Abstract
Purpose
This study aims to evaluate the long-term consistency of satisfaction with contralateral prophylactic mastectomy (CPM) and adverse psychosocial effects as well as to explore the effect of informed decision-making, personality traits, and quality of life (QOL) on satisfaction.
Methods
A previously established cohort of women with unilateral breast cancer who had undergone CPM between 1960 and 1993 were surveyed using study-specific and standardized questionnaires at two follow-up time points. The first survey was a mean of 10.7 years and the second survey a mean of 20.2 years after CPM.
Results
487 of the 583 women who responded to the first study were alive and resurveyed. Data from both surveys were available for 269 women. With longer follow-up, there was a small increase in the percentage of women satisfied (90%) and those who would choose CPM again (92%) (4% and 2% increase from first survey, respectively). Most adversely affected were body appearance (31%), feelings of femininity (24%), and sexual relationships (23%). Ninety-three percent of women felt they had made an informed decision. Perception of making an informed choice and current QOL were moderately associated with satisfaction with CPM (r = 0.37 and 0.37, respectively) while associations with trait anxiety and optimism were weak (r = 0.27 and 0.21, respectively).
Conclusions
Long-term satisfaction and adverse effects remained remarkably stable. It is important that women fully understand the benefits and adverse effects associated with CPM.
Contralateral prophylactic mastectomy (CPM) is an effective contralateral breast cancer risk-reduction approach, reducing risk by approximately 90–95%.1–5 Over recent years the proportion of patients undergoing mastectomy for breast cancer who elect CPM has significantly increased for both invasive and noninvasive breast cancer.6–8 However, this procedure is not without negative consequences. The most frequently cited adverse effects include difficulty with body appearance/image or feelings of femininity and sexual relationships.9–11 Despite these adverse effects, the majority of women, when surveyed one to several years after their procedure, are satisfied with their decision to pursue CPM and would elect CPM again.10–12
Several variables have been associated with the level of satisfaction/dissatisfaction or regret with CPM. These include level of satisfaction with body appearance, reconstruction and reconstruction-related complications, increased stress, and not being fully informed regarding options.10,13 No studies to date have examined the association between personality traits and satisfaction with CPM, despite several researchers’ notation about the potential importance of personality traits.10,14 If select personality traits are more strongly associated with dissatisfaction with CPM, additional decision support could be provided to individuals with those traits.
No studies have explored the consistency of satisfaction with CPM or the adverse effects experienced over time. This study aims to evaluate the long-term consistency of satisfaction with CPM and adverse psychological and social effects as well as to explore the effect of informed decision-making, personality traits, and quality of life (QOL) on satisfaction.
PATIENTS AND METHODS
Patient Cohort
A previously established cohort of 621 women with stage 0, I or II unilateral breast cancer and breast cancer family history who underwent CPM between 1960 and 1993 at Mayo Clinic Rochester received our first follow-up survey, and 583 responded.10 Of these women, 487 were alive and received a second follow-up survey approximately 10 years later. Nonresponders received a subsequent mailing followed by telephone contact. Of the 487 women, 269 (55%) responded to the second survey; subjects with data from both surveys formed our analysis sample. Medical record review collected demographic, medical, and procedure variables. The Mayo Clinic Institutional Review Board approved this study.
Questionnaire
The first follow-up survey utilized a study-specific questionnaire, while the second follow-up survey additionally included several standardized scales used to measure body image, optimism–pessimism, trait anxiety, decisional conflict, health concern, health distress, and quality of life.10
The original study-specific questionnaire was developed to meet the needs of a retrospective study with no baseline data. We used single-item ordinal scales for satisfaction with CPM, choice to have CPM again, overall quality of life, and how the following psychological and social variables were affected by CPM: self-esteem, body appearance, feelings of femininity, sexual relationships, and emotional stability. Satisfaction with CPM and choice to have CPM again were rated on a five-point ordinal scale. Open-ended questions were used to elicit the basis for their satisfaction with CPM and choice to have CPM again. Overall quality of life was rated on a 10-point ordinal scale ranging from “As bad as it can be” to “As good as it can be.” Question clarity, inclusiveness, and face validity were established by a panel of experts employed in the fields of medicine, psychology, nursing, survey research, and biostatistics and piloted with women who had prophylactic mastectomy for inclusiveness and clarity of items.
Several previously established, validated, and reliable scales were utilized in the second follow-up survey. The Body Image Scale was developed for use with individuals with a cancer diagnosis.15 The Medical Outcome Study subscales were used to measure health concerns and health distress.16 Anxiety-proneness considered intrinsic to one’s personality was measured using Spielberger’s trait anxiety scale.17 The personality factors of optimism/pessimism were measured using the Revised Life Orientation Test.18,19 The Decisional Conflict Scale Satisfaction Sub-scale was used to measure satisfaction with decision and if the choice was informed and reflected what is important to the patient.20
Data Analysis
Data were summarized using descriptive statistics. Paired comparisons between the first and second surveys were performed using McNemar’s test of paired proportions for dichotomous variables and paired t-tests for continuous and ordinal variables. Comparisons between groups, including between survey responders and nonresponders, are reported using chi-square tests or two-sample t-tests. We collapsed the psychological and social function items into adverse effect or no adverse effect, with the latter including no change or favorable effect responses. Univariate associations were estimated using Pearson correlation coefficients. Individual item nonresponse was <5% of the analysis sample for most questions and <10% in all cases. P values <0.05 were considered statistically significant. Analysis was performed using SAS (version 9.2; SAS Institute Inc., Cary, NC). Open-ended questions were coded for themes and concepts by two coders who discussed any discrepancies and came to agreement, and frequencies were tabulated.
RESULTS
The first survey was completed a mean of 10.7 years after CPM (range 1.9–35.4 years), and the second survey a mean of 20.2 years after CPM (range 11.4–44.5 years). These women were diagnosed with their index breast cancer between 1960 and 1993 and underwent CPM during the same time period. Women’s mean age at CPM was 47.4 years, while the mean ages at first and second surveys were 58.1 and 67.5 years, respectively (Table 1). In addition to age, marital status changed significantly (88% and 79% married, respectively, P < 0.0001) between the first and second surveys. Satisfaction at second follow-up was not associated with age at CPM, age at survey, marital status, time since procedure, reasons for electing CPM, or immediate versus delayed reconstruction.
TABLE 1.
Demographic and surgical variables
| Variable | N = 269 |
|---|---|
| Age at CPM, years, mean (range) | 47.4 (24.1, 75.3) |
| Age at 1st survey, years, mean (range) | 58.1 (31.7, 84.3) |
| Age at 2nd survey, years, mean (range) | 67.5 (41.8, 94.0) |
| Marital statusa, n (%) | |
| Married | 213 (79.2) |
| Single | 6 (2.2) |
| Divorced/separated | 19 (7.1) |
| Widowed | 28 (10.4) |
| Unknown | 3 (1.1) |
| Stated reason(s) for electing CPMb, n (%) | |
| Cancer in other breast | 202 (75.1) |
| Physician’s advice | 150 (55.8) |
| Family history | 120 (44.6) |
| Lumpy breasts | 79 (29.4) |
| Alleviate worry | 67 (24.9) |
| Others | 73 (27.1) |
| Type of CPM, n (%) | |
| Subcutaneous | 122 (45.4) |
| With reconstruction | 121 (45.0) |
| Without reconstruction | 1 (0.4) |
| Simple | 147 (54.7) |
| With reconstruction | 89 (33.1) |
| Without reconstruction | 58 (21.6) |
| Reconstruction type, n (%) | |
| Implants | 205 (97.6) |
| TRAM | 5 (2.4) |
| Reconstruction timing, n (%) | |
| At time of CPM | 201 (95.7) |
| Delayed | 9 (4.3) |
| Number of reoperations after reconstruction, n (%) | |
| 0 | 115 (54.8) |
| 1 | 70 (33.3) |
| ≥2 | 25 (11.9) |
Marital status at time of 2nd follow-up survey
Categories are not mutually exclusive since patients could state more than one reason for electing CPM
After controlling for reconstruction, there was no difference in satisfaction based on mastectomy type. Women with reconstruction had significantly lower satisfaction than women without reconstruction (P = 0.03). Among those with reconstruction, 45% underwent one or more reoperations, and satisfaction was lower in women with reoperation than those without (P = 0.04).
Consistency of Satisfaction, Choose CPM Again, and Adverse Effects
Satisfaction with CPM
A mean of 20 years after CPM, 90% of women were satisfied or very satisfied with the decision to undergo CPM. This was a 4% increase from the first survey, where 86% expressed satisfaction with CPM (Fig. 1a) (P = 0.60). Considering the satisfaction scale as three categories of satisfied, neutral, or dissatisfied, only 16% of the women changed their level of satisfaction between surveys. The level improved in 9.4% (including one patient with a shift from dissatisfied to neutral) and got worse in 6.6% (including seven patients with a shift from satisfied to neutral) (Table 2).
FIG. 1.
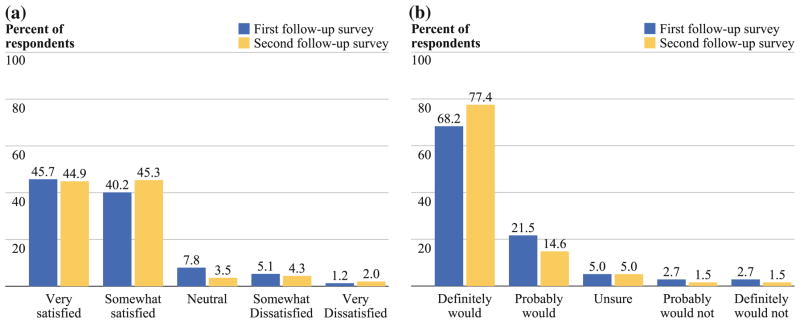
a Satisfaction with CPM. b Choose to have CPM again
TABLE 2.
Proportion of women changing satisfaction and choice of have CPM again
| 1st Follow-up survey | 2nd Follow-up survey, n (%)
|
||
|---|---|---|---|
| Same | Better | Worse | |
| How satisfied were you with CPM? (N = 256) | |||
| Satisfied | 208 (81.3) | – | 12 (4.7) |
| Neither | 1 (0.4) | 14 (5.5) | 5 (2.0) |
| Dissatisfied | 6 (2.3) | 10 (3.9) | – |
| Overall | 215 (84.0) | 24 (9.4) | 17 (6.6) |
| Would you choose to have CPM again? (N = 261) | |||
| Would | 222 (85.1) | – | 12 (4.6) |
| Unsure | 3 (1.1) | 8 (3.1) | 2 (0.8) |
| Would not | 4 (1.5) | 10 (3.8) | – |
| Overall | 229 (87.7) | 18 (6.9) | 14 (5.4) |
Answers to the open-ended question about reasons for satisfaction/dissatisfaction with CPM were similar to the first survey. Women reporting that they were satisfied/very satisfied most frequently noted that they were comfortable with their body image and sequelae, CPM provided peace of mind, and the risk reduction/enhanced detection provided. Women who were dissatisfied/very dissatisfied most frequently noted adverse body image and sequelae and adverse symptoms or complications. Women whose satisfaction changed from satisfaction to dissatisfaction reported adverse body image and sequelae or adverse symptoms/complications as a reason for their reported level of satisfaction on the second survey.
Choose CPM Again
On second survey, 92% of women reported that, knowing what they do now, they definitely or probably would choose CPM again, which was a 2% increase from the first survey (Fig. 1b). The percentage saying they definitely or probably would not choose CPM again was 3% on the second follow-up survey compared with 5% on the first. The responses on the second survey were significantly more favorable than on the first (P = 0.005), largely due to 13.8% who switched from probably to definitely would choose CPM again. Considering the scale as three categories of would do again, unsure, or would not do again, 12% of the women changed their response category between the first and second surveys. More women changed to a more favorable than to a less favorable category (7% versus 5%) (Table 2).
Answers to open-ended question about reasons for would choose CPM again were similar to the first survey. Women who reported that they probably/definitely would choose CPM again most frequently noted peace of mind and risk reduction/enhanced detection. Women who reported that they probably/definitely would not have CPM again most frequently noted either that new information is available today or that they would make a more careful/studied approach.
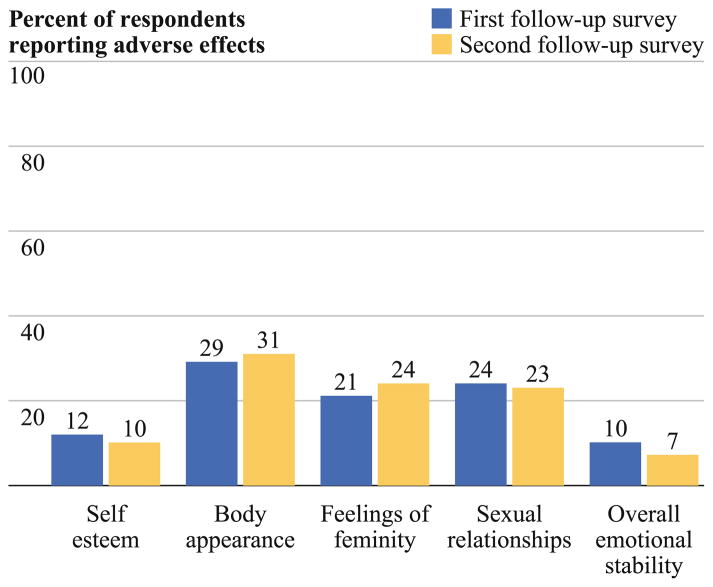
Psychological and Social Impact of CPM
The percentage of respondents reporting adverse effects of CPM for one or more psychological or social aspect was similar between the two surveys (45% and 44%). Which aspects were most adversely affected was also consistent (Fig. 2). Most adversely affected were body appearance (29% and 31%, respectively), feelings of femininity (21% and 24%, respectively), and sexual relationships (24% and 23%, respectively). Adverse effects were diminished (from 12% to 10%) for self-esteem and emotional stability (from 10% to 7%). The percentage reporting adverse effects did not differ significantly between surveys for any aspect Examining the CPM satisfaction ratings on the second follow-up survey, the impact of CPM on satisfaction with body appearance had a correlation of 0.32, feelings of femininity 0.28, self-esteem 0.26, sexual relationships 0.29, and emotional stability 0.24.
FIG. 2.
Perceived effect of CPM on psychological and social variables
We used the Body Image Scale on the second survey to more closely examine aspects of body image that were most significantly affected by CPM. Women most frequently reported either “quite a bit” or “very much” to the following items: feeling less sexually attractive (15%), dissatisfied with body (14%), dissatisfied with scar (12%), difficult to look at self naked (12%), feeling less physically attractive (11%), self-conscious about appearance (10%), felt less feminine (8%), feeling that CPM left body less whole (8%), and dissatisfied with appearance dressed (7%). Body Image Scale composite score was moderately correlated with CPM satisfaction (r = 0.48) (Table 3).
TABLE 3.
Association between CPM satisfaction and survey scales
| Measure | Possible range | N | Mean (SD) | Correlation with CPM satisfactiona |
|---|---|---|---|---|
| Decision-conflict scale | 1–5 (Higher score → Greater conflict) | 265 | 1.4 (0.6) | 0.48 |
| LOT-R optimism scale | 1–24 (Higher score → Greater optimism) | 258 | 18.5 (4.8) | 0.21b |
| Trait anxiety | 20–80 (Higher score → Greater anxiety) | 266 | 32.1 (8.5) | 0.27 |
| Health concern score | 0–100 (Higher score → Greater concern) | 262 | 55.8 (25.4) | 0.15 |
| Health distress score | 0–100 (Higher score → Greater distress) | 264 | 14.1 (17.0) | 0.21 |
| Overall quality of life | 0 (As bad as it can be) – 10 (As good as it can be) | 264 | 8.7 (1.5) | 0.37b |
| Body image scale | 0–30 (Higher score → Greater symptoms/distress) | 258 | 5.0 (5.5) | 0.48 |
Satisfaction measured on a 1 (very satisfied) to 5 (very dissatisfied) scale; all P values ≤0.02
Original scales for LOT-R optimism and overall quality of life were reversed when estimating correlation coefficients to be consistent with all other measures in that higher values represent a poorer aspect and are thus positively correlated with poorer satisfaction scores
Satisfaction: Significance of Informed Decision, Personality Traits, Health Concern, Health Distress, and Current Quality of Life (QOL)
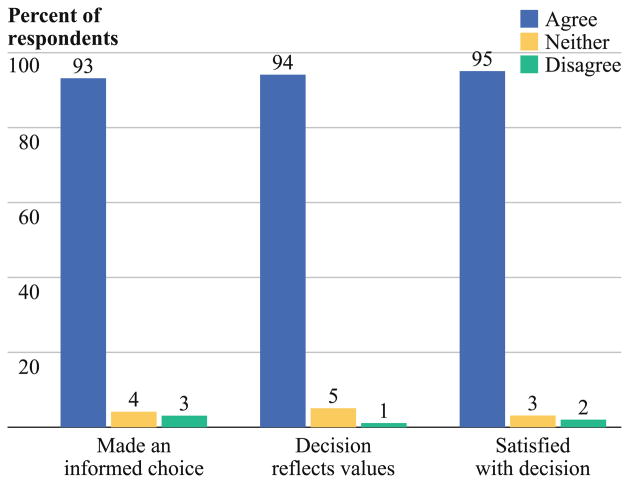
Perception of Making an Informed Decision
Ninety-three percent of the women reported that they felt they made an informed choice about their CPM, and 94% reported that the decision reflected their values. Three percent of the women reported that they did not feel their choice was informed, and 1% disagreed that their decision reflected what was important to them. Ninety-five percent of the women were satisfied with their decision, while 2% were dissatisfied (Fig. 3). CPM satisfaction was moderately correlated with each of the three questions from the Decisional Conflict Scale (r = 0.37 informed choice, r = 0.40 reflects important, and r = 0.52 satisfied with decision) as well as with the composite score (r = 0.48) (Table 3).
FIG. 3.
CPM decision-making
Personality Traits, Health Concern, Health Distress, and Quality of Life
We explored the significance of trait anxiety and optimism/pessimism in relation to satisfaction with CPM. Satisfaction with CPM was only weakly associated with optimism (r = 0.21) and trait anxiety (r = 0.27). The women as a group were optimistic and displayed a low level of trait anxiety at time of second survey (Table 3).
Satisfaction with CPM was only weakly associated with current health concern (r = 0.15) or health distress (r = 0.21). Women experienced a low level of health distress and a moderate level of health concern at the time of the second survey. Higher current QOL was moderately associated with higher satisfaction with CPM (r = 0.37). The women as a group had high QOL (Table 3).
Survey Nonresponse
The first follow-up survey had a very high response rate of 94%. Of the 487 alive at the time of the second follow-up survey, 269 (55%) returned the second survey. Comparing these 269 responders with the 218 nonresponders, they did not differ significantly in terms of age at CPM or type of CPM (subcutaneous versus total). They did differ significantly on whether reconstruction was performed (78% among responders, 66% among nonresponders, P = 0.002). Those who responded to the second survey also expressed more satisfaction (P = 0.004) on the first survey and were more likely to choose CPM again (P = 0.001) than those who did not respond to the second survey. The percentage satisfied or very satisfied on the first survey was 86% versus 79% for responders and non-responders, respectively, while the percentage saying they definitely or probably would choose CPM again was 90% versus 79%, respectively.
DISCUSSION
As time elapses, women age, and advances in science occur, the long-term consistency of women’s satisfaction with CPM and adverse effects are unknown. In this study we show that long-term satisfaction with CPM remained stable for the majority of women over a 10-year time period. An average of 20.2 years after CPM, most women remained satisfied with their decision and would choose CPM again. There was a small increase in the percentage of women satisfied (90%) and those who would choose CPM again (92%) (4% and 2% increase from the first survey, respectively).
This is the first study to evaluate the stability of satisfaction with CPM decision and is important as it provides women making these decisions with knowledge about the stability of satisfaction. Van Dijk et al. showed that most women’s preferences for prophylactic mastectomy from 1 week after blood sampling to 8 months after obtaining BRCA test results remained stable.21 One underlying factor may be that anticipated regrets are strongly associated with risk-management options.21 It is possible that the stability of women’s satisfaction with their decision is associated with anticipated regrets about not having CPM to reduce risk and their emotional comfort/discomfort with future risk. Open-ended statements from women in our study provide support for anticipated risk, with peace of mind and risk reduction cited as reasons for satisfaction. Additionally, women’s assertion of satisfaction with CPM despite coexisting adverse effects suggests the strong value these women place on peace of mind and reduced risk.
Similar numbers of women over time reported adverse effects with body appearance, sense of femininity, and sexual relationships. These variables also continued to be most adversely affected. However, when examining individual change, 13% did not report adverse effects on body appearance on the first survey but did on later follow-up, and 11% reported a decreased sense of femininity on the second but not the first survey. These were offset for the most part when reporting overall group values by women who no longer reported adverse effects on follow-up. In a study comparing breast cancer survivors with and without CPM, similar proportions of women reported body image and sexual satisfaction issues, the researchers concluding that common experiences such as age or breast cancer survivorship drive these outcomes more than CPM.12
The trend toward a difference in level of satisfaction based on type of mastectomy appears to be driven by reconstruction and the subsequent reoperations associated with reconstruction. At the time of the second follow-up, 95 patients (45%) had undergone at least one reoperation to address reconstructive complications. The potential for future surgery should be considered by individuals considering CPM with reconstruction.
Perception of making an informed decision and decisional conflict were moderately associated with CPM satisfaction. Consistent with our findings, one CPM study, two bilateral prophylactic mastectomy studies, and one study that included both CPM and bilateral prophylactic mastectomy have reported an association between regret/dissatisfaction and lack of information.13,22–24
We hypothesized a strong relationship between personality traits and satisfaction with CPM. How individuals react to a given situation is influenced by their personality. An optimistic person expects favorable outcomes, whereas individuals with high trait anxiety react to situations with increased intensity, affecting both perception and adjustment to stressful situations.17,19 We found a weak association between these personality traits and satisfaction with CPM. This may be related to the fact that women’s scores were skewed toward optimism and low trait anxiety scores.
Women in this study reported high current QOL. This is consistent with studies in which women who elected CPM showed similar levels of QOL to those who did not have CPM.12,25 It may seem counterintuitive that women experiencing adverse effects such as an unfavorable body image report high satisfaction and QOL. Although factors influ-encing adaptation are complex, most individuals adapt to their adverse situation and frame their QOL or satisfaction in terms of all aspects of their life, not just the unfavorable ones. It is the outside observer who is often overly focused on the adverse effects, letting that frame their assessment of the situation.26 Women in our study who had a lower QOL were more likely to be dissatisfied with CPM (r = 0.37). This may be a result of the coexisting associations between QOL and body image (r = 0.53), which was also moderately associated with satisfaction with CPM (r = 0.48).
Limitations to our study include the retrospective perspective in which women are asked to identify how CPM has affected psychosocial aspects of their life. We are also limited by a 55% return rate on the second follow-up survey, with some selection bias such that responders expressed more satisfaction and were more likely to choose CPM again on the first survey than nonresponders. However, the fact that we performed a paired comparison only among individuals who responded to both surveys does allow us to say confidently that satisfaction and willingness to choose CPM again did not degrade over time in this sample. The majority of women (74%) underwent bilateral mastectomies with immediate expander/implant reconstruction with very low rates of autologous tissue or delayed reconstruction, and 59 women (22%) underwent mastectomy without reconstruction. Therefore, these data are most applicable to women with immediate expander reconstruction or women without reconstruction.
A mean of 20.2 years after CPM, the majority of women are satisfied with CPM, would elect to have CPM again, and felt they made an informed decision. These factors remain remarkably stable over a 10-year period from a mean of 10.7 years to a mean of 20.2 years after CPM. The most adversely affected psychological and social variables include body appearance, sense of femininity, and sexual relationships. While perceived informed decision-making and current QOL are associated with satisfaction with CPM, the personality characteristics trait anxiety and optimism, health concern, and health distress were only weakly associated with satisfaction. These data provide women making decisions about CPM with additional information. It is important for both women and their counseling healthcare professionals to fully understand the benefits and potential adverse effects associated with pursuing CPM.
Acknowledgments
This work is supported, in part, by grants from the Department of Defense (DAMD17-94-J-4216) and the National Cancer Institute (U10 CA 37404 and R01 CA80181).
Footnotes
Presented in part at the annual meeting of the American Society of Breast Surgeons Meeting April 2011, Washington, DC.
References
- 1.Boughey JC, Hoskin TL, Degnim AC, et al. Contralateral prophylactic mastectomy is associated with a survival advantage in high-risk women with a personal history of breast cancer. Ann Surg Oncol. 2010;17:2702–9. doi: 10.1245/s10434-010-1136-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herrinton LJ, Barlow WE, Yu O, et al. Efficacy of prophylactic mastectomy in women with unilateral breast cancer: a cancer research network project. J Clin Oncol. 2005;23:4275–86. doi: 10.1200/JCO.2005.10.080. [DOI] [PubMed] [Google Scholar]
- 3.McDonnell SK, Schaid DJ, Myers JL, et al. Efficacy of contralateral prophylactic mastectomy in women with a personal and family history of breast cancer. J Clin Oncol. 2001;19:3938–43. doi: 10.1200/JCO.2001.19.19.3938. [DOI] [PubMed] [Google Scholar]
- 4.Peralta EA, Ellenhorn JD, Wagman LD, Dagis A, Andersen JS, Chu DZ. Contralateral prophylactic mastectomy improves the outcome of selected patients undergoing mastectomy for breast cancer. Am J Surg. 2000;180:439–45. doi: 10.1016/s0002-9610(00)00505-5. [DOI] [PubMed] [Google Scholar]
- 5.van Sprundel TC, Schmidt MK, Rookus MA, et al. Risk reduction of contralateral breast cancer and survival after contralateral prophylactic mastectomy in BRCA1 or BRCA2 mutation carriers. Br J Cancer. 2005;93:287–92. doi: 10.1038/sj.bjc.6602703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tuttle TM, Abbott A, Arrington A, Rueth N. The increasing use of prophylactic mastectomy in the prevention of breast cancer. Curr Oncol Rep. 2010;12:16–21. doi: 10.1007/s11912-009-0070-y. [DOI] [PubMed] [Google Scholar]
- 7.Tuttle TM, Habermann EB, Grund EH, Morris TJ, Virnig BA. Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. J Clin Oncol. 2007;25:5203–9. doi: 10.1200/JCO.2007.12.3141. [DOI] [PubMed] [Google Scholar]
- 8.Tuttle TM, Jarosek S, Habermann EB, et al. Increasing rates of contralateral prophylactic mastectomy among patients with ductal carcinoma in situ. J Clin Oncol. 2009;27:1362–7. doi: 10.1200/JCO.2008.20.1681. [DOI] [PubMed] [Google Scholar]
- 9.Altschuler A, Nekhlyudov L, Rolnick SJ, et al. Positive, negative, and disparate–women’s differing long-term psychosocial experiences of bilateral or contralateral prophylactic mastectomy. Breast J. 2008;14:25–32. doi: 10.1111/j.1524-4741.2007.00521.x. [DOI] [PubMed] [Google Scholar]
- 10.Frost MH, Slezak JM, Tran NV, et al. Satisfaction after contralateral prophylactic mastectomy: the significance of mastectomy type, reconstructive complications, and body appearance. J Clin Oncol. 2005;23:7849–56. doi: 10.1200/JCO.2005.09.233. [DOI] [PubMed] [Google Scholar]
- 11.Isern AE, Tengrup I, Loman N, Olsson H, Ringberg A. Aesthetic outcome, patient satisfaction, and health-related quality of life in women at high risk undergoing prophylactic mastectomy and immediate breast reconstruction. J Plast Reconstr Aesthet Surg. 2008;61:1177–87. doi: 10.1016/j.bjps.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 12.Geiger AM, West CN, Nekhlyudov L, et al. Contentment with quality of life among breast cancer survivors with and without contralateral prophylactic mastectomy. J Clin Oncol. 2006;24:1350–6. doi: 10.1200/JCO.2005.01.9901. [DOI] [PubMed] [Google Scholar]
- 13.Montgomery LL, Tran KN, Heelan MC, et al. Issues of regret in women with contralateral prophylactic mastectomies. Ann Surg Oncol. 1999;6:546–52. doi: 10.1007/s10434-999-0542-1. [DOI] [PubMed] [Google Scholar]
- 14.Bresser PJ, Van Gool AR, Seynaeve C, et al. Who is prone to high levels of distress after prophylactic mastectomy and/or salpingo-ovariectomy? Ann Oncol. 2007;18:1641–5. doi: 10.1093/annonc/mdm274. [DOI] [PubMed] [Google Scholar]
- 15.Hopwood P, Fletcher I, Lee A, Al Ghazal S. A body image scale for use with cancer patients. Eur J Cancer. 2001;37:189–97. doi: 10.1016/s0959-8049(00)00353-1. [DOI] [PubMed] [Google Scholar]
- 16.Stewart A, Ware J. Measuring functioning and well-being. Durham: Duke University Press; 1992. [Google Scholar]
- 17.Spielberger C. STAI (Form Y) Palo Alto, CA: Consulting Psychologists Press, Inc; 1983. State-Trait Anxiety Inventory. [Google Scholar]
- 18.Herzberg PY, Glaesmer H, Hoyer J. Separating optimism and pessimism: a robust psychometric analysis of the revised Life Orientation Test (LOT-R) Psychol Assess. 2006;18:433–8. doi: 10.1037/1040-3590.18.4.433. [DOI] [PubMed] [Google Scholar]
- 19.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67:1063–78. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 20.O’Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15:25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 21.van Dijk S, van Roosmalen MS, Otten W, Stalmeier PF. Decision making regarding prophylactic mastectomy: stability of preferences and the impact of anticipated feelings of regret. J Clin Oncol. 2008;26:2358–63. doi: 10.1200/JCO.2006.10.5494. [DOI] [PubMed] [Google Scholar]
- 22.Borgen PI, Hill AD, Tran KN, et al. Patient regrets after bilateral prophylactic mastectomy. Ann Surg Oncol. 1998;5:603–6. doi: 10.1007/BF02303829. [DOI] [PubMed] [Google Scholar]
- 23.Hatcher MB, Fallowfield L, A’Hern R. The psychosocial impact of bilateral prophylactic mastectomy: prospective study using questionnaires and semistructured interviews. BMJ. 2001;322:76. doi: 10.1136/bmj.322.7278.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bresser PJ, Seynaeve C, Van Gool AR, et al. Satisfaction with prophylactic mastectomy and breast reconstruction in genetically predisposed women. Plast Reconstr Surg. 2006;117:1675–82. doi: 10.1097/01.prs.0000217383.99038.f5. discussion 83–4. [DOI] [PubMed] [Google Scholar]
- 25.Tercyak KP, Peshkin BN, Brogan BM, et al. Quality of life after contralateral prophylactic mastectomy in newly diagnosed high-risk breast cancer patients who underwent BRCA1/2 gene testing. J Clin Oncol. 2007;25:285–91. doi: 10.1200/JCO.2006.07.3890. [DOI] [PubMed] [Google Scholar]
- 26.Sprangers MA, Schwartz CE. Reflections on changeability versus stability of health-related quality of life: distinguishing between its environmental and genetic components. Health Qual Life Outcomes. 2008;6:89. doi: 10.1186/1477-7525-6-89. [DOI] [PMC free article] [PubMed] [Google Scholar]