Abstract
Background
Nonmedical determinants of medical decision making were investigated in an international research project in the United States, the United Kingdom, and Germany. The key question in this paper is whether and to what extent doctors' diagnostic and therapeutic decisions in coronary heart disease (CHD) are influenced by patient gender.
Methods
A factorial experiment with a videotaped patient consultation was conducted. Professional actors played the role of patients with symptoms of CHD. Several alternative versions were taped featuring the same script with patient-actors of different gender, age, race, and socioeconomic status. The videotapes were presented to a randomly selected sample of 128 primary care physicians in each country. Using an interview with standardized and open-ended questions, physicians were asked how they would diagnose and treat such a patient after they had seen the video.
Results
Results show gender differences in the diagnostic strategies of the doctors. Women were asked different questions, CHD was mentioned more often as a possible diagnosis for men than for women, and physicians were less certain about their diagnosis with female patients. Gender differences in management decisions (therapy and lifestyle advice) are less pronounced and less consistent than in diagnostic decisions. Magnitude of gender effect on doctors' decisions varies between countries with smaller influences in the United States.
Conclusion
Although patients with identical symptoms were presented, primary care doctors' behavior differed by patients' gender in all 3 countries under study. These gender differences suggest that women may be less likely to receive an accurate diagnosis and appropriate treatment than men.
Introduction
The knowledge of gender differences in the morbidity and mortality of coronary heart disease (CHD) is well established (Central Health Monitoring Unit, 1994; Derby, Lapane, Feldman, & Carleton, 2000; National Center for Health Statistics, 2005; Statistisches Bundesamt, 2006; Tunstall-Pedoe, Morrison, Woodward, Fitzpatrick, & Watt, 1996). These differences are often described as results of biological processes and unhealthy lifestyle behaviors that influence coronary risk. Estrogens are discussed to have a protective effect for women (Mendelsohn, 2002; Rossouw et al., 2007). In contrast, men's different health lifestyles could cause a coronary illness. Gender-specific behaviors (e.g., smoking, a high level of alcohol consumption) increase the probability for CHD (Yusuf et al., 2004).
These gender differences in the prevalence of CHD and risk behavior are well known by most general practitioners, yet doctors could hold stereotypical views on what kind of patients are at risk for CHD and those who are not. These views could affect the probability of being correctly diagnosed and treated for certain patient groups (Bond et al., 2003; Van Ryn & Fu, 2003). For example, female patients who are at a lower risk of CHD (overall) are at risk of not being diagnosed accurately. Thus, mediated by these stereotypes, nonmedical factors could affect the doctors' decision making process and subsequently the therapeutic outcome of a patient with symptoms of CHD (Anand, Xie, & Metha, 2005; Arber et al., 2004, 2006; Bönte et al., 2007; Frich, Malterud, & Fugelli, 2006; McKinlay, Lin, Freund, & Moskowitz, 2002; Mikhail, 2006). In research on health disparities, provider behavior itself is often unaddressed, although it is important to understand the development of epidemiologic gender differences. Furthermore, information about gendered care pathways in CHD are relatively well documented, but primarily focused on differences within secondary care. Raine (2000) provides evidence for the existence of gender bias in the use of specialist services by critically appraising the literature. His review indicates that female patients are less likely than male patients to undergo CHD-related diagnostic investigations and surgical treatment. Recent studies from the United States show that gender disparities in the quality of health services provided to patients with acute myocardial infarction are a consistent phenomenon across different population groups (Correa-de-Araujo et al., 2006) and among patients with the same health insurance (Chou et al., 2007).
Another limitation of many studies on medical decision making is that they do not control for other potential patient factors (like age, ethnicity, or social status) or physicians' attributes (like gender and age) that might influence the doctors' decisions (Feldman, Freund, Burns, Moskowitz, & Kasten, 1997). In addition, results are often limited to 1 region or country and the role of the health care system in which patients are diagnosed and treated is often not taken into account. Comparative research in this field is important to determine the contribution of the health care system to health disparities (Blendon, Schoen, DesRoches, Osborn, & Zapert, 2003; Blendon et al., 2004; Herlitz et al., 2003; Schoen et al., 2004). In this regard, McKinlay et al. (2006) described how doctors in the United States and the United Kingdom manage the same patient. Without analyzing the effect of gender specifically, their results show a high level of consistency in medical decision making for CHD in the 2 countries. However, British doctors were less certain with the diagnosis and asked more additional questions than their American colleagues. Arber et al. (2004, 2006) analyzed the influence of patient gender on the decision making process for these 2 countries together. Findings indicate that doctors' diagnostic and management strategies relating to CHD vary by patient gender, to the disadvantage of women.
In this paper, gender effects on the diagnosis and treatment of CHD are presented separately for 3 countries with different health insurance systems (a largely private insurance-based health care system in the United States; a National Health Service that is a government-supported, taxation-based system in the United Kingdom; and a system characterized by decentralized care administered by social security agencies in Germany). The aim is to examine whether gender disparities in the diagnosis and treatment of CHD vary in different health care systems or if they are a cross-national invariant phenomenon.
Methods
Design and Contents of the Video Vignettes
In this study, a factorial experimental design with portrayed video vignettes was used (Feldman et al., 1997). To develop the script for the video vignettes, clinical consultants role played actual office visits. This step was essential to ensure clinical accuracy. Professional actors were used to portray medical encounters on videotape in which the “patient” presented with 7 signs and symptoms that are typical for CHD including chest pain; pain worsened with exertion, stress, and eating; relief after resting; discomfort for >3 months; pain through the back between the shoulder blades; and elevated blood pressure. In addition, a key nonverbal cue was incorporated, demonstrated by the “Levine fist,” where the patient clenched his fist to the sternum (Marcus et al., 2007). This single script was used for all videotapes presented to the physicians. Thus, all videotapes had exactly the same text. The patient in the videotapes was portrayed as consulting this doctor for the first time with these symptoms.
The portrayed physicians and patients in the United States had American accents, and the very same vignette physicians and patients in the United Kingdom had British accents. In Germany, the physician and patient voices were dubbed by a professional speaker. Professional actors were trained under experienced physician supervision to realistically portray a patient presenting the symptoms of disease to a primary care provider. Care was taken to construct a culturally neutral set, neutral clothes, and a cultureneutral facial expression.
The video was presented to primary care doctors in their practice. Actors on the tapes differed according to gender (male vs. female), age (55 vs. 75 years), race (black vs. white), and social status (low vs. high) to mirror respective patient characteristics. In the present analyses, we focus on differences between female and male patients.
Instruments
One CHD video was presented to each physician. Thereafter, physicians were asked various questions regarding diagnosis and treatment in a personal interview with standardized and open-ended questions. In terms of diagnostic decision making, the first question was whether the physician would ask the patient any additional questions and if so, what kind of question(s). Second, doctors were asked what they thought was going on with the patient and how certain they were with their diagnostic decision. Moreover, physicians were asked to name diagnostic tests they would order for this patient. In terms of the management of the patient, we wanted to know if they would prescribe or recommend any medication, if they would refer the patient to another health care professional, and when they would like to see the patient again. Finally, physicians were asked if they would recommend any lifestyle advice or behavior change.
Physician Sample
Physicians were randomly selected from lists provided by local health care organizations. Selection was made within 4 strata, defined by combinations of the physicians' gender and length of clinical experience (<5 years or >15 years). To be eligible for participation, physicians had to be internists or family practitioners in the United States and in Germany or general practitioners in the United Kingdom. In addition, they had to be working at least half time and had to be trained at an accredited medical school in the country in which they were practicing. A letter of invitation was sent to selected doctors who met these criteria. Thereafter, screening telephone calls were conducted to identify eligible physicians and an appointment was scheduled for a 1-hour, in-person, structured interview conducted in the physician's practice. Each physician subject was provided a modest stipend to partially offset lost revenue and to acknowledge their participation. The response rate was 64.9% in the United States, 59.6% in the United Kingdom, and 65.0% in Germany. Altogether, 384 interviews were conducted in the United States (Massachusetts) in the United Kingdom (the West Midlands, SW London, and Surrey) and in Germany (North Rhine-Westphalia). The final sample included 64 female and 64 male primary care doctors in each country, half of them with <5 years of clinical experience, the other half with >15 years. For a sample size of 128 per country the design has 80% power to detect differences of 25%. For example, if 25% of physicians would refer a female patient to a cardiologist/specialist facility and 50% of physicians would refer a male patient to a cardiologist/specialist facility (a difference of 25%), then we would expect to find a significant difference (at alpha = 0.05) 80% of the time. For a sample size of 384 (all 3 countries), the design has 80% power to detect of difference of 14.5%.
Analyses
Analysis of variance (ANOVA) was used to assess the effect of patients' gender on doctors' diagnostic and therapeutic decisions. Because a balanced factorial design was used, the effects due to patient gender are unconfounded (orthogonal to) with the other design effects (patient age, socioeconomic status, and race, as well as physician gender and physician level of experience). Precise p-values are reported in the tables. p <.05 was considered significant. For the data analysis of the open-ended questions, coding frames were developed and answers were summarized into categories (e.g., antihyperlipidemics, (β-blockers, calcium channel blockers, salicylates, and vasodilating agents were coded as CHD-appropriate prescriptions). These coding frames were finalized after achieving >90% intercoder reliability between medical advisers in the 3 countries.
Results
Questioning
Table 1 shows that women presenting with CHD symptoms would generally receive less attention than men. They would be asked fewer questions in the United Kingdom and in the United States, although this gender difference failed to reach statistical significance (p < .05). Moreover, the topics of the questions differ between women and men. This especially holds for the United Kingdom, where significantly more men would have been asked about their medical history, about smoking, alcohol consumption, and their psychological state, whereas significantly more women would have been asked about their general health status. In Germany, women are significantly less likely to be asked about smoking and alcohol, and in the United States gender differences are significant only for questions about smoking. Looking at the 3 countries together, the gender differences in all areas of physician's questioning are significant (p < .05).
Table 1. Gender comparison of the total number and kind of questions physicians would ask the patient by country.
| All 3 Countries | Germany | UK | US | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||||
| Male | Female | p | Male | Female | p | Male | Female | p | Male | Female | p | |
| No. of questions (mean) | 6.2* | 5.3* | .012* | 3.2 | 3.0 | .676 | 6.1 | 5.0 | .054 | 9.4 | 7.9 | .091 |
| Questions about (%) | ||||||||||||
| Medical history | 66* | 57* | .033* | 40 | 38 | .685 | 73* | 52* | .010* | 84 | 81 | .639 |
| Smoking | 55* | 29* | <.001* | 28* | 12* | .005* | 67* | 30* | <.001* | 69* | 45* | .004* |
| Alcohol | 32* | 17* | <.001* | 14* | 2* | .014* | 41* | 22* | .009* | 41 | 28 | .149 |
| Psychological state | 36* | 23* | .006* | 23 | 17 | .397 | 42* | 23* | .032* | 42 | 28 | .100 |
| General health status | 54* | 63* | .030* | 23 | 38 | .054 | 55* | 69* | .010* | 83 | 83 | 1.000 |
p < .05.
CHD Diagnosis
Table 2 shows that CHD was mentioned more often as a possible diagnosis for men than for women with a significant gender effect in Germany. In addition, on a scale from 0 (total uncertainty) to 100 (total certainty), doctors were significantly more certain of their CHD diagnosis with male than with female patients in the United Kingdom and in the United States. If they mentioned CHD as a possible diagnosis, significantly more doctors would order a test for CHD if the patient was a man in Germany. Again, looking at the 3 countries together, all gender differences related to the CHD diagnosis are significant at the 5% probability level.
Table 2. Gender comparison of correct CHD diagnosis, certainty of diagnosis, and test ordering for CHD by country.
| All 3 Countries | Germany | UK | US | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||||
| Male | Female | p | Male | Female | p | Male | Female | p | Male | Female | p | |
| CHD diagnosis (%) | 91* | 81* | .004* | 81* | 67* | .033* | 94 | 83 | .076 | 97 | 94 | .417 |
| Certainty of CHD diagnosis (0–100%) | 52* | 44* | .006* | 41 | 37 | .487 | 52* | 40* | .028* | 62* | 54* | .048* |
| Test for CHD (%) | 76* | 63* | .002* | 48* | 30* | .027* | 88 | 73 | .065 | 92 | 86 | .252 |
| No. of tests for CHD (mean) | 2.8* | 2.3* | .015* | 1.1 | 0.7 | .095 | 4.0 | 3.1 | .073 | 3.4 | 3.0 | .386 |
Abbreviation: CHD, coronary heart disease.
p < .05.
Therapy
As shown in Table 3, gender differences were also evident in doctors' management decisions. In the United Kingdom, men would be significantly more likely than women to receive an appropriate prescription for possible CHD after the first contact. Moreover, men would be more likely to be referred to a cardiologist or a specialist facility in Germany and in the United Kingdom. Gender difference in days to the next appointment was not significant in any country. Effects of patient's gender on therapeutic decisions were nonsignificant in the United States.
Table 3. Gender differences in the therapy for CHD by country.
| All 3 Countries | Germany | UK | US | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||||
| Male | Female | p | Male | Female | p | Male | Female | p | Male | Female | p | |
| CHD appropriate prescription (%) | 50* | 39* | .015* | 22 | 12 | .139 | 58* | 39* | .044* | 70 | 64 | .458 |
| Referral to a cardiologist or specialist facility (%) | 25* | 15* | .011* | 27* | 11* | .037* | 39* | 23* | .037* | 9 | 11 | .764 |
| Referral to other medical professional (%) | 33* | 25* | .044* | 61* | 42* | .027* | 31 | 30 | .853 | 8 | 3 | .185 |
| Days to next appointment (mean) | 9.6 | 10.5 | .167 | 4.7 | 6.8 | .080 | 12.3 | 14.0 | .218 | 11.8 | 10.7 | .510 |
Abbreviation: CHD, coronary heart disease.
p < .05.
Advice Giving
Doctors were asked if they would give the patient any advice to change their lifestyle behavior. Table 4 shows that on average 2.5 pieces of advice would be given to the patient across all countries combined. The amount of advice did not vary by gender overall or within a given country. Advice about smoking would be given to more male than female patients, although this failed to reach statistical significance (p < .05) in each of the 3 countries. There was only 1 significant difference in advice giving by patients' gender: Physicians would only recommend reducing weight if the patient was a man in Germany.
Table 4. Gender differences in the lifestyle advice for patients with CHD by country.
| All 3 Countries | Germany | UK | US | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||||
| Male | Female | p | Male | Female | p | Male | Female | p | Male | Female | p | |
| No. pieces of advise (mean) | 2.5 | 2.5 | .786 | 1.9 | 1.8 | .780 | 2.8 | 3.1 | .270 | 2.9 | 2.7 | .641 |
| Advice about (%) | ||||||||||||
| Diet | 52 | 54 | .537 | 50 | 52 | .858 | 47 | 59 | .149 | 58 | 53 | .603 |
| Smoking | 38* | 26* | .004* | 12 | 5 | .137 | 62 | 47 | .073 | 39 | 25 | .088 |
| Alcohol | 21 | 21 | 1.000 | 8 | 12 | .321 | 36 | 36 | 1.000 | 20 | 15 | .441 |
| Relaxation | 9 | 7 | .578 | 10 | 6 | .369 | 11 | 11 | 1.000 | 5 | 5 | 1.000 |
| Weight | 5 | 4 | .809 | 6* | 0* | .049* | 6 | 9 | .529 | 2 | 3 | .566 |
Abbreviation: CHD, coronary heart disease.
p < .05
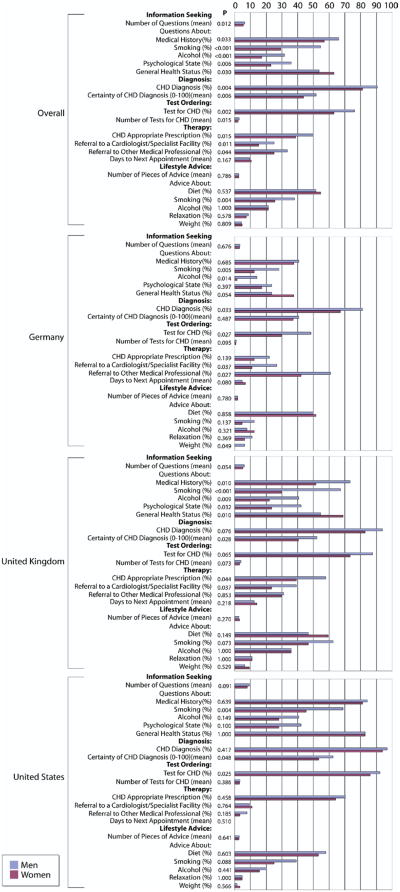
Figure 1 summarizes the results on gender differences in clinical decision making overall and by country. Although the significance level of many factors varies by county, it should be noted that there were no significant country by gender interactions (p > .05 for all tests).
Figure 1.
Gender differences in clinical decision making overall and by country.
Discussion
This paper focuses on the role of patient gender for clinical decision making in CHD in the United States, United Kingdom, and Germany. Because vignettes are a valid and comprehensive method for measuring the quality of care provided by physicians (Peabody, Luck, Glassman, Dresselhaus, & Lee, 2000), a factorial experiment with video vignettes was conducted in the 3 countries. Results show gender differences in the diagnostic strategies of the doctors (information seeking, possible diagnosis). Although there are cross-national differences in magnitude, indicating strongest effects of gender on doctors' questioning in the United Kingdom, a consistent general trend can be observed in all countries: Female patients would receive less questioning and were less likely to receive an accurate diagnosis by primary care doctors. Moreover, results indicate that differences in therapy decisions (prescription, referrals, and lifestyle advice) according to patients' gender are less pronounced and less consistent than in diagnostic decisions.
Gender differences in physician decision making among patients presenting with symptoms of CHD were described earlier (Arber et al., 2004, 2006). Based on this knowledge, we have chosen a comparative perspective for our analyses. Although all 3 countries show a similar trend, the magnitude of the gender effect on doctors' decisions varies between countries with smaller influences of the patient's gender in the United States.
Stereotypical beliefs about what kinds of patients are at risk for CHD might influence the decision making process (Arber et al., 2004, 2006; Adams et al., 2006; Bönte et al., 2007). If those stereotypes are aligned with the knowledge of sociodemographic differences in the risk structure of CHD, this strategy could lead to a more precise targeting of diagnostic and therapeutic arrangements. But working with standardized videotaped patients, where all male and female actors express exactly the same symptoms, treatment differences are not indicated. In fact, lower detection rates of CHD among female patients could have serious consequences for their health. It seems that the epidemiologic knowledge of higher CHD rates among men could lead the doctors to concentrate their attention on a coronary diagnosis among male patients and to underdiagnose CHD among women. This assumption is supported by the fact that gender differences in the diagnosis of CHD in the present study are more pronounced among midlife patients (55 years) than among older patients (75 years; results not shown). This “gendered ageism” (Arber et al., 2006) can be seen in the context of known prevalence and risk profiles. Well-known variations in illness rates by gender are therefore not only a consequence of differences in the biological or behavioral risk structure, but might also be socially constructed (Hor-ton, 2007). In a qualitative work, Adams et al. (2007) explored sources of gender bias in the decision making process of primary care doctors in the United Kingdom and United States. During the interviews that were part of the present study, doctors were asked to explain and justify diagnostic and therapeutic decisions for a CHD patient. Findings revealed an interaction of physicians' and patients' gender. Male doctors appeared less affected by patient gender, but both male and especially female doctors took more account of male patients' age and considered more age-related disease possibilities for men than women. It is a future task to analyze the qualitative data collected in the present study to provide more information on how patient gender affects doctors' cognitive processes during consultations.
Although the rigorous experimental design permits excellent internal validity, external validity remains a threat. Several precautionary steps were taken to minimize this threat. The physicians were specifically instructed to view the patient on the videotape as one of their own cases. In addition, the doctors viewed the tapes in the context of their practice day and not at a professional meeting, a course update, or in their home. Thus, it was likely they encountered real patients before and after they viewed the patient in the videotape. To enhance the clinical authenticity of the videotaped patient, the script of the vignette was based on role plays conducted with skilled physicians. During the production of the videos, experienced clinicians were present, and only professional and experienced actors were used. At the beginning of each interview, doctors were asked how typical the videotaped patient was compared with patients they see in their practice. In the United States, 90.6% of doctors, and 91.4% in the United Kingdom, and 81.3% in Germany considered them as very or reasonably typical. Using Tukey's multiple comparisons to test for differences between the 3 countries, we found that rating in Germany is significantly (p = .0102) lower than in the United Kingdom or in the United States. The lower rate in Germany might be a result of the dubbing that makes the scenario more unrealistic than in the 2 other countries.
Additionally, interviewers were carefully trained and certified and frequent transatlantic telephone calls were conducted to ensure standardized interviewing and to minimize interviewer variability (Johannes, Crawford, & McKinlay, 1997). Quality control interviews and site visits were conducted and selected tape recorded interviews were reviewed by supervisors on a regular basis to minimize variation within the 3 countries.
However, although substantial effort was devoted to produce the video vignettes as realistic as possible, videotapes are not the same as real patients. Diagnostic and therapeutic decisions result through the interaction of doctor and patient. This issue could not be addressed in a videotape-based experiment. In addition, doctors might have viewed the interview as a test. This could potentially bias the answers in the direction of social acceptability. To avoid this, the doctors were told that the interview is not a test and that there are no right or wrong answers.
These (potential) limitations are counterbalanced by several strengths. Through the factorial experimental approach, relevant influences on the decision-making process are controlled by the study design. This allows the estimation of the independent and unconfounded effects of the respective factors (e.g., gender of the patient) (Cochran & Cox, 1957; Feldman et al., 1997; Kirk, 1982). Moreover, the design offers the possibility to integrate nonverbal signs like the “Levine fist.” Finally, physicians were randomly selected to enhance generalizability.
In conclusion, gender differences in the diagnosis and management of CHD seem to be a generalized, although not invariant phenomenon. Future studies should give more attention to international variations in health care disparities to determine the contribution of the health care system to such disparities (McKinlay et al., 2006). To improve our understanding of the women's role as well as her cultural and socioeconomic status, other countries should be included in respective studies. Findings should be part of the physicians' further training in order to reduce gender disparities in the daily medical practice.
Acknowledgments
Supported by Grant No. AG 16747 from the National Institute on Aging, NIH.
References
- Adams A, Buckingham C, Arber S, McKinlay JB, Marceau L, Link C. The influence of patient's age on clinical decision-making about coronary heart disease in the USA and the UK. Ageing and Society. 2006;26:303–321. [Google Scholar]
- Adams A, Buckingham CD, Lindenmeyer A, McKinlay JB, Link C, Marceau L, et al. The influence of patient and doctor gender on diagnosing coronary heart disease. [Accessed September 5, 2007];Sociology of Health and Illness. 2007 29(2) doi: 10.1111/j.1467-9566.2007.01025.x. Available: www.blackwell-synergy.com/toc/shil/0/0. [DOI] [PubMed] [Google Scholar]
- Anand SS, Xie CC, Mehta S. Differences in the management and prognosis of women and men who suffer from acute coronary syndromes. Journal of the American College of Cardiology. 2005;46:1845–1851. doi: 10.1016/j.jacc.2005.05.091. [DOI] [PubMed] [Google Scholar]
- Arber S, McKinlay JB, Adams A, Marceau L, Link C, O'Donnell A. Influence of patient characteristics on doctors' questioning and lifestyle advice for coronary heart disease: A UK/US video experiment. British Journal of General Practice. 2004;54:673–678. [PMC free article] [PubMed] [Google Scholar]
- Arber S, McKinlay JB, Adams A, Marceau L, Link C, O'Donnell A. Patient characteristics and inequalities in doctors' diagnostic and management strategies relating to CHD: A video-simulation experiment. Social Science & Medicine. 2006;62:103–115. doi: 10.1016/j.socscimed.2005.05.028. [DOI] [PubMed] [Google Scholar]
- Blendon RJ, Schoen C, DesRoches C, Osborn R, Zapert K. Common Concerns amid Diverse Systems: Health Care Experiences in Five Countries. Health Affairs. 2003;22:106–121. doi: 10.1377/hlthaff.22.3.106. [DOI] [PubMed] [Google Scholar]
- Blendon RJ, Schoen C, DesRoches C, Osborn R, Zapert K, Raleigh E. Confronting competing demands to improve quality: A five-country hospital survey. Health Affairs. 2004;23:119–135. doi: 10.1377/hlthaff.23.3.119. [DOI] [PubMed] [Google Scholar]
- Bönte M, Knesebeck Ovd, Siegrist J, Marceau L, Link C, McKinlay JB. Einflüsse des Patientenalters und des Patientengeschlechts auf ärztliche Entscheidungen bei koronarer Herzkrankheit [Influence of patient's gender and age on doctors' decision making about coronary heart disease] Deutsche Mediz-inische Wochenschrift. 2007;132:1–6. doi: 10.1055/s-2007-991637. [DOI] [PubMed] [Google Scholar]
- Bond M, Bowling A, McKee D, Kenelly M, Banning AP, Dudley N, et al. Does ageism affect the management of ischaemic heart disease? Journal of Health Services Research & Policy. 2003;8:40–47. doi: 10.1177/135581960300800109. [DOI] [PubMed] [Google Scholar]
- Cochran WG, Cox DM. Experimental designs. New York: John Wiley & Sons; 1957. [Google Scholar]
- Derby CA, Lapane KL, Feldman HA, Carleton RA. Sex-specific trends in validated coronary heart disease rates in southeastern New England, 1980–1991. American Journal of Epidemiology. 2000;151:417–429. doi: 10.1093/oxfordjournals.aje.a010222. [DOI] [PubMed] [Google Scholar]
- Central Health Monitoring Unit. Coronary heart disease An epidemiological overview. London: Her Majesty's Stationery Office (HMSO); 1994. [Google Scholar]
- Chou AF, Scholle SH, Weisman CS, Bierman AS, Correa-de-Araujo R, Mosca L. Gender disparities in the quality of cardiovascular disease care in private managed care plans. Women's Health Issues. 2007;17:120–130. doi: 10.1016/j.whi.2007.03.002. [DOI] [PubMed] [Google Scholar]
- Correa-de-Araujo R, Stevens B, Moy E, Nilasena D, Chesley F, McDermott K. Gender differences across racial and ethnic groups in the quality of care for acute myocardial infarction and heart failure associated with co-morbidities. Women's Health Issues. 2006;16:44–55. doi: 10.1016/j.whi.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Feldman HA, Freund KM, Burns RB, Moskowitz MA, Kasten LE. Nonmedical influences on medical decision making: An experimental technique using videotapes, factorial design, and survey sampling. Health Services Research. 1997;32:343–366. [PMC free article] [PubMed] [Google Scholar]
- Frich JC, Malterud K, Fugelli P. Women at risk of coronary heart disease experience barriers to diagnosis and treatment: a qualitative interview study. Scandinavian Journal of Primary Health Care. 2006;24:38–43. doi: 10.1080/02813430500504305. [DOI] [PubMed] [Google Scholar]
- Herlitz J, McGovern P, Dellborg M, Karlsson T, Duval S, Karlson BW, et al. Comparison of treatment and outcomes for patients with acute myocardial infarction in Minneapolis/St. Paul, Minnesota, and Goteborg, Sweden. American Heart Journal. 2003;146:1023–1029. doi: 10.1016/S0002-8703(03)00531-3. [DOI] [PubMed] [Google Scholar]
- Horton K. Gender and the risk of falling: a sociological approach. Journal of Advanced Nursing. 2007;57:69–76. doi: 10.1111/j.1365-2648.2006.04061.x. [DOI] [PubMed] [Google Scholar]
- Johannes CB, Crawford SL, McKinlay JB. Interviewer effects in a cohort study. Results from the Massachusetts Women's Health Study. American Journal of Epidemiology. 1997;146:429–438. doi: 10.1093/oxfordjournals.aje.a009296. [DOI] [PubMed] [Google Scholar]
- Kirk RE. Experimental design. Belmont, CA: Brooks-Cole; 1982. [Google Scholar]
- Marcus GM, Cohen J, Varosy PD, Vessey J, Rose E, Massie BM, et al. The utility of gestures in patients with chest discomfort. The American Journal of Medicine. 2007;120:83–90. doi: 10.1016/j.amjmed.2006.05.045. [DOI] [PubMed] [Google Scholar]
- McKinlay JB, Link C, Arber S, Marceau L, O'Donnell A, Adams A. How do doctors in different countries manage the same patient? Results of a factorial experiment. Health Services Research. 2006;41:2182–2201. doi: 10.1111/j.1475-6773.2006.00595.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinlay JB, Lin T, Freund K, Moskowitz M. The unexpected influence of physician attributes on clinical decisions: Results of an experiment. Journal of Health and Social Behavior. 2002;43:92–106. [PubMed] [Google Scholar]
- Mendelsohn ME. The protective effects of estrogen on the cardiovascular system. American Journal of Cardiology. 2002;89:12–17. doi: 10.1016/s0002-9149(02)02405-0. [DOI] [PubMed] [Google Scholar]
- Mikhail GW. Coronary revascularisation in women. Heart. 2006;92(Suppl 3):iii19–iii23. doi: 10.1136/hrt.2005.070359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2005 With chartbook on trends in the health of Americans. Hyatts-ville, MD: Public Health Service; 2005. [PubMed] [Google Scholar]
- Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M. Comparison of vignettes, standardized patients, and chart abstraction: A prospective validation study of 3 methods for measuring quality. The Journal of the American Medical Association. 2000;283:1715–1722. doi: 10.1001/jama.283.13.1715. [DOI] [PubMed] [Google Scholar]
- Raine R. Does gender bias exist in the use of specialist healthcare? Journal of Health Services Research & Policy. 2000;5:237–249. doi: 10.1177/135581960000500409. [DOI] [PubMed] [Google Scholar]
- Rossouw JE, Prentice RL, Manson JE, Wu L, Barad D, Barnabei VL, et al. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since Menopause. Journal of the American Medical Association. 2007;297:1465–1477. doi: 10.1001/jama.297.13.1465. [DOI] [PubMed] [Google Scholar]
- Schoen C, Osborn R, Huynh PT, Doty M, Davis K, Zapert K, et al. Primary care and health system performance: Adults' experiences in five countries. Health Affairs. 2004;W4.487:487–503. doi: 10.1377/hlthaff.w4.487. [DOI] [PubMed] [Google Scholar]
- Statistisches Bundesamt. Gesundheit in Deutschland. Berlin: Robert Koch Institut; 2006. [Google Scholar]
- Tunstall-Pedoe H, Morrison C, Woodward M, Fitzpatrick B, Watt G. Sex differences in myocardial infarction and coronary deaths in the Scottish MONICA population of Glasgow 1985–1991. Circulation. 1996;93:1981–1992. doi: 10.1161/01.cir.93.11.1981. [DOI] [PubMed] [Google Scholar]
- Van Ryn M, Fu SS. Paved with good intentions: Do public health and human service providers contribute to racial/ethnic disparities in health? American Journal of Public Health. 2003;93:248–255. doi: 10.2105/ajph.93.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]