Abstract
Background
Child and family mental health services remain largely underutilized despite the relatively high rate of youth suffering from mental, emotional, and behavioral (MEB) disorders. As such, it is important to address challenges and examine factors related to child mental health service use and engagement, especially when it comes to children in need of services for anxiety.
Objective
Informed by the Behavioral Model of Health Services Use (BMHS), the present study sought to examine predictors of service use and engagement for families seeking assistance for their anxious children. Initial levels of engagement in culturally tailored services were predicted from predisposing characteristics (e.g., child age, ethnicity), enabling resources (e.g., Spanish services, transportation), and need characteristics (e.g., child clinical severity).
Method
Participants included Latino (n = 126) and Caucasian (n = 116) families who presented to a specialty clinic due to child emotional and behavior problems related to anxiety. Initial service utilization and engagement was assessed along the following levels toward services care: (1) initiated contact and completed a clinical intake, (2) completed a home screen, and (3) completed an on-site diagnostic assessment. All procedures were culturally tailored to the presenting needs of families.
Results
Predisposing characteristics, enabling resources and need characteristics emerged as significant predictors of child mental health service use, with some variations. Child age, ethnicity, referral source, and enabling resources predicted completion of a home screen. Proximity to services predicted completion of the on-site diagnostic assessment.
Conclusion
Knowledge of factors that predict engagement in child mental health services can help identify avenues to promote service utilization, especially among ethnic minority children and families. Our culturally tailored approach to serving families appears to be promising in bridging the cross-ethnic services gap and therefore has implications for practice.
Keywords: Mental health service use, anxiety, Latino, children and adolescents
Introduction
According to a recent report from the National Research Council and the Institute of Medicine, it is estimated that 17% of children and adolescents are diagnosed with a mental, emotional, or behavioral (MEB) disorder. Despite this relatively high rate, fewer than one in eight youth with MEB disorders is receiving services (e.g., treatment in mental health care systems) and only one in four has ever received care for MEB difficulties (Burns et al., 1995; Farmer, Burns, Phillips, Angold, & Costello, 2003; Kataoka, Zhang, & Wells, 2002). The relatively high rate of MEB disorders coupled with documented failure to receive related services is of public health concern for several reasons. First, MEB problems cause distress to children and families. Second, these problems interfere with youth’s abilities to achieve developmental milestones. Third, MEB difficulties place youth and families at increased risk for future psychopathology and poorer quality of life. Fourth, MEB disorders inflict relatively high financial costs to society (NCR/IOM, 2009). As such, it is important to identify factors that may help improve mental health service use as a way to help ameliorate suffering among youth with MEB problems (Andersen, 2008; Owens et al., 2002).
The Behavioral Model of Health Services Use (BMHS; Andersen, 1995; 2008) has served to advance understanding of health services use, define/measure equitable access to care, and assist policy development to promote evidence-based medicine and service utilization. Drawing on the BMHS, we sought to improve knowledge about service use/engagement among youth referred for MEB problems in general and anxiety difficulties in particular. The focus on youth referred for anxiety is important because anxiety disorders were found to be among the most common (~8%) diagnoses in recent meta-analyses of over 50 community surveys from around the world (NCR/IOM, 2009). Within the United States specifically, anxiety disorders have a relatively high rate of lifetime prevalence across childhood (4 to 18 years old; Merikangas et al., 2010). In addition, data show that anxiety is typically chronic and leads to significant impairment, including poor academic performance, depression, and early initiation of the use of alcohol, tobacco, and other illicit drugs (Conger & Rueter, 1996). Lastly, we also know that clinically anxious youth usually fail to receive mental health services for their MEB difficulties (Barrett & Turner, 2004; Chavira et al., 2004).
In this study, we specifically sought to improve knowledge about specialty mental health service use/engagement among anxious Latino youth, for whom anxiety may be especially problematic. Focusing on Latino youth is important because they seem to have higher rates of certain anxiety disorders (e.g., separation anxiety) as well as more worries related to health, danger/death and the unknown (Ginsburg & Silverman, 1996; McLaughlin, Hilt, & Nolen-Hoeksema, 2007; Varela, Sanchez-Sosa, Biggs, & Luis, 2008). There is also evidence that Latinos experience more distress and interference in response to anxiety symptoms. For example, Latino youth tend to experience more distress from anxiety-related somatic symptoms (Pina & Silverman, 2004) as well as more sleep difficulties related to anxiety (Alfano, Pina, Zerr, & Villalta, 2010).
In particular, the sample for the present study included a sizable proportion of Mexican-origin youth. Our reason for focusing on this segment of the Latino population is threefold. First, Mexicans comprise the largest population of Latinos living in the United States, including over 10 million Mexican-origin children and adolescents (Pew Hispanic Center, 2007). Second, unlike Cubans who are more likely to use mental health services (perhaps because of their eligibility for publicly financed health care, higher socioeconomic status, and immigration policies; Portes, Kyle, & Eaton, 1992), Mexican families typically face serious health care access difficulties (Vega, Kolody, & Aguilar-Gaxiola, 2001). Third, findings from the adult anxiety literature suggest that although anxious Latinos are more likely to utilize services than their non-anxious counterparts, utilization rates remain significantly lower compared to rates for Caucasians (Deacon, Lickel, & Abramowitz, 2008; Diefenbach, Robison, Tolin, & Blank, 2004).
To evaluate predictors of engagement in mental health specialty services, variables measured for the present study were organized using the Behavioral Model of Health Services Use. Figure 1 shows key aspects of the model, tailored for this study. As articulated by Andersen (1995), health behavior is thought to be a function of predispositions to use services, factors that enable use, and need for care. Among predisposing characteristics are demographic factors such as age and sex of the child, social structure factors such as minority status, and health beliefs such as past efforts to seek services. Enabling resources include personal/family and community factors that must be present for use/engagement to take place, such as having transportation to service sites. When it comes to need characteristics both perceived and evaluated are considered. Perceived needs include whether parents believe the problem is severe and impairing enough to engage in self-directed help-seeking behaviors or whether they believe the problem is severe and impairing enough to follow through when their children are referred for specialty services. Lastly, evaluated need refers to professional judgments of health status such as clinical severity and number/type of problems.
Figure 1.
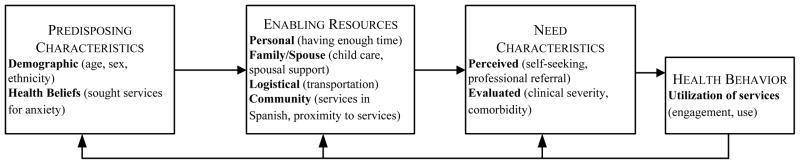
Application a Behavioral Model of Health Services Use to our Specialty Mental Health Services.
As far as health behavior, the present study is particularly concerned with various levels of service use/engagement as a primary outcome. Unlike past research, which has largely focused on assessing health behavior as a help-seeking event that did or did not occur, we believe it is important to capture a distinction between initial contact on the one hand and entry levels/continuity on the other. Capturing this distinction is important because predictors of health behaviors such as “contacting potential sources of assistance” likely differ from predictors of engaging in treatment. This is probable, for example, because parents typically contact several potential sources of assistance continuously prior to securing services. In addition, readiness and engagement typically varies by the client’s commitment and readiness for change (Prochaska & DiClemente, 1983; Prochaska, DiClemente, & Norcross, 1992; Prochaska & Velicer, 1997).
Building on the BMHS and past research (mostly studies reporting barriers to service utilization), we hypothesized that sex and age of the child could emerge as significant predictors of anxiety specialty service use/engagement. In the research literature, Chavira, Garland, Yeh, McCabe, and Hough (2009) did not find age or sex of the child to be related to service use and neither did Flores et al. (1998). However, Weathers, Minkovitz, O’Campo, and Dierner-West (2003) found that girls of migratory agricultural workers were more likely to receive medical services than boys. Yeh, McCabe, Hough, Dupuis, and Hazen (2003) found that as age increased so did the number of barriers to engaging in mental health service use. Among adults, Documèt and Sharma (2004) and Vega, Kolody, and Aguilar-Gaxiola (2001) found that Mexican women were more likely than men to use medical and mental health care. Another important factor examined in the present study was minority status (Latino/Mexican), which we hypothesized would be a significant predictor perhaps due to other interrelated measured variables. Briefly, Flores and Vega (1998) found in a review of the literature that parental Spanish language preference was linked to fewer medical visits; and in an empirical study, a survey of Latino parents (who attended an ethnically-focused pediatric clinic) revealed that Spanish language, poverty, and transportation difficulties predicted lower levels of service use (Flores, Abreu, Olivar, & Kastner, 1998) (similar findings were reported by Alegria et al., 2002; Andersen, Hongjian, Wyn, Brown, & Teleki, 2002; Dobalian & Rivers, 2008; Documèt & Sharma, 2004; Fiscella, Franks, Doescher, & Saver, 2002; Horwitz, Gary, Briggs-Gowan, & Carter, 2003; Scheppers, van Dongen, Dekker, Geertzen, & Dekker, 2006; and others). Based on these findings, Spanish language, poverty/income, and transportation could predict service use in the present study.
Additional measured variables were parents’ past efforts to seek services for the child’s problem (a proxy for health beliefs), family resources, proximity to services, and perceived/evaluated need (see Figure 1). Health beliefs are difficult to conceptualize because these may vary by type of problem, knowledge about its treatment, stigma, etc. (Andersen, 1995; Tanner, Cockerham, & Spaeth, 1983). In the present study, past efforts to seek services was used as a proxy for health beliefs because this variable may reflect values, attitudes, and knowledge about child health and services, both of which are known to impact utilization (Owens et al., 2002). With regard to the other variables, travel time (e.g., less than 20 minutes; Dobalian & Rivers, 2008) and family resources (support, dual parent status, cohesion; Horwitz et al., 2003; Dillman Carpentier et al., 2007) have been linked to increased service use/engagement. Similarly, greater problem severity and need (perceived, evaluated) has been linked to greater service use (Owens et al., 2002; Shi & Stevens, 2005, Vega, Kolody, & Aguilar-Gaxiola, 2001). For example, Weathers and colleagues (2003) found that children in poor health were almost 4 times more likely to receive medical care. Building on this knowledge, these variables were hypothesized to predict service use/engagement. However, given the scarcity of research focusing on these factors jointly, youth referred to anxiety specialty services, and Mexican-origin youth in particular, our hypotheses were exploratory in nature.
This study builds on past published research in several ways. First, the present study relied on a well-established conceptual framework to guide the evaluation of a broad range of factors that may be related to service use in child anxiety mental health specialty services. To our knowledge, Chavira, Garland, Yeh, McCabe, and Hough (2009) is the only study to focus on child anxiety by drawing data from public sectors of care (juvenile justice, child welfare) and relying on a narrower range of measured variables. Second, we attempted to capture factors that may be related to entry levels and/or continuity of service use which varies from past research focused on help seeking events that did or did not occur. Third, findings from the present study, especially those relevant to Mexican-origin youth, may help shape clinical practice and policy development for a growing and understudied segment of the U.S. population.
Method
Participants
Data corresponding to 242 child-mother dyads referred to child mental health specialty services focused on anxiety were examined in the current study (citation excluded for review). Participants were referred by school personnel (53%), self-referred (28%) (e.g., learned about the services via newspaper 10%, internet 6%, radio broadcasts 3%), pediatricians (10%) or mental health service providers (7%). Youths’ ages ranged from 4 to 16 years old (M = 10.06 years; SD = 2.89), about 45% of the child participants were girls, and all parent participants were mothers. We specifically focused on participation from mothers since they were the initial and primary contact for most families, and few fathers completed the home screen (n = 8). Fifty-two percent of participants were Latino (mostly Mexican-origin) and 48% Caucasian. Household income ranged from $21,168 to $117,487 (Median = $41,137, M = $45,445, SD = $14,797).
Measures
Measures are presented according to the Behavioral Model of Health Services Use (Andersen, 1995; 2008), which includes the following categories: predisposing characteristics, enabling resources, need characteristics, and health behavior.
Predisposing characteristics
Child age and sex, race/ethnicity, and history of help seeking behavior were obtained from the standardized clinical intake measure. Age and sex were treated as demographic variables and race/ethnicity was used as a measure of social structure. Given the demographic, social, and economic composition of the geographical region targeted for data collection, Latino ethnicity was coded as the minority group and Caucasian as majority. The clinical intake also included items about past help seeking behavior, and responses were dichotomously coded to reflect an event that did or did not occur.
Enabling resources
Personal, family, and community resource data were drawn from the standardized clinical intake measure and from a basic web mapping service application tool that uses public records. More specifically, the intake measure includes questions about family/work schedules, availability of childcare, spousal support, transportation to the service delivery site, and child/sibling care. Items were dichotomously coded to reflect resources that did or did not exist. Language service needs were coded as English or Spanish. Proximity to services was coded as travel time (< 20 or ≥ 20 minutes) based on convergence from web application tools. Socio-economic status was coded on the basis of family and neighborhood characteristics (i.e., median household income) by using another web application tool that relies on zip code-level census data.
Need characteristics
Perceived and evaluated need data were obtained from the intake measure and from the parent completed CBCL. Perceived need was derived from parental responses on the clinical intake indicating parents were either self-referred or referred by a professional (e.g., school psychologist, pediatrician). Evaluated need data was derived from the CBCL and focused on the number of DSM-oriented scales in the clinical range. Briefly, the CBCL contains a total of 118 items used to assess internalizing and externalizing behavior problems and the remaining 20 items assess child social competencies. Each of the 118 internalizing and externalizing behavior problem items are rated on a 3-point scale of: 0 (not true), 1 (somewhat or sometimes true), or 2 (very true or often true). The CBCL yields six DSM-oriented scales: Anxiety, Affective, Attention Deficit Hyperactivity Disorder (ADHD), Somatic, Oppositional Defiant Disorder (ODD), and Conduct Disorder (CD). The number of DSM-oriented scales in the clinical range (T scores greater than 69; Achenbach, Dumenci, & Rescorla, 2003) was used in the present study. The reliability and validity of the CBCL’s DSM-oriented scales is well-established (see Ebesutani et al., 2010; Nakamura, Ebesutani, Bernstein, & Chorpita, 2009).
Health behavior
Service utilization/engagement was the primary health behavior of interest in the present study and was coded in terms of continuity of engagement. Participants were grouped along the following levels: level 1: initiated contact and completed a clinical intake over the telephone, level 2: completed a home screen (i.e., CBCL), level 3: completed an on-site diagnostic interview and questionnaire battery with the child. All families that completed level 1 were invited for level 2 to complete a home screen. However, level 3 engagement was restricted to families that (a) completed the previous level 2 home screen (n = 133) and (b) were not referred out due to exclusionary criteria (n = 15). As such, the analyses predicting level 3 engagement only include the participants who were invited for the assessment, thus comprising a subset of participants from the initial sample.
Procedures
Data corresponding to each category were derived from a standardized clinical intake measure, public records, and a parent completed Child Behavior Checklist (CBCL; Achenbach, 1991). Training for implementing the standardized clinical intake measure was achieved via didactic materials, a 2-hour workshop, and five role-play feedback sessions. The clinical intake measure was administered at the initial telephone contact. After the clinical intake measure was administered, participant parents were mailed the CBCL along with a self-addressed stamped envelope. They were asked to complete and mail the CBCL to the clinic. After returning the CBCL to the clinic, participants who met inclusion criteria were invited for an on-site diagnostic assessment which included parent and child questionnaires and interviews.
In terms of our approach to being culturally responsive, recruitment and engagement strategies were tailored to increase participation among Latino families. Some of the issues considered in the cultural tailoring were language, stigma, and economic conditions (citation excluded for review). Language (i.e., needing services in Spanish) has been identified as the most important barrier by Latino parents (Flores et al., 1998) and is often related to mental health service utilization (Alegria et al., 2002; Cabassa, 2007; Yeh et al., 2003). As such, clinic staff were Spanish-speaking and the program was advertised in local Spanish newspapers and radio stations. Program and assessment materials were translated and evaluated by a team of native Spanish speakers trained within the field psychology. Most of the Latino families in our sample required/preferred delivery in Spanish, thus the translation of services proved to be an important tool for engaging many families. Additionally, the program was given a Spanish name based on a cultural idiom, “Acercamiento”, to reflect its cultural responsiveness and to promote recognizability among Latino families. Since stigma associated with mental health problems and services is often mentioned as a barrier for Latino families (Alvidriz, 1999; Magana, Garcia, Hernandez, & Cortez, 2007), clinical terminology was avoided and replaced with less technical alternatives (e.g., “anxiety disorders” were referred to as “anxiety difficulties” or difficult situations). Lastly, since barriers related to socioeconomic status are common for both European Americans and Latinos (Flores et al., 1998, Garcia & Weisz, 2002), services were offered free-of-charge and delivered in a location with free childcare and nearby public transportation (i.e., bus, trolley stops). Applying some of these cultural considerations seems to have been successful, given that the initial participation rate for Latino families (52%) was comparable to that of Caucasian families (48%) as well as population estimates for the surrounding area (48%, U.S. Census Bureau, 2010).
Results
For the primary analyses of interest, continuous variables were centered (Aiken & West, 1991) and logistic regressions were used to evaluate factors hypothesized to predict engagement according to the theoretical model (see Figure 1). Two sets of logistic regressions were implemented. One set focused on level 2 engagement (completion of the home screen) (n = 242; 133 completers, 109 non-completers). The second set focused on level 3 engagement (completion of the on-site diagnostic assessment about the child) (n = 118; 79 completers, 39 non-completers). For the regressions corresponding to the two sets of analyses, we report χ2 and Nagelkerke R2 statistics of model fit as well as unstandardized regression coefficients (B), Wald statistics, and odds ratios (OR) for significant (or marginally significant) individual predictors.
Preliminary analyses showed that 58% participants (n = 141) endorsed past help seeking behavior, including through psychologists or psychiatrists (49%), school services (16%), combination of services (16%), primary care/pediatrician (13%), or social services (7%). In terms of enabling resources, parents reported data across four different domains: Personal (e.g., having enough time, flexible work schedule) (4 items; M = 3.79, SD = .52), Family (e.g., child care) (3 items; M = 2.72, SD = .57), Spouse (e.g., spousal support, spouse has flexible work schedule) (3 items; M = 2.84, SD = .46), and Logistical (2 items; e.g., transportation) (M = 1.89, SD = .39). When it came to language needs, about 35% of the participants required services in Spanish whereas 65% were able to utilize services in English. In terms of distance from the service delivery site, participants lived between 3 and 57 minutes away in standard travel time (M = 22.24, SD = 10.27).
As far as clinical characteristics, results showed that several youth were in the clinical or borderline range of the CBCL DSM-oriented scales. More specifically, about 47% were in the clinical range on the affective scale (18% were in the borderline range) and about 72% were in the clinical range on the anxiety scale (11% were in the borderline range). Fewer youth were on the clinical range for the somatic, ADHD, ODD, and CD scales (31%, 16%, 20%, and 11%). A similar pattern was found on the borderline range for the somatic, ADHD, ODD, and CD scales (21%, 18%, 12%, and 14%). Means and standard deviations for the raw scales were as follows: affective: M = 7.49, SD = 4.96; anxiety: M = 7.18, SD = 2.97; somatic: M = 3.62, SD = 3.05; ADHD: M = 6.04, SD = 3.70; ODD: M = 4.18, SD = 2.62; CD: M = 3.38, SD = 3.71.
Primary findings corresponding to the first set of regressions evaluating predictors of level 2 engagement (i.e., completing the home screen) revealed that the model testing predisposing characteristics fit marginally better than the null model [χ2 (4, N = 230) = 8.58, p = .073, Nagelkerke R2 = .05; 56% accurate classification]. The model testing enabling resources did not fit significantly better than the null model [χ2 (4, N = 200) = 5.36, p = .25, Nagelkerke R2 = .04; 63% accurate classification]. The model testing need characteristics fit significantly better than the null model [χ2 (1, N = 235) = 10.51, p = .001, Nagelkerke R2 = .06; 62% accurate classification]. In terms of individual predictors of completing the home screen, results showed that parents/families who were professionally-referred (B = .95, Wald = 10.25, p = .001, OR = 2.57; 95% CI for OR = 1.44 to 4.59), Caucasian (B = .51, Wald = 3.43, p =.06, OR = 1.66; 95% CI for OR = .97 to 2.83), and with greater enabling resources (e.g., flexible family/work schedules, spousal approval of seeking help for the child, child/sibling care) (B = .22, Wald = 3.37, p =.067, OR = 1.29; 95% CI for OR = .99 to 1.58) were more likely to engage/complete the home screen. In addition, for every one year increase in child age, there was a 1.103 lower likelihood of having the parent complete the home screen (B = −.91, Wald = 4.05, p = .04, OR = .91; 95% CI for OR = .85 to 1.00), suggesting that service engagement decreased as youth aged.
In terms of the second set of regressions evaluating predictors of level 3 engagement (i.e., having completed the diagnostic assessment), results showed that the model testing predisposing characteristics did not fit significantly better than the null model [χ2 (4, N = 116) = 1.15, p = .89, Nagelkerke R2 = .01; 68% accurate classification]. The model testing enabling resources was marginal [χ2 (4, N = 105) = 7.71, p = .10, Nagelkerke R2 = .10; 73% accurate classification]. The model testing need characteristics did not fit significantly better than the null model [χ2 (2, N = 90) = 2.75, p = .25, Nagelkerke R2 = .05; 86% accurate classification]. In terms of individual predictors, proximity to the service delivery site was marginally associated with engaging/completing the on-site diagnostic assessment about the child [B = −.86, Wald = 3.33, p = .07, OR = .42; 95% CI for OR = .17 to 1.07]. Those residing more than 20 minutes away from services were two times more likely to complete the diagnostic assessment than those who lived closer. No additional factors emerged as significant predictors.
In addition to including ethnicity as a predictor variable, we also examined our models separately across ethnicities. Follow-up analyses revealed significant ethnic differences for both level 2 and level 3 engagement. For Latino (but not Caucasian) families, level 2 engagement was predicted by both enabling resources [χ2 (4, N = 117) = 8.92, p = .06, Nagelkerke R2 = .11, 61% accurate classification] and need characteristics [χ2 (1, N = 117) = 12.93, p < .001, Nagelkerke R2 = .13, 64% accurate classification] models. In terms of individual predictors, Latino families who were professionally-referred (B = 1.55, Wald = 11.36, p = .001, OR = 4.69; 95% CI for OR = 1.91 to 11.54) and with greater enabling resources (B = .37, Wald = 4.88, p =.027, OR = 1.45; 95% CI for OR = 1.04 to 2.01) were more likely to complete the home screen. For Caucasian families, service engagement was predicted by child’s age (B = −.13, Wald = 3.16, p =.075, OR = .88; 95% CI for OR = .76 to 1.01) with decreased engagement for older youth.
Cross-ethnic differences also emerged when comparing models of level 3 engagement. For Latinos, completion of the on-site diagnostic assessment was predicted by enabling resources [χ2 (4, N = 53) = 8.53, p = .07, Nagelkerke R2 = .23; 78% accurate classification] whereas needs characteristics predicted engagement for Caucasians [χ2 (2, N = 63) = 5.33, p = .07, Nagelkerke R2 = .18; 86% accurate classification]. In terms of individual predictors, level 3 engagement among Caucasians was predicted by proximity to the service delivery site [B = −1.08, Wald = 2.87, p = .09, OR = .34; 95% CI for OR = .10 to 1.19] as well as the number of DSM-oriented problems [B = −.73, Wald = 4.07, p = .04, OR = .48; 95% CI for OR = .24 to .98]. That is, engagement was higher for Caucasian families who lived more than 20 minutes away and for children with fewer problems in the clinical range. No other significant findings emerged.
Discussion
The present study built on past research by evaluating conceptually grounded predictors of mental health service utilization in a sample of clinic referred Latino and Caucasian youth. Guided by the Behavioral Model of Health Services Use (Andersen, 1995), factors relevant to predisposing characteristics (e.g., child age, ethnicity), enabling resources (e.g., Spanish services, transportation), and need characteristics (e.g., child clinical severity) were tested. In this study, the health services use model was somewhat valuable. Results showed that predisposing characteristics, enabling resources and need characteristics emerged as significant predictors of child mental health service use, with some variations. More specifically, when it came to identifying factors that predict caregiver completion of a behavior problem checklist screen (at home) about the child, findings showed that Caucasian parents were more likely to complete the screen compared to Latino parents. Consistent with the adult research area, parents whose youth were referred for services by primary care providers, pediatricians, school psychologists, and counselors were more likely to complete the home screen than those self-referred (e.g., Aiken, West, Woodward, Reno, & Reynolds, 1994). In addition, families with flexible work schedules, spousal approval/support of seeking help for the child, and/or child/sibling care were more likely to complete the home screen. Lastly, families residing more than 20 minutes away from the service delivery site were more likely to engage in the on-site diagnostic assessment about the child than those residing within closer proximity.
Follow-up analyses also revealed some interesting findings when comparing predictors of engagement for Latino and Caucasian families. For Latino families, enabling resources (e.g., work availability, spousal approval, child care) were consistent factors in predicting participation across both levels of engagement. Referrals from professionals also increased engagement among Latino families, particularly for completion of the home screen. On the other hand, child-level factors seemed to have a greater impact for engagement among Caucasian families. For example, Caucasian families engaged less as child age and number of child clinical problems increased. Engagement among Caucasians was also related to distance from the service site, with increased participation for families residing more than 20 minutes away.
Identifying factors that predict engagement in child services is important for several reasons. Regarding home completion of a behavior problem checklist screen about the child, selective and indicated prevention efforts often rely on parent reports of child behavior problems as a means to include youth in mental health inoculation efforts. Also, with HMO payment restrictions and limited time/resources, mental health clinics are increasingly screening patients to expedite the referral and service delivery process. Moreover, the focus on the identifying factors that predict engagement/completion of the on-site diagnostic assessment also is important because this service is typically a gateway to receiving adequate care. And, as it is well known, the rate of youth suffering from MEB problems is relatively high while mental health services remain largely underutilized (Burns et al., 1995; Farmer et al., 2003; Kataoka, Zhang, & Wells, 2002), especially among Latino youth and families (Vega, Kolody, & Aguilar-Gaxiola, 2001).
A few findings from the present study were unexpected. Specifically, Latino families were less likely to complete the behavior problem checklist screen about the child. This finding was unanticipated because upon initial telephone contact parents had the opportunity to share their concerns about the child with a trained professional, including in Spanish, and the checklist screen about the child was explained and made available in English or Spanish. One possibility is that some Latino parents found it difficult to complete the screen at home because of low reading proficiency or its length (113 questions). Another explanation for this finding could be lack of time to complete the screen. In Cardemil et al. (2007), “Not having enough time” was one of the most common reasons Latinos did not seek mental health services and this may be especially true for those who have larger families and therefore more responsibilities (U.S. Census Bureau, 2010). Other possibilities include concerns related to stigma and possibly “save face” (avoiding bringing shame on to the family; Alvidrez, 1999; Magana, Garcia, Hernandez, & Cortez, 2007; Leaf, Bruce, Tischler, & Holzer, 1987). There also might be some distrust of service providers and deportation concerns (Halfon, Wood, Valdez, Pereya, & Duan, 1997; Lewis, West, Bautista, Greenberg, & Done-Perez, 2005). Also unexpected was the finding that families residing more than 20 minutes away from the service site were twice as likely to attend the diagnostic assessment than those who lived closer. We believe this finding is related to a general lack of mental health services and resources in areas away from the urban area where the site is located. That is, areas about 20 minutes away include agricultural and rural communities where mental health resources are scant.
Different from past research (Flores et al. 1998; Alegria et al., 2002; Cabassa, 2007; Yeh et al., 2003), family income and language (English, Spanish) did not emerge as significant predictors of service underutilization in the present study; perhaps because services were offered at no cost and were made available in Spanish. Continuing with null results, past published research findings vary with regard to the relation between service use and sex, past help seeking behaviors, and service need (clinical severity) (e.g., Chavira, Garland, Yeh, McCabe, & Hough, 2009; Flores et al., 1998). Because the present study reports on a special population and these factors were not significant predictors, null findings should be considered with caution. Child age, on the other hand, was significantly and negatively related to completion of the home screen. This is consistent with past work suggesting that with age it may become more difficult for parents to facilitate youth engagement in services (Yeh, McCabe, Hough, Dupuis, & Hazen, 2003).
Conclusion
Based on findings from the present study, some recommendations are outlined. First, it seems critical to engage pediatricians, school counselors, and other community mental health agencies in the process of referring youth and families for specialty services. In Alegria et al. (2012), for example, minority youth identified and/or encouraged were more likely to seek services than their non-identified/encouraged counterparts. Second, it might be important to evaluate family enabling resources/barriers to engagement upon initial contact. Armed with this knowledge, providers could then help families devise plans to facilitate service use (e.g., arrange and locate child care, gain spousal support for engaging in services, or problem solve to overcome barriers to engagement). Third, based on the findings, it is possible that providers may better engage some Latino families by conducting home/clinic-based assessments rather than mailed screens about the child. In Roosa et al. (2008), for instance, engagement rates for Mexican origin families were as high as 70% and their assessment methods focused on telephone interviews scheduled evenings and weekends based on parent’s availability. Taken together, these are some ways the methods we utilized for serving families who presented to our clinic could be enhanced.
Findings and recommendations should be viewed, however, in light of several limitations. First, findings should be viewed as preliminary in nature because this is the first study to examine predictors of engagement in anxiety specialty mental health services with a sample of Latino (mostly Mexican-origin) and Caucasian families. Second, study participants contacted the service delivery site and thus there could be unknown self-selection biases influencing motivation to engage in services, the focal variable of interest. Third, the study did not examine factors that predict engagement in intervention or treatment services. However, there is research in the treatment completion/non-completion area (e.g., Kendall & Sugarman, 1997; Pina, Silverman, Weems, Kurtines, & Goldman, 2003). Fourth, findings might not necessarily generalize to youths and families seeking services for other child behavior problems, such as substance use or disruptive problems. Lastly, Andersen’s model was found to be only somewhat helpful in the present study since some predisposing characteristics, enabling resources, and need characteristics did not significantly predict levels of engagement. Considering additional facets such as structural/contextual characteristics of the service site and consumer satisfaction (Andersen, 2008) could help clarify patterns of service utilization in the child anxiety area. This is important because as knowledge about the most efficient and effective ways to engage youth and families in services increases, the possibility of improving youth mental health outcomes and family well-being is likely to become a reality.
Acknowledgments
This study was supported in part by award numbers K01MH086687 and L60MD001839 from the National Institute of Mental Health and the National Center on Minority Health and Health Disparities, as well as funding from the Institute for Mental Health Research awarded to A. Pina. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM, Dumenci L, Rescorla LA. DSM-oriented and empirically based approaches to constructing scales from the same item pools. Journal of Clinical Child and Adolescent Psychology. 2003;32:328–340. doi: 10.1207/S15374424JCCP3203_02. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG, Woodward CK, Reno RR, Reynolds KD. Increasing screening mammography in asymptomatic women: Evaluation of a second-generation, theory-based program. Health Psychology. 1994;13:526–538. doi: 10.1037/0278-6133.13.6.526. [DOI] [PubMed] [Google Scholar]
- Alegría M, Canino G, Ríos R, Vera M, Calderón J, Rusch D, Ortega AN. Mental health care for Latinos: Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatric Services. 2002;53:1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- Alegría M, Lin JY, Green JG, Sampson NA, Gruber MJ, Kessler RC. Role of referrals in mental health service disparities for racial and ethnic minority youth. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:703–711. doi: 10.1016/j.jaac.2012.05.005. doi: http://dx.doi.org/10.1016/j.jaac.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfano CA, Pina AA, Zerr AA, Villalta IK. Pre-sleep arousal and sleep problems of anxiety-disordered youth. Child Psychiatry and Human Development. 2010;41:156–167. doi: 10.1007/s10578-009-0158-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvidrez J. Ethnic variations in mental health attitudes and service use among low-income African American, Latina, and European American young women. Community Mental Health Journal. 1999;35:515–530. doi: 10.1023/A:1018759201290. [DOI] [PubMed] [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1-1–10. doi: 10.2307/2137284. [DOI] [PubMed] [Google Scholar]
- Andersen RM. National health surveys and the behavioral model of health services use. Medical Care. 2008;46:647–653. doi: 10.1097/MLR.0b013e31817a835d. [DOI] [PubMed] [Google Scholar]
- Andersen RM, Hongjian Yu R, Wyn PL, Brown ER, Teleki S. Access to medical care for low-income persons: How do communities make a difference? Medical Care Research and Review. 2002;59:384–411. doi: 10.1177/107755802237808. [DOI] [PubMed] [Google Scholar]
- Andersen RM, Newman JF. Societal and Individual Determinants of Medical Care Utilization in the United States. Milbank Quarterly. 2005;83 doi: 10.1111/j.1468-0009.2005.00428.x. Online-only. [DOI] [PubMed] [Google Scholar]
- Burns BJ, Costello EJ, Angold A, Tweed D, Stangl D, Farmer EM, Erkanli A. Children’s mental health service use across service sectors. Health Affairs. 1995;14:147–159. doi: 10.1377/hlthaff.14.3.147. [DOI] [PubMed] [Google Scholar]
- Barrett PM, Turner CM. In: Prevention strategies. Morris TL, March JS, editors. New York, NY, US: Guilford Press; 2004. [Google Scholar]
- Cabassa LJ. Latino immigrant men’s perceptions of depression and attitudes toward help seeking. Hispanic Journal of Behavioral Sciences. 2007;29:492–509. doi: 10.1177/0739986307307157. [DOI] [Google Scholar]
- Cardemil EV, Adams ST, Calista JL, Connell J, Encarnación J, Esparza NK, Wang E. The Latino mental health project: A local mental health needs assessment. Administration and Policy in Mental Health and Mental Health Services Research. 2007;34:331–341. doi: 10.1007/s10488-007-0113-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavira DA, Garland A, Yeh M, McCabe K, Hough RL. Child anxiety disorders in public systems of care: Comorbidity and service utilization. The Journal of Behavioral Health Services & Research. 2009;36:492–504. doi: 10.1007/s11414-008-9139-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavira DA, Stein MB, Bailey K, Stein MT. Child anxiety in primary care: Prevalent but untreated. Depression and Anxiety. 2004;20:155–164. doi: 10.1002/da.20039. [DOI] [PubMed] [Google Scholar]
- Conger RD, Rueter MA. In: Siblings, parents, and peers: A longitudinal study of social influences in adolescent risk for alcohol use and abuse. Brody GH, editor. Westport, CT, US: Ablex Publishing; 1996. [Google Scholar]
- Deacon B, Lickel J, Abramowitz JS. Medical utilization across the anxiety disorders. Journal of Anxiety Disorders. 2008;22:344–350. doi: 10.1016/j.janxdis.2007.03.004. [DOI] [PubMed] [Google Scholar]
- Diefenbach GJ, Robison JT, Tolin DF, Blank K. Late-life anxiety disorders among Puerto Rican primary care patients: Impact on well-being, functioning, and service utilization. Journal of Anxiety Disorders. 2004;18:841–858. doi: 10.1016/j.janxdis.2003.10.005. [DOI] [PubMed] [Google Scholar]
- Dillman Carpentier FR, Mauricio AM, Gonzales NA, Millsap RE, Meza CM, Dumka LE, Genalo MT. Engaging Mexican origin families in a school-based preventive intervention. The Journal of Primary Prevention. 2007;28:521–546. doi: 10.1007/s10935-007-0110-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobalian A, Rivers PA. Racial and ethnic disparities in the use of mental health services. The Journal of Behavioral Health Services & Research. 2008;35:128–141. doi: 10.1007/s11414-007-9097-8. [DOI] [PubMed] [Google Scholar]
- Documét PI, Sharma RK. Latinos’ health care access: Financial and cultural barriers. Journal of Immigrant Health. 2004;6:5–13. doi: 10.1023/B:JOIH.0000014638.87569.2e. [DOI] [PubMed] [Google Scholar]
- Ebesutani C, Bernstein A, Nakamura BJ, Chorpita BF, Higa-McMillan CK, Weisz JR. Concurrent validity of the child behavior checklist DSM-oriented scales: Correspondence with DSM diagnoses and comparison to syndrome scales. Journal of Psychopathology and Behavioral Assessment. 2010;32:373–384. doi: 10.1007/s10862-009-9174-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer EM, Burns BJ, Phillips SD, Angold A, Costello EJ. Pathways into and through mental health services for children and adolescents. Psychiatric Services. 2003;54:60–66. doi: 10.1176/appi.ps.54.1.60. [DOI] [PubMed] [Google Scholar]
- Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in health care by race, ethnicity, and language among the insured: Findings from a national sample. Medical Care. 2002;40:52–59. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- Flores G, Abreu M, Olivar MA, Kastner B. Access barriers to health care for Latino children. Archives of Pediatrics & Adolescent Medicine. 1998;152:1119–1125. doi: 10.1001/archpedi.152.11.1119. [DOI] [PubMed] [Google Scholar]
- Flores G, Vega LR. Barriers to health care access for Latino children: A review. Family Medicine. 1998;30:196–205. [PubMed] [Google Scholar]
- Garcia JA, Weisz JR. When youth mental health care stops: Therapeutic relationship problems and other reasons for ending youth outpatient treatment. Journal of Consulting and Clinical Psychology. 2002;70:439–443. doi: 10.1037/0022-006X.70.2.439. [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, Silverman WK. Phobic and anxiety disorders in Hispanic and Caucasian youth. Journal of Anxiety Disorders. 1996;10:517–528. doi: 10.1016/S0887-6185(96)00027-8. [DOI] [Google Scholar]
- Halfon N, Wood DL, Valdez RB, Pereyra M, Duan N. Medicaid enrollment and health services access by Latino children in inner-city Los Angeles. Journal of the American Medical Association. 1997;277:636–641. doi: 10.1001/jama.1997.03540320038032. [DOI] [PubMed] [Google Scholar]
- Horwitz SM, Gary LC, Briggs-Gowan MJ, Carter AS. Do needs drive services use in young children? Pediatrics. 2003;112:1373–1378. doi: 10.1542/peds.112.6.1373. [DOI] [PubMed] [Google Scholar]
- Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: Variation by ethnicity and insurance status. The American Journal of Psychiatry. 2002;159:1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Sugarman A. Attrition in the treatment of childhood anxiety disorders. Journal of Consulting and Clinical Psychology. 1997;65:883–888. doi: 10.1037/0022-006X.65.5.883. [DOI] [PubMed] [Google Scholar]
- Leaf PJ, Bruce ML, Tischler GL, Holzer CE. The relationship between demographic factors and attitudes toward mental health services. Journal of Community Psychology. 1987;15:275–284. doi: 10.1002/1520-6629(198704)15:2<275::AID-JCOP2290150216>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- Lewis MJ, West B, Bautista L, Greenberg AM, Done-Perez I. Perceptions of service providers and community members on intimate partner violence within a Latino community. Health Education & Behavior. 2005;32:69–83. doi: 10.1177/1090198104269510. [DOI] [PubMed] [Google Scholar]
- Magaña SM, García JIR, Hernández MG, Cortez R. Psychological distress among Latino family caregivers of adults with schizophrenia: The roles of burden and stigma. Psychiatric Services. 2007;58:378–384. doi: 10.1176/appi.ps.58.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Hilt LM, Nolen-Hoeksema S. Racial/ethnic differences in internalizing and externalizing symptoms in adolescents. Journal of Abnormal Child Psychology. 2007;35:801–806. doi: 10.1007/s10802-007-9128-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas K, He J, Burstein M, Swanson S, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the national comorbidity study-adolescent supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura BJ, Ebesutani C, Bernstein A, Chorpita BF. A psychometric analysis of the child behavior checklist DSM-oriented scales. Journal of Psychopathology and Behavioral Assessment. 2009;31:178–189. doi: 10.1007/s10862-008-9119-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council and Institute of Medicine (NCR/IOM) Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- Owens PL, Hoagwood K, Horwitz SM, Leaf PJ, Poduska JM, Kellam SG, Ialongo NS. Barriers to children’s mental health services. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:731–738. doi: 10.1097/00004583-200206000-00013. [DOI] [PubMed] [Google Scholar]
- Pew Hispanic Center. Indicators of Recent Migration Flows from Mexico. 2007 May; Retrieved June 14, 2011 from http://pewhispanic.org/files/factsheets/33.pdf.
- Pina AA, Silverman WK. Clinical phenomenology, somatic symptoms, and distress in Hispanic/Latino and European American youths with anxiety disorders. Journal of Clinical Child and Adolescent Psychology. 2004;33:227–236. doi: 10.1207/s15374424jccp3302_3. [DOI] [PubMed] [Google Scholar]
- Pina AA, Silverman WK, Weems CF, Kurtines WM, Goldman ML. A comparison of completers and noncompleters of exposure-based cognitive and behavioral treatment for phobic and anxiety disorders in youth. Journal of Consulting and Clinical Psychology. 2003;71:701–705. doi: 10.1037/0022-006X.71.4.701. [DOI] [PubMed] [Google Scholar]
- Portes A, Kyle D, Eaton WW. Mental illness and help-seeking behavior among Mariel Cuban and Haitian refugees in south Florida. Journal of Health and Social Behavior. 1992;33:283–298. doi: 10.2307/2137309. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology. 1983;51:390–395. doi: 10.1037/0022-006X.51.3.390. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: Applications to addictive behavior. American Psychologist. 1992;47:1102–1114. doi: 10.1037/0003-066X.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. American Journal of Health Promotion. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- Roosa MW, Liu FF, Torres M, Gonzales NA, Knight GP, Saenz D. Sampling and recruitment in studies of cultural influences on adjustment: A case study with Mexican Americans. Journal of Family Psychology. 2008;22:293–302. doi: 10.1037/0893-3200.22.2.293. doi: http://dx.doi.org/10.1037/0893-3200.22.2.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheppers E, van Dongen E, Dekker J, Geertzen J, Dekker J. Potential barriers to the use of health services among ethnic minorities: A review. Family Practice. 2006;23:325–348. doi: 10.1093/fampra/cmi113. [DOI] [PubMed] [Google Scholar]
- Shi L, Stevens GD. Disparities in access to care and satisfaction among U.S. children: The roles of race/ethnicity and poverty status. Public Health Reports. 2005;120:431–441. doi: 10.1177/003335490512000410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner JL, Cockerham WC, Spaeth JL. Predicting physician utilization. Medical Care. 1983;21:360–369. doi: 10.1097/00005650-198303000-00008. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. Profile of General Population and Housing Characteristics: 2010. 2010 Retrieved March 31, 2012, from http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=DEC_10_SF2_SF2DP1&prodType=table.
- Varela RE, Sanchez-Sosa JJ, Biggs BK, Luis TM. Anxiety symptoms and fears in Latin American and European American children: Cross-cultural measurement equivalence. Journal of Psychopathology and Behavioral Assessment. 2008;30:132–145. doi: 10.1007/s10862-007-9056-y. [DOI] [Google Scholar]
- Vega WA, Kolody B, Aguilar-Gaxiola S. Help seeking for mental health problems among Mexican Americans. Journal of Immigrant Health. 2001;3:133–140. doi: 10.1023/A:1011385004913. [DOI] [PubMed] [Google Scholar]
- Vega WA, Lopez SR. Priority issues in Latino mental health services research. Mental Health Services Research. 2001;3:189–200. doi: 10.1023/A:1013125030718. [DOI] [PubMed] [Google Scholar]
- Weathers A, Minkovitz C, O’Campo P, Dierner-West M. Health services use by children of migratory agricultural workers: Exploring the role of need for care. Pediatrics. 2003;111:956–963. doi: 10.1542/peds.111.5.956. [DOI] [PubMed] [Google Scholar]
- Yeh M, McCabe K, Hough RL, Dupuis D, Hazen A. Racial/ethnic differences in parental endorsement of barriers to mental health services for youth. Mental Health Services Research. 2003;5:65–77. doi: 10.1023/A:1023286210205. [DOI] [PubMed] [Google Scholar]


