Abstract
Background: Iran started a new public-private partnership model in form of health coopera¬tives which is somehow different from other types of health cooperatives throughout the world. In this study we compared the performance and quality of health services in public health cen¬ters (PHCs) and cooperative health centers (CHCs).
Methods: In this comparative study performance quality of two cohorts of public and coopera¬tive health centers were compared in several health service delivery programs over the time pe¬riod of 2001- 2002.
Results: Screening program: the rate of visited population during screening program was higher in CHCs. Maternal health care program: In some of studied programs CHCs had better results. Child health care: Most indicators were better or similar in CHCs. School health program and Health education: All indices were better or similar in CHCs. Environmental health: population based positive function was not significantly different for the population covered by CHCs compared to population covered by PHCs. Management: Client and staff satisfaction as well as participation and attitudes of personnel towards management was better in CHCs. Mean annual cost per capita of the covered population by PHCs was higher.
Conclusion: CHCs as a public private partnership model in Iran may deliver preventive health care services as effective as PHCs in many fields and even better in some areas.
Keywords: Health, Model, Public, Iran
Introduction
It is often argued that efficiency and quality of performance in private sector health services is higher than public sector. However, in developing countries government remains to be the largest single provider of primary health care services. The need to improve efficiency, increase quality, reduce costs and meet internal and external demands within health care provider units, poses huge challenges towards health policy makers in low and middle-income countries.
State domination on preventive health service delivery in many developing countries continues to be a major challenge during health reform programs. But it must also be taken into account, as stated in a world health report, that there is no necessary connection between public money and public provision, although traditionally most governments have spent most or all of their health funds on their own service providing institutions [1].The appropriate role of public and private finance/provision in health care has been the subject of debate and discussion in many countries [2-9].
Public health sector in Iran is responsible for a great majority of preventive health services using a subsidizing system. Private health sector although quite active in private clinics and hospitals but has been inactive in case of preventive health care. In part of a health reform program, Iran started a particular public-private partnership model through the establishment of health cooperatives. These cooperatives are somehow different from other types of health cooperatives throughout the world.
In Iran, based on state constitution, a separate ministry called “Ministry of Cooperatives” has been established. This powered the cooperatives to be quite active in many economic and industrial fields. Nevertheless, the first health cooperatives in Iran were established in East Azerbaijan Province just over the last decade. Cooperatives can form a new alternative for public health sector in delivering preventive health services.
We conducted the present study to compare the performance and quality of health services in public health centers (PHCs) versus cooperative health centers (CHCs). The CHCs’ roles and responsibilities as well as the process of their establishment are briefly described below.
Roles and Responsibilities of transferred health service delivery to CHCs:
Each CHC had to be responsible for delivering preventive health services to a population ranging from 9000 to 17000 people. These included immunization, maternal and child health care, family planning, environmental heath, school health, health education and outpatient visits. This is started with an annual census followed by periodic visits and health care delivery. Health care delivery was based on protocols designed as standard minimal necessary health services by Iranian Ministry of Health.
All health care costs were provided by governmental subsidy as a capitation-based payment method for each service package. It was done through contracts between provincial health department and CHCs. Amount of per-capita payment for each service package could differ based on the quality of delivered services. Quality evaluation was made by provincial and district health center experts every six months. This means that if health cooperatives delivered better quality services they earned more money. Most given preventive health services in each service package were predefined as free of charge services and customers did not pay for them. For some services not defined as free, CHCs charged customers directly but on governmentally established tariffs which are usually lower than private tariffs.
Payments to CHCs by government in this contracting system were done every three months. Cooperatives were responsible to cover all ongoing costs of health centers, except for vaccines, preventive heath drugs and data sheets for surveillance.
Process for establishment of health cooperative:
At first, a request for proposal (RFP) was announced describing project goals and objectives as well as application terms and conditions. Required qualifications announced are as follows:
Iranian citizenship
Having at least seven members as follows:
Two general practitioners preferably one male and one female.
- Two midwives or family health graduates with at least two years of academic education
- One midwife with four years of academic education
- One environmental health expert with 2-4 years of related academic education.
- A male nurse with 2-4 years of academic education.
- Not being currently employed by public or private sector
- Upper age limit of 30 years for males and 35 years for females.
Having certificate of completion of the post educational obligations and permanent medical license if needed (i.e. for general practitioners).
All qualified applicants underwent a process as described in following steps to start contribution in health service delivery as a health cooperative (Fig. 1).
Fig.1.
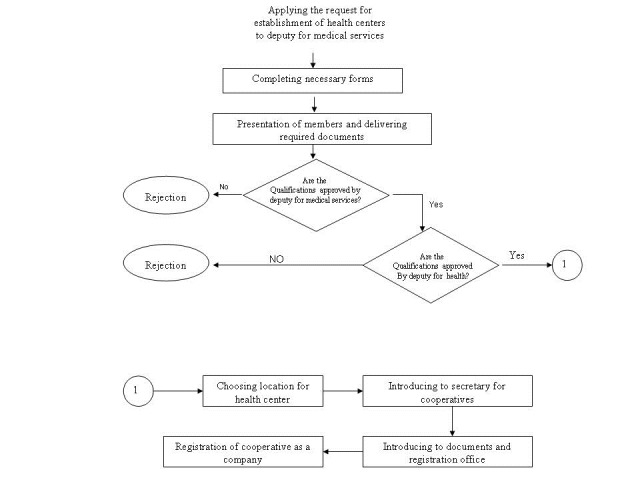
Flowchart for stages of a health cooperative establishment
Materials and Methods
Study design and population
In this comparative observational study, performance of two groups of public and cooperative health centers were compared in health service delivery programs over the time period 2001 - 2002. As this study was not designed before the intervention implemented, it was considered as an observational study conducted through a cross-sectional design. However as the key informants during implementation of the cooperative health centers in Iran are contributors to this study, we were able to provide further details of intervention. Study population was the recipient of health services from 18 PHCs versus population covered by nine health centers transferred to cooperatives called as CHCs. The CHCs were pre-established at the time this study was started and the researchers had no option in allocating areas. However, for each of the nine CHCs two public health centers were selected as controls based on socioeconomic similarities to make the comparisons acceptable.
Data collection and analysis
Different sources for data collection were used in this study:
The main method to compare the health services delivered by CHCs and PHCs was a population survey. A total of 572 households from the population, covered by 18 public health centers, and 428 households from population, covered by nine cooperative health centers, were investigated. Data were collected during a 3-month study period using special questionnaires designed with improved content validity sending them out to be evaluated by six experts. The main topics included in the questionnaire were coverage of health programs, quality of health care services, health education, health outcomes, customer satisfaction and administrative practice.
Assessing available household registers and health care records regarding different fields of health care corresponding information was collected.
All physicians and professional staff working in health centers were interviewed and filled in questionnaires with respect to job satisfaction.
Twenty clients randomly enrolled in each health center were also interviewed. Systematic random sampling based on patient registration consecutive order was used.
-
A checklist was designed to collect data regarding financial measurements used along with checking for financial registers. Income and costs of health centers were measured excluding supervision cost and property maintenance and property value.
Data were analyzed using SPSS 10 statistical software package. Chi-Squared and t tests were used to analyze data.
The study was approved by the Ethics Committee of Tabriz University of Medical Sciences and financed by a World Health organization grant.
Results
Some basic data revealing the similarities in both groups are given in Table 1. Various health service delivery programs were compared between CHCs and PHCs in several subheadings as follows.
Table 1. Basic characteristics of populations covered by CHCs and PHCs.
| CHCs | PHCs | P value | ||
| JOB | employees | 35.8 % | 33.1 % | NS |
| Workers | 4% | 3.7% | ||
| Other nongovernmental jobs | 25.2% | 26.2% | ||
| Housewives | 30.4% | 32.9% | ||
| No jobs | 4.6% | 4.1% | ||
| Education in years(mean) | 7.1 | 7 | NS | |
| Age(mean) | 29.7 | 29.4 | NS | |
| Number of household members(mean) | 4.3 | 4.3 | NS | |
| *NS: Statistically Non-significant(P value > 0.05) |
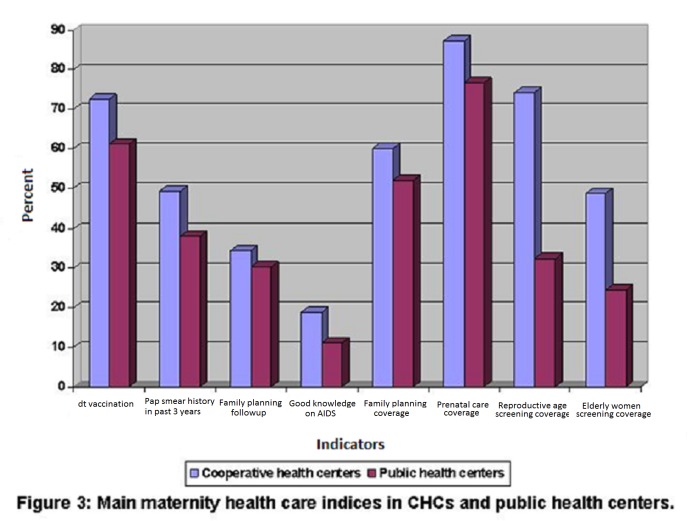
Case finding (screening) program
The center visitation rate for different age groups during case finding program was higher in cooperative health centers compared to public health centers. 23.2% of covered population for public health centers and 53.8% of covered population for cooperative health centers had received periodic medical examinations. A statistically significant difference was found among all age or target groups (P<0.001). Cooperative health centers had more desirable service delivery function (39.8%) than public health centers (17.8%) for high risk groups such as elderly people (Fig. 2).
Fig. 2.
Relative frequency of screened population in different age and sex groups
Child health care program
Following indices had statistically better status among CHCs compared to PHCs:
Ability of mothers in interpreting child growth charts; the figures were 81.3% in CHCs compared to 57.5% in PHCs (P< 0.05).
Infant health care coverage; the figures were 91.8% in CHCs compared to 82.5% in PHCs (P< 0.05).
The care coverage for 1- 6 year-year-old children; the figures were 69.6% in CHCs compared to 55.2% in PHCs (P< 0.01).
Following indices had no statistically significant difference between CHCs and PHCs:
Child care follow up in due time(50% in CHCs compared to 42.7% in PHCs)
Perfect filling of child growth sheets (69.4% in CHCs compared to 59% in PHCs)
Growth status of children based on growth percentiles (89.8% in CHCs and 74.3% in PHCs had favorable growth)
Mothers' knowledge about the health care status of their children was 77.6% in CHCs and 80.6% in PHCs.
The sole index found to have better status in PHCs was the percentage of children having a growth chart. The figure was equal to 67.5% in CHCs and 83.5% in PHCs (P<0.05)
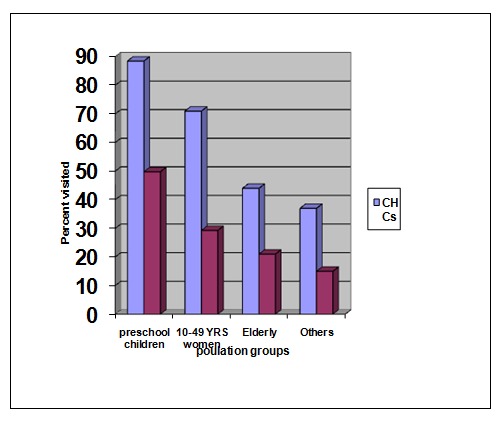
Maternal health care program
The proportion for those women having dt (diphtheria- tetanus) vaccination record (card) was higher in population covered by CHCs (65.2 vs. 61.2, P<0.01). The rate for performing a cervical smear examination during the national program for cervical cancer screening was higher for the women covered by CHCs (P<0.01) (49.3 vs. 38). No significant difference was found between the knowledge level of women covered by CHCs about the importance of cervical examination when compared with PHCs (59 and 52 respectively). Women covered by CHCs had higher knowledge about family planning methods (P<0.01). No significant difference was identified on using different types of family planning methods and willingly selection of family planning methods as well as satisfaction with the related services or type of the method (Fig.3).
Fig. 3.
Main maternity health care incidences in CHCS and public health centers
School health program
Screening and periodic student health care programs had similar outcomes results in both groups. But in some instances such as referral rate for third grade students and rate of periodic health care visits for this sixth grade students was higher for CHCs compared to PHCs (P<0.05). No important difference was noticed in total performance of school health program between schools covered by CHCs and PHCs.
Health Education
The education process was studied as number of educational sessions and number of the persons being educated and people’s general knowledge on public health matters such as using iodized salt and washing methods of vegetables. Comparing the means showed a better education process being implemented in CHCs compared to PHCs, but the difference was not statistically significant.
Environmental Health
In some areas the two groups of health centers were compared, such as supervisory visits to food premises and schools, that no difference was observed. Nevertheless, the supervisory visits to public premises had a higher rate for CHCs (P=0.02). There was a particular timing plan in CHCs for collecting garbage from the houses, but population based positive function was not significantly different for the population covered by CHCs compared to population covered by PHCs.
The cooperative health centers had held more meetings with different governmental sectors for coordinating environmental health issues than had the PHCs done (P< 0.01).
Cost of services
The mean final cost for each service (global cost of any type) provided by PHCs was 6748 Rials Official exchange rates are provided by the Central Bank of Iran, available at: http://www.cbi.ir/exrates/rates_en.aspx per unit of care per-capita compared to 5674 Rials for CHCs.
Official exchange rates are provided by the Central Bank of Iran, available at: http://www.cbi.ir/exrates/rates_en.aspx
Mean annual cost per-capita of the covered population by PHCs was 14279 Rials and it was 12784 Rials for CHCs.
Management
To facilitate the interpretation, results of study in management group will be discussed under four aspects as follows:
1-Personnel
Results indicated that attitudes of personnel towards management in CHCs were more positive than PHCs. Higher positive attitude was observed in following aspects: computer skills (P<0.05), personnel welfare programs(P< 0.01), annual plan available (P<0.01), welcoming attitude toward customers (P= 0.08), team work (P<0.05), personal abilities (P<0.05), professional empowerment of personnel (P< 0.01) taking advantage of customer viewpoints in decision making (P < 0.01), timely providing consumer goods (P < 0.01), timely providing equipments (P < 0.01).
Results showed that in CHCs there was better situation of honor for job (P < 0.01), feeling of job ownership (P < 0.01) and satisfaction with occupational relationships. Cooperatives were more successful in motivating their personnel with respect to limitations of governmental structures especially in the field of personnel payments.
2- Participation
As it was mentioned before, CHCs had a better performance in holding meetings on environmental health with other sectors compared to PHCs (P <0.01).
Eighty percent of the population covered by PHCs and 79% of the population covered by CHCs knew the health center responsible for their area. No statistically significant difference was observed.
Considering knowledge about the health-volunteers, 66% of people knew health-volunteers and had received some kind of education by them. No difference was found between the two groups.
3- Client (Customer) Satisfaction
Our study showed higher customer satisfaction rates for cooperative health centers than public health centers in following fields:
Cleanliness of health center (P <0.05)
Friendly attitude of personnel (P < 0.01)
Receiving sufficient and suitable education (P < 0.01)
Dedicating sufficient time for each service (P <0.001)
Timely availability of services (P < 0.01)
Acceptable waiting time for receiving services (P < 0.01)
Security of the place of receiving services (P < 0.01)
Perfect equipments (P < 0.01)
Overall satisfaction with services (P < 0.01).
In summary, mean Likert score for Client satisfaction was 4.14 ± 0.6 (mean ±SD) in CHCs and it was 3.9 ± 0.63 (mean ±SD) in PHCs. The difference for mean satisfaction score was statistically significant (P < 0.01).
It seems that health cooperatives can be a suitable solution for community dissatisfaction with governmental services in health sector. Another approval field for CHCs compared to public health centers was the higher rate of repeating to use services and recommending others to receive services from the same health centers. Differences were also statistically significant (P <0.05 for repeating to use the services& P < 0.01 for recommending others to use the service).
4- Others
It was shown that CHCs were more precise in data reporting compared with PHCs (P < 0.01).
There was no difference in number of personnel between two groups and the number of health care staff per 10000 population covered was nearly equal in two groups.
We found a significant difference in usable equipment between two groups (P< 0.01), and equipment usage management in CHCs was much better than PHCs.
Discussion
When the market fails to distribute health benefits to people who need them—especially to poor people in developing countries—partnerships between public and private organizations are often seen as offering an innovative method with a good chance of producing the desired outcomes [10]. It is broadly recognized that government’s key role is to make policy, regulate and provide stewardship [11].
Our study compared quality of preventive health services delivered by public and cooperative health centers as well as client satisfaction in both groups. This study showed that contract transferring of available PHCs to nongovernmental organizations can be a possible alternative. In case of our study, small size health cooperatives were engaged through public – private partnership and we found that health centers run by these cooperative can act at least as well as public health centers in achieving main quality indices in field of preventive health care services. The lower willingness of private sector versus public health clinics in delivering preventive care services is reported in a Chinese experience of transferring health clinics to private sector. However, some individual quality indicators including educational base of the health workers and capital input of the clinics were not different with respect to the ownership status [12].
Contrary to lower willingness of private sector for providing preventive health care services in china, in our study the main health services delivered by CHCs were preventive health cares. Besides distinguished public-private partnership advantages, this may also be due to the fact that there is not much of a need for larger financial resources to establish a health cooperative and run a cooperative health center. In case a cooperative health center is established instead of a previously available public health center, they can hire required building and even major equipments from the public sector. If they want to establish a new health center based on Act of Cooperatives in Iran they have other sources for financial support such as resources provided by ministry of cooperatives and subsidized bank loans.
Private sector is thought to be active and effective in delivering secondary and tertiary health services in Iran and many other countries. And in some countries it has been shown to be active in delivering preventive health services either. For example in USA 57% of childhood vaccinations were done by private sector and in a study in Dhaka 62% of all vaccinations were provided by private sector. A large percentage of immunization services are reported to be given by public facilities [13-15].
The practice of engaging private sector in order to provide better child health care is experienced by many countries. Bustreo suggests that systematic examination of the strategies in employing the private sector in an effective way is vital to improve the impact of child health programs in low and middle income countries [16].
Contracting is an effective way for private sector participation which along with quality assurance plans, can lead to quality improvement in health services and increased client satisfaction. This is a strategy used by many public organizations in developed countries [17].
In our study many of the features of child health service indices in CHCs were better and, at least in some fields, similar to PHCs. In a review of the last 20 years of experience in child health programs, Claeson & Waldman questioned the traditional focus of child health programs on public sector health service delivery alone, and called for an approach that focuses on people and households, in addition to providers and single-disease programs. Although international institutions and governments in developing countries have concentrated on working with and through the public sector, an increasing amount of data highlights the private sector's critical influence on child health in developing countries, including the health of poor children. A growing body of knowledge is forming on efficacy of engaging private sector to improve child health outcomes in countries with low income [16].
Client satisfaction as stated by WHO is one of the most important factors in evaluating health service delivery programs [1]. Our study showed both a higher customer satisfaction and staff satisfaction rates for CHCs than PHCs in many fields. In a study in Sheffield, assessing the role of general practitioner cooperatives, it was shown that although GPs had a higher satisfaction, a higher customer satisfaction was not gained [18]. Another study in UK by Glynn has shown that family doctor cooperatives had led to increased patient satisfaction providing out of hours care [19]. However it should also be considered that the health cooperatives in Iran are quite different from those mentioned above.
Maternal health care indices in our study were also better in CHCs nearly in all areas indicating that they perform better than PHCs. Contrary to other preventive health care services, maternal health care is widely provided in private clinics in Iran but the difference is that services delivered in PHCs are free of charge and focused on essential health cares aimed to increase equity of receiving these services. When Cooperatives are entered in this area, it seems that many problems with PHCs like low availability, lower quality and lower client satisfaction can be cleared while preserving the advantages of public service delivery. In an Indian study by Howard, it was shown that with the exception of measles vaccination, predicted probabilities of the receipt of vaccinations and prenatal care do not differ based on the type of provider at which children and women sought curative care(20). A basic requirement for establishing a CHC is providing different skills needed for an integrated health care delivery. Perrot states that production of health services by different providers with a different range of skills will not be achievable except when a systematic coordination exists [21].
In all other areas of health service delivery we found that CHCs had better health service delivery indicators and/or at least similar indicators compared to PHCs. The only exception for this rule was environmental health supervisory visits that CHCs didn’t show to be as effective as PHCs. We consider this to be due to legal limitations.
Overall, the Health Cooperatives experience in our study has some features and advantages as follows:
It is a public private partnership model through contracting
A partial government withdrawal from direct service provision frees up not only some staff resources directly engaged in service delivery but also decreases the logistic problems tolerated by district health center responsible for supporting peripheral health centers.
A mobilization of resources takes place.
Supervision and information management gets easier
Switching from a time oriented payment system into an output oriented payment can decrease the waste of resources.
Contrary to many European health cooperatives, in Iran's experience a considerable variety of health personnel with different types of skills work together not just physicians or nurses.
In our experience the health services transferred to Cooperatives is focused mostly on preventive health care.
Although some preventive health services like vaccination are being accomplished by private sector in many countries, but in Iran's experience health services delivered to cooperatives are to be provided in an integrated form and each cooperative is responsible for providing all given preventive health needs of a family covered by that cooperative such as family planning, planned child cares, maternal cares, health education, vaccination and so on.
As each Health Cooperative is responsible for providing health services to a given local population based on a contract and is responsible for preventive health needs of that population, this can be considered a form of decentralization.
Cooperatives can solely be asked to contract health service delivery of predetermined populations which enables the government for prioritizing.
The subsidizing and payment system in our experience is different from a fixed subsidization and per capita payment in that amount of payment can differ depending on quality of services as evaluated periodically by provincial health department. Management process inside each cooperative can be quite effective because of two reasons: first that Health Cooperatives are not large scaled and have small number of personnel, and second that all of the personnel in a Health Cooperative are responsible for their practice that directly affects their income by improving the quality of their service.
Limitations and strengths of the study
As the CHCs were pre-established and researchers had no option in allocating areas, no random assignment was possible to be conducted and study has the common limitations of observational studies like many other healthcare investigations. However, as matching controls were chosen for them to decrease the amount of possible systematic error and effect of a major cofounder, we assume the results of the study reasonably robust. Another limitation of the study was the unavailability of trends for this design which demands the repetition of the study or best to use a longitudinal design. However considering the exceptional specificities of this experience and the fact that these CHCs were the first established CHCs in Iran, the findings of the study seem to be of appropriate value for the researchers and healthcare policy makers. Another point of strength in this study was that given the consistent outcomes, the vast range of effect measurements improves the validity of results.
Conclusion
Cooperatives sector may perform not only as well as public sector in meeting the standards of the different health care programs but also functions better in some areas. This can be assumed as an achievement for the policy of transferring the health services to CHCs along with ongoing governmental supervision to be a successful public-private partnership model. But the design limitations should alert the reader to be cautious in interpreting the findings. We believe research needs to be continued in this setting.
Acknowledgments
We are grateful to WHO Eastern Mediterranean Region Office, especially to Dr. Mobasher, then WHO representative in Iran for financial and scientific support. We also thank Iranian National Management and Planning Organization and Ministry of Cooperatives for their collaboration. The authors declare that there is no conflict of interests.
References
- [1]. World Health Organization, The world health report 2000, Health systems: improving performance. Geneva: WHO; 2000. available at: http://www.who.int/whr/2000/en/whr00_en.pdf
- [2].Frenk J. The public-private mix and human resources for health. Health Policy Plann. 1993;8(4):315–26. doi: 10.1093/heapol/8.4.315. [DOI] [PubMed] [Google Scholar]
- [3].Jeong HS, Gunji A. The influence of system factors upon the macro-economic efficiency of health care: implications for the health policies of developing and developed countries. Health Policy. 1994;27:113–40. doi: 10.1016/0168-8510(94)90076-0. [DOI] [PubMed] [Google Scholar]
- [4].Flood CM, Stabile M, Tuohy CH. The borders of solidarity: how countries determine the public/private mix in spending and the impact on health care. Health Matrix. 2003;12:297–356. [PubMed] [Google Scholar]
- [5].Field JE, Peck E. Public-private partnerships in healthcare: the managers’ perspective. Health Soc Care Comm. 2003;11(6):494–501. doi: 10.1046/j.1365-2524.2003.00455.x. [DOI] [PubMed] [Google Scholar]
- [6].Hunter DJ, Robinson R. The changing public-private mix in health care. Brit J Health Care Manage. 2002;8(8):301–4. [Google Scholar]
- [7].Matteo LD. The determinants of the public-private mix in Canadian health care expenditures: 1975-1996. Health Policy. 2000;52(2):87–112. doi: 10.1016/s0168-8510(00)00071-3. [DOI] [PubMed] [Google Scholar]
- [8].Purohit B. Private initiatives and policy options: recent health system experience in India. Health Policy and Plann. 2001;16(1):87–97. doi: 10.1093/heapol/16.1.87. [DOI] [PubMed] [Google Scholar]
- [9].Hyoung-Sun J. Health care reform and change in Public-private mix of financing: a Korean case. Health Policy. 2005;74(2):133–145. doi: 10.1016/j.healthpol.2004.12.017. [DOI] [PubMed] [Google Scholar]
- [10]. Reich MR (2002). Public-Private partnerships for public health. Cambridge: Harvard Center for Population and Development Studies, Harvard University Press. available: http://www.hsph.harvard.edu/faculty/michael-reich/files/Partnerships_book.PDF
- [11]. Preker AS, Harding A. The economics of public and private roles in health care: insights from Institutional Economics and Organizational Theory. HNP discussion paper. The World Bank, Washington, USA; 2000. Available at: http://siteresources.worldbank.org/DEC/Resources/847971251813753820/64157391251814028691/preker_harding.pdf
- [12].Meng Q, Liu X, Shi J. Comparing the services and quality of private and public health clinics in rural china. Health Policy Plann. 2000;15(4):349–356. doi: 10.1093/heapol/15.4.349. [DOI] [PubMed] [Google Scholar]
- [13].Khan MM, Khan SH, Walker D, Fox-Rushby J, Cutts F, Akr-amuzzaman SM. Cost of delivering child immunization services in urban Bangladesh: a study based on facility-level surveys. JHPN. 2004;22(4):404–12. [PubMed] [Google Scholar]
- [14].LeBaron CW, Lyons B, Massoudi M, Stevenson J. Childhood vaccination providers in the United States. Am J Public Health. 2002;92(2):266–70. doi: 10.2105/ajph.92.2.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15]. Peters DH, Yazbeck AS, Sharma RR, Ramana GNV, Pritchett LH, Wagstaff A. Better health systems for India’s poor: findings, analysis and options. The World Bank, Washington, USA; 2002. available at: http://books.google.com/books?id=vX8VS0YTAE8C&printsec=frontcover&source=gbs_ge_summary_r&cad=0#v=onepage&q&f=false
- [16].Bustreo F, Harding A, Axelsson H. Can developing countries achieve adequate improvements in child health outcomes without engaging the private sector? Bull World Health Organ. 2003; 81(12):886–95. [PMC free article] [PubMed] [Google Scholar]
- [17].McPake B, Ngalande B, Anda E. Contracting out of health services in developing countries. Health Policy Plann. 1994;9(1):25–30. doi: 10.1093/heapol/9.1.25. [DOI] [PubMed] [Google Scholar]
- [18].Pickin DM, O'Cathain A, Fall M, Morgan AB, Howe A, Nicholl JP. The impact of a general practice co-operative on accident and emergency services, patient satisfaction and GP satisfaction. Fam Pract. 2004;21(2):180–2. doi: 10.1093/fampra/cmh213. [DOI] [PubMed] [Google Scholar]
- [19].Glynn LG, Byrne M, Murphy AW. Effect of rurality on patients’ satisfaction with out of hours care provided by a family doctor cooperative. Rural and Remote Health. 2004;4:320. [PubMed] [Google Scholar]
- [20].Howard DH, Roy K. Private care and public health: do vaccination and prenatal care rates differ between users of private versus public sector care in India? Health Serv Res. 2004;39(6 Pt 2):2013–26. doi: 10.1111/j.1475-6773.2004.00330.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21]. Perrot J, Carrin G, Sergent F. The contractual approach: new partnerships for health in developing countries, Geneva: WHO; 1997. Technical paper (Doc. WHO/ICO/MESD. 24, unpublished).