Abstract
Background
There is an increasing use of electronic health records in hospitals across the United States. The speed and accuracy of residents in documenting electronic health records has been insufficiently addressed.
Methods
We studied resident typing skills at New York Methodist Hospital. Participating residents typed a standard 100-word alphanumerical paragraph of a patient's medical history. Typing skills were assessed by calculating the net words per minute (WPM). Typing skills were categorized as follows: (1) fewer than 26 net WPM as very slow; (2) 26 to 35 net WPM as slow; (3) 35 to 45 net WPM as intermediate; and (4) greater than 45 net WPM as fast. Residents were further categorized into (1) American medical graduates; (2) American international medical graduates; and (3) non-American international medical graduates.
Results
A total of 104 of 280 residents (37%) participated in the study. There was equal representation from various specialties, backgrounds, and all postgraduate levels of training. The median typing speed was 30.4 net WPM. Typing skills were very slow (34 of 104, 33%), slow (28 of 104, 27%), intermediate (29 of 104, 28%), and fast (13 of 104, 12%) among the residents. Typing skills of non-American international medical graduates (mean net WPM of 25.9) were significantly slower than those of American medical graduates (mean net WPM of 35.9) and American international medical graduates (mean net WPM of 33.5).
Conclusions
Most residents (60%, 62 of 104) who participated in the study at our institute lacked typing skills. As the use of electronic health records increases, a lack of typing skills may impact residents' time for learning and patient care.
Introduction
Electronic health records (EHRs) are replacing handwritten records in hospitals across the United States. The US Office of the National Coordinator for Health Information Technology intends to implement EHRs nationwide.1 Physicians, including residents and fellows, enter much of their patients' medical information into EHRs. Lack of typing skills could result in added time required for documentation, if residents type fewer than 31 words per minute (WPM), which is the average handwriting speed.2
Montague and Asan3 evaluated the percentage of typing out of total communication time of 100 medical consultations involving 10 primary care physicians, by using videotaped observation. To our knowledge, no studies address the typing skills of residents. We assessed resident typing skills at New York Methodist Hospital (NYMH). Our hypothesis was that residents lack necessary typing skills.
Methods
All residents (N = 249) and fellows (N = 31) at NYMH were invited in person or via e-mail to voluntarily participate in the study. We collected the following demographic data: specialty, postgraduate year (PGY)-1 to PGY-7, citizenship, and the country where participants attended medical school. Participants were also asked when they learned to type (before high school/during high school/college/other) and whether they learned on a typewriter or a computer.
Residents were asked to rate their typing skills as slow (< 30 WPM), intermediate (31–45 WPM), or fast (> 45 WPM), and to indicate importance they assigned to typing for a resident (not important/somewhat important/very important). Participating residents were given a typing test, either in person or online, with a paragraph containing 100 alphanumeric words of a patient history.
The in-person typing portion of the assessment was recorded in seconds by a researcher using a stopwatch. Custom software that calculates typing speeds (Techforis Inc, Nashua, NH) was used for the online typing tests. Gross WPM were calculated from these data, and net WPM were calculated by subtracting errors (net WPM = gross WPM − number of errors). Residents' typing skills were categorized as follows: (1) fewer than 26 net WPM = very slow; (2) 26 to 35 net WPM = slow; (3) 35 to 45 net WPM = intermediate; and (4) greater than 45 net WPM = fast.
Resident participants were categorized into American medical graduates (AMGs); American international medical graduates (AIMGs); and non-American international medical graduates (IMGs). Typing skills were compared across AMGs, AIMGs, and IMGs. Skill levels were also compared between senior and junior, and male and female residents.
This study was approved by the Institutional Review Board of NYMH.
Statistical analysis was performed by using STATA statistical software version 12.1 (Stata Corp LP, College Station, TX). Various responses were collected, tabulated, summarized, and analyzed by using the appropriate statistical tests. P < .05 was considered significant.
Results
Thirty-seven percent (104 of 280) of residents participated in the study. Of the 104 residents, 66 participated online and 38 took the test in person. There was equal representation of male (47%) and female (53%) residents from various specialties, backgrounds, and PGY levels. There was equal distribution of AMGs (36%), AIMGs (29%), and IMGs (36%).
Thirty-four residents (33%) reported that they learned typing before high school, 37 (36%) during high school, and 33 (32%) in college and beyond. Those who learned typing before high school were faster than the other groups (62% [21 of 34] of this group had intermediate or fast skills) followed by the high school group (43% [16 of 37] of this group had intermediate or fast skills). Residents who learned after high school had the lowest typing skills (15% [5 of 33] of this group had intermediate skills; none had fast skills; P = .001).
Residents indicated that they had learned to type on computers (89%, 89 of 104), typewriters (9%, 9 of 104), and both computers and typewriters (2%, 2 of 104). They also agreed that good typing skills were important in their careers. Sixty percent (62 of 104) said it is very important, 38% (40 of 104) said it is somewhat important, and 2% (2 of 104) said typing skills are not important in their careers.
Results showed that most of the residents described themselves as having intermediate and fast typing skills; however, only 9 of 29 (31%) received a fast typing skills assessment on the typing test. For residents who self-reported slow typing skills, the test results were consistent with their self-classification. However, there was fair agreement (38%, P = .002) between the personal rating of typing and the typing skill level assigned by testing.
The median gross WPM was 36.3 with a median of 6 errors, giving a median net WPM of 30.4. Sixty percent (62 of 104) of the residents had slow or very slow typing skills, 28% (29 of 104) had intermediate typing skills, and 12% (13 of 104) had fast typing skills.
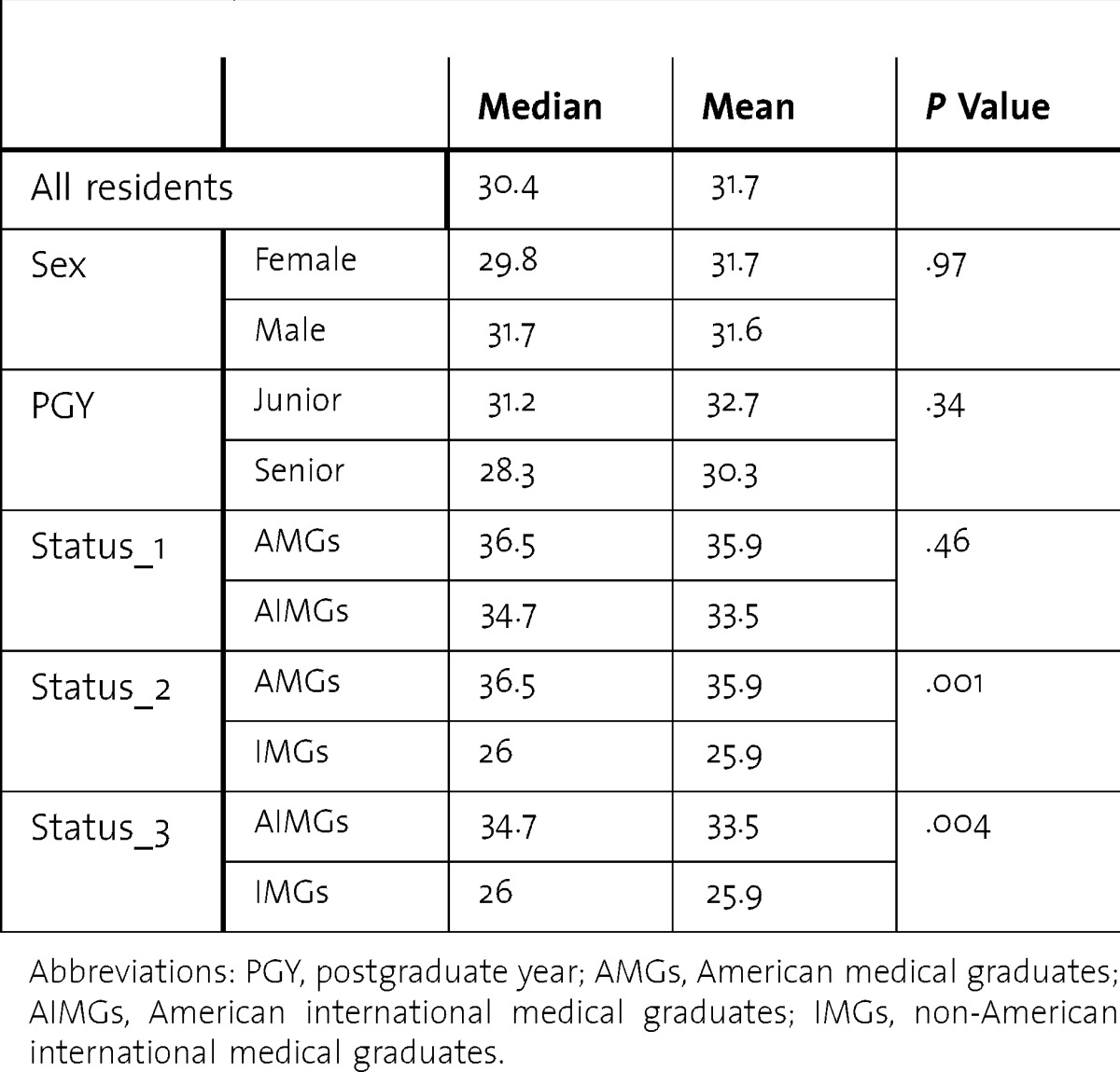
There was no difference in typing skills between male and female residents, senior and junior residents, and AMGs and AIMGs. Typing skills for most IMGs were significantly slower than their American counterparts (table).
TABLE.
Comparison of Typing Skills Among Residents
Discussion
To our knowledge, this is the first study that analyzed the typing proficiency of residents in the United States, where there is an ever-increasing use of EHR and a need for residents to type quickly and accurately. Our results show that there is a significant deficiency in the typing skills among the residents who participated.
IMGs in particular seem to be deficient in their typing skills when compared to their American counterparts. This could be due to lack of training in their home nations; it may also relate to the potential deficits in their English language skills. Identifying residents with slow or very slow typing skills early and instituting measures to improve skills may be helpful.
Typing involves fine motor skills, best learned between ages 6 and 12.4 Copy-texting is usually slower than typing memorized material.5 Our analysis involved copy-typing and reflects speeds that are likely to be slightly less than the actual typing speeds of these residents.
Adequate typing skills may need to be evaluated as part of medical school or residency curriculum. Curriculum additions may include providing protected time for resident practice sessions and making typing practice software available to residents. Future research should analyze typing skills for residents across multiple institutions and trends in typing skills over time.
Our study has several limitations. We did not use a standardized keyboard to test typing skills; however, residents used their own computers to complete the typing assessment (25.5KB, doc) . Also, the environment in which the resident performed the test was not standardized. The results may not be generalized to other institutions.
Conclusion
The sizable proportion of the residents who participated in our study lacked essential typing skills. As the use of EHRs increases, this lack of typing skills, if widespread, may reduce residents' time for learning and patient care.
Footnotes
All authors are at New York Methodist Hospital, except Ms Bronshteyn. Arun Kalava, MD, is Chief Resident, Anesthesiology; Sapna Ravindranath, MD, is Resident, Anesthesiology; Inessa Bronshteyn, BA, is a Student, Ross University School of Medicine; Ripudaman S. Munjal, MBBS, is Research Assistant; Joseph SchianodiCola, MD, is Chairman, Anesthesiology; and Joel M. Yarmush, MD, MPA, is Residency Program Director, Anesthesiology.
The authors would like to thank all the physicians in training at New York Methodist Hospital who participated in the study; Venkat Avvaru, President, Techforis Inc, Nashua, New Hampshire; Adel Guirguis, MD, MS, Biostatistician, New York Methodist Hospital, for his help with statistical data analysis; and Elliot Yung, MD, Attending Anesthesiologist, New York Methodist Hospital, for reviewing the manuscript.
Funding: This study was supported by the New York Methodist Hospital Department of Anesthesiology Research Fund.
References
- 1.Bush GW. 2004. Executive order: 13335: Incentives for the Use of Health Information Technology and Establishing the Position of the National Health Information Technology Coordinator; [Google Scholar]
- 2.Brown CM. Human-Computer Interface Design Guidelines. Norwood, NJ: Ablex Publishing; 1988. [Google Scholar]
- 3.Montague E, Asan O. Considering social ergonomics: the effects of HIT on interpersonal relationships between patients and clinicians. Work. 2012;41(suppl 1):4479–4483. doi: 10.3233/WOR-2012-0748-4479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stallings LM. Motor Skills: Development and Learning. Boston, MA: WCB/McGraw-Hill; 1973. [Google Scholar]
- 5.Inhoff AW. Word frequency during copytyping. J Exp Psychol Hum Percept Perform. 1991;17(2):478–487. doi: 10.1037//0096-1523.17.2.478. [DOI] [PubMed] [Google Scholar]


