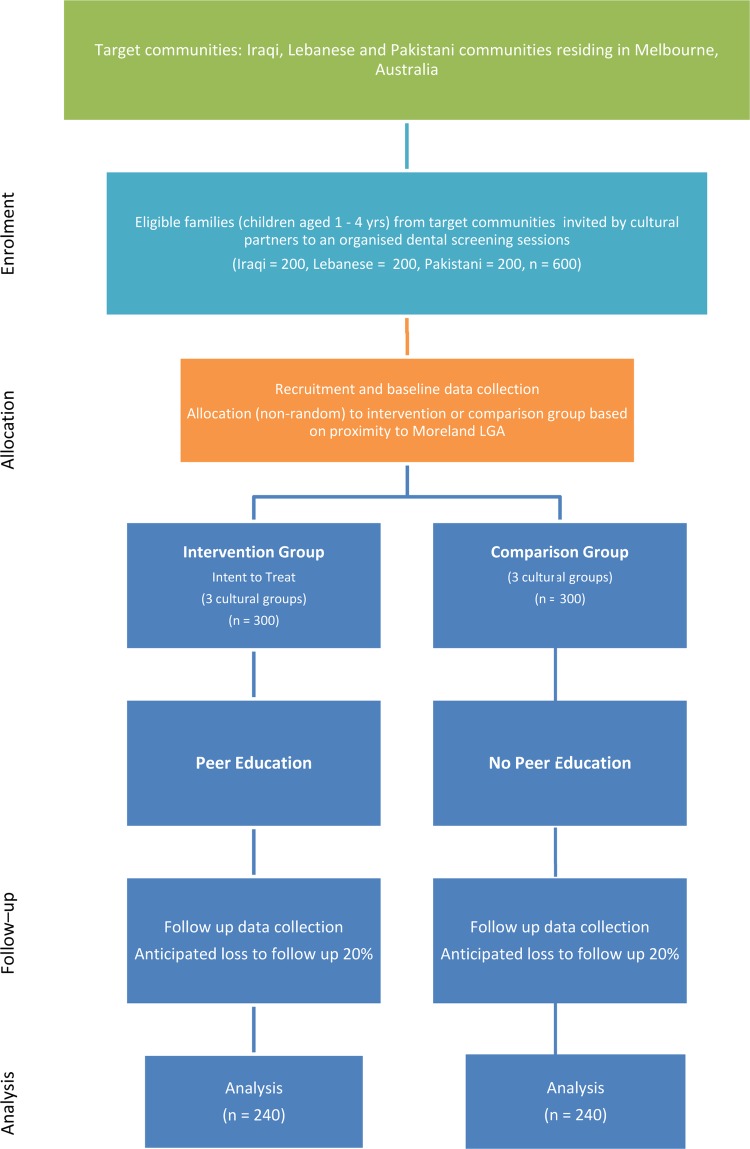
Allocation to intervention—peer education programme
Community participants were recruited to the intervention arm if their residential address was within Moreland or any adjacent LGAs, to ensure they had access to the peer educator led community oral health education sessions and the Merri Community Health Services and Moreland City Council services introduced as part of the CORe intervention programme. Families from outside these areas were treated as the comparison group (figure 3).
Figure 3.
Flow of participants through the trial.
Statistical power
The purpose of an exploratory trial is to assess the feasibility, relevance and affordability of the intervention rather than testing for significant change. However, given the target sample size of 600 was relatively large for an exploratory trial, we anticipated sufficient power to detect significant differences in relation to child tooth brushing, assessed by the frequency of tooth brushing and modified gingival index as a proximal indicator. The formative qualitative research in the first phase of Teeth Tales identified that parents did not consider the first dentition as requiring care because they fall out and are replaced. Therefore, the clean well message was considered likely to have the greatest impact, requiring fairly simple behaviour change. Assuming a sample size of 600 families (300 per arm), allowing for a 20% dropout, a two tailed α of 0.05 and no clustering effects, there is 95% power to detect a 25% change in tooth brushing frequency. This is consistent with the level of change seen in other oral health promotion intervention studies.20 41 We also anticipated that it would be possible to detect a difference in parent knowledge of child oral hygiene needs, with similar power calculations. While we acknowledge the potential for clustering effects by peer educator/practitioner, we did not include this in our power estimation as the small number of practitioners/peer educators per cultural group (from as low as 1 per cultural group) means that the practitioner effect cannot be estimated independently of the intervention effect. We attempted to minimise this practitioner clustering effect by having standardised information resources as well as peer educator training across the three different cultural groups.
Data collection
All of the following measures were scheduled to be conducted at baseline (from March to September 2012) and at 18 months of follow-up (from September 2013 to March 2014).
All children aged 1–4 years at baseline in the participating families received dental examinations carried out by trained dental professionals to assess their oral health status, using a protocol successfully applied in previous oral health studies conducted by the investigators.42 The dental examinations were held in community locations and took place immediately following recruitment. The examinations, conducted by one examiner and one recorder, assessed evidence of ECC, presence of plaque and gingival health as risk indicators for oral health and as an indicator of effective oral hygiene and combined, objective indicators of tooth brushing. The child was examined in a lap-to-lap position with their legs wrapped around their mother's (or primary carer) lap and with their head resting on the examiner's lap. Teeth and surfaces were examined in a standard order; from the upper right quadrant to the upper left quadrant and the lower left quadrant to the lower right quadrant, examining the surfaces in order, that is, distal, occlusal, mesial, buccal and lingual. The Federation Dentaire Internationale (FDI) two-digit tooth numbering system (ie, 11, 21, 55, 54, 53, etc) was employed. Dental caries were diagnosed and scored using codes of the International Caries Detection and Assessment System—ICDAS II,43 however, tooth surfaces were not dried using compressed air. Hence, ours will be a modified version of the ICDAS II. Cotton wool was used to clean the tooth surfaces. Plaque status was measured using the debris index and gingival health measured using the Modified Gingival Index.44 All examinations were carried out by visual inspection only, using a headlamp and disposable dental mirrors. Dental probes were not used and dental radiographs not taken.
Structured self-administered parent questionnaires were used to collect data on: sociodemographic-economic status; child feeding habits; child and parents/caregivers’ oral hygiene-related behaviour; self-reported oral and general health status for children and parent/care-giver; parent/care-giver's knowledge and attitudes about oral health and towards local dental health services; and confidence and capacity to implement positive oral health practices. However, translated questionnaires were available in Arabic and Urdu, it was recognised that some participants from these communities may have low literacy and need assistance. Peer educators explained the project to parents/care-givers, provided verbal translations of the questionnaire and assisted parents/care-givers with questionnaire completion when needed/requested.
The CORe staff survey consisted mainly of multiple-choice questions to assess staff perceptions of organisational cultural competence practices under the six cultural competency domains—governance; planning, monitoring and evaluation; communication; staff development; partnerships; and services and interventions. All participating organisations are multisite and multisetting so the survey asked staff to respond based on their own work site. The CORe document review will be conducted by a senior manager and a representative from CEH, to assess documentary evidence of cultural competence in relation to existing organisational policies and systems.
Process data will be collected through partner meetings and organisational documentation to monitor if the intervention is being implemented as intended, including focus group discussions at the end of the intervention period with peer educators and cultural organisation partners to review intervention processes, facilitators and barriers. Economic data will be collected through the parent questionnaires and through meetings with partner organisations to monitor resource use and assess cost implications of the Teeth Tales intervention for participating families and organisations. In addition, the economic analysis will be informed by records of resources used to implement the education sessions and CORe processes.
The alignment of the trial objectives, outcomes and measures are presented in table 1.
Data quality
Training and calibration of dental examiners in the use of the diagnostic protocol was conducted centrally and supervised by experienced investigators. This process was repeated annually. For quality assurance purposes approximately 5% of the sample will be re-examined. Data recorders were trained in data entry protocols. Data cleaning and management will be conducted by an experienced Research Fellow under direction of experienced investigators. Cross-training of partners will occur throughout: research staff were trained in culturally competent public health research methods; staff from the cultural and community partner organisations were also trained in relevant research methods. Location-based allocation of participants to intervention and comparison groups will potentially compromise the blinding of the dental examiners and researchers to the intervention status of the participants. Hence, the data management and analysis were designed to minimise this bias by employing controls such as, the researcher analysing the data will not perform electronic data entry, trial participants were allocated ID numbers by external personnel, and the data analysis plan developed a priori.
Participant information sheets and questionnaires were translated into the respective community languages and support provided by bilingual peer educators to ensure that the participants were able to make an informed decision regarding trial participation and able to clearly understand the questionnaire.
CORe was also conducted at the research centre leading the study, McCaughey Centre for Community Wellbeing, Melbourne School of Population and Global Health, University of Melbourne, to contribute to process evaluation, capacity building, cultural competence and to demonstrate commitment to the project aims and outcomes.
Data analysis
Descriptive analyses will first be conducted to illustrate participant characteristics stratified by cultural group. Design-weighted survey estimators will be used where required.
The Outcome data will be analysed using bivariable and multivariable analyses. Estimates and CIs for outcomes will be computed and compared across the intervention and comparison groups at baseline and follow-up. The difference in estimates between groups will be tested for significance for the primary outcomes. Subgroup analyses will be conducted for ethnicity, time in Australia, and socioeconomic status, in recognition of the potential influence of ethnicity and acculturation as well as demographic factors on outcomes.
Process data will be critically reviewed throughout the trial to identify any barriers and facilitators to change, and inform modifications in trial methods and processes to maintain study integrity and research rigour. Descriptive statistics of peer educator activity and intervention participation will also be generated to provide important information about intervention reach and dose. The qualitative components will adhere to the RATS guidelines on qualitative research (http://www.biomedcentral.com/ifora/rats).
Economic data on resources used will be analysed to assess costs of the intervention and to compare these costs with the outcomes achieved. Measured resource use will be valued (in 2012 Australian dollars) using standard unit cost data sources (eg, salary scales, RACV travel cost estimates).
CORe staff survey data—cross-sectional data will be analysed using descriptive statistics to describe participant characteristics and provide frequency distributions to each question. A score for the organisation across all respondents and responses will be derived in total for each domain score. Comparisons between predictor and outcome variables will be made using χ2 tests of associations. Logistic and multinomial regressions will also be conducted where appropriate. Differences in organisational scores will be compared between baseline and follow-up.
CORe document review data will be reviewed by expert staff from CEH to determine the extent to which organisations’ documented policies and procedures meet the CORe cultural competency guidelines within the following domains: governance; planning, monitoring and evaluation; communication; staff development; partnerships and services and interventions. A level of cultural competence will be assigned by the CEH staff member to the organisation for each domain, using the categories defined by Cross et al31—cultural destructiveness, cultural incapacity, cultural blindness, cultural precompetence, cultural competence and cultural proficiency.
Parallel data collection and analysis of each measure will be conducted to preserve methodological rigour. A mixed method analysis of findings will then be conducted to provide a more comprehensive understanding of trial impacts and outcomes.45
Discussion
The importance of the interacting influences of environmental, sociocultural and personal influences on individual health behaviours and population health outcomes is central to accepted socioenvironmental theoretical frameworks26 46 including the Fisher-Owens et al24 conceptual model of influences on children's oral health and the Ottawa Charter for Health Promotion47 which outlines the need for action at multiple levels. This guides the development of interventions by showing the importance of achieving a shift in environments and health behaviours to achieve health outcomes. To be sustainable, interventions need to be embedded into relevant systems and processes, and population-level interventions also need to include strategies to engage vulnerable groups within the population to ensure that there is no increase in health inequalities.48 Therefore, interventions addressing the needs of potentially vulnerable populations should be used as a complement to population approaches.
Teeth Tales is a multilevel community-based intervention informed by previous research that identified the sociocultural and environmental influences on child oral health in migrant and refugee communities in the Moreland LGA. The culturally competent, participatory processes adopted in phase 1 of Teeth Tales greatly enhanced the research process and the resultant findings. Therefore the study continued this approach into the trial phase of Teeth Tales. A CBPR process helps build a relationship of trust and partnership between the researcher and the communities being researched, and has been shown to be effective in reaching socially isolated communities; recruiting and sustaining large numbers of community participants in the research process; and engaging communities to adopt and sustain healthy practices.36 CBPR is defined as a collaborative approach to research that equitably involves all partners in the research process and recognises the unique strengths that each brings. CBPR begins with a research topic of importance to the community with the aim of combining knowledge and action for social change to improve community health and eliminate health disparities.36 As communities are directly involved there are more chances that positive outcomes will be sustainable and the empowered communities will take the initiative to push for policy and practice change to improve their circumstances.36 49 A culturally competent approach accounts for the added complexity of conducting CBPR in a culturally diverse setting.28 Accordingly in this study, there is a commitment at all stages of the research to develop and maintain an active partnership with community and cultural partners recognising the expertise of (1) community and government partners (community health including public dental services, local government and state government agency) in relation to the community context, service systems, policy and service delivery methods and options and (2) the expertise of cultural partners in relation to cultural beliefs, practices and concerns, information pathways and methods of engagement. This shared responsibility and decision-making is reflected in the costaffing arrangements for the study with funded Teeth Tales staff being employed by four of the partner organisations—University of Melbourne, Merri Community Health Services, Arabic Welfare and Victorian Arabic Social Services. Partner organisations, including Pakistan Australia Association Melbourne, also provide expert advice throughout development and implementation of the trial and practical assistance to the research process by embedding the research trial within their service delivery systems and disseminating research information. The capacity of community organisations as change advocates is highlighted by this approach and provides opportunities for all partner organisations to extend the trial benefits through ongoing application of the shared new knowledge as well as extension of the skills gained to collaboratively address other community-based health/social issues.
The piloting of the intervention trial in phase 2 of Teeth Tales further demonstrated the importance of taking a participatory approach in complex and multidimensional public health interventions in order to establish feasibility, effective implementation and relevance to the community and cultural context in which the intervention will operate. While there was considerable support for the pilot in North Richmond from local agencies, there was very limited involvement from cultural organisations either because of their limited resources or because they did not yet exist for new and emerging cultural groups being targeted. This meant regular adjustments to research processes to accommodate the complex nature of community-based service delivery, and the importance of stakeholder engagement throughout the entire process to provide advice on community and cultural considerations. In doing so it demonstrated the critical importance of the ongoing cultural partnerships operating in the community context and the importance of these relationships for success in reaching the target communities. Despite these learnings and the expressed need for child oral health support by the Moreland-based community groups and cultural organisations in the formative qualitative phase of Teeth Tales, recruitment of families to the intervention trial was still challenging. This reflects the reality of community-based research and the competing demands of family life that may make attendance at research and health promoting events a low priority unless they are linked to services or events families are already attending.
Social learning theory as a foundation for peer education relies strongly on role modelling, practising of learned behaviours and positive reinforcement.37 In Teeth Tales the peer educators model healthy eating and drinking through choice of refreshments provided in courses, teeth cleaning demonstrations, and reports of their own family changes in child eating and drinking behaviours. While there are various models of peer education, a key feature is seen to be the credibility of the person and the peer education model.39 In some cases, an informal approach by a peer can be more effective in reaching disengaged groups, while other groups prefer health education to come from ‘experts’ rather than peers. The Teeth Tales model addresses both of these scenarios by using cultural peers in informal settings but with a structured programme and the formal backing and training of key cultural, health and academic organisations. This has the advantage of increasing the likelihood of sustainability of the programme through ongoing opportunities for the partner organisations to utilise their trained staff and resources. However, it is also possible that this ‘blurring’ of distinction between expert and peer advice could reduce the impact of the peer education model.
It is necessary to find a balance when designing and implementing community-based intervention studies to address the demands of research rigour and requirements for strength of evidence, while still operating within existing systems and community processes. For example, the modifications to the trial design arising from the pilot phase meant that instead of nominating an intervention and a comparison community, we would instead have a defined intervention site and a broad recruitment catchment area with allocation to intervention and comparison groups determined by the residential address of the participant. This modification to trial design means that it was not possible to randomly allocate participants to the intervention, introducing a potential source of bias in our trial. However, it was agreed that being rigid in terms of study design would have reduced the relevance and applicability of the intervention.
Conclusion
Teeth Tales will provide an opportunity to address inequities in child oral health through the trial of a community-based child oral health promotion intervention trial targeted specifically for migrant and refugee communities in the Moreland area of Melbourne. The trial will inform policy and practice decision-making by participating partners in relation to cultural competence improvements. The trial findings will contribute to the limited evidence base relating to community interventions to improve child oral health in migrant communities. If the results from this trial are promising it will lead to the development of a model for a community-based child oral health intervention which would ideally be tested using a multisite cluster randomised controlled trial to inform policy and practice more widely. It is also expected that the outcomes from this exploratory trial will raise meaningful questions and pave the way for further research in relation to oral health inequities for migrant communities.
Supplementary Material
Acknowledgments
The authors would like to dedicate this paper in memory of Coralie Mathews, a much loved member of the Teeth Tales team and the heart and soul of the Teeth Tales project. The authors wish to thank research participants who were willing to participate in the trial, the peer educators who have shown considerable skill and commitment to the trial, and the many cultural, community and government organisations who have supported its development and implementation. In particular, they wish to acknowledge our colleagues and representatives from partner organisations on the Teeth Tales study who chose not to be authors on this paper but have contributed conceptually and in practical terms to the trial—Arabic Welfare, Victorian Arabic Social Services, North Richmond Community Health, Moreland City Council and Yarra City Council. The authors wish to gratefully acknowledge the Jack Brockhoff Foundation for infrastructure.
Footnotes
Contributors: LGibbs was principal investigator of the study and drafted the paper. All of the coauthors contributed to the study design and to the completion of the manuscript. Specifically, EW contributed to the cross-disciplinary approach and evidence base contributions. AdS contributed to the data analysis considerations. ER contributed to ethnicity and oral health evidence. LM contributed to the study design and statistical analysis. CA contributed to service delivery considerations. BJ contributed to piloting and development of study methods. MM contributed to the development of cultural competence measures. HC contributed to dental procedures and policy. MG contributed to the development of oral health measures and methods. DY contributed to community partnerships, intervention and data collection components. MT contributed to community health policy considerations. BC contributed to the data collection and data management. IG contributed to the cultural influences and networks. RW contributed to the international evidence. VP contributed to re-orientation of services components. MT contributed to the measurement of cultural competence. LGold contributed to economic analysis. All authors read and approved the final manuscript.
Funding: This project was funded by an Australian Research Council Linkage grant (LP100100223), with cash and in-kind contributions from Linkage partners—Merri Community Health Services, Dental Health Services Victoria, Moreland City Council, Victorian Arabic Social Services, Arabic Welfare and Pakistan Australia Association Melbourne. Additional funding support was also provided by Merri Community Health Services. Separate funding grants contributing to the overall research activities were also received from Dental Health Services Victoria and Moreland City Council. The authors wish to thank Colgate-Palmolive Australia for donating the toothbrushes and toothpastes which were included in gift bags for the intervention participants.
Competing interests: Consistent with the participatory approach of this study, many of the study authors (AdS, CA, MM, HC, DY, MT, IG) represented organisations, as listed in their affiliations, that have an interest in or are involved in the delivery of the services described in the intervention. Salary support for EW, LGibbs and AdS from Jack Brockhoff Foundation, and the Australian National Health and Medical Research Council for salary support for LGold, and La Trobe University for salary support for MG. MT is a grateful recipient of an Australian Postgraduate Award PhD scholarship. ER is supported by the Murdoch Childrens Research Institute which is supported by the Victorian Government's Operational Infrastructure Support Program.
Ethics approval: Ethics approval for this trial was granted by the University of Melbourne Human Research Ethics Committee and the Department of Education and Early Childhood Development Research Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ha DH, Roberts-Thomson KF, Armfield JM. The Child Dental Health Surveys Australia, 2005 and 2006. Dental statistics and research series no. 54. Canberra: AIHW, 2011 [Google Scholar]
- 2.Gussy MG, Waters EG, Walsh O, et al. Early childhood caries: current evidence for aetiology and prevention. J Paediatr Child Health 2006;42:37–43 [DOI] [PubMed] [Google Scholar]
- 3.Kruger E, Dyson K, Tennant M. Hospitalization of Western Australian children for oral health related conditions: a 5-8 year follow-up. Aust Dent J 2006;51:231–6 [DOI] [PubMed] [Google Scholar]
- 4.U. S. Department of Health and Human Services Oral health in America: a report of the Surgeon General. Rockville: U.S. Department of Health and Human Services, 2000 [Google Scholar]
- 5.Sheiham A. Dental caries affects body weight, growth and quality of life in pre-school children. Br Dent J 2006;201: 625–6 [DOI] [PubMed] [Google Scholar]
- 6.Watt RG. From victim blaming to upstream action: tackling the social determinants of oral health inequalities. Community Dent Oral 2007;35:1–11 [DOI] [PubMed] [Google Scholar]
- 7.Vargas CM, Ronzio CR. Disparities in early childhood caries. BMC Oral Health 2006;6(Suppl 1):S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kilpatrick NM, Neumann A, Lucas N, et al. Oral health inequalities in a national sample of Australian children aged 2-3 and 6-7 years. Aust Dent J 2012;57:38–44 [DOI] [PubMed] [Google Scholar]
- 9.Burnley IH. Immigrant city, global city? Advantage and disadvantage among communities from Asia in Sydney. Aust Geographer 1998;29:49–70 [Google Scholar]
- 10.Dye BA, Tan S, Smith V, et al. Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat 2007;. 11:1–92 [PubMed] [Google Scholar]
- 11.Pollick HF, Rice AJ, Echenberg D. Dental health of recent immigrant children in the Newcomer schools, San Francisco. Am J Public Health 1987;77:731–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davidson N, Skull S, Calache H, et al. Holes a plenty: oral health status a major issue for newly arrived refugees in Australia. Aust Dent J 2006;51:306–11 [DOI] [PubMed] [Google Scholar]
- 13.Australian Department of Immigration and Citizenship DIAC Settlement Reporting Facility. Melbourne, 2006 [Google Scholar]
- 14.Riggs E, Gemert CV, Gussy M, et al. Reflections on cultural diversity in oral health promotion and prevention. Global Health Promot 2012;19:60–3 [DOI] [PubMed] [Google Scholar]
- 15.Riggs E, Gibbs L, Kilpatrick N, et al. Breaking down the barriers: a qualitative study to understand child oral health in refugee and migrant communities in Australia. Ethn Health. 2014. In press [DOI] [PubMed] [Google Scholar]
- 16.Gibbs L, de Silva A, Waters E, et al. Lessons from piloting a culturally competent, systems-embedded child oral health promotion intervention: Teeth Tales. Health Promot J Aust under review [Google Scholar]
- 17.Ammari J, Baqain Z, Asley P. Effects of programs for prevention of early childhood caries. Med Princ Pract 2007;16:437–42 [DOI] [PubMed] [Google Scholar]
- 18.Feldens CA, Vítolo MR, Drachler ML. A randomized trial of the effectiveness of home visits in preventing early childhood caries. Community Dent Oral 2007;35:215–23 [DOI] [PubMed] [Google Scholar]
- 19.Harrison RL, Wong T. An oral health promotion program for an urban minority population of preschool children. Community Dent Oral Epidemiol 2003;31:392–9 [DOI] [PubMed] [Google Scholar]
- 20.Kowash MB, A P, Smith J, et al. Effectiveness on oral health of a long-term health education programme for mothers with young children. Br Dent J 2000;188:201–5 [DOI] [PubMed] [Google Scholar]
- 21.Marinho VC, Higgins JP, Sheiham A, et al. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2003;(1):CD002278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watt RG. Strategies and approaches in oral disease prevention and health promotion. Bull World Health Organ 2005; 83:711–18 [PMC free article] [PubMed] [Google Scholar]
- 23.Wennhall I, Matsson L, SchrÖDer U, et al. Outcome of an oral health outreach programme for preschool children in a low socioeconomic multicultural area. Int J Paediatr Dent 2008;18:84–90 [DOI] [PubMed] [Google Scholar]
- 24.Fisher-Owens SA, Gansky SA, Platt LJ, et al. Influences on children's oral health: a conceptual model. Pediatrics 2007;120:e510–20 [DOI] [PubMed] [Google Scholar]
- 25.Moreland City Council City of Moreland Community Profile. 2006 and 2001 Enumerated Census information for: City of Moreland. 2008
- 26.Lynch J. Social epidemiology: some observations about the past, present and future. Aust Epidemiol 2000;7:3 [Google Scholar]
- 27.Pacific Health Research Committee Guidelines on pacific health research. Auckland: Health Research Council, 2004 [Google Scholar]
- 28.Gibbs L, Waters EG, Renzaho A, et al. Moving towards increased cultural competency in public health research. In: Williamson A, DeSouza R, eds. Researching with communities: grounded perspectives on engaging communities in research. London: Muddy Creek Press, 2007 [Google Scholar]
- 29.NHMRC Cultural competency in health: a guide for policy, partnerships and participation. Canberra: Commonwealth of Australia, 2005 [Google Scholar]
- 30.Waters E, Gibbs L, Renzaho A, et al. Increasing cultural competence in public health and health promotion. Oxford, UK: Elsevier Inc, 2008 [Google Scholar]
- 31.Cross TL, Bazron BJ, Dennis KW, et al. Towards a culturally competent system of care: Vol 1. Washington, DC: National Technical Assistance Centre for Children's Mental Health, Georgetown University Child Development Centre, 1989 [Google Scholar]
- 32.OPHS Office of Minority Health National standards for culturally and linguistically appropriate services in health care. Washington, DC: U.S. Department of Health and Human Services, 2001 [Google Scholar]
- 33.Blumenthal D, DiClemente R. Community-based health research: issues and methods. New York: Springer Publishing Company, 2004 [Google Scholar]
- 34.Gibbs L, Gold L, Kulkens M, et al. Are the potential benefits of a community-based participatory approach to public health research worth the potential costs? Just Policy 2008(47):54–9 [Google Scholar]
- 35.Israel BA, Schulz AJ, Parker EA, et al. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health 1998;19:173–202 [DOI] [PubMed] [Google Scholar]
- 36.Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract 2006;7:312–23 [DOI] [PubMed] [Google Scholar]
- 37.Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice-Hall, 1977 [Google Scholar]
- 38.Thompson S, Phillips D. Reaching and engaging hard-to-reach populations with a high proportion of nonassociative members. Qual Health Res 2007;17:1292–303 [DOI] [PubMed] [Google Scholar]
- 39.Turner G, Shepherd J. A method in search of a theory: peer education and health promotion. Health Educ Res 1999;14:235–47 [DOI] [PubMed] [Google Scholar]
- 40.Linkins K. Indicators of cultural competence in heath care delivery organizations: an organizational cultural competence assessment profile: The Lewin Group for United States. Department of Health and Human Services, Health Resources and Services Administration (HRSA), 2002:1–10 [Google Scholar]
- 41.Roberts-Thomson KF, Slade GD, Bailie RS, et al. A comprehensive approach to health promotion for the reduction of dental caries in remote Indigenous Australian children: a clustered randomised controlled trial. Int Dent J 2010;60(3 Suppl 2):245–9 [PubMed] [Google Scholar]
- 42.Neumann AS, Lee KJ, Gussy MG, et al. Impact of an oral health intervention on pre-school children <3 years of age in a rural setting in Australia. J Paediatr Child Health 2011;47:367–72 [DOI] [PubMed] [Google Scholar]
- 43.Ismail AI, Sohn W, Tellez M, et al. The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol 2007;35:170–8 [DOI] [PubMed] [Google Scholar]
- 44.Lobene RR, Mankodi SM, Ciancio SG, et al. Correlations among gingival indices: a methodology study. J Periodontol 1989;60:159–62 [DOI] [PubMed] [Google Scholar]
- 45.Nastasi B, Hitchcock J, Brown L. An inclusive framework for conceptualizing mixed method design typologies. In: Tashakkori A, Teddlie C. eds. SAGE handbook of mixed methods in social & behavioral research. 2nd edn London: Sage, 2010;305–38. [Google Scholar]
- 46.McLeroy KR, Bibeau D, Steckler A, et al. An ecological perspective on health promotion programs. Health Educ Q 1988;15:351–77 [DOI] [PubMed] [Google Scholar]
- 47.World Health Organisation. 1986. Ottawa charter for health promotion.
- 48.Frohlich KL, Potvin L. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. Am J Public Health 2008;98:216–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health 2010;100(Suppl 1):S40–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.