Abstract
Atrial fibrillation is a common, global problem, with great personal, economic and social burdens. As populations age it increases in prevalence and becomes another condition that requires careful chronic management to ensure its effects are minimised. Assessment of the risk of stroke using well established risk prediction models is being aided by modern computerised databases and the choice of drugs to prevent strokes is ever expanding to try and improve the major cause of morbidity in AF. In addition, newer drugs for controlling rhythm are available and guidelines are constantly changing to reflect this. As well as medications, modern techniques of electrophysiology are becoming more widely embraced worldwide to provide more targeted treatment for the underlying pathophysiology. In this review we consider these factors to concisely describe how AF can be successfully managed.
Introduction
Atrial fibrillation (AF) is the commonest sustained cardiac arrhythmia and recent estimates of prevalence are around 2% of the population, although it may be greater than this. 1 It can cause debilitating symptoms, including from associated stroke; this comes with great cost to society. New therapies are emerging to limit the consequences of AF on individuals and on the greater community, such as advances in anticoagulation, the evolving role of drug therapy for maintaining sinus rhythm and the emerging invasive technologies for definitive AF treatments. The scope of this article is to consider the personal and societal consequences of AF, review approaches to defining an individual's risk of stroke in association with AF, look at how computer-based tools can help improve stroke risk management, discuss novel oral anticoagulant therapy, review guidelines for rhythm control strategies and look at evidence for more definitive treatment of AF with catheter ablation.
The prevalence, incidence and effect of atrial fibrillation, and is obesity contributing to the problem?
Atrial fibrillation is the most common cardiac arrhythmia and is undoubtedly a cause of substantial morbidity and mortality. 2 The prevalence of AF varies according to age and has been shown to approximately double per added decade of life, moving from a prevalence of 0.5% in the 6th decade of life to >10% in the 9th decade. 3 A more recent European study demonstrated a prevalence of 0.7% in those aged 55–59 rising to 17.8% in patients aged over 85; the same study estimated the lifetime risk of developing AF for males aged 55 to be 23.8% and for females of the same age 22.2%. 4
In the year 2000 in the United Kingdom an estimated 1.2% of the population had AF. 5 Again, in the UK, the Renfrew-Paisley project estimated the incidence as 0.54 cases per 1000 person years. 6 In Europe the prevalence of AF was estimated at 1%, 7 whereas in the USA the prevalence was said to be somewhere between 0.8 and 1.8 % (2.3–5.1 million) and set to reach an estimated 1.3%–3.8% (5.6–15.9 million) by 2050. 8,9 However, AF is often subclinical or too elusive to diagnose and such figures are likely to be an underestimate of the true prevalence of this condition.
Of course, the consequences of AF are wider reaching than the number of people suffering the condition. The risk of stroke is a major concern in patients with AF. It has been shown that the presence of AF can increase an individual's risk of stroke by a factor of 5, and 15–20% of all strokes can be attributed to AF. 10 In England alone, 12,500 strokes (out of a total of 89,000) per annum are suspected to be directly attributable to AF. 11 Strokes carry a significantly worse prognosis in the presence of AF than without; an ischaemic stroke in the presence of AF has a 1-year mortality approaching 50% 12 and those patients that do survive carry a higher degree of disability and are less likely to be discharged to their own homes. 13 The poorer outcomes of strokes seen in the context of AF can be explained by the greater severity at presentation, 13 as these patients are more likely to have severe limb weakness and be bedbound at presentation. 14 The financial burden of this is very substantial and in England the cost in the first year of a stroke due to AF is almost £12,000, 11 but this does not include the substantial costs of long-term care, such as care-homes, which can cost many thousands of pounds per year.
There is a growing prevalence of AF, as described above. Aging populations, particularly in developed countries, and especially where the burden of underlying cardiovascular disease is the greatest cause, are amongst the factors and causes for this reported rise. Obesity has emerged as an interesting candidate to help explain the rising global incidence of AF. Obesity has been shown to be an independent risk factor for developing AF and it has been suggested that for each unit rise in BMI the individual risk of AF increases by as much as 4%. 15 Potential mechanisms for this are debated and suggestions include a link for obesity with left atrial enlargement, itself a known precursor of AF. Obesity may predispose to left atrial enlargement via increased circulating volume, diastolic left ventricular dysfunction and neurohormonal activation. With the WHO demonstrating a doubling in global obesity since 1980, 16 and with predictions for further rises, the incidence and thus consequences of AF seems set to continue to increase. Other potential factors that may be fuelling the rise in prevalence of AF include sleep apnea, hypertension, diabetes and chronic kidney disease.
Determining the risk of stroke in atrial fibrillation
In order to effectively manage AF it is imperative to clarify a patient's risk of stroke to target those suitable for preventative therapies (discussed below). Until recently, the best-known risk assessment tool was the CHADS2 score, 17 validated for patients with non-rheumatic AF. This scoring system assigns 1 point for each of recent congestive cardiac failure, hypertension, age 75 years or greater or the presence of diabetes mellitus, and assigns 2 points for a personal history of either stroke or transient ischaemic attack (TIA). The summed score has a maximum of 6 and the adjusted stroke rate for each score is shown in Table 1. By subsequently dividing the resultant score into either low risk (score of 0), intermediate risk (score of 1) or high risk (score of 2 or more) the authors were able to identify suitable patients intended to benefit from anticoagulant treatment. 18
Table 1 .
Predicted stroke risk based on CHADS2 score.
| CHADS2 Score | Adjusted Stroke Rate per 100 patient years (95% confidence interval) |
| 0 | 1.9 (1.2–3.0) |
| 1 | 2.8 (2.0–.8) |
| 2 | 4.0 (3.1–5.1) |
| 3 | 5.9 (4.6–7.3) |
| 4 | 8.5 (6.3–11.1) |
| 5 | 12.5 (8.2–17.5) |
| 6 | 18.2 (10.5–27.4) |
Source: Adapted from Gage et al. 17
A refinement of the CHADS2 score may provide enhanced prediction and classification of those patients at higher risk of stroke or other thromboembolic events. 18 This has led to the use of a newer scoring system, known as CHA2DS2-VASC, which was derived in a cohort of 1034 non-valvular AF patients not on oral anticoagulant therapy. 19 The changes from CHADS2 are the awarding of 2 points for age equal to, or above, 75 years and 1 point for the additional risk factors of known vascular disease, age between 65 and 74, and female gender. The adjusted estimated rate of stroke per year based on the CHA2DS2-VASC score is shown in Table 2. 20
Table 2 .
Predicted annual stroke rate based on CHA2DS2VASC score.
| CHA2DS2VASC Score | Stroke rate per year adjusted for Warfarin use |
| 0 | 0.0 |
| 1 | 1.3 |
| 2 | 2.2 |
| 3 | 3.2 |
| 4 | 4.0 |
| 5 | 6.7 |
| 6 | 9.8 |
| 7 | 9.6 |
| 8 | 6.7 |
| 9 | 15.2 |
Source: Adapted from Lip et al. 20
A large cohort study in Denmark has tried to clarify which risk factors were important and which of the above scoring systems is most effective at predicting thromboembolic risk. 21 The authors defined low risk as a score of 0, intermediate risk as a score of 1 and high risk as a score of 2 or more. They found that patients defined as low and intermediate risk by CHADS2 were at a higher risk of stroke and other thromboembolic events than those in the low or intermediate risk group based on CHA2DS2-VASC, but both underestimated the risk of a previous thromboembolic event. Additionally they found that CHA2DS2-VASC performed better when predicting high-risk patients and had a slightly higher c-statistic indicating better predictive value of the model.
In addition to the above risk prediction models, other risk factors have been suggested as playing a role in predicting stroke in AF. It has been shown that by combining the CHADS2 score with monitoring atrial electrical activity, via a right atrial lead of a permanent pacemaker to define the duration of AF can improve the prediction of thromboembolic risk. 22 Here two discrete risk groups were defined, with 1-year risk of events of either 0.8% (low risk) or 5% (high risk). The low risk groups consisted of (1) patients with AF for less than 5 min per 24 h and with CHADS2 score 2 or less, (2) those with AF for greater than 5 min but less than 24 h per day and with a CHADS2 score of 1 or less, and (3) those with AF episodes for longer than 24 h and with a CHADS2 score of 0.
The presence of renal disease in patients with AF also seems to play a role in predicting the risk of stroke. 23 In a cohort of 10,908 patients the presence of proteinuria was shown to increase the risk of a thromboembolic event with a relative risk of 1.54 (95% confidence interval 1.29–1.85). Additionally, there was an increase in risk of events with decreasing estimated glomerular filtration rate.
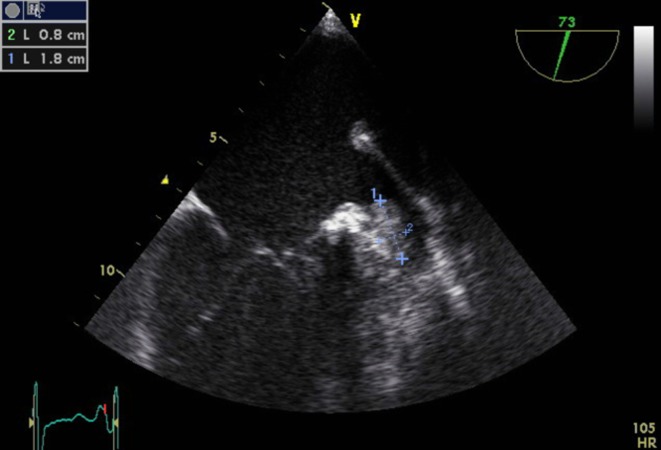
Echocardiography has also been shown as a useful tool in estimating an AF-patient's risk of stroke. Transthoracic echo can be used to estimate left ventricular (LV) dysfunction and correlate this to an individual's risk of stroke in AF, 24 where the presence of LV dysfunction was shown to carry a relative risk for stroke of 2.5 (95% confidence interval 1.5–4.4; p < 0.001). Patients with atrial fibrillation and significantly enlarged left atria are also at higher risk of stroke. In addition, a small proportion of patients will have significant valvular heart disease or cardiomyopathy. Transesophageal echocardiography (TEE) also has a role and higher rates of stroke have been shown in patients found to have dense spontaneous echocardiographic contrast, thrombus of the atrial appendage or aortic plaques. 25 An example of a left atrial appendage thrombus is shown in Figure 1. These additional tools in assessing risk may be useful in a small number of patients where the risk is not accurately reflected in the core risk factors measured in the CHADS2 and CHA2DS2-VASC systems; but these simpler clinical scoring systems remain the mainstay of stroke risk assessment for the vast majority of patients with AF.
Figure 1. .
Transoesphageal echocardiogram demonstrating a 1.8 cm (“1”) by 0.8 cm (“2”) thrombus in the left atrial appendage of a 57-year-old male with longstanding atrial fibrillation, despite being on warfarin but with subtherapeutic INR.
Anticoagulation in atrial fibrillation
Current guidelines for anticoagulation in AF rely on the risk factors and score as assessed mainly by the CHADS2 and CHA2DS2-VASC scores discussed above. Recently updated European Society of Cardiology (ESC) guidelines for the use of oral anticoagulant therapy 26 are summarised in Figure 2. The guideline advises the use of oral anticoagulant therapy in all cases of AF except for patients at low risk (lone AF and aged less than 65 years, of either sex). Therefore all patients with a CHA2DS2-VASC of one or greater should be offered oral anticoagulant therapy (except for CHA2DS2-VASC of 1 where the point is scored solely for female sex; in these patients no anticoagulation is advised). This is very similar to guidance from the American College of Chest physicians 27 (ACCP 9). This guidance uses the CHADS2 score and advocates that patients at low risk of stroke (CHADS2 score of 0) should not be given any therapy, whereas for those at intermediate and high risk of stroke (CHADS2 score ≥ 1) oral anticoagulant therapy is recommended. In terms of the type of AF, anticoagulant therapy should be considered for paroxysmal AF or AF controlled with a rhythm control strategy in the same way as for permanent AF. 27
Figure 2. .
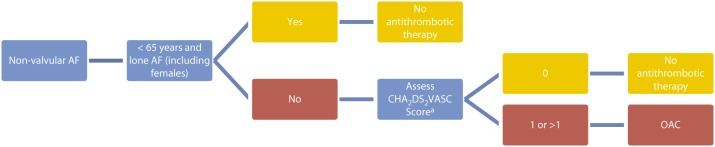
European Society of Cardiology guidelines for assessing need for oral anticoagulant (OAC) therapy in AF. Camm et al. 26 aComprised of 1 point for congestive cardiac failure, hypertension, diabetes mellitus, age 65–74, female sex and vascular disease, and 2 points for previous stroke/TIA/thromboembolism or age 75 years or greater.
Both of these guidelines also make clear that the risk of bleeding with oral anticoagulant therapy should be assessed and one way of assessing this risk is using the HAS-BLED 28 score, as suggested by the ESC guidelines. 26 This scoring system was originally derived and validated in a cohort of 3,978 European patients with AF. The scoring system uses seven risk factors for bleeding to make a simple summative scoring system to differentiate between patients at low or high risk of bleeding ( Tables 3 and 4). 27 In a large comparison against an older scoring system for bleeding risk, the HAS-BLED score was shown to be much simpler to use but of similar performance to the older, more complicated HEMORR2HAGES scoring system. 29 The ESC guidelines advise that those patients at higher risk of bleeding events (HAS-BLED score ≥ 3) require caution and more regular review of oral anticoagulant therapy. 26 An alternative to this is the score developed in the Anticoagulation and Risk Factors in Atrial Fibrillation Study (ATRIA); this uses five variables to assess bleeding risk (anaemia, severe renal disease, age, prior bleeding and hypertension). 30
Table 3 .
Characteristics composing the HAS-BLED bleeding risk score.
| Clinical characteristic | Definition | Points | |
| H | Hypertension | Systolic BP > 160 mmHg | 1 |
| A | Abnormal Renal Function | Chronic dialysis, renal transplantation or serum creatinine >200 mmol/L | 1 |
| Abnormal Liver Function | Chronic hepatic disease or biochemical evidence of significant hepatic derangement (bilirubin 2x upper limit of normal in association with ALT > 3 x upper limit of normal) | 1 | |
| S | Stroke | Previous history | 1 |
| B | Bleeding | Previous bleeding history or predisposition such as bleeding diathesis or anaemia | 1 |
| L | Labile INRs | Unstable or high INRs or < 60% of time in therapeutic range | 1 |
| E | Elderly | Age > 65 years | 1 |
| D | Drugs | Concomitant use of antiplatelet agents, NSAIDs | 1 |
| Alcohol | Alcohol abuse/excess | 1 |
Source: Adapted from Pisters et al. 28
Table 4 .
The risk of major bleeding based on HAS-BLED score (p value for trend 0.007).
| HAS-BLED score | Bleeds per 100 patient-years |
| 0 | 1.13 |
| 1 | 1.02 |
| 2 | 1.88 |
| 3 | 3.74 |
| 4 | 8.70 |
| 5 | 12.50 |
Source: Adapted from Pisters et al. 28
For many years, warfarin (and other oral vitamin K antagonists) has been the oral anticoagulant used to reduce the risk of stroke in AF patients, but there are now newer oral anticoagulants also available for use. Warfarin has long been shown to be superior to antiplatelet drugs, such as aspirin, and the benefits have been show to outweigh the added risk of bleeding events even in older patients traditionally thought to be in higher risk groups. 31 Three novel oral anticoagulants (NOAC) have come to the fore in recent guidelines for stroke risk in AF; indeed the NOAC are now preferred over warfarin for stroke prevention in AF by both the recent ESC guidelines update and ACCP 9 guidelines. 26,27
Dabigatran is a direct oral thrombin inhibitor and its safety and efficacy was assessed in a large non-inferiority trial in 18,113 patients with AF at risk of stroke. 32 This trial examined two doses of the drug (110 mg twice daily and 150 mg twice daily) against warfarin with primary outcomes of stroke or systemic embolus to assess efficacy and safety. At the conclusion of the trial the higher dose of dabigatran was shown to significantly reduce the incidence of ischaemic stroke or systemic emboli versus warfarin (relative risk 0.66; 95% confidence interval 0.53–0.82) with a similar rate of major bleeding (but dabigatran did have a higher rate of GI bleeding at this dose than in the warfarin arm). The lower dose was shown to have a similar rate of stroke compared to warfarin (relative risk 0.91; 95% confidence interval 0.74–1.11) with a significant reduction in major bleeding (major bleeding rate of 2.71% in low dose dabigatran arm compared to 3.36% in warfarin arm; p = 0.003). At both doses, dabigatran also showed a lower rate of intracranial haemorrhage compared to warfarin (0.38% per year in the warfarin group, as compared with 0.12% per year with 110 mg of dabigatran [p < 0.001] and 0.10% per year with 150 mg of dabigatran [p < 0.001]). When the data was further analysed to look at time in the therapeutic INR range even patients in the highest quartile had reduced risk of intracerebral haemorrhage (hazard ratio 0.39; 95% confidence interval 0.18–0.84). 33 The advantage of the higher dabigatran dose over Warfarin at preventing stroke disappeared, however, when the patients taking Warfarin had a time in the therapeutic INR range of greater than 73% (i.e. no advantage over well controlled warfarin). Dabigatran, unlike warfarin, is predominantly excreted via the kidneys and it has also been associated with GI side effects. Dabigatran at a dose of 150 mg twice daily is currently recommended in the ACCP 9 guidance for use, instead of warfarin, where an oral anticoagulant is required, 27 and is also the dose primarily recommended by the National Institute for Health and Clinical Excellence (NICE) in the UK as suitable for stroke prevention in at-risk patients with non-valvular AF. 34
Rivaroxaban, an oral factor Xa inhibitor, has also been shown in a large trial to be a suitable alternative to warfarin therapy for prevention of ischaemic stroke in patients with AF. 35 This double-blinded trial included 14,264 patients with non-valvular AF randomly assigned to receive either dose-adjusted warfarin (target INR of 2.5) or rivaroxaban 20 mg once daily with the primary end point of stroke or non-central nervous system embolism. The primary end point occurred less in the rivaroxaban arm (HR 0.79; 95% confidence interval 0.66–0.96) but this significant difference disappeared when the data was analysed on an intention to treat basis (rivaroxaban remained non-inferior to Warfarin, however). There was no overall reduction in the rate of major and non-major bleeding in the rivaroxaban arm, but there was a reduction specifically in intracranial bleeding (0.5% vs. 0.7%; p = 0.02) and fatal bleeding (0.2% vs. 0.5%; p = 0.003) compared to warfarin. Compared to the dabigatran study above, 32 the patients in this trial were at higher risk of stroke (a higher CHADS2 score). In both studies, there was relatively poor compliance with warfarin regimes, giving a time in therapeutic range of 55% overall, possibly reflecting the greater comorbidities and polypharmacy in these trials. In the UK, NICE has recently approved rivaroxaban as an alternative to warfarin for stroke and systemic embolus prevention in non-valvular AF and licensing bodies in both Europe and the US have also approved it. 36
A second oral factor Xa inhibitor, apixaban, has been investigated for a role in stroke prevention. This drug has a half-life of 12 h, is partially excreted via the kidneys and should be taken twice daily. It was first compared to aspirin for stroke prevention in patients who could not take warfarin and the trial was halted early due to the benefit of Abixaban. 37 A second randomized, double blind trial, then compared apixaban to warfarin in 18,201 patients with AF with at least one risk factor for stroke. 38 This study demonstrated an advantage of apixaban over warfarin for preventing ischaemic stroke or systemic embolism (HR 0.79; 95% confidence interval 0.66–0.95). It also showed a lower rate of major bleeding over warfarin (HR 0.69; 95% confidence interval 0.6–0.8) as well as a lower overall mortality compared to warfarin (3.52% per year vs. 3.94% per year; hazard ratio, 0.89; 95% CI, 0.80 to 0.99; p = 0.047). Apixaban also showed a trend to lower cardiovascular mortality (hazard ratio, 0.89; 95% CI, 0.76 to 1.04). Similar to the other novel oral anticoagulants, it showed a lower rate of intracranial haemorrhage (hazard ratio, 0.42; 95% CI, 0.30 to 0.58; p < 0.001), and similar to the trials on dabigatran & rivaroxaban, there was relatively poor adherence to INR targets in the warfarin arm (time in therapeutic range 62%). Apixaban has very recently been licensed in Europe for the prevention of stroke in patients with AF, and in the USA it is currently undergoing review for licensing.
We are likely to see greater usage of these newer therapies for stroke prevention, as they become more widely approved and as they avoid the need for frequent monitoring (compared to warfarin); thus becoming more acceptable to patients. It should be remembered, however, that experience with these drugs is relatively limited and that there are no currently available agents to reverse their effect in case of major complications, such as bleeding, although this is likely to be resolved in the near future. Indeed, a recent study in healthy volunteers showed the potential application of prothrombin complex concentrate to reverse rivaroxaban, and a recent oral abstract hinted at a role for monoclonal antibodies in reversing dabigatran's effect (http://www.improvement.nhs.uk/graspaf/ (accessed 18th January 2013)). 39 As the cost of these products diminish over time with more widespread uptake, then, taken together with the additional costs of monitoring warfarin (frequent blood tests and dedicated warfarin clinics) and dealing with the consequences of failing to achieve therapeutic targets (strokes, bleeds and the effects on cardioversion and ablation lists), the NOAC are likely to become more acceptable to commissioners (in the UK) and the wider medical community.
A new approach to identifying patients in need of anticoagulation – the GRASP-AF tool
The Guidance on Risk Assessment and Stroke Prevention for Atrial Fibrillation (GRASP-AF) tool is a service improvement application free to all general practice (GP) doctors in the UK. 40 It was first launched in November 2011 and has since been updated to adapt to the use of the CHA2DS2-VASC scoring system to assess stroke risk and incorporate the new oral anticoagulant medications. Using data from GP surgery databases it identifies patients with atrial fibrillation, assesses their risk of stroke (using both CHADS2 and CHA2DS2-VASC systems), searches for current blood thinning medication, searches for contraindications to warfarin therapy and alerts the clinician to those patients at risk of stroke but without adequate anticoagulant treatment.
Using this tool allows clinicians to easily identify those patients who are at risk of stroke from AF, but are not receiving any anticoagulant treatment. This of course has benefits at an individual patient level. The tool also has the ability to upload data to a national database so that individual practices can compare themselves to benchmarks and the countrywide performance figures. Pooling data in this way also contributes to a very large database of patients with AF and will help in providing more accurate information on prevalence and management.
Recent presentations by the NHS improvement team have suggested that strokes are already being prevented by the implementation of this tool. This form of nationwide tool should help to improve identification of patients in need of anticoagulation and prompt practitioners to start anticoagulation in these patients, especially as the use of novel oral anticoagulants becomes more commonplace in those patients not previously anticoagulated because of an inability to use warfarin.
Rhythm control in long-term atrial fibrillation and antiarrhythmic drugs
According to ESC guidelines, reasonable control of ventricular rate remains a goal in the long-term management of AF and a rhythm control strategy is appropriate for patients that remain symptomatic despite adequate rate control, or who are young and could potentially undergo catheter ablation (discussed below). 26,41 The use of drugs to control rhythm should be used in patients with recurrent AF. 26 Additionally, antiarrhythmic agents are often helpful in maintaining sinus rhythm following the use of direct current cardioversion. 26 Current ESC guidelines for drug selection to control rhythm are shown in Figure 3.
Figure 3. .
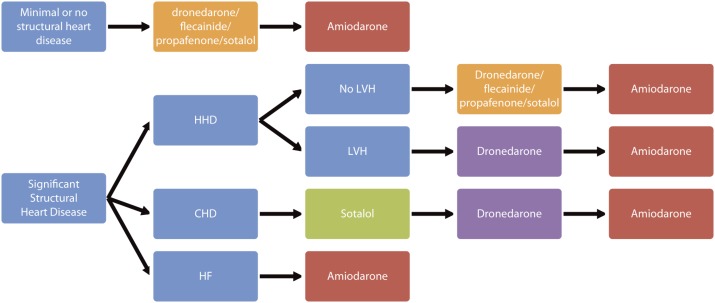
ESC guidelines for antiarrhythmic drug selection in AF. Adapted from Camm J et al. 26 . HHD – hypertensive heart disease; CHD – coronary heart disease; HF – heart failure; LVH – left ventricular hypertrophy.
The largest trial to compare rate and rhythm control strategies was the AFFIRM (Atrial Fibrillation Follow-up Investigation of Rhythm Management) trial reported in 2002. 42 A total of 4,060 patients were randomised to either a rhythm control strategy or a rate control strategy with the primary end point of all-cause mortality. At 5 years in, the rhythm control therapy group the mortality rate was 23.8% compared to 21.3% in the rate control arm (HR 1.15; 95% confidence interval 0.99–1.34; p = 0.08) and more patients in the rhythm control group were hospitalised. A further “on-treatment” analysis of the AFFIRM data 43 found that the presence of sinus rhythm was associated with a lower risk of death but confirmed that antiarrhythmic drugs are not associated with improved survival.
A Cochrane systematic review, updated in 2012, investigated the efficacy of antiarrhythmic drugs and their effect on mortality in AF patients undergoing cardioversion to restore sinus rhythm. 44 They found that several class 1A drugs (quinidine), 1C drugs (flecainide and propafenone) and class III drugs (amiodarone, dofetilide, dronedarone and sotalol) were all effective at maintaining sinus rhythm in patients post cardioversion ( Table 5). The beta-blocker, metoprolol, was also shown to be effective at maintaining sinus rhythm post cardioversion (odds ratio 0.62; 95% confidence interval 0.44–0.88; p = 0.008). Where studies compared two antiarrhythmic drugs, in general amiodarone compared more favourably at maintaining sinus rhythm. The study also assessed whether there was a benefit in mortality to taking antiarrhythmic drugs post cardioversion. They found that none of the drugs investigated provided a benefit in all-cause mortality, and class IA drugs and sotalol had a significantly higher mortality rate than controls.
Table 5 .
The efficacy of antiarrhythmic drugs at maintaining sinus rhythm post cardioversion from AF.
| Recurrence of atrial fibrillation (number of events/total) | ||||
| Drug | Drug | Control | Odds Ratio (95% confidence interval) | p-value |
| Quinidine | 741/1106 | 417/518 | 0.51 (0.40–0.65) | < .001 |
| Flecainide | 31/71 | 56/78 | 0.31 (0.16–0.60) | < 0.01 |
| Propafenone | 376/720 | 276/378 | 0.37 (0.28–0.48) | < 0.001 |
| Amiodarone | 200/428 | 209/245 | 0.19 (0.14–0.27) | < 0.001 |
| Dofetilide | 448/752 | 363/431 | 0.30 (0.23–0.39) | < 0.001 |
| Dronedarone | 648/982 | 353/461 | 0.59 (0.46–0.75) | < 0.001 |
| Sotalol | 1197/1791 | 955/1211 | 0.51 (0.43–0.60) | < 0.001 |
Source: Adapted from Lafuente-Lafuente et al. 44
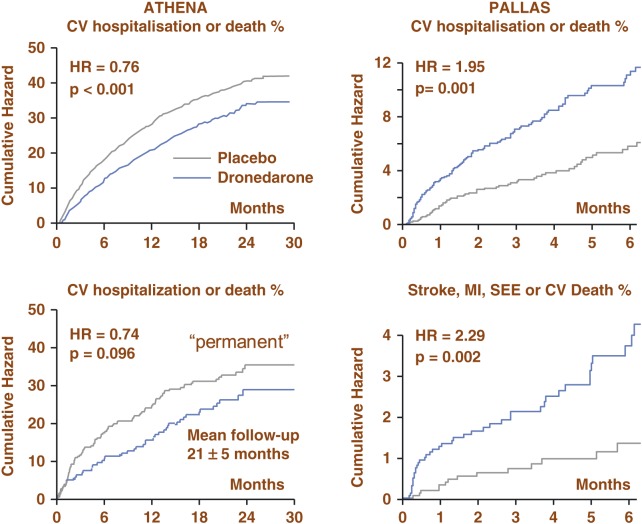
Dronedarone, a more recently approved antiarrhythmic drug, which is structurally related to amiodarone, is licensed for use in paroxysmal AF. A large trial of 4,628 patients randomised to dronedarone or placebo for control of paroxysmal or persistent AF, the ATHENA (A placebo-controlled, double-blind, parallel arm Trial to assess the efficacy of dronedarone 400 mg bid for the prevention of cardiovascular Hospitalisation or death from any cause in patients with Atrial fibrillation/atrial flutter) trial, found that the use of dronedarone reduced cardiovascular mortality and cardiovascular hospitalisations (hazard ratio for dronedarone 0.76; 95% confidence interval 0.69–0.84; p < 0.001). 45 There was also a reduction in first hospitalisations for cardiovascular events (hazard ratio 0.74; 95% confidence interval 0.67–0.82; p value < 0.001). Due to improved endpoints, regardless of achievement of sinus rhythm, a trial was undertaken for dronedarone use in permanent AF, known as the PALLAS (Permanent Atrial fibrillation outcome Study using dronedarone on top of standard therapy) trial. 46 Looking at the first co-primary outcome of the composite of stroke, myocardial infarction, cardiovascular death and systemic embolism the trial was halted early due to an increased number of cardiovascular events in the dronedarone arm. This first outcome occurred in 43 out of 1,619 patients in the dronedarone arm compared to 19 out of 1,617 in the placebo arm (hazard ratio of dronedarone 2.29; 95% confidence interval 1.34–3.94; p value 0.002). The second co-primary outcome this study investigated was all-cause mortality and unplanned cardiovascular hospitalisation, and in the dronedarone arm 127 experienced this outcome compared to 67 in the placebo group (hazard ratio for dronedarone 1.95; 95% confidence interval 1.45–2.62; p value < 0.001). As a result of these data, dronedarone is only indicated for patients with non-permanent AF and is contraindicated in patients with permanent AF or those with heart failure. 26 A summary of these trials is seen in Figure 4.
Figure 4. .
Summary of outcomes in PALLAS and ATHENA trials. In PALLAS, there was an increased incidence in the first coprimary outcome of stroke, myocardial infarction, systemic embolism or CV death for dronedarone compared to placebo and an increased incidence in the second coprimary outcome unplanned cardiovascular hospitalisation or death for dronedarone compared to placebo. As a result dronedarone should not be used in this permanent high risk AF patient population. Standard therapy may have included rate control agents (beta-blockers, and/or Ca-antagonist and/or digoxin) and/or anti-thrombotic therapy (Vit. K antagonists and /or aspirin and other antiplatelets therapy) and/or other cardiovascular agents such as ACEIs/ARBs and statins. Source: Adapted from Hohnloser et al. 45 ; Connolly et al. 46
As seen in Figure 3, currently recommended antiarrhythmic drugs in the ESC guidelines are amiodarone, dronedarone, flecainide, propafenone and sotalol.
Ablation therapies for atrial fibrillation
The European Society of Cardiology included recommendations for catheter ablation as a treatment for AF in the 2010 guidelines and has updated the recommendations in 2012. 26,40 The current guidelines recommend catheter ablation of paroxysmal AF in patients who have symptomatic recurrences whilst on antiarrhythmic drug therapy when performed by an experienced practitioner. They also recommend catheter ablation should be considered as a first line treatment in selected patients with symptomatic paroxysmal AF as an alternative to rhythm control drugs (discussed below).
In an early trial, which was not randomised, comparing ablation with medical treatment for AF, ablation performed better than medical therapy at improving AF free survival (78% AF free in ablation arm compared to 37% in medical group at 3 years; p value < 0.001) and at preventing adverse events. 47 This has led to randomised trials being conducted as well as multiple systematic reviews and meta-analyses. One of these reviews concluded that studies of radiofrequency ablation report higher rates of success than studies of antiarrhythmic drugs with lower rates of complications. 48 The CACAF trial (Catheter Ablation for the Cure of Atrial Fibrillation) looked at 245 patients in which 137 patients with paroxysmal or persistent AF (who had failed drug therapy) were randomised to receive ablation and arrhythmic drug therapy, showed that this group remained significantly more free of AF at one year than those randomised to drug therapy alone (56% free of AF in ablation arm vs. 9% in drug arm; p value < 0.001). 49 A second large randomised trial, APAF (Ablation for Paroxysmal Atrial Fibrillation), of 198 patients with paroxysmal AF who had failed drug therapy for rhythm control showed those randomised to ablation were again more likely to be free of atrial fibrillation at one year (86% in ablation group vs. 22% in drug therapy group; p < 0.001). 50
These studies considered evidence for paroxysmal AF where antiarrhythmic drug therapy has failed, but new evidence is emerging for a benefit in the first-line use of ablation in the treatment of paroxysmal AF as suggested by the recent update to the ESC guidelines. 26 The recently published MANTRA-PAF (Medical ANtiarrhythmic Treatment or Radiofrequency Ablation in Paroxysmal Atrial Fibrillation) trial reports a reduction in AF burden and AF symptoms at 24 months in a group of relatively healthy AF patients receiving ablation as a first line treatment compared to antiarrhythmic drug therapy (at 24 months burden of AF 22/146 in ablation group versus 43/148 in the drug therapy group; p value 0.004; at 24 months AF symptoms 10/146 in the ablation group versus 24/148 in the drug therapy group; p = 0.012). 51 This agrees with findings from a smaller study of 70 patients with symptomatic AF not all treated with antiarrhythmics where those randomised to ablation therapy were more likely to be free of symptomatic AF at 1 year than those randomised to drug therapy (13% of ablation group compared to 63% of drug therapy group had recurrence of symptomatic AF at 1 year follow up; p value < 0.001). 52 Further evidence on this subject is expected to emerge upon completion of the Catheter Ablation vs Anti-arrhythmic Drug Therapy for Atrial Fibrillation (CABANA) trial in 2015.
Evidence for longer-term benefit of ablation therapy is also beginning to emerge. In one such study, 100 patients, with PAF or long-standing persistent AF, referred for ablation were followed up for a period of 5 years and found to be arrhythmia free in 29% of cases after one procedure, but this rate of arrhythmia free survival was improved considerably, to 63%, after multiple procedures (median of 2 ablations per patient). 53 A 4-year follow up in a randomised trial showed that of the 99 patients randomised to receive ablation therapy, where 27 patients had undergone a repeat procedure, 72.7% were free of AF as compared to 56.5% in the drug therapy arm on an intention to treat basis; p value 0.017. 54
Conclusion
Atrial fibrillation places a large burden on an individual as well as on society. There are robust and easy to use tools to assess a patient's risk of developing serious complications such as stroke and systemic emboli, and anticoagulation is of paramount importance in managing patients with AF, especially with emerging novel oral anticoagulant drugs. Antiarrhythmic drugs still have an important role to play but are probably less effective at providing long-term freedom from AF than more definitive catheter ablation procedures. New guidelines for the management of AF are constantly emerging in the face of rapidly progressing evidence for interventional therapies.
References
- [1].Ruigomez A, Johansson S, Wallander M-A, Rodriguez LAG. Incidence of chronic atrial fibrillation in general practive and its treatment pattern. J Clin Epidemiol. 2002;55(4):358–363. doi: 10.1016/s0895-4356(01)00478-4. [DOI] [PubMed] [Google Scholar]
- [2]. NICE clinical guideline 36 Costing Report. 2006.
- [3].Kannel WB, Wolf PA, Benjamin EJ, Levy D. Prevalence, incidence, prognosis and predisposing conditions for atrial fibrillation: population based estimates. Am J Cardiol. 1998;82(8A):2N–9N. doi: 10.1016/s0002-9149(98)00583-9. [DOI] [PubMed] [Google Scholar]
- [4].Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, Stijnen T, Lip GY, Witteman JC. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Euro Heart J. 2006;27(8):949–953. doi: 10.1093/eurheartj/ehi825. [DOI] [PubMed] [Google Scholar]
- [5].Majeed A, Moser K, Carroll K. Trends in the prevalence and management of atrial fibrillation in general practice in England and Wales, 1994–1998: analysis of data from the general practice research database. Heart. 2001;86(3):284–288. doi: 10.1136/heart.86.3.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Stewart S, Hart CL, Hole DJ, McMurray JJV. Population prevalence, incidence, and predictors of atrial fibrillation in the Renfrew/Paisley study. Heart. 2001;86:516–521. doi: 10.1136/heart.86.5.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Fuster V, Ryda´n LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Leeuzey JY, Kay GN, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann S, Task Force on Practice Guidelines, American College of Cardiology/American Heart Association; Committee for Practice Guidelines, European Society of Cardiology; European Heart Rhythm Association; Heart Rhythm Society ACC/AHA/ESC guidelines. Eur Heart J. 2006;27:1979–2030. doi: 10.1093/eurheartj/ehl176. [DOI] [PubMed] [Google Scholar]
- [8].Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- [9].Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, Seward JB, Tsang TS. Secular trends in incidence of atrial fibrillation in OlmstedCounty, Minnesota, 1980–2000, and implications on the projections for future prevalence. Circulation. 2006;114(2):119–125. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- [10].Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22(8):983–988. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- [11]. NHS Improvement. June 2009. Available at http://www.improvement.nhs.uk/heart/Portals/0/documents2009/AF_Commissioning_Guide_v2.pdf. Accessed August 24, 2012.
- [12].Marini A, De Santis F, Sacco S, Russo T, Olivieri L, Totaro R, Carolei A. Contribution of atrial fibrillation to incidence and outcomes of ischaemic stroke: results from a population-based study. Stroke. 2005;36(6):1115–1119. doi: 10.1161/01.STR.0000166053.83476.4a. [DOI] [PubMed] [Google Scholar]
- [13].Jorgensen HS, Nakayama H, Reith J, Raaschou HO, Olsen TS. Acute stroke with atrial fibrillation. The Copenhagen Stroke Study. Stroke. 1996;27(10):1765–1769. doi: 10.1161/01.str.27.10.1765. [DOI] [PubMed] [Google Scholar]
- [14].Dulli DA, Stanko H, Levine RL. Atrial fibrillation is associated with severe acute ischaemic stroke. Neuroepidemiology. 2003;22:118–123. doi: 10.1159/000068743. [DOI] [PubMed] [Google Scholar]
- [15].Wang PH, Levy D, D'Agostino RB, Sr, Wolf PA, Vasan RS, Benjamin EJ. Obesity and the risk of new-onset atrial fibrillation. JAMA. 2004;292(20):2471–2477. doi: 10.1001/jama.292.20.2471. [DOI] [PubMed] [Google Scholar]
- [16]. WHO Fact Sheet No 311. May 2012. Available at http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed August 24, 2012.
- [17].Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke. JAMA. 2001;285(22):2864–2870. doi: 10.1001/jama.285.22.2864. [DOI] [PubMed] [Google Scholar]
- [18].Gage BF, van Walraven C, Pearce L, Hart RG, Koudstaal PJ, Boode BSP, Peterson P. Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin. Circulation. 2004;110(16):2287–2292. doi: 10.1161/01.CIR.0000145172.55640.93. [DOI] [PubMed] [Google Scholar]
- [19].Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–272. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- [20].Lip GY, Frison L, Halperin JL, Lane DA. Identifying patients at high risk for stroke despite anticoagulation. Stroke. 2010;41:2731–2738. doi: 10.1161/STROKEAHA.110.590257. [DOI] [PubMed] [Google Scholar]
- [21].Olesen JB, Lip GY, Hansen ML, Hansen PR, Tolstrup JS, Lindhardsen J, Selmer C, Ahlehoff O, Olsen AM, Gislason GH, Torp-Pedersen C. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;342:d142. doi: 10.1136/bmj.d124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Botto GL, Padeletti L, Santini M, Capucci A, Gulizia M, Zolezzi F, Favale S, Molon G, Ricci R, Biffi M, Russo G, Vimercati M, Corbucci G, Boriani G. Presence and duration of atrial fibrillation detected by continuous monitoring: crucial implications for the risk of thromboembolic events. J Cardiovasc Electrophysiol. 2009;20(3):241–248. doi: 10.1111/j.1540-8167.2008.01320.x. [DOI] [PubMed] [Google Scholar]
- [23].Go AS, Fang MC, Udaltsova N, Chang Y, Pomernacki NK, Borowsky L, Singer DE, ATRIA Study Investigators Impact of proteinuria and glomerular filtration rate on risk of thromboembolism in atrial fibrillation: the anticoagulation and risk factors in atrial fibrillation (ATRIA) study. Circulation. 2009;119(10):1363–1369. doi: 10.1161/CIRCULATIONAHA.108.816082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Atrial Fibrillation Investigators. Echocardiographic predictors of stroke in patients with atrial fibrillation. Arch Intern Med. 1998;158(12):1316–1320. doi: 10.1001/archinte.158.12.1316. [DOI] [PubMed] [Google Scholar]
- [25].SPAF Investigators. Transesophageal echocardiographic correlates of thromboembolism in high risk patients with nonvalvular atrial fibrillation. Ann Intern Med. 1998;128:639–647. doi: 10.7326/0003-4819-128-8-199804150-00005. [DOI] [PubMed] [Google Scholar]
- [26].Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, Hindricks G, Kirchhof P, ESC Committee for Practice Guidelines (CPG), Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, Document Reviewers, Vardas P, Al-Attar N, Alfieri O, Angelini A, Blömstrom-Lundqvist C, Colonna P, De Sutter J, Ernst S, Goette A, Gorenek B, Hatala R, Heidbüchel H, Heldal M, Kristensen SD, Kolh P, Le Heuzey JY, Mavrakis H, Mont L, Filardi PP, Ponikowski P, Prendergast B, Rutten FH, Schotten U, Van Gelder IC, Verheugt FW. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation. Eur Heart J. 2012;33(21):2719–2747. doi: 10.1093/eurheartj/ehs253. doi: 10.1093/eurheartj/ehs253. Epub August 24, 2012. [DOI] [PubMed] [Google Scholar]
- [27].You JJ, Singer DE, Howard PA, Lane DA, Eckman MH, Fang MC, Hylek EM, Schulman S, Go AS, Hughes M, Spencer FA, Manning WJ, Halperin JL, Lip GY, American College of Chest Physicians Antithrombotic therapy for atrial fibrillation: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141:e531S–e575S. doi: 10.1378/chest.11-2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro heart survey. Chest. 2010;138(5):1093–1100. doi: 10.1378/chest.10-0134. [DOI] [PubMed] [Google Scholar]
- [29].Olesen JB, Lip GY, Hansen PR, Lindhardsen J, Ahlehoff O, Andersson C, Weeke P, Hansen ML, Gislason GH, Torp-Pedersen C. Bleeding risk in “real world” patients with atrial fibrillation: comparison of two established bleeding prediction schemes in a nationwide cohort. J Thromb Haemost. 2011;9(8):1460–1467. doi: 10.1111/j.1538-7836.2011.04378.x. [DOI] [PubMed] [Google Scholar]
- [30].Fang MC, Go AS, Chang Y, Borowsky LH, Pomernacki NK, Udaltsova N, Singer DE. A new risk scheme to predict warfarin-associated hemorrhage, The ATRIA (anticoagulation and risk factors in atrial fibrillation) study. J Am Coll Cardiol. 2011;58(4):395–401. doi: 10.1016/j.jacc.2011.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Mant J, Hobbs FD, Fletcher K, Roalfe A, Fitzmaurice D, Lip GY, Murray E, BAFTA investigators; Midland Research Practices Network (MidReC) Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation (the Birmingham atrial fibrillation treatment of the aged study, BAFTA): a randomised control trial. Lancet. 2007;370(9586):493–503. doi: 10.1016/S0140-6736(07)61233-1. [DOI] [PubMed] [Google Scholar]
- [32].Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L, RE-LY Steering Committee and Investigators Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–1151. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- [33].Wallentin L, Yusuf S, Ezekowitz MD, Alings M, Flather M, Franzosi MG, Pais P, Dans A, Eikelboom J, Oldgren J, Pogue J, Reilly PA, Yang S, Connolly SJ, RE-LY investigators Efficacy and safety of dabigatran compared with warfarin at different levels of international normalised ratio control for stroke prevention in atrial fibrillation: an analysis of the RE-LY trial. Lancet. 2010;376(9745):975–983. doi: 10.1016/S0140-6736(10)61194-4. [DOI] [PubMed] [Google Scholar]
- [34]. NICE technology appraisal guidance 249. March 2012. Available at www.guidance.nice.org.uk/ta249. Accessed August 18, 2013.
- [35].Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Paolini JF, Berkowitz SD, Fox KA, Califf RM, ROCKET AF Investigators Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–891. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]
- [36]. NICE technology appraisal guidance 256. May 2012. Available at www.guidance.nice.org.uk/ta256. Accessed August 18, 2013.
- [37].Connolly SJ, Eikelboom J, Joyner C, Diener HC, Hart R, Golitsyn S, Flaker G, Avezum A, Hohnloser SH, Diaz R, Talajic M, Zhu J, Pais P, Budaj A, Parkhomenko A, Jansky P, Commerford P, Tan RS, Sim KH, Lewis BS, Van Mieghem W, Lip GY, Kim JH, Lanas-Zanetti F, Gonzalez-Hermosillo A, Dans AL, Munawar M, O'Donnell M, Lawrence J, Lewis G, Afzal R, Yusuf S, AVERROES Steering Committee and Investigators Apixaban in patients with atrial fibrillation. N Engl J Med. 2011;364(9):806–817. doi: 10.1056/NEJMoa1007432. [DOI] [PubMed] [Google Scholar]
- [38].Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, Al-Khalidi HR, Ansell J, Atar D, Avezum A, Bahit MC, Diaz R, Easton JD, Ezekowitz JA, Flaker G, Garcia D, Geraldes M, Gersh BJ, Golitsyn S, Goto S, Hermosillo AG, Hohnloser SH, Horowitz J, Mohan P, Jansky P, Lewis BS, Lopez-Sendon JL, Pais P, Parkhomenko A, Verheugt FW, Zhu J, Wallentin L, ARISTOTLE Committees and Investigators Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–992. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- [39].Eerenberg ES, Kamphuisen PW, Sijpkens MK, Meijers JC, Buller HR, Levi M. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate. Circulation. 2011;124:1573–1579. doi: 10.1161/CIRCULATIONAHA.111.029017. [DOI] [PubMed] [Google Scholar]
- [40].van Ryn J, Litzenburger T, Gan G, Coble K, Schurer J. In vitro Characterization, Pharmacokinetics and Reversal of supratherapeutic doses of dabigatran-induced bleeding in rats by a specific antibody fragment antidote to dabigatran. Oral Presentation 9928. Presented on 5 November 2012 at the American Heart Association Scientific Sessions 2012. [Google Scholar]
- [41].European Heart Rhythm Association; European Association for Cardio-Thoracic Surgery. Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, Van Gelder IC, Al-Attar N, Hindricks G, Prendergast B, Heidbuchel H, Alfieri O, Angelini A, Atar D, Colonna P, De Caterina R, De Sutter J, Goette A, Gorenek B, Heldal M, Hohloser SH, Kolh P, Le Heuzey JY, Ponikowski P, Rutten FH. Guidelines for the management of atrial fibrillation. Euro Heart J. 2010;31:2369–2429. doi: 10.1093/eurheartj/ehq278. [DOI] [PubMed] [Google Scholar]
- [42].The AFFIRM investigators. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347:1825–1833. doi: 10.1056/NEJMoa021328. [DOI] [PubMed] [Google Scholar]
- [43].Corley SD, Epstein AE, DiMarco JP, Domanski MJ, Geller N, Greene HL, Josephson RA, Kellen JC, Klein RC, Krahn AD, Mickel M, Mitchell LB, Nelson JD, Rosenberg Y, Schron E, Shemanski L, Waldo AL, Wyse DG, AFFIRM Investigators Relationships between sinus rhythm, treatment, and survival in the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) study. Circulation. 2004;109(2):1509–1513. doi: 10.1161/01.CIR.0000121736.16643.11. [DOI] [PubMed] [Google Scholar]
- [44].Lafuente-Lafuente C, Mouly S, Longas-Tejero MA, Bergmann JF. Antiarrhythmics for maintaining sinus rhythm after cardioversion of atrial fibrillation. Cochrane Database Syst Rev. 2012;5:CD005049. doi: 10.1002/14651858.CD005049.pub3. [DOI] [PubMed] [Google Scholar]
- [45].Hohnloser SH, Crijns HJ, van Eickels M, Gaudin C, Page RL, Torp-Pedersen C, Connolly SJ, ATHENA Investigators Effect of dronedarone on cardiovascular events in atrial fibrillation. N Engl J Med. 2009;360(7):668–678. doi: 10.1056/NEJMoa0803778. [DOI] [PubMed] [Google Scholar]
- [46].Connolly SJ, Camm AJ, Halperin JL, Joyner C, Alings M, Amerena J, Atar D, Avezum Á, Blomström P, Borggrefe M, Budaj A, Chen SA, Ching CK, Commerford P, Dans A, Davy JM, Delacrétaz E, Di Pasquale G, Diaz R, Dorian P, Flaker G, Golitsyn S, Gonzalez-Hermosillo A, Granger CB, Heidbüchel H, Kautzner J, Kim JS, Lanas F, Lewis BS, Merino JL, Morillo C, Murin J, Narasimhan C, Paolasso E, Parkhomenko A, Peters NS, Sim KH, Stiles MK, Tanomsup S, Toivonen L, Tomcsányi J, Torp-Pedersen C, Tse HF, Vardas P, Vinereanu D, Xavier D, Zhu J, Zhu JR, Baret-Cormel L, Weinling E, Staiger C, Yusuf S, Chrolavicius S, Afzal R, Hohnloser SH, PALLAS Investigators Dronedarone in permanent high risk atrial fibrillation. N Engl J Med. 2011;365(24):2268–2276. doi: 10.1056/NEJMoa1109867. [DOI] [PubMed] [Google Scholar]
- [47].Pappone C, Rosanio S, Augello G, Gallus G, Vicedomini G, Mazzone P, Gulletta S, Gugliotta F, Pappone A, Santinelli V, Tortoriello V, Sala S, Zangrillo A, Crescenzi G, Benussi S, Alfieri O. Mortality, morbidity and quality of life after circumferential pulmonary vein ablation for atrial fibrillation: outcomes from a controlled nonrandomized long-term study. J Am Coll Cardiol. 2003;42(2):185–197. doi: 10.1016/s0735-1097(03)00577-1. [DOI] [PubMed] [Google Scholar]
- [48].Calkins H, Reynolds MR, Spector P, Sondhi M, Xu Y, Martin A, Williams CJ, Sledge I. Treatment of atrial fibrillation with antiarrhythmic drugs or radiofrequency ablation: two systematic literature reviews and meta-analyses. Circ Arrhythm Electrophysiol. 2009;2(4):349–361. doi: 10.1161/CIRCEP.108.824789. [DOI] [PubMed] [Google Scholar]
- [49].Stabile G, Bertaglia E, Senatore G, De Simone A, Zoppo F, Donnici G, Turco P, Pascotto P, Fazzari M, Vitale DF. Catheter ablation treatment in patients with drug-refractory atrial fibrillation: a prospective, multi-centre, randomized, controlled study (Catheter Ablation for the cure of atrial fibrillation study) Euro Heart J. 2006;27(2):216–221. doi: 10.1093/eurheartj/ehi583. [DOI] [PubMed] [Google Scholar]
- [50].Pappone C, Augello G, Sala S, Gugliotta F, Vicedomini G, Gulletta S, Paglino G, Mazzone P, Sora N, Greiss I, Santagostino A, LiVolsi L, Pappone N, Radinovic A, Manguso F, Santinelli V. A randomized trial of circumferential pulmonary vein ablation versus antiarrhythmic drug therapy in paroxysmal atrial fibrillation: the APAF study. J Am Coll Cardiol. 2006;48(11):2340–2347. doi: 10.1016/j.jacc.2006.08.037. [DOI] [PubMed] [Google Scholar]
- [51].Cosedis Nielsen J, Johannessen A, Raatikainen P, Hindricks G, Walfridsson H, Kongstad O, Pehrson S, Englund A, Hartikainen J, Mortensen LS, Hansen PS. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl J Med. 2012;367:1587–1595. doi: 10.1056/NEJMoa1113566. [DOI] [PubMed] [Google Scholar]
- [52].Wazni OM, Marrouche NF, Martin DO, Verma A, Bhargava M, Saliba W, Bash D, Schweikert R, Brachmann J, Gunther J, Gutleben K, Pisano E, Potenza D, Fanelli R, Raviele A, Themistoclakis S, Rossillo A, Bonso A, Natale A. Radiofrequency ablation vs. antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation: a randomized trial. JAMA. 2005;293(21):2634–2640. doi: 10.1001/jama.293.21.2634. [DOI] [PubMed] [Google Scholar]
- [53].Weerasooriya R, Khairy P, Litalien J, Macle L, Hocini M, Sacher F, Lellouche N, Knecht S, Wright M, Nault I, Miyazaki S, Scavee C, Clementy J, Haissaguerre M, Jais P. Catheter ablation for atrial fibrillation: are results maintained at 5 years of follow up? J Am Coll Cardiol. 2011;57(2):160–166. doi: 10.1016/j.jacc.2010.05.061. [DOI] [PubMed] [Google Scholar]
- [54].Pappone C, Vicedomini G, Augello G, Manguso F, Saviano M, Baldi M, Petretta A, Giannelli L, Calovic Z, Guluta V, Tavazzi L, Santinelli V. Radiofrequency catheter ablation and antiarrhythmic drug therapy: a prospective, randomised, 4 year follow up trial: the APAF study. Circ Arrhythm Electrophysiol. 2011;4(6):808–814. doi: 10.1161/CIRCEP.111.966408. [DOI] [PubMed] [Google Scholar]