Abstract
Low positive and high negative affect predict low rates of smoking abstinence among smokers making a quit attempt. Positive Psychotherapy can both increase positive affect and decrease negative affect and therefore may be a useful adjunct to behavioral smoking counseling. The purpose of the present study was to assess the feasibility and acceptability of a Positive Psychotherapy for Smoking Cessation (PPT-S) intervention that integrates standard smoking cessation counseling with nicotine patch and a package of positive psychology interventions. We delivered PPT-S to 19 smokers who were low in positive affect at baseline. Rates of session attendance and satisfaction with treatment were high, and most participants reported using and benefiting from the positive psychology interventions. Almost one-third of participants (31.6%) sustained smoking abstinence for 6 months after their quit date. Future studies to assess the relative efficacy of PPT-S compared to standard smoking cessation treatment are warranted.
Keywords: smoking, smoking cessation, positive psychotherapy, behavioral treatment, positive affect, depressive symptoms
Depressive symptoms and mood disturbance during and after smoking cessation attempts predict poor smoking outcomes (Berlin & Covey, 2006; Burgess et al., 2002; Covey, Glassman, & Stetner, 1990; Ginsberg, Hall, Reus, & Munoz, 1995; Kinnunen, Dohert, Militello, & Garvey, 1996; West, Hajek & Belcher, 1989), and smoking cessation treatments that incorporate components that target mood have generated considerable interest. For the subgroup of smokers with a history of multiple depressive episodes, smoking cessation treatments that incorporate cognitive-behavioral therapy for depression (CBT-D) or mood management skills that target depressogenic behaviors and cognitions are efficacious in enhancing quit smoking rates (Brown et al., 2001; Haas, Munoz, Humfleet, Reus & Hall, 2004). However, these approaches have not shown efficacy for individuals without a history of recurrent depressive episodes, are not differentially effective for smokers with elevated depressive symptoms, and do not reduce negative moods compared to standard smoking treatment (Brown et al., 2001; Brown et al., 2007). In fact, CBT-D/mood management for smoking cessation may increase negative moods and depressive symptoms relative to standard treatment (Kahler et al., 2002; Schueller et al., in press), perhaps by attuning participants to the likelihood of negative moods during smoking cessation. Thus, the investigation of alternate interventions to address mood during smoking cessation is warranted.
Mood entails dimensions of positive and negative affect (Watson & Tellegen, 1985), which are psychometrically distinct (Watson & Clark, 1997), associate with different neural underpinnings (Davidson, Ekman, Saron, Senulis, & Friesen, 1990), and have unique psychosocial correlates (Watson & Clark, 1997). Although the role of positive affect in smoking cessation has received less attention than negative affect, positive affect and related traits, such as anhedonia, are indeed important predictors of smoking cessation success above and beyond the effects of negative affect (Cook, Spring, McChargue, & Doran, 2010; Leventhal, Ramsey, Brown, LaChance & Kahler, 2008; Zvolensky, Stewart, Vujanovic, Gavric, & Steeves, 2009). Additionally, positive affect has been found to decrease in the weeks prior to quitting and greater reductions in positive affect on quit day are associated with greater risk of smoking lapse (Strong et al., 2009; Strong et al., 2011). Finally, a recent study found that greater positive affect at the start of an internet-based smoking cessation treatment predicted better smoking cessation outcome (Branstrom, Penilla, Perez-Stable, & Munoz, 2010). Furthermore, among smokers with low baseline levels of positive affect, treatment incorporating mood management resulted in better quit smoking outcomes than a comparison condition (Branstrom et al., 2010).
Given the importance of positive affect to smoking cessation outcome, behavioral smoking cessation interventions that either increase positive affect or prevent it from decreasing may be valuable. Behavioral activation (BA), which focuses on improving moods by increased contact with positive reinforcement, is one potential method to address both positive and negative affect. In a pilot study that compared standard smoking treatment with nicotine patch to standard treatment plus BA in smokers with elevated depressive symptoms, BA resulted in higher smoking abstinence rates than the control intervention over a 26-week follow up period (MacPherson et al., 2010). Moreover, BA, compared to control, was associated with significantly lower depressive symptoms during follow-up; however, no effect on positive affect was demonstrated.
An alternative means of addressing moods in smoking cessation treatment is to incorporate interventions developed in positive psychology. Positive psychology interventions attempt to enhance positive feelings, behaviors, or cognitions, and a meta-analysis of these interventions indicates that they both enhance well-being (r = .29) and decrease depressive symptoms (r = .31), especially when delivered individually to participants with evidence of depression, and when intervention extends for greater than 4 weeks (Sin & Lyubomirsky, 2009). These interventions may be particularly effective when combined in a single protocol, as has been done with Positive Psychotherapy (PPT; Seligman et al., 2006). The demonstrated ability of PPT to reduce depressive symptoms and increase positive affect and subjective happiness suggests that PPT may serve as a useful enhancement to traditional behavioral smoking cessation counseling. We know of no studies to date that have tested such an approach. There are, however, multiple potential challenges to integrating PPT into smoking cessation treatment including: (a) that PPT exercises must be clearly linked to smoking cessation so that they are not seen as tangential to the quitting process, (b) that there are significant time constraints in a combined intervention that has to incorporate both PPT and standard behavioral smoking counseling, and (c) that participants' motivation to learn and practice new PPT-related exercises may wane as they progress further past their initial quit smoking date.
The purposes of the present study were (a) to develop and refine a manualized intervention for smoking cessation that incorporates empirically-supported positive psychotherapy exercises, called Positive Psychotherapy for Smoking Cessation (PPT-S), and (b) to test its feasibility and utility in smokers selected for low positive affect who were seeking cessation treatment. We describe the iterative treatment development and refinement process and present empirical data on patient attendance and satisfaction with treatment. In this process, we sought to develop a manual that clinicians agreed was easy to deliver and with which participants reported high satisfaction. After describing the manual development, we present clinical outcomes including smoking abstinence, positive and negative moods, and depressive symptoms before, during, and after the quit attempt. We did not include a comparison group at this stage of treatment development because we could not run a randomized control trial in which the PPT-S manual would change during the trial. Therefore, we discuss clinical outcomes against related studies in the field to gauge whether PPT-S may be promising.
Method
Participants
Participants were 19 smokers from the community who wanted help quitting smoking, and who reported low positive affect. To be included, participants had to (1) be at least 18 years of age; (2) smoke at least 10 cigarettes per day for longer than one year with no other ongoing tobacco product use; (3) be willing to use the transdermal nicotine patch; (4) score at or below an average item score of 2.5 on the positive affect subscale of the Center for Epidemiological Studies – Depression Scale (CES-D; Radloff, 1977) administered during a telephone screen (i.e., feeling happy less than “most of the time); and (5) report at least a 5 on a 0 to 10 scale rating the importance of quitting smoking (where 10 = extremely important). Participants were excluded if they (1) were currently experiencing psychotic symptoms, affective disorder (major depression or mania), or substance use disorder other than nicotine dependence; (2) were taking prescribed psychotropic medication or receiving other forms of psychotherapy; (3) were concomitantly using other pharmacotherapies for smoking cessation; (4) had any contraindications for use of the transdermal nicotine patch.
From February 2011 through November 2011, participants were recruited through advertisements on newspaper, radio, television, Facebook, Craigslist, public transportation, and other community bulletin boards and community events. Potential participants were screened by telephone before completing a baseline interview, at which point they completed an informed consent approved by the Brown University Institutional Review Board. Of the 103 screened, 27 did not meet preliminary inclusion/exclusion criteria, 22 met screening criteria but did not show up for baseline, and 20 declined to participate in the study after telephone screen. Of the 34 baseline assessments completed, 14 were deemed ineligible to participate. One additional individual dropped out prior to receiving any treatment materials, was not followed further, and is not included in outcome analyses. Therefore, results are based on 19 participants entering treatment rather than a potential intention-to-treat sample of 20.
Design and Procedure
All participants received individual PPT-S in an uncontrolled pre-post design. Participants also received 8 weeks of transdermal nicotine patch, consistent with the federal guidelines for smoking cessation treatment (Fiore et al, 2008). We used an iterative process in which PPT-S was modified successively as we gathered experience in implementing the intervention. The positive psychology interventions in PPT-S were adapted from the original PPT manual (Parks & Seligman, 2007), which used an 8-session group treatment to enhance positive emotions. Prior studies have found that increasing the number of smoking cessation counseling sessions from 1 to 4–8 sessions significantly increases long-term abstinence rates, but that abstinence rates appear to plateau at 6 to 7 sessions (Fiore et al, 2008). We decided to limit treatment to 6 individual counseling sessions to maximize the potential for future dissemination.
The target quit smoking date occurred at the third PPT-S session, allowing two weeks before quit date to practice the initial PPT exercises. To allow tapering off of counseling as participants progressed in their quit attempt, the sixth and final session occurred two weeks after the fifth session; thus, counseling was provided for 4 weeks after participants initiated their quit attempt. Sessions ranged in length from 60 minutes for Session 1 to 30–45 minutes for Sessions 2–6. Exercises designed to boost positive mood were introduced throughout PPT-S, and in the final session, participants reviewed all of the PPT exercises they engaged in to identify which were most helpful and which they would like to continue to do after treatment. Participants completed brief assessments at each treatment session, and follow-ups were conducted 8, 16, and 26 weeks after participants' quit smoking date.
Measures
At baseline, severity of nicotine dependence was assessed using the FTND (Heatherton et al. 1991), a well-validated measure with scores ranging from 0–10. Diagnostic exclusions and lifetime prevalence of key Axis I diagnoses was determined by the SCID-Non-Patient (First, Spitzer, Gibbons, & Williams, 1995). Adequate reliability of the Axis I SCID has been demonstrated (Spitzer, Williams, Gibbon, First, 1989).
Depressive symptoms were assessed at baseline, at treatment sessions (S1-S6), and at each follow-up (weeks 8, 16, and 26) using the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). The CES-D is a 20-item scale that is commonly used to screen for symptoms of depression in the community by asking participants to describe their mood during the past week.
Positive affect (PA) and negative affect (NA) were measured using the Positive and Negative Affect Schedule (PANAS: Watson, Clark, & Tellegen, 1988). Both PA and NA subscales consist of 10-items (e.g., PA: alert, enthusiastic, excited; NA: afraid, irritable, upset), designed to capture the broad and general dimensions of positive and negative emotional experiences (Watson & Clark, 1994; p. 1). The PANAS was administered at baseline, at treatment sessions (S1–S6) and at each follow-up (weeks 8, 16, and 26).
Smoking status
Seven-day point prevalence smoking abstinence (i.e., reported abstinence of at least 7 days prior to the assessment day) was assessed 8, 16, and 26 weeks after each participant's quit date. Self-reported abstinence was verified at all assessments by alveolar carbon monoxide (CO) using a Bedfont Scientific Smokelyzer® breath CO monitor, with a CO ≤ 10 ppm confirming abstinence, and at 16 and 26 weeks with saliva cotinine radioimmune assay analysis, with cotinine ≤ 15 ng/ml confirming abstinence (SRNT Subcommittee on Biochemical Verification, 2002).
General satisfaction with treatment was assessed at the 8-week follow-up with the Client Satisfaction Questionnaire (CSQ-8; Larsen et al., 1979). The CSQ contains 8 items (e.g., “How would you rate the quality of the counseling your received;” “To what extent has our program met your needs?”) rated with 4-point response scales where 0 reflects very low satisfaction and 3 reflects very high satisfaction (Cronbach's alpha= .75).
A Treatment Component Evaluation was administered at the 8-week follow-up to assess participants' appraisal of the utility of each exercise they completed. Responses were on a 0 = `not at all' to 4 = `extremely useful' Likert-type scale. Participants also completed a Quitting Strategies Questionnaire which assessed how often they used strategies taught in PPT-S such as using the nicotine patch each day and expressing gratitude to others. Responses were measured on a 1 = `strongly disagree' to 5= `strongly agree' Likert-type scale. Finally, participants were asked the degree to which they enjoyed the positive focus of the treatment using the same response scale.
Data Analysis Plan
We present means and percentages for sessions attended, satisfaction with treatment, use and evaluation of treatment components, smoking cessation outcomes, and mood-related outcomes. For the evaluation of the treatment components, we included only those participants who were exposed to each exercise evaluated and who completed the 8-week follow-up (n = 13). Because of the small sample size and the lack of a comparison group, we did not conduct inferential statistics. In the discussion, we compare our results to those from other clinical trials to provide a context in which to understanding our findings.
Treatment providers
One male and four female counselors, all of whom had doctoral-level training in clinical psychology, provided treatment. Each counselor audiotaped sessions and used detailed manuals to ensure standardization of treatment delivery.
Process of iterative manual development
Using the original group-based PPT manual as a framework (Seligman & Parks, 2007), the PPT-S manual was developed in an iterative fashion guided by participant response and counselor feedback. Counselors met weekly to review every session delivered in the past week. These meetings identified issues that arose in delivering the treatment content (e.g., timing of session components, framing of the PPT exercises and their relation to smoking cessation) and participant reactions to each exercise (e.g., understanding, compliance, and perceived utility). When participants struggled in understanding or implementing a given exercise or found that the exercise was not helpful, we examined these concerns in light of that participant's experience with other components of PPT-S and the experience of other participants in the trial. When there was a consensus among counselors that a given exercise should be modified, we proceeded by either (a) changing the timing of when the exercise was introduced, (b) modifying the content of the exercise, or (c) dropping that exercise from the manual. The primary considerations in evaluating the positive emotion focused interventions were the ease and extent to which participants reported carrying out the exercise and the extent to which participants described the exercises as useful for their quit smoking efforts. Our intention was to adapt the manual rapidly as soon as issues were identified and there was consensus among investigators as to the modifications that would address concerns. In total, we made eight substantive revisions to the treatment manual over the 11 months that the trial was conducted. The final components of the intervention and their timing are shown in Table 1.
Table 1.
Smoking cessation and PPT treatment components by session
| Session # | Smoking Cessation Components | PPT Components |
|---|---|---|
| 1 | Reasons for quitting | Positive Introductions |
| Smoking as physical addiction and habit | Smoking and positive moods | |
| Identifying high-risk situations | 3 Good Things | |
|
| ||
| 2 | Proper use of the nicotine patch | 3 Good Things |
| Planning for high-risk situations | Gratitude Visit | |
| Social support for quitting | Signature strengths in quitting smoking | |
| Preparing for quit date | ||
|
| ||
| 3 (quit date) | Quit date review | 3 Good Things |
| Starting nicotine patch | Savoring | |
| Planning for high-risk situations | Signature strengths in quitting smoking | |
|
| ||
| 4 | Managing smoking `slips' | 3 Good Things |
| Nicotine patch review | Active/Constructive Responding | |
| Planning for high-risk situations | Signature strengths in quitting smoking | |
|
| ||
| 5 | Benefits of quitting | 3 Good Things |
| Managing smoking `slips' | Savoring Kindness | |
| Nicotine patch review | Signature strengths in quitting smoking | |
| Planning for high-risk situations | ||
|
| ||
| 6 | Benefits of quitting | Review of PPT exercises |
| Managing smoking `slips' | Choosing PPT exercises to continue | |
| Nicotine patch tapering | ||
| Planning for high-risk situations | ||
Intervention Components
Positive Psychology Intervention Components
We started by integrating 6 exercises that were originally included in the clinical trials of PPT for mild to moderate depression (Seligman et al., 2006) and our standard behavioral smoking cessation counseling platform used in a prior clinical trial (Kahler et al., 2008). The 6 exercises we started with were (1) using Signature Strengths in a new way, (2) Three Good Things, (3) Gratitude Visit, (4) Savoring, (5) Active/constructing Responding, and (6) Positive Service. A Savoring Kindness exercise was later added in place of Positive Service, while the Signature Strengths exercise was modified to focus solely on using one's strengths to aid smoking cessation. A description of these components and how they were modified for the context of smoking cessation is provided below.
Signature strengths
Participants completed the Values in Action Survey (VIAS; Park, Peterson & Seligman, 2004) at baseline. This survey asks about 24 different “Signature Strengths,” which are core virtues or positive attributes that one shows across many situations, that bring satisfaction, and that help one to meet the challenges of life (e.g., Love of learning; Bravery; Kindness; Appreciation of beauty; etc.). Participants' strengths are rank-ordered based on their responses to the VIAS, with the top 5 strengths considered “signature strengths.” During the first treatment session, counselors asked participants to consider ways that these strengths fit with how they viewed themselves and to provide an example of how they had used one of their strengths recently. Counselors stressed that none of the qualities from the VIAS were “weaknesses,” but that the top 5 strengths were anticipated to be most helpful in one's quit attempt. Initially, counselors asked participants to think of new ways to use their signature strengths each day. However, after nine participants had completed this exercise, counselors observed that few participants were engaged in and successful with it. Therefore, given the context in which participants were presenting to counseling, the manual was modified so that participants were only asked to consider how they could utilize their signature strengths to facilitate quitting smoking and to cope with high-risk situations (see Table 2 for examples).
Table 2.
Signature Strengths and Associated Strategies for Smoking Cessation
| Strength | Strategy for Quitting |
|---|---|
| Strengths of Wisdom & Character | |
| Creativity | Brainstorm multiple different ways to avoid situations in which you might want a cigarette. |
| Curiosity | Use the internet or other resources to learn about many strategies that others have used to get through difficult cravings. |
| Judgment | Use your open-mindedness to consider the ways that being a non-smoker might enhance your life. |
| Love of Learning | Take the perspective that you might not know how to live as a non-smoker yet, but that you're open to learning about how to do that; think of quitting smoking as a job that needs to be completed thoroughly. |
| Perspective | Consider the “big picture” and think about how smoking might not fit into the way that you wish to conduct your life and relationships; take the needs of those who are close to you into account. |
| Strengths of Courage | |
| Bravery | Acknowledge that getting through a craving is very difficult, and that you are not one to shy away from difficult things. |
| Perseverance | Persevere through each craving, day, and week with strength; consider quitting smoking to be one more example to show that you are not someone who gives up. |
| Honesty | Be open with your friends and loved ones about your desire to be a non-smoker; remind them (and yourself) that you follow through with your commitments. |
| Zest | Take on a novel activity that requires “pep”; consider whether smoking enhances or lessens your feelings of vitality. Attack this challenge as you have other challenges. |
| Strengths of Humanity | |
| Love | Think of those whom you love and how you would do anything for them, including quitting smoking; commit yourself to enhancing the welfare of those you love by having a healthier, longer life. |
| Kindness | Do something kind for yourself when it feels difficult to remain a non-smoker just as you would for someone else; think of how quitting smoking will benefit the greater good (e.g., healthcare costs, air pollution, being your healthiest self to help others). |
| Social Intelligence | Use your ability to understand your emotions to learn when cravings might be coming so that you can manage them more effectively; think about what your friends and family will think of you as a non-smoker. |
| Strengths of Justice | |
| Teamwork | Think of quitting smoking as a task that improves the world. Involve others in helping you create a quitting team that can support you. |
| Fairness | Consider how quitting smoking is giving you the best chance at a healthy life; respect others by not smoking. |
| Leadership | Organize social plans with family and friends that do not involve smoking. Show others who smoke that it is possible to quit. |
| Strengths of Temperance | |
| Forgiveness | If you have a slip or find yourself craving a cigarette, don't be too hard on yourself. Acknowledge mistakes and move on. |
| Humility | Show others that you have quit smoking instead of telling them that you plan to quit. |
| Prudence | Make a plan for each day, allowing no room for smoking breaks; plan ahead for high-risk situations. Think about the benefits of quitting smoking each day. |
| Self-Regulation | Set a standard for yourself as a non-smoker and work to meet that standard each day. Think about the long-term gain of quitting smoking. Make plans for the times when you might be tempted to smoke. |
| Strengths of Transcendence | |
| Appreciation of Beauty and Excellence | Allow yourself to feel in awe of yourself for getting through difficult times; take pleasure in your successes (large and small) during your quit attempt. |
| Gratitude | Think of your life as a gift, and how quitting smoking allows you to appreciate this gift fully |
| Hope | If you have a slip, focus on the next opportunity and your plan for doing better; expect the best out of every situation in which you might want to smoke. Know that you can do this. |
| Humor | Don't allow your quit attempt get in the way of your playful attitude; try to make jokes with others about quitting. |
| Spirituality | Consider the purpose that your “higher power” has for your life - is smoking involved?; ask your “higher power” for strength when you need it |
Three Good Things
After quitting smoking, some individuals may feel that they are “missing out” on the enjoyment provided by smoking. To maintain a focus on the positive experiences in their life (including quitting smoking), participants were asked to write down three good things that happened each day. These could be ordinary and small in importance, or relatively large in importance. Three Good Things was initiated in Session 1 and continued throughout treatment given that this exercise seems to have a relatively delayed effect on mood (Seligman et al., 2006). After quitting smoking, participants were asked to record good things that happened in their efforts to quit smoking each day, in addition to other good things.
Gratitude Visit
Participants were asked to think of someone who helped them in their life and whom they wanted to thank more fully. Participants were asked to write a gratitude letter to the chosen individual and deliver it in person by reading it aloud. As part of the visit, participants were instructed to let the person know about their commitment to quit smoking in order to increase social support for quitting. This exercise was assigned in Session 2 (one week before quit date) given that it has shown a particularly strong and immediate effect on improving mood (Seligman et al., 2006).
Savoring
Smoking may be a psychopharmacologic means of enhancing pleasure garnered from positive experiences (Dawkins, Acaster, & Powell, 2007). PPT-S used savoring as alternative means of boosting pleasure and happiness from positive experience during the week after quitting smoking, when craving and mood disturbance are greatest. After an in-session example and practice, participants were asked to savor at least two experiences (e.g., their morning coffee; the sun on their face) each day for one week, for at least 2–3 minutes per experience. To effectively savor, participants were encouraged to be “in the moment” and “take in” all that a given experience had to offer. Participants also were asked to write down the two things they savored each day. This exercise was not modified for the context of smoking cessation, although the rationale for the exercise explained that it was important to find alternative sources of pleasure when giving up smoking.
Active-Constructive Responding
As an additional way to pay increased attention to positive events, participants were asked to spend one week listening carefully when people reported good events. Then, participants were asked to go out of their way to respond actively and constructively (e.g., to display genuine excitement and capitalize on the good news by seeking elaboration, suggesting celebratory activities, etc.; Gable, Reis, Impett, & Asher, 2004). Participants were asked to write about these experiences by noting the good news, their response to the good news, and how the other person responded.
Positive Service/Savoring Acts of Kindness
In the initial phase of manual development, participants were asked to choose two domains in which they wanted to serve (e.g., politics, religion, family, science, community) by exercising their strengths (i.e., Positive Service). They wrote down these ideas for service and selected one to put into action the following week. This exercise was introduced near the end of treatment, with the rationale being that participants would be more able to focus outside of themselves once they had passed the initial phases of quitting. However, Positive Service proved difficult to implement with the first six participants who reached this point in the treatment because there was insufficient time in session to explain this more complex exercise and to assess experiences with it afterwards. Therefore, we switched to a Savoring Kindness exercise, which asked participants to become aware of when they exhibited kind behavior toward another person and to savor this kind behavior by noticing it and writing it down. This exercise was based on a prior study showing that writing down one's acts of kindness enhanced well-being (Otake, Shimai, Tanaka-Matsumi, Otsui, & Fredrickson, 2006). Treatment providers emphasized that there was no specific number of kind things they “should” do each day.1
Standard Smoking Cessation Components
The standard smoking cessation components of the intervention remained constant across all participants. Participants smoking more than 10 cigarettes per day at baseline received treatment with transdermal nicotine patch with the initial dose starting on quit date at 21 mg for four weeks, followed by two weeks of 14 mg patch, and then two weeks of 7 mg patch. Participants smoking 5–10 cigarettes per day started with 14 mg for six weeks, followed by two weeks of 7 mg patch. Standard behavioral treatment was based on recent clinical practice guidelines for smoking cessation (Fiore, 2008) and interventions we have previously delivered (e.g., Kahler et al., 2008). The focus of the first two sessions was on identifying reasons for quitting, seeking social support for quitting, and problem solving regarding high-risk situations for smoking relapse. Participants were also instructed on the proper use of nicotine patch. Identifying and planning for high-risk situations remained the focus of the treatment after quit date with counselors providing support, reinforcing success, and bolstering self-efficacy, as well as managing slips in the event that participants smoked after quit date.
Results
Sample Characteristics
The 19 participants had a mean age of 45.0 (SD = 9.9) and a mean of 13.1 years of education (SD = 2.0); 31.6% were female, 74% were White, 21.0% were Black/African American, and 5.3% were American Indian, with 5.3% identifying as Hispanic/Latino, and 52.6% were married or living with a partner. Participants smoked an average of 18.3 (SD = 5.2) cigarettes per day with a mean of 5.7 (SD = 1.7) on the Fagerström Test for Nicotine Dependence (FTND; Heatherton et al. 1991).
Treatment Attendance
Participants attended an average of 4.68 (SD = 1.86) out of a possible 6 treatment sessions, with 63.1% completing all 6 sessions. Of the 19 participants who started treatment, 16 (84.2%) completed in-person assessments at the 8-, 16-, and 26-week follow-ups. Of those missing a follow-up, one missed all follow-ups, two missed 2 follow-ups, and one missed 1 follow-up. Each of the 12 participants who completed all 6 treatment sessions also completed the 8-week follow-up.
Treatment Evaluation and Use of Strategies
Treatment Satisfaction
On the CSQ completed at the 8-week follow-up, participants indicated very high levels of satisfaction with treatment, averaging a 2.65 (SD = 0.36) on the 0 to 3 scale. Participants also reported high levels of enjoyment of the positive focus of the treatment with a mean response of 4.73 (SD = 0.59) on a 1 to 5 scale.
Use of strategies
Table 3 shows the mean levels of use of each strategy broken down by smoking cessation-specific strategies and PPT-related strategies. Overall, self-reported use of PPT-consistent strategies was high, with mean responses averaging between agree and strongly agree for whether participants used each strategy while quitting. By contrast, participants reported relatively less avoidance of situations that would make them want to smoke. The strategy most commonly endorsed was thinking about the benefits of quitting.
Table 3.
Use of Strategies to Quit Smoking (N = 16)
| Item | Mean | SD |
|---|---|---|
| General Smoking Cessation Strategies | ||
| 1. I used the nicotine patch the way I was supposed to (one patch every day). | 3.93 | 1.57 |
| 2. I avoided situations that would make me want to smoke. | 3.50 | 1.31 |
| 3. I thought about high risk situations for smoking and planned how to deal with them. | 4.44 | 0.89 |
| 4. I thought about the benefits of quitting smoking. | 4.94 | 0.25 |
| PPT Consistent Strategies | ||
| 5. I thought often about things I was grateful for. | 4.63 | 0.62 |
| 6. I tried to express my gratitude to others more often. | 4.48 | 0.96 |
| 7. I focused on the good things that happened each day. | 4.44 | 0.89 |
| 8. I found new ways to do positive things for other people. | 4.13 | 0.72 |
| 9. I tried to savor the positive and pleasurable experiences in my daily life. | 4.56 | 0.63 |
Note: Scale ranges from 1 = `strongly disagree' to 5 = `strongly agree'
PPT-S component evaluation
Perceived usefulness of treatment components is presented in Table 3, which shows the % of participants finding each exercise moderately useful, extremely useful, or less than moderately useful in quitting smoking. The nicotine patch was considered extremely useful by over 3/4 of participants, consistent with its proven effectiveness in smoking cessation. Although counseling was seen as moderately or extremely useful overall, there was variability among the various PPT components. In particular, over 30% found the Three Good Things, Gratitude Visit, and Active/Constructive Responding exercises less than moderately useful. These evaluations aligned with the end of treatment discussions with counselors, during which Three Good Things, Gratitude Visit, and Savoring were the only exercises that participants indicated that they would continue to do after counseling ended.
Smoking Outcomes
Biochemically-verified point prevalence abstinence was 47.4% at 8-weeks, 36.9% at 16 weeks, and 31.6% at 26 weeks. Six of 19 (31.6%) participants were continuously abstinent from quit date through the 26-week follow-up.
Mood Outcomes
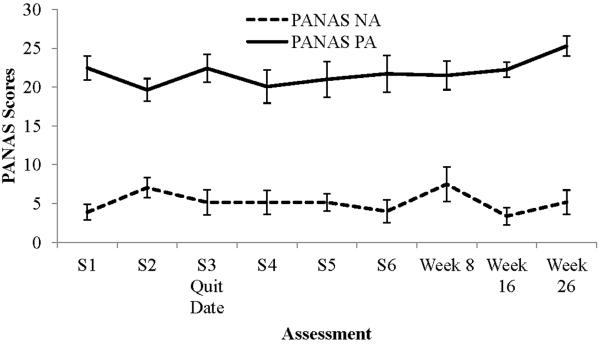
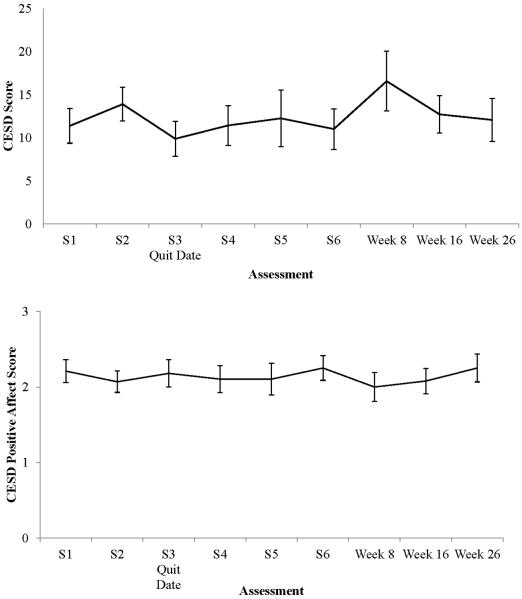
Figure 1 shows negative and positive affect across the 6 sessions of treatment and all follow-ups as assessed by the PANAS. Figure 2 shows the mean values and standard errors for the CES-D sum score and the Positive Affect subscale at those assessments. For all of these measures, the trajectories of change were relatively flat indicating that there were not substantial mood changes during and after smoking cessation.
Figure 1.
PANAS Scores over the 6 sessions of counseling and the 3 follow-ups. Error bars represent standard errors. PANAS = Positive Affect and Negative Affect Scales; NA= Negative Affect; PA=Positive Affect. Scores on each scale can range from 0 to 40.
Figure 2.
CESD total scores and Positive Affect subscale scores over the 6 sessions of counseling and the 3 follow-ups. Error bars represent standard errors. CESD=Center for Epidemiologic Studies Depression Scale. Total scores can range from 0 to 60. Positive Affect scores are the item average for positive affect items on the CES-D and range from 0 to 3.
Discussion
Results of this formative research support the feasibility and acceptability of incorporating positive psychology interventions into smoking cessation. Participants reported very high satisfaction with counseling, enjoying the positive focus of the treatment, and using the strategies taught in the program. About 49% of participants who appeared eligible at phone screen never attended a baseline session, a no-show rate typical of smoking cessation trials. For example, in the MacPherson et al. (2010) study of smokers with elevated depressive symptoms, 67.7% of participants screening eligible did not show for a baseline assessment, and 38% of participants eligible at baseline never showed for a treatment session. Participants completed an average of 78% of sessions in the present study, which is comparable to attendance rates in similar studies addressing mood in smoking cessation: 75% (Brown et al., 2007), 73.5% (Brown et al., 2001), and 81% (MacPherson et al., 2010).
Although there was no comparison condition in this study, making it difficult to draw conclusions about the potential effects of PPT-S relative to standard smoking cessation treatment, the 31.6% rate of abstinence at 6 months was relatively high. Meta-analyses suggest that the 6-month abstinence rates for smokers receiving nicotine patch averages about 23% (Fiore et al, 2008). The relatively high abstinence rates after PPT-S are especially notable because participants were selected based on low positive affect on the CESD, which is a robust predictor of poor smoking outcomes (Leventhal et al., 2008). In the MacPherson et al. (2010) study of smokers with elevated depressive symptoms, the abstinence rate at 6 months was 0% in the control condition and 19.2% in the behavioral activation condition.
Mood outcomes also are difficult to judge because of the lack of a comparison group. On the one hand, it was disappointing that there was relatively little movement in depressive symptoms, negative affect, and positive affect during treatment. There was a slight increase in depression scores at session 2 (prior to the quit date), which dropped again on the day of the quit, and then stayed stable throughout the remainder of the treatment. There was a modest increase in depressive symptoms between the end of treatment and the 8-week follow-up, but this disappeared at the 16- and 26-week follow-ups. It is not clear whether this represents random variation or a potential increase in negative moods associated with the program ending. Mood changes typically occur with smoking cessation, often worsening up to and including on quit date and then slowly improving (Strong et al., 2009). That moods remained stable during treatment and did not dramatically worsen on the quit date can be considered a promising outcome for PPT-S.
We used an iterative, counselor-consensus process to modify the manual as we accumulated experience with it. Two primary modifications were made. First, we modified the Signature Strengths exercise to focus exclusively on using strengths in smoking cessation, given that this was the reason that participants were presenting to counseling. Second, we replaced Positive Service with a Savoring Kindness exercise because we believed it required less effort for participants to implement, especially at the end of treatment when motivation to implement new exercises may be lower. However, because Savoring Kindness was only administered to six participants, we are less able to determine whether this was a useful addition to the protocol. Three Good Things, the Gratitude Visit, and Active/Constructive Responding were modified only slightly to integrate with smoking cessation and were viewed favorably by most participants, although a minority did not find such exercises useful. Savoring was particularly well-received by participants. It is important to note, however, that these results were based on clinical consensus and examination of rating scales; a qualitative approach was not employed to gauge participant responses and would be useful for further refinement of the manual.
Conclusions
The integration of positive psychology interventions into smoking cessation treatment is a novel direction for the field that may be broadly applicable to many behavior change interventions. The next step in this research is to conduct an initial investigation of the efficacy of PPT-S compared to a standard smoking cessation treatment that does not contain mood management components. Additional research also would be valuable to identify whether a smaller number of positive psychology exercises (e.g.., Schueller & Parks, in press) or allowing participants to choose exercises (e.g., Schueller et al., 2013) would improve the efficacy of PPT-S.
Table 4.
Evaluation of Treatment Components (N = 13)
| < Moderately Useful % (n) | Moderately Useful % (n) | Extremely Useful % (n) | |
|---|---|---|---|
| How useful was the nicotine patch? | 14.4% (2) | 7.7% (1) | 76.9% (10) |
| Overall, how useful was the counseling your received? | 0.0% (0) | 38.5% (5) | 61.5% (8) |
| How useful was it for you to try to use your signature strengths in quitting smoking? | 14.4% (2) | 46.1% (6) | 38.5% (5) |
| How useful were the “Three Good Things” exercises? | 30.8% (4) | 30.8% (4) | 38.5% (5) |
| How useful was writing about things you were grateful for? | 30.8% (4) | 46.2% (6) | 23.1% (3) |
| How useful was the Daily Savoring exercise? | 7.7% (1) | 61.5% (8) | 30.8% (4) |
| How useful was the active/constructive responding exercise? | 46.2% (6) | 38.5% (5) | 14.4% (2) |
Note: Response options range from 0 = `not at all useful' to 4 = `extremely useful
Acknowledgements
This research was supported by the National Cancer Institute grant R01CA156241 to CWK.
Footnotes
Note that initially, participants were asked not only to notice but also to count their acts of kindness (following Otake, Shimai, Tanaka-Matsumi, Otsui, & Fredrickson, 2006). However, we changed the exercise from “counting” to “savoring” given concerns that the act of counting made some participants feel like they were “gloating” or being artificial.
References
- Berlin I, Covey LS. Pre-cessation depressive mood predicts failure to quit smoking: The role of coping and personality traits. Addiction. 2006;101:1814–1821. doi: 10.1111/j.1360-0443.2006.01616.x. doi: http://dx.doi.org/10.1111/j.1360-0443.2006.01616.x. [DOI] [PubMed] [Google Scholar]
- Bränström R, Penilla C, Pérez-Stable EJ, Muñoz RF. Positive affect and mood management in successful smoking cessation. American Journal of Health Behavior. 2010;34:553–562. Retrieved from http://search.proquest.com/docview/815570913?accountid=14168. [PubMed] [Google Scholar]
- Brown RA, Kahler CW, Niaura R, Abrams DB, Sales SD, Ramsey SE, Miller IW. Cognitive–behavioral treatment for depression in smoking cessation. Journal of Consulting and Clinical Psychology. 2001;69:471–480. doi: 10.1037//0022-006x.69.3.471. doi: http://dx.doi.org/10.1037/0022-006X.69.3.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Niaura R, Lloyd-Richardson E, Strong DR, Kahler CW, Abrantes AM, Miller IW. Bupropion and cognitive-behavioral treatment for depression in smoking cessation. Nicotine & Tobacco Research. 2007;9:721–730. doi: 10.1080/14622200701416955. doi: http://dx.doi.org/10.1080/14622200701416955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess ES, Brown RA, Kahler CW, Niaura R, Abrams DB, Goldstein MG, Miller IW. Patterns of change in depressive symptoms during smoking cessation: Who's at risk for relapse? Journal of Consulting and Clinical Psychology. 2002;70:356–361. doi: 10.1037//0022-006X.70.2.356. doi: http://dx.doi.org/10.1037/0022-006X.70.2.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook J, Spring B, McChargue D, Doran N. Effects of anhedonia on days to relapse among smokers with a history of depression: A brief report. Nicotine & Tobacco Research. 2010;12:978–982. doi: 10.1093/ntr/ntq118. doi: http://dx.doi.org/10.1093/ntr/ntq118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covey LS, Glassman AH, Stetner F. Depression and depressive symptoms in smoking cessation. Comprehensive Psychiatry. 1990;31:350–354. doi: 10.1016/0010-440x(90)90042-q. doi: http://dx.doi.org/10.1016/0010-440X(90)90042-Q. [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Ekman P, Saron CD, Senulis JA, Friesen WV. Approach-withdrawal and cerebral asymmetry: Emotional expression and brain physiology: I. Journal of Personality and Social Psychology. 1990;58:330–341. doi: http://dx.doi.org/10.1037/0022-3514.58.2.330. [PubMed] [Google Scholar]
- Dawkins L, Acaster S, Powell JH. The effects of smoking and abstinence on experience of happiness and sadness in response to positively valenced, negatively valenced, and neutral film clips. Addictive Behaviors. 2007;32:425–431. doi: 10.1016/j.addbeh.2006.05.010. doi: http://dx.doi.org/10.1016/j.addbeh.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Jaén C, Baker T, et al. Treating Tobacco Use and Dependence: 2008 Update. U.S. Department of Health and Human Services; Rockville, MD: 2008. Public Health Service 2008. [Google Scholar]
- First M, Spitzer L, Gibbon M, Williams J. Structured clinical interview for Axis I DSM-IV disorders (SCID) American Psychiatric Association; Washington, DC: 1995. [Google Scholar]
- Gable SL, Reis HT, Impett EA, Asher ER. What do you do when things go right? the intrapersonal and interpersonal benefits of sharing positive events. Journal of Personality and Social Psychology. 2004;87:228–245. doi: 10.1037/0022-3514.87.2.228. doi: http://dx.doi.org/10.1037/0022-3514.87.2.228. [DOI] [PubMed] [Google Scholar]
- Ginsberg D, Hall SM, Reus VI, Muñoz RF. Mood and depression diagnosis in smoking cessation. Experimental and Clinical Psychopharmacology. 1995;3:389–395. doi: http://dx.doi.org/10.1037/1064-1297.3.4.389. [Google Scholar]
- Haas AL, Muñoz RF, Humfleet GL, Reus VI, Hall SM. Influences of mood, depression history, and treatment modality on outcomes in smoking cessation. Journal of Consulting and Clinical Psychology. 2004;72:563–570. doi: 10.1037/0022-006X.72.4.563. doi: http://dx.doi.org/10.1037/0022-006X.72.4.563. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström K. The fagerström test for nicotine dependence: A revision of the fagerström tolerance questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. doi: http://dx.doi.org/10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Brown RA, Ramsey SE, Niaura R, Abrams DB, Goldstein MG, Miller IW. Negative mood, depressive symptoms, and major depression after smoking cessation treatment in smokers with a history of major depressive disorder. Journal of Abnormal Psychology. 2002;111:670–675. doi: 10.1037//0021-843x.111.4.670. doi: http://dx.doi.org/10.1037/0021-843X.111.4.670. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Metrik J, LaChance HR, Ramsey SE, Abrams DB, Monti PM, Brown RA. Addressing heavy drinking in smoking cessation treatment: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2008;76:852–862. doi: 10.1037/a0012717. doi: http://dx.doi.org/10.1037/a0012717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinnunen T, Doherty K, Militello FS, Garvey AJ. Depression and smoking cessation: Characteristics of depressed smokers and effects of nicotine replacement. Journal of Consulting and Clinical Psychology. 1996;64:791–798. doi: 10.1037//0022-006x.64.4.791. doi: http://dx.doi.org/10.1037/0022-006X.64.4.791. [DOI] [PubMed] [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning. 1979;2:197–207. doi: 10.1016/0149-7189(79)90094-6. http://dx.doi.org/10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Ramsey SE, Brown RA, LaChance HR, Kahler CW. Dimensions of depressive symptoms and smoking cessation. Nicotine & Tobacco Research. 2008;10:507–517. doi: 10.1080/14622200801901971. doi: http://dx.doi.org/10.1080/14622200801901971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyubomirsky S, King L, Diener E. The benefits of frequent positive affect: Does happiness lead to success? Psychological Bulletin. 2005;131:803–855. doi: 10.1037/0033-2909.131.6.803. doi: http://dx.doi.org/10.1037/0033-2909.131.6.803. [DOI] [PubMed] [Google Scholar]
- MacPherson L, Tull MT, Matusiewicz AK, Rodman S, Strong DR, Kahler CW, Lejuez CW. Randomized controlled trial of behavioral activation smoking cessation treatment for smokers with elevated depressive symptoms. Journal of Consulting and Clinical Psychology. 2010;78:55–61. doi: 10.1037/a0017939. doi: http://dx.doi.org/10.1037/a0017939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otake K, Shimai S, Tanaka-Matsumi J, Otsui K, Fredrickson BL. Happy people become happier through kindness: A counting kindnesses intervention. Journal of Happiness Studies. 2006;7:361–375. doi: 10.1007/s10902-005-3650-z. doi: http://dx.doi.org/10.1007/s10902-005-3650-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park N, Peterson C, Seligman MEP. Strengths of character and well-being. Journal of Social and Clinical Psychology. 2004;23:603–619. doi: http://dx.doi.org/10.1521/jscp.23.5.603.50748. [Google Scholar]
- Parks AC, Seligman MEP. 8-week group Positive Psychotherapy (PPT) Manual. 2007. Unpublished manual, available by request. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: http://dx.doi.org/10.1177/014662167700100306. [Google Scholar]
- Schueller SM, Pérez-Stable EJ, Muñoz RF. A mood management intervention in an Internet stop smoking randomized controlled trial does not prevent depression: A cautionary tale. Clinical Psychological Science. doi: 10.1177/2167702613484717. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman MEP, Csikszentmihalyi M. Positive psychology: An introduction. American Psychologist. 2000;55:5–14. doi: 10.1037//0003-066x.55.1.5. doi: http://dx.doi.org/10.1037/0003-066X.55.1.5. [DOI] [PubMed] [Google Scholar]
- Seligman MEP, Rashid T, Parks AC. Positive psychotherapy. American Psychologist. 2006;61:774–788. doi: 10.1037/0003-066X.61.8.774. doi: 10.1037/1089-2680.5.4.323. [DOI] [PubMed] [Google Scholar]
- Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. Journal of Clinical Psychology. 2009;65:467–487. doi: 10.1002/jclp.20593. doi: http://dx.doi.org/10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. Structured Clinical Interview for DSM 111(R)-Patient edition (SCID-P). Biometrics Research Department, New York State Psychiatric Institute; New York: 1989. [Google Scholar]
- SRNT Subcommittee on Biochemical Verification Biochemical verification of tobacco use and cessation. Nicotine & Tobacco Research. 2002;4:149–59. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- Strong DR, Kahler CW, Leventhal AM, Abrantes AM, Lloyd-Richardson E, Niaura R, Brown RA. Impact of bupropion and cognitive–behavioral treatment for depression on positive affect, negative affect, and urges to smoke during cessation treatment. Nicotine & Tobacco Research. 2009;11:1142–1153. doi: 10.1093/ntr/ntp111. doi: http://dx.doi.org/10.1093/ntr/ntp111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong DR, Leventhal AM, Evatt DP, Haber S, Greenberg BD, Abrams D, Niaura R. Positive reactions to tobacco predict relapse after cessation. Journal of Abnormal Psychology. 2011;120:999–1005. doi: 10.1037/a0023666. doi: http://dx.doi.org/10.1037/a0023666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark L. The PANAS-X: Manual for the Positive and Negative Affect Schedule*Expanded Form. The University of Iowa; Iowa City, IA: 1994. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. doi: http://dx.doi.org/10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Introduction to the special issue on personality and psychopathology. Journal of Abnormal Psychology. 1994;103:3–5. doi: http://dx.doi.org/10.1037/h0092429. [PubMed] [Google Scholar]
- Watson D, Clark LA. Measurement and mismeasurement of mood: Recurrent and emergent issues. Journal of Personality Assessment. 1997;68:267–296. doi: 10.1207/s15327752jpa6802_4. doi: http://dx.doi.org/10.1207/s15327752jpa6802_4. [DOI] [PubMed] [Google Scholar]
- Watson D, Tellegen A. Toward a consensual structure of mood. Psychological Bulletin. 1985;98:219–235. doi: 10.1037//0033-2909.98.2.219. doi: http://dx.doi.org/10.1037/0033-2909.98.2.219. [DOI] [PubMed] [Google Scholar]
- West RJ, Hajek P, Belcher M. Severity of withdrawal symptoms as a predictor of outcome of an attempt to quit smoking. Psychological Medicine. 1989;19:981–985. doi: 10.1017/s0033291700005705. doi: http://dx.doi.org/10.1017/S0033291700005705. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Stewart SH, Vujanovic AA, Gavric D, Steeves D. Anxiety sensitivity and anxiety and depressive symptoms in the prediction of early smoking lapse and relapse during smoking cessation treatment. Nicotine & Tobacco Research. 2009;11:323–331. doi: 10.1093/ntr/ntn037. doi: http://dx.doi.org/10.1093/ntr/ntn037. [DOI] [PMC free article] [PubMed] [Google Scholar]