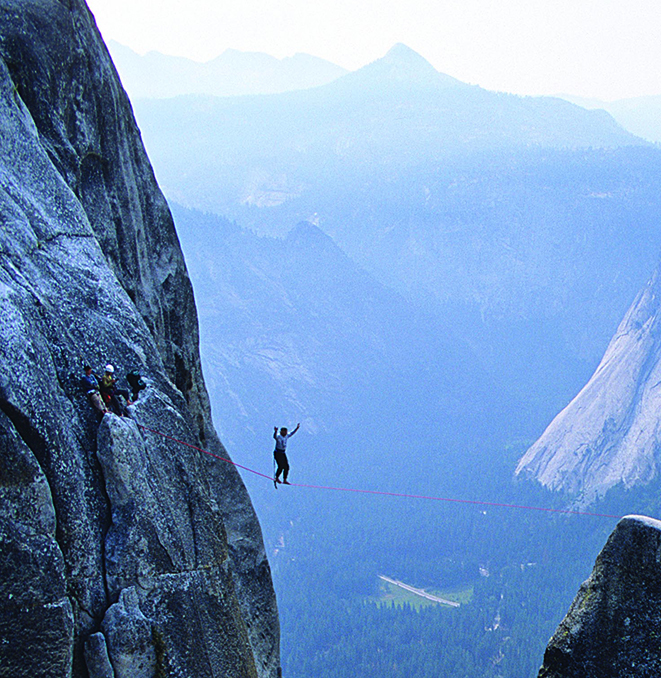
On 30 June 1859 Charles Blondin successfully crossed the 340 metre span of the Niagara gorge on a tightrope suspended 50 metres above the rushing water. As if this wasn’t enough, he repeated the feat several times over the next few months with some added twists: he crossed on stilts, he crossed blindfolded, he carried a stove across and made an omelette on it, and then he pushed a wheelbarrow across. On reaching the other side he apparently asked the rapturous crowd whether they believed he could push a man across in the wheelbarrow. Their affirmative cheers drowned out the roaring river, but when he asked for a volunteer they fell silent ...
INTRODUCING PATIENT SAFETY
The emerging field of patient safety already has some very apt metaphors. Reason’s ‘Swiss Cheese’ model suggests patients suffer preventable harm when a number of holes (system weaknesses) temporarily align; high profile media reports of serious patient safety incidents (PSIs) are the ‘tip of the iceberg’; while the Indian fable of the blind men interacting with different parts of an elephant illustrates how perceptions of safe care varies between patients, clinicians, researchers, and policymakers. We can add another parallel: delivering safe care in general practice is like balancing on tightropes. Increasing numbers of patients scamper willingly into our wheelbarrows every day, with the full expectation that we will deliver them safely (and quickly) to the other side. And for the most part we do, even if it increasingly requires running back and forth or hanging on precariously by one arm from the rope.
Unfortunately, slips and accidents do happen on tightropes, as they do in health care. While patient harm in general practice is yet to be reliably quantified, there is compelling evidence that it does occur, and not infrequently.1 Hardly surprising, many would say, given the associated complexity and uncertainty, and the high risk and dynamic nature of the job. However, many PSIs are judged as preventable. Implicit in this knowledge is the assumption that there should be a strong imperative to further improve patient safety.
IMPROVING THE SAFETY OF CARE
A number of established strategies exist to help improve clinical effectiveness and enhance patient safety including, for example, the Quality & Outcomes Framework (QOF), appraisal, revalidation, and significant event analysis (SEA). However, efforts are hampered by variations in standards of clinical practices, the availability of good IT infrastructure, poor care system designs, and limited safety science knowledge among the workforce. It is accepted, therefore, that there are no ‘magic bullets’, and that mixed-methods improvement approaches are apposite including strategic prioritisation at the national level. Accordingly, the UK home countries are implementing formal patient safety initiatives, albeit with different approaches.
In Scotland, for example, a recent 2-year Health Foundation funded collaborative facilitated the testing of the trigger review method, safety climate assessment, and clinical care bundles in around 60 practices in four NHS Boards. Building on this, the Scottish Patient Safety Programme for Primary Care (SPSP-PC) was then launched in March 2013. Consequently, all Scottish general practices are now QOF-incentivised to periodically measure safety climate perceptions and perform trigger reviews of the records of high risk patient groups. On the horizon, newer interventions such as a human factors-based approach to SEA, safe systems guidance for managing laboratory results, and a ‘never event’ list are in development as further possibilities for focusing greater attention on patient safety.
The effectiveness of specific interventions to reliably reduce harm in general practice remains unknown. In hospital care, patient safety has improved for selected clinical conditions managed in specialised units as part of national improvement programmes. However, improvements are seldom sustained or spread and are dependent on many highly context-specific factors. It is true that the safety glass today is ‘fuller than it seems’ but there is limited evidence that health care overall is substantially safer today than it was 15 years ago, despite much effort, investment, and rhetoric.2,3 The problem of patient safety is proving to be a far tougher nut to crack than many had envisioned.
To illustrate why, let us consider three issues which often contribute to preventable patient harm: diagnostic error; prescribing error; and errors during care transitions.
DIAGNOSTIC ERROR
Diagnostic error is the major reason for malpractice claims. Around half of all claims are successful, and the current lifetime risk of a claim against a GP is 12%; although recent annual figures show an upward trend in claims, suggesting even greater risk.4 If we imagine clinicians navigate virtual tightropes during successive consultations, committing a diagnostic error would be like lurching to the left of the rope or even plunging over the edge. To compensate, balance is shifted to the right; for example, practising ‘defensive medicine’. This risks overdiagnosis, which is associated with significant patient harm and squandering of limited resources: the annual financial cost of overdiagnosis in the US, for example, is estimated at over $200 billion.5
PRESCRIBING ERROR
In general practice, prescribing errors are the most common type made by clinicians. Older, frail patients are especially at risk of adverse drug events and in some UK nursing homes medication errors have been detected in three-quarters of patient records with a mean of 1.9 errors per resident.6 Inappropriate prescribing has become synonymous with polypharmacy. However, it equally applies to instances where drug treatments have not been optimised.
ERRORS DURING CARE TRANSITIONS
Approximately one in five patients are readmitted within 30 days of their hospital discharge, with up to 60% of these considered preventable.7 The most important reasons for readmissions are poor transition planning and unmet social needs, but there are on average more than eight different factors associated with all aspects of care from the index stay through the discharge process to delivery of follow-up care. The current expectation that GPs should do more to prevent readmissions by performing compensatory clinical balancing acts (for example, reviewing all patients soon after discharge) seems intuitively sensible and worthwhile, even though it requires re-allocating scarce resources (including time). However, in reality this may have had the paradoxical and unintended consequence in some instances of increasing the rate of readmissions, while many important risk factors simply are not under the control of GPs.
THE WAY FORWARD (AND ACROSS)
The tightrope analogy demonstrates that safety cannot be assured or improved simply by adopting the opposite behaviour to that which may have (inadvertently) led to error, nor by relying on intuition about what may (or may not) work, or placing all of our hope and trust in the ability of individual clinicians, however skilled and capable. To reliably improve patient safety in general practice will require action on at least three fronts.
Firstly, greater evidence-based knowledge of patient safety science in general practice is needed. This task is underway, with funded networking activity and research at the pan-European level and in England to develop a patient safety toolkit for general practice.8 Additional evidence should also be sourced from formal evaluations of the development and testing of all safety interventions, specifically to identify context-specific factors that facilitate or hinder improvement and provide a cost analysis (return-on-investment). This is essential to reconcile policy rhetoric with the frontline reality, and reliably answer what works, how, for whom, and to what extent?
Secondly, for clinicians to engage with and normalise care improvement approaches as part of their ‘day-to-day’ practice, they need ‘to set aside time and space to conduct the required, appropriate reflection effectively’.9 This sounds deceptively simple. However, protected time is subject to political vagaries and comes at an opportunity cost meaning other competing service priorities may be forsaken; while time allocation decisions of this sort are not always under the full control of many clinicians.
The third ingredient is a strong safety culture within practices, which will only increase in importance as complex health and social care is increasingly delivered by multiprofessional teams in larger organisational premises. High-performing teams are characterised by excellent leadership, effective communication, and team members who support each other and learn together: all are vital components that contribute towards a positive safety culture.
CONCLUSIONS
‘Safety’ is often defined as a condition where ‘nothing goes wrong’, which is a fine description of a successful aeroplane journey or an incident-free day at a nuclear power plant.10 However, in the general practice context, this translational meaning of safety is improbable. Perhaps it is more realistic at the outset, therefore, to focus our safety improvement efforts on known issues that can be prevented, such as the preliminary list of never events reported in the BJGP last month.11 Irrespective of the starting point though, the necessary supporting work to further improve care will require protected time, clinician and management engagement, system-centred redesign, good quality data, a strong and just safety culture, and, above all else, a keen sense of balance.
Postscript
In August 1859 Charles Blondin crossed the Niagara gorge while carrying his manager on his back.
Provenance
Commissioned; not externally peer reviewed.
REFERENCES
- 1.Tsang C, Majeed A, Banarsee R, et al. Recording of adverse events in English general practice: analysis of data from electronic patient records. Inform Prim Care. 2010;18(2):117–124. doi: 10.14236/jhi.v18i2.761. [DOI] [PubMed] [Google Scholar]
- 2.Pronovost PJ, Wachter RM. Progress in patient safety: a glass fuller than it seems. Am J Med Qual. 2014;29(2):165–169. doi: 10.1177/1062860613495554. [DOI] [PubMed] [Google Scholar]
- 3.Landrigan CP, Parry GJ, Bones CB, et al. Temporal trends in rates of patient harm resulting from medical care. N Engl J Med. 2010;363:2124–2134. doi: 10.1056/NEJMsa1004404. [DOI] [PubMed] [Google Scholar]
- 4.Wallace E, Lowry J, Smith SM, Fahey T. The epidemiology of malpractice claims in primary care: a systematic review. BMJ Open. 2013;3(7):e002929. doi: 10.1136/bmjopen-2013-002929. pii: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moynihan R, Doust J, Henry D. Preventing overdiagnosis: how to stop harming the healthy. BMJ. 2012;344:e3502. doi: 10.1136/bmj.e3502. [DOI] [PubMed] [Google Scholar]
- 6.Opondo D, Eslami S, Visscher S, et al. Inappropriateness of medication prescriptions to elderly patients in the primary care settings: a systematic review. PLoS One. 2012;7(8):e43617. doi: 10.1371/journal.pone.0043617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feigenbaum P, Neuwirth E, Trowbridge L, et al. Factors contributing to all-cause 30-day readmissions a structured case series across 18 hospitals. Med Care. 2012;50(7):599–605. doi: 10.1097/MLR.0b013e318249ce72. [DOI] [PubMed] [Google Scholar]
- 8. LINNEAUS EURO-PC. Learning from international networks about errors and understanding safety in primary care. http://www.linneaus-pc.eu/index.html (accessed 11 Mar 2014).
- 9.Jacobson L, Elwyn G, Robling M, Jones RT. Error and safety in primary care: no clear boundaries. Fam Pract. 2003;20(3):237–241. doi: 10.1093/fampra/cmg302. [DOI] [PubMed] [Google Scholar]
- 10.Hollnagel E. Is safety a subject for science? Safety Science. 2014 in press. [Google Scholar]
- 11.De Wet C, O’Donnell C, Bowie P. Development of a preliminary ‘never event’ list for general practice using consensus-building methods. Br J Gen Pract. 2014 doi: 10.3399/bjgp14X677536. [DOI] [PMC free article] [PubMed] [Google Scholar]


