Abstract
Background: The present study was conducted to scrutinize Public- Private Partnership (PPP) models in public hospitals of different countries based on performance indicators in order to se-lect appropriated models for Iran hospitals.
Methods: In this mixed (quantitative-qualitative) study, systematic review and expert panel has been done to identify varied models of PPP as well as performance indicators. In the second step we prioritized performance indicator and PPP models based on selected performance indicators by Analytical Hierarchy process (AHP) technique. The data were analyzed by Excel 2007 and Expert Choice11 software’s.
Results: In quality – effectiveness area, indicators like the rate of hospital infections (100%), hospital accidents prevalence rate (73%), pure rate of hospital mortality (63%), patient satisfaction percentage (53%), in accessibility equity area indicators such as average inpatient waiting time (100%) and average outpatient waiting time (74%), and in financial – efficiency area, indicators including average length of stay (100%), bed occupation ratio (99%), specific income to total cost ratio (97%) have been chosen to be the most key performance indicators. In the pri¬oritization of the PPP models clinical outsourcing, management, privatization, BOO (build, own, operate) and non-clinical outsourcing models, achieved high priority for various performance in¬dicator areas.
Conclusion: This study had been provided the most common PPP options in the field of public hospitals and had gathered suitable evidences from experts for choosing appropriate PPP option for public hospitals. Effect of private sector presence in public hospital performance, based on which PPP options undertaken, will be different.
Keywords: Public – private partnership, Hospitals, Performance indicator
Introduction
Public-Private Partnerships (PPP) as a widespread universal approach to health care issues were created throughout the late 1990s [1]. The term PPP describes a cooperative events between public and private sectors, built on expertise of each partner, that best meets clearly defined public needs through the suitable allocation of resources, risks and rewards [2]. The aim of PPP is transferring tasks and risks to the private sector in order to gain efficiency and cost reduction [3]. In public hospitals it can cover up a variety of transactions ranging from relatively short term service contract to concession contract or joint ventures [4]. These options for involving private sector in public hospitals, vary with regards to ownership, operation, maintenance, financing, risk share, and durations [5].
According to WHO suggestion, governments should investigate ways of adopting the PPP model for delivery of health and welfare services. At the same time, the conference emphasize that there is a lack of exact evidence regarding to the effectiveness of these, in other word the success of PPP in this situation appears to be mixed [1,6-8]. Therefore an essential aspect of PPP in health sector is the ability to identify situational requirements' and desired outcomes.
With theses conceptual backgrounds and considering that the health system of Iran faces variety of challenges and problems in the issues of quality, relevancy, effectiveness, and progressing pressures to cut costs and to operate efficiently [9]. At the same time this system allocated more than 50% of total health funds to hospital sector. Hospitals of Iran have more than 130 thousand employee (50% of health staffs) however the low occupancy of hospital beds (about 54%) in comparison with developed countries (with bed occupancy of 80% to 85%) shows the need for proper utilization of limited resources [10], so it will be necessary to promote performance indicators and efficient management of hospitals by implementing various strategies. The strategy of PPP that was proposed in several studies [11-17] seems to be an important solution in order to solve problems mentioned above. Nowadays there are powerful orientations in Iran such as appropriate legal requirements of general policies of the article 44 of the constitution of Iran and the third and fourth national development programs for better interaction with the private sector, especially in the areas of health and public hospitals [10,18-20]. On the other hand performance measures are essential to implement desired health sector reforms and to measure their effects [21]. Iranian health system, similar to other systems, is still in an early stage of performance measurement, and basic steps can still be taken to improve the effectiveness of its measurement systems especially in hospital sector [22].
Numerous studies and experiences indicate that PPP is an ongoing approach to compact hospital sector problems [23-31]. Thus, identifying models of PPP in public hospitals and potential of each model to improve hospital performance indicators in the absence of sufficient evidence in this regard are required for decision making and involving private sector in public hospitals.
This study aimed to identify the types of PPP and performance indicators in public hospitals and prioritize PPP models based on performance indicators.
Materials and Methods
This is a mixed (quantitative-qualitative) study. Depending on the different stages of research, various tools have been used. In order to identify PPP models in public hospital as well as performance indicators, first related literature was reviewed and then expert’s panel was used (qualitative part). In order to prioritize performance indicators and PPP models, Analytic Hierarchy Process (AHP) technique was used (quantitative part).
To identify public – private partnership models in public hospital and different kind of hospitals performance indicators a systematic review of literature was done on 28/12/2010, 29/12/2010, 30/12/2010. Inter science, Pub Med , Cochran library, Springer Link, Elsevier, Proquest, Scopus, Emerald, Google scholar, SID and Irandoc databases were searched, with key words of Public – private Partnership & hospital, PPP & hospital, Public – Private mix & hospital, Public – private Partnership models &hospital, PPP models & hospital, PPP models & performance indicators, performance indicators and hospital and with Persian equivalent of these key words in Persian databases as SID and Irandoc, for the period of January 1980 to December 2010. This strategy resulted 18931 articles. Inclusion and exclusion criteria were articles in English and Persian, assessing PPP models or pointing hospital performance indicator. First, titles of the all articles were reviewed and 18690 were excluded due to inconsistency with the study aims and 79 article were duplicated among databases, second abstracts of remaining articles were studied and 76 articles were excluded too because attention to administrative aspects of PPP. Fifty one articles were excluded, for not focusing on PPP models and their performance outcomes, in the results. Then 35 (20 articles in area of PPP and 15 articles in area of hospital performance indicator) most relevance articles to the topic and study aim were studied perfectly (Fig. 1). All articles were reviewed by two of the authors and attributed and themes identified in any articles were written in extraction tables. This made a two independent list with common PPP models and hospital performance indicators.
Fig. 1.
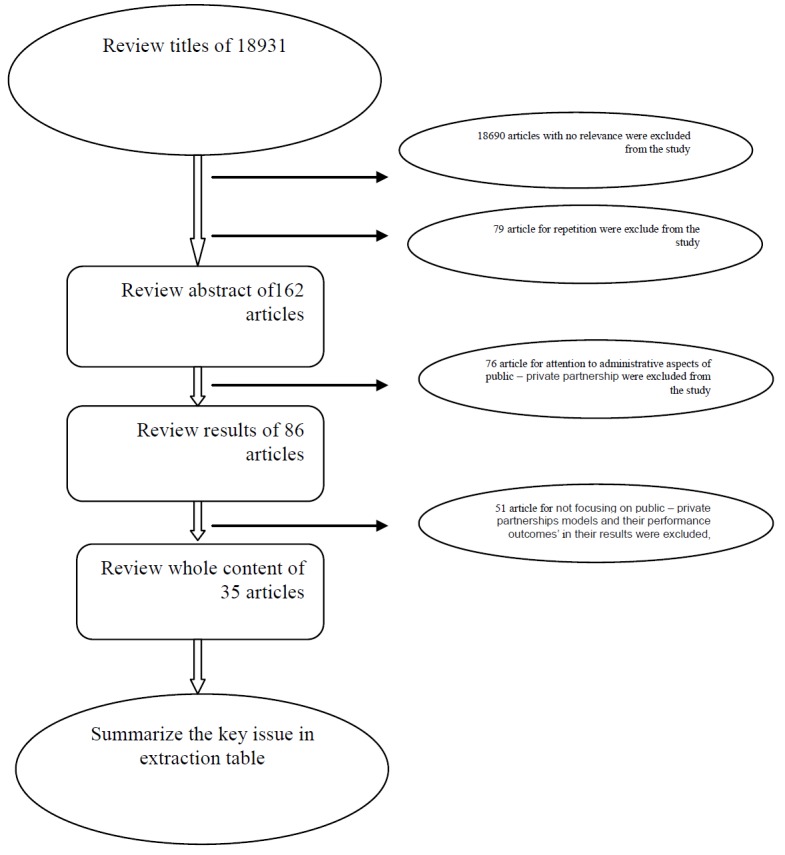
Systematic review process
Expert panel
We hold 3 expert panels with 5 individuals with PhD degree of health care management from Health Care Management and Social Medicine Departments of Tabriz University of Medical Sciences to identify hospital performance indicators and complete these indicators list. In two, three hours sessions, 113 indicators were extracted through nominal group technique. In third session this indicators gather together with indicators were obtained from literature review and their content validity were examined by 6 criteria (as clarity, relatively, simplicity, necessity, measurability and sensitivity [32]. Thirty nine indicators were selected during internal expert panel, these selected indicators were entered in to questionnaires and sent to 20 external (Administrators employed in health organizations) experts who had PhD degree in health care management or health policy making or health economic and they had adequate experience in hospital performance indicators by post. We took 1 month to complete content validity and performance indicators classification questionnaires, and we alarmed finishing time of completion questionnaire by electronic mail (email) two days before. We collected 75% of questionnaires after one month, this questionnaire’s data were compiled to excel 2007 software and after analysis, number of performance indicators was decreased to 16 and three performance areas (Quality- Effectiveness, Efficiency-Financing and Accessibility- Equity) were defined for indicators by combining experts opinion and taking into consideration common classification in the literature.
Analytic Hierarchy Process (AHP) Technique
Third step of the research was spent to determine the selected performance indicators and selected PPP models based on selected performance indicators, through AHP questionnaire. AHP is a standard technique for multiple choice decisions making. In this technique scores obtained from expert panel entered to Expert Choice software for quantitative synthesis and leading in ranking of the performance indicators and PPP models. AHP captures both subjective and objective evaluation measures, providing a useful mechanism for checking performance indicators, consistency relative to considered alternatives, thus reducing bias in decision making. Saaty (1997) introduced this technique to help decision making; accurate and easy selecting among choices [33-34].
We sent AHP questionnaires to 20 internal and external experts. After gathering questionnaire, data entered to excel 2007 to calculate means of performance indicator. Performance indicators means were entered to Expert Choice 11 software (Expert Choice InC, Arlington, USA) and their weight, priority and consistency were extracted. Priority of performance indicators was used as a criterion to compare and prioritize PPP models through AHP technique.
Results
After reading the articles associated with PPP, common model was extracted from various studies (Table 1). During the study of articles and expert panel, about 203 performance indicators of hospitals were obtained. Initially, and during internal expert panel, about 39 indicators were selected. They were decreased to 16 after the external expert panel. Performance indicators, as it was mentioned, are classified into 3 areas of: Quality- Effectiveness, Efficiency-Financing and Accessibility- Equity simultaneously with confirmed content validity (Table2).
Table 1. Common model of public – private partnership in hospitals.
| PPP models | Definition | Sub Models |
| Service contract | ■ The state will pay a private institution to perform certain tasks. These tasks may be performed within or outside the hospital. | ■ Clinical services |
| ■ None clinical services | ||
| outsourcing contract | ■ The government will pay private institution to management and provide the required services in a health institution or a special section of it. Decisions regarding health care staff’s employment, logistics and purchasing medicines and medical supplies are the responsibility of private institution. The risk of contract-related data such as labor can move to a private institution, but the government remains responsible for capital expenditures. | ■ Outsourcing clinical services |
| ■ Outsourcing none clinical services | ||
| Management contract | ■ Government will pay a private institution for the management of government hospital to administrative hospital and provide needed services, but specialized decisions of health care staffs employment, logistics and purchasing medicines and medical supplies is done by the government. Commercial risk and the responsibility for capital expenditures remain with government. | - |
| Leases contract | ■ Private institutions pay to the government to rent the public hospital and then be responsible for managing and providing service in this center. Instead, a private firm acquires the right to collect revenue from their performance. In this case, all commercial risks are transformed to private institutions. The government is still responsible for capital expenditures. | - |
| DBFO(Design, Build, Finance, Operate) contract-PFI(Private Finance Initiative) contract | ■ In this model, private sector, which often form alliances, are responsible for providing public services and it undertakes all stages of the hospital. Private sector is responsible for investment, establishment, management, and providing non-clinical services (such as nutrition, laundry, security, parking services, logistics, etc.) But government still will have responsibility for delivering hospital core services. This model’s basic difference with concession model is in the funding ways of two models. In this model’s private funds that are spent for facilities and public duties, reimbursed by the government and not be reimbursed by the final consumer. | - |
| Concession contract | Public hospital rights will be awarded to private sector. Private institutions with paying fee to the government will operate and, maintains the public hospital. In these types of contracts, capital expenditures will be transferred to private institutions. | ■ Build, Owo, Operate Contract(BOO) |
| 1. BOO CONTRACTS: In this contract, the private sector will take over financing, building, operation, and provide clinical services, non-clinical or both of them. Ownership and control responsibility also will be with the private sector. Private sector will bear construction, investments, commercial risks, without transforming hospital ownership to the public sector at the end of the contract.
2. BOT CONTRACTS: In these contracts, the private sector is responsible for financing, design, building and operation of the public hospital. Ownership and formal control will be with the public sector that will be transferred to this sector the end of the contract period |
■ Build. Operate, Transfer Contract(BOT) | |
| Divesture Contract(privatization) | ■ In these models, government owned hospitals will be sold to private sector. The property will be transformed private institutions and these institutions will be responsible for providing service and capital expenditures. But governments control a monitoring will be maintained. | - |
| Concession contract | Public hospital rights will be awarded to private sector. Private institutions with paying fee to the government will operate and, maintains the public hospital. In these types of contracts, capital expenditures will be transferred to private institutions. | ■ Build, Own, Operate Contract(BOO) |
|
1. BOO CONTRACTS: In this contract, the private sector will take over financing, building, operation, and provide clinical services, non-clinical or both of them. Ownership and control responsibility also will be with the private sector. Private sector will bear construction, investments, commercial risks, without transforming hospital ownership to the public sector at the end of the contract.
2. BOT CONTRACTS: In these contracts, the private sector is responsible for financing, design, building and operation of the public hospital. Ownership and formal control will be with the public sector that will be transferred to this sector the end of the contract period |
■ Build. Operate, Transfer Contract(BOT) | |
| Divesture Contract (privatization) | ■ In these models, government owned hospitals will be sold to private sector. The property will be transformed private institutions and these institutions will be responsible for providing service and capital expenditures. But governments control a monitoring will be maintained. | - |
The selected performance indicators were included into AHP questionnaire and completed by experts. After entering data into the software, the following results were obtained. Based on expert’s idea, respectively area of quality- effectiveness (100%), Accessibility- Equity (35%) and Efficiency-Financing (33%) were selected as priority performance indicators’ areas with consistency ration of 0.006.
Table 2. The selected performance indicators by content validity confirmation.
| Type of indicator | Title of indicator | Type of indicator | Title of Indicator |
| Efficiency-Financing | Beds occupation ratio | Quality- Effectiveness | The pure rate of hospital mortality |
| Beds exchange interval | Readmission number based on diagnose differences | ||
| Average length of stay Based on different diagnosis | Hospital infection rate based on ward / diagnose/ procedure | ||
| Relationship between private income and total costs in hospital | Patients satisfaction percentage | ||
| Hospitals the pharmaceutical costs relation to total costs to hospitals | Staffs satisfaction percentage | ||
| Accessibility- Equity | Average outpatients waiting time | Hospital accidents prevalence rate | |
| Average inpatients waiting time | legal complaint from hospital within one year | ||
| Relation between total number of staffs to active beds | Success to hospitals in obtaining certificates of management quality |
Throughout the Quality- Effectiveness constituent, selected indicators were the rate of hospital infections (100%), hospital accidents prevalence rate (73%), pure degree for hospital mortality (63%), and patients’ satisfaction percentage (53%). All these indicators were considered as prioritized indicators in this area with consistency rate of 0.02.
In Accessibility- Equity area the indicators like average outpatients waiting time (100%), and average inpatients waiting time (74%), with consistency rate of 0.09, were selected.
In Efficiency-Financing area indicators like average length of stay based on different diagnosis (100%), beds occupation ratio (99%), and Relationship between private income and total costs in hospital (97%), with consistency rate of 0.06 were selected (Table 3).
Table 3. Results of prioritizing hospitals performance indicators.
| Areas of Performance Indicators | Indicators, Percent (%) | Consistency Rate | |
| Quality- Effectiveness | The pure rate of hospital mortality Readmission number based on diagnose differences Hospital infection rate based on ward / diagnose/ procedure Patients satisfaction percentage Staffs satisfaction percentage Hospital accidents prevalence rate legal complaint from hospital within one year Success to hospitals in obtaining certificates of management quality 23 |
63 20 100 53 21 72 25 23 |
0.02 |
| Accessibility- Equity | Average outpatients waiting time Average inpatients waiting time Relation between total number to staffs to active beds 54 |
74 100 54 |
0.09 |
| Efficiency-Financing | Beds occupation ratio Beds exchange interval Average length of stay Based on different diagnosis Relationship between private income and total costs in hospital Hospitals the pharmaceutical costs relation to total costs to hospitals |
99 82 100 97 53 |
0.06 |
In the prioritization of PPP models based on performance indicators of hospitals with AHP technique results were mentioned in Table 4.
Table 4. Results of prioritizing public – private partnership models based on performance indicators of hospitals.
| Performance Indicators | PPP models (%) | Consistency Rate |
| Hospital infection rate based on ward / diagnose/ procedure | Clinical Services Contracts(97) | 0.02 |
| None Clinical Services Contracts(44) | ||
| Outsourcing Clinical Services(100)* | ||
| Outsourcing None Clinical Services(61) | ||
| Management Contract(79) | ||
| Leases Contract(51) | ||
| Design, build, finance ( DBFO) or private | ||
| finance initiative(PFI) (41) | ||
| Build,Owo,Operate Contract(BOO) (47) | ||
| Build.Operate,Transfer Contract(BOT)(42) | ||
| Divesture Contract(privatization)(50) | ||
| hospital incidents break out rate | Clinical Services Contracts(58) | 0.03 |
| None Clinical Services Contracts(47) | ||
| Outsourcing Clinical Services(77) | ||
| Outsourcing None Clinical Services(73) | ||
| Management Contract(94) | ||
| Leases Contract(78) | ||
| Design,build,finance ( DBFO) or private | ||
| finance initiative(PFI) (56) | ||
| Build,Owo,Operate Contract(BOO)(100)* | ||
| Build.Operate,Transfer Contract(BOT)(75) | ||
| Divesture Contract(privatization)(89) | ||
| The pure rate of hospital mortality | Clinical Services Contracts(70) | 0.02 |
| None Clinical Services Contracts(45) | ||
| Outsourcing Clinical Services(100)* | ||
| Outsourcing None Clinical Services(68) | ||
| Management Contract(64) | ||
| Leases Contract(65) | ||
| Design,build,finance ( DBFO) or private finance initiative(PFI) (33) | ||
| Build,Owo,Operate Contract(BOO)(66) | ||
| Build.Operate,Transfer Contract(BOT)(52) | ||
| Divesture Contract(privatization)(60) | ||
| Patient satisfaction percentage | Clinical Services Contracts(65) | 0.02 |
| None Clinical Services Contracts(68) | ||
| Outsourcing Clinical Services(89) | ||
| Outsourcing None Clinical Services(100)* | ||
| Management Contract(98) | ||
| Leases Contract(77) | ||
| Design,build,finance ( DBFO) or private finance initiative(PFI) (80) | ||
| Build,Owo,Operate Contract(BOO)(85) | ||
| Build.Operate,Transfer Contract(BOT)(76) | ||
| Divesture Contract(privatization)(81) | ||
| Average inpatients waiting time | Clinical Services Contracts(64) | 0.04 |
| None Clinical Services Contracts(24) | ||
| Outsourcing Clinical Services(100)* | ||
| Outsourcing None Clinical Services(24) | ||
| Management Contract(62) | ||
| Leases Contract(54) | ||
| Design,build,finance ( DBFO) or private finance initiative(PFI) (66) | ||
| Build,Owo,Operate Contract(BOO)(70) | ||
| Build.Operate,Transfer Contract(BOT)(52) | ||
| Divesture Contract(privatization)(79) | ||
| Average outpatients waiting time | Clinical Services Contracts(65) | 0.04 |
| None Clinical Services Contracts(23) | ||
| Outsourcing Clinical Services(92) | ||
| Outsourcing None Clinical Services(23) | ||
| Management Contract(100)* | ||
| Leases Contract(53) | ||
| Design,build,finance ( DBFO) or private finance initiative(PFI) (59) | ||
| Build,Owo,Operate Contract(BOO)(86) | ||
| Build.Operate,Transfer Contract(BOT)(51) | ||
| Divesture Contract(privatization)(96) | ||
| Average length of stay Based on different diagnosis | Clinical Services Contracts(40) | 0.05 |
| None Clinical Services Contracts(28) | ||
| Outsourcing Clinical Services(59) | ||
| Outsourcing None Clinical Services(34) | ||
| Management Contract(61) | ||
| Leases Contract(43) | ||
| Design,build,finance ( DBFO) or private finance initiative(PFI) (50) | ||
| Build,Owo,Operate Contract(BOO)(58) | ||
| Build.Operate,Transfer Contract(BOT)(37) | ||
| Divesture Contract(privatization)(100)* | ||
| Beds occupation ratio | Clinical Services Contracts(50 | 0.05 |
| None Clinical Services Contracts(30) | ||
| Outsourcing Clinical Services(71) | ||
| Outsourcing None Clinical Services(42) | ||
| Management Contract(55) | ||
| Leases Contract(61) | ||
| Design,build,finance ( DBFO) or private finance initiative(PFI) (69) | ||
| Build,Owo,Operate Contract(BOO)(87) | ||
| Build.Operate,Transfer Contract(BOT)(54) | ||
| Divesture Contract(privatization)(100)* | ||
| Relationship between private income and total costs in hospital | Clinical Services Contracts(58) | 0.06 |
| None Clinical Services Contracts(37) | ||
| Outsourcing Clinical Services(75) | ||
| Outsourcing None Clinical Services(47) | ||
| Management Contract(63) | ||
| Leases Contract(56) | ||
| Design,build,finance ( DBFO) or private finance initiative(PFI) (76) | ||
| Build,Owo,Operate Contract(BOO)(57) | ||
| Build.Operate,Transfer Contract(BOT)(47) | ||
| Divesture Contract(privatization)(100)* |
*high Priority PPP model in selected performance indicator
Discussion
The PPP models in this study were classified in seven categories (based on design and build, operation, management, service delivery, ownership, and payment mechanism’s criteria); this classification is consistent with the classification of most studies [2,5,29,35-44].
Through the present study all hospital indicators were classified under three categories of quality- effectiveness, efficiency-financing and accessibility- equity, and indicators like hospital infection rate based on ward / diagnose/ procedure, hospital accidents prevalence rate. The pure rate of hospital mortality, patient satisfaction percentage, average inpatients waiting time, average outpatients waiting time, average length of stay based on different diagnosis. Beds occupation ratio and relationship between private income and total costs in hospital were chosen as key performance indicators.
In the similar way, performance frameworks of Australasian hospitals are made of quality, relevance, access and equity, and efficiency areas [45]. Classification of hospital performance indicators in other studies is consistent with the classification of this study in some areas [46-48].
Various studies have introduced several key performance indicators. As an example Jonidi, have mentioned hospital performance indicators according to the Ministry of Health and Medical Education (MOHME), indicators like active beds to fixed beds ratio, the bed occupancy, bed-performance ratio, the rotation of beds, admissions per bed and the average stay duration of patient admitted to all admitted ratio[49]. Another study elected performance indicators of stay duration, percentage of bed occupancy and bed turnover as key performance indicators [50]. This study used performance indicators of stay duration and hospital bed occupancy rate, which is consistent with recent research findings. But our study considered wider range than that of Zabolie’s study in choosing indicators by classifying them. Selected key indicators in other studies in some areas are compatible with finding of our study [51-53].
In prioritization of PPP based on hospital’s performance indicators, according to the experts view, models such as clinical services outsourcing descent to indicators like hospital infection rate, pure rate of hospital mortality, average inpatients waiting time, build ,own, Operate(BOO) model descent to hospital accidents prevalence rate, none clinical services outsourcing model descent to patient satisfaction percentage, management model descent to average outpatients waiting time and privatization model descent to indicators like average length of stay based on different diagnosis, beds’ occupation ratio and relationship between private income and total costs were selected.
In this study, the outsourcing of clinical services has the ability to improve hospital infection rate, pure rate of hospital mortality, and average inpatients waiting time. While at study of Davis, to reduce hospital infection rate, outsourcing non-clinical services (cleaning contract) is recommended [54]. The cause of this mismatch in the Davis study and this research may be due to implementing a limited approach in the study of Davis. Because alongside with environmental factors, clinical factors and other factor are affecting hospital infections, so we should have a holistic perspective to this concern.
The reason why outsourcing clinical services have an effect on reducing mortality is maybe due to the maximum effort of private contractors to maintain quality of clinical processes to retain maximum customers or effect of public sectors’ high degree standards that forced private sector to continuously improve quality which lead to reduce the mortality rate in the hospital.
Barati in their study, has explained that outsourcing in addition to improve service quality and patient satisfaction also increased access to services [55]. These findings, confirmed the results of our study.
In present study outsourcing non-clinical services was determined as priority model based on patient satisfaction percentage. Different studies are approved using outsourcing none clinical service's model to increase patient satisfaction [56-63].
In the present study, build, own, operation (BOO) model was selected as the top model in the base of incidence of hospital events indicator. This selection can be due to the presence of private sector in all stages of construction and the need to establish public sector standards in all phases of construction and operation of hospitals by the private sector. Failure to meet the agreed criteria and standards for public sector led to the consideration paying fines and punishments, and in severe cases will result in contract termination. Private sector efforts to eliminate and reduce hazards and risks in compliance with the standards of hospital and this will ultimately reduce accidents.
Also in this study, management model was selected as a top PPP model, based on the average waiting time of outpatient services indicator. It may be related to competencies and technical - managerial skills of private sector, contract standards and payment to the private sector.
Privatization was chosen as the priority model based on all indicators of efficiency- financing area (indicators like average length of stay based on different diagnosis, beds occupation ratio and relationship between private income and total costs in hospital). This is due to the nature of the private sector in order to earn more profit returns. Private sector will be used variety of methods for maximum utilization of capacity and get a higher monetary value. In fact, what should be considered more than other models in the model of full privatization, supervisory and regulatory power of government to put pressure on the private sector monopolistic behavior?
In study of Sharifzaree, privatization caused approximately 4% decrease on bed occupancy rate and increased cost of hospital since 1990 to 2005 [64]. These studies’ findings are inconsistent with the present findings that concluded privatization model has a capacity to improve the rate of bed occupancy and increased revenues for the hospital, the cause of conflict in this area may be non-normative classification of contract or executable inability of private sector.
According to Van de, private investment in hospitals leads to innovation, improve efficiency and reduce costs. These findings about improving efficiency are in agreement with our studies’ findings [65].
Conclusion
Implementing PPP models are one of the government's key policy tools. In most of studies it were reported that PPP hospitals were remarkably more efficient, performing better than unreformed hospitals in a number of areas, PPP hospitals represent major improvements and productivity, with no evidence of quality shortfalls [60,66-72].
As a final result of study, presence of private sector in non clinical affairs of public hospitals will increase services customer and presence of this sector in clinical affairs will increase the quality of clinical services. Privatization also has full potential for increased hospital efficiency and better use of hospital resources. On equity indicators, especially patient waiting time, using private sector management will be upgraded these indicators.
Iran policy makers for solving hospital financing problems and in response to legal spaced provided to participate with private sector in public hospitals needs to be familiar with different PPP options and their effect on hospitals performance, this study had been provided most common PPP options in the field of hospitals and gathered suitable evidences from experts for choosing appropriate PPP option for public hospitals. This study can be an Initiator research for Future studies concerning the PPP in Iran’s hospital.
Limitation
PPP is a new issue in hospitals of Iran and a low number of specialists exist in this field for the survey and consultation. We had accessed limited free databases to search references in our study.
Suggestion for future studies
Public – private partnership is not one-way relationship and both of public and private sectors can use capabilities of opponent in their hospitals, but in this study because of new lows in our country supporting public sector to use private sectors capability to reduce government sizes and reducing government tasks (legal requirements of general policies of 44 articles” and “the third and fourth national development programs) our study‘s aim was to identify which models help to enforcement of these laws. We can suggest as a topic for future research, identifying and survey on models of participating public sector in private hospitals.
Acknowledgments
We would like to express our gratitude to all those who gave us the possibility to complete this article. We want to thank the Vice Chancellor for Research and Technology of Tabriz University of Medical Sciences for financial support of this research. The authors declare that there is no conflict of interest.
References
- [1].Barr DA. Ethics in public health research: a research protocol to evaluate the effectiveness of public-private partnerships as a means to improve health and welfare systems worldwide. Am J Public Health. 2007;97(1):19–25. doi: 10.2105/AJPH.2005.075614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2]. Dowdeswell B, Heasman M. Public private partnerships in health, a comparative study. Durham: University of Durham. England; 2004.
- [3]. Alfen H, Kalidindi S, Ogunlana S, Wang S, Abednego M, Jungbecker A, et al. Public-private partnership in infrastructure development case studies from Asia and Europe. Weimar: Bauhaus-University Weimar, Germany; 2009.
- [4].Grimsey D, Lewis M. Are public- private partnerships values for money? Evaluating alternative approaches and comparing academic and practitioner views. Account Forum. 2005;29:345–78. [Google Scholar]
- [5]. Rwelamola PD. Private financing of construction projects and procurement Systems: an integrated approach. CIB World Building Congress, Wellington, New Zealand, pp 259; 2001.
- [6]. World Health Organization (2002). Health and Welfare Systems Development in the 21st Century: Proceedings of the Third Global Symposium. Kobe, Japan, pp.6-8.
- [7].Mckee M, Edwards N, Atun R. Public-private partnerships for hospitalsBull. World Health Organ. 2006;84(11):890–6. [PMC free article] [PubMed] [Google Scholar]
- [8].Barrows D, Macdonald I, Supapol A. Public private partnerships in Canadian healthcare a case study of the Brampton civic hospital . Prepared for the OECD. Canada: York University; 2011. 51-61 [Google Scholar]
- [9].Jabbari Beyrami H, Joodati A, Bakhshiyan F. Results of staff units downsizing in the health network of Iran (Tabriz metropolis experience) Health Manage. 2006;9(23):51–8. [Google Scholar]
- [10]. Jabbari Beyrami H, Bakhshiyan F. Decentralization in health systems: NPMC press. Tabriz; 2007.
- [11].Das A. Public-private partnerships for providing healthcare services. Indian J Med Ethics. 2007;4(4):174–5. doi: 10.20529/IJME.2007.069. [DOI] [PubMed] [Google Scholar]
- [12]. Haarhoff K. Public- private partnerships as an alternative service delivery option: a multiple case study of the health care sector in South Africa: Stellenbosch, South Africa; 2008.
- [13].Hanlin R, Chataway J, Smith J. Global health public-private partnerships: IAVI, partnerships and capacity building. Afr J Med Sci. 2007;36:69–75. [PubMed] [Google Scholar]
- [14].Jabbari Beyrami H, Tabibi J, Delgoshayi B, Mahmudi M, Bakhshiyan F. Mechanisms of decentralization in provision of health services in health system of selected countries and planning a model for Iran. Health Manage. 2007;10(27):33–40. [Google Scholar]
- [15].Jabbari Beyrami H, Bakhshiyan F. Decentralization in the stewardship function of different countries health systems and provide a template for Iran. Med J Tabriz Uni Med Sci. 2007;29(1):7–8. [Google Scholar]
- [16].Hentschel CC. Public-private partnerships: new ways to discover develop and deliver drugs for tropical diseases. Southeast Asian J Trop Med Publ Health. 2004;35:1–4. [PubMed] [Google Scholar]
- [17].Easton A. Public-private partnerships and public health practice in the 21st century: looking back at the experience of the Steps Program. Prev Chronic Dis. 2009;6(2):A38. [PMC free article] [PubMed] [Google Scholar]
- [18]. Article 44 of the Constitution of the Islamic Republic of Iran; 2006.
- [19]. Third program of Economic, Social and Cultural improvement of Islamic Republic of Iran; 2000.
- [20]. Fourth plan of Economic, Social and Cultural improvement of Islamic Republic of Iran; 2004.
- [21].Roski J, McClellan M. Measuring health care performance now, not tomorrow: Essential steps to support effective health reform. Health Affairs. 2011;30(4):682. doi: 10.1377/hlthaff.2011.0137. [DOI] [PubMed] [Google Scholar]
- [22]. Smith PC, Mossialos E, Papanicolas I. Performance measurement for health system improvement: experiences, challenges and prospects. World Health Organization, on behalf of the European observatory on health systems and policies. Tallin, Estonia; 2008.
- [23].Widdus R. Widdus RPublic-private partnerships for health: their main targets, their diversity, and their future directionsBull. World Health Organ. 2001;79(8):713–20. [PMC free article] [PubMed] [Google Scholar]
- [24].Vrangbaek K. Public-private partnerships in the health sector: the Danish experience. Health Econ Policy Law. 2008;3(Pt 2):141–63. doi: 10.1017/S1744133108004465. [DOI] [PubMed] [Google Scholar]
- [25].Vining AR, Globerman S. Contracting- out health care services: a conceptual framework. Health Policy. 1999;46:77–96. doi: 10.1016/s0168-8510(98)00056-6. [DOI] [PubMed] [Google Scholar]
- [26].Van der Z, Van der VT, De Jonge H. Private investment in hospitals: a comparison of three health care systems and possible implications for real estate strategies. HERD Journal. 2010;3(3):70–86. doi: 10.1177/193758671000300308. [DOI] [PubMed] [Google Scholar]
- [27].Turani S, Maleki M, Godusi Mogadam S, Gohari M. Efficiency and effectiveness of Firuzgar hospital before and after outsourcing. Health Manage. 2009;12(38):59–70. [Google Scholar]
- [28].Thomason J, Rodney A. Public-private partnerships for health--what does the evidence say? P N G Med J. 2009;52(3-4):166–78. [PubMed] [Google Scholar]
- [29]. Taylor R, Blair S. Public Hospitals: Options for Reform through Public-Private Partnerships, The World Bank’s Private Sector and Infrastructure Network, Washington, USA; 2002.
- [30].Smith ER. Public-private partnerships in health care. Can J Cardiol. 2003;19(12):1446–7. [PubMed] [Google Scholar]
- [31].Silversides A. Public-private partnerships, part 1: the next hospital wave. CMAJ 2008. 21;179(9):883–5. doi: 10.1503/cmaj.081540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Yaghmale F. Content validity and its estimation. Med Edu. 2003;3(1):25–27. [Google Scholar]
- [33].Dyer Js. Remarks on Analytic Hierarchy Process. Manage Sci. 1990;36(3):249. [Google Scholar]
- [34].Saaty TL. Decision making with the analytic hierarchy process. Int J Services Sciences. 2008;1(1):83–98. [Google Scholar]
- [35]. Nikolic IA, Maikisch H. Public - private partnership and collaboration in health sector (An overview with case studies from recent European experience). Washington. USA; 2006.
- [36]. Mehta A, Bhatia A, Chatterjee A. Improving health and education service delivery in India through public–private partnerships. Mandaluyong City, Philippines; 2010.
- [37].Pessoa A. Public - private partnerships in developing countries: are infrastructures responding to the new ODA strategy. Int Dev. 2008;1(20):311–25. [Google Scholar]
- [38].Adams J, Young A, Zhihong Wu. Public - private partnership in China. Int J Public Sector Manage. 2006;19(4):384–96. [Google Scholar]
- [39].Bojovie V. Public - private partnership as a last resort for traditional public procurement. Panoeconomicus. 2006;3:299–311. [Google Scholar]
- [40].Sadka E. Public - private partnership; a public economics perspective. Cesifo Econ Stud. 2007;53(3):466–90. [Google Scholar]
- [41]. Guidebook on Promoting Good Governance in Public-Private Partnerships. Europe UNECF, editor. Geneva (Switzerland): United Nations; 2008.
- [42].McKee M, Edwards N, Atun R. Public-private partnerships for hospitals. Bull World Health Organ. 2006;84(11):890–6. [PMC free article] [PubMed] [Google Scholar]
- [43]. Iossa E, Spangnolo G, Vellez M. Contract design in public-private partnerships. World Bank, Washington, USA; 2007.
- [44]. Jasso H Z. Public- private partnerships: a multi dimensional model for contracting. University of Navara, Pamplona, Spain; 2005.
- [45]. Yusefiyan S, Najafi M. Reported in the literature review "assessing organizational performance"(hospital centers) Tehran, Iran; 2008.
- [46].Basu A, Howell R, Gopinath D. Clinical performance indicators: intolerance for variety? Int J Health Care Qual Assurance. 2010;23(4):436–49. doi: 10.1108/09526861011037489. [DOI] [PubMed] [Google Scholar]
- [47].Groene O, K.H.Skau K, Frqlich A. An international review of projects on hospital performance assessment. Int J Qual Health Care. 2008;20(3):162–71. doi: 10.1093/intqhc/mzn008. [DOI] [PubMed] [Google Scholar]
- [48].Veillard J, Champange F, Klazinga N, Kazandjian V. A performance assessment framework for hospitals: the WHO regional office for Europe PATH project. Int J Qual Health Care. 2005;17(6):487–96. doi: 10.1093/intqhc/mzi072. [DOI] [PubMed] [Google Scholar]
- [49].Jonidi N, Sadegi M, Izadi M, Ranjbar R. Compare a Tehran hospital's indicators with National standards. Miliatary Med. 2010;12(4):223–8. [Google Scholar]
- [50].Zaboli R, Seyedin SH, Khosravi S, Tofigi S. Effect of per- case reimbursement on performance indicators of a military hospitals ward. Military Med. 2011;13(3):155–8. [Google Scholar]
- [51].Nasiripour AA, Gohari MR, Nafisi A. Branding and functional indicators relationship. Health Admin. 2009;13(41):15–20. [Google Scholar]
- [52].Sajjadi H, Sajjadi Z, Hadi M. Is there a method for the simultaneous comparison of key hospital performance indicators? Health Inform Manage. 2011;8(1):71–81. [Google Scholar]
- [53].EbadifardAzar F, Ansari H, Rezapur A. Survey of hospital bed-day cost and performance indicators in selected hospitals of Iran University of Medical Sciences. Manage Med Inform. 2004;7(18):37–44. [Google Scholar]
- [54]. Davies S. Fragmented management, hospital contract cleaning and infection control. Policy Polit 2010 (3): 445–63.
- [55].Vatankhah S, Maleki MR, Tofighi SH, Barati O, Rafiei S. The study of management contract conditions in healthcare organizations of selected countries. Health Manage. 2012;3(9):224–231. [Google Scholar]
- [56].Tabibi SJ, Kakhani MJ, Ehsanichime E. Reduction strategy evaluation policies in hospital support services subsidiary of the Ministry of Health and Medical Education. Health Manage. 2007;10(30):59–66. [Google Scholar]
- [57]. Novinruz S. Experience of partnerships with non-governmental sector in Tabriz in the 80s. Tabriz university of Medical sciences, Tabriz, Iran; 2007.
- [58]. Farahabadi SM, Jandagiyan M, Nagdi P, Hagigat M, Ferdosi M. Measuring effectiveness of nonclinical hospital services and need to develop outsourcing to reduce costs. Health Care Management.Kerman University of Medical Sciences, Kerman, Iran; 2008.
- [59]. Judi K. Kitchen affairs cooking materials hospitals. Esfahan University of Medical Sciences, Esfehan, Iran; 2006.
- [60].Marr JA, Tam R, Simms S, Bacchus F. An integrated outsourcing solution at York central hospital. Health Care Quart. 2011;14(1):95–7. doi: 10.12927/hcq.2011.22165. [DOI] [PubMed] [Google Scholar]
- [61]. Rejaliyan F, Farahabadi SM, Hagigat M, Ferdosi M. Outsourcing hospitals medical records services, challenge point in health system goals. Health Care Management. Kerman University of Medical Sciences, Kerman, Iran; 2008.
- [62].Moschuris S, Kondylis M. Outsourcing in public hospitals: a Greek perspective. J Health Organ Manage. 2006;20(1):4–14. doi: 10.1108/14777260610656534. [DOI] [PubMed] [Google Scholar]
- [63].Lorence DP, Spink A. Health care information systems outsourcing. Int J Inform Manage. 2004;24:131–45. [Google Scholar]
- [64]. Sharifzare M. Appresial of outsourcing effectiveness in education hospitals. Esfahan University of Medical Sciences. Esfehan, Iran; 2005.
- [65].Van JD. Monitoring health care processes: a framework for performance indicators. Int J Health Care Qual Assurance. 1999;12(5):214–21. [Google Scholar]
- [66].La Forgia GM, Harding A. Public-private partnerships and public hospital performance in Sao Paulo, Brazil. Health Aff (Millwood) 2009;28(4):1114–26. doi: 10.1377/hlthaff.28.4.1114. [DOI] [PubMed] [Google Scholar]
- [67].Sekhri N, Feachem R, Ni A. Public-private integrated partnerships demonstrate the potential to improve health care access, quality, and efficiency. Health Aff (Millwood) 2011;30(8):1498–507. doi: 10.1377/hlthaff.2010.0461. [DOI] [PubMed] [Google Scholar]
- [68].Castella F. Outsourcing in hospital services. Health Estate. 1999;53(5):32–4. [PubMed] [Google Scholar]
- [69].Danvers K, Nikolov P. Does outsourcing affect hospital profitability? J Health Care Financ. 2010;37(1):13–29. [PubMed] [Google Scholar]
- [70].Tavakol P, Labruto F, Bergstrand L, Blomqvist L. Effects of outsourcing magnetic resonance examinations from a public university hospital to a private agent. Acta Radiol. 2011;52(1):81–5. doi: 10.1258/ar.2010.090320. [DOI] [PubMed] [Google Scholar]
- [71].Yigit V, Tengilimoglu D, Kisa A, Younis MZ. Outsourcing and its implications for hospital organizations in Turkey. J Health Care Financ. 2007;33(4):86–92. [PubMed] [Google Scholar]
- [72].Carey K, Dor A. Trends in contract management: the hidden evolution in hospital organization. Health Aff (Millwood) 2004;23(6):192–9. doi: 10.1377/hlthaff.23.6.192. [DOI] [PubMed] [Google Scholar]


