Abstract
Background/Aims
Gastroesophageal reflux disease (GERD), functional dyspepsia (FD), and peptic ulcer disease (PUD) impact the daily lives of affected individuals. The aim of this study was to compare the risk factors and impacts on life quality of overlapping FD or PUD in patients with GERD.
Methods
Data from patients diagnosed with GERD were collected between January and November 2009. FD was defined using the Rome III diagnostic criteria. The overlapping GERD-FD or GERD-PUD groups were classified as concomitant GERD and FD or peptic ulcers. The characteristics of these individuals were analyzed.
Results
There were 63, 48, and 60 patients in the GERD only, overlapping GERD-FD, and overlapping GERD-PUD groups, respectively. Significantly younger age, female gender, lower body weight and body mass index, and higher rates of tea consumption were noted in the GERD-FD group. Patients in the GERD-FD group exhibited the lowest quality of life scores, both with respect to physical and mental health, on the Short Form 36 domains.
Conclusions
Patients with concomitant GERD and FD were more likely to be younger and female. Overlapping GERD and FD had the worst impact on the quality of life of the affected individuals.
Keywords: Functional dyspepsia, Gastroesophageal reflux disease, Organic dyspepsia, Peptic ulcer disease, Quality of life
INTRODUCTION
Gastroesophageal reflux disease (GERD) and functional dyspepsia (FD) are very common in the general population, and both have a considerable impact on the daily lives of affected individuals. According to the Montreal definition, GERD is a condition which develops when the reflux of stomach contents causes troublesome symptoms and/or complications.1 Based on the Rome III diagnostic criteria, FD is a disorder in which bothersome postprandial fullness or epigastric pain persists for 3 months, without evidence of structural disease.2 FD can be further divided into postprandial distress syndrome (PDS) and epigastric pain syndrome (EPS) based upon different presentations. Since GERD and FD are both prevalent, coexistence may often be observed. Another type of dyspepsia, structural or organic dyspepsia, is mostly caused by peptic ulcer disease (PUD), erosive esophagitis, and rarely, gastrointestinal malignancy or biliary disease.3 Similarly, PUD, the most of the structural dyspepsia, also impairs physical activities and reduces productivity in the affected cases. The aim of this study was to evaluate the risk factors and impacts on life quality of overlapping FD or PUD in a Chinese population with GERD.
MATERIALS AND METHODS
Data from consecutive patients diagnosed with GERD in our hospital, Taichung Veterans General Hospital, according to the Montreal definition, were collected between January and November 2009. All patients underwent an open-access transoral upper gastrointestinal endoscopy. Exclusion criteria were as follows: 1) GERD combined with esophageal or gastric malignancy, 2) prior gastric surgery, 3) use of antacid medication, such as proton pump inhibitors or H2-receptor antagonists, for more than 2 months prior to enrollment, and 4) pregnancy.
All the enrolled patients were asked to complete a current lifestyle questionnaire and the Short Form 36 (SF-36) questionnaire. The SF-36 questionnaire measures generic quality of life, which measures health status in eight domains: physical functioning, role limitations-physical, bodily pain, general health, vitality, social functioning, role limitations-emotional, and mental health. Scores on the SF-36 range from 0 to 100 on each dimension, with higher scores indicating better quality of life.4
The cases with symptoms compatible with FD, based on the Rome III diagnostic criteria and negative endoscopic findings, were assigned to the overlapping GERD-FD group. The cases with dyspepsia symptoms and PUD, comfirmed by endoscopic findings, were assigned to the overlapping GERD-PUD group. Patients without symptoms of dyspepsia were categorized as the GERD only group. All patients received biopsies taken from the gastric antrum during the endoscopy for the detection of Helicobacter pylori infection by a rapid urease test. The general data, endoscopic findings, and questionnaire scores of these participants were collected and compared.
Patients with FD were further divided into PDS, EPS, or concomitant PDS/EPS subgroups, according to the Rome III diagnostic criteria, and the characteristics of these cases were also investigated and analyzed.
Data are expressed as standard deviation of the mean for each of the measured parameters. Gender, lifestyle questionnaire item scores, H. pylori infection, and hiatal hernia rates are expressed as percentages of the total patient number. A p-value below 0.05 was considered statistically significant. Pearson chisquare test or Fisher exact test was used to compare the effects of gender, lifestyle questionnaire item scores and the H. pylori infection rate. An independent t-test was used to analyze age, body weight, body mass index (BMI), and SF-36 questionnaire scores.
RESULTS
Among all consecutive enrolled patients in our study, 63, 48, and 60 patients were in the GERD only, overlapping GERD-FD, and overlapping GERD-PUD groups, respectively. Patients' characteristics are summarized in Table 1. A comparison of the age and gender of participants in each group revealed that patients were significantly younger and the ratio of females to males was higher in the GERD-FD group (mean, 40.54 years old; 70.8% female) than in the GERD only group (mean, 51.43 years old; 34.9% female), or the GERD-PUD group (mean, 51.53 years old; 46.7% female). Patients in the GERD only group were prone to have significantly higher body weight and BMI than patients in the other two groups.
Table 1.
Basic Characteristic and Disease Pattern of Patients
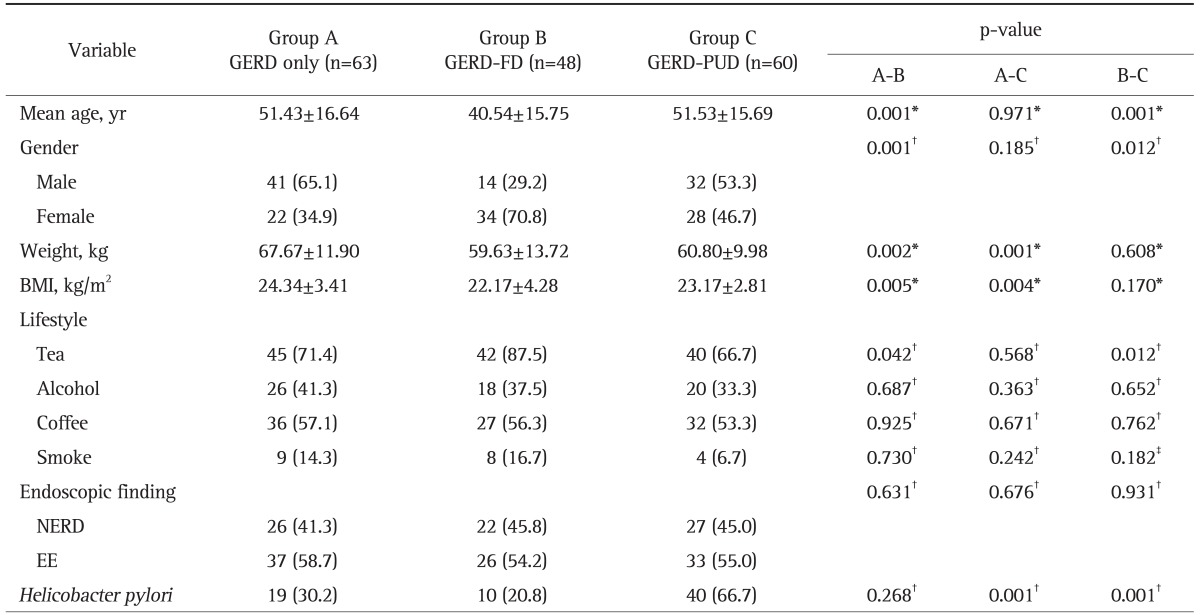
Data are presented as mean±SD or number (%). p-value A-B means p-value between group A and B; p-value A-C means p-value between group A and C; p-value B-C means p-value between group B and C.
GERD, gastroesophageal reflux disease; FD, functional dyspepsia; PUD, peptic ulcer disease; BMI, body mass index; NERD, nonerosive reflux disease; EE, erosive esophagitis.
*t-test; †Pearson chi-square test; ‡Fisher exact test.
The lifestyle characteristics and disease patterns among these patients are also displayed in Table 1. Significantly higher rates of tea consumption (87.5%) were noted in the GERD-FD group compared with the other two groups, but the rates of cigarette smoking, alcohol and coffee consumption were similar among all groups. The rates of erosive esophagitis (EE) and nonerosive reflux disease (NERD) were also similar among the three groups, but the rate of H. pylori infection was significantly higher in the GERD-PUD group (66.7%) than in the GERD only group (30.2%) and the GERD-FD group (20.8%).
The quality of life scores as measured by the SF-36 questionnaire are shown in Table 2. The GERD only group had the highest physical (mean, 71.27) and mental health scores (mean, 68.33). On the contrary, the GERD-FD group had the lowest physical (mean, 58.13) and mental health scores (mean, 50.46) than the others. One subscale of the SF-36 domain, physical function, showed no decline in any of the three groups.
Table 2.
Short Form 36 Scores of the Three Groups of Patients
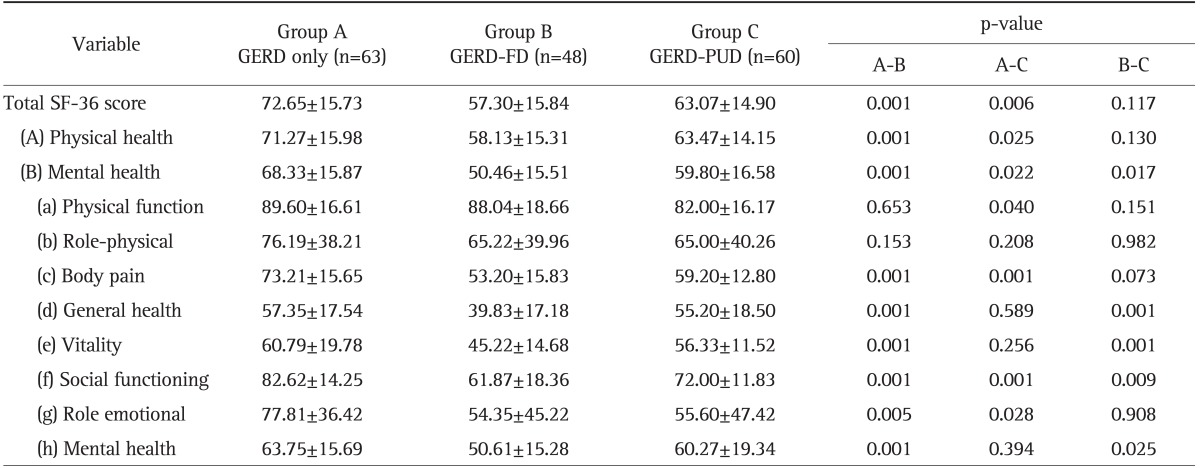
All analyzed by the Kruskal-Wallis one-way ANOVA test. Data are presented as mean±SD. p-value A-B means p-value between group A and B; p-value A-C means p-value between group A and C; p-value B-C means p-value between group B and C.
GERD, gastroesophageal reflux disease; FD, functional dyspepsia; PUD, peptic ulcer disease; SF-36, Short Form 36.
Among the 48 patients with FD, 23 (47.9%), 12 (25%), and 13 (27.1%) cases were further divided into the PDS, EPS, and concomitant PDS/EPS subgroups, respectively, as shown in Table 3. The general data and endoscopic findings among these three subgroups disclosed similar results, except for a higher EE rate in the GERD-PDS subgroup (73.9%) than that in the GERD-PDS/EPS subgroup (23.1%). The physical and mental health scores of these subgroups, as measured by the SF-36 questionnaire, were not different among subgroups.
Table 3.
Basic Characteristics and Disease Patterns of Patients
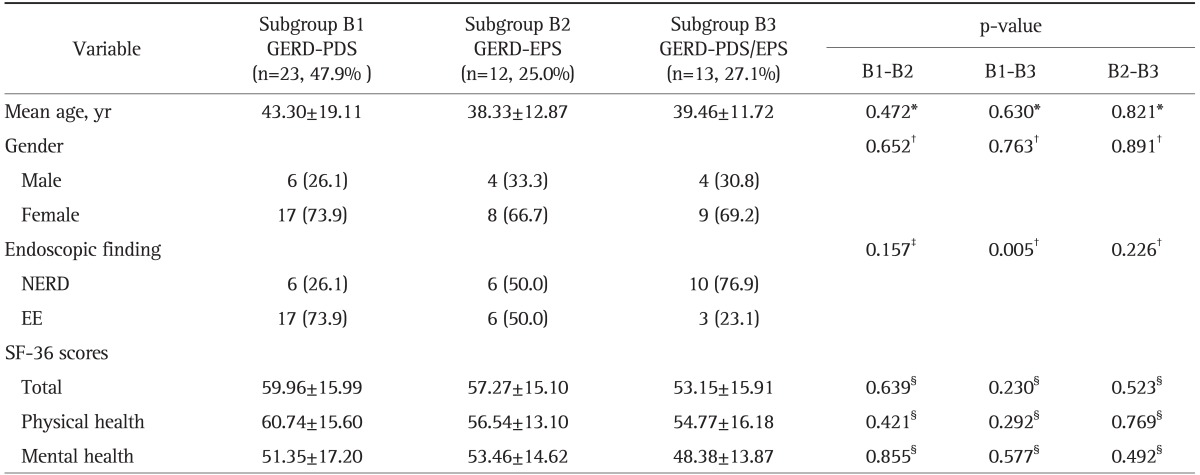
Data are presented as mean±SD or number (%). p-value B1-B2 means p-value between subgroup B1 and B2; p-value B1-B3 means p-value between subgroup B1 and B3; p-value B2-B3 means p-value between subgroup B2 and B3.
GERD, gastroesophageal reflux disease; PDS, postprandial distress syndrome; EPS, epigastric pain syndrome; NERD, nonerosive reflux disease; EE, erosive esophagitis; SF-36, Short Form 36.
*t-test; †Fisher exact test; ‡Pearson chi-square test; §Kruskal-Wallis one-way ANOVA test.
DISCUSSION
GERD is a chronic disease which has a major impact on the daily lives of affected individuals by interfering with physical activity, impairing social functioning, disturbing sleep, and reducing productivity at work.5-7 Functional gastrointestinal disorders (FGIDs), such as irritable bowel syndrome (IBS), FD, and chronic constipation, pose an extensive healthcare burden and negatively affect quality of life. Patients with GERD suffer more commonly from FGIDs. In clinical practice, the differentiation of the manifestations of GERD and FD is difficult, particullary in patients presenting with long-lasting symptoms.
Past epidemiological studies that investigated the prevalence of dyspeptic and esophageal symptoms have reported a higher prevalence of dyspeptic symptoms in patients with GERD, suggesting that the degree of overlap is greater than could be predicted by chance alone.8 For example, Guillemot et al.9 showed an FD overlap as high as 17% in GERD patients using the Rome II diagnostic criteria. According to a previous report, the prevalence of dyspepsia decreases with age, but the distribution of subtypes of FD does not vary by age.10 Besides, the majority of FGIDs are more prevalent in women than in men.11 The pathogenesis might be associated with delayed gastric emptying and lower tolerance of the intragastric content in the female gender.12 Our study found female predominance and younger age in the cases with overlapping GERD-FD, compared to those with GERD only or overlapping GERD-PUD.
A previous study reported cigarette smoking was significantly associated with overlaps among GERD, FD, and IBS in Japanese adults.13 H. pylori is associated with PUD, and arguably with nonulcer dyspepsia. Furthermore, NERD has been reported to be more frequently overlapped with FD.14 However, the results of our study failed to confirm the impacts of the above risk factors in the cases with overlapping GERD-FD compared to those with GERD only. In contrast, the only item with positive correlation to overlaps of GERD-FD was tea consumption. These differences might be due to ethnic variation (Chinese population versus Western population) or different definitions of FD (Rome III versus Rome II or I) adopted in individual studies.
A recent study revealed the overlap of GERD with FD had a statistically significant impact on SF-36 scores for bodily pain compared with FD only.15 Our results show that the overlapping GERD-FD group, compared with the GERD only group, indicated a significant impairment in most SF-36 domains, except for physical role and physical function.
Aro et al.15 reported that individuals with organic dyspepsia had slightly lower scores in every SF-36 domain except for physical functioning compared with individuals with FD. Moreover, PUD had an insignificant impact compared with FD on scores in the domains of physical and emotional roles. In contrast, Talley et al.16 reported that quality of life may be more impaired in patients with FD than in those with organic dyspepsia. Our data proved that patients with overlapping GERD-PUD had significantly lower physical and mental health scores than those with GERD only, and higher mental scores than those with overlapping GERD-FD. Namely, the patients with overlapping GERD-FD had the worst quality of life scores among all participants in our study.
As a past study, subjects with PDS tend to have lower scores in all SF-36 domains than those with EPS do, and EPS had a significant impact on bodily pain and vitality.15 However, taking into consideration GERD overlapping with PDS or EPS, as in our study, there was no significant difference between these two subgroups in scores for the impairment of quality of life. This might be due to the limited number of cases in our study, which may make the final results insignificant, or GERD and FD may share a common pathophysiological mechanism.
There are some limitations in our study. Firstly, a significant number of cases had different predominant symptoms, which may easily lead to bias. Secondly, comorbidity of diseases, which tend to adversely influence quality of life, such as chronic heart failure or chronic obstructive pulmonary disease, were not recorded, and this might have led to scoring bias in the questionnaire. Thirdly, there was a lack of placebo controls. Lastly, our study design was hospital-based. Further research should include representative samples from the general population to confirm these results.
In conclusion, this study revealed that the overlapping of GERD and FD tends to occur in younger individuals and females. The overlapping of GERD and FD or PUD had a significant negative impact on quality of life of affected patients, especially those with FD. The subtypes PDS and EPS had similar disease characteristics and impacts on patients with GERD.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920. doi: 10.1111/j.1572-0241.2006.00630.x. [DOI] [PubMed] [Google Scholar]
- 2.Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology. 2006;130:1466–1479. doi: 10.1053/j.gastro.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 3.Rabeneck L, Wray NP, Graham DY. Managing dyspepsia: what do we know and what do we need to know? Am J Gastroenterol. 1998;93:920–924. doi: 10.1111/j.1572-0241.1998.277_e.x. [DOI] [PubMed] [Google Scholar]
- 4.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 5.Wiklund I. Review of the quality of life and burden of illness in gastroesophageal reflux disease. Dig Dis. 2004;22:108–114. doi: 10.1159/000080308. [DOI] [PubMed] [Google Scholar]
- 6.Lee SW, Chang CM, Chang CS, Kao AW, Chou MC. Comparison of presentation and impact on quality of life of gastroesophageal reflux disease between young and old adults in a Chinese population. World J Gastroenterol. 2011;17:4614–4618. doi: 10.3748/wjg.v17.i41.4614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee SW, Lien HC, Chang CS, Peng YC, Ko CW, Chou MC. Impact of body mass index and gender on quality of life in patients with gastroesophageal reflux disease. World J Gastroenterol. 2012;18:5090–5095. doi: 10.3748/wjg.v18.i36.5090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Locke GR, 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ., 3rd Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448–1456. doi: 10.1016/s0016-5085(97)70025-8. [DOI] [PubMed] [Google Scholar]
- 9.Guillemot F, Ducrotté P, Bueno L. Prevalence of functional gastrointestinal disorders in a population of subjects consulting for gastroesophageal reflux disease in general practice. Gastroenterol Clin Biol. 2005;29:243–246. doi: 10.1016/s0399-8320(05)80756-0. [DOI] [PubMed] [Google Scholar]
- 10.Chang L, Toner BB, Fukudo S, et al. Gender, age, society, culture, and the patient's perspective in the functional gastrointestinal disorders. Gastroenterology. 2006;130:1435–1446. doi: 10.1053/j.gastro.2005.09.071. [DOI] [PubMed] [Google Scholar]
- 11.Chang L. Review article: epidemiology and quality of life in functional gastrointestinal disorders. Aliment Pharmacol Ther. 2004;20(Suppl 7):31–39. doi: 10.1111/j.1365-2036.2004.02183.x. [DOI] [PubMed] [Google Scholar]
- 12.Talley NJ, Verlinden M, Jones M. Can symptoms discriminate among those with delayed or normal gastric emptying in dysmotility-like dyspepsia? Am J Gastroenterol. 2001;96:1422–1428. doi: 10.1111/j.1572-0241.2001.03683.x. [DOI] [PubMed] [Google Scholar]
- 13.Fujiwara Y, Kubo M, Kohata Y, et al. Cigarette smoking and its association with overlapping gastroesophageal reflux disease, functional dyspepsia, or irritable bowel syndrome. Intern Med. 2011;50:2443–2447. doi: 10.2169/internalmedicine.50.6012. [DOI] [PubMed] [Google Scholar]
- 14.Noh YW, Jung HK, Kim SE, Jung SA. Overlap of erosive and non-erosive reflux diseases with functional gastrointestinal disorders according to Rome III criteria. J Neurogastroenterol Motil. 2010;16:148–156. doi: 10.5056/jnm.2010.16.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aro P, Talley NJ, Agréus L, et al. Functional dyspepsia impairs quality of life in the adult population. Aliment Pharmacol Ther. 2011;33:1215–1224. doi: 10.1111/j.1365-2036.2011.04640.x. [DOI] [PubMed] [Google Scholar]
- 16.Talley NJ, Weaver AL, Zinsmeister AR. Impact of functional dyspepsia on quality of life. Dig Dis Sci. 1995;40:584–589. doi: 10.1007/BF02064375. [DOI] [PubMed] [Google Scholar]


