Abstract
Background: The aim of this study was to suggest a suitable context to develop efficient hospital systems while maintaining the quality of care at minimum expenditures.
Methods: This research aimed to present a model of efficiency for selected public and private hospitals of East Azerbaijani Province of Iran by making use of Data Envelopment Analysis approach in order to recognize and suggest the best practice standards.
Results: Among the six inefficient hospitals, 2 (33%) had a technical efficiency score of less than 50% (both private), 2 (33%) between 51 and 74% (one private and one public) and the rest (2, 33%) between 75 and 99% (one private and one public).
Conclusion: In general, the public hospitals are relatively more efficient than private ones; it is recommended for inefficient hospitals to make use of the followings: transferring, selling, or renting idle/unused beds; transferring excess doctors and nurses to the efficient hospitals or other health centers; pensioning off, early retirement clinic officers, technicians/technologists, and other technical staff. The saving obtained from the above approaches could be used to improve remuneration for remaining staff and quality of health care services of hospitals, rural and urban health centers, support communities to start or sustain systematic risk and resource pooling and cost sharing mechanisms for protecting beneficiaries against unexpected health care costs, compensate the capital depreciation, increasing investments, and improve diseases prevention services and facilities in the provincial level.
Keywords: Data envelopment analysis, Efficiency, Hospital efficient management, Hospital
Introduction
An efficient health care system saves time, money, and human resources, and finally, excellently serves patients in a more timely fashion. There are various ways to improve efficiency such as eliminating unnecessary paperwork, building the innovative organization, and effective teams, improving organizational culture, and finally yet importantly, doing work with using optimum amount of resources and reforming the system. According to the WHO, “Since provision of health care services like production and provision of other goods and services follow the economic rules, thereby it is necessary and a must to use the scarce resources at its minimum to achieve the health care system’s objectives” [1].
The main questions in this paper are related to the following issues: (i) the extent of efficiency of the current public and private hospitals (mixed system); (ii) the highest and lowest efficiencies among public and private hospitals and determining bench-marks; (iii) reforms and ways to save money, time, and scarce resources that can improve inefficient hospitals’ efficiency and eventually the healthcare system. In this study we intended to investigate the efficiency of the use of the huge financial resources which are annually spent in the hospitals of the province and by analysis of various kinds of efficiency indicators, to be able to help the system to optimize the use of public and private resources so that the saved amounts might be used for the promotion of individuals’ life, health and their well-being. In order to make the importance of the issue clear, we looked at the funding of health care in East Azarbaijan (Fig. 1). On the basis of Iranian Budget Act in 2007-8, general budget of East Azerbaijan was 4.53 percent of the whole national budget (about PPP US$240 millions [2]) and credits of provincial health care sector was 21 percent of the provincial budget of which PPP US $130 million was exactly allocated to the health care programs (almost all to the public hospitals) and PPP US$0.5 million was devoted to the non-public health services plan (nearly all to the private sector, charities, or institutional health centers) [3].
Fig. 1.
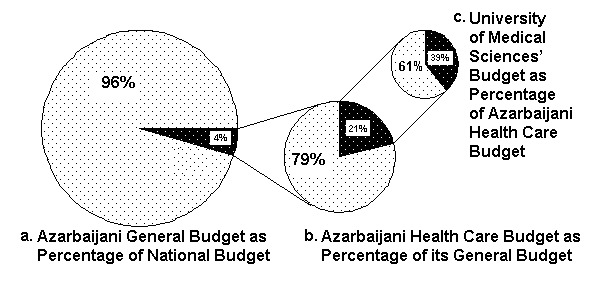
Azarbaijani Health Care Budget as Percentage of its General Budget
We should note that these amounts are usually increased with specific percentages annually depending on the incomes of the government–mostly oil incomes–and governmental monetary and fiscal policies.
a. Iranian Health Care System
According to the WHO’s report, Iran as a oil exporter and medium income country, the fourth country in Asia with 30 provinces, 885 cities, and nearly 68,000 villages has a 94 rank on the human development index among 177 countries and 69.5 years of life expectancy at birth. Recent remarkable progresses in health sector (PHC) such as establishing health networks have caused to improving various health indicators. However, in general, one of the most important problems is that about 8 to 10 percent of people do not have access to any insurance plans, and then they have to tolerate the out-of-pocket and catastrophic payments to reach the health care services [4]. In 2006, there were 773 treatment institutes (hospitals, maternities, home cares) and 116,474 beds in the whole country. In addition, the number of (public, private, and other) institutes with their relevant beds was 505 public institutes (65.3%) with 79,772 beds (68.5%); 128 private institutes (16.6%) with 12,594 beds (10.8%); and 140 other institutes (18.1%) with 24,108 beds (20.7%) respectively [5].
b. East Azerbaijani Health Care System
Based on the latest country’s divisions in 2004, East Azerbaijani Province consists of 19 townships, 42 districts, 57 towns, and 141 rural districts. Moreover, according to the general population and housing census in 1986, 1996, and 2006, Azerbaijani population with annually growth rate 0.85 percent has been increased from 3,077,882, to 3,325,540, and then to 3,603,456 people respectively and the life expectancy was 70.7 years in 2005. In addition, the population of the province was almost 5.1 percent of the whole country’s population [6].
In 2006, there were 38 treatment institutes (4.9 percent of the whole country) which their ownership status were as follows: 29 public (76.3%), 5 private (13.2%), and 4 other institutes (10.5%). Also, in 2006, there were 5,964 active beds (5.1 percent of the active beds in the whole country) which their ownership situation were as follows: 4,867 public (81.6%), 537 privates (9%), and 560 beds others (9.4%) including treatment institutes affiliation to Social Security Organization, Charities affaires, Banks, and etc.). Moreover, 25 out of 42 hospitals (about 60%) and the rest (17 out of 42, almost 40%) have been located in Tabriz and other townships respectively [7].
c. Literature Review
This section does not intend to do a comprehensive review of the health-related Data Envelopment Analysis (DEA) literature. Rather, it plans to provide brief information about just a limited number of usages of this effective and developing method in the efficiency evaluation and various aspects of the health systems. The DEA has been extensively used in the various sectors of the developed countries’ economies to estimating the degree of the efficiency and planning the health care systems. Furthermore, the powerful DEA approach method has been gradually used in the developing and even some poor countries in Africa. Ersoy et al. [8] analyzed technical efficiencies of Turkish hospitals using the DEA method. Majumdar [9] applied DEA to measure relative efficiency points within the Indian pharmaceutical sector. Chang [10] applied DEA to determine technical efficiency of six class one public hospitals in Taiwan for five years. Using a variable return to scale (VRS) for DEA model, Wan et al. [11] investigated the technical efficiency among 57 nursing units, in a third level care medical centre in Taiwan (Republic of China). In Africa, some studies intended to apply DEA in the health industry. Kirigia et al. [12] employed DEA to assess the technical and scale efficiency, and productivity change over a four-year period among 17 public health centers in Seychelles. Kirigia et al. [13] used DEA to find out what portion of 55 public hospitals of Kwazulu–Natal Province of South Africa were operating efficiently, and for those inefficient hospitals, what inputs and outputs contribute most to inefficiency. Kirigia et al. [14] applied DEA to estimate the technical efficiencies among 155 primary health care clinics in Kwazulu–Natal Province of South Africa. Eyob [15] estimated the technical efficiency among 86 public hospitals in Eastern, Northern, and Western Cape Provinces of South Africa. In Zambia, Felix Masiye et al. [16] estimated technical, allocative, and economic (cost) efficiencies for 40 private and public health centers. This study figured out that private centers had been run more efficient than public ones. In other study on 18 public hospitals, 8 charity hospitals (affiliated with the church), and 4 private hospitals (overall 30 hospitals) Masiye [17] estimated technical efficiency. Kirigia et al. [18] assessed technical efficiencies of 32 public health centers and 54 district level public hospitals in Kenya. In Ghana, Daniel Osey et al. [19] analyzed technical and scale efficiencies of 17 district hospitals and 17 health centers. In Iran, there has been no similar study but some researches in different subjects [20-23].
The aim of this study was to suggest a suitable context to develop efficient hospital systems while maintaining the quality of care at minimum expenditures. To the best of our knowledge, the present study is the first in its own kind in Iran.
Materials and Methods
a. Methodology
The present study tries to prepare the ground for optimizing interferences by presenting a given economic model, i.e., obtaining Pareto optimal in the management of the province and whole country’s hospitals through concept of cost-minimization, efficiencies, and DEA approach.
Sample Size and Sampling: Hospitals’ Efficiency
In the present research, data and information obtained from the third level hospital were used. In general, there are 42 first, second, and third level (rank) hospitals in the East Azerbaijan Province as follows: 25 out of 42 hospitals have been located in Tabriz (nearly 60 percent) and the rest (about 40 percent) in other districts in the province. Thirty-three hospitals out of 42 public ones (79% = 5% army forces [Sepah and Artesh] + 5% Social Security Organization [Alinasab and 29 Bahman hospitals] + 69% [29 hospitals] are affiliated with Tabriz University of Medical Sciences). In addition, 6 hospitals out of 42 private hospitals (14%), are affiliated with the following organizations : 1 hospital out of 42, Zakaria nonprofit hospital (2%, affiliated with Tabriz Azad University), 1 hospital out of 42, Tabriz Amir-al-momenin Charity hospital (2%, general and urology), and finally 1 hospital out of 42, Fajr hospital (2% affiliated with Janbazan Affairs Organization).
It was finally decided that 11 sample hospitals (6 samples from the first class public hospitals and 5 samples from the private ones) to be selected (26 percent of the whole provincial hospitals).
The first class public hospitals, which were selected, include Hospital 1: Imam, Hospital 2: Nikokari, Hospital 3: Alzahra, Hospital 4: Sina, Hospital 5: Kodakan (all located in Tabriz) and Hospital 6: Amir-al-momenin, which is the only first class hospital (from point of view of both the general and ward evaluations) outside of Tabriz (located in Maragheh). Since all of the province’s private hospitals have been located in Tabriz, thus all five private sample hospitals were selected from Tabriz.
There are just 6 private hospitals named Shams, Bahbod, Shahryar (Azar), Nor Nejat, Shafa, and Mehr (ophthalmic hospital). And only one (Shams) out of these 6 hospitals has been recognized as class one hospital and the rest just class two by the evaluation of health authorities/provincial vice chancellorship of treatment. In the meanwhile, except Mehr hospital, which was an ophthalmology hospital, the rest run as general ones? As a result, 5 sample of private hospitals out of 6, the total provincial private hospitals are as follows: Hospital 7: Shams, Hospital 8: Behbod, Hospital 9: Shahryar, Hospital 10: Nor Nejat, Hospital 11: Shafa (all general, almost 83% of total private hospitals). In other words, Mehr (ophthalmology) private hospital is the only one, which was not investigated. Finally, it was mentioned and highlighted that 7 out of 11 selected hospitals (6 public hospitals and one private one) have been chosen among the class one and important provincial hospitals. Thereby, in general, 10 hospitals out of 25, the total number of Tabriz hospitals (40%) have been selected as the samples.
If “number of active bed” is taken into account as a measure of “size of hospital” and we look at the samples from this point of view, 1,759 out of 5,964 total numbers of the provincial active beds (29.49%) belong to the selected hospitals.
Data Collection and Tools
Data of this investigation were collected by various tools such as checklist, interview, documental profiles review including the regulation booklet of the ministry of health, booklets, professional magazines, annual reports of creditable domestic and international organizations such as the WHO and UNDP, internet sources, websites affiliated with Tabriz Medical or other universities, research centers and national or foreign medical statistical data institutes.
The information and data has been collected by referring to the hospitals personally and filling out the checklist about the inputs, outputs, and health services’ prices.
b. DEA’s Conceptual and Mathematical Framework
Through the production process, inputs (production factors) are converted into outputs such as health status (medical and health services) by hospitals and medical centers. The inputs can be divided up into three general groups as follows: labor force, materials, and capital; although each group can be exposed into smaller components. The labor force contains professional staff such as physician, nurse, paramedic, manager, and supporting employee and nonprofessional one like driver, guardian, and butler. The materials consist of medication, all nondrug materials, and other product to serve medical outcomes. Finally, the capital contains land, building, medical equipments, vehicle, and bed. The relationship between inputs and resulting outputs (production process) has been revealed by Fig. 2. It is obvious that hospitals and medical centers use from multiple inputs for producing multiple outputs.
Fig. 2.
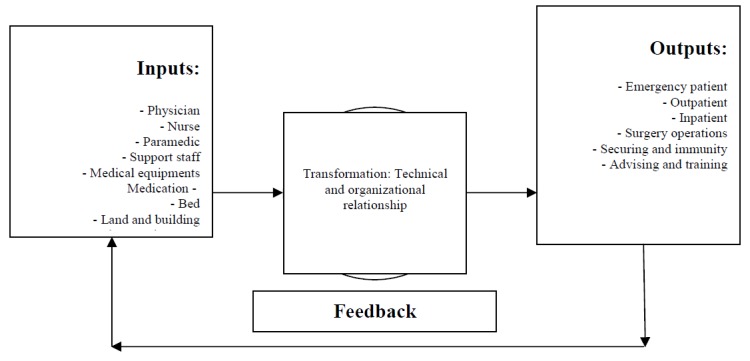
A Simplified System of a Typical Hospital
The DEA model is a unique, almost unacquainted especially in Iran, and powerful to estimate and analyze of efficiency of multiple inputs and multiple outputs, which can have very different units of measurement. As Ali Emrouznejad mentioned in his homepage [24] , “The measurement of relative efficiency where there are multiple possibly incommensurate inputs and outputs” was addressed by Farrell and developed by Farrell and Fieldhouse focusing on the construction of a hypothetical efficient unit, as a weighted average of efficient units, to act as a comparator for an inefficient unit.
A common measure for relative efficiency is:
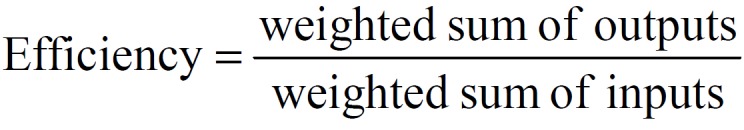
which introducing the usual notation can be written as
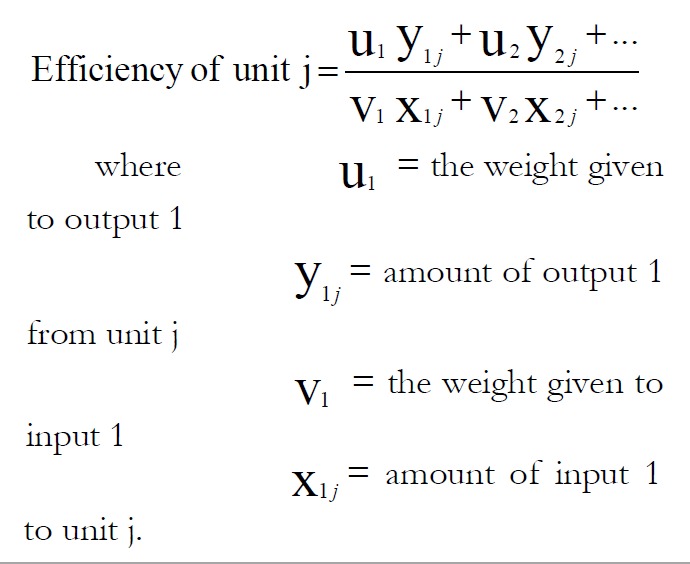
(Note efficiency is usually constrained to the range [0,1]).
The variables of the above problem are the weights and the solution produces the weights most favorable to unit J0 and produces a measure of efficiency [25].
Technical efficiency (TE) is about ensuring no resources are wasted, i.e. the maximum amount of output is obtained from the available inputs [26]. Based on Fig. 3, Health centers I, Q and S are technically efficient because they are operating on the production function or isoquant or efficiency frontier. Their efficiency score is one (or 100%). Health centers P and T are inefficient because they are using more nurses and clinic officers time to produce the same level of output as health centers I, Q and S. The extent of technical inefficiency of health center ‘P’ can be expressed as: [1-(OQ/OP)] [27], which is the amount by which all inputs could be proportionately reduced without a reduction in output. Allocative efficiency (AE) is about using resources to produce outputs with the highest possible value. AE implies the isoquant (IS) and isocost (AB) lines are tangential. Even though health centers I and Q are technically efficient, they are allocatively inefficient. Health center S is both technically and allocatively efficient. Allocative efficiency of facility P=OR/OQ.
Fig. 3.
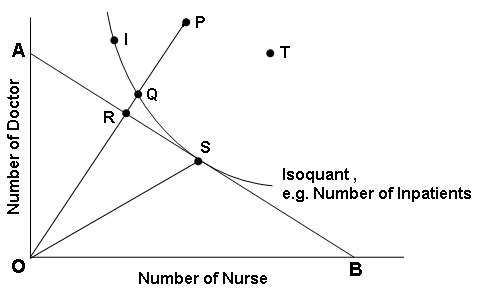
Hospitals’ technical and allocative efficiencies
The formulation for determining the degree of allocative efficiency for the J0 th health center is given by estimating the linear program formulation [28]:
And cost efficiency of facility as follows:
CE = P = OR/OP = (OQ/OP) × (OR/OQ) = TE × AE, [29].
c. Inputs and Outputs selection
In this study, adequate experimental analyses were done to obtain finalized inputs and outputs. Using SPSS 15 software, Spearman’s correlation coefficient tests (2-tailed) were applied between potential paired variables and examined multiple linear regression in various scenarios to achieve acceptable inputs and outputs. Also, sensitivity analysis through relatively many potential input-output variables was used; and considering Emanuel Thanassoulis [30] point of view that “the ultimate aim is that the input-output set used should conform to the exclusivity, exhaustiveness and exogeneity requirements and should involve as few variables as possible”; and of course taking into account practical statistical data gathering possibilities, some indices, experience, expertise opinion [31]; some of variables were combined together if applicable and then named in the same group as new variable and others just omitted from the model and ultimately the following inputs and outputs were selected and finalized for analyzing:
Inputs
Input 1: number of specialist physicians and above?
Input 2: number of general physicians + number of nurses + number of residents + number of medical team having a degree (bachelor) or above?
Input 3: number of medical team having 14 years diploma or lower + number of nonmedical and support staff
Input 4: number of active beds
Outputs
Output 1: number of emergency patients
Output 2: number of outpatients
Output 3: number of inpatients × average daily inpatients’ residing
Average inpatient’s residing in one given period equals ratio of day bed occupancy rate to number of whole released patients and mortalities in that period. In the present study, it was used statistical data of average residing in the various wards of the East Azerbaijani hospitals (average daily residing = 33 ÷ 9.24 = 1.64) [32].
We know that in order to calculate allocative efficiency score, we need the information related to production costs and prices in addition to quantities. In fact, one of the main factors limiting calculation of allocative efficiency is more technical and financial facilities needed and being able to estimate the costs and prices related to inputs and outputs properly. That is why some researchers, in addition to the reasons mentioned before, reduce the number of their inputs and outputs to make calculation of allocative efficiency feasible. Anyway, the prices of the inputs 1, 2, and 3 figured out on the base of the country’s standard monthly basic salary of PhD holder (equivalent to specialist); arithmetic mean of monthly basic salary of professional doctor, master degree holder, and bachelor degree holder; and arithmetic mean of monthly basic salary of diploma holder, high school diploma holder, and under high school diploma [33]. In the meanwhile, the price of input 4, that is, the value or cost of the each hospital bed was estimated using cost opportunity concept and based on the current and market value, assuming 15 years as life span and zero as scrap value.
Results
Using DEA approach, Table 1 reveals mean and standard deviation amounts for inputs and outputs of the eleven hospitals. In Table 2, there are general means of technical, scale, and allocative efficiencies of the selected hospitals. Table 3 and 4 show the situation of technological structure and the scores of technical, scale, allocative, and cost efficiencies about all selected hospitals in both public and private hospitals separately. It is particularly important to note that the extent of effectiveness amounts ranges from 0 (completely inefficient) to 1 (100% that is efficient). Finally, the structure of technology is defined by returns-to-scale properties. The shape of the efficiency frontier (and therefore DEA scores) will depend upon whether constant returns to scale (CRS) or non-increasing returns to scale (NIRS) or variable returns to scale (VRS) are assumed. In addition, it is reasonable to anticipate that hospital size is more likely to be influenced by market environment more than institutional or geographical constraints, implying that a CRS assumption is likely to be thick. Thus, the less restrictive CRS assumption is specified [34].
Table 1. Mean and Standard Deviation of inputs and outputs of the hospitals.
| Input and Output | Efficient Hospitals | Inefficient Hospitals | ||
| Mean | Standard Division | Mean | Standard Division | |
| Input 1 | 119.0 | 83.2 | 79.5 | 48.6 |
| Input 2 | 529.6 | 589.3 | 92.5 | 93.3 |
| Input 3 | 411.0 | 455.5 | 149.5 | 90.4 |
| Input 4 | 225.4 | 186.4 | 105.3 | 46.7 |
| Output 1 | 34972.8 | 15773.1 | 11070.0 | 14098.2 |
| Output 2 | 168866.8 | 93104.7 | 28582.2 | 33750.0 |
| Output 3 | 111384.0 | 102821.2 | 20244.8 | 13038.1 |
Input 1: number of specialist physicians and above
Input 2: number of general physicians + number of nurses + number of residents + number of medical team having a degree (bachelor) or above
Input 3: number of medical team having 14 years diploma or lower + number of nonmedical and support staff
Input 4: number of active beds
Output 1: number of emergency patients
Output 2: number of outpatients
Output 3: number of inpatients × average daily inpatients’ residing
Table 2. Mean and Standard Deviation of Efficiencies.
| Indictors | Technical Efficiency | Scale Efficiency | Allocative Efficiency | Cost Efficiency |
| Mean | 0.79 | 0.83 | 0.76 | 0.61 |
| Standard Deviation | 0.24 | 0.24 | 0.19 | 0.27 |
Table 3. Technical, Scale, Allocative, and Cost Efficiencies in Public Hospitals.
| Hospitals (DMUs) | Return to Scale | Technical Efficiency* | Scale Efficiency | Allocative Efficiency | Cost Efficiency |
| 1: Imam | CRS | 1.00 (8) | 1.00 | 1.00 | 1.00 |
| 2: Nikokari | CRS | 1.00 (7) | 1.00 | 0.94 | 0.94 |
| 3: Alzahra | IRS | 0.82 (0) | 0.97 | 0.70 | 0.57 |
| 4: Sina | CRS | 1.00 (3) | 1.00 | 0.50 | 0.50 |
| 5: Kodakan | CRS | 1.00 (4) | 1.00 | 0.67 | 0.67 |
| 6: Amir al Momenin | IRS | 0.51 (0) | 0.51 | 0.80 | 0.41 |
| Mean | - | 0.89 | 0.89 | 0.77 | 0.68 |
| Standard Deviation | - | 0.20 | 0.20 | 0.18 | 0.24 |
* Amounts into parentheses show that how many times each hospital has been referenced as a “bench mark”.Technical efficiency scores were obtained based on constant return to scale.
Table 4. Technical, Scale, Allocative, and Cost Efficiencies in Private Hospitals.
| Hospitals (DMUs) | Return to Scale | Technical Efficiency* | Scale Efficiency | Allocative Efficiency | Cost Efficiency |
| 7: Shams | IRS | 0.65 (0) | 0.99 | 0.96 | 0.62 |
| 8: Behbod | CRS | 1.00 (8) | 1.00 | 1.00 | 1.00 |
| 9: Shahryar | IRS | 0.81 (0) | 0.81 | 0.48 | 0.39 |
| 10: Nor Nejat | IRS | 0.40 (0) | 0.40 | 0.75 | 0.30 |
| 11: Shafa | IRS | 0.49 (0) | 0.49 | 0.61 | 0.30 |
| Mean | - | 0.67 | 0.74 | 0.76 | 0.52 |
| Standard Deviation | - | 0.24 | 0.28 | 0.22 | 0.30 |
* Amounts into parentheses show that how many times each hospital has been referenced as a “bench mark”.Technical efficiency scores were obtained based on constant return to scale.
Based on Table 3 and 4, 45% of selected hospitals are run under CRS and the rest (55%) under VRS. Consideration of technical efficiency results confirms this issue. In other words, all hospitals under CRS obtained technical efficiency scores 1 (100%), while the inefficient hospitals -with technical efficiency scores less than one- had been run under VRS. This means that efficient hospitals do not need to change their inputs and outputs’ amounts to improve their efficiency scores since they had already been located on the production possibilities frontier (Hospital 1, Hospital 2, Hospital 4, Hospital 5, and Hospital 8 hospitals), while on the contrary, ineffective hospitals with regard to technical issues were located under the production possibilities frontier and therefore need to enhance their activities (revising inputs and outputs’ quantities and some policy making issues) so as to reach their optimum points (Hospital 3, Hospital 6, Hospital 7, Hospital 9, Hospital 10, and Hospital 11).
Out of the 11 hospitals included in the analysis, 5 (45%) were technically and scale efficient, whereas the remaining 6 (55%) were technically and scale inefficient. Two out of 6 (33%) of technically and scale inefficient hospitals belonged to public sector and the rest (4 hospitals, 67%) technically and scale inefficient were under private sector’s ownership. Among the six inefficient hospitals, 2 (33%) had a TE score of less than 50% (both private), 2 (33%) between 51 and 74% (one private and one public) and the rest (2, 33%) between 75 and 99% (one private and one public). In the meanwhile, Hospital 8 was the only one that had technical, scale efficiency of 100%, and was under CRS. As a result, private hospitals were relatively more technically and scale inefficient than public ones.
In general, the selected hospitals had an average TE score and a standard deviation of 0.79 and 0.24 respectively. In addition, the inefficient hospitals had an average TE score of 61% and a standard deviation of 18%. This implies that on average, they could reduce their utilization of all inputs by about 39% without reducing outputs. This is just the concept of downsizing that has already been determined through the initial proposal’s goals.
It has to be mentioned that under VRS consumption, only Hospital 3 (public) and Hospital 7 (private) were chosen as inefficient ones with technically efficient scores 0.85 and 0.66 respectively.
The digits into the parentheses in TE column in Table 3 indicate the number of times each hospital had been selected as the best practice in repetitive process of linear programming. Optimum hospitals from technical efficiency view of point were Hospital 1 (public) and Hospital 8 (private) hospitals, which had been, referenced 8 times each as benchmark. Next ranks belonged to Hospital 2 (7 times), Hospital 5 (4 times), and Hospital 4 (3 times). It is necessary to note that the referenced hospitals are those that were able to deliver the same amount of medical services using relatively less amounts of inputs were being employed by inefficient hospitals.
Based on Table 2, mean of allocative and cost efficiencies for the selected hospitals were 76% and 61% respectively. Furthermore, Table 3 and 4 present interesting data of allocative and cost efficiencies in both individual public and private hospitals: the mean of allocative efficiencies of public and private hospitals were 77% and 76% (almost equal) and the mean of cost efficiencies of public and private hospitals were 68% and 52% respectively.
Discussion
This study was aiming to determine efficiency scores for public and private hospitals in the province. DEA method revealed that 55 percent of 11 selected hospitals were technical and scale inefficient and public hospitals were relatively more efficient than private ones. To improve efficiency scores, either their costs (inputs) should be cut for delivering given medical services (outputs) or their quantity of medical services must be increased, subject to fixing hospital’s expenditures, that is, optimal value. It is clear that we can practically reduce a certain percentage of the costs by increasing a certain percentage of medical services simultaneously. Table 5 presents exact amounts of required changes of inputs and outputs in order to convert inefficient hospitals into efficient ones.
Table 5. Input Reductions and/or Output Increases Needed to Make Individual Inefficient Hospitals Efficient*.
| Inefficient Hospitals | Inputs | Outputs | |||||
| Public | Input 1 | Input 2 | Input 3 | Input 4 | Output 1 | Output 2 | Output 3 |
| Alzahra (%) | 10.9 (18.1) | 49.7 (18.1) | 61.6 (27.5) | 32.6 (26.3) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) |
| Amir-al-momenin** (5) | 10.2 (48.6) | 33.0 (48.6) | 41.3 (48.6) | 76.9 (80.1) | 0.0 (0.0) | 1072.0 (10.9) | 0.0 (0.0) |
| Total Public | 21.1 | 82.7 | 102.9 | 109.5 | 0.0 | 1,072.0 | 0.0 |
| Private | Input 1 | Input 2 | Input 3 | Input 4 | Output 1 | Output 2 | Output 3 |
| Shams (%) | 48.0 (34.8) | 36.2 (34.8) | 118.4 | 111.6 (60.0) | 0.0 (0.0) | 208324.0 567.0) | 0.0 (0.0) |
| Shahryar (%) | 115.0 (82.7) | 9.7 (18.6) | 22.0 (18.6) | 64.8 (64.8) | 1859.2 (51.0) | 6896.3 (56.8) | 0.0 (0.0) |
| No Nejat (%) | 38.8 (80.8) | 15.0 (60.0) | 51.6 (60.0) | 38.3 (76.6) | 0.0 (0.0) | 6538.0 (126.2) | 0.0 (0.0) |
| Shafa (%) | 59.5 (83.8) | 16.4 (51.3) | 44.1 (51.3) | 61.0 (80.2) | 1933.9 181.9) | 0.0 (0.0) | 0.0 (0.0) |
| Total Private | 261.3 | 77.3 | 236.1 | 275.7 | 3793.1 | 221758.3 | 0.0 |
*Amounts in cells show quantities of inputs and outputs and figures into parentheses reveal the percent
of required increase or decrease of inputs or outputs to current situation.
** Amir-al-momenin hospital is located in Maragheh and the rest are located in Tabriz
The observed inefficiency shows that these hospitals have made use of too much input as compared with efficient ones, in other words they have not been able to provide enough medical services using this amount of resources. Table 5 also contains valuable information on possibility of reducible amount of each input in inefficient hospitals. Officials and policy makers of Iran’s health care system can make use of the percentage of variation in each input in order to determine the actual targets of their interventions. For example, Hospital 7 as an inefficient hospital is basically able to downsize input 1 (number of specialist and post specialist physicians), input 2 (number of general physicians + number of nurses + number of residents + number of medical team having a degree (bachelor) or upper, input 3 (number of medical team having 14 years diploma or lower + number of nonmedical and support staff), input 4 (number of active beds) 48.0, 36.2, 118.4, and 111.6 units respectively without perceiving any negative impact on its medical services. Furthermore, this hospital could consider the percentages mentioned in the parentheses as clear suggestions of policymaking and planning pattern and reduces its inputs of 1, 2, 3, and 4, during a specific period of time, up to 34.8, 34.8, 39.7, and 60.0 percent respectively without any reduction in the quantity of medical services (outputs).
Note that cost inefficiency is when it is under public sector. In private sector where profit maximization is the driving motive, they would do it by increasing per patient cost while providing more personal care. DEA will be ineffective in such a situation. In this study, it was specified that 82 percent of the selected hospitals were run under allocative and cost inefficiency’s status. Therefore, to improve the status of allocative and cost inefficiency, it is necessary to take all the items of costs into consideration to make sure that they are being used in the most worthwhile means.
Inefficient hospitals can to take two different perspectives: (i) policies do not intervention and insist in continuing to operate with the current inefficiencies; (ii) doing intervention as follows: ending current inefficiencies via issuing inefficiency warning to those staffs who work under acceptable standard level, terminating contracts of the excess staff and/or taking over the excess staff’s contract, benchmarking management procedures and organization from efficient hospitals. Simultaneously considering whether all this translates into improvement in indicators of health rather than just increasing the number of patients passing through a hospital.
It is necessary that the policy makers of health system make a set of policies and develop methods, which are based on Table 5 findings to improve the efficiency of inefficient hospitals as follows:
1. Transferring excess inputs of inefficient hospitals to efficient ones such as specialized physicians, general physicians, residents, nurses, medical staff, nonmedical and support staff, and finally active beds. This policy would remarkably strengthen these hospitals’ efficiency and potentially will improve provincial health care financial situation via using idle and/or excess human recourses and facilities in order to enhance the capacity of medical services to respond to people’s legitimate expectations.
2. Sending excess administrative and subordinate staff on early retirement. The saving could be used to improve remuneration and benefits for the remaining staff.
3. In regards to excess beds, either: (i) transfer them to efficient hospitals; (ii) sell them; or (iii) enter into a contract with private clinics practitioners or hospitals to use them at a price, which should not be less than the marginal costs.
4. In general, the authorities and managers should take provincial saving and frugality and excess nonwage expenditure into account either: (i) to improve the degree of responsiveness of hospitals to patient’s legitimate expectations; (ii) to improve rural and urban health centers quality of services; and (iii) to support communities to start or sustain systematic risk and resource pooling and cost sharing mechanisms for protecting beneficiaries against unexpected health care costs. The saved funds could be used to boost the capacity of the existing community-based health insurance schemes. According to Carrin et al. [35] the government has four basic functions for enhancing the capacity of Nonprofit Health Insurance Schemes (NPHIS): that of promoter of health insurance, monitor of NPHIS activities, trainer in all dimensions of insurance, and that of co-financier [36].
5. The government role in health care section should be gradually changed from mostly ownership to stewardship and monitoring. In other words, the government acts unfairly like an influential player or party who has the first chance of winning this game, instead of being impartial arbiter, and doing its vital duties which are taking care of principle players (private sector), preparation and observation of standards, regulations and rules of the game. Note that we do not mean to eliminate all public hospitals and giving the whole health care system to the private sector. Rather, we mean that the government should change its role from extremist ownership and incumbency to controlling and watching the services provided by the private sector in this regard. For the time being, the government is too laden and cumbersome to be accurately able to perform these vital responsibilities. Almost, in the most developed countries which have a modern health care system, the private sector provides the main medical services together with a very limited number of public hospitals; but the difference is that the government and/or insurance companies is the financial mediator between the patient and hospital. In other words, the government as public funder has the main responsibility of monitoring and financing of delivered health and medical services by the private sector [37].
6- More public hospitals are efficient probably because they are overloaded and afford less time per individual patients.
7- Consultants from private hospitals maybe helping to support the government owned facilities too.
The impacts of operationalizing the findings of this study and interfering in the system can be different for public and private hospitals. The savings from allocating resources in the public sector can help the process of converting a big and ineffective government to a small but effective one by resorting to economics thought and pave the way for the formation of a welfare state from the reserved resources which is one of the main needs of Iran’ society. It is clear that the very same idea can be applicable in other public sectors such as education, banks, and other public departments.
Considering the tendency of general international economic system towards privatization, the results of this study can provide the necessary resources for compensation of the costs of private hospitals’ depreciation and connection to the network of international health care markets (globalization) by optimizing the private sector and also enhancing new investments and eventually change the path into a smooth one by reinforcing privatization.
The main limitation of this study was the limited financial resources to do the job perfectly. For example, with adequate budget the current research would be expanded to practice the Malmquist Productivity Index as well. Also, for a better understanding of the nature of the care unites’ efficiency scores, the Meta Analysis would be recommended to be able to compare our study’s results with other similar researches in different societies and situations.
Acknowledgments
During this study, we have collaborated with many colleagues and people for whom we have great regard and wish to extend our warmest thanks to all authorities and those who have helped us with our work in East Azerbaijani Office of Treatment Deputy Minister of Ministry of Health like East Azerbaijani Management and Planning Organization as the study’s main sponsor, provincial public and private hospitals, and Tabriz University of Medical Sciences. The authors declare that there is no conflict of interests.
References
- [1]. World Health Organization. Health Systems: Concepts, Design and Performance (Tutor’s Guide). Working Document, Geneva; 2001; 48.
- [2]. Management and Planning Organization. Iran’s Budget Act: 2008-9, Acts, Tables, Resources (Incomes) and Expenditures of Governmental General Budget; 2007-8. [cited 2008 Feb. 25]. Available: http://www.majlis.ir/mhtml/
- [3]. Management and Planning Organization (2006-7) Iran’s Budget Act: 2007-8, Acts, Tables, Resources (Incomes) and Expenditures of Governmental General Budget, [cited 2007 Feb.15]. Available from: http://law.majlis.ir/home
- [4]. Sheikhzadeh, Y, Vahidi, RG, Seth VK. An Investigation on the Oil Income Elasticity of Health Care Expenditures during 1979-2004 and Lost and Faulty Links of Flow of Funds in Health Care System of Iran, presented at the 2nd International Conference of Health Financing in Developing Countries, CERDI, University of Auvergne, Clermont-Ferrand, France; 2006. [cited 2008 Feb. 27]. Available from: www.cerdi.org
- [5]. Selected Statistical Data 2006/07 (2006). Iranian Statistics Canter. Available from: http://www.sci.org.ir/portal/faces/public/sci/sci.gozide/sci.YearBook
- [6]. Statistical Year Book of East Azerbaijan (2006-7). East Azerbaijani Management and Planning Organization, [cited 2008 Feb.19]. Available: http://www.mpo-as.ir/sal/index.htm
- [7]. East Azerbaijani Management and Planning Organization. East Azerbaijani Economical, Social, and Cultural Report: 2005-6, Deputy Minister of Economical and Planning Affairs; 2007.
- [8].Ersoy K, Kavuncubasi S, Ozcan YA, Harris I IJM. Technical efficiencies of Turkish hospitals: DEA Approach. J Med Syst. 1997;21:2–67. doi: 10.1023/a:1022801222540. [DOI] [PubMed] [Google Scholar]
- [9].Majumdar SK. Assessing firms capabilities—theory and measurement—as study of Indian pharmaceutical, industry. Econ Polit Weekly. 1994;29:M83–M89. [Google Scholar]
- [10].Chang H. Determinants of hospital efficiency: the case of central government-owned hospitals in Taiwan. Omega-Int J Manage S. 1998;26:2–307. [Google Scholar]
- [11].Wan TTH, Hsu N, Feng R, Ma A, Pan S, Chou M. Technical efficiency of Nursing Units in a tertiary care hospital in Taiwan. J Med Syst. 2002;26:1–21. doi: 10.1023/a:1013086703159. [DOI] [PubMed] [Google Scholar]
- [12].Kirigia JM, Emrouznejad A, Gama R, Bastiene VH, Padayachy J. A comparative assessment of performance and productivity of health centers in Seychelles. IJPPM. 2008;57:1–72. [Google Scholar]
- [13].Kirigia JM, Sambo LG, Scheel H. Technical efficiency of public clinics in Kwazulu-Natal province of South Africa. East Afr Med J. 2001;78:3–S1. doi: 10.4314/eamj.v78i3.9070. [DOI] [PubMed] [Google Scholar]
- [14].Kirigia JM, Lambo E, Sambo LG. Are public hospitals in Kwazulu-Natal Province of South Africa technically efficient? Afr J Health Sci. 2000;7:3–32. [PubMed] [Google Scholar]
- [15]. Eyob ZA. Hospital efficiency in Sub-Saharan Africa: Evidence from South Africa. Working Paper, No. 187. The United Nations University World Institute for Development Economics Research; 2000.
- [16].Kirigia JM, Emrouznejad A, Sambo LG, Mounkaila A, Chimfwembe D, Okello D. Efficient Management of Health Centers Human Resources in Zambia. J Med Syst. 2006;30:6–473. doi: 10.1007/s10916-006-9032-1. [DOI] [PubMed] [Google Scholar]
- [17]. Masiye F. Investigating health system performance: An application of data envelopment analysis to Zambian hospitals, BMC Health Services Research; 2007. [cited 2008 Feb.19]. Available from: http://www.biomedcentral.com/1472-6963/7/58 [DOI] [PMC free article] [PubMed]
- [18].Kirigia JM, Emrouznejad A, Sambo LG, Munguti N, Liambila W. Using Data Envelopment Analysis to Measure the Technical Efficiency of Public Health Centers in Kenya. J Med Syst. 2004;28:2. doi: 10.1023/b:joms.0000023298.31972.c9. [DOI] [PubMed] [Google Scholar]
- [19]. Oseil D, Almeida S, George M, Kirigia JM, Mensah AO, Kainyu LH. Technical efficiency of public district hospitals and health centers in Ghana: a pilot study (2005); [cited 2008 Feb.5]. Available:http://www.resourceallocation.com/content/pdf/1478-7547-3-9.pdf [DOI] [PMC free article] [PubMed]
- [20].Hajialiafzali H, Moss J, Mahmood M. Efficiency Measurement for Hospitals Owned by the Iranian Social Security Organisation. J Med Syst. 2007;31:3–166. doi: 10.1007/s10916-007-9051-6. [DOI] [PubMed] [Google Scholar]
- [21].Mahani AS, Goudarzi GR, Barouni M, Khakiyan M. Estimation of Technical Efficiency of General Hospitals of Kerman University of Medical Sciences by Data Envelopment Analysis (DEA) Method. J Kerman Univ Med Sci. 2007;17:1–59. [Google Scholar]
- [22].Hatam N. The role of Data Envelopment Analysis (DEA) pattern in the efficiency of social security hospitals in Iran. IRCMJ. 2008;10:3–208. [Google Scholar]
- [23].Ketabi S. Efficiency Measurement of Cardiac Care Units of Isfahan Hospitals in Iran. J Med Syst. 2011;35:2–143. doi: 10.1007/s10916-009-9351-0. [DOI] [PubMed] [Google Scholar]
- [24]. Emrouznejad A’s DEA HomePage, [cited 2008 Feb.28]. Warwick Business School, Warwick University, UK . Available from: http://www.deazone.com
- [25].Kirigia JM, Emrouznejad A, Sambo LG, Munguti N, Liambila W. Using Data Envelopment Analysis to Measure the Technical Efficiency of Public Health Centers in Kenya. J Med Syst. 2004;28:2–158. doi: 10.1023/b:joms.0000023298.31972.c9. [DOI] [PubMed] [Google Scholar]
- [26].Kirigia JM, Sambo LG, Scheel H. Technical efficiency of public clinics in Kwazulu-Natal province of South Africa. East Afr Med J. 2001;78:3–S1. doi: 10.4314/eamj.v78i3.9070. [DOI] [PubMed] [Google Scholar]
- [27]. Eyob ZA. Hospital efficiency in Sub-Saharan Africa: Evidence from South Africa. Working Paper, No. 187. The United Nations University World Institute for Development Economics Research; 2000.
- [28]. Osei1 D, Almeida S, George M, Kirigia JM, Mensah AM, Kainyu LH. Technical efficiency of public district hospitals and health centers in Ghana: a pilot study, 2005 [cited 2008 Feb.08]. Available from:http://www.resourceallocation.com/content/pdf/1478-7547-3-9.pdf [DOI] [PMC free article] [PubMed]
- [29]. Coelli TJ. A guide to DEAP Version 2.1: A Data Envelopment Analysis Programme, CEPA, Working Paper 96/8, Department of Econometrics, University of New England, UK.; 1996.
- [30]. Thanassoulis E. Introduction to the Theory and Application of Data Envelopment Analysis: A Foundation Test with Integrated Software. 1st ed. Hingham MA: Kluwer Academic; 2001.
- [31]. Phone Interview with Emrouznejad A from Auston University in Feb.17, 2008.
- [32]. Treatment vice-president of Tabriz Medical University; [cited 2008 Feb.27]. Available: http://healthdata.tbzmed.ac.ir/
- [33]. Human Resources Management Office, Tabriz Medical Science University.
- [34].Masiye F, Kirigia JM, Emrouznejad A, Sambo LG, Mounkaila A, Chimfwembe D, Okello D. Efficient Management of Health Centers Human Resources in Zambia. J Med Syst. 2006;30:6–473. doi: 10.1007/s10916-006-9032-1. [DOI] [PubMed] [Google Scholar]
- [35]. Carrin G, Desmet M, Basaza R. Social health insurance development in low-income developing countries: New roles for government and nonprofit health insurance organizations in Africa and Asia, Building Social Security: The Challenge of Privatization. Chap. 10, Transaction publishers, New Brunswick, NJ, 2000.
- [36]. Kirigia JM, Emrouznejad A, Sambo LG, Munguti N, Liambila W. IBID; 2004. [DOI] [PubMed]
- [37]. Sheikhzadeh Y. An Acquaintance with Health Care Systems of Canada and Ten Developed Countries: USA, England, France, Germany, Netherlands, Denmark, Sweden, Japan, Australia, and New Zealand. Workshop, NPMC, Tabriz, 2007.


