Abstract
Introduction
The inspiratory flow pattern influences CO2 elimination by affecting the time the tidal volume remains resident in alveoli. This time is expressed in terms of mean distribution time (MDT), which is the time available for distribution and diffusion of inspired tidal gas within resident alveolar gas. In healthy and sick pigs, abrupt cessation of inspiratory flow (that is, high end-inspiratory flow (EIF)), enhances CO2 elimination. The objective was to test the hypothesis that effects of inspiratory gas delivery pattern on CO2 exchange can be comprehensively described from the effects of MDT and EIF in patients with acute respiratory distress syndrome (ARDS).
Methods
In a medical intensive care unit of a university hospital, ARDS patients were studied during sequences of breaths with varying inspiratory flow patterns. Patients were ventilated with a computer-controlled ventilator allowing single breaths to be modified with respect to durations of inspiratory flow and postinspiratory pause (TP), as well as the shape of the inspiratory flow wave. From the single-breath test for CO2, the volume of CO2 eliminated by each tidal breath was derived.
Results
A long MDT, caused primarily by a long TP, led to importantly enhanced CO2 elimination. So did a high EIF. Effects of MDT and EIF were comprehensively described with a simple equation. Typically, an efficient and a less-efficient pattern of inspiration could result in ± 10% variation of CO2 elimination, and in individuals, up to 35%.
Conclusions
In ARDS, CO2 elimination is importantly enhanced by an inspiratory flow pattern with long MDT and high EIF. An optimal inspiratory pattern allows a reduction of tidal volume and may be part of lung-protective ventilation.
Introduction
Ventilator-induced lung injury is an important problem in the acute respiratory distress syndrome (ARDS). It may be caused by barotrauma related to high airway, alveolar, and transpulmonary pressures or by shear forces at lung collapse and opening during tidal breaths. Among efforts to provide lung-protective ventilation in ARDS, a reduction of tidal volume (VT) is a central issue [1-5]. By using lower than traditional VT, both of the mentioned damaging mechanisms may be mitigated. Recently, Bruhn et al. [6] showed by dynamic CT that cyclic collapse and opening is reduced by lower VT, providing direct evidence that low VT ventilation may be lung protective by reducing this phenomenon. However, the decrease in minute ventilation induced by low VT can be difficult to offset by increasing respiratory rate and may induce hypercapnia. So, adequate CO2 elimination under well-controlled airway pressure and tidal volume (VT) is an important clinical issue, particularly in ARDS.
Accordingly, dead-space reduction plays a role in a rational lung-protection strategy. This suggests an optimal pattern of inspiratory gas delivery [7-10]. Characteristics of this pattern are the time for gas insufflation (TI), the postinspiratory pause time (TP) after TI, and the inspiratory flow wave pattern, denoted SHAPE. SHAPE may be constant: that is, square flow, increasing; or accelerating flow or decreasing that is decelerating flow. TI, TP, and SHAPE affect mean distribution time (MDT), that is, time available for distribution and diffusion of inspired tidal gas with resident alveolar gas [6-8]. The definition of MDT is recapitulated in Figure 1. A longer TP prolongs MDT and enhances CO2 elimination [11]. It reduces dead space in healthy pigs and in pigs with acute lung injury [12]. The positive effects were more closely related to lnMDT than to MDT. In ARDS patients, a long TP reduces dead space and leads to reduced PaCO2, without a clinically significant increase in intrinsic positive end-expiratory pressure (PEEP) or negative hemodynamic effects [7,8]. In one study, the TP was varied, but also the TI and SHAPE. The results indicated that positive effects were related not only to a high value of MDT but also to an abrupt cessation of end-inspiratory flow (EIF) that follows from shortening TI or using an increasing flow pattern [12]. The definition of EIF is explained in Figure 2e.
Figure 1.
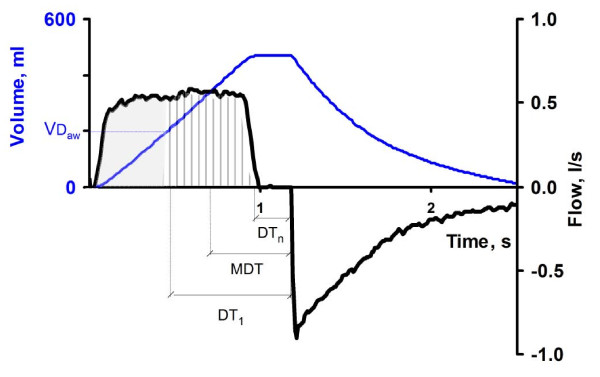
Mean distribution time (MDT). MDT is the mean time during which consecutive fractions of inspired tidal volume remain in the respiratory zone of the lung (that is, the time available for distribution and mixing by diffusion of inspired gas with resident alveolar gas. The graph shows flow (black) and volume change (blue) of a breath against time. Until airway dead space (VDaw) has been inhaled (shaded area), no fresh gas arrives to alveoli, and this volume does not contribute to MDT. The following fractions of inhaled volume, N° 1 to N° n, (vertically striped area) have different distribution times in alveoli. For N° 1 distribution time is marked DT1 and for N° n DTn. MDT is the volume-weighted mean of DT1 to DTn.
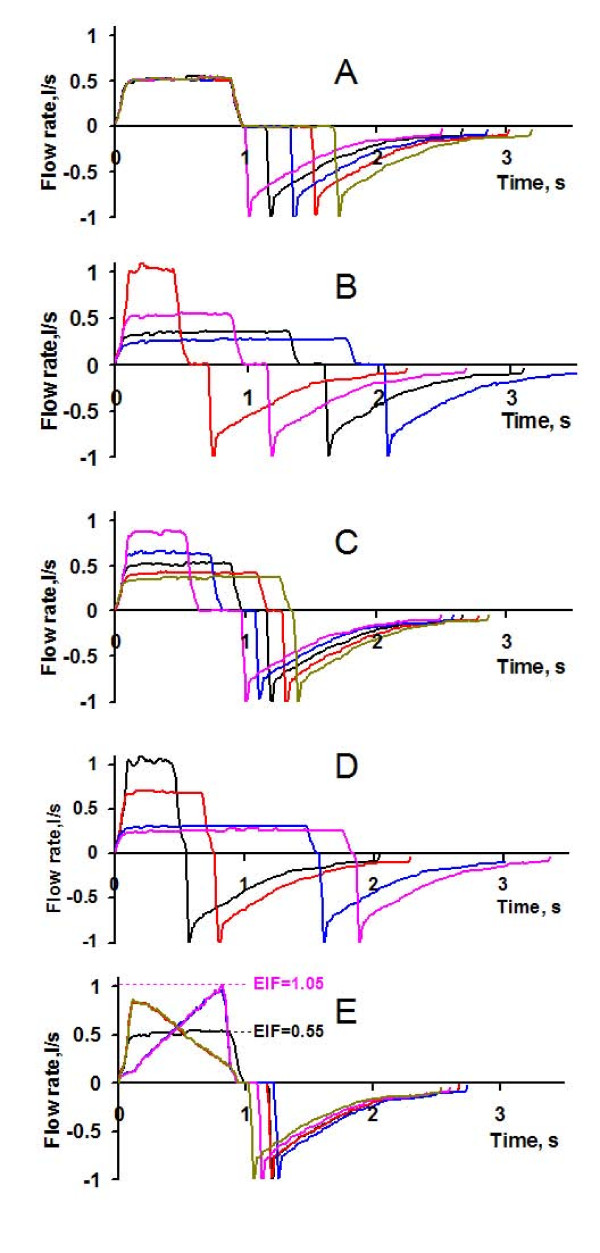
Figure 2.
Flow patterns. Different flow patterns studied, all at similar VT, PEEP, and expiratory time. Inspiratory flow rate is positive. (a) Only TP modified. (b) Only TI modified. (c) TI and TP modified, maintaining constant MDT. (d) TI modified at shortest possible TP (1%). (e) Shape and TP modified. The definition of end-inspiratory flow (EIF) is illustrated for increasing flow and constant flow in (e). For decreasing flow, EIF is zero, because flow rate ceases during inspiration.
No previous study investigated how various combinations of TI, TP, and SHAPE affect CO2 elimination in ARDS patients, and no previous study distinguished between effects of MDT and EIF. The objective of the present study was to test in ARDS patients the hypothesis that the effects of the inspiratory gas-delivery pattern on CO2 exchange can be comprehensively described from effects related to MDT, and also from effects of EIF, and to quantify the influence of these variables.
Materials and methods
Eight mechanically ventilated subjects (Table 1) fulfilled criteria for ARDS [13]. Exclusion criteria were as follows: younger than 18 years, presence of a chest tube, contraindication to sedation or paralysis, intracranial disease, and a PaO2/FIO2 < 75 mm Hg. Sedation and neuromuscular blockade were achieved by continuous infusion of midazolam and atracurium. The Ethics Committee of French Intensive Care Society approved the protocol, which was part of another study looking at different PEEP settings and FIO2 [14]. This is the background behind the values of PEEP and FIO2 in individual patients. Patients' next of kin were informed and gave consent to the study and its publication.
Table 1.
Characteristics of the subjects
| Subject | Age | SAPS II | Cause of ARDS | Underlying disease | Days of ARDS |
|---|---|---|---|---|---|
| 1 | 44 | 28 | Sepsis | Meningitis | 5 |
| 2 | 56 | 58 | Septic shock | Lymphoma | 3 |
| 3 | 68 | 73 | Pneumonia | Thrombotic microangiopathy | 2 |
| 4 | 58 | 64 | Heat stroke | Alcoholism | 0 |
| 5 | 66 | 81 | Septic shock | Aortic valve replacement | 5 |
| 6 | 64 | 76 | Sepsis | Arterial hypertension | 2 |
| 7 | 51 | 44 | Pneumonia | Cirrhosis | 0 |
| 8 | 75 | 73 | Pneumonia | Obliterating artery disease | 2 |
SAPS II, new simplified acute physiology score.
The patients were ventilated at volume control (ServoVentilator 900 C with a mainstream CO2 Analyzer 930; Siemens-Elema, Solna, Sweden). Each patient had an arterial line. For ordinary breaths during basal ventilation, TI was 33%, and TP, 10%. Set PEEP was 5 cm H2O. This low level of PEEP reflects the initial settings of the previous study [14]. The patients were ventilated with an effective VT of about 6 ml/kg ideal body weight [1]. Measured volumes were corrected with respect to gas compression in ventilator tubing. Individual ventilation parameters are given in Table 2.
Table 2.
Ventilation characteristics of the subjects at baseline ventilation before measurements
| Subject |
Effective V
T
(ml/kg IBW) |
Respiratory rate (min-1) | Plateau pressure (cmH2O) | FIO2. |
PaO
2
/F
I
O
2
(mm Hg) |
PaCO
2
(mm Hg) |
|---|---|---|---|---|---|---|
| 1 | 6.5 | 25 | 19 | 0.6 | 145 | 45 |
| 2 | 5.9 | 19 | 29 | 0.6 | 108 | 58 |
| 3 | 5.6 | 21 | 18 | 1.0 | 165 | 36 |
| 4 | 6.0 | 22 | 21 | 0.6 | 115 | 57 |
| 5 | 5.0 | 25 | 30 | 1.0 | 173 | 48 |
| 6 | 5.8 | 24 | 25 | 0.6 | 263 | 39 |
| 7 | 5.6 | 24 | 23 | 1.0 | 209 | 39 |
| 8 | 6.7 | 25 | 26 | 0.6 | 62 | 57 |
IBW, ideal body weight.
The ServoVentilator was controlled by a personal computer that emitted analog signals to the socket for external control of ventilator function [15,16]. By controlling respiratory rate and minute ventilation, the computer instantly controlled inspiratory flow rate and durations of inspiratory flow (TI) and postinspiratory pause (TP), while maintaining constant tidal volume [12].
The computer was programmed to perform six recording sequences, each comprising 12 consecutive breaths. Breaths numbers 3, 6, 9, and 12 were modified. In six different sequences, single breaths were modified with respect to TI (0.4 to 2.0 seconds), TP (0.0 to 0.9 seconds), and inspiratory flow wave form (SHAPE). In total, breaths with 20 different flow patterns were studied (Figure 2). As seen, SHAPE was square (constant flow) or triangular, with increasing or decreasing flow rate. Average values from the four ordinary breaths representing basal ventilation immediately preceding the modified breaths were used as reference for the modified breaths in each recording sequence. VT, PEEP, and expiratory time were constant for all breaths.
Signals representing airway flow and fraction of CO2 at airway opening in percentage (FCO2) were fed to the A/D converter of a personal computer and sampled at 100 Hz [12,16]. Recorded data were transferred to an Excel workbook for analysis (Microsoft Corp., Redmond, WA, USA).
MDT was calculated from the average time that consecutive fractions of inspired gas remained in the respiratory zone, from their arrival in the zone until start of expiration (Figure 1) [7]. Further analysis was based on the single-breath test for CO2, SBT-CO2. SBT-CO2 allows calculation of airway dead space, essentially from the maximal rising slope of the curve, as described in detail by Åström et al. [17]. When PaCO2 is measured in steady state, alveolar dead space also can be determined [18]. Both dead-space fractions are affected by a modified inspiratory flow pattern, but only airway dead space can be studied at transient variations of ventilation. Therefore, in this study, the main studied variables were the volume of CO2 eliminated during a single tidal breath (VTCO2) and particularly the change in VTCO2 (ΔVTCO2) in breaths modified with respect to inspiratory flow pattern (Figure 3). ΔVTCO2 was expressed in percentage of VTCO2 of ordinary breaths in the same recording sequence (ΔVTCO2%). A positive ΔVTCO2 or ΔVTCO2% indicates enhanced CO2 elimination.
Figure 3.
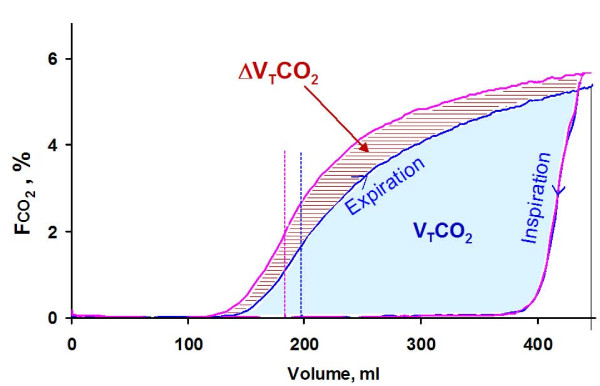
Single-breath test for CO2 at ordinary and long postinspiratory pause in subject 4, depicting fraction of CO2 at airway opening, FCO2, against expired volume. The blue loop shows the SBT-CO2 from an ordinary breath, and the magenta loop, a breath with a prolonged TP. The blue area corresponds to VTCO2 of an ordinary breath. The additional volume of CO2 eliminated at the longer TP, ΔVTCO2, indicated by hatched area, is caused partly by a lower-airway dead space (indicated by interrupted lines) and partly by a higher level of the alveolar plateau.
Protocol
The subjects were studied in supine position when stable with respect to ventilation, blood pressure, heart rhythm, and metabolism, judged from CO2 elimination. If needed, endotracheal suction was performed well before the study and was not repeated during data collection, which lasted about 20 minutes. Each of the six types of recording sequences was in random order, performed twice, but in some patients, only once, when care of the patient was indicated.
Statistical methods
Data are presented as mean ± standard deviation (SD). Regression analysis was used to study variations of volumes of CO2 in relation to parameters describing the inspiratory flow pattern. Significance implies that P < 0.05.
Results
On average, 110 breaths were analyzed per patient, equal numbers of ordinary reference breaths and modified breaths with all combinations of TI, TP, and SHAPE (Figure 2). MDT varied between 0.12 seconds and 1.45 seconds, and EIF between 0 at decreasing flow and up to 1.7 L/sec, at increasing flow.
TP variations: effects of MDT variation on ΔVTCO2%
When TP was increased, VTCO2 increased significantly because of lower-airway dead space and a higher alveolar plateau (Figure 3).
For all breaths in which only TP was modified, the ΔVTCO2% showed, in each patient, a strongly significant positive correlation to lnMDT; Figure 4. Notably, in these breaths, the inspiratory flow pattern was square, and VT, TI, and EIF were constant.
Figure 4.
Effects of TP variation. When only TP was modified, ΔVTCO2% increased with MDT, shown by different colors for each patient. Each dot represents one breath. To illustrate the close correlation between ΔVTCO2% and lnMDT, lines for each subject represent the relation: ΔVTCO2% = m × lnMDT + n.
Combined EIF and MDT variations: effects on ΔVTCO2%
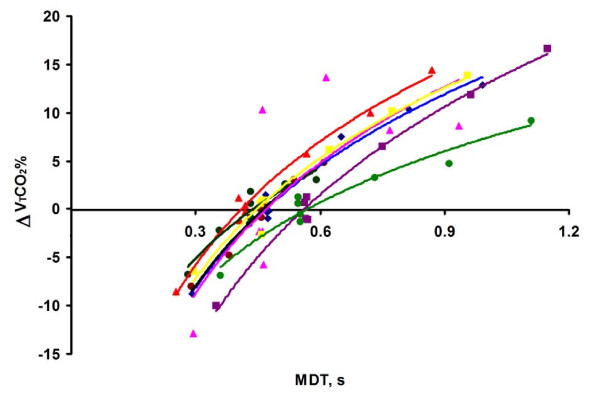
In contrast to breaths modified only with respect to TP, in breaths modified with respect to SHAPE, no correlation was found between ΔVTCO2% and lnMDT. To explore the reason for this finding, all breaths of individual patients were separated into groups with narrow ranges of EIF and analyzed. Groups of breaths with high EIF were at specific values of MDT associated with high ΔVTCO2% (Figure 5). Within each group of breaths with similar EIF, the ΔVTCO2% strongly correlated to lnMDT.
Figure 5.
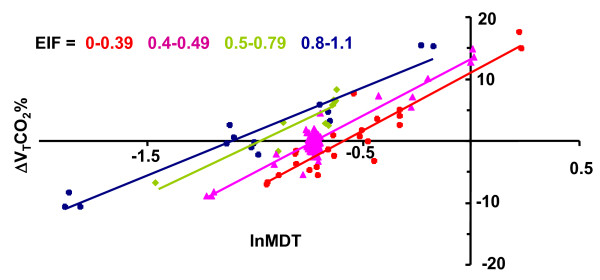
ΔVTCO2% plotted against lnMDT in subject 4. Groups of breaths with EIF within specified ranges are indicated by separate colors. For each range of EIF, a linear relation between lnMDT and ΔVTCO2% was observed.
The ΔVTCO2% was, for all breaths in each subject, correlated to lnMDT and EIF by using the equation:
| (1) |
To translate data of coefficients a, b and c (Table 3) to information more comprehensible from a clinical point of view, the ΔVTCO2% was calculated for different inspiratory flow patterns (Table 4). The calculations were based on mean values among subjects for coefficients a, b and c in Eq. 1 and values for the subject with the highest coefficient b that indicates a strong influence of EIF (subject 4).
Table 3.
| Subject | a | b | c | R2 |
|---|---|---|---|---|
| 1 | 12.9 | 2.3 | 9.0 | 0.71 |
| 2 | 16.4 | 11.5 | 4.8 | 0.76 |
| 3 | 11.7 | 6.4 | 4.6 | 0.59 |
| 4 | 16.7 | 12.8 | 6.4 | 0.84 |
| 5 | 14.5 | 0.4NS | 12.9 | 0.74 |
| 6 | 13.4 | 5.6 | 7.8 | 0.34 |
| 7 | 15.6 | 1.9NS | 11.0 | 0.58 |
| 8 | 10.9 | -2.2NS | 10.4 | 0.40 |
| Mean | 14.0 | 4.8 | 8.4 | 0.62 |
| SD | 2.2 | 5.3 | 3.0 | 0.18 |
NS, not significantly different from zero.
Table 4.
Effects of different inspiratory patterns on EIF, MDT, and lnMDT
| TI 33%, TP 10% | TI 15%, TP 28% | TI 15%, TP 35% | |||||||
|---|---|---|---|---|---|---|---|---|---|
| SHAPE | Increasing flow | Constant flow | Decreasing flow | Increasing flow | Constant flow | Decreasing flow | Increasing flow | Constant flow | Decreasing flow |
| EIF, ml/s | 1,106 | 553 | 0 | 2,433 | 1,217 | 0 | 2,433 | 1,217 | 0 |
| MDT | 0.41 | 0.52 | 0.71 | 0.80 | 0.86 | 0.95 | 0.99 | 1.05 | 1.14 |
| lnMDT | -0.90 | -0.66 | -0.34 | -0.22 | -0.15 | -0.05 | -0.01 | 0.05 | 0.13 |
| ΔVTCO2%, all subjects | 1 | 2 | 4 | 17 | 12 | 8 | 20 | 15 | 10 |
| ΔVTCO2%, subject 4 | 5 | 2 | 1 | 34 | 19 | 6 | 37 | 23 | 9 |
Effects on ΔVTCO2 were calculated by using mean coefficients a and b for all subjects (Eq. 1) and coefficients for subject 4 who had a high coefficient b.
At TI 33% and TP 10%, one observes that for mean a, b and c values, a decreasing flow has a slightly positive ΔVTCO2% (Table 4, left columns). This reflects that, in most patients, the positive effect of a longer MDT outweighs a modest negative effect of an EIF that is zero at decreasing flow. In contrast, in subject 4, increasing flow implying a high EIF enhanced CO2 elimination.
If one would redistribute the total inspiratory time by shortening TI and prolonging TP, the ΔVTCO2% would increase, and much more so at increasing flow because of high EIF at that pattern (Table 4, middle columns). The effect would be very important in subject 4. Further enhancement of CO2 elimination would result from an increase in total inspiratory time from 43% to 50% of the respiratory cycle (Table 4, right columns).
Discussion
The computer-controlled ventilator allowed elaborate modification of inspiratory flow wave pattern on a breath-by-breath basis at constant tidal volume. Within 20 minutes of study time, about 20 types of modified breaths were studied. The ΔVTCO2% expresses how an alternative inspiratory pattern affects VTCO2 relative to ordinary breaths in the same recording sequence. Thereby, changes in CO2 exchange due to variable physiological conditions between patients and in a single patient with time were minimized. With this technique and focusing on ΔVTCO2, we could for the first time comprehensively describe and distinguish effects of MDT and EIF in ARDS patients.
The most uncomplicated breath modification is when only TP was modified, as this does not affect EIF. The findings confirm that the ΔVTCO2% is significantly affected by the length of the pause and tightly positively correlated to lnMDT [7,12]. A comprehensive analysis of variation in TI, TP, and SHAPE has previously not been performed in patients. Such analysis showed that both MDT and EIF influence the VTCO2 and that the effects can be described with the simple equation:
| (2) |
At decreasing flow, more inhaled gas reaches alveoli early during inspiration. Thereby, MDT is prolonged. This will tend to enhance CO2 exchange. However, EIF and MDT are negatively correlated to one another for breaths varied with respect to SHAPE. For example, for breaths with decreasing flow, MDT is long, but EIF is zero. This implies that EIF will balance and obscure effects of MDT; in agreement with that, no correlation between ΔVTCO2% and MDT was found among breaths with varying SHAPE.
Gas transfer over the boundary zone between fresh inhaled gas and resident alveolar gas and gas mixing within the alveolar zone are complex phenomena. Diffusion is a strictly time-dependent phenomenon and is believed to be the main phenomenon behind effects of MDT in ARDS. Diffusion drives gas transfer through the whole respiratory zone between capillary blood and conducting airways. In 1970, Knelson et al. [12] reported that a postinspiratory pause led to a more efficient alveolar gas exchange. They showed theoretically that this is due not only to improved distribution of ventilation but also to alveolar perfusion during the pause during which alveolar CO2 tension approaches that of mixed venous blood. Fletcher et al. [19] further developed this concept. Aboab et al. [14] reasoned that a higher level of the alveolar plateau associated with a long pause might partly be due to continuing delivery of CO2 by alveolar perfusion. In their study, a detailed analysis of breaths with similar MDT but variable distribution between TI and TP led to the suggestion that time for alveolar perfusion during inspiration is of low importance compared with time for distribution and diffusion within the alveolar zone, as expressed by MDT. Still, delivery of CO2 to alveoli during TI and TP may to some extent contribute to positive effects of decreasing flow and a long TP.
In a theoretic study, Jansson and Jonson [20] showed that a decreasing flow in combination with postinspiratory pause is favorable with respect to an even distribution of ventilation in the presence of uneven airway obstruction, a phenomenon associated with so-called pendelluft. They also postulated a small opposite effect in lungs with uneven compliance. In ARDS, effects on gas distribution to different lung regions are complex. Nevertheless, the influence of the inspiratory pattern is thought to relate more closely to diffusion within lung units than to distribution of ventilation between lung units.
Effects of EIF may reflect that high-frequency flow and pressure transients at airway opening are transmitted through the airways to the periphery of the lungs. This is the basis behind impulse oscillometry used for diagnostic purposes [21,22]. In mechanical ventilation, it also is important for high-frequency oscillation [23]. Sudden interruption of flow at the end of inspiration, as expressed by EIF, implies that oscillations covering a broad spectrum of frequencies are transmitted through the airways down to the alveolar zone. Such oscillations serve to mix gas in the boundary zone between conducting airways and alveoli. This is the conceivable mechanism for the observed positive effect of a high EIF on CO2 exchange.
The effect of the MDT on the ΔVTCO2% was similar among subjects (Figure 4, Table 3). In contrast, the effect of EIF varied importantly among subjects, as shown by large variation in coefficient b. The basis behind impulse oscillometry is that transmission of flow oscillations through the airways reflects differences in distributed resistance, compliance, and inertia along the airways. As lung mechanics is complexly perturbed in ARDS, the finding that EIF is of variable importance among patients could be expected.
In the present study, CO2 exchange was studied only for single modified breaths at a time. It has been shown that a change in VTCO2 measured with the present technique will be followed by a corresponding change in PaCO2 in the opposite direction [8,10,12,24]. At constant respiratory rate, an observed change in VTCO2 after a change in tidal volume or inspiratory flow pattern will affect PaCO2 in animals and in humans, in health and in disease. The layout of this study, based on studies of single breaths, has the strength of making it possible to study a large spectrum of inspiration and pause patterns within a short period, during which the physiological status of the patient remains essentially stable. Conversely, further studies are indicated in which particular patterns of inspiration are studied in steady state to evaluate effects on arterial blood gases, physiological dead space, and other parameters.
The results show that it is possible to enhance CO2 elimination by about 12% to 15% just by modifying TI and TP at constant VT in most ARDS patients and to about 20% in some patients (Table 4). At long TP, further enhancement is possible by using increasing inspiratory flow. On modification of TI and TP leading to a higher I:E ratio, we could until now only partly understand clinical observations of immediate very important increments in CO2 elimination observed on the 930 CO2 Analyzer, followed by corresponding decrease in PaCO2 after a switch to a more efficient pattern of inspiration. On the basis of the present results, an I:E ratio of 1:1 with a long TP seems appropriate.
In most ARDS patients, it is more important to reduce VT than to enhance CO2 elimination. This would be the case in the present material in which hypercapnia was not a problem. Hypercapnia may have a lung-protective effect in itself. Such effects are not proven to improve outcome in ARDS [25]. However, hypercapnia combined with an efficient pattern of inspiration will allow particularly low tidal volumes, which may enhance lung protection. A combination of methods and approaches is needed for optimal reduction of dead space. Jonson et al. [26] showed that expiratory flushing of airways, later denoted tracheal gas injection [27], may be used to clear the airways from CO2 down to trachea. To avoid potential problems of humidification of injected gas and of jet streams in the trachea, aspiration of dead space (ASPIDS) was developed and tested in animals and patients [28,29]. With ASPIDS, dead-space gas is aspirated during late expiration through a catheter at the tip of the tracheal tube and simultaneously replaced by an equally large flow of fresh gas through the ordinary inspiratory pathway, avoiding all other influences on ventilation. In a porcine ARDS model, one can, with a combination of ASPIDS and the MDT concept, achieve normocapnia at very low VT ventilation, as shown by Uttman et al. [10]. Despite the high metabolic rate in adolescent pigs, VT was 4 ml/kg body weight. Notably, this very low VT was achieved at respiratory rates of about 80 breaths/min. At high respiratory rates, MDT becomes shorter. Then, it is particularly important to choose a ventilation pattern that is optimal with respect to CO2 exchange, which is a short TI, a long TP, combined with a short expiratory phase. This may augment intrinsic PEEP, an effect that should be balanced by a reduction of set PEEP. The study of Uttman et al. [10] illustrates that a reduced dead space paves the way for a higher respiratory rate. Theoretically, at dead space approaching zero, VT could be reduced toward zero at very high respiratory rates.
Right-to-left intrapulmonary shunt contributes to alveolar dead space. As recently shown, this contribution increases at high metabolic rate, low cardiac output, low hemoglobin concentration, metabolic acidosis, and respiratory alkalosis [30]. Accordingly, conventional critical care measures aiming at homeostasis have the advantage of dead-space reduction. By addressing all meansfor dead-space reduction, in combination with much higher respiratory rates and much lower tidal volume than conventionally applied, adequate CO2 elimination may be achieved in ARDS patients. Eventually one may reduce the use of extracorporeal gas exchange. The field for research remains wide open
Conclusions
CO2 exchange at different inspiratory patterns can be described according to a simple equation based on MDT and EIF. Just by setting the ventilator to a pattern that enhances CO2 exchange, one may reduce dead space and significantly increase CO2 elimination or alternatively reduce VT. This option merits use in clinical routine and, particularly, in further studies of optimal ventilation in ARDS.
Key messages
• In ARDS, CO2 exchange is importantly affected by the inspiratory flow wave pattern.
• Mean distribution time (MDT) and end-inspiratory flow (EIF) influence of CO2 exchange, as expressed with a simple equation.
• The effect of MDT is similar among ARDS patients, whereas that of EIF is variable.
• A short insufflation followed by a long postinspiratory pause enhances CO2 exchange.
• An efficient pattern of insufflation may be lung protective by allowing a lower tidal volume.
Abbreviations
ARDS: acute respiratory distress syndrome; EIF: end-inspiratory flow; FCO2: fraction of CO2 at airway opening; FIO2: fractional inspired oxygen; IBW: ideal body weight; MDT: mean distribution time; PaCO2: arterial carbon dioxide tension; PaO2: arterial oxygen tension; PEEP: positive end-expiratory pressure; SAPS II: new simplified acute physiology score; SBT-CO2: single-breath test for CO2; TI: insufflation time; TP: postinspiratory pause time; VT: tidal volume; VTCO2: eliminated volume of CO2 per breath; ΔVTCO2%: change in VTCO2 in percentage of the value of ordinary breaths.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
BJ, LB, JA, and LU participated in study design. JA and BJ performed data collection. LN made computer programs and performed primary data analysis. All authors participated in manuscript preparation and read and approved the final manuscript.
Contributor Information
Jerome Aboab, Email: Jerome.Aboab@rpc.aphp.fr.
Lisbet Niklason, Email: Lisbet.Nicklason@med.lu.se.
Leif Uttman, Email: Leif.Uttman@med.lu.se.
Laurent Brochard, Email: Laurent.Brochard@hcuge.ch.
Björn Jonson, Email: bjorn.jonson@med.lu.se.
Acknowledgements
This study was supported by INSERM U651 and the Swedish Heart Lung Foundation.
References
- ARDS Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome: The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;16:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;16:347–354. doi: 10.1056/NEJM199802053380602. [DOI] [PubMed] [Google Scholar]
- Brochard L, Roudot-Thoraval F, Roupie E, Delclaux C, Chastre J, Fernandez-Mondejar E, Clementi E, Mancebo J, Factor P, Matamis D, Ranieri M, Blanch L, Rodi G, Mentec H, Dreyfuss D, Ferrer M, Brun-Buisson C, Tobin M, Lemaire F. Tidal volume reduction for prevention of ventilator-induced lung injury in acute respiratory distress syndrome: The Multicenter Trail Group on Tidal Volume reduction in ARDS. Am J Respir Crit Care Med. 1998;16:1831–1838. doi: 10.1164/ajrccm.158.6.9801044. [DOI] [PubMed] [Google Scholar]
- Brower RG, Shanholtz CB, Fessler HE, Shade DM, White P Jr, Wiener CM, Teeter JG, Dodd-o JM, Almog Y, Piantadosi S. Prospective, randomized, controlled clinical trial comparing traditional versus reduced tidal volume ventilation in acute respiratory distress syndrome patients. Crit Care Med. 1999;16:1492–1498. doi: 10.1097/00003246-199908000-00015. [DOI] [PubMed] [Google Scholar]
- Stewart TE, Meade MO, Cook DJ, Granton JT, Hodder RV, Lapinsky SE, Mazer CD, McLean RF, Rogovein TS, Schouten BD, Todd TR, Slutsky AS. Evaluation of a ventilation strategy to prevent barotrauma in patients at high risk for acute respiratory distress syndrome: Pressure- and Volume-Limited Ventilation Strategy Group. N Engl J Med. 1998;16:355–361. doi: 10.1056/NEJM199802053380603. [DOI] [PubMed] [Google Scholar]
- Bruhn A, Bugedo D, Riquelme F, Varas J, Retamal J, Besa C, Cabrera C, Bugedo G. Tidal volume is a major determinant of cyclic recruitment-derecruitment in acute respiratory distress syndrome. Minerva Anestesiol. 2011;16:418–426. [PubMed] [Google Scholar]
- Aboab J, Niklason L, Uttman L, Kouatchet A, Brochard L, Jonson B. CO2 elimination at varying inspiratory pause in acute lung injury. Clin Physiol Funct Imaging. 2007;16:2–6. doi: 10.1111/j.1475-097X.2007.00699.x. [DOI] [PubMed] [Google Scholar]
- Devaquet J, Jonson B, Niklason L, Si Larbi AG, Uttman L, Aboab J, Brochard L. Effects of inspiratory pause on CO2 elimination and arterial PCO2 in acute lung injury. J Appl Physiol. 2008;16:1944–1949. doi: 10.1152/japplphysiol.90682.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uttman L, Jonson B. A prolonged postinspiratory pause enhances CO2 elimination by reducing airway dead space. Clin Physiol Funct Imaging. 2003;16:252–256. doi: 10.1046/j.1475-097X.2003.00498.x. [DOI] [PubMed] [Google Scholar]
- Uttman L, Ögren H, Niklason L, Drefeldt B, Jonson B. Computer simulation allows goal-oriented mechanical ventilation in acute respiratory distress syndrome. Crit Care. 2007;16:R36. doi: 10.1186/cc5719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knelson JH, Howatt WF, DeMuth GR. Effect of respiratory pattern on alveolar gas exchange. J Appl Physiol. 1970;16:328–331. doi: 10.1152/jappl.1970.29.3.328. [DOI] [PubMed] [Google Scholar]
- Åström E, Uttman L, Niklason L, Aboab J, Brochard L, Jonson B. Pattern of inspiratory gas delivery affects CO2 elimination in health and after acute lung injury. Intensive Care Med. 2008;16:377–384. doi: 10.1007/s00134-007-0840-7. [DOI] [PubMed] [Google Scholar]
- Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R. The American-European Consensus Conference on ARDS: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;16:818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- Aboab J, Jonson B, Kouatchet A, Taille S, Niklason L, Brochard L. Effect of inspired oxygen fraction on alveolar derecruitment in acute respiratory distress syndrome. Intensive Care Med. 2006;16:1979–1986. doi: 10.1007/s00134-006-0382-4. [DOI] [PubMed] [Google Scholar]
- Servillo G, Svantesson C, Beydon L, Roupie E, Brochard L, Lemaire F, Jonson B. Pressure-volume curves in acute respiratory failure: automated low flow inflation versus occlusion. Am J Respir Crit Care Med. 1997;16:1629–1636. doi: 10.1164/ajrccm.155.5.9154868. [DOI] [PubMed] [Google Scholar]
- Svantesson C, Drefeldt B, Sigurdsson S, Larsson A, Brochard L, Jonson B. A single computer-controlled mechanical insufflation allows determination of the pressure-volume relationship of the respiratory system. J Clin Monit Comput. 1999;16:9–16. doi: 10.1023/A:1009916905078. [DOI] [PubMed] [Google Scholar]
- Åström E, Niklason L, Drefeldt B, Bajc M, Jonson B. Partitioning of dead space: a method and reference values in the awake human. Eur Respir J. 2000;16:659–664. doi: 10.1034/j.1399-3003.2000.16d16.x. [DOI] [PubMed] [Google Scholar]
- Beydon L, Uttman L, Rawal R, Jonson B. Effects of positive end-expiratory pressure on dead space and its partitions in acute lung injury. Intensive Care Med. 2002;16:1239–1245. doi: 10.1007/s00134-002-1419-y. [DOI] [PubMed] [Google Scholar]
- Fletcher R, Jonson B, Cumming G, Brew J. The concept of deadspace with special reference to the single breath test for carbon dioxide. Br J Anaesth. 1981;16:77–88. doi: 10.1093/bja/53.1.77. [DOI] [PubMed] [Google Scholar]
- Jansson L, Jonson B. A theoretical study on flow patterns of ventilators. Scand J Respir Dis. 1972;16:237–246. [PubMed] [Google Scholar]
- Dubois AB, Brody AW, Lewis DH, Burgess BF Jr. Oscillation mechanics of lungs and chest in man. J Appl Physiol. 1956;16:587–594. doi: 10.1152/jappl.1956.8.6.587. [DOI] [PubMed] [Google Scholar]
- Hellinckx J, Cauberghs M, De Boeck K, Demedts M. Evaluation of impulse oscillation system: comparison with forced oscillation technique and body plethysmography. Eur Respir J. 2001;16:564–570. doi: 10.1183/09031936.01.00046401. [DOI] [PubMed] [Google Scholar]
- Bohn DJ, Miyasaka K, Marchak BE, Thompson WK, Froese AB, Bryan AC. Ventilation by high-frequency oscillation. J Appl Physiol. 1980;16:710–716. doi: 10.1152/jappl.1980.48.4.710. [DOI] [PubMed] [Google Scholar]
- Taskar V, John J, Larsson A, Wetterberg T, Jonson B. Dynamics of carbon dioxide elimination following ventilator resetting. Chest. 1995;16:196–202. doi: 10.1378/chest.108.1.196. [DOI] [PubMed] [Google Scholar]
- Laffey JG, O'Croinin D, McLoughlin P, Kavanagh BP. Permissive hypercapnia: role in protective lung ventilatory strategies. Intensive Care Med. 2004;16:347–356. doi: 10.1007/s00134-003-2051-1. [DOI] [PubMed] [Google Scholar]
- Jonson B, Similowski T, Levy P, Viires N, Pariente R. Expiratory flushing of airways: a method to reduce deadspace ventilation. Eur Respir J. 1990;16:1202–1205. [PubMed] [Google Scholar]
- Burke WC, Nahum A, Ravenscraft SA, Nakos G, Adams AB, Marcy TW, Marini JJ. Modes of tracheal gas insufflation: comparison of continuous and phase-specific gas injection in normal dogs. Am Rev Respir Dis. 1993;16:562–568. doi: 10.1164/ajrccm/148.3.562. [DOI] [PubMed] [Google Scholar]
- De Robertis E, Sigurdsson SE, Drefeldt B, Jonson B. Aspiration of airway dead space: a new method to enhance CO2 elimination. Am J Respir Crit Care Med. 1999;16:728–732. doi: 10.1164/ajrccm.159.3.9712140. [DOI] [PubMed] [Google Scholar]
- De Robertis E, Servillo G, Tufano R, Jonson B. Aspiration of dead space allows isocapnic low tidal volume ventilation in acute lung injury: relationships to gas exchange and mechanics. Intensive Care Med. 2001;16:1496–1503. doi: 10.1007/s001340101046. [DOI] [PubMed] [Google Scholar]
- Niklason L, Eckerström J, Jonson B. The influence of venous admixture on alveolar dead space and carbon dioxide exchange in acute respiratory distress syndrome: computer modelling. Crit Care. 2008;16:R53. doi: 10.1186/cc6872. [DOI] [PMC free article] [PubMed] [Google Scholar]