Abstract
Background: Type 2 diabetes mellitus (T2DM) is a major public health problem worldwide. Hypertension and inflammation are well recognized as risk factors for the macrovascular complications of diabetes. The aim of this study was to assess the impact of vitamin E supplementation on blood pressure (BP), serum high-sensitivity C-reactive protein (hs-CRP) and fasting blood glucose in patients with T2DM.
Methods: In a double blind, randomized, controlled clinical trial, 83 patients with T2DM were divided randomly into two groups of vitamin E (400 mg/d, n=42) and placebo (n=41). All patients received the pearls for 8 weeks. Baseline and eighth week BP, serum hs-CRP, fasting blood glucose, anthropometric and dietary intake data were obtained from each patient. Data were analyzed using SPSS version 11.5.
Results: Vitamin E supplementation significantly increased serum levels of vitamin E (P < 0.001) and decreased mean arterial pressure and fasting blood glucose (P = 0.047, P = 0.028, respectively) in vitamin E group as compared with placebo group. A significant decrease in systolic blood pressure and diastolic blood pressure was observed in the vitamin E group comparing with baseline values (all P < 0.01). There were no significant changes in serum hs-CRP in both of the studied groups.
Conclusion: Vitamin E had beneficial effects on serum vitamin E, BP and blood glucose in patients with T2DM. Improvement in BP and glucose control may contribute to reducing complications of diabetes including cardiovascular risk in these patients.
Keywords: Vitamin E, Blood pressure, Inflammation, Type 2 diabetes
Introduction
Type 2 diabetes mellitus (T2DM) and cardiovascular disease (CVD), as non-communicable diseases, are the main public health challenge for the 21st century [1]. T2DM or non-insulin-dependent diabetes mellitus is a chronic disease characterized by hyperglycemia and insulin resistance [2]. The prevalence of type 2 diabetes is increasing at an alarming rate. The number of people with diabetes worldwide is expected to rise to well over 366 million by 2030 [3]. Changes in human behavior and lifestyle such as nutritional habits over the last century have resulted in a dramatic increase in the incidence of diabetes worldwide [1].
Patients with type 2 diabetes have a significantly higher risk of developing coronary heart disease and atherosclerosis. Possible reasons for accelerated atherosclerosis in these patients are oxidative stress, hypertension, and increased subclinical systemic inflammation [4-6]. Abnormally high levels of free radicals due to an over production or inadequate removal and simultaneous decline in antioxidant defense mechanism can damage cellular proteins, nucleic acids and membrane lipids [7]. It is noteworthy that hyperglycemia induces reactive oxygen species (ROS) generation [8]. The levels of ROS are controlled by various cellular defense mechanisms [9]. Vitamin E (α-tocopherol), the well-known scavenger of free radicals, facilitates the reduction in ROS production and increases the antioxidant defense system [10]. Vitamin E is a lipid-soluble antioxidant found in virtually all cell membranes. This vitamin neutralizes free radicals, preventing the chain reaction that contributes to oxidative damage [11].
There has been an increasing interest in the involvement of low-grade inflammation (high-sensitivity C-reactive protein [hs-CRP]) in the pathogenesis of type 2 diabetes. Hs-CRP is an inflammatory marker with proinflammatory and proatherogenic properties, produced and released by the liver under the stimulation of cytokines [12,13]. Higher levels of hs-CRP in diabetic patients were showed in the previous studies [14,15]. Elevated hs-CRP levels may predict CVD as well as the development of diabetes mellitus [16].
Several studies have reported that serum vitamin E is lower in type 2 diabetic patients compared to healthy people [2,17-19]. It is postulated that vitamin E has beneficial effects on metabolic control of diabetes and delays the long-term complications of diabetes including CVD [10,20].
Low dietary intakes and plasma concentrations of antioxidants are associated with enhanced risk of hypertension [6]. However, the results of clinical studies on the effects of vitamin E supplementation on blood pressure (BP) are inconclusive [21-24].
Since we did not find any published data about the effect of sole vitamin E supplementation on BP in type 2 diabetic patients and the scanty and conflicting data about the impact of vitamin E on inflammation in these patients, we aimed to evaluate the effects of oral vitamin E supplementation on BP, serum hs-CRP and fasting blood glucose in type 2 diabetic patients.
Materials and Methods
This double-blinded, randomized, controlled clinical trial was approved by the Ethics Committee of Tabriz University of Medical Sciences and was registered on the Iranian Registry of Clinical Trials website (available at: http:// www.irct.ir, identifier: IRCT138904263664N2). Written informed consent was obtained from all studied subjects.
Eighty-four type 2 diabetic patients aged 30 to 60 years with a body mass index (BMI) lower than 35 kg/m2 were recruited for this study from the Endocrinology Clinic, Sina Hospital in Tabriz, Iran. Diagnosis of T2DM was assessed at least 1 year prior to our examination. Exclusion criteria included insulin treatment, smoking, nutritional supplements intake or consumption during 3 months before the study, use of estrogen, progesterone, diuretics, β-blockers and non-steroidal anti-inflammatory drugs, presence of renal, liver, heart, thyroid and inflammatory disorders, and pregnancy or breast-feeding.
The patients were randomized into two groups matched for sex, age, and BMI. The vitamin E group (n = 42) received 400 IU/day of vitamin E (400 mg of dl- α-tocopheryl acetate) and the control group (n = 42) received placebo for 8 weeks. Both vitamin E and placebo pearls were supplied by Zahravi Pharmacutical Company, Tehran, Iran. The vitamin E supplement and placebo had an identical appearance. The participants were asked to continue their routine dietary intake and lifestyle and to avoid any changes in medication, if possible.
Information on anthropometric measurements and dietary intakes, were collected by trained personnel at the beginning and end of the trial. Weight and height were measured to the nearest 0.5 kg and 0.1 cm, respectively. BMI was calculated by dividing body weight (kilograms) by height squared (meters). Dietary intakes during 3 days (including 2-week days and 1 weekend) were estimated using a 24-h dietary recall and analyzed by Nutritionist 4 software.
The systolic and diastolic blood pressure (SBP and DBP) (5 minutes seated rest, mean of two readings) were measured with a mercury sphygmomanometer at baseline and after 8 weeks of supplementation. Mean arterial pressure (MAP) was calculated using following formula: (SBP+2DBP)/3 [6].
Blood Ssampling
Venous blood samples (10 ml) were obtained from patients at the beginning and at the end of the trial. Samples were taken after 12 h fasting period and before taking any oral hypoglycemic agents (OHAs). Serum was separated from whole blood by centrifugation. Fasting blood glucose assay was conducted on the same day, which samples were collected and other serum aliquots were frozen immediately at -70˚C until the assay.
Biochemical Assays
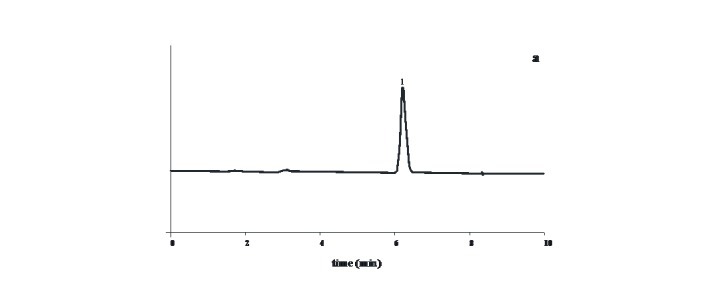
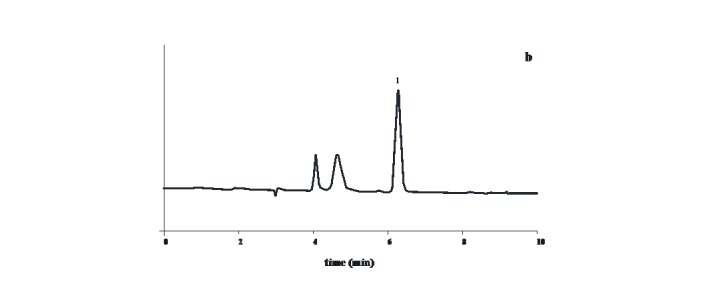
Serum concentrations of α-tocopherol were determined by high-performance liquid chromatography (HPLC) with UV detection (CE1200, High performance variable wavelength monitor) according to the method of Karpinska et al. [25]. Briefly, plasma proteins were precipitated with methanol and lipids extracted with n-hexane. After evaporation, dry residue was dissolved with mobile phase (methanol) and mixed and then this solution was injected into a guard-column (ACE 3μm C18 column (4.6×100 mm): ACE-111-1046). Samples were run at a flow rate of 1.0 ml/min on a HPLC system (Cecil 1100 series, Cambridge, England). Absorption was monitored at 292 nm for α-tocopherol. Concentrations were calculated from areas under the curve using an external calibration curve.
Fig. 1: (a) Chromatogram of α-tocopherol standard at 292 nm;
(b) chromatogram of serum at 292 nm. Peak 1: α-tocopherol
a.
b.
Serum hs-CRP level was determined using the immunoturbidometric method with a Parsazmun kit (Karaj, Iran).
Fasting blood glucose was measured using the standard enzymatic methods by Parsazmun kit (Karaj, Iran) by an autoanalyzer (Abbott Model Alcyon 300, USA).
Statistical Aanalysis
Data were analyzed using SPSS version 11.5. The normal distribution of variables was tested and confirmed by Kolmogorov-Smirnov test. For the hs-CRP and SBP that did not follow normal distribution, analyses were performed after log transformation. The background characteristics and dietary intakes of patients in the two groups were compared using independent samples t-test and chi-square test for quantitative and qualitative variables, respectively. Differences between the two groups after the intervention were determined by analysis of covariance, adjusting for baseline measurements and potential confounders (duration of diabetes and dietary vitamin E intake). The changes in biochemical and anthropometric measurements and dietary intakes of the patients between the beginning and the end of the trial were compared by paired-samples t test in each group. Results with P < 0.05 were considered as statistically significant.
Results
One patient was excluded from the statistical analysis because he changed his medication during the trial. Baseline and anthropometric characteristics and dietary vitamin E intakes of the patients in the study groups are shown in Table 1. The initial characteristics were similar in the vitamin E and placebo groups (P > 0.05). There were no significant changes in BMI and dietary vitamin E intake during the study period (data not shown). Results of 24-h dietary recall showed no significant differences in the intakes of energy and macronutrients between the two groups at baseline and during the trial period (data not shown).
Table 1. Baseline characteristics of the studied subjects.
| Variables | Placebo group (n=41) | Vitamin E group (n=42) |
| Age (yr) | 35.49 ± 8.02 | 35.10 ± 6.93 |
| Male/female (n) | 14/27 | 15/27 |
| Weight (kg) | 74.94 ± 9.53 | 74.76 ± 11.35 |
| BMI (kg/m2) | 29.88 ± 3.63 | 28.54 ± 3.57 |
| Duration of diabetes (years) | 6.76 ± 5.77 | 6.28 ± 5.19 |
| Duration of OHAs treatment (years) | 5.57 ± 5.05 | 4.32 ± 4.20 |
| Dietary vitamin E intake (mg/d) | 4.74 ± 2.78 | 4.76 ± 2.52 |
BMI: body mass index; OHAs: oral hypoglycemic agents
The results are expressed as the mean ± SD
There were no significant differences between groups by independent samples t-test or χ2-test (all P > 0.05).
At the beginning of the study, the groups were similar based upon serum levels of vitamin E, SBP, DBP, MAP, hs-CRP and blood glucose (Table 2). After 8 weeks of supplementation, serum levels of vitamin E increased significantly (P < 0.001) and MAP and fasting blood glucose decreased significantly (P = 0.047, P = 0.047, respectively) in vitamin E group compared with placebo group. Following intervention, SBP, DBP and MAP decreased significantly in vitamin E group comparing to baseline values (all P < 0.01). We did not find any significant changes in serum hs-CRP in both of the studied groups (P > 0.05).
Table 2. Mean ± SEM of vitamin E, SBP, DBP, MAP, hs-CRP and glucose in type 2 diabetic patients at baseline and the eighth week of study.
| Variables | Placebo group (n=41) | Vitamin E group (n=42) | |||||
| Baseline | After intervention | P ‡ | Baseline | After intervention | P ‡ | ||
| Serum vitamin E (mg/L)* | 3.14 ± 0.10 | 3.11 ± 0.13 | NS | 3.11 ± 0.13 | 6.30 ± 0.26 | <0.001 | |
| SBP (mmHg) | 134.38 ± 3.01 | 132.88 ± 3.32 | NS | 137.25 ± 5.02 | 127.38 ± 3.47 | <0.01 | |
| DBP (mmHg) | 81.38 ± 1.33 | 78.88 ± 1.64 | NS | 83.25 ± 2.28 | 75.88 ± 2.09 | <0.01 | |
| MAP (mmHg) † | 99.04 ± 1.77 | 96.88 ± 1.98 | NS | 101.25 ± 3.10 | 93.04 ± 2.37 | <0.01 | |
| Serum hs-CRP (mg/L) | 1.43 ± 0.19 | 1.50 ± 0.20 | NS | 1.24 ± 0.14 | 1.21 ± 0.15 | NS | |
| Blood glucose (mg/dL) † | 120.18 ± 4.93 | 124.70 ± 4.61 | NS | 128.13 ± 5.33 | 119.03 ± 3.47 | <0.05 | |
SBP: systolic blood pressure; DBP: diastolic blood pressure; MAP: Mean arterial pressure; hs-CRP: high-sensitivity C-reactive protein; NS: Non-significant.
* Significant differences between groups after intervention using analysis of covariance (adjusted for duration of diabetes, vitamin E intake, and baseline values): P < 0.001
† Significant differences between groups after intervention using analysis of covariance (adjusted for duration of diabetes, vitamin E intake, and baseline values): P < 0.05
‡ using paired samples t-test
Discussion
This study (Table 1) showed that daily dietary intake of vitamin E in all of participants was lower than dietary reference intakes (15 mg/day) [26]. At the beginning of the study (Table 2), subjects in both groups had vitamin E serum levels lower than the reference range (5.7-20 mg/L) [27]. After supplementation, significant increase in serum vitamin E level was observed in vitamin E group. Lower serum vitamin E levels were previously observed in type 2 diabetic patients [2,17-19].
Cardiovascular complications are the most common cause of high mortality rate in type 2 diabetes. Hypertension and inflammation are contributory factors that promote the development of complications [6,15]. The SHEP study (the Systolic Hypertension in the Elderly Program) has clearly shown twice the absolute risk reduction in cardiovascular events following tight BP control in type 2 diabetic subjects than in non-diabetics [28]. Data from the UKPDS (UK Prospective Diabetes Study Group) showed that BP control in a cohort of newly diagnosed subjects with type 2 diabetes was effective in reducing microvascular complications [29], and BP reduction would slow the progression of diabetic nephropathy [30].
Our data (Table 2), indicated that vitamin E significantly decreased MAP in the vitamin E group comparing with the control group and reduced SBP and DBP in this group in comparison to the baseline values. It had been shown that BP is sensitive to alteration of weight and dietary intakes [6], but these variables did not change in our studied groups. Therefore, the observed findings after intervention could not have been caused by the alterations in weight and dietary intakes. Several studies confirmed the results of the present study. Vitamin E in the long term can reduce BP in patients with mild hypertension [21]. Its supplementation can improve BP status in rats [24]. Enhancement of antioxidant status by supplementation with vitamins C and E in patients with essential hypertension is associated with decreased BP [31].
Several data indicate that intracellular magnesium may play a key role in modulating vascular tone and hypertension [32]. It is proposed that increased oxygen free radical production lowers the intracellular Mg concentration, and, in light of such evidence, vitamin E administration may regulate the intracellular Mg concentration [6]. In this way, vitamin E supplementation may increase intracellular magnesium and therefore decrease BP. Our findings confirm the anti-hypertensive properties of vitamin E. Therefore, vitamin E may have a potential beneficial effect regarding CVD.
CRP is a risk factor for CVD and it could contribute to atherosclerosis [33]. Vitamin E therapy, especially at high doses, has been shown to decrease release of pro-inflammatory cytokines (including interleukin-1beta, interleukin-6, and tumor necrosis factor-alpha), and inflammatory markers such as CRP, and to decrease adhesion of monocytes to endothelium [4,34]. High dose of vitamin E supplementation (1200 IU/day) significantly lowered the levels of hs-CRP in type 2 diabetic patients with high baseline levels of hs-CRP [15]. In the present study, 400 mg/day vitamin E did not have any effect on serum hs-CRP in type 2 diabetic patients (Table 2). Our findings are similar to the result obtained by Wu et al. in a trial with 500 mg/day α-tocopherol for 6 weeks on patients with T2DM [5].
CRP levels are categorized for risk as low (<1 mg/L); average (2 to 3 mg/L) and high (>3 mg/L) [35]. The baseline value of hs-CRP in all of our patients was lower than 2 mg/L. No significant change of serum hs-CRP by vitamin E in this study may be due to lower baseline levels of hs-CRP in our patients or insufficient dose of vitamin E supplement. Other studies are needed to evaluate the impact of vitamin E supplements on other inflammatory parameters in type 2 diabetic patients.
We observed that the serum level of fasting blood glucose was significantly reduced after vitamin E supplementation in the intervention group as compared with the placebo group (Table 2). This result is in agreement with some previous reports on type 2 diabetic patients [36,37]. Paolisso et al. reported an improvement in fasting blood glucose after 900 IU/day vitamin E supplementation during 3 months [36]. Similar result was observed after 800 IU/day supplementation of vitamin E for one month in these patients [37]. It is suggested that vitamin E can be effective in inhibiting hyperglycemia by scavenging ROS [10]. However, some studies did not show any changes in fasting blood glucose after intervention with vitamin E on patients with T2DM [17,20,38]. Part of this discrepancy can be due to differences in the duration of the intervention, studied subjects, or dose of vitamin E supplements.
Conclusion
This study demonstrated that vitamin E had beneficial effects on serum vitamin E, BP and blood glucose in type 2 diabetic patients. Improvement in BP and glucose control may contribute to reducing cardiovascular risk or complications of diabetes in these patients.
Acknowledgments
The authors thank the Research Vice-Chancellor and Nutritional Research Center of Tabriz University of Medical Sciences, Tabriz, Iran for the financial support; and patients who participated in the study. The authors declare that there is no conflict of interests.
References
- [1]. Zimmet P, Alberti K G and Shaw J. Global and societal implications of the diabetes epidemic. Nature 2001, 414, 782-7. [DOI] [PubMed]
- [2]. Merzouk S, Hichami A, Madani S, Merzouk H, Berrouiguet A Y, Prost J, et al. Antioxidant Status and Levels of Different Vitamins Determined by High Performance Liquid Chromatography in Diabetic Subjects with Multiple Complications. Gen Physiol Biophys 2003, 22, 15-27. [PubMed]
- [3]. Wild S, Roglic G, Green A, Sicree R and King H. Global Prevalence of Diabetes, Estimates for the year 2000 and projections for 2030. Diabetes Care 2004, 27, 1047-53. [DOI] [PubMed]
- [4]. Jialal I, Devaraj S and Venugopal S. Oxidative stress, inflammation, and diabetic vasculopathies: the role of alpha tocopherol therapy. Free Radic Res 2002, 36, 1331-6. [DOI] [PubMed]
- [5]. Wu J H, Ward N C, Indrawan A P, Almmedia C A, Hodgson J M, Proudfoot J M, et al. Effects of α-Tocopherol and Mixed Tocopherol Supplementation on Markers of Oxidative Stress and Inflammation in Type 2 Diabetes. Clin Chem 2007, 53, 511-9. [DOI] [PubMed]
- [6]. Farvid M S, Jalali M, Siassi F, Saadat N and Hosseini M. The Impact of Vitamins and/or Mineral Supplementation on Blood Pressure in Type 2 Diabetes. J Am Coll Nutr 2004, 23, 272-9. [DOI] [PubMed]
- [7]. Hashim Z and Zarina S. Assessment of paraoxonase activity and lipid peroxidation levels in diabetic and senile subjects suffering from cataract. Clin Biochem 2007, 40, 705-9. [DOI] [PubMed]
- [8]. Lakshman M R, Gottipati C S, Narasimhan S J, Munoz J, Marmillot P and Nylen E S. Inverse correlation of serum paraoxonase and homocysteine thiolactonase activities and antioxidant capacity of high density lipoprotein with the severity of cardiovascular disease in persons with type 2 diabetes mellitus. Metabolism 2006, 55, 1201-6. [DOI] [PubMed]
- [9]. Aydin A, Orhan H, Sayal A, Ozata M, Sahin G and Isimer A. Oxidative stress and nitric oxide related parameters in type II diabetes mellitus: effects of glycemic control. Clin Biochem 2001, 34, 65-70. [DOI] [PubMed]
- [10]. Jain N, Naseem I and Ahmad J. Evaluation of DNA damage and metabolic syndrome parameters in diabetic rabbits supplemented with antioxidants. Fundam Clin Pharmacol 2009, 23, 197-205. [DOI] [PubMed]
- [11]. Aksoy N, Vural H, Sabuncu T, Arslan O and Aksoy S. Beneficial effects of vitamins C and E against oxidative stress in diabetic rats. Nutr Res 2005, 25, 625-30.
- [12]. Wang Z and Hoy W E. C-reactive protein and the risk of developing type 2 diabetes in Aboriginal Australians. Diab Rese and Clin Pract, in press. [DOI] [PubMed]
- [13]. Moldoveanu E, Tanaseanu C, Tanaseanu S, Kosaka T, Manea G, Marta D S, et al. Plasma markers of endothelial dysfunction in type 2 diabetics. Eur J Intern Med 2006, 17, 38-42. [DOI] [PubMed]
- [14]. Ford E S. Body mass index, diabetes, and C-reactive protein among U.S. adults. diabetes Care 1999, 22, 1971-7. [DOI] [PubMed]
- [15]. Devaraj S and Ishwarlal J. Alpha tocopherol supplementation decreases serum C-reactive protein and monocyte interleukin-6 levels in normal volunteers and type 2 diabetic patients. Free Radic Biol Med 2000, 29, 790-2. [DOI] [PubMed]
- [16]. Dullaart R P F, Vries R D, Sluiter W J and Voorbij H A M. High plasma C-reactive protein (CRP) is related to low paraoxonase-I (PON-I) activity independently of high leptin and low adiponectin in type 2 diabetes mellitus. Clin Endocrinol 2009, 70, 221-6. [DOI] [PubMed]
- [17]. Paolisso G, Amore A D, Giugliano D, Ceriello A and Varricchio M. Pharmacologic doses of vitamin E improve insulin action in healthy subjects and non-insulin-dependent diabetic patients. Am J Clin Nutr 1993, 57, 650-6. [DOI] [PubMed]
- [18]. Skrha J, Sindelka G, Kvasnicka J and Hilgertova J. Insulin action and fibrinolysis influenced by vitamin E in obese Type 2 diabetes mellitus. Diabetes Res Clin Pract 1999, 44, 27-33. [DOI] [PubMed]
- [19]. Ahmad M, Khan M A and Khan A S. Naturally occurring antioxidant vitamin levels in patients with type-II diabetes mellitus. J Ayub Med Coll Abbottabad 2003, 15, 54-7. [PubMed]
- [20]. Ble-Castillo J L, Carmona-Diaz E, Mendez J D, Laris-Medina F J, Medina-Santillan R, C;eva-Villanueva G, et al. Effect of a-tocopherol on the metabolic control and oxidative stress in female type 2 diabetics. Biomed Pharmacother 2005, 59, 290-5. [DOI] [PubMed]
- [21]. Boshtam M, Rafiei M, Sadeghi K and Sarraf-Zadeghan N. Vitamin E can reduce blood pressure in mild hypertensives. Int J Vitam Nutr Res 2002, 72, 309-14. [DOI] [PubMed]
- [22]. Palumbo G, Avanzini F, Alli C, Roncaqlioni M C, Ronchi E, Cristofari M, et al. Effects of vitamin E on clinic and ambulatory blood pressure in treated hypertensive patients. Am J Hypertentions 2000, 13, 564-7. [DOI] [PubMed]
- [23]. Aryaeian N, Shahram F, Djalali M, Eshragian M R, Djazayeri A, Sarrafnejad A, et al. Effect of conjugated linoleic acid, vitamin E and their combination on lipid profi les and blood pressure of Iranian adults with active rheumatoid arthritis. Vasc Health Risk Manag 2008, 4, 1423-32. [DOI] [PMC free article] [PubMed]
- [24]. Seifi B, Kadkhodaee M, Karimian S M, Zahmatkesh M, Shams S and Bakhshi E. Reduction of Kidney Damage by Supplementation of Vitamins C and E in Rats With Deoxycorticosterone-Salt- Induced Hypertension. Iran J Kidney Dis 2009, 3, 197-202. [PubMed]
- [25]. Karpinska J, Mikoluc B, Motkowski R and Piotrowska-Jastrzebska J. HPLC method for simultaneous determination of retinol, alpha-tocopherol and coenzyme Q10 in human plasma. J Pharm Biomed Anal 2006, 42, 232-6. [DOI] [PubMed]
- [26]. Gallagher M L. Intake: The nutrients and their metabolism. In: Mahan LK, Escott-Stump S, Raymond J, editors. Krause's Food and the Nutrition Care Process. 13th ed. USA: Saunders Company; 2012.
- [27]. Mahan L, Escott-Stump S and Raymond J. Krauseʼs Food and the Nutrition Care Process. 13th ed. Saunders Company. USA; 2012.
- [28]. Curb J D, Pressel S L, Cutler J A, Savaqe P J, Appleqate W B, Black H, et al. Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. Systolic Hypertension in the Elderly Program Cooperative Research Group. JAMA 1996, 276, 1886-92. [PubMed]
- [29]. Turner R, Holman R, Stratton I, Coll C, Frighi V, Manley S, et al. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ 1998, 317, 703-13. [PMC free article] [PubMed]
- [30]. Marks J B and Raskin P. Nephropathy and hypertension in diabetes. Med Clin North Am 1998, 82, 877-907. [DOI] [PubMed]
- [31]. Rodriqo R, Part H, Passalacqua W, Araya J and Bachler J P. Decrease in oxidative stress through sup-plementation of vitamins C and E is associated with a reduction in blood pressure in patients with essential hypertension. Clin Sci 2008, 114, 625-34. [DOI] [PubMed]
- [32]. Barbagallo M, Dominquez L J, Galioto A, Ferlisi A, Cani C, Malfa L, et al. Role of magnesium in insulin action, diabetes and cardio-metabolic syndrome X. Mol Aspects Med 2003, 24, 39-52. [DOI] [PubMed]
- [33]. Sinqh U, Devaraj S and Jialal I. Vitamin E, oxidative stress, and inflammation. Annu Rev Nutr 2005, 25, 151-74. [DOI] [PubMed]
- [34]. Sinqh U and Jialal I. Anti-inflammatory effects of alpha-tocopherol. Ann N Y Acad Sci 2004, 1031, 195-203. [DOI] [PubMed]
- [35]. Raymond J L and Couch S C. Medical Nutrition Therapy for Cardiovascular Disease. In: Mahan LK, Escott-Stump S, Raymond J, editors. Krauseʼs Food and the Nutrition Care Process. 13th ed. USA: Saunders Company; 2012.
- [36]. Paolisso G, Amore AD, Galzerano D, Balbi V, Giugliano D, Varricchio M, et al. Daily vitamin E supplements improve metabolic control but not insulin secretion in elderly type II diabetic patients. Diabetes Care 1993, 16, 1433-7. [DOI] [PubMed]
- [37]. Gokkusu C, Palanduz S, Ademoglu E and Tamer S. Oxidant and antioxidant systems in NIDDM patients: influence of vitamin E supplementation. Endocr Res 2001, 27, 377-86. [DOI] [PubMed]
- [38]. Gomez-Perez F J, Valles-Sanchez V E, Lopez-Alvarenga J C, Choza-Romero R, ibarra Pascuali J J, Gonzalez Orellana R, et al. Vitamin E modifies neither fructosamine nor HbA1c levels in poorly controlled diabetes. Rev Invest Clin 1996, 48, 421-4. [PubMed]


