Abstract
The management of recurrent patellofemoral instability is challenging. The etiology of the instability is multifactorial, requiring the examination of lower limb alignment, relationship of the patella to the trochlear groove and tibial tubercle, and the soft-tissue restraints. As initial surgical efforts were aimed at isolated soft-tissue repair or reconstruction, patients often had continued instability. Thus, a heightened interest in trochleoplasty has occurred as trochlear dysplasia has been found in 85% of patients with recurrent instability. Different types of trochleoplasties have been developed depending on the type of dysplasia including the trochlear lengthening osteotomy, the proximal open trochleoplasty, the deepening trochleoplasty, and the arthroscopic deepening trochleoplasty. The techniques, benefits, and results of these trochleoplasties will be presented in this review.
Keywords: trochlear dysplasia, trochleoplasty, patellofemoral instability
Patellofemoral instability is both complex and multifactorial. After an initial patellar dislocation, recurrent patellofemoral pain and disability may ensue. After a first time patellar dislocation, historical data show that there is a 17% incidence of recurrent dislocation over a 5-year period.1 However, for individuals with a history of instability, the recurrence rate is 49% for patellar dislocation.1 This high recurrence rate is associated with a young age at the first time of the first dislocation and is often associated with preexisting anatomic factors that reduce patellar constraint.2 These factors are trochlear dysplasia, patella alta, increased lateralization of the tibial tubercle in relation to the trochlear groove, axial rotation of the femur and tibia, and insufficient medial retinacular restraint.2
Trochlear dysplasia involves an abnormality of the shape and depth of the trochlear groove and has been found in 85% of individuals with recurrent patellofemoral instability.3 Dejour et al.,3 described several different types of dysplasia with some involving a shallower trochlear groove, a flat groove, and even a trochlear bump present in some. In an effort to treat individuals with recurrent patellofemoral instability secondary to trochlear dysplasia, there are multiple different procedures that address the morphologic abnormality of the trochlear groove. These “trochleoplasties” are designed to change and normalize the shape of the trochlear groove. They include the proximal open trochleoplasty, the deepening trochleoplasty, the trochlear lengthening osteotomy, and the arthroscopic deepening trochleoplasty.
To help better understand the role of trochleoplasty, it is necessary to understand the nature and severity of trochlear dysplasia. We therefore will first briefly review the Dejour classification and then elucidate which specific aspect of dysplasia can be corrected with each of these 4 procedures. We will then describe the techniques briefly and review the clinical data available to judge the success of these procedures. Finally, we will formulate a recommendation as to when best to address trochlear morphology surgically, based upon today’s best evidence.
CLASSIFICATION OF TROCHLEAR DYSPLASIA
Different classification schemes have been used in the past to provide the clinician with information to guide treatment decisions. Maldague and Malghem 4 introduced a classification system that is based on the lateral radiograph and the corresponding depth of the sulcus. Although this is the earliest classification system it is not widely used. More commonly used is the "Dejour modified classification" which describes 4 distinct types.5 This classification system is based on lateral and axial views of the knee.
The 4 distinct types of the Dejour classification direct the focus onto the respective anatomic portion of the trochlea that is dysplastic. These elements are:
the entry into the trochlear groove (proximal convexity or trochlear bump);
the lateral trochlear facet;
the medial trochlear facet.
Using these anatomic aspects of the patella-femoral trochlea, Dejour described the following subtypes:
-
Type A: has a crossing sign seen on the lateral radiograph and a sulcus angle >145 degrees on the axial view.
= >This represents a nearly normally configured trochlea groove that is shallow but otherwise normally configured. This may also be considered as a normal anatomic variant.
-
Type B: demonstrates a supratrochlear spur sign on lateral radiographs and the axial views show a flat trochlea.
=>This represents a shallow trochlear groove that has a proximal convexity (supratrochlear spur or bump). The lateral and medial trochlear facets are otherwise normal.
-
Type C: has both a crossing sign and a double contour on the lateral radiograph; whereas, the axial view demonstrates the convexity of the lateral trochlear facet and the hypoplasia of the medial trochlear facet.
=>This trochlea may show a normal superior entry. The lateral facet, however, is flat or convex and leads into a hypoplastic and sometimes down-sloping medial trochlear facet.
-
Type D: has a crossing sign, supratrochlear spur, and the double contour sign on the lateral radiograph; whereas, the axial view demonstrates the asymmetry of the facets with a cliff between the medial and lateral trochlear facets.
=>This is the most severe dysplasia. It has a convex lateral trochlear facet that ends proximally into a significant supratrochlear spur (or bump). The medial trochlear facet is minimal or absent, sometimes creating a "cliff"-like appearance on the axial [magnetic resonance imaging (MRI)] images.
INDICATION / CONTRAINDICATION OF TROCHLEOPLASTIES
A trochleoplasty is a surgical correction of the femoral trochlea to restore a normal or nearly normal entry of the patella into the trochlear groove during extension and flexion. Some general prerequisites are necessary to performing this procedure successfully.
As a trochleoplasty aims to reshape the bony anatomy of the trochlea with the ultimate goal to reshape the cartilaginous groove it is necessary to have normal or nearly normal (International Cartilage Repair Society grade 1 or 2) articular cartilage in the trochlea. Higher grade articular cartilage changes or established patellofemoral arthritis (Iwano >=2) cannot be addressed with a trochleoplasty.6
It is important to understand that trochleoplasties do often require additional surgical procedures such as a Fulkerson osteotomy or a medial patellofemoral ligament reconstruction depending on the extent of the underlying injury history and symptoms.
Any of these procedures are clearly contraindicated in patients who complain about anterior knee pain without any signs of patellofemoral instability!
TYPES OF TROCHLEOPLASTIES
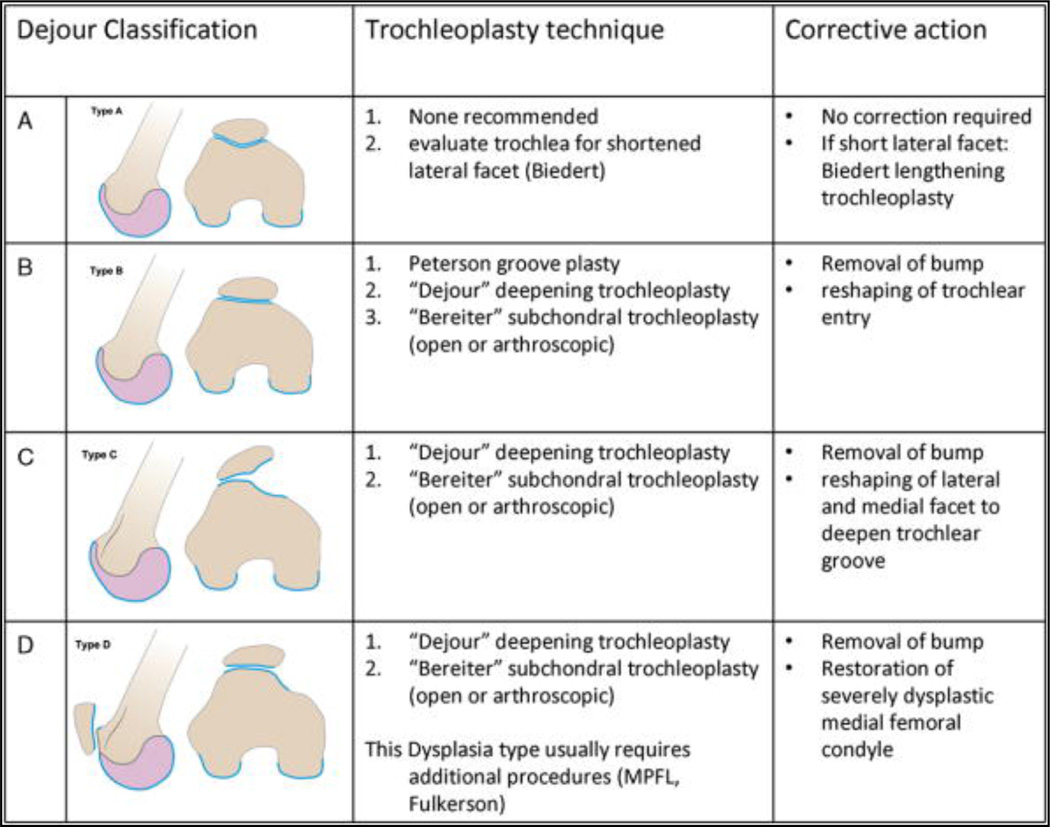
Following the Dejour concept one can distinguish the different types of surgical trochleoplasties according to which one of the main three anatomic factors of dysplasia they alter. This defines their utility and indication.
The most simple trochleoplasty technique is the one described by Peterson et al 7 in 1988. This proximal open "groove plasty" addresses the supratrochlear spur by essentially removing the spur and creating a bony grove in the superior trochlea to guide the entry of the patella into the trochlea. The lateral or medial trochlear facet cannot be corrected using this technique. This technique therefore may be useful for patients who have a Dejour type 2 deformity with a prominent supratrochlear spur but no other dysplastic signs.7
The classic Dejour deepening trochleoplasty is designed to deepen the proximal trochlea. It allows for the removal of the supratrochlear spur and for reduction of the convexity of the lateral facet. It is therefore able to correct the Dejour type B and C dysplasia most adequately. It is difficult with this technique to anatomically rebuild a dysplastic medial trochlear facet but it can be used for Dejour type D deformities. In this case it is often combined with other additional procedures [i.e., medial patellofemoral ligament (MPFL), Fulkerson osteotomy].8
The subchondral deepening trochleoplasty as described by Bereiter and popularized arthroscopically by Blond and Schoettle, offers the same spectrum as the Dejour deepening trochleoplasty.9–11 Technically more difficult but potentially less invasive, it allows for the removal of the supratrochlear spur and for recontouring of the lateral trochlear facet.
A different pathology can be addressed by the lateral lengthening trochleoplasty as described by Biedert.12 This technique addresses a hypoplastic lateral trochlear facet and will be described later in this discourse (Fig. 1).
Figure 1.
Indications for different types of trochleoplasties on the basis of the Dejour classification.
Deepening Trochleoplasty (Dejour Technique)
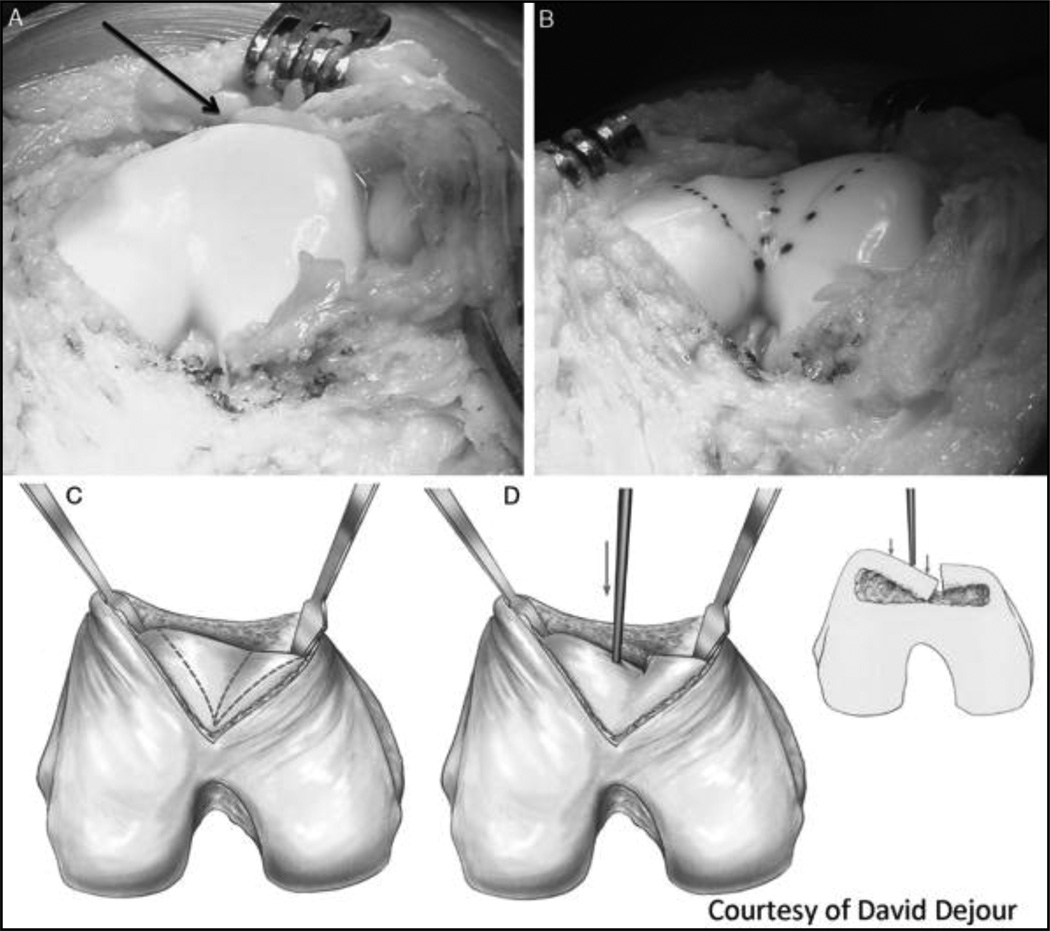
With the patient in the supine position, the affected leg is prepped and draped. With the knee flexed at 90 degrees, a midline incision is made over the knee extending from the superior pole of the patella to the lower region of the patella. Full thickness flaps are then developed and a mid-vastus arthrotomy is performed for visualization of the knee joint. This procedure can also be carried out through a superolateral parapatellar incision.
The patella is then either subluxed or everted to allow for access to the trochlea. The supratrochlear region is then cleared of synovium and adipose tissue. The periosteum is incised and elevated to reveal the anterior cortex of the femur.
Next, planning for the new trochlea is performed. A straight line is drawn from midpoint at the top of the intercondylar notch and is extended proximal in a 3- to 6-degree lateral manner. Two additional divergent lines are drawn, starting from the top of the intercondylar notch and extending medial and laterally. These will represent the new medial and lateral trochlear facets.
To gain access to the cancellous bone of the trochlea, one must remove a thin strip of cortical bone at the osteochondral edge at the supratrochlear region. This is completed with an osteotome. Cancellous bone from the trochlea must now be removed. This can be achieved with a special burr and a guide that maintains a 5-mm thick osteochondral flap or can be done free hand. More bone needs to be removed centrally within the groove than medial or lateral. The burr must be extended to the intercondylar notch. Once sufficient bone has been removed, the trochlea groove will become more mobile and light pressure may be applied to determine if the osteochondral flap is mobile enough. If additional mobility is needed, the medial and lateral facets may need to be osteotomized externally first with a scalpel and then completed with an osteotome.
Once the medial and lateral facets with appropriate deepening of the trochlea is completed, the 2 facets are bent into the new trochlear bed and fixed. Fixation has initially been described by using 2 hand-made staples using 1-mm K-wirefixation.5 Alternatively, biodegradable double-pitched screws (Arthrex; Naples,FL) or nonresorbable screws (Accutrak, Acumed Hillsboro, OR) can be used for this purpose. All implants are countersunk below the chondral surface to prevent any damage to the patella in the future. The periosteum and synovium are then repaired (Fig. 2).
Figure 2.
(A–D). "Dejour" deepening trochleoplasty. This is a case of a patient who has a Dejour type B deformity with a prominent supratrochlear spur ("bump" is indicated by the black arrow) (A). After correction with the Dejour technique a normalized trochlear groove is restored and the bump has disappeared (B). Technically, this is carried out by identifying the center of the trochlear groove (C) and subsequently undermining the lateral facet and the bump to reshape the trochlea using either a burr or an osteotome. The undermined lateral (and or medial) flap can then be gently be pushed onto the neotrochlear bed after the center of trochlear groove has been split sharply with an osteotome (D). The flaps can then be fixed using a staple or headless screws (metal or bioabsorbable). This case is courtesy of David Dejour.
At this time, any additional realignment procedures can be performed safely.
Subchondral Deepening Trochleoplasty (Bereiter Technique)
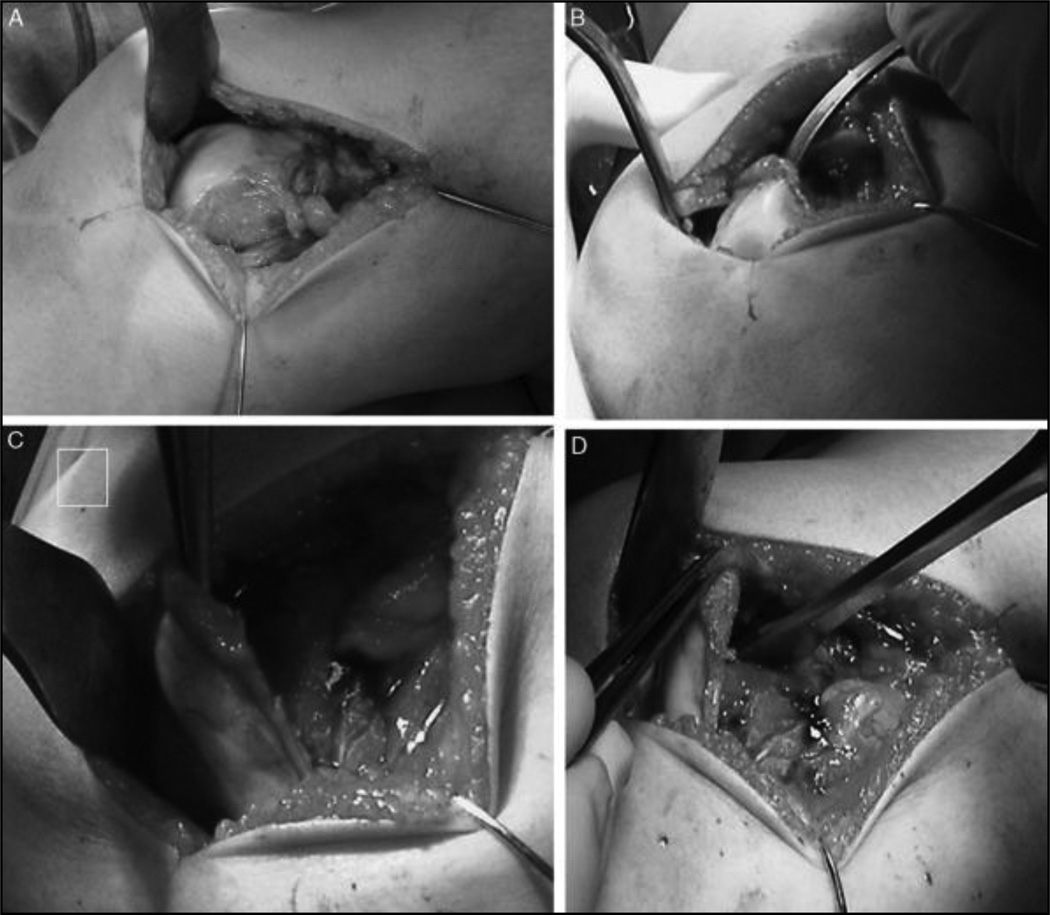
The approach is identical to the approach described for the Dejour technique and can be performed through a midline or superolateral parapatellar approach. To allow for improved visualization, the synovial tissue is removed from the region just proximal to the trochlear groove, using an electrocaustic. Sufficient amount of tissue must be cleared down to cortical bone.
The next step involves separating the cartilaginous trochlea from the underlying bone. Typically, a sharp curved osteotome is used to create this "cartilage flake," starting from the proximal lateral trochlea.11 This cartilage flake is developed gradually, avoiding damage to the cartilage. It is crucial to remove the underlying bone from the cartilage using a bur or shaver to allow for the cartilage flake to plastically conform to the contour of the deepened trochlear groove.
The next step involves deepening the trochlear groove using a burr or straight osteotome. Starting proximally and laterally, the groove is deepened until a more normal contour of the groove has been developed. The cartilage flake is then pressed onto the newly remolded groove and assessment is made if further deepening is needed at that time (Fig. 3).
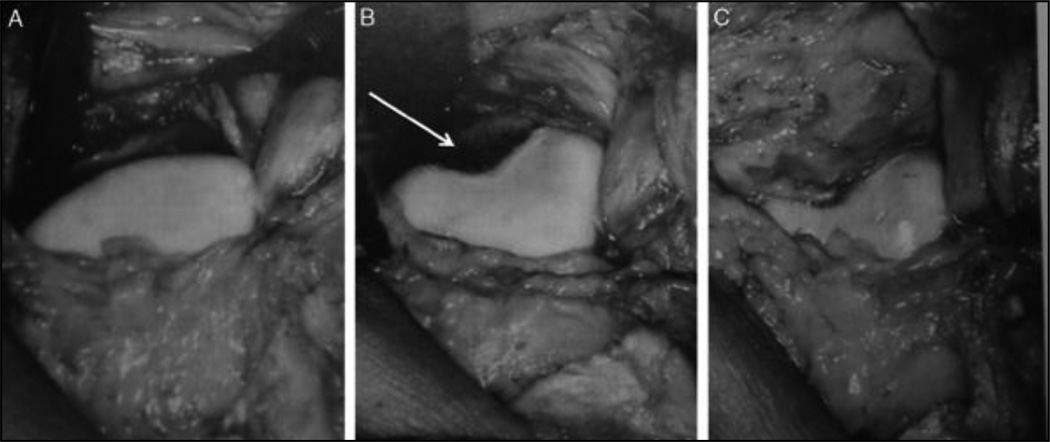
Figure 3.
"Bereiter" deepening trochleoplasty. The Bereiter deepening trochleoplasty can be performed open or arthroscopically. In this open example the trochlea is exposed through a superolateral parapatellar approach (A). A sharp curved osteotome is used to divide the subchondral bone sharply from the articular cartilage. Great care must be taken not to cut the cartilage flap during this process. (B) Once the flap is sufficiently elevated (C) the deepening of the trochlear groove can be performed using a straight osteotome (D). Images courtesy of Philipp Schottle.
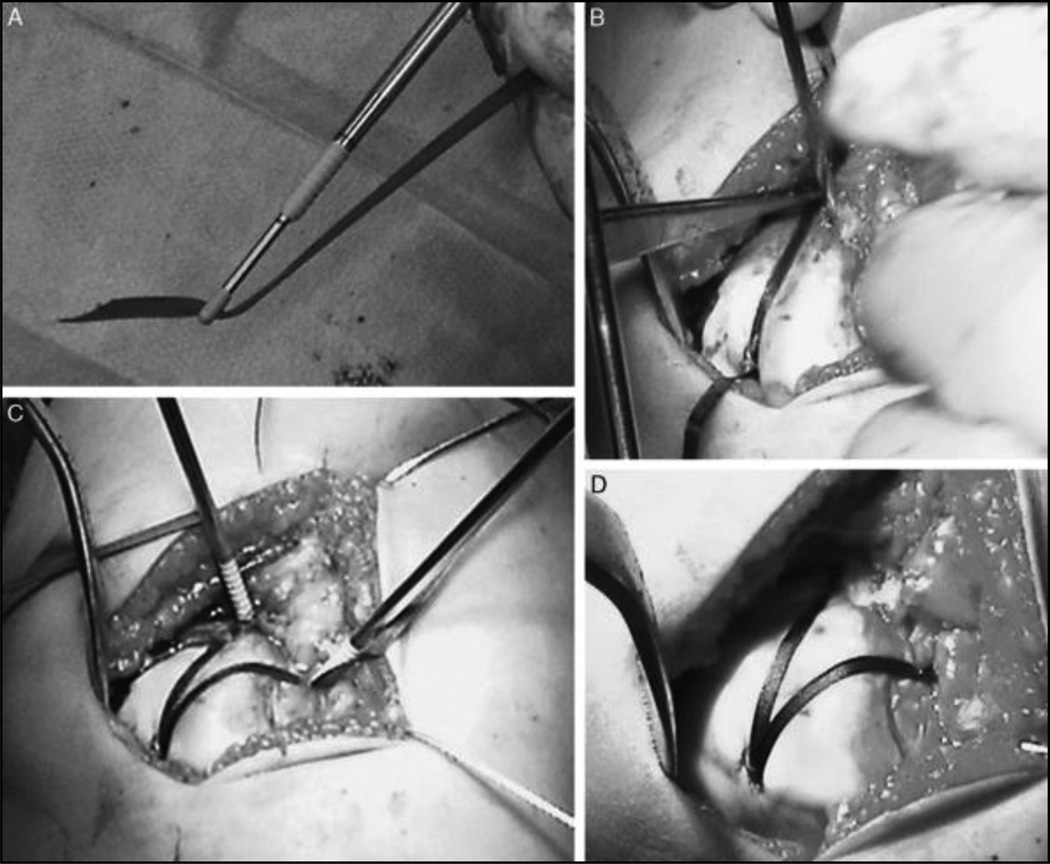
Fixation of the cartilage flake is then achieved with 3 knotless suture anchors (pushlock). The anchor is loaded with a 3-mm resorbable tape. Fixation is first made distally. A hole for the anchor is drilled just distal to the cartilage flake in the central portion of the groove. The anchor is then inserted securing the tape within the bone. Placement of the 2 remaining anchors is done centrally at the proximal most extent of the trochlea (Fig. 4). The remaining tape end is shuttled into the third suture anchor and is placed over the lateral trochlea and secured over the lateral trochlear ridge into the distal femur under tension. This restores the curvature and shape of the trochlea and secures the cartilage flap to the neotrochlea. This procedure can also be performed arthroscopically as described by Biedert.13
Figure 4.
"Bereiter" deepening trochleoplasty (cont). Once the trochlear groove is sufficiently prepared the cartilage flap is rolled into the neotrochlea. Fixation of the cartilage flap is carried out using an Arthrex pushlock anchor (Arthrex; Naples, FL). The normal sutures of this anchor have to be exchanged with a 3-mm resorbable tape (A). The tape is loaded halfway leaving equal length of tape on both ends. The loaded pushlock anchor is placed in the center of the trochlear groove at the inferior pole of the trochlea and secured to bone. Then the 1 end of the tape is brought proximal along the deep center ridge of the neotrochlea and a second pushlock anchor is loaded onto the tape. The second pushlock anchor is secured at the proximal most extension of the trochlear groove (B, C). The lateral limb of the tape is then brought over the lateral trochlear ridge and secured to the distal femur tensioning the entire construct and firmly securing the cartilage flap to the neotrochlea (C, D). Images courtesy of Philipp Schottle.
Proximal Open Trochleoplasty (Groove Plasty)
With the patient in the supine position, the affected leg is prepped and draped. With the knee flexed at 90 degrees, midline incision is made over the knee extending from the superior pole of the patella to the lower region of the patella. Full thickness flaps are then developed and a medial or lateral arthrotomy is performed for visualization of the knee joint.
The synovial lining is released from the articular border of the proximal trochlea in a proximal direction. Then a line is drawn from the center of the top of the intercondylar notch to the proximal extent of the cartilaginous trochlea. Measuring from the proximal trochlea to a point approximately 10 mm distal on this central line, additional lines are drawn both proximal medial and proximal lateral. This creates a V-shaped configuration on the trochlear groove. Using a curved osteotome, cartilage and bone are then removed from this central portion to a depth of approximately 5 mm. Additional bone can be removed from the proximal extent of this concavity to provide a smooth transition. To ensure enough bone has been removed, the patella can be monitored during flexion/extension and additional bone may be removed depending on the type of trochlear dysplasia.
The previously released synovial lining is then sutured to the cartilage border at the distal aspect of the deepened groove using reabsorbable suture. It is best to start the suture through the synovial lining and then penetrate the cartilage layer to a depth of 10 mm. The suture is brought through and then the suture is placed back through the cartilage layer approximately 2 to 3 mm away from the previous exit point. The suture is brought through the synovium next to perform a horizontal mattress suture. Then, additional sutures are placed in a similar manner at 6- to 8-mm intervals until the synovium has been brought back to the cartilage layer. If difficulty is encountered with this step, then a transverse release can be performed proximally of the synovium so that there is not a gap between the synovium and the cartilage.
The final step is to inject fibrin glue to fix the synovial lining. Firm pressure should be applied with a dry sponge on the synovium for 2 minutes to allow for the synovium to adhere to the cartilage.
Trochlear Lengthening Osteotomy (Biedert)
Biedert 13 identified a further variant of trochlear dysplasia: the too short lateral trochlea. It is important to note that Biedert 13 identified that this new subset of patients will not present with the typical radiographic findings associated with trochlear dysplasia. Instead, the radiographs will only show the typical dysplastic findings if it is associated with another type of dysplasia (Fig. 5).
Figure 5.
"Peterson" proximal groove plasty. The supratrochlear bump is exposed (A). Then a round osteotome is used to create a neotrochlea in the proximal portion of the trochlear entry. This step will remove a portion of the dysplastic trochlea articular cartilage (white arrow) proximally (B). Then the supratrochlear synovium is carefully advanced and sutured to the proximal cartilage border of the remaining trochlea covering the neotrochlea (C). These images are courtesy of Lars Peterson.
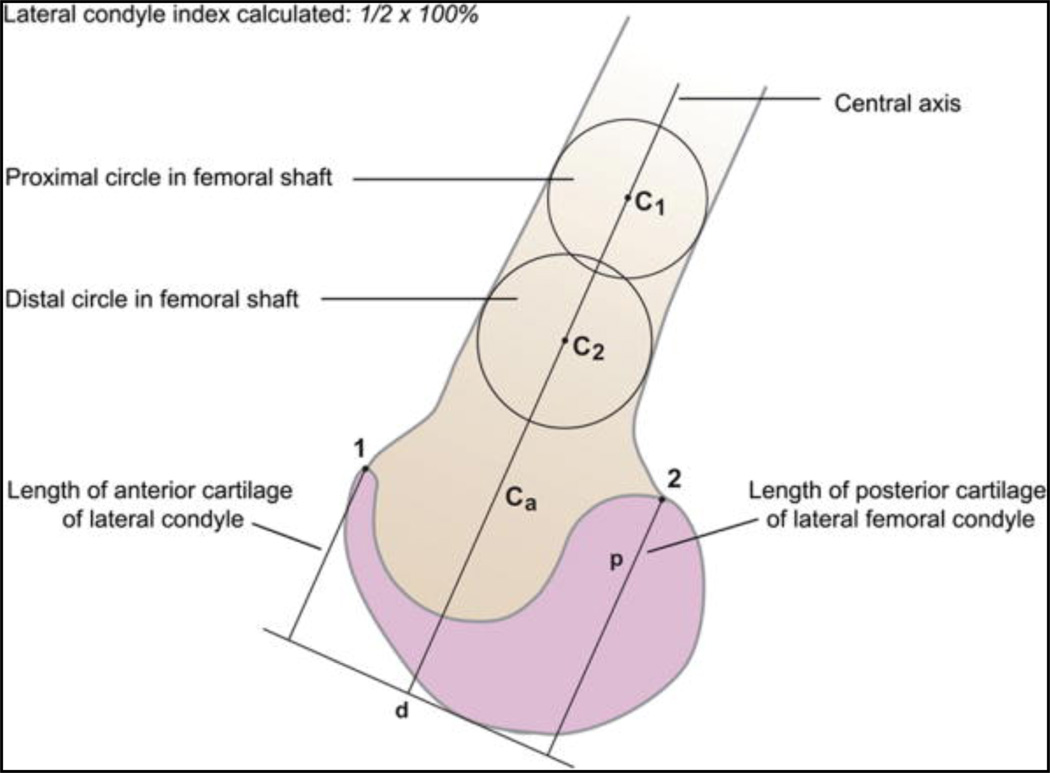
To diagnose this dysplastic lateral trochlea, MRI is required to examine the proximal portion of the trochlea and determine if the lateral trochlea is too short. To make this diagnosis, Biedert 14 developed the lateral condyle index, which is demonstrated in Figure 6. In brief, this index is based upon the length of the lateral trochlea's anterior surface in relation to the lateral trochlea's posterior surface on the sagittal MRI sequence. Biedert 14 found that in normal individuals, this index was on average 93%. Individuals with a deficient lateral trochlea show an average value of 84%.14 Thus, they concluded that individuals with lateral condyle indices of =93% have a normal lateral trochlea. In individuals with an index between 86% and 93% the trochlea may be too short and a contributing factor, however, no clear pathology can be assigned and the clinician must assure that no other risk factors may be present.14 Thus, the trochlear lengthening osteotomy is indicated when patients present with patellar instability and the MRI demonstrates a shortened lateral trochlea based on the lateral condyle index (Fig. 7).14
Figure 6.
Lateral trochlear index. To calculate the lateral femoral condyle index, a perpendicular is drawn to the line denoting the Ca. The distance between this perpendicular and point 1 is divided by the distance between the perpendicular and point 2 and is expressed as a percentage. C1 indicates proximal circle in the femoral shaft; C2, distal circle in the femoral shaft; Ca, central axis of femur; 1, superior most aspect of anterior cartilage of the lateral condyle; 2, superior most aspect of posterior cartilage of the lateral condyle.
Figure 7.
"Biedert" lengthening trochleoplasty. This is a case of a young patient who has recurrent lateral patella dislocations and a lateral trochlea index of <86%. She had a short lateral trochlea (A), however, otherwise normal radiographic findings. Through a superolateral parapatellar approach the lateral trochlea was exposed and the osteotomy was carried from the edge of the lateral trochlea into the distal femur for approximately 1 cm proximal to the previous superior trochlear length (B). The osteotomy was then elevated using bone graft by approximately 5 mm with the apex of the neotrochlea 6 to 7 mm (in this particular case as measured by the trochlear index) more proximal (C, the white arrow indicates the new apex of the trochlea). The black arrow indicates the prior superior apex of the lateral trochlea (C). These images are courtesy of Roland Biedert.
Surgical Technique
Through a lateral parapatellar incision, a layered lateral retinacular lengthening is performed first. The superficial lateral retinaculum is localized and is incised longitudinally 1 cm from the border of the patella. This portion is then separated from the oblique portion of the retinaculum.
The oblique portion and synovial layer are then incised to gain access to the patellofemoral joint.
The superficial portion will be repaired at the conclusion of the procedure to allow for its effective lengthening.12
Inspection of the relationship of the patella to the lateral trochlear facet allows one to determine the appropriate amount of lengthening that is required. Biedert and Albrecht,15 determined the patellotrochlear index or overlap of the patella with the lateral trochlea in full extension to be one third. To perform the osteotomy, one begins approximately 5 mm from the cartilage edge at the sulcus terminalis. The osteotome is inserted approximately 1 to 1.5 cm deep and the cut is propagated proximally towards the femoral shaft. Once this cut has been made, the length of the osteotomy can be adjusted based upon attempting to recreate the normal patellofemoral overlap indicated previously. The osteotomy is then spread through the osteotome. There is potential for distal fracture of the cartilage, which should be avoided. With the osteotomy complete, elevation of the lateral facet may be needed as well. Cancellous autograft bone can be obtained from the ipsilateral posterior lateral femoral condyle or proximal tibia and impacted under the osteotomy. The lateral trochlear facet is typically elevated approximately 5 to 6 mm (Fig. 4). It is important not to overcorrect the flat trochlea to avoid lateral hypercompression.12 Postoperatively, the patients are maintained on protective weight bearing for 3 to 4 weeks to prevent hypercompression of the osteotomy. To help establish the patellofemoral gliding mechanism and form the new osteotomy, continuous passive motion is established early in the postoperative period, as with all trochleoplasties.
CLINICAL AND RADIOGRAPHIC OUTCOMES OF TROCHLEOPLASTIES
Only few studies have reported on the radiographic and clinical outcomes after trochleoplasties. The results from trochleoplasty have been promising in regards to recreating normal radiographic indices. Fucentese et al 16 examined 17 knees after trochleoplasty using computed tomography. They found that the trochlear depth improved from 0 to 5.9 mm in the proximal trochlea; and, the sulcus angle improved from 172.1 to 133 degrees postoperatively. These values correlate to the lateral radiographic results obtained by Schottle et al.9 In their study of 19 knees, the trochlear depth improved from 0.6 to 7 mm.
From a stability standpoint, trochleoplasty improves the stability of the patella during range of motion. In the same study by Schottle et al 9 referenced earlier, they found a 0% redislocation rate. This improved stability has been confirmed by additional studies as well.10,17 It should be noted that Fucentese et al 17 found a 25% persistent apprehension sign in full extension and emphasized the need to perform a MPFL reconstruction at the time of the trochleoplasty to provide additional stability when the knee is in full extension.
Donell and colleagues followed 15 patients who underwent deepening trochleoplasty with a mean follow-up of 3 years. Trochleoplasty was indicated if there was a loss of >6 mm, and associated procedures were performed as required. They found that in 17 knees (15 patients), 9 had had previous surgery for patellar instability. At 3 years of follow-up, 11 knees tracked normally and 6 had a slight J-sign. Seven knees had mild residual apprehension. Seven patients were very satisfied, 6 were satisfied, and 2 were disappointed. The Kujala score improved from an average of 48 to 75. However, 8 of the 15 patients achieved this result after additional arthroscopic surgeries for arthrofibrosis between 6 and 12 weeks postoperatively.18
The results with regard to pain and satisfaction with the procedure have been mixed. Utting et al 19 found a 92% satisfaction rate after trochleoplasty with an improvement in the Kujala score from 62 to 76. The Schottle study found a similar improvement in the Kujala score, improving from 56 to 80.9 In a longer follow-up at 14 years, von Knoch et al 10 found the final Kujala scores to be 94.9. In this same study, all but 1 patient experienced an increased level of sporting activity. However, the reliability for a decrease in knee pain on a subjective scale was less predictable after trochleoplasty. von Knoch et al 10 found only a 49% improvement in subjective knee pain with 9% of the patients having no change and 33% of the patients having increased pain after the trochleoplasty. Fucentese et al 17 had similar results for pain control after the procedure with only 14 patients having improvement in their pain, whereas 27 patients had no change in their pain, and 3 patients had increased pain.
Dejour examined 2 separate cohorts of patients. One cohort of 18 patients with previously failed patellofemoral surgeries and 1 cohort of 44 patients who have not had previous surgery. He followed both groups for an average of 6 years and reported their subjective outcomes based upon the International Knee Documentation Committee score. He found that patients without previous surgery were satisfied or very satisfied in 85%, whereas patients with previous surgery had slightly lower satisfaction ratings being satisfied or very satisfied in 65%. Dejour pointed out that there is a significant difference with regards to residual pain in follow-up. Patients without previous surgery reported residual pain only in 5%, whereas patients with previous surgeries reported pain in 28%.20
These data were corroborated by Verdonk and colleagues, who reported on long-term results 7 to 10 years after Dejour trochleoplasty of 12 patients. Using the less commonly used Larsen-Lauridsen subjective scale, they showed a 77% good or very good subjective rating. They mentioned that the objective scale ratings were mostly fair and poor and did not seem to correlate with the subjective patient-reported outcomes.21
These studies underline that most patients undergoing trochleoplasty have had previous surgical failures and thus represent a difficult patient population. It is necessary to manage expectations in this patient population. Counseling should include the fact that there is a significant amount of patients that may continue to have some residual pain even though the patellofemoral joint is stable.
The radiographic outcome for osteoarthritis after this procedure has been encouraging. The 14-year follow-up data by von Knoch et al 10 showed that almost 70% of the patients only had grades 0 or 1 osteoarthritis according to the Iwano patellofemoral osteoarthritis classification.6 Of the remaining patients in their study, the majority of the patients (22%) still only had grade 2 osteoarthritis. The relative success of at least preventing severe progression of osteoarthritis has also been documented on follow-up osteochondral biopsy at 6, 8, and 9 months postoperatively.22 The postoperative analysis of the cartilage found viable chondrocytes and normal matrix and cell distribution of the cartilage.22 Remarkable is, that these findings were obtained using the subchondral trochleoplasty indicating that the cartilage actually normally reattaches to the subchondral bone after this procedure.
In a recent systematic review of the literature, Smith and colleagues evaluated a total of 6 publications reporting on radiographic and clinical outcomes after corrective trochleoplasty.9,10,17,18,21,23,24 In this review he pointed out that the overall quality of the literature is poor. However, that with respect to correction of the instability these procedures appear to be very effective as only 1 author described 1 patient with recurrent apprehension.25 His conclusion was that the trochleoplasties appear to be a safe procedure over a mid-term follow-up, however, higher quality studies have to be designed in providing a prospective longitudinal follow-up of patients undergoing this procedure.
Bollier and Fulkerson 26 also reviewed the literature in a systematic review. He came to overall very similar conclusions cautioning the use of trochleoplasty and advising to reserve this procedure only for cases where other pathologies have been corrected.
SUMMARY
It has been accepted at this point that trochlear dysplasia is an important factor to consider in the diagnosis and treatment of patellofemoral malalignment and resulting instability. The trochlear anatomy is 1 factor that plays a role among several other factors that influence patella stability. To date no clear algorithm exists as to when a trochleoplasty is clearly indicated. It is important to understand which aspect of trochlear dysplasia will require surgical correction to choose the appropriate technique. The literature has shown that trochleoplasty can be successful in the short and long term and achieves relatively high satisfaction among patients. However, there is a significant amount of patients that may have residual pain after this procedure. This needs to be addressed when counseling the patient.
The work of Dejour, Biedert, and others has been able to inform us regarding the correct technique for the underlying trochlear deformity. Despite the case series presented by these authors a general guideline as to when to perform and when not to perform a trochleoplasty cannot be given based upon the literature. It appears that in the case of a prominent supratrochlear spur the removal of the spur can be reliably achieved. The further deepening of the groove may be appropriate in a Dejour type C deformity of the femoral trochlea. However, given the fact that in almost all cases additional procedures such as medial soft-tissue reefings, MPFL reconstructions, or associated tibial tubercle transfers are being performed on almost all patients undergoing concomitant trochleoplasty it is difficult to isolate the true value of this procedure. Bollier and Fulkerson 26 pointed out in his recent systematic review that trochleoplasty should be reserved for patients with extreme dysplasia, using it as a salvage operation given the potential pain that the patient may experience at the expense of stability. This recommendation appears sound for the majority of patients with previous surgeries and lengthy histories of unsuccessful treatment. The data that Dejour and colleagues presented on patients undergoing a trochleoplasty as a primary procedure, however, is intriguing and warrants further careful investigation to evaluate the deepening trochleoplasty as a potential primary treatment option.21
In 2012, the recommendation based upon a thorough review of the current literature is that because of its technical difficulty and the need for a thorough understanding of the patellofemoral anatomy trochleoplasty is not a procedure that should be carried out routinely. It has its place in the arsenal of procedures available to orthopedic surgeons who have a special interest and experience in the treatment of patellofemoral instability and malalignment. Trochleoplasties provide a fascinating concept of recreating normal anatomy in the patellofemoral trochlea and deserve further careful investigation in order for this procedure to be utilized to its fullest potential for the benefit of our patients.
Footnotes
Disclosure: The authors declare no conflict of interest.
REFERENCES
- 1.Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114–1121. doi: 10.1177/0363546503260788. SFX Bibliographic Links. [DOI] [PubMed] [Google Scholar]
- 2.Fithian D, Neyret P, Servien E. Patellar instability: the Lyon experience. Tech Knee Surg. 2007;6:112–123. [Google Scholar]
- 3.Dejour H, Walch G, Nove-Josserand L, et al. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. doi: 10.1007/BF01552649. SFX. [DOI] [PubMed] [Google Scholar]
- 4.Malghem J, Maldague B. Depth insufficiency of the proximal trochlear groove on lateral radiographs of the knee: relation to patellar dislocation. Radiology. 1989;170:507–510. doi: 10.1148/radiology.170.2.2911676. SFX Bibliographic Links. [DOI] [PubMed] [Google Scholar]
- 5.Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc Rev. 2007;15:39–46. doi: 10.1097/JSA.0b013e31803035ae. Ovid Full Text. [DOI] [PubMed] [Google Scholar]
- 6.Iwano T, Kurosawa H, Tokuyama H, et al. Roentgenographic and clinical findings of patellofemoral osteoarthrosis. With special reference to its relationship tofemorotibial osteoarthrosis and etiologic factors. Clin Orthop Relat Res. 1990;252:190–197. Ovid Full Text. [PubMed] [Google Scholar]
- 7.Peterson L, Karlsson J, Brittberg M. Patellar instability with recurrent dislocation due to patellofemoral dysplasia. Results after surgical treatment. Bull Hosp Jt Dis Orthop Inst. 1988;48:130–139. SFX Bibliographic Links. [PubMed] [Google Scholar]
- 8.Dejour D, Saggin P. The sulcus deepening trochleoplasty-the Lyon's procedure. Int Orthop. 2010;34:311–316. doi: 10.1007/s00264-009-0933-8. SFX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schottle PB, Fucentese SF, Pfirrmann C, et al. Trochleaplasty for patellar instability due to trochlear dysplasia: a minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthop. 2005;76:693–698. doi: 10.1080/17453670510041781. SFX. [DOI] [PubMed] [Google Scholar]
- 10.von Knoch F, Bohm T, Burgi ML, et al. Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. J Bone Jt Surg Br. 2006;88:1331–1335. doi: 10.1302/0301-620X.88B10.17834. [DOI] [PubMed] [Google Scholar]
- 11.Bereiter H, Gautier E. Die trochleaplastik als chirurgische therapie der rezidivierenden patellaluxation bei trochleadysplasie des femurs [Trochleoplasty as surgical approach for the treatment of recurrent patella instability in patients with trochlear dysplasia of the femur] Arthroskopie. 1994;7:281–286 [German]. [Google Scholar]
- 12.Biedert R, Zaffagnini S, Dejour D, Arendt EA. Patellofemoral Pain, Instability, and Arthritis. Berlin: Springer-Verlag; 2010. Trochlear lengthening osteotomy with or without elevation of the lateral trochlear facet; pp. 209–215. [Google Scholar]
- 13.Biedert R. International Patellofemoral Study Group Meeting. Lausanne, Switzerland: 2005. Measurements of the length of proximal and distal trochlea and the trochleardepth on sagittal MRI in patients with lateral patellar subluxation. [Google Scholar]
- 14.Biedert RM. Patellar instability with increased knee flexion due to lateral femoral condyle distal dysplasia: a report of two cases. Knee. 2012;19:140–143. doi: 10.1016/j.knee.2010.12.003. SFX. [DOI] [PubMed] [Google Scholar]
- 15.Biedert RM, Albrecht S. The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc. 2006;14:707–712. doi: 10.1007/s00167-005-0015-4. SFX. [DOI] [PubMed] [Google Scholar]
- 16.Fucentese SF, Schottle PB, Pfirrmann CW, et al. CT changes after trochleoplasty for symptomatic trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2007;15:168–174. doi: 10.1007/s00167-006-0140-8. SFX. [DOI] [PubMed] [Google Scholar]
- 17.Fucentese SF, Zingg PO, Schmitt J, et al. Classification of trochlear dysplasia as predictor of clinical outcome after trochleoplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19:1655–1661. doi: 10.1007/s00167-011-1410-7. SFX. [DOI] [PubMed] [Google Scholar]
- 18.Donell ST, Joseph G, Hing CB, et al. Modified Dejour trochleoplasty for severe dysplasia: operative technique and early clinical results. Knee. 2006;13:266–273. doi: 10.1016/j.knee.2006.01.004. SFX. [DOI] [PubMed] [Google Scholar]
- 19.Utting MR, Mulford JS, Eldridge JD. A prospective evaluation of trochleoplasty for the treatment of patellofemoral dislocation and instability. J Bone Jt Surg Br. 2008;90:180–185. doi: 10.1302/0301-620X.90B2.20017. [DOI] [PubMed] [Google Scholar]
- 20.Moreel P, Dejour D, Neyret P. Les donnees classiques de la radiographie standard dans la pathologie femoro-patellaire. Journees Lyonnaises de Chirurgie du Genou. 2002:12–16. [Google Scholar]
- 21.Verdonk R, Jansegers E, Stuyts B. Trochleoplasty in dysplastic knee trochlea. Knee Surg Sports Traumatol Arthrosc. 2005;13:529–533. doi: 10.1007/s00167-004-0570-0. SFX. [DOI] [PubMed] [Google Scholar]
- 22.Schottle PB, Schell H, Duda G, et al. Cartilage viability after trochleoplasty. Knee Surg Sports Traumatol Arthrosc. 2007;15:161–167. doi: 10.1007/s00167-006-0148-0. [DOI] [PubMed] [Google Scholar]
- 23.Beals RK, Buehler K. Treatment of patellofemoral instability in childhood with creation of a femoral sulcus. J Pediatr Orthop. 1997;17:516–519. Ovid Full Text Bibliographic Links. [PubMed] [Google Scholar]
- 24.Smith TO, Davies L, Toms AP, et al. The reliability and validity of radiological assessment for patellar instability. A systematic review and meta-analysis. Skelet Radiol. 2011;40:399–414. doi: 10.1007/s00256-010-0961-x. SFX. [DOI] [PubMed] [Google Scholar]
- 25.Smith T, Leigh D. Outcomes following trochleoplasty for patellar instability with trochlear dysplasia: a systematic review. Eur J Orthop Surg Traumatol. 2008;18:425–433. SFX. [Google Scholar]
- 26.Bollier M, Fulkerson JP. The role of trochlear dysplasia in patellofemoral instability. J Am Acad Orthop Surg. 2011;19:8–16. doi: 10.5435/00124635-201101000-00002. SFX. [DOI] [PubMed] [Google Scholar]