Introduction
Granular cell tumour (GCT) is an uncommon soft tissue neoplasm, first discovered in 1926 by the Russian pathologist Alexei Ivanovich Abrikossoff. It has a reported prevalence ranging from 0.019 % to 0.03 % of all the human neoplasm’s and accounts for about 0.5 % of all soft tissue tumors [1]. Although a great majority of the GCTs are benign, a very small percentage of them can exhibit an aggressive local behavior, a malignancy and even distant metastases [2]. These tumors usually present as a solitary asymptomatic nodule, <3 cm in size involving the subcutaneous or sub mucosal tissues with an intact overlying epithelium. We present a rare case of possibly the largest reported GCT in literature in a 36- year-old lady and discuss its management highlighting its atypical presentation and the reconstructive challenges.
Case Report
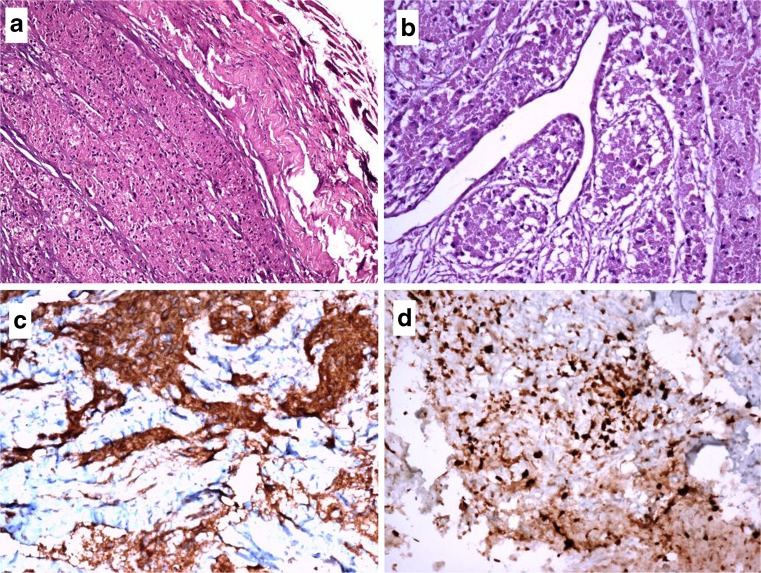
A 36-year-old lady without any co-morbid illnesses presented to us with a painless hard swelling of her tongue, progressively increasing over a year. Clinical examination revealed a predominantly sub mucosal tumor measuring 11 × 5 cm arising from the right side of the dorsal surface of the tongue and going onto involve almost the entire substance of the tongue, leading to ankyloglossia. The rest of the oropharynx and the upper aero digestive tract were clinically normal. There was insignificant cervical adenopathy. A CT scan of the head, neck and chest showed a large heterodense soft tissue lesion measuring 11 × 5 cm in the tongue predominantly involving the right side, with obliteration of the right side of oropharynx, the lung parenchyma was normal (Fig. 1). Histopathology of the incisional biopsy revealed a tumor composed of round or oval cells with ill defined outlines, abundant granular eosinophillic cytoplasm, prominent nucleoli with nuclear pleomorphism with moderate atypia and areas of spindling. A few sub epithelial lymphatics showed tumor emboli, vascular and perineural invasion was seen. The overlying epithelium was found to be locally infiltrated by tumor. The neoplastic cells on immunohistochemistry showed granular positivity to S-100- and were also strongly positive to the neural marker CD56. 30 % of the tumor cells showed strong nuclear positivity to Ki67. The histological along with the immunohistochemical findings were consistent with a diagnosis of a malignant GCT of the tongue (Fig. 2a–d).
Fig. 1.
An Axial C.T scan of the head and neck showing a large heterodense soft tissue lesion measuring in the tongue predominantly involving the right side, with obliteration of the right side of oropharynx
Fig. 2.
a H&E×20—Showing tumor composed of round or oval cells with ill defined outlines, abundant granular eosinophillic cytoplasm, prominent nucleoli with nuclear pleomorphism with moderate atypia and areas of spindling with perineural invasion. b H&E×20—Granular cell tumor with lymphatic invasion. c IHC×20—Tumor cells showing immunopositivity to CD 56. d IHC×20—30 % of the tumor cells positivity to Ki-67
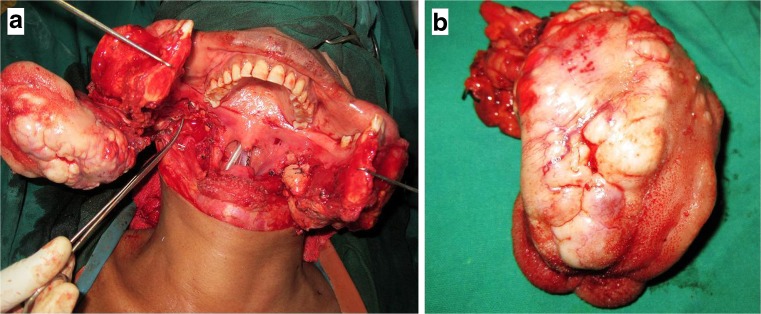
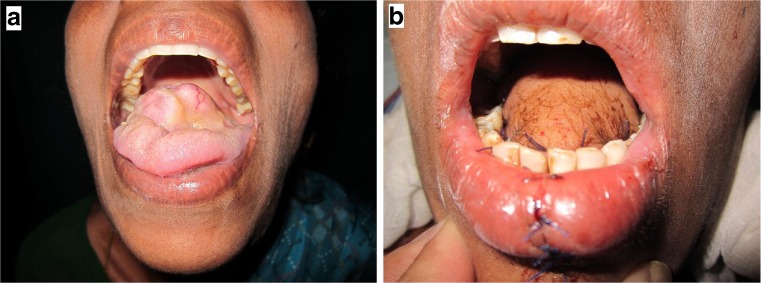
The patient was subsequently planned for a definitive surgery. A Visor (transverse neck) flap was raised, a midline lip and a mandibular split was additionally performed to gain access to the tumor in the oral cavity. Radical excision of the tumor which necessitated a total glossectomy, was performed, the tumor was seen coursing along the right lingual nerve (Fig. 3a, b). After confirming a tumor free margin on a frozen section, a left antero lateral thigh microvascular flap was used for the creation of a neo tongue (Fig. 4a, b). The patient was considered for adjuvant radiotherapy (40Grey of External Beam Radiotherapy) in view of the malignant nature of the tumor, large size (11 × 4.5 × 3 cm) and the associated perineural invasion, vascular and lymphatic emboli. The patient was put on an intensive speech and swallowing rehabilitation program and is currently disease free and is on follow up for more than a year now.
Fig. 3.
a Intra operative clinical photograph following radical excision of the tumor which necessitated a total glossectomy, the tumor is seen coursing along the right lingual nerve. b Specimen photograph following total glossectomy
Fig. 4.
a Preoperative clinical photograph at initial presentation. b Post operative clinical photograph following reconstruction with an antero lateral thigh microvascular flap
Discussion
GCTs can occur in a wide variety of anatomical sites throughout the body; more than 50 % of the lesions occur in the head and neck region, the commonest sub site being the tongue followed by buccal mucosa and hard palate [2, 3]. In the tongue, 48 % of the lesions occur on the dorsum with loss of papillae and atrophy of overlying mucosa and about 15 % reportedly occur on the lateral border followed by the ventral surface. GCTs have a female preponderance (M: F = 1:2) and can occur at any age [4], but commonly occur in the fourth to sixth decades of life.
The histological origin of GCT is controversial, ever since its original description by Abrikossoff, who assumed it to be a tumor of the striated muscle. There have been many proposed theories regarding the origin of this tumor i.e. histiocytic, fibroblastic, myoepithelial, and neuronal origins resulting in a wide array of nomenclature, granular cell myoblastoma, granular cell schwannoma, granular cell neurofibroma among others. The widely accepted hypothesis is that GCT results from the altered metabolism of schwann cells suggesting a neural origin [5].
A definitive diagnosis of GCT can only be made following accurate histological examination aided by immunohistochemistry correlation [6]. In GCTSs involving the tongue, the pseudoepitheliomatous hyperplasia may be so pronounced that it can be misinterpreted as a squamous cell carcinoma [7]. Such an erroneous diagnosis can occur if the tissue biopsy fragment is either too small or too superficial [8]. Further, it has been suggested that fine needle aspiration cytology is inherently unreliable in the diagnosis of a GCT [7].
Although a majority of the GCT’s are benign, about 10 % of cases may clinically demonstrate malignant behavior and < 2 % of cases may in fact present with distant metastasis [2, 9]. The malignant variety of GCT was first reported by Ravich et al. in 1945who found the tumor akin to a high grade sarcoma with high frequency of metastasis and short survival. Some authors have suggested that the distinction between benign and malignant types is fairly difficult because there is striking histological similarity between both varieties and a lack of reliable criteria to provide a prediction of development of a malignant behavior [8]. It was therefore suggested that only the presence of regional and distant metastasis would aid in the differentiating benign GCTs from its malignant counterpart [7]. Some authors have reported that malignancy of GCT is suggested by its rapid growth, broad dimensions (>4 cm) and the presence of necrotic and hemorrhagic areas, high mitotic index and cellular and nuclear pleomorphism [4].
According to an study by Fanburg et al. [5] malignancy in a GCT can be suggested by the presence of 3 or more of the following 6 criteria: The presence of a high mitotic activity, the presence of necrosis, the emergence of spindle cells, a vacuolar nucleus with an enlarged nuclear body, increase in the nuclear cytoplasmic ratio and the presence of polymorphisms. The tumor is considered benign if none of these criteria is met. If one or two criteria are met, the tumor is considered to be atypical and if three or more criteria are met, the tumor is considered as malignant.
Surgical excision is the only curative treatment of choice for all GCTs, regardless of whether the lesion is benign or malignant, solitary or multifocal. Since the GCTs have a poorly defined margin, the recommended treatment is excision with a wide margin of safety (2–3 cm) [10]. But in some cases a microscopic margin free removal may not possible due to the extensive nature of the disease, as the surgery can possibly result in unacceptable morbidity.
The role of adjuvant chemotherapy and radiotherapy in malignant GCT is controversial; these tumors have traditionally been considered to be radio resistant [4]. Adjuvant radiotherapy and chemotherapy is not routinely used in management of malignant GCTs, these modalities are be reserved only for selected cases i.e. large size, with margins positive after resection and presence of mitosis.
The prognosis of benign GCTs are generally good, recurrences are uncommon and are frequently a result of incomplete excision of the original lesion [8]. The prognosis of patients with the malignant GCTs are poor with frequent metastasis (>50 % overall) and 30–50 % mortality over 3 years [5]. A long-term follow-up is considered essential, because of the risk of local or distant recurrence even several years after surgery.
In conclusion, GCT should be considered in the differential diagnosis of oral submucosal lesions, particularly when they are located in the tongue and a high index of malignancy should be entertained for tumors > 3 cm or in the clinical setting of rapid growth and ulceration.
Acknowledgments
Conflict of Interest
None declared.
Funding
None.
Ethical Approval
Not required.
References
- 1.Ayadi L, Khabir A, Fakhfakh I, et al. Granular cell tumor. Rev Stomatol Chir Maxillofac. 2008;109:158–162. doi: 10.1016/j.stomax.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 2.Son HY, Kim JP, Ko GH, Lee EJ, Woo SH. Lingual squamous cell carcinoma surrounded by granular cell tumor. Chonnam Med J. 2012;48:65–68. doi: 10.4068/cmj.2012.48.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andrade ES, Filho JR, Rocha NS, Neto IC, Camargo IB. Isolated intra-oral granular cell tumor: report of two cases and review of the literature. Acta Odontol Latinoam. 2010;23:99–104. [PubMed] [Google Scholar]
- 4.Barbieri M, Musizzano Y, Boggio M, Carcuscia C. Granular cell tumour of the tongue in a 14-year-old boy: case report. Acta Otorhinolaryngol Ital. 2011;31:186–189. [PMC free article] [PubMed] [Google Scholar]
- 5.Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG. Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation. Am J Surg Pathol. 1998;22:779–794. doi: 10.1097/00000478-199807000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Cole E, Rahman N, Webb R. Case series: two cases of an atypical presentation of oral granular cell tumour. Case Rep Med. 2012;2012:159803. doi: 10.1155/2012/159803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nagaraj PB, Ongole R, Bhujanga-Rao BR. Granular cell tumor of the tongue in a 6-year-old girl. A case report. Med Oral Pathol Oral Cir Bucal. 2006;11:E162–E164. [PubMed] [Google Scholar]
- 8.Sposto MR, Navarro CM, de Andrade CR. Granular cell tumour (Abrikossof tumour): case report. Oral Oncol Extra. 2006;42:194–197. doi: 10.1016/j.ooe.2005.11.009. [DOI] [Google Scholar]
- 9.Giuliani M, Lajolo C, Pagnoni M, Boari A, Zannonni GF. Granular cell tumor of the tongue (Abrikossoff’s tumor). A case report and review of the literature. Minerva Stomatol. 2004;53:465–469. [PubMed] [Google Scholar]
- 10.Eguia A, Uribarri A, Gay-Escoda C, Crovetto MA, Martinez- Conde R, Aguirre JM. Granular cell tumour: report of 8 intraoral cases. Med Oral Pathol Oral Cir Bucal. 2006;11:E425–E428. [PubMed] [Google Scholar]