Abstract
Background
Little is known about the competences of residents as clinical teachers in African health care institutions.
Objective
We evaluated the clinical teaching skills of internal medicine residents from the perspective of medical students in a tertiary teaching institution in Africa.
Methods
We used the augmented Stanford Faculty Development Program Questionnaire, which has evidence of validity and reliability. To avoid a Hawthorne effect, students completed the questionnaire anonymously and confidentially after clinical teaching sessions by residents. A minimum score of 4 on a scale of 1 to 5 was defined a priori as possession of good clinical teaching skills.
Results
Sixty-four medical students assessed all 20 internal medicine residents in the Department of Medicine, University of Ibadan. Mean performance scores for the domains ranged from 3.07 to 3.66. Residents performed best in creating a good learning climate and worst in the promotion of understanding and retention. Sex of the resident, duration of residency, and rank had no significant impact (.09 < P < .94) on their teaching skills.
Conclusions
Consistent with other observations in the literature, residents' clinical teaching skills were suboptimal, particularly in their ability to promote understanding and retention. To enhance these skills, we recommend the integration of appropriately tailored programs to teach pedagogic skills programs in residency training.
Editor's Note: The online version (125.5KB, doc) of this article contains the Clinical Teaching Assessment Instrument used in this study.
Introduction
Development of clinical acumen through good clinical teaching is a key component of medical education. It is particularly critical in resource-limited settings where technology-assisted diagnosis is not readily accessible. Clinical teaching gives the opportunity to simultaneously impart, formatively assess, and actively improve the full range of skills required of a physician, including cognitive, psychomotor, decision-making, self-learning, and communication skills.
Residents play an important role in imparting these skills to junior learners.1–4 In the United States, residents provide up to 70% of clinical teaching of medical students.1–8 They are also playing a significant role in Nigeria as in other African countries, where there are too few physician-educators to cope with the expanding student population.9,10
Little is known about the clinical teaching skills of residents globally and in Africa.9–11 Studies are needed to identify areas of deficiencies that can be targeted by interventions.
The objective of our study was to evaluate the clinical teaching skills of medical residents from the perspective of medical students in a Nigerian teaching hospital.
Methods
We conducted this study in all units of the Department of Medicine, University College Hospital, University of Ibadan. All medical students who had their internal medicine rotation during the study period (January 2011–June 2011) and gave consent were enrolled. Respondents were fifth-year medical students undergoing their second 8-week clinical rotation. Our study excluded residents in other departments and dental students rotating through the department to avoid heterogeneous responses. The curriculum for the rotation included history taking, examination, and clinical reasoning skills spanning the various aspects of internal medicine.
Ethical approval was obtained from the University of Ibadan/University College Hospital Human Research Ethics Committee.
Instrument
Methods for evaluating the effectiveness of residents' clinical teaching skills include different areas of assessment (knowledge, attitudes, and skills); various types of evaluators (self, learner, or faculty); and different ways of conducting the assessment (questionnaires, observation, and narrative feedback).1–4,12–14 Written feedback may be more valuable than narrative feedback for improving resident performance and increasing resident satisfaction and interest in teaching.1 An example is the Clinical Teaching Perception Inventory, which is clinically oriented and uses self-reporting by teachers.14
We conducted a student-based evaluation by using the Stanford Faculty Development Program Questionnaire (SFDPQ), a psychometrically robust instrument for evaluation of clinical teachers. It consists of 58 items in 8 domains and uses a closed Likert-type format (1 = strongly disagree to 5 = strongly agree). A score of 4 indicates agreement by the students that the residents possessed the respective skills, while a score of 5 indicates excellent demonstration of the corresponding teaching skill.
The SFDPQ assesses the ability of the teacher to establish a positive learning climate; effectively manage, focus, and pace the teaching encounter; communicate teaching goals; promote effective understanding and retention; evaluate learner's achievements and give feedback; and promote self-directed learning.12 The SFDPQ is considered the most comprehensive, well-structured, learner-centered, valid, and reliable assessment of teaching skills.13 However, it does not assess the teacher's knowledge and subject mastery, necessitating the addition of 5 items to measure teachers' knowledge.13 In addition, the SFDPQ does not assess teachers' enthusiasm, warmth, accessibility, optimism, and empathic skills. We included a ninth domain on teacher's attitude, comprising 7 items to produce an augmented SFDPQ (provided as online supplemental material). The additional teacher's attitude domain demonstrated internal consistency reliability (Cronbach α = 0.89) and good construct validity in relation to the original SFDPQ (ρ = 0.647, P < .001).
Assessment
We administered the questionnaire (provided as online supplemental material) to medical students after bedside teaching sessions organized by residents. This was performed after the fourth week of the rotation following several encounters with the residents. They were required to complete the questionnaire confidentially and anonymously. To eliminate a Hawthorne effect, residents were not informed that they were being assessed.8
Data Analysis
We generated and summarized domain and total scores by using measures of central tendency and dispersion. On the SFDPQ, a score of 4 indicates agreement that the teacher possesses the respective skill, while a score of 5 indicates excellent demonstration of the corresponding skill. We a priori selected a score of 4 as indicating that a resident possessed good clinical teaching skills for the respective item or domain.12
We explored possible associations between sex, duration of residency training, rank of the residents, and teaching skill scores by using Mann-Whitney U and Spearman rank correlation statistics as appropriate. We set the level of significance at P < .05.
Results
Twenty residents (15 men and 5 women; 9 registrars and 11 senior registrars) were assessed by 64 medical students (49 men, 15 women) on medical posting in the 7 subspecialties in the Department of Medicine, University College Hospital, Ibadan. Sixty-four of 68 questionnaires were returned for a response rate of 94%.
Female medical students significantly rated the residents better in the “evaluation domain” than male medical students. (Mann-Whitney U = 109.5, P = .03). There was no significant difference in rating between female and male medical students in other domains and on the global scale (31.0 < Mann-Whitney U < 188.0; .14 < P < .80).
Residents' Clinical Teaching Skills
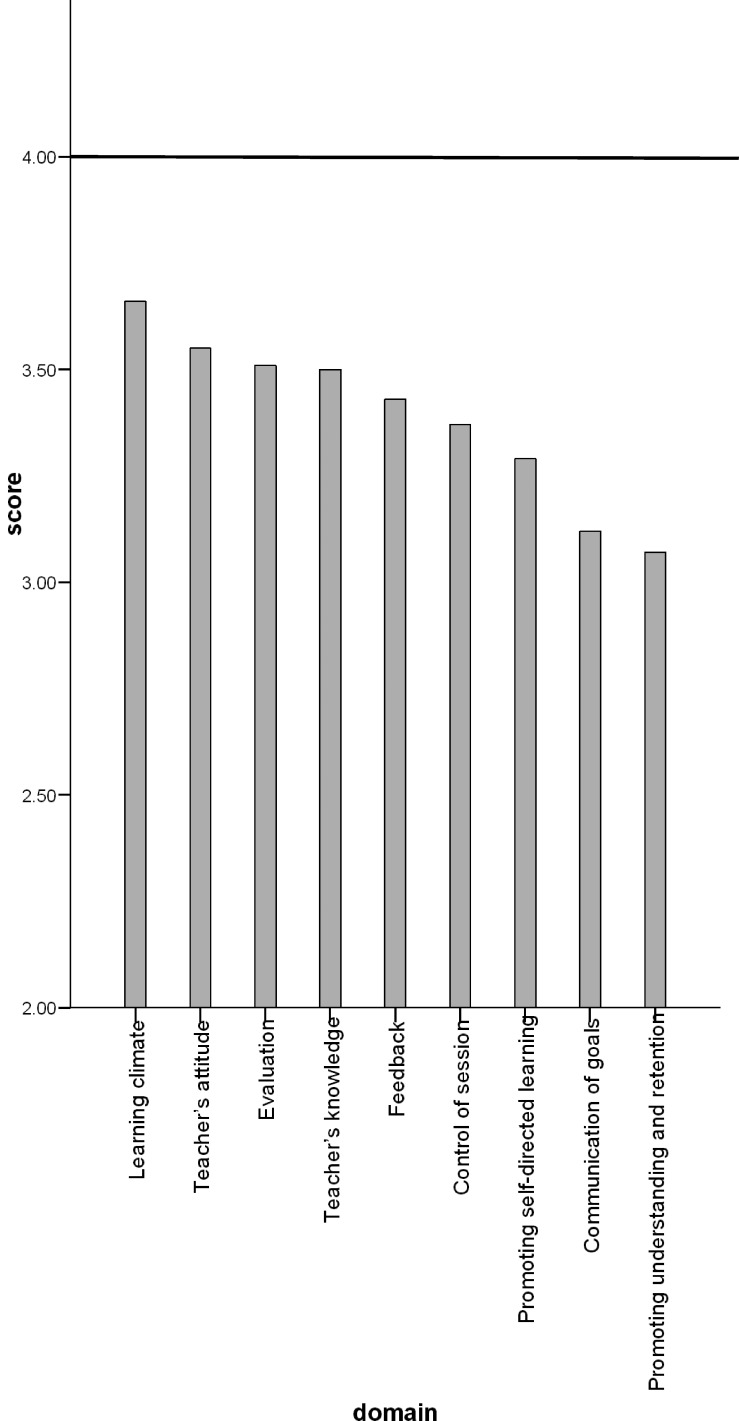
Residents' mean performance scores were suboptimal, ranging from 3.07 to 3.66 (table), with a score of 4 (the a priori determined score signifying the resident possessed the respective skills) not reached in any domain. Residents performed best in creating a good learning climate and least well in promoting understanding and retention (figure).
TABLE.
Evaluation of Clinical Teaching Skills of Residents
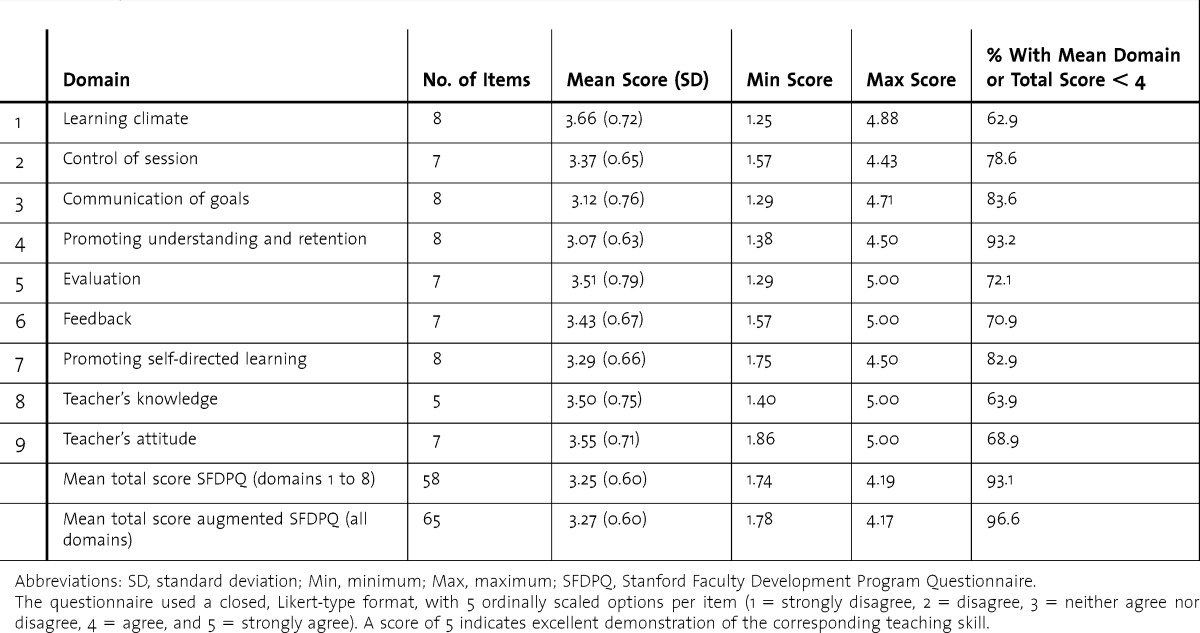
FIGURE .
Clinical Teaching Skills (Mean Performance Scores) of Residents, Arranged in Descending Order
The questionnaire used a closed, Likert-type format, with 5 ordinally scaled options per item (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, and 5 = strongly agree). A score of 4 indicates satisfactory demonstration of the corresponding teaching skill.
Determinants of Clinical Teaching Skills
The mean total SFDPQ scores were 3.28 ± 0.13 for male residents and 3.11 ± 0.21 for female residents. The sex of the residents had no significant impact on the SFDPQ domain and total scores (54.0 < Mann-Whitney U < 287.5; .09 < P < .94).
The mean total SFDPQ scores were 3.15 ± 0.15 for senior residents and 3.42 ± 0.16 for junior residents. The level of the resident (junior versus senior) had no significant effect on SFDPQ domain and total scores (99.0 < Mann-Whitney U < 343.5; .16 < P < .54). In addition, the duration of residency did not correlate significantly with the clinical teaching skills (−0.022 < ρ < −0.197; .13 < P < .87).
Discussion
This is a novel study that evaluates the clinical teaching skills of residents in an African institution from the perspective of medical students, using a comprehensive formal assessment with an instrument with established validity. Our survey response rate of 94% is considered satisfactory.
In a Dutch study, in which residents assessed their clinical teachers by using a modified 26-item version of the SFDPQ, communication of goals had the lowest score (mean = 3.41), and the highest score achieved was 4.07 for “professional attitude toward the residents.”15 The higher-scoring domains (with mean score of > 3.5) in our assessment were learning climate, teacher's attitude, and evaluation. The remaining domains (including the communication of goals domain) were worse, with the domain assessing the promotion of understanding and retention being the worst (table).
The lowest scoring attribute, the ability of the resident to promote understanding and retention, is a crucial learning goal. It depends on the teacher's ability to present well-organized material, explain relationships in the material, answer learners' questions clearly, emphasize what he or she wanted the learners to remember, have learners reformulate materials, and apply teaching materials to the learners' own experiences.12 Our observed performance gaps suggest specific pedagogic learning needs for residents, which are similar to the needs identified in a study of residents in Mexico.11 We sought to identify possible factors influencing these performance gaps.
Among the residents, duration of residency did not correlate significantly to clinical teaching skills, and sex and level of training also had no significant influence on clinical teaching skills. Although these negative findings may be due to our relatively small sample size, similar observations have been made elsewhere.11,15
Limitations of our study include the fact that it was conducted in a single site, reducing the generalizability of our findings. It is also possible that our a priori determined score for competence in clinical teaching may have been set too high for residents as teachers. The Dutch study15 found a number of scores below 4 for faculty serving as teachers. It may well be that clinical teaching skills need to be improved in both residents and faculty.
Intervention programs to address the limitations and performance gaps in clinical teaching by residents are warranted. There is mounting evidence that such tailored interventions to address pedagogic skills are effective and produce satisfaction and positive change in satisfaction, knowledge, attitude, behavior, and performance.1,12,13,16–18
Conclusion
We found suboptimal clinical teaching skills in residents, as perceived by medical students, particularly in the ability to promote understanding and retention. To enhance clinical teaching skills, formal pedagogic programs should be integrated into residency training. Larger multi-institutional studies are needed to identify factors influencing the clinical teaching skills of resident physicians on the African continent.
Footnotes
Mayowa O. Owolabi, MBBS, MSc, DM, MWACP, FMCP, Cert Epid & Glob Health (Dundee), is Senior Lecturer, Department of Medicine, University College Hospital, Ibadan, Nigeria, and Subdean (Postgraduate), Faculty of Clinical Sciences, University of Ibadan, Ibadan, Nigeria; Adefemi O. Afolabi, MBBS, FWACS, is Senior Lecturer, Department of Surgery, and former Subdean (Postgraduate), Faculty of Clinical Sciences, University of Ibadan; and Akinyinka O. Omigbodun, MBBS, FWACS, FMCOG, FAS, is Professor, Department of Obstetrics and Gynecology, and former Provost, College of Medicine, University of Ibadan.
Funding: The ACP-EU Cooperation Programme in Higher Education (EDULINK) provided a grant (No. 9 ACP RPR 12 # 31).
The authors would like to thank the African, Caribbean, and Pacific Group of States (ACP Secretariat) at the European Union through the ACP-EU Cooperation Programme in Higher Education (EDULINK), which provided a grant (No. 9ACP RPR 12 # 31) to establish the Master of Science in Biomedical Education program at the Faculty of Clinical Sciences, University of Ibadan. Dr Owolabi was 1 of the sponsored pioneer students and the data in this article were part of his dissertation, which won the award for the best dissertation in the cohort.
References
- 1.Wilson FC. Teaching by residents. Clin Orthop Relat Res. 2007;454:247–250. doi: 10.1097/BLO.0b013e31802b4944. [DOI] [PubMed] [Google Scholar]
- 2.Huynh A, Savitski J, Kirven M, Godwin J, Gil KM. Effect of medical students' experiences with residents as teachers on clerkship assessment. J Grad Med Educ. 2011;3(3):345–349. doi: 10.4300/JGME-03-03-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Snell L. The resident-as-teacher: it's more than just about student learning. J Grad Med Educ. 2011;3(3):440–441. doi: 10.4300/JGME-D-11-00148.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rotenberg BW, Woodhouse RA, Gilbart M, Hutchinson CR. A needs assessment of surgical residents as teachers. Can J Surg. 2000;43(4):295–300. [PMC free article] [PubMed] [Google Scholar]
- 5.Roop SA, Pangaro L. Effect of clinical teaching on student performance during a medicine clerkship. Am J Med. 2001;110(3):205–209. doi: 10.1016/s0002-9343(00)00672-0. [DOI] [PubMed] [Google Scholar]
- 6.Polan HJ, Riba M. Creative solutions to psychiatry's increasing reliance on residents as teachers. Acad Psychiatry. 2010;34(4):245–247. doi: 10.1176/appi.ap.34.4.245. [DOI] [PubMed] [Google Scholar]
- 7.Akins R, Handal GA. Resident block-rotation in clinical teaching improves student kearning. Acad Leadership J. 2010;8(3) http://www.academicleadership.org/article/Resident_Block-rotation_in_Clinical_Teaching_Improves_Student_Learning. Accessed August 10, 2012. [Google Scholar]
- 8.McCarney R, Warner J, Iliffe S, van Haselen R, Griffin M, Fisher P. The Hawthorne Effect: a randomised, controlled trial. BMC Med Res Methodol. 2007;7:30. doi: 10.1186/1471-2288-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Sub-Saharan African Medical School Study (SAMSS) http://samss.org/literature/default.aspx?literature. Accessed June 30, 2013. [Google Scholar]
- 10.Gukas ID. Global paradigm shift in medical education: issues of concern for Africa. Med Teach. 2007;29(9):887–892. doi: 10.1080/01421590701814286. [DOI] [PubMed] [Google Scholar]
- 11.Sánchez-Mendiola M, Graue-Wiechers EL, Ruiz-Pérez LC, García-Durán R, Durante-Montiel I. The resident-as-teacher educational challenge: a needs assessment survey at the National Autonomous University of Mexico Faculty of Medicine. BMC Med Educ. 2010;10:17. doi: 10.1186/1472-6920-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Litzelman DK, Stratos GA, Marriott DJ, Skeff KM. Factorial validation of a widely disseminated educational framework for evaluating clinical teachers. Acad Med. 1998;73(6):688–695. doi: 10.1097/00001888-199806000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Coverdale JH, Ismail N, Mian A, Dewey C. Toolbox for evaluating residents as teachers. Acad Psychiatry. 2010;34(4):298–301. doi: 10.1176/appi.ap.34.4.298. [DOI] [PubMed] [Google Scholar]
- 14.Morrison EH, Hitchcock MA, Harthill M, Boker JR, Masunaga H. The on-line Clinical Teaching Perception Inventory: a “snapshot” of medical teachers. Fam Med. 2005;37(1):48–53. [PubMed] [Google Scholar]
- 15.Lombarts MJ, Bucx MJ, Rupp I, Keijzers PJ, Kokke SI, Schlack W. An instrument for the assessment of the training qualities of clinician-educators. Ned TijdschrGeneeskd. 2007;151(36):2004–2008. [PubMed] [Google Scholar]
- 16.Morrison EH, Rucker L, Boker JR, Gabbert CC, Hubbell FA, Hitchcock MA, et al. The effect of a 13-hour curriculum to improve residents' teaching skills: a randomized trial. Ann Intern Med. 2004;141(4):257–263. doi: 10.7326/0003-4819-141-4-200408170-00005. [DOI] [PubMed] [Google Scholar]
- 17.Steinert Y, Mann K, Centeno A, Dolmans D, Spencer J, Gelula M, et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach. 2006;28(6):497–526. doi: 10.1080/01421590600902976. [DOI] [PubMed] [Google Scholar]
- 18.Wachtel JK, Greenberg MR, Smith AB, Weaver KR, Kane BG. Residents as teachers: residents' perceptions before and after receiving instruction in clinical teaching. J Am Osteopath Assoc. 2013;113(1):23–33. [PubMed] [Google Scholar]