Abstract
Background
Intensive care unit (ICU) use at the end of life is rising. Little research has focused on associations among critical care fellows' training, institutional support, and bedside tools with ICU use at the end of life.
Objective
We evaluated whether hospital and critical care medicine program interventions were associated with ICU use in the last 6 months of life for patients with chronic illness.
Methods
Our observational, retrospective study explored associations between results from a survey of critical care program directors and hospital-level Medicare data on ICU use in the last 6 months of life. Program directors evaluated quality of palliative care education in their critical care fellowships and reported on the number of bedside tools and the presence or absence of an inpatient palliative care consultation service.
Results
For the 89 hospitals and 71 affiliated training programs analyzed, there were statistically significant relationships between 2 of the explanatory variables—the quality of palliative care education and the number of bedside tools—in ICU use. Each level of increased educational quality (1–5 Likert scale) was associated with a 0.57-day decrease in ICU days, whereas, for each additional, evidence-based bedside tool, there was a 0.31-day decrease. The presence of an inpatient palliative care program was not a significant predictor of ICU use.
Conclusions
We found that the quality of palliative care training in critical care medicine programs and the use of bedside tools were independently associated with reduced ICU use at the end of life.
What was known
There is increasing intensive care unit (ICU) use by patients at the end of life.
What is new
Data on whether critical care medicine program interventions, focused on the quality of palliative care training and beside tools, are independently associated with ICU use in the last 6 months of life for patients with chronic illness.
Limitations
Subjective definition used for the quality of palliative care education.
Bottom line
Reduced ICU use at the end of life was associated with the quality of palliative care training and the use of bedside tools.
Introduction
A rising proportion of end-of-life care takes place in the intensive care unit (ICU). Nearly 30% of Medicare patients used the ICU in their last month of life, increased from 24% a decade ago.1 Patients and families may opt for a treatment trial in an ICU when faced with progressive illness necessitating critical care because prognosis and mortality can be difficult to predict.2,3 The ICU is an important setting for end-of-life decision making, and critical care physicians play a crucial role in those decisions.
However, intensive care use at the end of life varies widely by hospital, suggesting that factors other than disease severity and patient preferences affect ICU use.4 Hospital and medical education leaders have worked to address concerns about the increasing amount and significant variation in end-of-life ICU use. Individual institutions have developed and evaluated a variety of interventions that include a more proactive approach to the provision of palliative care, educational initiatives targeting ICU staff, and bedside tools for communication and symptom management.5–8 Researchers have also implemented and evaluated multisite, controlled trials.9,10 The Accreditation Council for Graduate Medical Education (ACGME) requires palliative and end-of-life care training for critical care medicine fellows.11
Research assessing factors associated with the quantity of end-of-life ICU care at the state and national levels has focused on structural variables.12 In contrast, provider behavior theory suggests that provider characteristics, such as the tools to enhance the patient encounter and institutional support, can independently influence practice.13 To our knowledge, no studies have addressed training program initiatives and their influence on subsequent ICU use at the end of life.
The objective of our study was to evaluate how factors consistent with the provider behavior theory13 at the critical care medicine training program level, including quality of palliative care education, evidence-based bedside tools, and availability of a palliative care consultation service, affect ICU use in the last 6 months of life for Medicare patients with chronic illnesses.14 Previous research has used the last 6 months of life to assess hospital variation in end-of-life care use.14,15
Methods
Study Design
We conducted a cross-sectional study to identify associations between the results of a survey by the American College of Chest Physicians Palliative and End-of-Life Care NetWork (PEOLC NetWork) and hospital-level Medicare data. This survey assessed quality of education and competencies for palliative and end-of-life care, educational and practice tools, and characteristics of respondents and training programs. Questions were iteratively developed and piloted by members of the PEOLC NetWork committee to assess construct and content validity. The questions were pilot-tested with clinicians in training programs; subsequent interviews helped improve questions for increased comprehension and reliability. The survey was e-mailed to all program directors in the Association of Pulmonary and Critical Care Medicine Program Directors. The PEOLC NetWork members made up to 3 follow-up attempts (e-mail and telephone) to improve response rates. Additional details related to methods and results were previously presented (unpublished data).
Variable Selection
We chose explanatory variables from the PEOLC NetWork survey based on a modified version of the Quality Enhancement Research Initiative's health care provider behavior model.13 That theoretical model identifies distinct elements that influence provider behavior, including provider characteristics (such as education), tools to influence the patient encounter, and organizational support. Our version focused on intervention components that could be implemented by local leadership. Each of these elements has been shown to influence patient outcomes and has provided the basis for multifaceted interventions in critical care.7,9,16–18
We identified specific survey questions a priori that were related to our 3 elements: (1) quality of provider education, (2) evidence-based bedside tools for the patient encounter, and (3) institutional support (inpatient palliative care consultation service [IPCCS]). We used program director survey responses about the overall quality of palliative care education in their training program to characterize the education element. Previous work has shown good correlation between program directors' perspectives and externally validated metrics.19 To quantify evidence-based support to affect the patient encounter, we identified bedside tools published in the medical literature.18,20,21 The identified tools included a family booklet,22 a point-of-care communication card,17 withdrawal of life-sustaining treatment protocol,20 a bereavement brochure,17 and a comfort measure order set.21 The survey questions identified the presence or absence of these evidence-based tools, and the number present within the program was counted with a possible range of 0 to 5. We selected the availability of an IPCCS as a yes or no proxy for institutional support.
Using Dartmouth Atlas23 methodology, we identified our dependent variable as hospital-level ICU days in the last 6 months of life for patients who had previous hospitalization with at least 1 chronic condition (box) in the previous 2 years. Our sample included patients who died between January 1, 2003, and December 31, 2007. We chose a 6-month window to best incorporate repeat hospitalizations. Patients who are admitted to the ICU typically have a decompensation that can trigger new conversations about goals of care and care limitations.24,25 Such conversations may affect future ICU use for patients who survive. This 6-month window has been previously used to assess hospital-level variation at the end of life.14 Considering Medicare patients hospitalized in the last 2 years of life with at least 1 of 9 chronic conditions is a commonly used method to identify those who may be more amenable to care limitations.14,23 Patients were assigned to the hospital where they had the most admissions.
Box Chronic Condition Diagnoses
Malignant cancer, leukemia
Chronic pulmonary disease
Coronary artery disease
Congestive heart failure
Peripheral vascular disease
Severe chronic liver disease
Diabetes with end organ damage
Chronic kidney disease
Dementia
Program and Hospital Selection
Medical critical care and pulmonary/critical care programs were identified through the ACGME website.26 We searched each program's website to identify nonfederal hospitals where trainees performed critical care rotations. For programs with multiple nonfederal hospital affiliations, we specifically identified the hospitals where trainees provide critical care medicine. Federal hospitals (ie, VA and Department of Defense) were excluded because they lack available Medicare data. We accessed the Dartmouth Atlas website27 and obtained the corresponding hospital-level data for ICU days in the last 6 months of life.
We classified training programs as responders or nonresponders. Responders completed at least 2 of the 3 questions on our independent variables from the NetWork survey.
The VA Greater Los Angeles Healthcare System Institutional Review Board approved the study protocol and waived the need for consent.
Analysis
Descriptive analyses of the 3 independent variables were performed based on both individual program results and associated hospital results because some training programs provided critical care for more than 1 hospital. We analyzed descriptive statistics of hospital-level ICU days in the last 6 months of life and assessed whether a linear model was acceptable or transformation was needed. A histogram revealed the presence of an outlier (SD = 4.8 from the mean and not the program's main teaching hospital), which was removed. Student t tests compared responding and nonresponding institutions' ICU days in the last 6 months of life.
Univariate analyses were performed using ordinary least squares to evaluate for associations. From those, we developed a multivariate regression model, using our 3 identified variables, and tested for multicollinearity. Sensitivity analyses were performed with bootstrapping and multiple imputations to assess the effect of missing variables, including responders who only answered 2 of the 3 questions. Statistical analyses were performed using Stata Statistical Software version 11 (StataCorp LP, College Station, TX).
Results
Our response rate was 49% (82 of 167 ACGME programs, encompassing 184 affiliated hospitals). Of those, we excluded 4 programs because they lacked data from the Dartmouth Atlas and excluded another 7 because they did not respond to at least 2 of the 3 survey questions. A total of 71 programs and 89 affiliated hospitals were used in the analysis.
Patients associated with responder hospitals had a mean of 4.84 (95% confidence interval [CI] = 4.38–5.30) ICU days in their last 6 months of life, whereas similar patients in nonresponder hospitals had a mean of 5.32 (95% CI = 4.80–5.85) ICU days. Student t tests showed no difference in ICU days between responder and nonresponder hospitals.
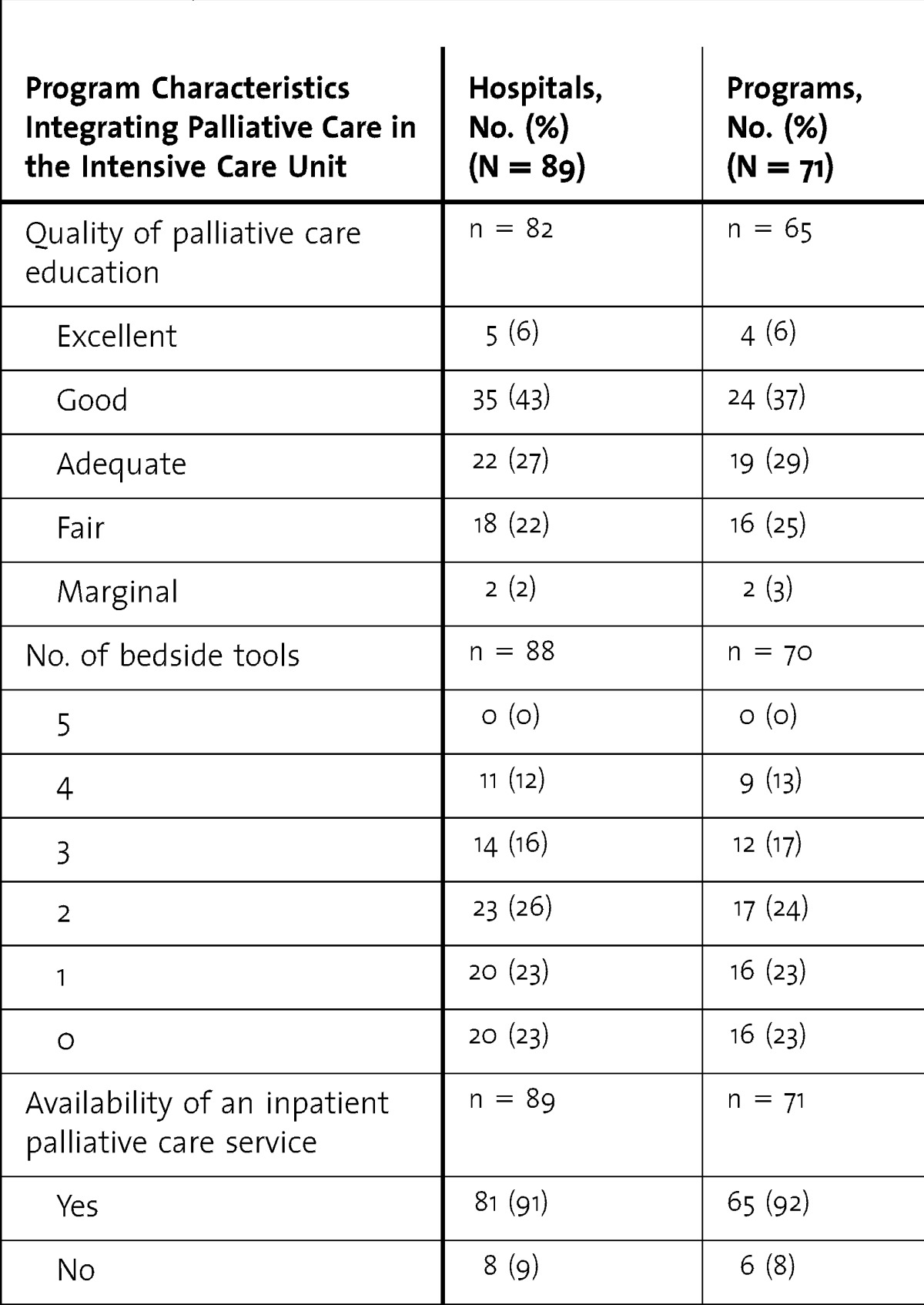
Characteristics of the 3 selected components of palliative care in the responder training programs and affiliated hospitals are shown in table 1. The distribution of the overall quality of education had a mean (SD) score of 3.2 (1). Most of the programs and hospitals had 2 or fewer bedside tools available, with a range of 0 to 4 (table 1). More than 90% (81 of 89) of the hospitals had an IPCCS.
TABLE 1.
Characteristics of Hospitals and Training Programs as Rated by Critical Care Program Directors
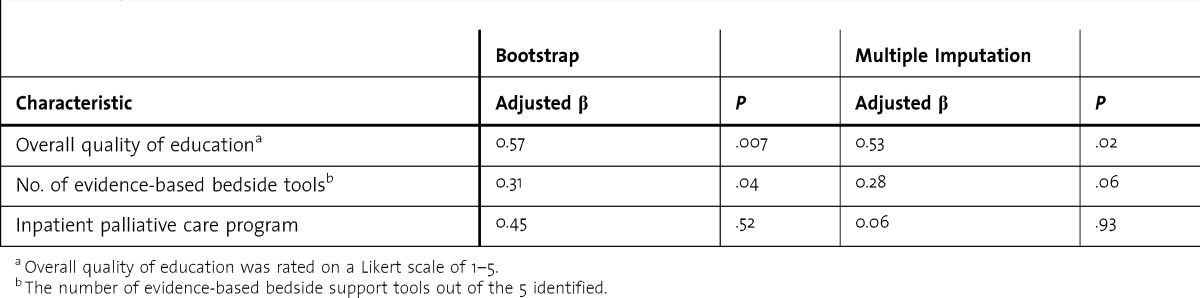
Our univariate evaluation of program and hospital characteristics identified statistically significant associations with ICU use at the end of life (table 2). Multicollinearity analysis revealed no significant correlation between the 3 independent variables: quality of education, number of evidence-based bedside tools, and availability of an IPCCS (r < 0.1). Our multivariate regression model showed that for each additional improvement in the rating level of education quality there was a 0.57 ICU-day decrease mean per patient (P = .007), whereas, for each additional report of any of 5 evidence-based bedside tools, there was a 0.31 ICU-day decrease mean per patient (P = .02). The availability of an IPCCS was not associated with a significant difference in ICU days (table 3). These results were supported by sensitivity analyses, assessing variance, and missing data with multiple imputation (table 4).
TABLE 2.
Univariate Analysis of Hospital-Level Program Characteristics and Intensive Care Unit (ICU) Use During the Last 6 Months of Life
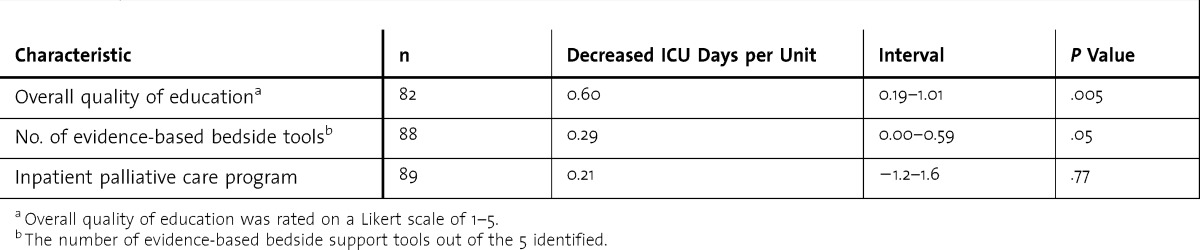
TABLE 3.
Characteristics' Influence on Intensive Care Unit (ICU) Days in the Last 6 Months of Life in a Multivariate Linear-Regression Model
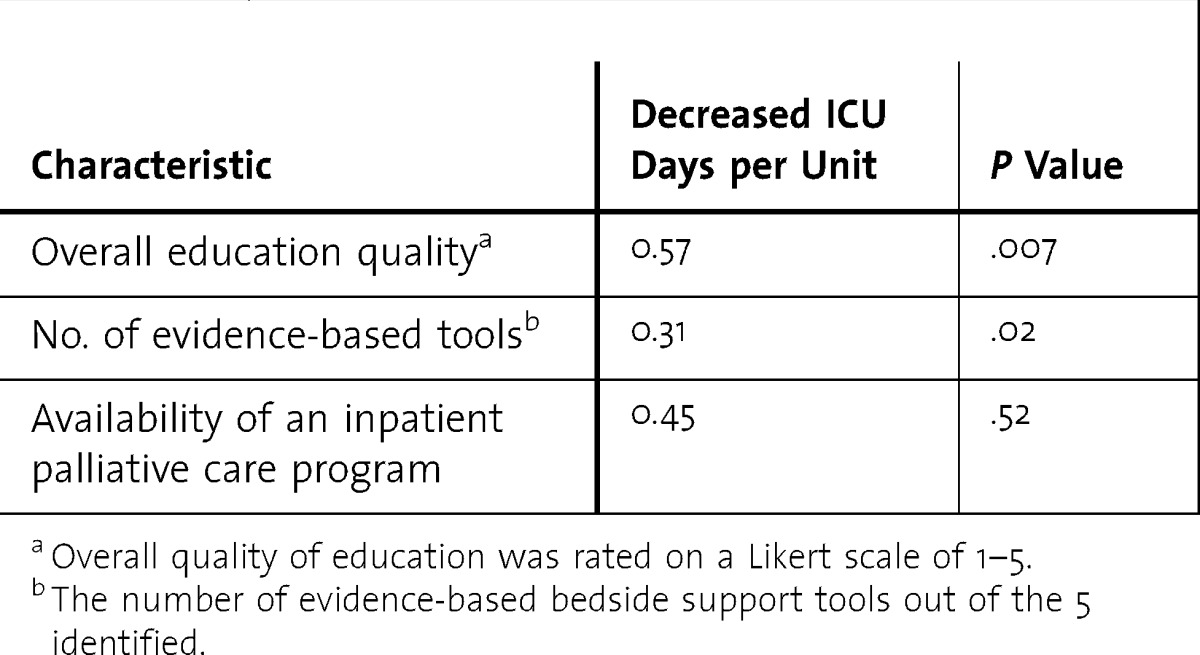
TABLE 4.
Sensitivity Analysis of Program Characteristics Influencing Decrease in Intensive Care Unit (ICU) Days During the Last 6 Months of Life
Discussion
Our findings demonstrate that the quality of palliative care education in critical care medicine training programs, as perceived by the program directors, and the number of evidence-based bedside tools were independently associated with reduced ICU use in the last 6 months of life in the same program. In contrast, availability of an IPCCS was not significantly associated with end-of-life ICU use. To our knowledge, this is the first cross-sectional study to evaluate the effect of either educational quality or availability of practice bedside assistance tools in training programs for ICU clinicians as they occur within their natural environment. Our results are consistent with design theory highlighting the importance of combining bedside tools to enhance the practice of critical care physicians and quality of education related to palliative care.13
One possible explanation for the strong effect of these components is their organic relationship to the training program. Unlike trials of educational interventions, our study captures organizational elements that were internally motivated and locally driven9 and that were likely designed to fit the needs of the local environment.28 Our observational study of effectiveness of behavioral interventions in the actual program settings may be more generalizable than previous randomized, controlled trials.29 Authors of a recent, randomized, controlled trial suggested the lack of locally driven and customized support as a potential reason that intervention did not show a reduction in length of ICU stay.9
The lack of an association with IPCCS was unexpected and may be due to a high rate of IPCCS among the participating programs. An IPCCS is increasingly available and has been shown to influence ICU use at the end of life,7,8,30,31 but its high prevalence (>80%) in our sample reduced our ability to detect differences. Additionally, we do not have information about how an IPCCS is integrated into the ICU.
Our study had several limitations. We used program directors' perceptions to measure the quality of education. Our study was limited in its ability to assess the effect of potential confounders on ICU use, including race, socioeconomic status of patients, hospital competition,12 availability of inpatient hospice beds, or information on the presence of a hospitalist program. Furthermore, the cross-sectional nature of our study did not provide detailed information on how often the bedside tools were used, whether and with which health care professional the patients completed their advanced directives, or how often the IPCCS was consulted. In training programs that staffed ICUs at multiple hospitals, we assumed that each hospital had a similar number of bedside tools and availability of an IPCCS. We also assumed that patients with chronic illnesses were typically cared for by medical intensivists at the end of life. Other training programs that focus on postsurgical care, anesthesia, and surgery may have skewed results.
Conclusion
Our study showed that in an actual fellowship setting, both the quality of palliative care education and the number of available bedside tools were independently associated with reduced ICU use at the end of life. The potential benefits of improving critical care physicians' palliative care training and availability of bedside tools should be considered by critical care program directors. Future research should evaluate other potentially beneficial outcomes of palliative care training, such as the quality of death and dying,32 family satisfaction,33 and psychological outcomes.
Footnotes
Howard L. Saft, MD, MSHS, is Assistant Professor, Division of Pulmonary and Critical Care, David Geffen School ofMedicine, University of California, Los Angeles, and the VA Greater Los Angeles Healthcare System; Paul S. Richman, MD, is Assistant Professor, Division of Pulmonary and Critical Care Medicine, Stony Brook University; Andrew R. Berman, MD, is Associate Professor of Clinical Medicine, New Jersey Medical School; Richard A. Mularski, MD, MSHS, MCR, is Investigator and Adjunct Associate Professor of Medicine, Center for Health Research, Kaiser Permanente Northwest; Paul A. Kvale, MD, is Master FCCP, Henry Ford Health System; Daniel E. Ray, MD, is Chief, Section of Palliative Medicine and Hospice Medicine, Lehigh Valley Medical Center; Paul Selecky, MD, is Medical Director of Respiratory Care, Hoag Memorial Hospital; Dee W. Ford, MD, MSCR, is Associate Professor of Medicine, Medical University of South Carolina; and Steven M. Asch, MD, MPH, is Director of Health Services Research & Development Center for Innovation to Implementation, VA Palo Alto Health Care System.
Funding: The VA Health Services Research and Development postdoctoral training grant provided salary and statistical support for Dr Saft.
The authors would like to thank Lee Ann Fulton, BS, Project Manager at the Chest Foundation, for her efforts in providing data from the survey; Tranh Huong, PhD, Jack Needleman, PhD, Andrew Barnes, PhD, and the UCLA Academic Technology Services Statistical Consulting group for their statistical guidance; and Lynn O. Peterson, MA, for her assistance with manuscript preparation.
References
- 1.Teno JM, Gozalo PL, Bynum JP, Leland NE, Miller SC, Morden NE, et al. Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309(5):470–477. doi: 10.1001/jama.2012.207624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Curtis JR. Caring for patients with critical illness and their families: the value of the integrated clinical team. Respir Care. 2008;53(4):480–487. [PubMed] [Google Scholar]
- 3.Ong MK, Mangione CM, Romano PS, Zhou Q, Auerbach AD, Chun A, et al. Looking forward, looking back: assessing variations in hospital resource use and outcomes for elderly patients with heart failure. Circ Cardiovasc Qual Outcomes. 2009;2(6):548–557. doi: 10.1161/CIRCOUTCOMES.108.825612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wennberg JE, Fisher ES, Stukel TA, Skinner JS, Sharp SM, Bronner KK. Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States. BMJ. 2004;328(7440):607. doi: 10.1136/bmj.328.7440.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnold R, Nelson J, Prendergast T, Emlet L, Weinstein E, Barnato A, et al. 2010. Educational modules for the critical care communication (C3) course—a communication skills training program for intensive care fellows. http://www.capc.org/palliative-care-professional-development/Training/c3-module-ipal-icu.pdf. Accessed October 29, 2013. [Google Scholar]
- 6.Lilly CM, Sonna LA, Haley KJ, Massaro AF. Intensive communication: four-year follow-up from a clinical practice study. Crit Care Med. 2003;31(suppl 5):394–399. doi: 10.1097/01.CCM.0000065279.77449.B4. [DOI] [PubMed] [Google Scholar]
- 7.Campbell ML, Guzman JA. A proactive approach to improve end-of-life care in a medical intensive care unit for patients with terminal dementia. Crit Care Med. 2004;32(9):1839–1843. doi: 10.1097/01.ccm.0000138560.56577.88. [DOI] [PubMed] [Google Scholar]
- 8.Norton SA, Hogan LA, Holloway RG, Temkin-Greener H, Buckley MJ, Quill TE. Proactive palliative care in the medical intensive care unit: effects on length of stay for selected high-risk patients. Crit Care Med. 2007;35(6):1530–1535. doi: 10.1097/01.CCM.0000266533.06543.0C. [DOI] [PubMed] [Google Scholar]
- 9.Curtis JR, Nielsen EL, Treece PD, Downey L, Dotolo D, Shannon SE, et al. Effect of a quality-improvement intervention on end-of-life care in the intensive care unit: a randomized trial. Am J Respir Crit Care Med. 2011;183(3):348–355. doi: 10.1164/rccm.201006-1004OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Curtis JR, Treece PD, Nielsen EL, Downey L, Shannon SE, Braungardt T, et al. Integrating palliative and critical care: evaluation of a quality-improvement intervention. Am J Respir Crit Care Med. 2008;178(3):269–275. doi: 10.1164/rccm.200802-272OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Accreditation Council for Graduate Medical Education. 2013. ACGME program requirements for graduate medical education in critical care medicine. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/142_critical_care_int_med_07132013.pdf. Accessed January 17, 2014. [Google Scholar]
- 12.Lin CY, Farrell MH, Lave JR, Angus DC, Barnato AE. Organizational determinants of hospital end-of-life treatment intensity. Med Care. 2009;47(5):524–530. doi: 10.1097/MLR.0b013e31819261bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rubenstein LV, Mittman BS, Yano EM, Mulrow CD. From understanding health care provider behavior to improving health care: the QUERI framework for quality improvement. Quality Enhancement Research Initiative. Med Care. 2000;38(6)(suppl 1):I129–I141. [PubMed] [Google Scholar]
- 14.Wennberg JE, Fisher ES, Stukel TA, Skinner JS, Sharp SM, Bronner KK. Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States. BMJ. 2004;328(7440):607. doi: 10.1136/bmj.328.7440.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dartmouth Medical School Center for the Evaluative Clinical Sciences. The Quality of Medical Care in the United States: A Report on the Medicare Program. Chicago, IL: American Hospital Association Press; 1999. Dartmouth Atlas; Cat No. 04401. [Google Scholar]
- 16.Treece PD, Engelberg RA, Shannon SE, Nielsen EL, Braungardt T, Rubenfeld GD, et al. Integrating palliative and critical care: description of an intervention. Crit Care Med. 2006;34(suppl 11):380–387. doi: 10.1097/01.CCM.0000237045.12925.09. [DOI] [PubMed] [Google Scholar]
- 17.Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, Adrie C, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007;356(5):469–478. doi: 10.1056/NEJMoa063446. [DOI] [PubMed] [Google Scholar]
- 18.Nelson JE, Walker AS, Luhrs CA, Cortez TB, Pronovost PJ. Family meetings made simpler: a toolkit for the intensive care unit. J Crit Care. 2009;24(4):626.e7–626.e14. doi: 10.1016/j.jcrc.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Langenau EE, Pugliano G, Roberts WL. Relationships between high-stakes clinical skills exam scores and program director global competency ratings of first-year pediatric residents. Med Educ Online. 2011;16:7362. doi: 10.3402/meo.v16i0.7362. doi: 10.3402/meo.v16i0.7362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Treece PD, Engelberg RA, Crowley L, Chan JD, Rubenfeld GD, Steinberg KP, et al. Evaluation of a standardized order form for the withdrawal of life support in the intensive care unit. Crit Care Med. 2004;32(5):1141–1148. doi: 10.1097/01.ccm.0000125509.34805.0c. [DOI] [PubMed] [Google Scholar]
- 21.Walling AM, Ettner SL, Barry T, Yamamoto MC, Wenger NS. Missed opportunities: use of an end-of-life symptom management order protocol among inpatients dying expected deaths. J Palliat Med. 2011;14(4):407–412. doi: 10.1089/jpm.2010.0328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Azoulay E, Pochard F, Chevret S, Jourdain M, Bornstain C, Wernet A, et al. Impact of a family information leaflet on effectiveness of information provided to family members of intensive care unit patients: a multicenter, prospective, randomized, controlled trial. Am J Respir Crit Care Med. 2002;165(4):438–442. doi: 10.1164/ajrccm.165.4.200108-006oc. [DOI] [PubMed] [Google Scholar]
- 23.Dartmouth Reagents. 2009. The Dartmouth atlas of health care 2008: appendix on methods. http://www.dartmouthatlas.org/downloads/methods/2008_Atlas_Methods.pdf. Accessed June 15, 2013. [Google Scholar]
- 24.Reichner CA, Thompson JA, O'Brien S, Kuru T, Anderson ED. Outcome and code status of lung cancer patients admitted to the medical ICU. Chest. 2006;130(3):719–723. doi: 10.1378/chest.130.3.719. [DOI] [PubMed] [Google Scholar]
- 25.Prendergast TJ, Luce JM. Increasing incidence of withholding and withdrawal of life support from the critically ill. Am J Respir Crit Care Med. 1997;155(1):15–20. doi: 10.1164/ajrccm.155.1.9001282. [DOI] [PubMed] [Google Scholar]
- 26.Accreditation Council for Graduate Medical Education. ACGME website. http://www.acgme.org. Accessed July 20, 2011. [Google Scholar]
- 27.The Dartmouth Institute for Health Policy and Clinical Practice. Care of Chronic Illness in Last Two Years of Life. http://www.dartmouthatlas.org/data/topic/topic.aspx?cat=1. Accessed March 15, 2013. [Google Scholar]
- 28.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Staines GL, Cleland CM. Observational studies versus randomized controlled trials of behavioral interventions in field settings. Rev Gen Psychol. 2012;16(1):37–58. [Google Scholar]
- 30.O'Mahony S, McHenry J, Blank AE, Snow D, Eti Karakas S, Santoro G, et al. Preliminary report of the integration of a palliative care team into an intensive care unit. Palliat Med. 2010;24(2):154–165. doi: 10.1177/0269216309346540. [DOI] [PubMed] [Google Scholar]
- 31.Morrison RS, Penrod JD, Cassel JB, Caust-Ellenbogen M, Litke A, Spragens L, et al. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med. 2008;168(16):1783–1790. doi: 10.1001/archinte.168.16.1783. [DOI] [PubMed] [Google Scholar]
- 32.Curtis JR, Engelberg RA, Wenrich MD, Nielsen EL, Shannon SE, Treece PD, et al. Studying communication about end-of-life care during the ICU family conference: development of a framework. J Crit Care. 2002;17(3):147–160. doi: 10.1053/jcrc.2002.35929. [DOI] [PubMed] [Google Scholar]
- 33.Heyland DK, Tranmer JE Kingston General Hospital ICU Research Working Group. Measuring family satisfaction with care in the intensive care unit: the development of a questionnaire and preliminary results. J Crit Care. 2001;16(4):142–149. doi: 10.1053/jcrc.2001.30163. [DOI] [PubMed] [Google Scholar]


