Abstract
Objectives
The Walking Impairment Questionnaire (WIQ) measures self-reported walking distance, walking speed, and stair-climbing ability in men and women with lower extremity peripheral arterial disease (PAD). We determined whether poorer WIQ scores are associated with higher all-cause and cardiovascular disease (CVD) mortality in individuals with and without PAD.
Methods
1048 men and women with and without PAD were identified from Chicago-area medical centers. Participants completed the WIQ at baseline and were followed for a median of 4.5 years. Cox proportional hazards models were used to relate baseline WIQ scores with mortality, adjusting for age, sex, race, the ankle brachial index (ABI), comorbidities, and other covariates.
Results
461 participants (44.0%) died during follow-up, including 158 deaths from cardiovascular disease. PAD participants in the lowest baseline quartile of the WIQ stair-climbing scores had higher all-cause mortality (HR = 1.70 [95% Confidence Interval (CI) 1.08-2.66, p=0.02] and higher CVD mortality (HR = 3.11 [95% CI 1.30 – 7.47, p=0.01]) compared to those with the highest baseline WIQ stair climbing score. Among PAD participants there were no significant associations of lower baseline WIQ distance or speed scores with rates of all-cause mortality (p for trend = 0.20 and 0.07, respectively) or CVD mortality (p for trend = 0.51 and p for trend = 0.33, respectively). Among non-PAD participants there were no significant associations of lower baseline WIQ stair climbing, distance, or speed score with rates of all-cause mortality (p for trend = 0.94, 0.69, and 0.26, respectively) or CVD mortality (p for trend = 0.28, 0.68, and 0.78, respectively).
Conclusions
Among participants with PAD, lower WIQ stair climbing scores are associated with higher all-cause and CVD mortality, independently of the ABI and other covariates.
INTRODUCTION
Lower extremity peripheral arterial disease (PAD) is a common condition that affects more than 8 million Americans(1). Compared to persons without PAD, affected individuals are at significantly increased risk for all-cause and cardiovascular mortality(2). Objective measures that predict survival in men and women with PAD include the ankle brachial index (ABI)(3) and functional performance measures, such as the six-minute walk test and four-meter walking velocity (4).
Subjective measures of overall health status that include assessment of general mobility, such as the EuroQol Questionnaire, have been used in recent studies to predict survival in participants with PAD(5). The Walking Impairment Questionnaire (WIQ) was developed as a simple self-administered instrument to measure self-reported walking distance, walking speed, and stair climbing limitations in patients with PAD in the outpatient setting (6). We investigated associations of the WIQ distance, speed, and stair-climbing scores with all-cause and cardiovascular disease mortality in individuals with PAD and without PAD. We hypothesized that lower WIQ scores would be associated with higher all-cause and CVD mortality among participants with PAD and without PAD. If our hypotheses are correct, the WIQ could potentially be used by clinicians to assess mortality risk in patients with PAD and without PAD.
METHODS
Participant Identification
Participants for this analysis were identified from the Walking and Leg Circulation Study (WALCS) and WALCS II studies. The WALCS and WALCS II are prospective, observational studies designed to identify clinical characteristics associated with functional impairment, functional decline, and mortality in men and women with PAD (7, 8). The WALCS cohort was assembled from October 1998 to March 2000. The WALCS II cohort was assembled from November 2002 to April 2004. WALCS II included WALCS participants who were alive and consented to participation in WALCS II as well as newly identified participants. WALCS participants were followed for up to eight years, while newly identified participants for WALCS II were followed for up to four years. For both WALCS and WALCS II, PAD participants were identified consecutively from among patients diagnosed with PAD in three Chicago-area non-invasive vascular diagnostic laboratories. Participants without PAD were identified from among consecutive patients in a general medicine practice at Northwestern University and had an ABI of 0.90 and greater and less than 1.40. The institutional review boards of Northwestern University and collaborating sites approved the study protocol. Written informed consent was obtained.
Exclusion criteria
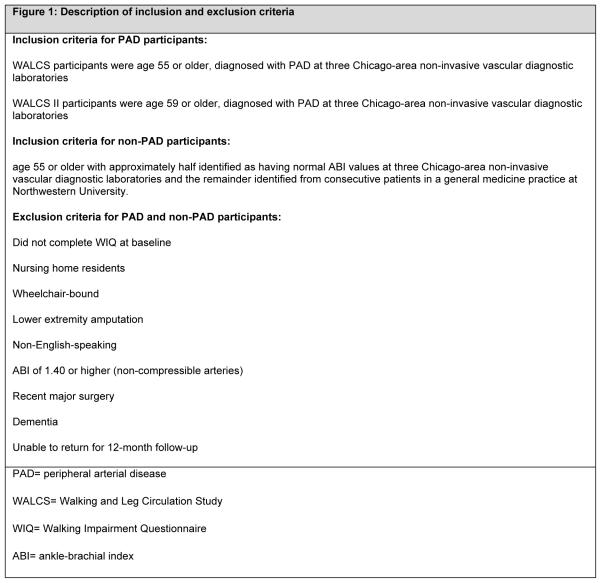
For participants with PAD, we excluded individuals with an ABI ≥ 0.90 at baseline because they either did not have PAD or because they had non-compressible arteries which did not allow accurate assessment of PAD severity. At enrollment for WALCS and WALCS II, PAD and non-PAD persons with above- or below-knee amputations or ulcers, nursing home residents and wheelchair-bound patients were excluded due to severely limited functional capacity at baseline. Participants with prior lower extremity revascularization procedures were not excluded. Non-English-speaking participants were excluded as the data collectors were fluent only in the English language. At baseline, participants with recent major surgery and self-identified or physician-identified dementia as well as those unlikely to return for 12-month follow-up because of medical illness or logistical issues were excluded (Figure 1).
Figure 1.
Description of inclusion and exclusion criteria
Walking Impairment Questionnaire
Participants self-administered the WIQ forms at baseline. In the WIQ distance score, the participant is asked to assess the degree of difficulty in walking specific distances (ranging from walking indoors to 1500 feet, or 5 blocks) on a graded scale from zero to four. A score of zero represents the inability to walk the distance in question and a score of four represents no difficulty. In the WIQ speed score, the participant is asked to assess the degree of difficulty in walking one block at specific speeds ranging from walking slowly to jogging on a graded scale ranging from zero to four. In the WIQ stair-climbing score, the participant is asked to report the degree of difficulty climbing specific numbers of flights of stairs ranging from one to three flights of stairs on a graded scale ranging from zero to four. This graded score is multiplied by a pre-specified weight for each distance, speed, or number of stair flights. The products are summed and divided by the maximum possible score to obtain a percent score, ranging from 0 (representing the inability to perform any of the tasks) to 100 (representing no difficult with any of the tasks) (9). The WIQ scores have been shown to improve in response to lower extremity revascularization (10) and supervised exercise therapy(11).
ABI measurement
Using a handheld Doppler probe (Nicolet Vascular Pocket Dop II, Nicolet Biomedical, Golden, Colorado), systolic pressures were measured in the right and left brachial, posterior tibial, and dorsalis pedis arteries and then again in reverse order. The ABI was calculated by dividing the mean of the posterior tibial and dorsalis pedis pressures in each leg by the mean of the four brachial pressures (12). Average brachial pressures in the arm with highest pressure were used when one brachial pressure was higher than the opposite brachial pressure in both measurement sets and the two brachial pressures differed by 10 or more mmHg in at least one measurement set, because in such cases, subclavian stenosis is possible (13). The lowest leg ABI was used in the analyses. This method was used as it has been shown to be the most closely associated with impaired lower extremity functioning (12).
Comorbidities
We measured and verified baseline comorbidities that would potentially influence WIQ scores and mortality: history of congestive heart failure, angina, myocardial infarction, diabetes, cancer and chronic pulmonary disease. This was done using algorithms developed for the Women’s Health and Aging Study(17) which combine data from medical record review, medications, patient self-report, selected laboratory values, and a questionnaire completed by the participant’s primary care provider.
Participant-reported physical activity
At the initial study visit, participant-reported physical activity was measured with a questionnaire derived from the Harvard Alumni Activity Study that has previously been validated in participants with PAD (18). Participants were asked the following question: “During the last week, how many city blocks or their equivalent did you walk? Let 12 city blocks equal 1 mile.”
Other measures
At the initial visit, height and weight were measured and body mass index (BMI) was calculated by dividing the weight in kilograms by the square of the height in meters. Cigarette smoking history was self-reported. Leg symptoms for PAD participants were characterized using the San Diego claudication questionnaire (19). Participants were classified into previously described symptom categories as follows: 1) asymptomatic PAD (no exertional leg symptoms); 2) intermittent claudication (exertional calf pain that does not begin at rest, causes the participant to stop walking, and resolves within 10 minutes of rest), 3) pain on exertion and rest (exertional leg symptoms that sometimes begin at rest); 4) atypical exertional leg pain/carry on (exertional leg pain that does not cause the participant to stop walking); 5) atypical exertional leg pain/stop (exertional leg pain that does not begin at rest, causes the participant to stop walking, and is otherwise atypical because it does not involve the calf or does not resolve within 10 minutes of rest)(20).
Six-minute walk distance and four meter walking velocity (usual and fast paced) were measured at baseline using previously published methods.(14-16)
The principal study investigator reviewed the medication list for each participant at the initial visit, unaware of all other patient data, and identified the use of statins and ACE inhibitors for each participant.
Death
Information on deaths was obtained annually from proxies, the Social Security Administration death database, and primary care providers. Death certificate information from the state in which the death occurred, family members, or from the participants’ medical records was also obtained. Deaths from cardiovascular disease (CVD) were those with ICD-10 codes in the range I00.0 through I99. This included deaths due to stroke, peripheral vascular disease, coronary heart disease and sudden cardiac death.
Statistical analyses
Age-adjusted baseline characteristics of participants across quartiles of each WIQ score (distance, speed, and climb score) were compared using linear models for continuous variables and logistic models for categorical variables.
Proportional hazards analyses were used to compare differences in all-cause and CVD mortality across WIQ score quartiles, with the highest (best) quartile for each WIQ domain used as the referent. The use of WIQ score quartiles, as opposed to continuous WIQ score values, was to facilitate assessment for a threshold effect as well as to allow findings to be more accessible to the practicing clinician. Pairwise comparisons were performed with p values calculated between the lowest (first or worst) and highest (fourth or best) quartile, between the second and fourth quartile, and between the third and fourth quartile. Overall p for trend was also calculated. Analyses were adjusted for age, sex, race, ABI, BMI, current smoking status, comorbidities (history of congestive heart failure, angina, myocardial infarction, diabetes, cancer and chronic pulmonary disease), statin and ACE inhibitor use, and physical activity. Follow-up of participants was not censored after a medical intervention.
An additional analysis was done to estimate Pearson correlation coefficients to measure the strength of association between the WIQ domain scores and baseline ABI, among PAD participants.
RESULTS
Baseline Characteristics
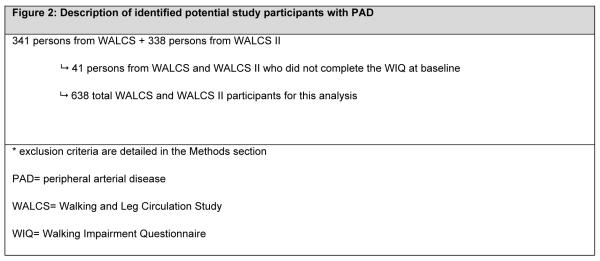
Figure 2 depicts reasons for exclusion among individuals identified for the study. Of the 679 participants with PAD from WALCS and WALCS II, 41 (6.0%) participants were excluded from the analyses because they did not complete the WIQ at baseline. Of the 431 participants without PAD from WALCS and WALCS II, 21 (5.1%) were excluded from the analyses for the same reason. Baseline characteristics did not differ between those who completed the WIQ vs. those who did not (Table I).
Figure 2.
Description of identified potential study participants with PAD
Table I. Baseline Clinical Characteristics of Peripheral Arterial Disease Participants With and Without Walking Impairment Questionnaire.
| Without WIQ (N=41) |
With WIQ (N=638) |
p value | |
|---|---|---|---|
| Age, y | 72.4 (10.2) | 72.7 (8.3) | 0.82 |
| Male, % | 56.1 | 56.6 | 0.95 |
| Black race, % | 24.4 | 16.8 | 0.21 |
| ABI | 0.64 (0.1) | 0.65 (0.2) | 0.79 |
| BMI, kg/m2 | 26.5 (4.9) | 27.7 (5.1) | 0.15 |
| Current Smoker, % | 22.0 | 18.1 | 0.62 |
| Angina, % | 26.8 | 33.5 | 0.38 |
| CHF, % | 29.3 | 22.7 | 0.34 |
| MI, % | 22.0 | 24.6 | 0.70 |
| Pulmonary Disease, % | 41.3 | 35.7 | 0.46 |
| Cancer, % | 19.5 | 17.6 | 0.75 |
| Diabetes, % | 39.0 | 31.8 | 0.34 |
| Blocks walked in the past week, n | 32.1 (70.1) | 32.5 (56.1) | 0.96 |
Values shown are mean (Standard deviation) unless otherwise indicated. WIQ = Walking Impairment Questionnaire; PAD = peripheral arterial disease; ABI = ankle brachial index; BMI = body mass index; CHF = congestive heart failure; MI = myocardial infarction.
Overall, in the entire PAD cohort, mean age was 72.7 years ± 8.4 years, ABI was 0.65 ± 0.15, and prevalence of intermittent claudication was 32%. In the non-PAD cohort, mean age was 71.5 ± 7.7 years, and ABI was 1.09 ± 0.09.
Two hundred twenty-one (34.6%) PAD participants died during a median follow-up of 4.5 years. Of these, 78 deaths (35.3%) were attributed to cardiovascular disease. 10 repeated imputations were used in competing risk analyses in cases where death certificates were unobtainable. Table II lists the age-adjusted baseline characteristics of PAD participants by WIQ stair-climbing, WIQ distance, and WIQ speed score quartiles. Lowest (worst) quartiles for the WIQ stair-climbing score were associated with fewer blocks walked in the past week, higher BMI, and higher prevalences of females, black race, angina, heart failure, prior myocardial infarction, and pulmonary disease. Lower PAD participant WIQ stair-climbing scores were also associated with a higher prevalence of pain on exertion and rest, a lower prevalence of atypical exertional leg pain/carry on, and a lower prevalence of asymptomatic PAD.
Table II. Age-adjusted Clinical Characteristics of Peripheral Arterial Disease Participants Across WIQ Score Quartiles (n=638).
| WIQ Stair Climbing Score Quartiles | |||||
|---|---|---|---|---|---|
| 1st Quartile [≤ 25.0] |
2nd Quartile [25.0 – 41.7] |
3rd Quartile [41.7 – 66.7] |
4th Quartile [> 66.7] |
p for trend |
|
| Male, % | 40.3* | 52.2* | 63.2 | 73.9* | < 0.001 |
| Black race, % | 23.3 | 11.3 | 13.9 | 16.4 | 0.06 |
| ABI | 0.64 (0.01) | 0.63 (0.01) | 0.66 (0.01) | 0.66 (0.01) | 0.10 |
| BMI, kg/m2 | 29.0* (0.4) | 27.2 (0.4) | 27.5 (0.4) | 26.6 (0.4) | < 0.001 |
| Current Smoker, % | 15.6 | 18.8 | 16.1 | 19.0 | 0.37 |
| Angina, % | 36.0* | 41.8 | 30.8 | 25.8 | 0.01 |
| CHF, % | 32.7* | 29.2 | 13.7 | 15.6* | < 0.001 |
| MI, % | 31.0* | 28.4 | 23.4 | 14.9* | 0.002 |
| Pulmonary Disease, % | 49.9* | 37.1 | 31.6 | 22.2* | < 0.001 |
| Cancer, % | 12.0 | 20.1 | 21.1 | 16.7 | 0.31 |
| Diabetes,% | 40.0 | 26.2 | 25.3 | 31.1 | 0.05 |
| Blocks walked in the past week, n |
14.3* (4.1) | 26.5* (4.6) | 43.4 (4.1) | 48.9 (4.6) | < 0.001 |
| Pain on exertion and rest | 35.1 | 22.1 | 11.3 | 7.68 | < 0.0001 |
| Atypical exertional leg pain/stop |
18.0 | 14.9 | 30.3 | 21.5 | 0.088 |
| Atypical exertional leg pain/carry on |
1.67 | 9.86 | 7.45 | 20.2 | < 0.0001 |
| Asymptomatic PAD | 19.2 | 12.7 | 20.4 | 28.4 | 0.015 |
| Intermittent claudication | 25.5 | 40.0 | 29.8 | 22.1 | 0.263 |
| Six minute walk, ft | 846.6 (24.5) | 1091.4 (27.0) | 1271.2 (24.1) | 1311.6 (27.1) | <.0001 |
| Four meter velocity at usual speed, m/sec |
0.74 (0.01) | 0.87 (0.02) | 0.94 (0.01) | 0.96 (0.02) | <.0001 |
| Four meter velocity at fast speed, m/sec |
1.00 (0.02) | 1.17 (0.02) | 1.27 (0.02) | 1.31 (0.02) | <.0001 |
| Statin use,% | 40.2 | 44.2 | 46.6 | 41.6 | 0.63 |
| Inhibitor use, % | 29.4 | 27.1 | 27.3 | 27.6 | 0.73 |
| WIQ Distance Score Quartiles | |||||
|---|---|---|---|---|---|
| 1st Quartile [≤ 14.5] |
2nd Quartile [14.5 – 37.1] |
3rd Quartile [37.1 – 67.9] |
4th Quartile [> 67.9] |
p for trend |
|
| Male, % | 49.0* | 53.5* | 56.6 | 67.9* | < 0.001 |
| Black race, % | 24.1 | 20.2 | 9.0 | 12.6* | 0.001 |
| ABI | 0.59* (0.01) | 0.64* (0.01) | 0.66* (0.01) | 0.70 (0.01) | < 0.001 |
| BMI, kg/m2 | 28.9* (0.4) | 27.8 (0.4) | 27.2 (0.4) | 26.7 (0.4) | < 0.001 |
| Current Smoker, % | 14.0 | 19.8 | 18.2 | 16.8 | 0.90 |
| Angina, % | 40.5 | 32.8* | 35.5 | 25.0* | 0.01 |
| CHF, % | 31.0 | 22.0 | 17.4 | 19.2* | 0.002 |
| MI, % | 31.6* | 27.7 | 20.6 | 17.3* | 0.001 |
| Pulmonary Disease, % | 46.4 | 32.8 | 35.7 | 28.6* | 0.001 |
| Cancer, % | 16.7 | 19.7 | 17.0 | 16.6 | 0.92 |
| Diabetes,% | 40.0 | 26.5 | 26.1 | 31.7 | 0.18 |
| Blocks walked in the past week, n |
10.9* (4.2) | 23.9* (4.1) | 31.4* (4.2) | 64.4 (4.2) | < 0.001 |
| Pain on exertion and rest | 32.4 | 19.9 | 18.1 | 7.65 | < 0.0001 |
| Atypical exertional leg pain/stop |
17.1 | 22.0 | 27.1 | 20.5 | 0.48 |
| Atypical exertional leg pain/carry on |
1.27 | 5.65 | 7.75 | 21.8 | < 0.0001 |
| Asymptomatic PAD | 11.3 | 15.1 | 15.7 | 38.5 | < 0.0001 |
| Intermittent claudication | 37.5 | 36.4 | 30.4 | 11.3 | < 0.0001 |
| Six minute walk, ft | 783.8 (24.6) | 1107.1 (24.0) | 1230.8 (24.2) | 1375.9 (24.2) | < 0.0001 |
| Four meter velocity at usual speed, m/sec |
0.76 (0.02) | 0.87 (0.02) | 0.91 (0.02) | 0.96 (0.02) | < 0.0001 |
| Four meter velocity at fast speed, m/sec |
1.03 (0.02) | 1.18 (0.02) | 1.24 (0.02) | 1.29 (0.02) | <.0.0001 |
| Statin use,% | 43.2 | 39.8 | 46.0 | 42.8 | 0.99 |
| Inhibitor use, % | 29.2 | 24.9 | 28.5 | 28.1 | 0.75 |
| WIQ Speed Score Quartiles | |||||
|---|---|---|---|---|---|
| 1st Quartile [≤ 17.4] |
2nd Quartile [17.4 – 32.6] |
3rd Quartile [32.6 – 54.3] |
4th Quartile [> 54.3] |
p for trend |
|
| Male, % | 47.5* | 50.4* | 58.2 | 71.4* | < 0.001 |
| Black race, % | 24.0 | 16.8 | 12.0 | 14.0* | 0.04 |
| ABI | 0.62* (0.01) | 0.62* (0.01) | 0.67 (0.01) | 0.68 (0.01) | < 0.001 |
| BMI, kg/m2 | 29.4* (0.4) | 27.6* (0.4) | 27.1 (0.4) | 26.5 (0.4) | < 0.001 |
| Current Smoker, % | 12.4 | 19.1 | 18.3 | 19.0 | 0.62 |
| Angina, % | 40.0 | 30.8* | 38.0 | 25.4* | 0.02 |
| CHF, % | 31.4* | 28.3* | 20.0 | 11.2* | < 0.001 |
| MI, % | 32.6 | 23.3 | 24.1 | 18.0* | 0.01 |
| Pulmonary Disease, % | 41.0* | 40.2 | 33.2 | 27.2* | < 0.001 |
| Cancer, % | 11.4 | 20.5 | 20.1 | 17.0 | 0.05 |
| Diabetes,% | 37.5 | 35.8 | 27.4 | 23.9 | 0.01 |
| Blocks walked in the past week, n |
11.5* (4.2) | 22.6* (4.2) | 37.3* (4.1) | 59.8 (4.3) | < 0.001 |
| Pain on exertion and rest | 32.7 | 23.9 | 15.7 | 6.50 | < 0.0001 |
| Atypical exertional leg pain/stop |
16.9 | 22.6 | 22.9 | 21.9 | 0.4924 |
| Atypical exertional leg pain/carry on |
3.10 | 3.77 | 11.4 | 18.2 | < 0.0001 |
| Asymptomatic PAD | 16.3 | 15.7 | 18.5 | 31.0 | 0.001 |
| Intermittent claudication | 30.3 | 33.2 | 30.8 | 22.4 | 0.035 |
| Six minute walk, ft | 815.0 (24.2) | 1037.2 (23.7) | 1248.0 (23.2 | 1397.5 (24.6) | <.0001 |
| Four meter velocity at usual speed, m/sec |
0.74 (0.01) | 0.84 (0.01) | 0.92 (0.01) | 0.99 (0.01) | <.0001 |
| Four meter velocity at fast speed, m/sec |
1.00 (0.02) | 1.13 (0.02) | 1.27 (0.02) | 1.34 (0.02) | <.0001 |
| Statin use,% | 43.5 | 42.7 | 47.2 | 39.2 | 0.78 |
| Inhibitor use, % | 27.7 | 36.5 | 28.4 | 20.4 | 0.08 |
Values shown are mean (Standard Error) unless otherwise indicated. WIQ = Walking Impairment Questionnaire; PAD = peripheral arterial disease; ABI = ankle brachial index; BMI = body mass index; CHF = congestive heart failure; MI = myocardial infarction.
for pairwise comparison with 4th quartile (best) as referent, p value < 0.05
Lower (worse) quartiles for the PAD participant WIQ distance score were associated with lower ABI values and higher prevalences of females, black race, angina, heart failure, history of myocardial infarction, and pulmonary disease. Lower WIQ distance scores were associated with a higher prevalence of pain on exertion and rest, a higher prevalence of intermittent claudication, a lower prevalence of asymptomatic PAD, and a lower prevalence of atypical exertional leg pain/carry on.
Lower (worse) quartiles for the PAD participant WIQ speed score were associated with lower ABI and higher prevalences of females, black race, angina, heart failure, history of myocardial infarction, pulmonary disease, and diabetes. Furthermore, participants in the lowest (worst) quartiles for WIQ speed score had a higher prevalence of pain on exertion and rest, a higher prevalence of intermittent claudication, a lower prevalence of asymptomatic PAD and a lower prevalence of atypical exertional leg pain/carry on.
Table III lists the age-adjusted baseline characteristics of non-PAD participants by WIQ stair-climbing, WIQ distance, and WIQ speed score quartiles. Lower (worse) quartiles for the non-PAD participant WIQ stair-climbing score were associated with a lower prevalence of males, higher BMI, fewer blocks walked in the past week, higher prevalences of black race, angina, CHF, MI, pulmonary disease, and diabetes. Lower quartiles were also associated with shorter six minute walk distance and slower four meter walking velocity, at both usual and fast speeds.
Table III. Age-adjusted Clinical Characteristics of Non-PAD Participants Across WIQ Score Quartiles (n=410).
| WIQ Stair Climbing Score Quartiles | |||||
|---|---|---|---|---|---|
| 1st Quartile [≤ 41.7] |
2nd Quartile [41.7 –66.7] |
3rd Quartile [66.7 – 87.5] |
4th Quartile [> 87.5] |
p for trend |
|
| Male, % | 32.21% | 54.14% | 47.04% | 62.72% | 0.0001 |
| Black race, % | 26.27% | 17.86% | 14.29% | 10.24% | 0.003 |
| ABI | 1.08( 0.01) | 1.09( 0.01) | 1.09( 0.01) | 1.11( 0.01) | 0.018 |
| BMI, kg/m2 | 31.83( 0.49) | 29.02( 0.50) | 26.36( 0.59) | 26.47( 0.70) | <0.0001 |
| Current Smoker, % | 7.50% | 9.52% | 7.10% | 2.56% | 0.11 |
| Angina, % | 35.67% | 22.48% | 12.42% | 7.81% | <0.0001 |
| CHF, % | 23.65% | 14.14% | 10.21% | 4.85% | <0.0001 |
| MI, % | 22.04% | 12.90% | 10.11% | 8.25% | 0.01 |
| Pulmonary Disease, % | 42.53% | 34.94% | 25.36% | 11.67% | <0.0001 |
| Cancer, % | 14.60% | 18.30% | 16.93% | 16.53% | 0.97 |
| Diabetes,% | 30.18% | 21.93% | 17.54% | 8.69% | 0.001 |
| Blocks walked in the past week, n | 32.24( 5.12) | 39.18( 5.25) | 66.05( 6.20) | 59.33( 7.30) | <0.0001 |
| Six minute walk, ft | 1085.6( 46.77) | 1460.8( 45.62) | 1601.0( 60.60) | 1632.6( 71.12) | <.0001 |
| Four meter velocity at usual speed, m/sec |
0.82( 0.02) | 0.97( 0.02) | 1.02( 0.03) | 1.01( 0.04) | <.0001 |
| Four meter velocity at fast speed, m/sec |
1.09( 0.03) | 1.29( 0.03) | 1.41( 0.05) | 1.36( 0.05) | <.0001 |
| Statin use,% | 26.80% | 33.12% | 23.53% | 24.44% | 0.74 |
| Inhibitor use, % | 23.72% | 24.23% | 21.30% | 18.35% | 0.42 |
| WIQ Distance Score Quartiles | |||||
|---|---|---|---|---|---|
| 1st Quartile [≤ 44.6] |
2nd Quartile [44.6 – 83.0] |
3rd Quartile [83.0 – 100] |
p for trend |
||
| Male, % | 38.45% | 55.38% | 46.87% | 0.13 | |
| Black race, % | 31.17% | 20.01% | 11.43% | <.0001 | |
| ABI | 1.07( 0.01) | 1.08( 0.01) | 1.10( 0.01) | 0.01 | |
| BMI, kg/m2 | 32.01( 0.56) | 29.65( 0.55) | 26.90( 0.40) | <.0001 | |
| Current Smoker, % | 9.07% | 11.97% | 3.89% | 0.02 | |
| Angina, % | 37.64% | 24.72% | 13.00% | <.0001 | |
| CHF, % | 26.03% | 14.97% | 9.12% | <.0001 | |
| MI, % | 18.99% | 15.34% | 11.64% | 0.07 | |
| Pulmonary Disease, % | 47.74% | 31.54% | 23.76% | <.0001 | |
| Cancer, % | 17.16% | 16.26% | 15.75% | 0.95 | |
| Diabetes,% | 36.22% | 23.84% | 12.35% | <.0001 | |
| Blocks walked in the past week, n | 20.27( 5.65) | 35.34( 5.54) | 64.89( 4.03) | <.0001 | |
| Six minute walk, ft | 1067.6( 49.95) | 1371.9( 54.52) | 1591.8( 37.76) | <.0001 | |
| Four meter velocity at usual speed, m/sec |
0.81( 0.03) | 0.92( 0.03) | 1.01( 0.02) | <.0001 | |
| Four meter velocity at fast speed, m/sec |
1.08( 0.04) | 1.22( 0.04) | 1.38( 0.03) | <.0001 | |
| Statin use,% | 30.25% | 26.69% | 26.77% | 0.54 | |
| Inhibitor use, % | 26.40% | 22.89% | 20.30% | 0.14 | |
| WIQ Speed Score Quartiles | |||||
|---|---|---|---|---|---|
| 1st Quartile [≤ 32.6] |
2nd Quartile [32.6 – 50.0] |
3rd Quartile [50.0 – 71.7] |
4th Quartile [> 71.7] |
p for trend |
|
| Male, % | 41.06% | 37.08% | 55.47% | 56.99% | 0.001 |
| Black race, % | 27.31% | 20.47% | 10.72% | 14.48% | 0.003 |
| ABI | 1.07( 0.01) | 1.06( 0.01) | 1.11( 0.01) | 1.12( 0.01) | <.0001 |
| BMI, kg/m2 | 32.15( 0.54) | 29.28( 0.54) | 27.72( 0.59) | 25.99( 0.57) | <.0001 |
| Current Smoker, % | 13.43% | 3.49% | 5.74% | 4.98% | 0.02 |
| Angina, % | 39.07% | 22.22% | 16.67% | 9.19% | <.0001 |
| CHF, % | 27.40% | 18.30% | 7.89% | 4.21% | <.0001 |
| MI, % | 18.76% | 16.65% | 11.33% | 9.83% | 0.047 |
| Pulmonary Disease, % | 48.96% | 29.82% | 25.76% | 18.16% | <.0001 |
| Cancer, % | 16.93% | 19.29% | 14.75% | 15.31% | 0.80 |
| Diabetes,% | 34.31% | 28.86% | 9.40% | 10.23% | <.0001 |
| Blocks walked in the past week, n | 20.74( 5.60) | 46.41( 5.57) | 60.07( 6.12) | 62.22( 5.92) | <.0001 |
| Six minute walk, ft | 1106.1( 48.24) | 1347.5( 49.28) | 1525.1( 60.67) | 1736.1( 58.48) | <.0001 |
| Four meter velocity at usual speed, m/sec |
0.84( 0.03) | 0.91( 0.03) | 0.98( 0.03) | 1.08( 0.03) | <.0001 |
| Four meter velocity at fast speed, m/sec |
1.11( 0.03) | 1.21( 0.04) | 1.30( 0.04) | 1.49( 0.04) | <.0001 |
| Statin use,% | 30.23% | 29.69% | 24.33% | 25.29% | 0.75 |
| Inhibitor use, % | 26.73% | 29.73% | 13.20% | 19.07% | 0.07 |
Values shown are mean (Standard Error) unless otherwise indicated. WIQ = Walking Impairment Questionnaire; PAD = peripheral arterial disease; ABI = ankle brachial index; BMI = body mass index; CHF = congestive heart failure; MI = myocardial infarction.
for pairwise comparison with 4th quartile (best) as referent, p value < 0.05
Given a very large number of non-PAD participants with a WIQ distance score of 100, the software used in this analysis grouped both 3rd and 4th quartile scoring participants into the 3rd quartile. Lower (worse) quartiles for the non-PAD participant WIQ distance score were associated with higher BMI, fewer blocks walked in the past week, higher prevalence of black race, angina, CHF, pulmonary disease, and diabetes. Lower quartiles were also associated with shorter six minute walk distance and slower four meter walking velocity at both usual and fast speeds.
Lower (worse) quartiles for the non-PAD participant WIQ speed score were associated with a lower prevalence of males, higher BMI, fewer blocks walked in the past week, higher prevalences of black race, angina, CHF, MI, pulmonary disease, and diabetes. Lower quartiles were also associated with shorter six minute walk distance and slower four meter walking velocity at both usual and fast speeds.
WIQ stair-climbing score and mortality
Table IVa and Table IVb show the associations of WIQ stair-climbing score quartiles with all-cause and CVD mortality among PAD and non-PAD participants, respectively. These data are adjusted for age, sex, race, ABI, BMI, smoking status, comorbidities, statin and ACE inhibitor use, and physical activity.
Table IVa. Adjusted Associations of WIQ stair climbing score quartiles with total and cardiovascular disease mortality among PAD Participants. (n = 638).
| HR | pairwise | ||
|---|---|---|---|
| (95% Confidence Interval) | p value | p for trend | |
| All-cause mortality | |||
|
| |||
| 1st quartile [≤ 25.0] | 1.70 (1.08 – 2.66) | 0.02 | 0.02 |
| 2nd quartile [25.0 – 41.7] | 1.75 (1.13 – 2.70) | 0.01 | |
| 3rd quartile [41.7 – 66.7] | 1.26 (0.82 – 1.91) | 0.29 | |
| 4th quartile [> 66.7] | 1.0 (referent) | NA | |
| Cardiovascular disease mortality | |||
|
| |||
| 1st quartile [≤ 25.0] | 3.11 (1.30 – 7.47) | 0.01 | 0.04 |
| 2nd quartile [25.0 – 41.7] | 3.32 (1.43 – 7.72) | 0.01 | |
| 3rd quartile [41.7 – 66.7] | 2.03 (0.88 – 4.71) | 0.10 | |
| 4th quartile [> 66.7] | 1.0 (referent) | NA | |
Adjusted for age, sex, race, body mass index, smoking status, ankle brachial index, comorbidities, physical activity, statin use and ACE inhibitor use. WIQ = Walking Impairment Questionnaire; CVD = cardiovascular disease; PAD = peripheral arterial disease; HR = hazard ratio. Pairwise p value shows statistical significance relative to the 4th quartile.
Table IVb. Adjusted Associations of WIQ stair climbing score quartiles with total and cardiovascular disease mortality among non-PAD Participants.
| HR | pairwise | ||
|---|---|---|---|
| (95% Confidence Interval) | p value | p for trend | |
| All-cause mortality | |||
|
| |||
| 1st quartile [≤ 41.7] | 0.70( 0.29 - 1.67) | 0.42 | 0.94 |
| 2nd quartile [41.7 – 66.7] | 0.71( 0.31 - 1.60) | 0.41 | |
| 3rd quartile [66.7 – 87.5] | 0.43( 0.18 - 1.04) | 0.06 | |
| 4th quartile [> 87.5] | 1.0 (referent) | NA | |
| Cardiovascular disease mortality | |||
|
| |||
| 1st quartile [≤ 41.7] | 2.62( 0.45 - 15.21) | 0.28 | 0.29 |
| 2nd quartile [41.7 – 66.7] | 2.55( 0.49 - 13.41) | 0.27 | |
| 3rd quartile [66.7 – 87.5] | 0.48( 0.07 - 3.36) | 0.46 | |
| 4th quartile [> 87.5] | 1.0 (referent) | NA | |
Adjusted for age, sex, race, body mass index, smoking status, ankle brachial index, comorbidities, physical activity, statin use and ACE inhibitor use. WIQ = Walking Impairment Questionnaire; CVD = cardiovascular disease; PAD = peripheral arterial disease; HR = hazard ratio. Pairwise p value shows statistical significance relative to the 4th quartile.
Poorer WIQ stair-climbing scores at baseline were associated with higher all-cause mortality (p for trend = 0.02) among PAD participants. PAD participants in the first and second WIQ stair climbing quartiles had adjusted hazard ratios of 1.70 (95% CI 1.08 – 2.66, p=0.02) and 1.75 (95% CI 1.13 – 2.70, p=0.01), respectively, for all-cause mortality when compared to those in the highest (best) WIQ stair climbing quartile. Poorer WIQ stair-climbing scores were also significantly associated with higher CVD mortality (p for trend = 0.04) among PAD participants. When compared to those in the highest (best) quartile, PAD participants in the first and second WIQ stair climbing quartiles had adjusted hazard ratios of 3.11 (95% CI 1.30 – 7.47, p = 0.01) and 3.32 (95% CI 1.43 – 7.72, p = 0.01) for CVD mortality, respectively (Table IVa). No significant associations were observed between WIQ stair-climbing score and all-cause mortality (p for trend = 0.94) or CVD mortality (p for trend = 0.29) among non-PAD participants (Table IVb).
WIQ distance score
After adjusting for age, sex, race, ABI, BMI, smoking status, comorbidities, statin and ACE inhibitor use, and physical activity, no significant associations were observed between the WIQ distance score and all-cause mortality (p for trend = 0. 20) or CVD mortality (p for trend = 0.51) among PAD participants. (Table Va). No significant associations were observed between WIQ distance score and all-cause mortality (p for trend = 0.69) or CVD mortality (p for trend = 0.69) among non-PAD participants. (Table Vb).
Table Va. Adjusted Associations of WIQ distance score quartiles with total and cardiovascular disease mortality among PAD Participants. (n = 638).
| HR (95% CI) | p value | p for trend | |
|---|---|---|---|
| All-cause mortality | |||
|
| |||
| 1st quartile [≤ 14.5] | 1.22 (0.79 - 1.88) | 0.38 | 0.20 |
| 2nd quartile [14.5 – 37.1] | 1.49 (0.98 - 2.25) | 0.06 | |
| 3rd quartile [37.1 – 67.9] | 1.26 (0.84 - 1.89) | 0.27 | |
| 4th quartile [> 67.9] | 1.0 (referent) | NA | |
| Cardiovascular disease mortality | |||
|
| |||
| 1st quartile [≤ 14.5] | 1.30 (0.60 - 2.81) | 0.51 | 0.51 |
| 2nd quartile [14.5 – 37.1] | 1.13 (0.51 - 2.50) | 0.77 | |
| 3rd quartile [37.1 – 67.9] | 1.30 (0.63 - 2.69) | 0.48 | |
| 4th quartile [> 67.9] | 1.0 (referent) | NA | |
Adjusted for age, sex, race, body mass index, smoking status, ankle brachial index, comorbidities, physical activity, statin use and ACE inhibitor use. WIQ = Walking Impairment Questionnaire; CVD = cardiovascular disease; PAD = peripheral arterial disease; HR = hazard ratio. Pairwise p value shows statistical significance relative to the 4th quartile.
Table Vb. Adjusted Associations of WIQ distance score quartiles with total and cardiovascular disease mortality among non-PAD Participants.
| HR (95% CI) | p value | p for trend | |
|---|---|---|---|
| All-cause mortality | |||
|
| |||
| 1st quartile [≤ 44.6] | 1.36( 0.69 - 2.69) | 0.37 | 0.69 |
| 2nd quartile [44.6 – 83.0] | 1.05( 0.56 - 1.95) | 0.88 | |
| 3rd quartile [83.0 –100] | 1.0 (referent) | NA | |
| Cardiovascular disease mortality | |||
|
| |||
| 1st quartile [≤ 44.6] | 1.09( 0.35 - 3.37) | 0.88 | 0.68 |
| 2nd quartile [44.6 – 83.0] | 1.55( 0.58 - 4.13) | 0.38 | |
| 3rd quartile [83.0 –100] | 1.0 (referent) | NA | |
Adjusted for age, sex, race, body mass index, smoking status, ankle brachial index, comorbidities, physical activity, statin use and ACE inhibitor use. WIQ = Walking Impairment Questionnaire; CVD = cardiovascular disease; PAD = peripheral arterial disease; HR = hazard ratio. Pairwise p value shows statistical significance relative to the 4th quartile.
WIQ speed score
After adjusting for age, gender, race, ABI, BMI, smoking status, comorbidities, statin and ACE inhibitor use, and physical activity, no significant associations were observed between the WIQ speed score and all-cause mortality (p for trend = 0.07) or CVD mortality (p for trend = 0.33) among PAD participants. In pairwise comparisons, PAD participants with WIQ speed scores in the second quartile had an adjusted hazard ratio of 1.71 (95% CI 1.12 – 2.60) for all-cause mortality compared to those with WIQ speed scores in the fourth (best) quartile (Table VIa). There were no other significant associations of WIQ speed quartiles with mortality among PAD participants. No significant associations were observed between WIQ speed score and all-cause mortality (p for trend = 0.26) or CVD mortality (p for trend = 0.78) among non-PAD participants. (Table VIb).
Table VIa. Adjusted Associations of WIQ speed score quartiles with total and cardiovascular disease mortality among PAD Participants. (n = 638).
| HR (95% CI) | p value | p for trend | |
|---|---|---|---|
| All-cause mortality | |||
|
| |||
| 1st quartile [≤ 17.4] | 1.57 (1.00 - 2.44) | 0.05 | 0.07 |
| 2nd quartile [17.4 – 32.6] | 1.71 (1.12 - 2.60) | 0.01 | |
| 3rd quartile [32.6 – 54.3] | 1.34 (0.88 - 2.05) | 0.17 | |
| 4th quartile [> 54.3] | 1.0 (referent) | NA | |
| Cardiovascular disease mortality | |||
|
| |||
| 1st quartile [≤ 17.4] | 1.61 (0.75 - 3.49) | 0.23 | 0.33 |
| 2nd quartile [17.4 – 32.6] | 1.80 (0.84 - 3.82) | 0.13 | |
| 3rd quartile [32.6 – 54.3] | 1.50 (0.71 - 3.16) | 0.30 | |
| 4th quartile [> 54.3] | 1.0 (referent) | NA | |
Adjusted for age, sex, race, body mass index, smoking status, ankle brachial index, comorbidities, physical activity, statin use and ACE inhibitor use. WIQ = Walking Impairment Questionnaire; CVD = cardiovascular disease; PAD = peripheral arterial disease; HR = hazard ratio. Pairwise p value shows statistical significance relative to the 4th quartile.
Table VIb. Adjusted Associations of WIQ speed score quartiles with total and cardiovascular disease mortality among non-PAD Participants.
| HR (95% CI) | p value | p for trend | |
|---|---|---|---|
| All-cause mortality | |||
| 1st quartile [≤ 32.6] | 1.43( 0.64 - 3.19) | 0.38 | 0.26 |
| 2nd quartile [32.6 – 50.0] | 1.06( 0.47 - 2.39) | 0.89 | |
| 3rd quartile [50.0 – 71.7] | 0.89( 0.39 - 2.05) | 0.79 | |
| 4th quartile [> 71.7] | 1.0 (referent) | NA | |
| Cardiovascular disease mortality | |||
| 1st quartile [≤ 32.6] | 1.38( 0.35 - 5.50) | 0.65 | 0.78 |
| 2nd quartile [32.6 – 50.0] | 2.25( 0.59 - 8.61) | 0.24 | |
| 3rd quartile [50.0 – 71.7] | 0.94( 0.21 - 4.27) | 0.94 | |
| 4th quartile [> 71.7] | 1.0 (referent) | NA |
Adjusted for age, sex, race, body mass index, smoking status, ankle brachial index, comorbidities, physical activity, statin use and ACE inhibitor use. WIQ = Walking Impairment Questionnaire; CVD = cardiovascular disease; PAD = peripheral arterial disease; HR = hazard ratio. Pairwise p value shows statistical significance relative to the 4th quartile.
Correlation of WIQ domain scores and ABI among PAD participants
Statistically significant but weak correlations were observed between ABI and WIQ distance and WIQ speed scores (0.270, p < 0.0001 and 0.178, p <0.0001; respectively). No correlation was observed between WIQ stair climbing score and ABI with a Pearson coefficient of 0.074, p = 0.06 (Table VII).
Table VII. Correlation between baseline ABI and WIQ domain score in PAD participants.
| Pearson coefficient |
p value |
|
|---|---|---|
| WIQ stair climbing score | 0.074 | 0.06 |
| WIQ distance score | 0.270 | < 0.0001 |
| WIQ speed score | 0.178 | < 0.0001 |
ABI = ankle brachial index
WIQ = Walking Impairment Questionnaire
PAD = peripheral arterial disease
P < 0.05 is statistically significant
DISCUSSION
Among 638 men and women with PAD, lower baseline WIQ stair-climbing scores were associated with higher all-cause and cardiovascular disease mortality, respectively, over a median follow-up of 4.5 years. After adjustment for baseline ABI, comorbidities, age, and other confounders, those in the lowest WIQ stair-climbing score quartile were 1.70 times more likely to die from any cause and 3.11 times more likely to die from cardiovascular disease compared to those in the highest (best) WIQ stair-climbing score quartile at baseline. In contrast, we found no statistically significant associations between baseline WIQ speed or WIQ distance scores with all-cause or cardiovascular disease mortality, among the PAD participants. Furthermore, no independent association was observed between baseline WIQ stair-climbing, WIQ distance, and WIQ speed scores with all-cause and CVD mortality among non-PAD participants.
Previous studies have also assessed associations of subjective measures of walking performance or global health-related quality of life with mortality in patients with PAD. In the Peripheral Arteriopathy and Cardiovascular Events (PACE) study(21), the Walking Impairment Questionnaire was administered to 60 Italian participants with PAD and intermittent claudication. Over a median follow-up of 24 months, WIQ speed and WIQ stair-climbing scores below the median were associated with an increased risk of cardiovascular events as compared to scores above the median after adjusting for ABI and other confounders(21). As compared to this prior work, the current study includes PAD participants both with and without intermittent claudication symptoms. Since most people with PAD do not have classic symptoms of intermittent claudication(20), the current data are more generalizable to the typical individual with PAD. More recently, Issa et al.(5) reported that among 503 Dutch PAD patients undergoing non-cardiac vascular surgery, those with a poor subjective health-related quality of life, measured with the EuroQol Questionnaire one year after surgery, were at highest risk for all-cause mortality over three year follow-up when compared to those who reported the highest subjective health-related quality of life. Participants who reported severe mobility impairment at baseline were at greatest risk for three-year mortality. As compared to the data reported here, the study by Issa et al. did not adjust for ABI and included a higher proportion of participants with claudication. It is possible that baseline ABI is a confounder of the association of patient reported walking ability and quality of life with mortality. In addition, the EuroQol Questionnaire focuses more on global health-related quality of life and incorporates a non-specific and generalized mobility measure. In contrast, the WIQ, a PAD-specific questionnaire, is a more precise measure of patient-perceived mobility across specific dimensions such as stair-climbing ability, walking distance, and walking speed.
In contrast to the WIQ stair-climbing score, data presented here show that the WIQ distance and speed scores were not associated independently with all-cause or cardiovascular disease mortality. This association may represent greater precision of the WIQ stair-climbing score as a measure of overall cardiovascular fitness, as compared to the WIQ walking distance and walking speed. Similarly, objectively measured stair-climbing ability is generally considered a reliable surrogate of peak oxygen consumption and has been used as a preoperative screening tool in patients undergoing lung resection to predict risk for perioperative death (22). While to our knowledge no published literature is available that provides data on the predictive ability of the WIQ stair-climbing score and peak oxygen consumption in PAD patients, earlier studies by Brunelli et al. found that patients who performed poorly in a stair-climbing test were at higher risk for postoperative death after lung resection (23, 24). Thus, poor WIQ stair-climbing scores, as compared to WIQ walking distance or walking speed abilities, may better identify a subset of patients with poorer overall cardiovascular status and greater mortality risk when used in men and women with PAD.
Limitations
Study participants were identified from medical centers within Chicago. Although data may not be generalizable to PAD participants outside of Chicago, there is no reason to believe that the relationships reported here would not be maintained in other settings. Also, 6% of eligible participants were excluded from analysis as they did not complete the WIQ at baseline. However, the baseline characteristics of those who did not complete the WIQ did not differ significantly from those who completed it.
Finally, while we adjusted for confounders including comorbidities, we cannot rule out the possibility that residual confounding or unidentified characteristics among participants with poorer WIQ scores contributed to the observed association with mortality risk.
Conclusion
Men and women with PAD who have poorer WIQ stair-climbing scores are at higher all-cause and cardiovascular disease mortality risk compared to those with higher WIQ stair-climbing scores. Data reported here demonstrate that the WIQ stair-climbing score provides additional data about all-cause and CVD mortality risk, beyond that provided by baseline ABI. These findings may potentially be helpful for clinicians who use the WIQ scores to assess patient perceived walking performance and risk. These results also help to place into better perspective the potential significance of interventions that improve WIQ stair climbing scores. Future study is necessary to confirm findings reported here and determine whether interventions that improve WIQ stair-climbing score are associated with a survival benefit.
Acknowledgments
Funding Sources: This study was supported by grants K12-HL083790, R01-HL083064, R01-HL64739, and R01-HL71223 from the National Heart, Lung, and Blood Institute and by grant RR-00048 from the National Center for Research Resources, National Institutes of Health. This study was also supported by the National Institute on Aging.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: No competing interest declared.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, et al. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121(7):e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Heald CL, Fowkes FGR, Murray GD, Price JF, Collaborat ABI Risk of mortality and cardiovascular disease associated with the ankle-brachial index: Systematic review. Atherosclerosis. 2006;189(1):61–9. doi: 10.1016/j.atherosclerosis.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 3.Sikkink CJ, van Asten WN, van ’t Hof MA, van Langen H, van der Vliet JA. Decreased ankle/brachial indices in relation to morbidity and mortality in patients with peripheral arterial disease. Vasc Med. 1997;2(3):169–73. doi: 10.1177/1358863X9700200302. [DOI] [PubMed] [Google Scholar]
- 4.McDermott MM, Tian L, Liu K, Guralnik JM, Ferrucci L, Tan J, et al. Prognostic value of functional performance for mortality in patients with peripheral artery disease. J Am Coll Cardiol. 2008;51(15):1482–9. doi: 10.1016/j.jacc.2007.12.034. PMCID: 2459324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Issa SM, Hoeks SE, Scholte op, Reimer WJ, Van Gestel YR, Lenzen MJ, Verhagen HJ, et al. Health-related quality of life predicts long-term survival in patients with peripheral artery disease. Vasc Med. 2010;15(3):163–9. doi: 10.1177/1358863X10364208. [DOI] [PubMed] [Google Scholar]
- 6.Regensteiner JG, Steiner JF, Hiatt WR. Exercise training improves functional status in patients with peripheral arterial disease. J Vasc Surg. 1996;23(1):104–15. doi: 10.1016/s0741-5214(05)80040-0. [DOI] [PubMed] [Google Scholar]
- 7.McDermott MM, Greenland P, Liu K, Guralnik JM, Celic L, Criqui MH, et al. The ankle brachial index is associated with leg function and physical activity: the Walking and Leg Circulation Study. Ann Intern Med. 2002;136(12):873–83. doi: 10.7326/0003-4819-136-12-200206180-00008. [DOI] [PubMed] [Google Scholar]
- 8.McDermott MM, Hoff F, Ferrucci L, Pearce WH, Guralnik JM, Tian L, et al. Lower extremity ischemia, calf skeletal muscle characteristics, and functional impairment in peripheral arterial disease. J Am Geriatr Soc. 2007;55(3):400–6. doi: 10.1111/j.1532-5415.2007.01092.x. PMCID: 2645649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Regensteiner J, Steiner JF, Panzer RJ, Hiatt WR. Evaluation of Walking Impairment by Questionnaire in Patients with Peripheral Arterial Disease. Journal of Vascular Medicine and Biology. 1990;2:142–52. [Google Scholar]
- 10.Nicolai SP, Kruidenier LM, Rouwet EV, Graffius K, Prins MH, Teijink JA. The walking impairment questionnaire: an effective tool to assess the effect of treatment in patients with intermittent claudication. J Vasc Surg. 2009;50(1):89–94. doi: 10.1016/j.jvs.2008.12.073. [DOI] [PubMed] [Google Scholar]
- 11.McDermott MM, Ades P, Guralnik JM, Dyer A, Ferrucci L, Liu K, et al. Treadmill exercise and resistance training in patients with peripheral arterial disease with and without intermittent claudication: a randomized controlled trial. JAMA. 2009;301(2):165–74. doi: 10.1001/jama.2008.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McDermott MM, Criqui MH, Liu K, Guralnik JM, Greenland P, Martin GJ, et al. Lower ankle/brachial index, as calculated by averaging the dorsalis pedis and posterior tibial arterial pressures, and association with leg functioning in peripheral arterial disease. J Vasc Surg. 2000;32(6):1164–71. doi: 10.1067/mva.2000.108640. [DOI] [PubMed] [Google Scholar]
- 13.Shadman R, Criqui MH, Bundens WP, Fronek A, Denenberg JO, Gamst AC, et al. Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol. 2004;44(3):618–23. doi: 10.1016/j.jacc.2004.04.044. [DOI] [PubMed] [Google Scholar]
- 14.Montgomery PS, Gardner AW. The clinical utility of a six-minute walk test in peripheral arterial occlusive disease patients. J Am Geriatr Soc. 1998;46(6):706–11. doi: 10.1111/j.1532-5415.1998.tb03804.x. [DOI] [PubMed] [Google Scholar]
- 15.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332(9):556–61. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 17.Guralnik J. The Women’s Health and Aging Study: Health and Social Characteristics of Older Women with Disability. National Institute on Aging, National Institutes of Health; Bethesda, MD: 1995. [Google Scholar]
- 18.Garg PK, Liu K, Tian L, Guralnik JM, Ferrucci L, Criqui MH, et al. Physical activity during daily life and functional decline in peripheral arterial disease. Circulation. 2009;119(2):251–60. doi: 10.1161/CIRCULATIONAHA.108.791491. PMCID: 2888033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Criqui MH, Denenberg JO, Bird CE, Fronek A, Klauber MR, Langer RD. The correlation between symptoms and non-invasive test results in patients referred for peripheral arterial disease testing. Vasc Med. 1996;1(1):65–71. doi: 10.1177/1358863X9600100112. [DOI] [PubMed] [Google Scholar]
- 20.McDermott MM, Greenland P, Liu K, Guralnik JM, Criqui MH, Dolan NC, et al. Leg symptoms in peripheral arterial disease: associated clinical characteristics and functional impairment. JAMA. 2001;286(13):1599–606. doi: 10.1001/jama.286.13.1599. [DOI] [PubMed] [Google Scholar]
- 21.Schiano V, Brevetti G, Sirico G, Silvestro A, Giugliano G, Chiariello M. Functional status measured by walking impairment questionnaire and cardiovascular risk prediction in peripheral arterial disease: results of the Peripheral Arteriopathy and Cardiovascular Events (PACE) study. Vasc Med. 2006;11(3):147–54. doi: 10.1177/1358863x06074830. [DOI] [PubMed] [Google Scholar]
- 22.Colice GL, Shafazand S, Griffin JP, Keenan R, Bolliger CT. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: ACCP evidenced-based clinical practice guidelines. Chest. (2nd edition) 2007;132(3 Suppl):161S–77S. doi: 10.1378/chest.07-1359. [DOI] [PubMed] [Google Scholar]
- 23.Brunelli A, Sabbatini A, Xiume F, Borri A, Salati M, Marasco RD, et al. Inability to perform maximal stair climbing test before lung resection: a propensity score analysis on early outcome. Eur J Cardiothorac Surg. 2005;27(3):367–72. doi: 10.1016/j.ejcts.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 24.Brunelli A, Monteverde M, Al Refai M, Fianchini A. Stair climbing test as a predictor of cardiopulmonary complications after pulmonary lobectomy in the elderly. Ann Thorac Surg. 2004;77(1):266–70. doi: 10.1016/s0003-4975(03)01327-4. [DOI] [PubMed] [Google Scholar]