Abstract
The integration of new technologies has raised an interest in liver tumor radiotherapy, with literature evolving to support its efficacy. These advances, particularly stereotactic body radiation therapy (SBRT), have been critical in improving local control or potential cure in liver lesions not amenable to first-line surgical resection or radiofrequency ablation. Active investigation of SBRT, particularly for hepatocellular carcinoma (HCC), has recently started, yielding promising local control rates. In addition, data suggest a possibility that SBRT can be an alternative option for HCC unfit for other local therapies. However, information on optimal treatment indications, doses, and methods remains limited. In HCC, significant differences in patient characteristics and treatment availability exist by country. In addition, the prognosis of HCC is greatly influenced by underlying liver dysfunction and treatment itself in addition to tumor stage. Since they are closely linked to treatment approach, it is important to understand these differences in interpreting outcomes from various reports. Further studies are required to validate and maximize the efficacy of SBRT by a large, multi-institutional setting.
Keywords: Hepatocellular carcinoma, Liver cirrhosis, Liver neoplasms, Radiation therapy, Stereotactic body radiation therapy
Core tip: The integration of new technologies has raised an interest in radiotherapy for hepatocellular carcinoma (HCC), with literature evolving to support its efficacy. These advances, particularly stereotactic body radiation therapy (SBRT), have been critical in improving local control or potential cure in liver lesions not amenable to first-line surgical resection or radiofrequency ablation. Active investigation of SBRT has recently started, yielding promising local control rates. However, information on optimal treatment indications, doses, and methods remains limited. In HCC, significant differences in patient characteristics and treatment availability exist by country. Further studies are required to validate and maximize the efficacy of SBRT.
INTRODUCTION
Hepatocellular carcinoma (HCC) is currently the fifth most common solid tumor worldwide and the third leading cause of cancer-related death[1]. The definitive treatment for HCC has evolved primarily to be surgery, orthotopic liver transplantation, percutaneous ablation, or partial transarterial chemoembolization (TACE)[2]. However, in some patients, these therapies are not feasible. This review describes the evolution of and current practices for radiation therapy, with particular focus on stereotactic body therapy (SBRT) in treating these types of tumors in patients who are not candidates for definitive treatment. We also discuss the emerging role of SBRT as well as current outcomes, toxicities, and pathological and radiological findings after SBRT.
EPIDEMIOLOGY
The incidence of HCC is increasing in several developed countries, such as European nations and the United States, while in areas such as Japan and Singapore, the incidence of HCC seems to have stabilized or even fallen slightly[3,4]. The geographic variability in the incidence of HCC is largely explained by the distribution of hepatitis B and C viruses, and by the patterns of exposure to key risk factors in each population. The prevalence of such infections is being controlled by vaccination, which should also influence future trends in HCC occurrence. Heavy alcohol consumption, obesity, and diabetes are also risk factors and substantial causes of HCC in Europe and the United States.
The broad spectrum of HCC epidemiology and treatments is expected to affect prognosis. When referring to the literature on HCC treatment outcomes, it is important to carefully understand the differences in patient characteristics in each report, because these factors significantly affect outcomes as well as clinical application of various treatments.
STANDARD LOCAL TREATMENT OPTIONS FOR HCC
In HCC, prognosis is greatly influenced by underlying liver dysfunction and treatment itself, as well as tumor stage, while in other solid tumors, it is generally only related to tumor stage[2]. Unlike other cancers, many staging systems are used for HCC, including the Barcelona Clinic Liver Cancer (BCLC) staging[2], tumor-node-metastasis[5], Okuda[6], Cancer of the Liver Italian Program[7], and Japan Integrated Staging[8] scoring systems. Among these, the BCLC staging system considers the relevant parameters of all important dimensions and divides patients into very early/early, intermediate, advanced, and end-stage to recommend optimal treatment. Early-stage HCC patients are considered for potentially curative options such as resection, ablation, and transplantation. Patients with intermediate stage disease may benefit from TACE, whereas patients with advanced stage disease, or who cannot benefit from other options, are given sorafenib, an oral multikinase inhibitor, as the standard treatment.
Despite recent advances in early detection and diagnosis, only 30%-40% of patients with HCC may benefit from radical therapies. For patients who are not eligible for these curative therapies, two randomized trials have shown improved survival using TACE compared with symptomatic therapy alone[9,10]. However, TACE is somewhat controversial: a review from the Cochrane library that considered all randomized trials that compared TACE vs placebo, sham, or no intervention concluded that no firm evidence exists to support or refute TACE for patients with unresectable HCC[11]. In addition, the local control rate for TACE is inferior to those of resection and percutaneous ablation (82%-98% at 3 years)[12]. At best, the 3-year local control rate of superselective TACE was reported to be 65.3% in 123 patients with HCC < 5 cm in diameter[13]. Nevertheless, patients who have limited tumor burden but are not suitable for radical therapies usually undergo TACE despite its relatively low efficacy. Improving the outcomes of these patients is one of the major challenges in HCC management.
DIFFERENCE IN TREATMENT APPROACH BY COUNTRIES
The differences in patient characteristics or treatment availability by country are closely linked to the treatment approaches used in each county. Currently, early HCC diagnosis is increasingly feasible in countries with wider implementation of surveillance policies, which enables the application of curative treatments. Applicability of standard local treatments varies according to geographic distribution, with 50%-70% of cases in Japan being suitable for curative treatment, compared to only 25%-40% of cases in Europe and the United States, and 10% in Africa[14]. Once a high-risk cohort is identified, follow-up surveillance has contributed to early detection of HCC, although its efficacy appears to vary by country. In fact, in a recent Japanese cohort including 1432 patients, careful ultrasonography surveillance performed by highly skilled operators resulted in the average size of detected tumors being 1.6 cm ± 0.6 cm, with < 2% of the cases exceeding 3 cm[15].
Treatment differences by country are also prominent for organ transplantation. Orthotopic liver transplantation offers the best chance for cure, particularly in patients with decompensated liver disease. Excellent results can be achieved in patients with solitary HCC < 5 cm, or up to three nodules < 3 cm, and without extrahepatic or vascular spread, known as the Milan criteria[16]. However, the chance of transplantation is extremely limited in many countries due to the lack of sufficient liver donors. Furthermore, in contrast to western countries, Asia has cultural and religious barriers to organ donation from deceased individuals. The number of deceased donors per million population ranges from 0.07-6.5 among Asian transplantation centers, which is far below those of western countries (e.g., 35.1 per million population in Spain and 25.2 per million population in the United States)[17].
RADIATION THERAPY FOR HCC
Historically, treatment with conventionally fractionated (1.8-2 Gy/fraction over several weeks) and 2-dimensionally-planned radiation is associated with high rates of local progression and short median survival duration. While a radiation dose-response has been observed in unresectable HCC, the delivery of high doses of radiation using conventional techniques has been limited by hepatotoxicity. Given these limitations, radiation therapy is usually not curative. Compared to other local therapies, the clinical data supporting evidence for radiotherapy in HCC patients are extremely limited[18].
As Dr. Dawson[19] descriptively discussed regarding how radiation therapy fit into the spectrum of liver cancer local therapies, HCC patients suitable for focal irradiation extend from very early to intermediate BCLC stage. For those who are unsuitable for resection, transplantation, or ablation, definitive radiotherapy or radiotherapy can be administered as a bridge to transplantation[20-22]. Definitive radiotherapy is also considered for those patients who are unsuitable for or refractory to TACE. For those patients who have portal invasion, systemic chemotherapy (e.g., sorafenib) can be added to definitive radiotherapy.
SBRT
Numerous advances in external-beam radiation therapy allow for more accurate targeting, and make aggressive dose-fractionation strategies possible using techniques such as SBRT. Originally developed for the treatment of intracranial malignancies (i.e., radiosurgery), SBRT has since been adopted for the treatment of extracranial diseases. For example, SBRT has been shown to be a highly effective and well-tolerated treatment in patients with medically inoperable or high-risk operable stage I non-small cell lung cancer[23].
The use of SBRT for liver malignancies was pioneered by Dr. Blomgren et al[24] at the Karolinska Institute, Stockholm in the early 1990s. SBRT refers to the use of stereotactic non-coplanar conformal radiation therapy intended for a small number of significantly larger fraction sizes (usually 8-12 Gy/fraction), while limiting the dose to adjacent normal tissues. The steep dose gradient within the target volume leads to tight conformity with steep and isotropic dose fall-off and high dose delivery to the target volume (Figure 1).
Figure 1.
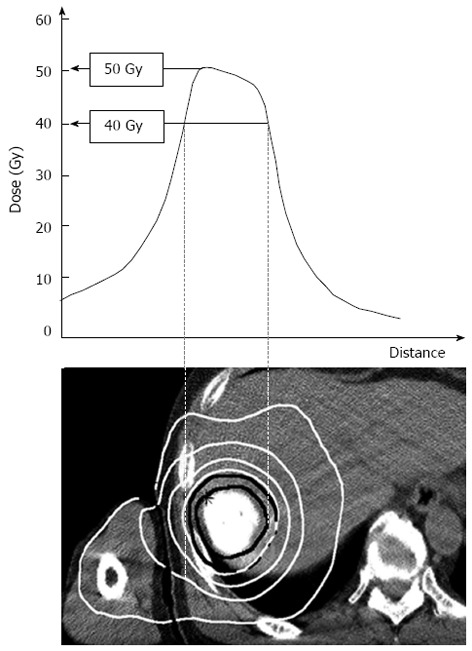
Dose distribution of stereotactic body radiation therapy for hepatocellular carcinoma at a dose of 40 Gy in 5 fractions, prescribed at the periphery of the target volume. The isodose lines (white solid lines) from inner to outer represent 40, 30, 20 and 10 Gy, respectively. The center of the tumor receives as high as 125% of the prescribed dose.
SBRT should be implemented with accurate patient repositioning, target localization, and control of breathing-related motion by breathing control devices such as abdominal compression, gating, and tracking systems, as well as some form of image-guided radiation therapy (IGRT) to improve set-up accuracy and treatment delivery[25].
INDICATIONS FOR SBRT
Although the indications for SBRT for hepatic malignancy have evolved, the role of SBRT in HCC is less clear. Future studies should focus not only on maximizing efficacy, but also on determining how SBRT should be used in the context of other previously established therapies. Careful patient selection is required and SBRT should be considered only after thorough discussion within a multi-disciplinary team, with all legitimate treatment options also considered.
Eligibility criteria for different treatment techniques are outlined in Table 1. In general, SBRT and other local therapies can complementarily divide the roles between each modality. SBRT is feasible even for lesions that are not eligible for surgery or percutaneous ablation. For example, patients whose lesions are located in a central portal area or regions adjacent to great vessels or the biliary system are good candidate for SBRT[26]. In addition, lesions located just below the diaphragm or at the surface of the liver are also excellent targets for SBRT. Figure 2 illustrates typical liver locations for which SBRT can be safely delivered. SBRT is difficult to perform for lesions near the bowels due to the risk of gastrointestinal perforation, bleeding, and ulcer. Examples of patients who could not be treated with other local therapies but received SBRT are shown in Figures 3-5.
Table 1.
Eligibility criteria for different treatment modalities
| Surgery | Percutaneous ablative therapy | TACE | SBRT | |
| Tumor size | < 5 cm (or more) | < 3 cm | > 3-5 cm | 4 (or 5) cm |
| Number of tumors | < 3 | Depends on location | 1-multiple (> 4) | < 1-3 |
| Location or characteristics | Depends on liver function | Away from large vessels or biliary system | Hypervascular lesions | Away from bowels |
| Local control (2 yr) | > 90% | > 90% | < 65% | > 90% |
| Level of evidence | High | Intermediate-high | Intermediate-high | Low |
| Invasiveness | High | Less | Less | None |
| Damage to the liver | High | Low | Low-moderate | Low-moderate |
SBRT: Stereotactic body radiation therapy; TACE: Transarterial chemoembolization.
Figure 2.
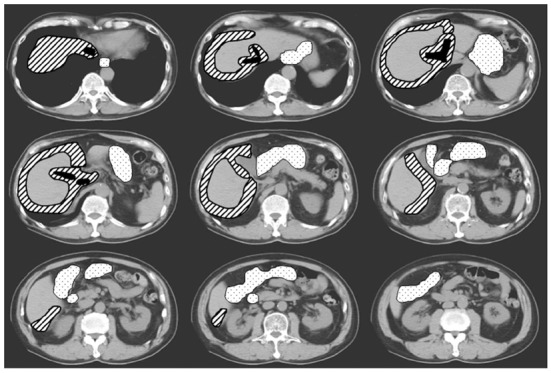
Computed tomography sections demonstrating typical locations treated with stereotactic body radiation therapy. Areas indicated with hatched lines can be safely treated with stereotactic body radiation therapy (SBRT), although these areas are difficult to approach for percutaneous ablation. Liver tumors located adjacent to the stomach and bowels (dotted areas) are not suitable for SBRT. Other unmarked areas can be treated either with SBRT or percutaneous ablation.
Figure 3.
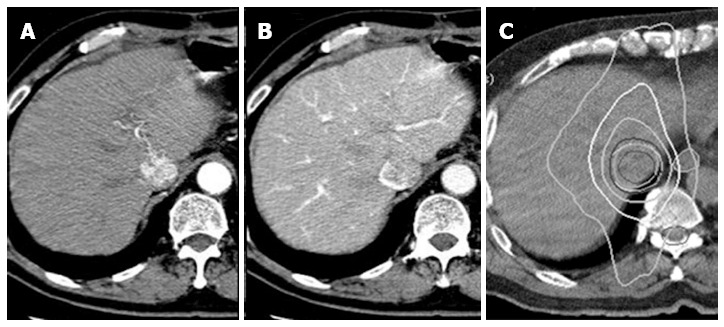
Hepatocellular carcinoma case that could not be effectively or safely treated with any treatment except for stereotactic body radiation therapy. The tumor invading the vena cava is enhanced in arterial phase and shows a defect in portal phase on dynamic computed tomography (A and B). An axial view of radiation dose distribution. The isodose lines (white lines) from inner to outer represent 40, 30, 20, and 10 Gy, respectively (C).
Figure 5.
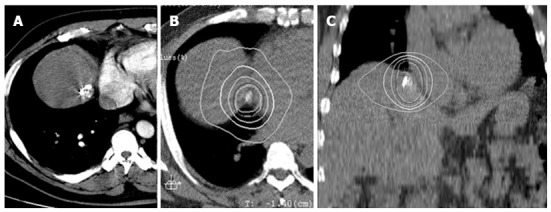
Case of hepatocellular carcinoma. Located adjacent to the right atrium (A). Axial and coronal view of radiation dose distribution (B and C). The isodose lines (white lines) from inner to outer represent 40, 30, 20, and 10 Gy, respectively.
Figure 4.
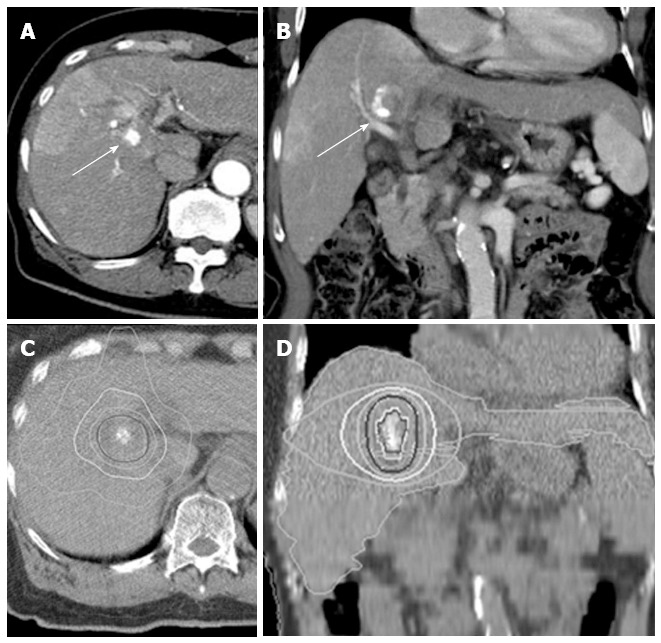
Case of hepatocellular carcinoma located in the hepatic hilum. Surgical resection would have required a right lobectomy. Percutaneous ablative therapy was impossible due to involvement of the biliary system and large vessels near the tumor. Axial and coronal views of a tumor with partial lipiodol deposit (A and B, arrows). Axial and coronal views of radiation dose distribution (C and D). The isodose lines (white lines) from inner to outer represent 40, 30, 20, and 10 Gy, respectively.
There is always a waiting period between listing and transplantation, and this varies between institutions. Many therapies have been used as a “bridge” to transplantation, and SBRT has also been evaluated as a means to bridge to transplantation. As a bridging therapy, SBRT has been reported to be feasible and well tolerated[20,21,27]. Furthermore, it enables patients to remain on the list for frequently curative transplantation while waiting for donated livers to become available.
SBRT OUTCOMES AND OPTIMAL DOSES
Outcomes of SBRT for HCC are summarized in Table 2[28-43]. A total of four prospective studies that exclusively evaluated HCC, as well as other retrospective studies demonstrated promising treatment effects (Table 3). The number of reports of successful SBRT studies had been increasing since 2006. Earlier studies involving SBRT for liver tumors included not only HCC but also cholangiocarcinoma and metastatic liver tumors, which made it difficult to compare the results between studies. Although the literature for SBRT is primarily composed of retrospective, small, single-institution series, SBRT has been associated with high local control rates, mostly in the range of 70%-90% at 1-2 years.
Table 2.
Prospective studies of stereotactic body radiation therapy for hepatocellular carcinoma and other liver tumors
| Ref. | Country | Patient number | Median volume, mL | Median size, cm | Median dose (range)/fraction, Gy | Median follow-up (range), mo | Local control | Overall survival |
| Cárdenes et al[29] | United States (Indiana) | 17 | 34(8-95) | - | VariableCP-A: 36-48 Gy/3 frCP-B: 40 Gy/5 fr | 24(10-42) | 100% | 75% (1 yr)60% (2 yr) |
| Andolino et al[37] | United States (Indiana) | 60 | 29(2-112) | 3.2(1-6.5) | FixedCP-A: 44 Gy/3 frCP-B: 40 Gy/5 fr | 27(2-52) | 90% (2 yr) | 67% (2 yr) |
| Bujold et al[30] | Canada | 102 | 117(1-1913) | 7.2(1.4-23.1) | Variable36 (24-54) Gy/6 fr | 31(2-36) | 87% (1 yr) | Median 17 mo |
| Kang et al[31] | South Korea | 47 | 15(2-213) | 2.9(1.3-7.8) | 57 (42-60) Gy/3 fr | 17(6-38) | 95% (2 yr) | 69% (2 yr) |
| (Korea Inst. of Radiological and Medical Sciences) |
CP: Child-Pugh.
Table 3.
Retrospective studies of stereotactic body radiation therapy for hepatocellular carcinoma and other liver tumors
| Ref. | Country | Patient number | Median volume (mL) | Median size, cm | Median dose (range)/fraction, Gy | Median follow-up (range) (mo) | Local control | Overall survival |
| Choi et al[32], 2006 | South Korea(The Catholic Univ. of Korea) | 20 | - | 3.8 (2-6.5) | Fixed50 Gy/5 or 10 fr | 23(3-55) | 100% | 70%(1 yr)43%(2 yr) |
| Zhang et al[72], 2007 | China(Hebei) | 27 | - | < 5 cm: 18%3-5 cm: 41%> 5 cm: 41% | Median40 (32-42) Gy/5 fr | 10(3-21) | 22%(1 yr) | - |
| Choi et al[33], 2008 | South Korea(The Catholic Univ. Korea) | 31 | 25(4-57) | - | Variable33 (30-39) Gy/3 fr | 11(2-19) | 100% | 81%(1 yr) |
| Louis et al[34], 2010 | Belgium | 25 | 48(7-363) | - | Fixed45 Gy/3 fr | 13(1-24) | 95%(1 yr) | 79%(1 yr)52%(2 yr) |
| Kwon et al[35], 2010 | South Korea(The Catholic Univ. of Korea) | 42 | 15(3-82) | - | Variable30-39 Gy/3fr | 29(8-4) | 72%(1 yr)68%(3 yr) | 93%(1 yr)59%(3 yr) |
| Seo et al[36], 2010 | South Korea(Korea Inst. of Radiological and Medical Sciences) | 38 | 41(11-464) | - | Variable33-57 Gy/3-4 fr | 15(3-27) | 66%(2 yr) | 61%(2 yr) |
| Huang et al[38], 2012 | Taiwan | 36 | - | 4.4(1.1-12) | Variable37 (25-48 Gy)/4-5 fr | 14(2-35) | 88%(1 yr)75%(2 yr) | 64%(2 yr) |
| Honda et al[39], 2012 | Japan(Hiroshima) | 30 | - | 1.6(1-3) | Fixed 48 Gy/4 fr or 60 Gy/8 fr | 12(6-38) | 100% | 100%(1 yr)100%(3 yr) |
| Bae et al[40], 2013 | South Korea(Korea Inst. of Radiological and Medical Sciences) | 35 | 131(21-2189) | - | Variable45 (30-60) Gy/3-5 fr | 14(1-44) | 69%(1 yr)51%(3 yr) | 52%(1 yr)21%(2 yr) |
| Xi et al[41], 2013 | China(Sun Yat-sen Univ.) | 41 | 65 (± 48) | - | Variable36 (30-48) Gy/6 fr | 10(4-25) | 95% | 50%(1 yr) |
| Sanuki et al[43], 2013 | Japan(Ofuna) | 185 | 8(1.5-65) | - | FixedCP-A: 40 Gy/5 fr/CP-B: 35 Gy/5 fr/ | 24(3-80) | 91%(3 yr) | 70%(3 yr) |
CP: Child-Pugh.
Various prescribed doses and treatment planning strategies are presently employed by different groups[28-43], and information about optimal treatment doses remains limited. Some studies employed SBRT alone, while others combined TACE as part of the treatment. Tumor size varied from 2-3 cm to approximately 5-7 cm. These differences are attributed to the geographic variability in HCC etiology and treatment availability, as previously mentioned. Therefore, the prescribed doses are expected to vary between studies even if only SBRT is used.
In general, fixed doses are employed for relatively small tumors with a median diameter of approximately 3 cm, e.g., 36 Gy/3 fractions or 40 Gy/5 fractions (Table 2). In contrast, modified doses are employed for relatively larger targets according to normal liver tolerance depending on tumor size and normal liver volume. Using normal tissue complication probability models[44], prescribed doses can be prospectively assigned while maintaining the same estimated risk of liver complication. With this approach, an iso-toxic SBRT regimen was developed at Princess Margaret Hospital at the University of Toronto[45]. The dose per fraction was determined based on the effective volume of normal liver irradiated (Veff). On a 6-fraction schedule, when the Veff was low (< 25%), doses of 54 Gy (9 Gy × 6) were delivered. For patients with a high Veff (25%-60%), doses from 30-45 Gy (5 to 7.5 Gy × 6) were delivered. In their phase I study of 102 HCC patients, the majority of whom had portal vein tumor thrombosis, the 1-year local control rate was 87%[30]. Univariate analysis revealed that higher SBRT doses were associated with higher local control (HR = 0.96; P = 0.02).
Both fixed-dose and variable-dose prescription approaches have their own rationale, and it is important to understand the differences in treatment intention (curative or semi-radical) and objectives (early or advanced). Two potential concepts may define the prescribed radiation dose: one is to deliver the maximum dose if dose constraints to the organs at risk are satisfied (the maximum tolerable dose); the other is to administer the necessary minimum dose with sufficient efficacy (the minimum effective dose, or, the ALARA: as low as reasonably achievable principal). The former concept appears to be suitable for larger tumors to maximize antitumor effects. In contrast, the latter concept may be reasonable for small HCCs, because intrahepatic recurrences frequently occur after treatment (68% in 5 years)[46] and they are repeatedly treated while underlying cirrhosis progressively develops over time.
It is also important to note that many reports include cholangiocarcinoma or metastatic liver tumors (Table 4); therefore, it is difficult to compare their survival with those who underwent resection and ablation[24,45,47-54]. While patients with liver metastatic disease have relatively normal liver function and tolerate radiation, patients with HCC have pre-existing liver dysfunction, and radiation tolerance is less well established. In addition, radiosensitivity of these tumors appears to be different[55]. While metastatic lung tumors (particularly those from colorectal cancer) are reported to require dose escalation due to relatively low radiosensitivity[56], increasing the dose for HCC tumors may not be necessary. In fact, in a study of 185 patients with HCC (median diameter, 27 mm) treated with SBRT of 35 Gy or 40 Gy in 5 fractions, both local control (91% and 89%, respectively; Log-rank P = 0.99) and overall survival (66% and 72%, respectively; P = 0.54) rates were equivalent between the two dose groups[43].
Table 4.
Studies of liver tumors including hepatocellular carcinoma, cholangiocarcinoma, and liver metastasis
| Ref. | Country | Study design | Tumors(patient number) | Median volume (mL) | Median size (cm) | Median dose (range)/fraction, Gy | Median follow-up (range) (mo) | Local control | Overall survival |
| Blomgren et al[24], 1995 | Sweden | Retrospective | HCC+CCC/metastasis(20/21) | 22 | - | Fixed30 Gy/2-3 fr | 11 | HCC + CCC: 100%Metastasis: 95% | - |
| Tse et al[28], 2008 | Canada | Phase I | HCC/CCC(31/10) | 173(9-1913) | - | VariableMedian 36 (24-54) Gy/6 fr | 18(11-39) | 65% (1 yr) | 48% (1 yr) |
| Herfarth et al[47], 2001 | Germany | Phase I-II | HCC/CCC(4/54) | 10 (1-132) | - | Dose escalation14-26 Gy/1 fr | 6(1-26) | 81%(18 mo) | - |
| Wulf et al[48], 2006 | Switzerland | Prospective | HCC + CCC/metastasis(5/51) | HCC+CCC: 14-516Metastasis: 9-355 | - | VariableLow dose:30 Gy/3 fr or28 Gy/4 frHigh dose: 36-38 Gy/3 fr or26 Gy/1 fr | HCC + CCC:15 (2-48)Metastasis:15 (2-85) | HCC + CCC: 100%Metastasis: 99% (1 yr), 66% (2 yr) | 72% (1 yr)32% (2 yr) |
| Méndez-Romero et al[49], 2006 | The Netherland | Retrospective | HCC/metastasis(11/34) | 22(10-322) | 3.2(0.5-7.2) | VariableNo cirrhosis and ≥ 4 cm: 37.5 Gy/3 frCirrhosis and< 4 cm: 25 Gy/5 fr or30 Gy/3 fr | 13(0.5-31) | 94% (1 yr)82% (2 yr) | HCC: 75%(1 yr), 40% (2 yr)Metastasis: 82% (1 yr), 54% (2 yr) |
| Iwata et al[50], 2010 | Japan(Nagoya City University) | Retrospective | HCC/metastasis(6/12) | - | 2.3(1.2-3.5) | Variable50 or 55 Gy/10 fr | 15 | 86% (1 yr) | 94% (1 yr) |
| Goodman et al[51], 2010 | United States (Memorial Sloan Kettering Cancer Center) | Phase I | HCC/metastasis(2/24) | 33(0.8-147) | Dose escalation18-30 Gy/1 fr | 17(2-55) | 77% (1 yr) | 50% (2 yr) | |
| Dewas et al[53], 2012 | France | Retrospective | HCC + CCC/metastasis(54/99) | 32(0.2-500) | 3.3(0.5-11) | Variable45 Gy/3 fr | 15(12-18) | 84% (1 yr)75% (2 yr) | - |
| Ibarra et al[54], 2012 | United States (Cleveland) | Retrospective, multicenter | HCC/CCC(21/11) | HCC: 334 (10-1914)CCC: 80 (31-819) | - | HCC: 22 (18-26) Gy/1 frCCC: 30 (22-30) Gy/1 fr | 13(0.5-54) | 84% (1 yr)75% (2 yr) | 87% (1 yr)55% (2 yr) |
CCC: Cholangiocarcinoma; HCC: Hepatocellular carcinoma.
Other factors may also affect treatment outcomes. Some reports on SBRT for HCC use TACE as a part of their treatment, or for validation of tumor location in each treatment session by visualizing the tumor with lipiodol on computed tomography (CT), while other reports treat patients with SBRT alone. In addition, since patients in most of the series were previously treated by other standard therapies, outcomes of these patients are much worse than those in whom surgery is performed as the first treatment. While achieving high local control rates (approximately 90%-100% in 2 years) with SBRT, the 2-year overall survival rates, which range from 52%-69%, seem to be compromised, most likely due to the inclusion of large tumors or heavily pretreated patients with repeated recurrences. In a retrospective analysis of 63 patients who had previously untreated HCC with a median tumor size of 2.6 cm, SBRT delivered 35-40 Gy in 5 fractions yielded 2- and 3-year local control rates of 95% and 92%, respectively, with a median follow-up duration of 31.1 mo[57]. In this study, the overall survival rate was 73% in 3 years, which was comparable to outcomes treated with surgery or percutaneous ablation, considering these candidates were medically unfit for radical therapies. In the Japanese Nationwide Survey, the 3-year overall survival rates of patients with solitary tumors ≤ 2 cm and 2-5 cm treated with resection were 83%-90% and 70%-81%, respectively. Those treated with percutaneous ablation were 82%-88% and 66%-82%, respectively[58]. According to these results, it is indicated that a high local control rate for SBRT similar to other standard local therapies can achieve equivalent overall survival.
TOXICITIES AFTER SBRT
Radiation-induced liver disease (RILD) is a dose-limiting complication of liver irradiation. This could be an important issue, particularly in patients with HCC, primarily in the context of underlying liver cirrhosis. Originally, RILD was thought to involve anicteric hepatomegaly, ascites, and elevated alkaline phosphatase typically occurring 2-12 mo after therapy. This endpoint can occur in patients who have otherwise fairly well functioning pretreatment livers and can be fatal once it occurs (“classic” RILD)[59]. Caution must be exercised in patients with HCC derived from pre-existing liver disease, because patients with more severe liver disease are significantly less likely to tolerate radiation[60], which can manifest as “nonclassic” RILD. A review article by Pan et al[59] referred to nonclassic RILD as ≥ Grade 3 elevated liver transaminases or worsening of Child-Pugh score by ≥ 2. However, information about nonclassic RILD remains limited, and the clinical significance of such liver toxicities has not been validated, particularly for hypofractionated SBRT.
In general, SBRT can be performed safely. In sequential phase I and II trials of SBRT of 24 to 54 Gy in 6 fractions for 102 locally advanced HCCs, ≥ Grade 3 toxicity was observed in 30% of patients. In these trials, there were seven deaths (7%) possibly related to treatment (1.1-7.7 mo after SBRT)[28]. In a large retrospective study of 185 HCC patients treated with SBRT of 35 or 40 Gy in 5 fractions, acute but transient ≥ Grade 3 toxicities were observed in 24 (13.0%) patients, and grade 5 liver failure occurred in 2 patients (1.3%)[43].
Another major concern of SBRT-induced complications involves gastrointestinal toxicity. Gastric or duodenal ulcer or perforation has been reported[38,40]. Such toxicities can be avoided when the target is approximately > 2 cm from the bowels. If the target is less than that distance, the dose or fraction size that can be delivered safely to the target often needs to be decreased to respect the radiation tolerance. In contrast, it appears that SBRT can be safely delivered to tumors located within or near the biliary system[26].
PATHOLOGICAL AND RADIOLOGICAL FEATURES OF HCC AND NORMAL LIVER AFTER SBRT
Effect of SBRT to normal liver parenchyma
Normal liver changes after high-dose irradiation have been recognized to have the histopathologic features of veno-occlusive disease (VOD)[61,62]. Olsen et al[22] reported on the histopathologic features underlying focal liver reactions to irradiation in 2 patients who underwent surgical resection following SBRT. They identified areas of radiation injury as having histologic characteristic of focal VOD with centrilobular congestion and fibrosis. These distinct areas were observed with clear demarcation between the irradiated and nonirradiated liver.
Radiographic normal tissue changes caused by irradiation have been described after SBRT in the absence of clinical manifestations of RILD. Most notable is a well-demarcated focal hypodensity of liver parenchyma that appears in the first few months after SBRT on CT, often referred to as focal liver reaction to radiation[22,63-65] (Figure 6). They typically present as sharply demarcated areas from the surrounding liver tissue, which presents, often enhanced, in the portal-venous or late phases. According to a report on radiation-induced focal liver reactions in cirrhotic livers evaluated on dynamic CT, it began at a median of 3 mo, peaked at 6 mo, and disappeared about 9 mo later, and these appearances remained for more than 12 mo in at least one-third of patients[64]. It is important that this type of reaction following SBRT to the liver is recognized, and it should not be misinterpreted as local recurrence, because the duration of tumor viability after SBRT overlaps with this time period[63,65].
Figure 6.
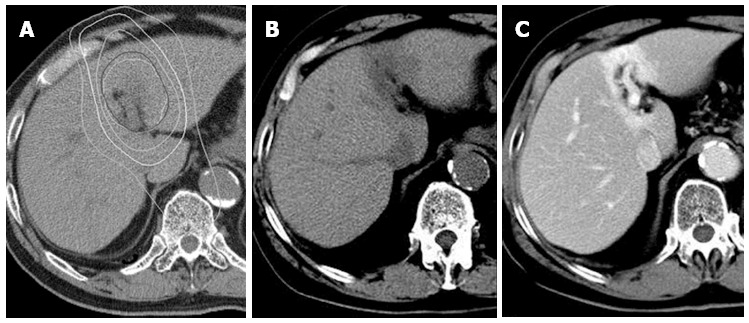
Typical focal liver reaction 3 mo after stereotactic body radiation therapy seen on computed tomography. An axial view of radiation dose distribution (A). The isodose lines (white lines) from inner to outer represent 40, 30, 20, and 10 Gy, respectively. Pre-enhancement computed tomography shows a low-density lesion corresponding to a high-dose area (B). A well-demarcated enhancement due to contrast retention indicating congestion is seen in portal phase (C).
Focal liver reaction has primarily been evaluated using CT, and it can also be recognized on magnetic resonance imaging (MRI). The role of the contrast agent gadoxetate acid (Gd-EOB-DTPA) for MRI in the detection and characterization of HCC has been an area of active laboratory and clinical research[66,67]. After intravenous injection, Gd-EOB-DTPA is gradually taken up by hepatocytes and is eventually excreted via the biliary pathway. Hepatocyte-phase Gd-EOB-DTPA-enhanced MRI can be used for the detection or characterization of hepatic lesions and potentially for the measurement of hepatocyte function. Figure 7 shows a clear demarcated focal liver reaction corresponding to a highly-irradiated area, seen as low signal intensity of adjacent liver parenchyma typically observed 1-6 mo after treatment in hepatobiliary phase images (15-20 min after Gd-EOB-DTPA injection).
Figure 7.
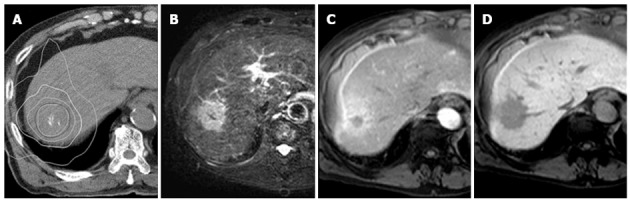
Typical focal liver reaction 4 mo after stereotactic body radiation therapy seen on gadoxetate acid-enhanced magnetic resonance imaging. An axial view of radiation dose distribution (A). The isodose lines (white lines) from inner to outer represent 40, 30, 20, and 10 Gy, respectively. A T2-weighted image shows a high-intensity area corresponding to a high-dose area (B), which is seen as an enhanced area in early phase after injection of gadoxetate acid (C). The hepatobiliary phase shows a well-demarcated low-intensity area (D).
Effect of SBRT to tumor
SBRT as a bridging therapy to orthotopic liver transplantation provided an opportunity to study the histopathologic features of tumors treated with SBRT[20,21,27]. According to these studies, this therapy can achieve a complete response rate of 27%. In contrast, most SBRT series reported a local control rate of 70%-100%, which implies that the effect of SBRT takes a considerable time to cause tumor cell death. Such discrepancy appears to be attributable to the difference in evaluation time; the interval between bridging SBRT to liver transplantation was approximately 4-7 mo while radiological response rate evaluation was performed at a median follow-up of approximately 12-24 mo. In fact, a retrospective study described the long-term imaging appearance of 42 small hypervascular HCCs following SBRT[68]. In this study, the complete response rate increased from 24% (n = 10) at 3 mo to 67% (n = 28) and 71% (n = 30) at 6 and 12 mo, respectively. The 2-year local control rate was 97% and the overall complete response rate at maximum follow-up was 93% (n = 39), yet three enhanced tumors persisted for more than 2 years without evidence of progression. Cautious and continuous observation until tumor regrowth is required to evaluate the true effect of this treatment.
FUTURE RESEARCH DIRECTIONS
The most common site of first recurrence was the liver outside the irradiated volume, providing the rationale for studies combining regional or systemic therapies with SBRT. The Radiation Therapy Oncology Group (RTOG) has initiated a phase III study of sorafenib vs SBRT followed by sorafenib in HCC (ClinicalTrials.gov identifier, NCT01730937). Eligible patients have locally advanced HCC that is unsuitable for resection, transplantation, or radiofrequency ablation, or is unsuitable for TACE or refractory to TACE (BCLC Intermediate [B] or Advanced [C]). Dozens of additional clinical trials utilizing SBRT for HCC are being conducted around the world, suggesting that it is a promising and actively investigated treatment option. Among these studies, a Japanese multicenter group is conducting a study of SBRT for previously untreated solitary HCC patients who are unfit for resection or ablation (primarily BCLC stage 0 and A). The results should provide new information about the effect of SBRT as an alternative option for early HCC.
In addition to conformal photon external-beam delivery, data suggest improved outcomes with proton or charged-particle therapies[69-71], particularly for large tumors. The optimal indication needs to be defined for SBRT and particle-beam therapies to separate the specific roles for each modality.
While the early outcomes of SBRT use in unresectable HCC are encouraging, further studies are required to validate these favorable results. A large, multi-institutional phase II study should be performed to evaluate the efficacy and toxicity of SBRT for unresectable HCC, as well as the feasibility of this treatment in a multi-institutional setting.
ACKNOWLEDGMENTS
Figures are generated from our own study which received an institutional review board approval in our institution.
Footnotes
P- Reviewers: Gong Y, Mihaila RG, Yan LN, Zhao HT S- Editor: Wen LL L- Editor: A E- Editor: Wang CH
References
- 1.Jemal A, Ward E, Hao Y, Thun M. Trends in the leading causes of death in the United States, 1970-2002. JAMA. 2005;294:1255–1259. doi: 10.1001/jama.294.10.1255. [DOI] [PubMed] [Google Scholar]
- 2.Forner A, Reig ME, de Lope CR, Bruix J. Current strategy for staging and treatment: the BCLC update and future prospects. Semin Liver Dis. 2010;30:61–74. doi: 10.1055/s-0030-1247133. [DOI] [PubMed] [Google Scholar]
- 3.Umemura T, Ichijo T, Yoshizawa K, Tanaka E, Kiyosawa K. Epidemiology of hepatocellular carcinoma in Japan. J Gastroenterol. 2009;44 Suppl 19:102–107. doi: 10.1007/s00535-008-2251-0. [DOI] [PubMed] [Google Scholar]
- 4.Bosetti C, Levi F, Boffetta P, Lucchini F, Negri E, La Vecchia C. Trends in mortality from hepatocellular carcinoma in Europe, 1980-2004. Hepatology. 2008;48:137–145. doi: 10.1002/hep.22312. [DOI] [PubMed] [Google Scholar]
- 5.Izumi R, Shimizu K, Ii T, Yagi M, Matsui O, Nonomura A, Miyazaki I. Prognostic factors of hepatocellular carcinoma in patients undergoing hepatic resection. Gastroenterology. 1994;106:720–727. doi: 10.1016/0016-5085(94)90707-2. [DOI] [PubMed] [Google Scholar]
- 6.Okuda K, Ohtsuki T, Obata H, Tomimatsu M, Okazaki N, Hasegawa H, Nakajima Y, Ohnishi K. Natural history of hepatocellular carcinoma and prognosis in relation to treatment. Study of 850 patients. Cancer. 1985;56:918–928. doi: 10.1002/1097-0142(19850815)56:4<918::aid-cncr2820560437>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 7.A new prognostic system for hepatocellular carcinoma: a retrospective study of 435 patients: the Cancer of the Liver Italian Program (CLIP) investigators. Hepatology. 1998;28:751–755. doi: 10.1002/hep.510280322. [DOI] [PubMed] [Google Scholar]
- 8.Kudo M, Chung H, Osaki Y. Prognostic staging system for hepatocellular carcinoma (CLIP score): its value and limitations, and a proposal for a new staging system, the Japan Integrated Staging Score (JIS score) J Gastroenterol. 2003;38:207–215. doi: 10.1007/s005350300038. [DOI] [PubMed] [Google Scholar]
- 9.Lo CM, Ngan H, Tso WK, Liu CL, Lam CM, Poon RT, Fan ST, Wong J. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002;35:1164–1171. doi: 10.1053/jhep.2002.33156. [DOI] [PubMed] [Google Scholar]
- 10.Llovet JM, Real MI, Montaña X, Planas R, Coll S, Aponte J, Ayuso C, Sala M, Muchart J, Solà R, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002;359:1734–1739. doi: 10.1016/S0140-6736(02)08649-X. [DOI] [PubMed] [Google Scholar]
- 11.Oliveri RS, Wetterslev J, Gluud C. Transarterial (chemo) embolisation for unresectable hepatocellular carcinoma (Review) New York: John Wiley & Sons, Ltd; 2012. [DOI] [PubMed] [Google Scholar]
- 12.Lin SM, Lin CJ, Lin CC, Hsu CW, Chen YC. Randomised controlled trial comparing percutaneous radiofrequency thermal ablation, percutaneous ethanol injection, and percutaneous acetic acid injection to treat hepatocellular carcinoma of 3 cm or less. Gut. 2005;54:1151–1156. doi: 10.1136/gut.2004.045203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miyayama S, Matsui O, Yamashiro M, Ryu Y, Kaito K, Ozaki K, Takeda T, Yoneda N, Notsumata K, Toya D, et al. Ultraselective transcatheter arterial chemoembolization with a 2-f tip microcatheter for small hepatocellular carcinomas: relationship between local tumor recurrence and visualization of the portal vein with iodized oil. J Vasc Interv Radiol. 2007;18:365–376. doi: 10.1016/j.jvir.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 14.Llovet JM. Updated treatment approach to hepatocellular carcinoma. J Gastroenterol. 2005;40:225–235. doi: 10.1007/s00535-005-1566-3. [DOI] [PubMed] [Google Scholar]
- 15.Sato T, Tateishi R, Yoshida H, Ohki T, Masuzaki R, Imamura J, Goto T, Kanai F, Obi S, Kato N, et al. Ultrasound surveillance for early detection of hepatocellular carcinoma among patients with chronic hepatitis C. Hepatol Int. 2009;3:544–550. doi: 10.1007/s12072-009-9145-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693–699. doi: 10.1056/NEJM199603143341104. [DOI] [PubMed] [Google Scholar]
- 17.de Villa V, Lo CM. Liver transplantation for hepatocellular carcinoma in Asia. Oncologist. 2007;12:1321–1331. doi: 10.1634/theoncologist.12-11-1321. [DOI] [PubMed] [Google Scholar]
- 18.European Association For The Study Of The Liver; European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908–943. doi: 10.1016/j.jhep.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 19.Dawson LA. Overview: Where does radiation therapy fit in the spectrum of liver cancer local-regional therapies? Semin Radiat Oncol. 2011;21:241–246. doi: 10.1016/j.semradonc.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 20.Katz AW, Chawla S, Qu Z, Kashyap R, Milano MT, Hezel AF. Stereotactic hypofractionated radiation therapy as a bridge to transplantation for hepatocellular carcinoma: clinical outcome and pathologic correlation. Int J Radiat Oncol Biol Phys. 2012;83:895–900. doi: 10.1016/j.ijrobp.2011.08.032. [DOI] [PubMed] [Google Scholar]
- 21.O’Connor JK, Trotter J, Davis GL, Dempster J, Klintmalm GB, Goldstein RM. Long-term outcomes of stereotactic body radiation therapy in the treatment of hepatocellular cancer as a bridge to transplantation. Liver Transpl. 2012;18:949–954. doi: 10.1002/lt.23439. [DOI] [PubMed] [Google Scholar]
- 22.Olsen CC, Welsh J, Kavanagh BD, Franklin W, McCarter M, Cardenes HR, Gaspar LE, Schefter TE. Microscopic and macroscopic tumor and parenchymal effects of liver stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys. 2009;73:1414–1424. doi: 10.1016/j.ijrobp.2008.07.032. [DOI] [PubMed] [Google Scholar]
- 23.Chi A, Liao Z, Nguyen NP, Xu J, Stea B, Komaki R. Systemic review of the patterns of failure following stereotactic body radiation therapy in early-stage non-small-cell lung cancer: clinical implications. Radiother Oncol. 2010;94:1–11. doi: 10.1016/j.radonc.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 24.Blomgren H, Lax I, Näslund I, Svanström R. Stereotactic high dose fraction radiation therapy of extracranial tumors using an accelerator. Clinical experience of the first thirty-one patients. Acta Oncol. 1995;34:861–870. doi: 10.3109/02841869509127197. [DOI] [PubMed] [Google Scholar]
- 25.Dawson LA, Eccles C, Bissonnette JP, Brock KK. Accuracy of daily image guidance for hypofractionated liver radiotherapy with active breathing control. Int J Radiat Oncol Biol Phys. 2005;62:1247–1252. doi: 10.1016/j.ijrobp.2005.03.072. [DOI] [PubMed] [Google Scholar]
- 26.Eriguchi T, Takeda A, Sanuki N, Oku Y, Aoki Y, Shigematsu N, Kunieda E. Acceptable toxicity after stereotactic body radiation therapy for liver tumors adjacent to the central biliary system. Int J Radiat Oncol Biol Phys. 2013;85:1006–1011. doi: 10.1016/j.ijrobp.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 27.Facciuto ME, Singh MK, Rochon C, Sharma J, Gimenez C, Katta U, Moorthy CR, Bentley-Hibbert S, Rodriguez-Davalos M, Wolf DC. Stereotactic body radiation therapy in hepatocellular carcinoma and cirrhosis: evaluation of radiological and pathological response. J Surg Oncol. 2012;105:692–698. doi: 10.1002/jso.22104. [DOI] [PubMed] [Google Scholar]
- 28.Tse RV, Hawkins M, Lockwood G, Kim JJ, Cummings B, Knox J, Sherman M, Dawson LA. Phase I study of individualized stereotactic body radiotherapy for hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J Clin Oncol. 2008;26:657–664. doi: 10.1200/JCO.2007.14.3529. [DOI] [PubMed] [Google Scholar]
- 29.Cárdenes HR, Price TR, Perkins SM, Maluccio M, Kwo P, Breen TE, Henderson MA, Schefter TE, Tudor K, Deluca J, et al. Phase I feasibility trial of stereotactic body radiation therapy for primary hepatocellular carcinoma. Clin Transl Oncol. 2010;12:218–225. doi: 10.1007/s12094-010-0492-x. [DOI] [PubMed] [Google Scholar]
- 30.Bujold A, Massey CA, Kim JJ, Brierley J, Cho C, Wong RK, Dinniwell RE, Kassam Z, Ringash J, Cummings B, et al. Sequential phase I and II trials of stereotactic body radiotherapy for locally advanced hepatocellular carcinoma. J Clin Oncol. 2013;31:1631–1639. doi: 10.1200/JCO.2012.44.1659. [DOI] [PubMed] [Google Scholar]
- 31.Kang JK, Kim MS, Cho CK, Yang KM, Yoo HJ, Kim JH, Bae SH, Jung da H, Kim KB, Lee DH, et al. Stereotactic body radiation therapy for inoperable hepatocellular carcinoma as a local salvage treatment after incomplete transarterial chemoembolization. Cancer. 2012;118:5424–5431. doi: 10.1002/cncr.27533. [DOI] [PubMed] [Google Scholar]
- 32.Choi BO, Jang HS, Kang KM, Lee SW, Kang YN, Chai GY, Choi IB. Fractionated stereotactic radiotherapy in patients with primary hepatocellular carcinoma. Jpn J Clin Oncol. 2006;36:154–158. doi: 10.1093/jjco/hyi236. [DOI] [PubMed] [Google Scholar]
- 33.Choi BO, Choi IB, Jang HS, Kang YN, Jang JS, Bae SH, Yoon SK, Chai GY, Kang KM. Stereotactic body radiation therapy with or without transarterial chemoembolization for patients with primary hepatocellular carcinoma: preliminary analysis. BMC Cancer. 2008;8:351. doi: 10.1186/1471-2407-8-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Louis C, Dewas S, Mirabel X, Lacornerie T, Adenis A, Bonodeau F, Lartigau E. Stereotactic radiotherapy of hepatocellular carcinoma: preliminary results. Technol Cancer Res Treat. 2010;9:479–487. doi: 10.1177/153303461000900506. [DOI] [PubMed] [Google Scholar]
- 35.Kwon JH, Bae SH, Kim JY, Choi BO, Jang HS, Jang JW, Choi JY, Yoon SK, Chung KW. Long-term effect of stereotactic body radiation therapy for primary hepatocellular carcinoma ineligible for local ablation therapy or surgical resection. Stereotactic radiotherapy for liver cancer. BMC Cancer. 2010;10:475. doi: 10.1186/1471-2407-10-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Seo YS, Kim MS, Yoo SY, Cho CK, Choi CW, Kim JH, Han CJ, Park SC, Lee BH, Kim YH, et al. Preliminary result of stereotactic body radiotherapy as a local salvage treatment for inoperable hepatocellular carcinoma. J Surg Oncol. 2010;102:209–214. doi: 10.1002/jso.21593. [DOI] [PubMed] [Google Scholar]
- 37.Andolino DL, Johnson CS, Maluccio M, Kwo P, Tector AJ, Zook J, Johnstone PA, Cardenes HR. Stereotactic body radiotherapy for primary hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2011;81:e447–e453. doi: 10.1016/j.ijrobp.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 38.Huang WY, Jen YM, Lee MS, Chang LP, Chen CM, Ko KH, Lin KT, Lin JC, Chao HL, Lin CS, et al. Stereotactic body radiation therapy in recurrent hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2012;84:355–361. doi: 10.1016/j.ijrobp.2011.11.058. [DOI] [PubMed] [Google Scholar]
- 39.Honda Y, Kimura T, Aikata H, Kobayashi T, Fukuhara T, Masaki K, Nakahara T, Naeshiro N, Ono A, Miyaki D, et al. Stereotactic body radiation therapy combined with transcatheter arterial chemoembolization for small hepatocellular carcinoma. J Gastroenterol Hepatol. 2013;28:530–536. doi: 10.1111/jgh.12087. [DOI] [PubMed] [Google Scholar]
- 40.Bae SH, Kim MS, Cho CK, Kim KB, Lee DH, Han CJ, Park SC, Kim YH. Feasibility and efficacy of stereotactic ablative radiotherapy for Barcelona Clinic Liver Cancer-C stage hepatocellular carcinoma. J Korean Med Sci. 2013;28:213–219. doi: 10.3346/jkms.2013.28.2.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xi M, Zhang L, Zhao L, Li QQ, Guo SP, Feng ZZ, Deng XW, Huang XY, Liu MZ. Effectiveness of stereotactic body radiotherapy for hepatocellular carcinoma with portal vein and/or inferior vena cava tumor thrombosis. PLoS One. 2013;8:e63864. doi: 10.1371/journal.pone.0063864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fuss M, Thomas CR. Stereotactic body radiation therapy: an ablative treatment option for primary and secondary liver tumors. Ann Surg Oncol. 2004;11:130–138. doi: 10.1245/aso.2004.10.907. [DOI] [PubMed] [Google Scholar]
- 43.Sanuki N, Takeda A, Oku Y, Mizuno T, Aoki Y, Eriguchi T, Iwabuchi S, Kunieda E. Stereotactic body radiotherapy for small hepatocellular carcinoma: A retrospective outcome analysis in 185 patients. Acta Oncol. 2014;53:399–404. doi: 10.3109/0284186X.2013.820342. [DOI] [PubMed] [Google Scholar]
- 44.Ben-Josef E, Normolle D, Ensminger WD, Walker S, Tatro D, Ten Haken RK, Knol J, Dawson LA, Pan C, Lawrence TS. Phase II trial of high-dose conformal radiation therapy with concurrent hepatic artery floxuridine for unresectable intrahepatic malignancies. J Clin Oncol. 2005;23:8739–8747. doi: 10.1200/JCO.2005.01.5354. [DOI] [PubMed] [Google Scholar]
- 45.Dawson LA, Eccles C, Craig T. Individualized image guided iso-NTCP based liver cancer SBRT. Acta Oncol. 2006;45:856–864. doi: 10.1080/02841860600936369. [DOI] [PubMed] [Google Scholar]
- 46.Okuwaki Y, Nakazawa T, Shibuya A, Ono K, Hidaka H, Watanabe M, Kokubu S, Saigenji K. Intrahepatic distant recurrence after radiofrequency ablation for a single small hepatocellular carcinoma: risk factors and patterns. J Gastroenterol. 2008;43:71–78. doi: 10.1007/s00535-007-2123-z. [DOI] [PubMed] [Google Scholar]
- 47.Herfarth KK, Debus J, Lohr F, Bahner ML, Rhein B, Fritz P, Höss A, Schlegel W, Wannenmacher MF. Stereotactic single-dose radiation therapy of liver tumors: results of a phase I/II trial. J Clin Oncol. 2001;19:164–170. doi: 10.1200/JCO.2001.19.1.164. [DOI] [PubMed] [Google Scholar]
- 48.Wulf J, Hädinger U, Oppitz U, Thiele W, Ness-Dourdoumas R, Flentje M. Stereotactic radiotherapy of targets in the lung and liver. Strahlenther Onkol. 2001;177:645–655. doi: 10.1007/pl00002379. [DOI] [PubMed] [Google Scholar]
- 49.Méndez Romero A, Wunderink W, Hussain SM, De Pooter JA, Heijmen BJ, Nowak PC, Nuyttens JJ, Brandwijk RP, Verhoef C, Ijzermans JN, et al. Stereotactic body radiation therapy for primary and metastatic liver tumors: A single institution phase i-ii study. Acta Oncol. 2006;45:831–837. doi: 10.1080/02841860600897934. [DOI] [PubMed] [Google Scholar]
- 50.Iwata H, Shibamoto Y, Hashizume C, Mori Y, Kobayashi T, Hayashi N, Kosaki K, Ishikawa T, Kuzuya T, Utsunomiya S. Hypofractionated stereotactic body radiotherapy for primary and metastatic liver tumors using the novalis image-guided system: preliminary results regarding efficacy and toxicity. Technol Cancer Res Treat. 2010;9:619–627. doi: 10.1177/153303461000900610. [DOI] [PubMed] [Google Scholar]
- 51.Goodman KA, Wiegner EA, Maturen KE, Zhang Z, Mo Q, Yang G, Gibbs IC, Fisher GA, Koong AC. Dose-escalation study of single-fraction stereotactic body radiotherapy for liver malignancies. Int J Radiat Oncol Biol Phys. 2010;78:486–493. doi: 10.1016/j.ijrobp.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 52.Gunvén P, Jonas E, Blomgren H, Rutkowska E, Karlsson K, Lax I, Levitt S. Undetectable late hepatic sequelae after hypofractionated stereotactic radiotherapy for liver tumors. Med Oncol. 2011;28:958–965. doi: 10.1007/s12032-010-9567-3. [DOI] [PubMed] [Google Scholar]
- 53.Dewas S, Bibault JE, Mirabel X, Fumagalli I, Kramar A, Jarraya H, Lacornerie T, Dewas-Vautravers C, Lartigau E. Prognostic factors affecting local control of hepatic tumors treated by Stereotactic Body Radiation Therapy. Radiat Oncol. 2012;7:166. doi: 10.1186/1748-717X-7-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ibarra RA, Rojas D, Snyder L, Yao M, Fabien J, Milano M, Katz A, Goodman K, Stephans K, El-Gazzaz G, et al. Multicenter results of stereotactic body radiotherapy (SBRT) for non-resectable primary liver tumors. Acta Oncol. 2012;51:575–583. doi: 10.3109/0284186X.2011.652736. [DOI] [PubMed] [Google Scholar]
- 55.van Laarhoven HW, Kaanders JH, Lok J, Peeters WJ, Rijken PF, Wiering B, Ruers TJ, Punt CJ, Heerschap A, van der Kogel AJ. Hypoxia in relation to vasculature and proliferation in liver metastases in patients with colorectal cancer. Int J Radiat Oncol Biol Phys. 2006;64:473–482. doi: 10.1016/j.ijrobp.2005.07.982. [DOI] [PubMed] [Google Scholar]
- 56.Takeda A, Kunieda E, Ohashi T, Aoki Y, Koike N, Takeda T. Stereotactic body radiotherapy (SBRT) for oligometastatic lung tumors from colorectal cancer and other primary cancers in comparison with primary lung cancer. Radiother Oncol. 2011;101:255–259. doi: 10.1016/j.radonc.2011.05.033. [DOI] [PubMed] [Google Scholar]
- 57.Takeda A, Sanuki N, Eriguchi T, Kobayashi T, Iwabutchi S, Matsunaga K, Mizuno T, Yashiro K, Nisimura S, Kunieda E. Stereotactic ablative body radiotherapy for previously untreated solitary hepatocellular carcinoma. J Gastroenterol Hepatol. 2014;29:372–379. doi: 10.1111/jgh.12350. [DOI] [PubMed] [Google Scholar]
- 58.Arii S, Sata M, Sakamoto M, Shimada M, Kumada T, Shiina S, Yamashita T, Kokudo N, Tanaka M, Takayama T, et al. Management of hepatocellular carcinoma: Report of Consensus Meeting in the 45th Annual Meeting of the Japan Society of Hepatology (2009) Hepatol Res. 2010;40:667–685. doi: 10.1111/j.1872-034X.2010.00673.x. [DOI] [PubMed] [Google Scholar]
- 59.Pan CC, Kavanagh BD, Dawson LA, Li XA, Das SK, Miften M, Ten Haken RK. Radiation-associated liver injury. Int J Radiat Oncol Biol Phys. 2010;76:S94–100. doi: 10.1016/j.ijrobp.2009.06.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xu ZY, Liang SX, Zhu J, Zhu XD, Zhao JD, Lu HJ, Yang YL, Chen L, Wang AY, Fu XL, et al. Prediction of radiation-induced liver disease by Lyman normal-tissue complication probability model in three-dimensional conformal radiation therapy for primary liver carcinoma. Int J Radiat Oncol Biol Phys. 2006;65:189–195. doi: 10.1016/j.ijrobp.2005.11.034. [DOI] [PubMed] [Google Scholar]
- 61.Ingold JA, Reed GB, Kaplan HS, Bagshaw MA. Radiation hepatitis. Am J Roentgenol Radium Ther Nucl Med. 1965;93:200–208. [PubMed] [Google Scholar]
- 62.Reed GB, Cox AJ. The human liver after radiation injury. A form of veno-occlusive disease. Am J Pathol. 1966;48:597–611. [PMC free article] [PubMed] [Google Scholar]
- 63.Herfarth KK, Hof H, Bahner ML, Lohr F, Höss A, van Kaick G, Wannenmacher M, Debus J. Assessment of focal liver reaction by multiphasic CT after stereotactic single-dose radiotherapy of liver tumors. Int J Radiat Oncol Biol Phys. 2003;57:444–451. doi: 10.1016/s0360-3016(03)00586-8. [DOI] [PubMed] [Google Scholar]
- 64.Sanuki-Fujimoto N, Takeda A, Ohashi T, Kunieda E, Iwabuchi S, Takatsuka K, Koike N, Shigematsu N. CT evaluations of focal liver reactions following stereotactic body radiotherapy for small hepatocellular carcinoma with cirrhosis: relationship between imaging appearance and baseline liver function. Br J Radiol. 2010;83:1063–1071. doi: 10.1259/bjr/74105551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Takeda A, Oku Y, Sanuki N, Kunieda E, Koike N, Aoki Y, Ohashi T, Iwabuchi S, Takatsuka K, Takeda T, et al. Dose volume histogram analysis of focal liver reaction in follow-up multiphasic CT following stereotactic body radiotherapy for small hepatocellular carcinoma. Radiother Oncol. 2012;104:374–378. doi: 10.1016/j.radonc.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 66.Asayama Y, Tajima T, Nishie A, Ishigami K, Kakihara D, Nakayama T, Okamoto D, Fujita N, Aishima S, Shirabe K, et al. Uptake of Gd-EOB-DTPA by hepatocellular carcinoma: radiologic-pathologic correlation with special reference to bile production. Eur J Radiol. 2011;80:e243–e248. doi: 10.1016/j.ejrad.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 67.Tamada T, Ito K, Sone T, Kanki A, Sato T, Higashi H. Gd-EOB-DTPA enhanced MR imaging: evaluation of biliary and renal excretion in normal and cirrhotic livers. Eur J Radiol. 2011;80:e207–e211. doi: 10.1016/j.ejrad.2010.08.033. [DOI] [PubMed] [Google Scholar]
- 68.Sanuki N, Takeda A, Mizuno T, Oku Y, Eriguchi T, Iwabuchi S, Kunieda E. Tumor response on CT following hypofractionated stereotactic ablative body radiotherapy for small hypervascular hepatocellular carcinoma with cirrhosis. AJR Am J Roentgenol. 2013;201:W812–W820. doi: 10.2214/AJR.12.10169. [DOI] [PubMed] [Google Scholar]
- 69.Mizumoto M, Okumura T, Hashimoto T, Fukuda K, Oshiro Y, Fukumitsu N, Abei M, Kawaguchi A, Hayashi Y, Ookawa A, et al. Proton beam therapy for hepatocellular carcinoma: a comparison of three treatment protocols. Int J Radiat Oncol Biol Phys. 2011;81:1039–1045. doi: 10.1016/j.ijrobp.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 70.Fukumitsu N, Sugahara S, Nakayama H, Fukuda K, Mizumoto M, Abei M, Shoda J, Thono E, Tsuboi K, Tokuuye K. A prospective study of hypofractionated proton beam therapy for patients with hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2009;74:831–836. doi: 10.1016/j.ijrobp.2008.10.073. [DOI] [PubMed] [Google Scholar]
- 71.Skinner HD, Hong TS, Krishnan S. Charged-particle therapy for hepatocellular carcinoma. Semin Radiat Oncol. 2011;21:278–286. doi: 10.1016/j.semradonc.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhang W, Zhang J, Yan W, You G, Bao Z, Li S, Kang C, Jiang C, You Y, Zhang Y, et al. Whole-genome microRNA expression profiling identifies a 5-microRNA signature as a prognostic biomarker in Chinese patients with primary glioblastoma multiforme. Cancer. 2013;119:814–824. doi: 10.1002/cncr.27826. [DOI] [PubMed] [Google Scholar]


