Abstract
Objectives
To characterize the burden of care and musculoskeletal discomfort associated with caring for adults with chronic physical disability among informal caregivers and to describe the most physically demanding caregiving activities, and contributing factors, as perceived by informal caregivers of adults with physical disabilities.
Methods
A mixed methods approach was used for the study. Forty-six informal caregivers of adults with physical disability participated in the study.
Results
Most of the caregivers were classified as “high burden” caregivers. They reported high levels of physical strain and musculoskeletal discomfort. Caregivers identified several activities related to mobility and self-care as the most physically demanding. Factors affecting physical demand included caregiver and care recipeint characteristics, activity requirements, and the physical environment.
Conclusion
Interventions that specifically target high demand caregiving activities, including all three aspects of caregiving activity performance, are necessary to support, in the home, adults with disabilities and their caregivers.
Keywords: Caregivers, musculoskeletal discomfort, activity performance
Informal (family; unpaid) caregivers provide care to millions of Americans valued at $350 -$375 billion per year (Houser & Gibson, 2008). The care they provide can delay or prevent institutionalization (Mittelman, Haley, Clay, & Roth, 2006), reduce hospital stays (Picone, Wilson, & Chou, 2003), and reduce expenditures for inpatient and long term care services (van Houtven & Norton, 2008). Extensive caregiving, however, has been shown to impact the physical and psychological health of caregivers. Informal caregivers may experience poorer mental health than non-caregivers (Schultz & Sherwood, 2008; Covinsky, Newcomer, Fox, Wood, Sands, Dane, et al., 2003; Haley, LaMonde, Han, Burton, & Schonwetter, 2003, Cannuscio, Jones, Kawachi, Colditz, Berkman, & Rimm, 2002; Yates, Tennstedt, & Chang, 1999). They also may experience poorer physical health (Pinquart & Sorenson, 2003; Vitaliano, Zhang, & Scanlan, 2003), engage in poor health behaviors (Burton, Zdaniuk, Schulz, Jackson, & Hirsch, 2003), and experience higher morbidity and mortality than non-caregivers (Shultz & Beach, 1999). It should not be surprising that declining caregiver physical health is a predictor of cessation of caregiving (McCann, Hebert, Bienias, Morris, & Evans, 2004).
Musculoskeletal health is an important aspect of physical health. Current evidence suggests that caregivers may be at increased risk of musculoskeletal symptoms and injury, perhaps as a result of caregiving duties. In a study of rural, informal caregivers, caregivers described physical symptoms such as fatigue, backache, and headache attributable to their caregiving activities (Sandford, Johnson, & Townsend-Rocchiccioli, 2005). Among informal caregivers of adults with multiple sclerosis, 31% sustained a physical injury due to caregiving and 49% experienced physical exhaustion (NAC, 2012). In their studies of informal caregivers of veterans with stroke, Hayes, Chapman, Young, and Rittman (2009) and Hartke, King, Heinemann, and Semik (2006), found that 24% of informal caregivers sustained injuries while providing care and 30% of informal caregivers experienced accidents such muscle strains, and contusions, respectively.
Injuries in caregivers may be associated with the burden of care. The Level of Care Index, a composite measure of hours of caregiving and assistance with activities of daily living (ADL), provides an estimate of burden of care (NAC, 1997). In 2009, 32% of informal caregivers in the U.S. experienced a “high burden” of care (NAC, 2009). These caregivers were more likely to be age sixty-five or older, were more likely to live with their care recipient, provided an average of 47 hours of care per week, and assisted with an average of three ADL per week (NAC, 2009). Some of the most common ADL included transfers, bathing, and dressing. Among caregivers with the highest burden of care, 83-88% were assisting with these ADL (NAC, 2004). Providing assistance with ADL can require require substantial physical exertion on the part of the caregiver. Not surpsingly, 28% of high burden caregivers reported a high degree of physical strain associated with caregiving activities (NAC, 2009) and Hayes et al. (2009) found that the level of care was a significant predictor of caregiver injury.
Little information has been reported in the literature about the physical demands placed on informal caregivers, and any association with musculoskeletal injury. However, evidence regarding physically demanding activities that place physical strain on professional caregivers is widely available. Transfers, lifts and patient repositioning are associated with musculoskeletal injuries in professional caregivers (e.g. nurses; rehabilitation personnel) (Hui, Ng, Yeung, & Hui-Chan, 2001; Menzel, 2004; Campo, Weiser, Koenig & Nordin, 2008; Nelson, Motacki, & Menzel, 2009; Darragh, Campo, & King, 2012). The biomechanical loads imposed by relatively straight forward transfer activities (e.g. sit-to-stand or stand pivot transfers) can exceed tissue tolerances and increase the risk of injury (Hess, Kincl, & Mandeville, 2007; Marras, Davis, Kirking, & Bertsche, 1999). Exposure to these tasks is one explanation for the high rates of work-related musculoskeletal disorders (MSDs) that occur in paid home health care workers (home health aides), as well as homecare nursing and rehabilitation personnel (Smedley, Egger, Cooper, and Coggon, 1995; Engels, van der Gulden, Senden, and van’t Hof, 1996; Craib, Hackett, Back, Cvitkovich, & Yassi, 2007; Campo et al., 2008; Darragh, Huddleston & King, 2009).
High burden informal caregivers, likely to be older than 65 and living with their care recipient, are vulnerable to injuries. Their injuries may be associated with caregiving tasks and yet few ever receive training in how to perform these tasks efficiently or safely (NAC, 2004). In addition, caregivers provide these services in the home: non-medical, unpredictable environments presenting their own unique challenges for care provision (such as small, cluttered spaces) (Hess et al., 2007). Therefore, it is important to both further define musculoskeletal discomfort and characterize the caregiving tasks that place caregivers at risk.
The current study sought to examine musculoskeletal discomfort, burden of care, and the physical demands associated with caregiving activities among informal caregivers of adults with physical disability. The purpose of the study was to:
Characterize the burden of care and musculoskeletal discomfort associated with caring for adults with chronic physical disability among informal caregivers.
Describe the physically demanding caregiving activities, and the factors associated with that demand, as perceived by informal caregivers of adults with physical disabilities.
Method
Study Design
Multiple methods were used for this study, including both qualitative and quantitative methods. Study participants completed a quantitative, caregiver questionnaire in order to gather demographic information and to characterize burden of care and musculoskeletal discomfort. The questionnaire also included questions about caregiving activities, and served as a reference during the qualitative phase of the study.
The purpose of the qualitative phase of the study was to gain a deeper understanding of the caregving activities that were most physically demanding and the factors that contributed to activity difficulty, from the perspective of informal caregivers. Semi-structured focus groups and individual interviews were used as the method of data collection. The focus group interview was chosen for this study because focus groups emphasize participant interaction, thereby stimulating discussion of important topics, and they are an efficient way to collect data [Morgan, 1988]. The option of individual interviews was added when potential participants expressed difficulty with attending a meeting outside the home during the scheduled time periods. The caregivers were extremely busy, some had no one to cover for them if they left the home, many had unexpected challenges that arose, and some felt more comfortable meeting one-on-one. Individual interviews allowed us to include those caregivers who required this type of flexibility.
Selection and Enrollment of Participants
Purposeful sampling was used to recruit participants who were likely to be providing assistance with ADL. Participants were recruited through word of mouth and through informational flyers distributed through local hospitals, rehabilitation centers, community agencies and community support groups. Eligibility was determined through telephone screening. Informal caregivers met the following inclusion criteria: 1) caregiving for an adult with an adult-onset, chronic physical disability affecting mobility, 2) serving as a family caregiver for at least 3 months; and 3) sharing a residence with the care recipient. Those caring for an adult whose primary diagnosis was a chronic mental illness or dementia (without mobility impariment) were excluded. Study team members explained the purpose of the study and all procedures to potential participants at the time of contact, and determined eligibility acccording to the inclusion/exclusion criteria specified above. Interested and eligible participants were then scheduled for a group or individual interview.
This study was approved by the Institutional Review Boards of the authors’ universities. All participants reviewed and signed informed consent documents. Participants received a $40 gift card for their participation.
Assessments and Measures
Questionnaire
Participants completed a written, caregiver questionnaire to obtain information about the individual for whom they were caring (e.g. diagnosis, age, weight), their personal health (e.g. diagnoses that may contribute to musculoskeletal discomfort), and background information (e.g. the number of hours they provided caregiving each week). They also provided the information necessary to characterize burden of care and musculoskeletal discomfort.
To describe the burden of care experienced by study caregivers, we assessed caregiver level of care, physical strain, emotional stress, and the amount of assistance care recipients provided during activity performance. Level of care was calculated based on the Level of Care Index established by the NAC/AARP (NAC, 1997). The NAC/AARP Level of Care Index assigns caregivers to one of five levels of care, with level 1 being least intense and level 5 being most intense, based on a combined score derived from the number of hours they provide care each week and the number of activities of daily living (ADL) and instrumental activities of daily living (IADL) with which they provide assistance. Activities of daily living and IADL were recorded on an Activity Table, a list of caregiving activities whose items were dervied from the NAC/AARP study and a review of the literature. Caregivers also answered questions regarding the emotional stress and physical strain they experienced, using a 5-point Likert scale (no stress/strain to extreme stress/strain) also based on the NAC/AARP study.
In order to characterize the musculoskeletal discomfort experienced by caregivers of adults with chronic physical disability, study participants answered questions on the questionnaire about musculoskeletal discomfort, using a modified version of the Nordic Musculoskeletal Questionnaire (Kuorinka, Jonsson, and Kilbom, 1987) on which they reported discomfort severity (measured on a 0 – 10 point scale), the body part in which discomfort was experienced, symptoms they felt were related to their caregiving activities, and the effects of musculoskeletal discomfort on work, caregiving and life activities. Discomfort was defined as an ache, pain, discomfort, burning, numbness, tingling, or other symptom.
Focus groups and individual interviews
To conduct the interviews, investigators used a facilitator’s guide, which was developed based on their prior work and the relevant research literature. Both the guide and the questionnaire were reviewed by an advisory panel of researchers and service providers for feedback. The guide was designed to engage the participants in a discussion regarding the types of caregiving activities performed, with an emphasis on the strenuous routine activities, the methods they used to complete the activities, and the musculoskeletal discomfort associated with those activities.
To characterize the physicality of caregiving activities, participants provided in-depth explanations of the most difficult activities they performed. Study participants were able to discuss any activity they chose, referring to the Activity Table they completed in the questionnaire if necessary. When additional clarification was necessary, the investigators asked follow up questions about the steps involved in the activity, equipment, frequency and duration of the activity in order to fully understand the process. Participants also were asked what they felt made the activity difficult, and any musculoskeletal discomfort they experienced related to caregiving activities.
Procedures
Forty-seven eligible participants were invited to participate in a focus group or individual interview. The focus group interviews occurred in community locations, such as local library meeting rooms or community centers. Individual interviews occurred at a location specified by the participant, typically in the participant’s home. One interview involved two individuals caring for the same person. There were five focus group interviews (with a total of 27 people) and twenty individual interviews. Each participant was interviewed only once.
Each focus group interview included between two and nine participants and lasted approximately two hours. Individual interviews lasted from one to two hours. Each session began with introductions, and the investigators provided background information about their credentials, experience and rationale for the research study. Participants completed the questionnaire at the start of the session. At least two investigators experienced with focus group research facilitated each group discussion; individual interviews were conducted with either one or two interviewers present. One investigator served as the lead, or primary, facilitator. The others used probes to follow up or clarify comments made by the participants. This is particularly useful in group interviews to manage multiple streams of conversation. The groups were audio-recorded, transcribed, and checked for accuracy.
Data Analysis
Analysis procedures
All questionnaire data were analyzed with descriptive statistics, including median, inter-quartile range, and percentages, using SPSS v 19 (IBM-SPSS, 2010). A qualitative approach was used to analyze the focus group and individual interviews. In order to identify physically demanding caregiving activities consistently, an activity coding structure was developed using definitions of activities of daily living (ADL) and instrumental activities of daily living (IADL) from the Occupational Therapy Practice Framework (OTPF) (AOTA, 2008). In order to characterize the factors that contributed to activity difficulty, a coding structure was derived from the textual data. In both cases, the investigators used a method of constant comparison, in which codes are compared to the structure throughout the analysis, and modified as necessary [Glaser and Strauss, 1967], to ensure that the textual data were represented accurately by the coding scheme. As a result, several changes were made to the activity coding structure during the analysis. Wound care was added, and was defined as ‘assisting with the care of surgical wounds, infections, and pressure sores’. Falls also were added to the coding structure, and were defined as ‘assisting the care recipient during or after a fall, including catching, repositioning, or lifting up from the floor’.This was added as a separate category because it was identified specifically by caregivers, and could occur during any activity. Bowel and bladder management, which included incontinence, was collapsed into toilet hygiene.Transfers that occured during toileting, which were included in both the OTPF definition of transfer and of toilet hygiene, were coded as transfers. In addition, the codes included in the ADL “functional mobility” were assigned to subcategories of ambulation, transfers, repositioning, and stairs.
Two investigators coded the transcripts independently to identify the activites that were identified as physically difficult and to characterize the aspects of the activity performance that contributed to physical demand. They compared codes during consensus meetings with the third investigator, who maintained the audit trail, reviewed their coding, challenged coding decisions, facilitated the process of consensus, and helped establish the final coding scheme. The final coding scheme was verified with an uncoded interview to be sure it captured the information correctly. NVivo v 9 (QSR International Pty Ltd, 1999-2011) was used to organize the data and aid in the process of coding the interviews.
Strategies to increase trustworthiness
In order to improve the trustworthiness of the results, multiple verification strategies were used during the study. At least two investigators were present during the focus groups to ensure all perspectives were captured and questions were not asked in a leading or biased manner. The individual interviews were conducted with one or two interviewers present, depending on the participant’s level of comfort and the necessity of flexible scheduling. Reflexivity, bracketing, and peer checking, were used during the analyses to reduce bias and improve trustworthiness [Lincoln and Guba, 1985]. Investigators reflected on their own biases prior to the analysis. These biases were then discussed, bracketed and set aside. Triangulation of analysts was used during the analysis: textual data were analyzed by two investigators separately. They then met with the third analyst, who maintained the role of peer reviewer, to reflect on their conclusions, draw comparisons, facilitate consensus, and modify categories or themes as necessary. An audit trail documenting the process of analysis was maintained.
Results
Participant and Care Recipient Characteristics
A total of 47 individuals participated in the study (Table 1). The questionnaire and responses of one participant were excluded when it became apparent during the interview that her care recipient did not have any mobility impairments. The final sample included 46 caregivers. Most caregivers were women (89%) and most care recipients were men (65%), typically a spouse or parent. Over 90% of the participants were either White or African American. Almost 70% reported an annual household income of 49,000 dollars or less. The diagnoses of the care recipients varied widely (Table 1). Though many had more than one diagnosis, all had at least one medical condition that resulted in chronic physical disability and mobility impairment.
Table 1.
Selected Demographic and Background Characteristics of Study Participants & Care Recipients
| Characteristic | Caregiver n (%) |
Care Recipient n (%) |
|---|---|---|
| Sex (n=46) | ||
| Female | 41 (89.1) | 16 (34.8) |
| Male | 5 (10.9) | 30 (65.2) |
| Age (n=46) | ||
| 18 – 29 | 2 (4.4) | |
| 30 – 44 | 1 (2.2) | 3 (6.5) |
| 45 – 54 | 7 (5.2) | 4 (8.7) |
| 55 – 64 | 10 (21.7) | 5 (10.9) |
| 65 – 74 | 7 (15.2) | 13 (28.3) |
| 75 – 84 | 15 (32.6) | 15 (32.6) |
| 85 – 89 | 7 (15.2) | 2 (4.4) |
| 90+ | 2 (4.4) | |
| Caring for (n=45): | ||
| Spouse or partner | 25 (55.6) | |
| Parent | 11 (24.4) | |
| Child | 1 (2.2) | |
| Friend | 3 (6.7) | |
| Sibling | 2 (4.4) | |
| Unknown | 3 (6.7) | |
| Ethnicity/Race (n=46) | ||
| White/Caucasian | 23 (50.0) | |
| African American | 19 (41.3) | |
| Asian | 3 (6.5) | |
| Did not report | 1 (2.2) | |
| Diagnoses* | ||
| Neurological | 48 | |
| Orthopedic | 33 | |
| Cardiac/Respiratory | 25 | |
| Medical | 22 | |
| Duration of Care (n=44) | ||
| <1 year | 5 (11.4) | |
| 1 – 4 years | 21 (47.7) | |
| 5+ years | 18 (40.9) | |
| Annual Household Income (n=42) | ||
| Less than $30,000 | 17 (40.5) | |
| $30,000 – $49,000 | 12 (28.6) | |
| $50,000 – $99,000 | 10 (23.8) | |
| More than $100,000 | 3 (7.1) |
Neurological diagnoses include ALS, stroke, dementia, post-polio; Orthopedic diagnoses include amputation, arthritis, hip dysplasia, fibromyalgia, fracture, joint replacement, spine fusion; Cardiac/Respiratory diagnoses include COPD, CHF, HTN; Medical diagnoses include cancer, diabetes, decubiti, surgery unspec, Marfan syndrome
Study participants primarily resided in urban and suburban areas; 80% lived in single-family homes, 11% lived in apartments, 7% lived in multi-family homes and 1 participant lived in a condo. Of these, 52% lived in a home with 2 or more levels and 48% lived in a one-level home, with or without a basement. Study participants described a number of home modifications they made, often in response to the recommendations of health care professionals (Table 2)
Table 2.
Home Modifications and Equipment Present in the Home of Informal Caregivers
| Equipment and Home Modification | n (%) |
|---|---|
| Installed grab bars | 25 (54.3) |
| Removed throw rugs | 25 (54.3) |
| Removed interior rugs | 5 (10.9) |
| Moved furniture | 20 (43.5) |
| Added shower chair/bath bench | 25 (54.3) |
| Added raised toilet seat | 20 (43.5) |
| Added floor lift | 6 (13.0) |
| Added hospital bed | 9 (19.6) |
| Installed a ramp | 13 (28.3) |
| Widened doorways | 3 (6.5) |
| Installed a ceiling lift | 1 (2.2) |
| Modified the bathroom | 10 (21.7) |
| Modified the kitchen | 5 (10.9) |
Burden of Care
More than half (53%) of the study participants provided more than 20 hours per week of care. Seventy-three percent met the criteria for a Level of Care Index 4 or 5, representing the highest burden of care (Table 3). Study participants reported emotional and physical stress associated with caregiving: 58% reported high to very high emotional stress and 38% reported high to very high levels of physical strain associated with caregiving activities (Table 3). When asked to estimate the amount of assistance their care recipients were able to provide during caregiving activities, 65% reported that their care recipients were able to perform 50% or less of the activity. Forty-five percent reported that they received no assistance from another caregiver (paid or unpaid).
Table 3.
The Frequency Distribution of the Level of Care Burden Reported by the Study Participants
| Care Burden | n (%) |
|---|---|
| Level of Care (n=40) | |
| 1 (Least intense) | 4 (10.0) |
| 2 | 2 (5.0) |
| 3 | 5 (12.5) |
| 4 | 18 (45.0) |
| 5 (Most intense) | 11 (27.5) |
|
| |
| Emotional Stress (n=45) | |
| 1 (No stress) | 4 (8.9) |
| 2 | 7 (15.6) |
| 3 | 8 (17.8) |
| 4 | 12 (26.7) |
| 5 (Very high stress) | 14 (31.1) |
| Physical Strain (n=45) | |
| 1 (No strain) | 10 (22.2) |
| 2 | 8 (17.8) |
| 3 | 10 (22.2) |
| 4 | 7 (15.6) |
| 5 (Very high strain) | 10 (22.2) |
Musculoskeletal Discomfort
Ninety-four percent of study participants reported musculoskeletal discomfort in at least one body part during the preceding four weeks and 79% perceived that caregiving either caused or made their symptoms worse (Table 4). Eighty-two percent experienced musculoskeletal discomfort in more than one body part in the preceding 4 weeks. The low back was the most commonly reported site of musculoskeletal discomfort, reported by approximately three-fourths of the participants (76%). Over half reported that their symptoms affected work, caregiving, and other life activities (Table 4).
Table 4.
Reported Musculoskeletal Discomfort Prevalence and Severity in Study Participants
| Musculoskeletal Discomfort Severity and Body Part (0 – 10 scale) |
Discomfort Present in Past 4-weeks n (%) |
4-week Severity (Typical) Median (IQR) |
4-week Severity (Peak) Median (IQR) |
|---|---|---|---|
| Any Body Part (n=46) | 43 (93.5) | ||
| Discomfort in Multiple Body Parts (n=43) | 37 (81.8) | ||
| Low Back | 35 (76.1) | 5.0 (7.0-4.0) | 7.0 (8.0-5.0) |
| Knee | 20 (43.5) | 5.0 (5.5-3.5) | 6.0 (8.0-3.5) |
| Shoulder | 20 (43.5) | 4.0 (5.5-3.0) | 6.5 (8.0-4.0) |
| Wrist/Hand | 20 (43.5) | 3.0 (5.0-2.5) | 5.0 (7.0-3.0) |
| Neck | 19 (41.3) | 4.5 (6.0-3.5) | 6.0 (7.0-5.0) |
| Hip/Thigh | 14 (30.4) | 5.0 (7.0-3.0) | 7.0 (8.0-2.5) |
| Ankle | 13 (28.3) | 5.0 (7.0-5.0) | 7.0 (9.0-5.0) |
| Elbow/Forearm | 8 (17.4) | 5.0 (5.0-4.0) | 5.5 (8.0-2.0) |
| Upper Back | 8 (17.4) | 4.0 (5.0-4.0) | 5.5 (7.5-1.5) |
| Musculoskeletal Discomfort and Caregiving |
Impact n (%) |
|---|---|
| Caregiving Exacerbates MSD | 33 (78.6) |
| MSD Impacts Work | 20 (54.1) |
| MSD Impacts Caregiving | 22 (56.4) |
| MSD Impacts Life | 26 (66.7) |
Among caregivers reporting symptoms, the median four week discomfort severity on the 0 to 10 point scale (10 being the highest rating) ranged between 3 in the wrist and hand and 5 for several other body parts such as the low back and knee (Table 4). These caregivers also reported peak severity, which reached a level of 7 in the low back, ankle, and elbow/forearm.
Caregiving Activities
On the questionnaire, caregivers identified multiple caregiving activities they performed on a regular basis (Table 5). Transfers, bathing, and dressing were the most frequently identified ADL for which caregivers provided assistance. Study participants provided assistance for multiple IADL. At least 60% of study participants provided help with community mobility, financial management, grocery shopping, health management, home management, meal preparation, and medication management.
Table 5.
The Percentage of Respondents Who Reported Specific ADL and IADL Tasks Associated With Caring for an Adult with Chronic Physical Disability*.
| n (%) | |
|---|---|
| Activities of Daily Living (ADL) | |
|
| |
| Bathing/Showering | 36 (78.3) |
| Dressing | 30 (65.2) |
| Feeding | 11 (23.9) |
| Functional Mobility | |
| Transfers (getting in and out of beds and chairs) | 29 (63.0) |
| Repositioning (moving up or down in bed or wheelchair) | 17 (37.0) |
| Ambulating (getting to and from the toilet) | 15 (32.6) |
| Stairs (going up or down stairs inside the home) | 19 (41.3) |
| Toileting: Incontinence/Use of a bed pan | 23 (50.0) |
|
| |
| Instrumental Activities of Daily Living (IADL) | |
|
| |
| Arranging or supervising services | 21 (45.7) |
| Community Mobility (transportation to appointments, elder care) | 37 (80.4) |
| Financial Management (paying bills or filling out insurance claims) | 35 (76.1) |
| Grocery Shopping | 43 (93.5) |
| Health Management | |
| Assisting with home therapy programs | 23 (50.0) |
| Giving medicines, injections; blood sugar testing | 28 (60.9) |
| Scheduling and/or attending care recipients medical appointments | 39 (84.8) |
| Home management (housework) | 44 (95.7) |
| Meal Preparation | 41 (89.1) |
| Medication management | 39 (84.8) |
This information is derived from the caregiver questionnaire.
In addition to caregiving tasks identified on the questionnaire, our qualitative analyses of focus group and interview transcripts were also able to determine the activities that were the most physically demanding. These included transfers, falls, bathing, toilet hygiene (including incontinence; colostomies), and stairs. Transfers were identified more often than any other activity, and included, in order of frequency of identification, toilet transfer, into and out of bed, tub/shower transfer, out of/up from chair, car, and those involving a wheelchair. For a complete list of activities cited by respondents in focus groups or interviews, see Table 6.
Table 6.
Caregiving Activities Identified as Physically Demanding*
| Activity | Frequency (n) |
|---|---|
|
| |
| Transfers | 43 |
| Toilet | 11 |
| Into and Out of Bed | 11 |
| Tub/Shower | 8 |
| Out of/Up from Chair | 5 |
| Car | 5 |
| Wheelchair | 3 |
| Falls (picking up from, catching, etc) | 11 |
| Bathing | 9 |
| Toilet Hygiene | 8 |
| Stairs | 7 |
| Repositioning | 6 |
| Ambulate | 5 |
| Dressing | 5 |
| Home Establishment and Management | 5 |
| Community Mobility | 5 |
| Wheelchair Mobility | 3 |
| Wound Care | 2 |
| Leisure | 2 |
| Personal Hygiene and Grooming | 1 |
| Feeding | 1 |
| Meal preparation and Cleanup | 1 |
| Shopping | 1 |
These items were derived from the group and individual interviews
Several themes regarding activity demand emerged from the data: Caregiver-Care Recipient Characteristics and Relationship, the Physical Requirements of the Caregiving Activities, and the Characteristics of the Physical Environment. The process of caregiving is a shared activity, involving the participation of both the caregiver and the care recipient. Therefore, codes for care recipient characteristics and caregiver characteristics were combined into one theme. The physicality of caregiving activities was influenced by the characteristics of both caregiver and care recipient, as well as by the caregiver’s understanding of the likes and preferences of their care recipient. The Physical Requirements of the Caregiving Activities included the methods used, positions required for, and the frequency and duration of the activity. Finally, the Characteristics of the Physical Environment influenced activity performance, including factors such as the amount of space available, the layout, and other physical features of the home.
The themes and their interactions are reflected in Figure 1. Person-centered characteristics were mentioned most frequently as contributing to physical demand, followed by factors related to activity requirements and then physical environment. The frequency with which these are mentioned may or may not reflect the relative importance of each contribution, so we have represented each theme in an equally-sized circle.
Figure 1.
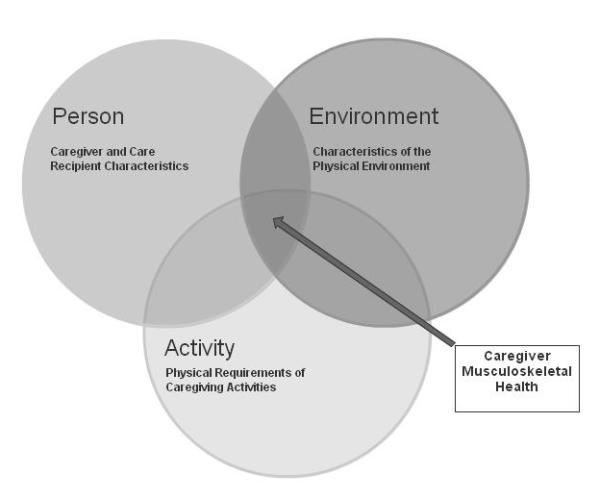
Factors affecting the physical demands on informal caregivers when performing caregiving activities
Theme 1: Caregiver-care recipient characteristics and relationship
Characteristics of the care recipient that affected activity performance included the extent to which they were able to assist with the activity, their functional mobility, overall strength or endurance, and cognitive ability.
Physical limitations increased the difficulty of the caregiving activity, “Well, she has a, she’s a diabetic and she has a broken leg so, and she’s overweight, so I just have to figure out how to turn her to one side, bathe her on that side.” In other instances, the cognitive or behavioral characteristics of the care recipient affected the physical demand of the activity.
“What makes it really difficult is because his last stroke has affected his cognition, temper, um, you know, causes him to not you know cooperate or he gets confused and he doesn’t move the way he needs to, it’s just like you know you do something a thousand times, it’s just like you have to re-teach it every time like it’s new …
The care recipient’s ability to assist during the activity was also a factor in caregiver strain,
“When I pick him up once he’s fallen and I have to pick him up, you know he’s dead weight and we struggle with that.”
The characteristics or actions of the caregiver contributed to or influenced activity performance. Caregivers experienced physical difficulty because of factors such as decreased strength, endurance, injury and/or pain. Several caregivers described their own health conditions that influenced care. They had conditions that were exacerbated by the activities of caregiving:
“I before had chronic, from like swimming years ago and sitting at a computer all of our lives now, I mean its chronic, but it’s when I lift him and stuff it just triggers …”
Others described symptoms or injuries that they believed were at least in part associated with caregiving itself.
“I did have a torn rotator cuff and we don’t know whether it happened when care giving or happened at a different time because by the time that I was… it didn’t start really bothering me until I was doing the lifting and stuff last year with him.”
The relative size of care recipient and caregiver also contributed to activity difficulty. “Probably bathroom issues absolutely. As a whole, personal care with somebody that’s a lot bigger than you are is really tough.”
It is important to note that some of the decisions the caregivers made about task performance were based on their understanding of the likes, dislikes, or preferences of the care recipient:
“She likes to smell good so I have to put her a little spray on her, then I get her up and get her in her chair, change her bed and I sprinkle powder in her bed cause she like that”
This participant commented on her husband’s willingness to allow outside help, “Yeah, he doesn’t like 911 (laughs) so I had to pick him up or get my neighbor.”
Theme 2: The physical requirements of the caregiving activities
The physical requirements of the activity contributed to overall perception of demand. Activities, such as transfers, were perceived as difficult when they involved lifting or moving the care recipient, “I had to help her stand up”. Caregiving activities also were physically hard because caregivers assumed awkward and/or sustained postures
“We’ll get, it’s like you want to be careful so you’re getting your body in awkward positions so they don’t fall.”
“… it was the exhaustion of staying there for longer than you would have ever been inclined to do on your own …”
They also were bending, lifting, and pulling to complete the activity and to maintain the care recipient’s safety, movements they reported as fatiguing and painful.
Participant 1: “ … he has a balance problem so you’re not only adjusting the clothes or putting them on and off, you’re…also holding him at the same time so …”
Participant 2: “You know, and we’re bending around and down and it’s…”
Participant 1: “It’s a lot of… It’s exhausting.”
In addition, factors such as activity complexity, the number of times it was performed each day, and the length of time it took to complete each influenced physical demand. One woman described the process of giving her mother a bed bath, which included carrying water and supplies to the bed, bathing her, applying powder, dressing her, and mopping the floor. Not only was the activity complex, it took approximately one hour and 20 minutes, and she performed it every other day. Similarly, toilet hygiene associated with incontinence was another activity that included multiple components, including dressing, undressing, changing adult incontinence pads, and possibly cleaning the person if they were soiled. This could occur multiple times in a day:
“There’s times when he’s gone so much in the [adult incontinence pads] that we have to completely take everything off sometimes we have to change everything … and, um, of course getting down to take the stuff off and putting the stuff back on four or five times a day.”
Some activities occurred many times during the day, in the context of multiple activities. One woman transferred her husband in and out of the wheelchair for a total of ten transfers each day. These included transfers between the wheelchair and the toilet, and transfers between the wheelchair and the bed.
Wheelchairs in particular were identified as difficult, both to maneuver and transport. This participant struggled to push the wheelchair up the ramp into their home.
“But pushing him up that ramp is, I have a hard time and … it’s 200 pounds, trying to go up.”
Others described the challenges associated with lifting the wheelchair, for example, down the stairs or, as in the example below, in and out of the car.
“Actually the wheelchair was more hard [than a scooter] because it’s one big, big piece … even though they’re semi-light they’re still heavy.”
Theme 3: Characteristics of the physical environment
Environmental factors included small, cramped spaces, stairs, narrow corridors, and clutter.
“Showering is awfully hard, awfully hard … because of the physical limitations of our small bathroom … um, we have to get ourselves out of the way in order to get him into the tub.”
Environmental modifications can be helpful, but are not always present in all areas of the home, as illustrated below:
Participant: “… We have one toilet upstairs that has the grab bars on it but the one downstairs doesn’t so …
Interviewer: “So do you have to help her stand up then afterwards?”
Participant: “Sometimes, yeah”
Thematic interactions
It is important to consider that these aspects of activity performance interact, and that these interactions influence the physical demand of caregiving. Interactions between characteristics of the caregiver and care recipient and the requirements of the activity are one way that task difficulty increased. One caregiver (below) describes how her physical symptoms (caregiver characteristics), combined with the task of showering (activity requirements) being “too much” on her and her mother (care recipient characteristics), resulted in changing the task to a bed bath (activity requirements).
“My mostly physical demand of being tired or my body feels real achy or tired is when I bathe her because like I put in my paper that when I first started I was bathing her, I was giving her a bath in the shower, I was showering her. Now it’s too much on her and me to do it in the shower, so I bed bath, bathe her now. And that’s a lot of work.”
In another example, the following caregiver describes how the presence of an accessible bathroom on an upper level (environment) combined with her care recipient’s need for assistance on the stairs (care recipient characteristic) and an inefficient activity method involving lifting his legs while bending over (activity requirements) illustrates the importance of acknowledging these interactions
Participant: “If he decides he wants to go up (the stairs), I’ll help him up but I have to lift one leg at a time for him to go up because he can’t, his legs are so heavy he can’t lift them.”
Interviewer: “So if he goes up the stairs you lift his legs? So what are you doing, sitting on the stairs and lifting his legs up?”
Participant: “No I’m not, I’m just bending down and lifting his legs up and he has a walker at the top of the stairs.”
All four aspects of activity performance combine in the example below, in which the caregiver transports her care recipient (care recipient characteristic) down the stairs (environment), five times a week (activity frequency) on her back (activity method), in the home,
“I usually hold him on my back. I usually put his arms over my shoulders and that’s the only way I can do it. That’s the only way I can have the strength, because if I try to lift him this way I couldn’t do it so I just put him on back and kind of lean over like that, he’s probably dragging his legs I know. But that’s about the only way I can do it.”
Discussion
The purpose of the study was twofold: to characterize the burden of care and musculoskeletal discomfort of caregivers of adults with physical disability and to characterize the caregiving activities that are perceived as physically demanding or difficult.
As compared to U.S. caregivers in general, the sample of caregivers in the present study represent a distinct group of older (63% were 65 years or older compared to 13% of U.S. caregivers), co-resident (all compared to 29% of U.S. caregivers), primary caregivers. A higher proportion of these caregivers reported lower incomes (42% with annual household incomes of less than $30,000/year compared to 22% of U.S. caregivers), described themselves as African American (43% as compared to 13% of U.S. caregivers), and had been providing care for five or more years (40% compared to 32% of U.S. caregivers) (NAC, 2009).
Study participants in this sample experienced substantial burden of care, especially when compared to U.S. caregivers in general. Over one-third reported high or very high physical strain associated with caregiving, over half reported high emotional stress, and about three-quarters were classified as having high burden on the Level of Care Index. More caregivers in this study reported a high level of physical strain (38%) compared to the caregivers in the most recent NAC survey (14%) but closely matched those identified by NAC as more at risk for reporting high strain: older, primary, co-resident caregivers with a high burden index who provide 21+ hours of care per week (NAC, 2009). More study participants described caregiving as highly stressful (57%) than U.S. caregivers (31%) but, similar to physical strain, study caregivers met many of the NAC descriptors for those who experienced more emotional stress: female, providing 21+ hours of care, and have the role of primary caregiver (NAC, 2009). Study participants also were more likely to be classified as experiencing a high burden of care (73% in the present study compared to 32% of U.S. caregivers) (NAC, 2009).
It is evident that this study represents a group of particularly vulnerable caregivers performing complex and intense care, whose needs may be different from the population of caregivers in general. While physical demand was the focus here, this subset of caregivers may experience stressors in addition to physical demand that could impact their health and perceptions of the caregiving experience, and that were not explored. A recent study by Reinhard, Levine, & Samis (2012) examined complex caregiving and the performance of medical/nursing tasks. Caregivers in their study identified tasks that were hard for any reason, not just physically, and identified incontinence, medication management, wound care, and preparing special diets as the hardest tasks (Reinhard, Levine, & Samis, 2012). Managing incontinence, included here under toilet hygiene, also was one of the most frequently identified tasks in the present study. Participants attributed physical difficulty to clothing management, frequency of performance, awkward positioning, and exertion. Wound care was performed by a minority of participants in the present study, but the participants who performed this task described complex dressing changes performed in awkward positions for long durations,
“ … the problem I found was bending over the bed because he’s in a queen size bed and um, just the odd angles of taking care of that … it took me about two hours a day for the wounds on his torso, and then it took me about an hour in the evening for the wound on his arm.”
Medication management and preparation of special diets were frequently identified as hard in Reinhard et al., but not as physically demanding in the present study. However, it must be noted that 85% of caregivers in the present study reported that they were managing medication, and 61% reported that they were performing tasks such as giving injections, testing blood sugar, and administering medication. While these tasks may not be physically demanding, there is no doubt they are complicated, time consuming, and stressful. This adds an interesting and important dimension to caregiver burden, and the effects of performing tasks that are complex for reasons of frequency, duration, skills required, as well as physical difficulty, on caregiver health may need more definition and exploration.
Among caregivers in the present study, 94% reported musculoskeletal discomfort. Most caregivers reported that their symptoms were either caused by or made worse by caregiving activities. The activities they described are similar to the activities associated with musculoskeletal disorders in healthcare personnel, transfers in particular. Transfers were identified as physically demanding more often than any other activity. Transfers are associated with musculoskeletal disorders in nursing and rehabilitation personnel (Menzel et al., 2004, Campo et al., 2008; Darragh et al, 2012). Given the musculoskeletal burden associated with transferring individuals requiring moderate or maximal assist (care recipient requires more than 50% assistance with an activity), this result is not surprising (Marras et al., 1999).
Participants also reported that assisting with activities such as toileting and bathing, climbing stairs, and assisting care recipients off the floor after a fall were physically difficult. These tasks required the caregiver to assume awkward postures and/or overexert themselves while assisting a care recipient with physical and/or cognitive disabilities, often multiple times per day, and in a challenging environment. The same factors have been associated with work-related injuries in paid caregivers. Awkward postures and overexertion are well-established risk factors for the development of work-related musculoskeletal disorders (NIOSH, 1997). Patient characteristics such as the inability to follow directions, combative or aggressive behaviors, level of dependence, or unpredictable movements may place healthcare workers at risk of injury (Waters, 2007). The frequency and duration of transfers and lifting activities also are associated with increased risk of injury (Waters, 2007; Campo et al., 2008).
Finally, the home environment presents unique circumstances for the performance of tasks that also place healthcare workers at risk, such as small, cluttered spaces (Waters, 2007). For example, among home health aides (paid caregivers working in the home) over 8,070 injuries involving days away from work were reported in 2010 (BLS, 2010). Over 29,000 injuries involving days away from work were reported among nurses, occupational and physical therapists in 2010, and patients and the environment are identified as the source of injury in approximately 60% of injuries and illnesses experienced by healthcare workers (BLS, 2010). The family caregiver faces the same challenges as the paid caregiver, yet receives little training or support, and many are providing care services in excess of 40 hours per week. It is worth noting that challenges with care persisted even though many of the caregivers in this study reported that they had installed equipment and made modifications to the home presumable with the intent of easing the burden of care. Further investigation of the usefulness and limitations of the equipment and modifications is warranted.
Study Limitations
The caregiver-care recipient relationship is intense, complex, and multi-dimensional. While it was beyond the scope of this study to examine all aspects of this relationship, it is possible that some influences on the physical difficulties experienced by the caregivers were missed. For example, a deeper investigation of the nature of the relationship between caregiver and care recipient would add an additional, and important, perspective to this topic. Additionally, we had a small sample of a very specific group of caregivers, so generalization will be limited.
Recommendations for Future Research
The results of the present study reveal the necessity for interventions directed at reducing the physical demands of caregiving, including assessment of caregiver, care recipient, the activities performed, and the caregiving environment. Study participants experienced high physical strain and moderate to severe musculoskeletal discomfort, which was either caused or exacerbated by their caregiving activities. They represent a particularly vulnerable subgroup of caregivers who provide intense, demanding, and long-term care, distinguishing them from caregivers in general. Interventions directed at their specific needs can be developed using the model described here (Figure 1). Interventions must be tailored to the individual needs of the care recipient and caregiver and account for the activity requirements and physical environment. This type of individualized, targeted approach is supported by current systematic reviews of caregiver interventions, which argue that interventions should be grounded in a theoretical model, based on individualized needs, include activities relevant to the caregivers’ daily lives, and involve active participation of clients (Glasdam, Timm, & Vittrup, 2010; Smith, Forster, & Young, 2009; Visser-Meily, van Heugten, Post, Schepers, & Lindeman, 2005). It is also important to note that health care providers, such as nurses, physical therapists and occupational therapists, are often the professionals visiting patients and their caregivers at home. These professions should consider the demands placed on caregivers as they make recommendations about activity performance and home modification.
Conclusions
Informal caregivers experience significant musculoskeletal discomfort that they attribute to caregiving activities. These symptoms interfere with their ability to provide caregiving, as well as to work and participate in life activities. Interventions currently emphasize cognitive-behavioral and psychosocial approaches designed to address quality of life, mental health, and, in some cases, global physical health. Interventions that specifically target activity performance, including all three aspects of caregiving activity performance, are necessary to support, in the home, adults with disabilities and their caregivers.
Acknowledgments
The authors would like to acknowledge Jesse Cook and Tierney Bumgardner for their assistance with study management, focus groups and interviews. Both were Master of Occupational Therapy students at The Ohio State University, School of Health and Rehabilitation Sciences at the time of the study.
The project described was supported by award number 8UL1RR025755 from the National Center for Research Resources, funded by the Office of the Director, National Institutes of Health (OD) and supported by the NIH Roadmap for Medical Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health
Contributor Information
Amy R. Darragh, School of Health and Rehabilitation Sciences The Ohio State University 453 W 10th Avenue Columbus, OH 43210 (614) 292-0370.
Carolyn M. Sommerich, Integrated Systems Engineering & School of Health and Rehabilitation Sciences The Ohio State University.
Steve A. Lavender, Integrated Systems Engineering & Orthopaedics The Ohio State University.
Kelly J. Tanner, School of Health and Rehabilitation Sciences The Ohio State University.
Kasey Vogel, School of Health and Rehabilitation Sciences The Ohio State University.
Marc Campo, Division of Health Professions Mercy College.
References
- American Occupational Therapy Association Occupational therapy practice framework: Domain and process (2nd Edition) American Journal of Occupational Therapy. 2008;62(6):625–683. doi: 10.5014/ajot.62.6.625. [DOI] [PubMed] [Google Scholar]
- Burton LC, Zdaniuk B, Schulz R, Jackson S, Hirsch C. Transitions in spousal caregiving. The Gerontologist. 2003;43(2):230–241. doi: 10.1093/geront/43.2.230. [DOI] [PubMed] [Google Scholar]
- Campo M, Weiser S, Koenig KL, Nordin M. Work-related musculoskeletal disorders in physical therapists: A prospective cohort study with 1-year follow-up. Physical Therapy. 2008;88(5):608–619. doi: 10.2522/ptj.20070127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannuscio CC, Jones C, Kawachi I, Colditz GA, Berkman L, Rimm E. Reverberations of family illness: A longitudinal assessment of informal caregiving and mental health status in the nurses’ health study. American Journal of Public Health. 2002;92(8):1305–1311. doi: 10.2105/ajph.92.8.1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covinsky KE, Newcomer R, Fox P, Wood J, Sands L, Dane K, et al. Patient and caregiver characteristics associated with depression in caregivers of patients with dementia. Journal of General Internal Medicine. 2003;18(12):1006–1014. doi: 10.1111/j.1525-1497.2003.30103.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craib KJP, Hackett G, Back C, Cvitkovich Y, Yassi A. Injury rates, predictors of workplace injuries, and results of an intervention program among community health workers. Public Health Nursing. 2007;24(2):121–131. doi: 10.1111/j.1525-1446.2007.00616.x. [DOI] [PubMed] [Google Scholar]
- Darragh AR, Huddleston W, King P. Work-related musculoskeletal injuries and disorders among occupational and physical therapists. American Journal of Occupational Therapy. 2009;63(3):351–362. doi: 10.5014/ajot.63.3.351. [DOI] [PubMed] [Google Scholar]
- Darragh AR, Campo M, King P. Work-related activities associated with injury in occupational and physical therapists in five practice areas. Work: A Journal of Prevention, Assessment, and Rehabilitation. 2012;42(3):373–384. doi: 10.3233/WOR-2012-1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engels JA, Van der Gulden JWJ, Senden TF, van’t Hof B. Work-related risk factors for musculoskeletal complaints in the nursing profession: Results of a questionnaire survey. Occupational and Environmental Medicine. 1996;53:636–641. doi: 10.1136/oem.53.9.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasdam S, Timm H, Vittrup R. Support efforts for caregivers of chronically ill persons. Clinical Nursing Research. 2010;19(3):233–265. doi: 10.1177/1054773810369683. [DOI] [PubMed] [Google Scholar]
- Glaser BG, Strauss AL. The discovery of grounded theory: Strategies for qualitative research. Aldine; Chicago: 1967. [Google Scholar]
- Haley WE, LaMonde LA, Han B, Burton AM, Schonwetter R. Predictors of depression and life satisfaction among spousal caregivers in hospice: Application of a stress process model. Journal of Palliative Medicine. 2003;6:215–224. doi: 10.1089/109662103764978461. [DOI] [PubMed] [Google Scholar]
- Hartke RJ, King RB, Heinemann AW, Semik P. Accidents in older caregivers of persons surviving stroke and their relation to caregiver stress. Rehabilitation Psychology. 2006;51(2):150–156. [Google Scholar]
- Hayes J, Chapman P, Young LJ, Rittman M. The prevalence of injury for stroke caregivers and associated risk factors. Topics in Stroke Rehabilitation. 2009;16(4):300–307. doi: 10.1310/tsr1604-300. [DOI] [PubMed] [Google Scholar]
- Hess JA, Kincl LD, Mandeville DS. Comparison of three single-person manual for bed-to-wheelchair transfers. Home Healthcare Nurse. 2007;25(9):572–575. doi: 10.1097/01.NHH.0000296114.33696.e5. [DOI] [PubMed] [Google Scholar]
- Houser A, Gibson MJ. Valuing the invaluable: The economic value of family caregiving, 2008 update. 13. AARP Public Policy Institute; 2008. [PubMed] [Google Scholar]
- Hui L, NG GYF, Yeung SSM, Hui-Chan CWY. Evaluation of physiological work demands and low back neuromuscular fatigue on nurses working in geriatric wards. Applied Ergonomics. 2001;32:479–483. doi: 10.1016/s0003-6870(01)00025-4. [DOI] [PubMed] [Google Scholar]
- Kuorinka I, Jonsson B, Kilbom A, et al. Standardized nordic questionnaires for the analysis of musculoskeletal symptoms. Applied Ergonomics. 1987;18:233–237. doi: 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- Lincoln YS, Guba EG. Naturalistic Inquiry. Sage; Beverly Hills, CA: 1985. [Google Scholar]
- Marras WS, Davis KG, Kirking BC, Bertsche PK. A comprehensive analysis of low-back disorder risk and spinal loading during the transferring and repositioning of patients using different techniques. Ergonomics. 1999;42:904–926. doi: 10.1080/001401399185207. [DOI] [PubMed] [Google Scholar]
- McCann JJ, Hebert LE, Bienias JL, Morris MC, Evans DA. Predictors of beginning and ending caregiving during a 3-year period in a biracial community population of older adults. American Journal of Public Health. 2004;94(10):1800–1806. doi: 10.2105/ajph.94.10.1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menzel NN. Back pain prevalence in nursing personnel: Measurement issues. American Association of Occupational Health Nurses Journal. 2004;52(2):54–65. [PubMed] [Google Scholar]
- Mittelman MS, Haley WE, Clay OJ, Roth DL. Improving caregiver well-being delays nursing home placement of patients with Alzheimer Disease. Neurology. 2006;67(9):1592–1599. doi: 10.1212/01.wnl.0000242727.81172.91. [DOI] [PubMed] [Google Scholar]
- Morgan DL. Qualitative Methods #16. Sage Publishing; Thousand Oaks: (188) [Google Scholar]
- National Alliance for Caregiving & American Association of Retired Persons Family caregiving in the U.S.: Results of a national survey. 1997 Retrieved from http://www.caregiving.org/pdf/research/finalreport97.pdf.
- National Alliance for Caregiving & American Association of Retired Persons Caregiving in the U.S., 2004. 2004 Retrieved from http://www.caregiving.org/pdf/research/04finalreport.pdf.
- National Alliance for Caregiving & American Association of Retired Persons Caregiving in the U.S., 2009. 2009 Retrieved from http://www.caregiving.org/pdf/research/Caregiving_in_the_US_2009_full_report.pdf.
- National Alliance for Caregiving Multiple Sclerosis Caregivers. 2012 Retrieved from http://www.caregiving.org/pdf/research/MSCaregivers2012_FINAL.pdf.
- Nelson AL, Motacki K, Menzel N. Safe patient handling and movement. Springer Publishing Company, LLC; New York, NY: 2009. [Google Scholar]
- Picone G, Wilson MR, Chou SY. Analysis of hospital length of stay and discharge destination using hazard functions with unmeasured heterogeneity. Health Economics. 2003;12(12):1021–1034. doi: 10.1002/hec.800. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sorensen S. Correlates of physical health of informal caregivers: A meta-analysis. Journal of Gerontology. 2007;62B(2):P126–P137. doi: 10.1093/geronb/62.2.p126. [DOI] [PubMed] [Google Scholar]
- Reinhard SC, Levine C, Samis S. Home alone: Family caregivers providing complex chronic care. AARP Public Policy Institute; [Retrieved on 4/11/2013]. 2012. from http://www.uhfnyc.org/publications/880853. [Google Scholar]
- Sanford JT, Johnson AD, Townsend-Rocchiccioli JT. The health status of rural caregivers. Journal of Gerontological Nursing. 2005;31(4):25–31. doi: 10.3928/0098-9134-20050401-07. [DOI] [PubMed] [Google Scholar]
- Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. American Journal of Nursing. 2008;108(9):23–27. doi: 10.1097/01.NAJ.0000336406.45248.4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Beach SR. Caregiving as a risk factor for mortality: The caregiver health effects study. Journal of the American Medical Association. 1999;282(23):2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- Smedley J, Egger P, Cooper C, Coggon D. Manual handling activities and risk of low back pain in nurses. Occupational and Environmental Medicine. 1995;52:160–165. doi: 10.1136/oem.52.3.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J, Forster A, Young J. Cochrane review: information provision for stroke patients and their caregivers. Clinical Rehabilitation. 2009;23:195–206. doi: 10.1177/0269215508092820. [DOI] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics Table R11. Number of nonfatal occupational injuries and illnesses involving days away from work by occupation and selected sources of injury or illness, private industry. 2010.
- U.S. Department of Health and Human Services. Public Health Service. Centers for Disease Control and Prevention. National Institute of Occupational Safety and Health Musculoskeletal disorders and workplace factors. 1997. (DHHS-NIOSH Publication No: 97-141)
- Van Houtven CH, Norton EC. Informal caregivers and medicare expenditures: Testing for heterogeneous treatment effects. Journal of Health Economics. 2008;27(1):134–156. doi: 10.1016/j.jhealeco.2007.03.002. [DOI] [PubMed] [Google Scholar]
- Visser-Meily A, van Heugten C, Post M, Schepers V, Lindeman E. Intervention studies for caregivers of stroke survivors: a critical review. Patient Education and Counseling. 2005;56:257–267. doi: 10.1016/j.pec.2004.02.013. [DOI] [PubMed] [Google Scholar]
- Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to One’s physical health? A meta-analysis. Psychological Bulletin. 2003;129(6):946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- Waters T. When is it safe to manually lift a patient? American Journal of Nursing. 2007;107(8):53–58. doi: 10.1097/01.NAJ.0000282296.18688.b1. [DOI] [PubMed] [Google Scholar]
- Yates ME, Tennstedt S, Chang B. Contributors to and mediators of psychological well-being for informal caregivers. The Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 1999;54B(1):P12–P22. doi: 10.1093/geronb/54b.1.p12. [DOI] [PubMed] [Google Scholar]


