Abstract
Objective. To identify reasons for drinking, determine the patterns of alcohol abuse, and explore relationships between drinking motives and alcohol abuse patterns in pharmacy students.
Methods. A cross-sectional anonymous, voluntary, self-administered paper survey instrument was administered to first-year (P1) through third-year (P3) pharmacy students as part of a professional seminar.
Results. Survey instruments were completed by 349 pharmacy students (95.9% cooperation rate). Using the Alcohol Use Disorders Identification Test criteria, 23.2% of students reported hazardous or harmful use and 67.2% of students reported consuming alcohol at hazardous levels during the past year. Students who were male (37.0%), single (25.3%), and attended the main campus (26.2%) were more likely than their counterparts to report hazardous or harmful alcohol use. Pharmacy students reported social motives as the most common reason for drinking; however, coping and enhancement motives were more predictive of harmful or hazardous alcohol use.
Conclusion. Approximately 1 in 4 pharmacy students (23%) reported hazardous or harmful alcohol use. Education about the dangers of alcohol abuse and intervention programs from colleges and schools of pharmacy are recommended to help address this issue.
Keywords: pharmacy students, alcohol abuse, drinking, substance abuse
INTRODUCTION
Alcohol abuse is a complex public health issue that is associated with a variety of destructive social conditions, such as failure in school and lost productivity.1 Given the prevalence of alcohol abuse and its damaging consequences, the United States Department of Health and Human Services outlined several objectives in its Healthy People 2020 initiative focusing on alcohol consumption, including reducing binge drinking during the past 2 weeks in college students, reducing binge drinking during the past 30 days in adults aged 18 years and older, and reducing average annual alcohol consumption.1 Binge drinking among college students has received increased attention because college students, when compared to their noncollege peers of the same age, exhibited higher rates of alcohol use (60.8% vs 52.0%), binge alcohol use (39.1% vs 35.4%), and heavy alcohol use (13.6% vs 10.5%).2 The 21- to 25-year-old group exhibited the highest proportion of past year alcohol use (83.9%), past month use (69.7%), binge drinking (45.4%), and heavy alcohol use (13.7%). Considering that most pharmacy students are within this age group, it is important to determine whether pharmacy students exhibit similar patterns of abuse.3
Because substance abuse and addiction are major concerns for pharmacy students and pharmacists, the American Association of Colleges of Pharmacy (AACP) Special Committee on Substance Abuse and Pharmacy Education recommends that colleges and schools of pharmacy address these disorders in their curricula.4 This AACP committee also recommended an increase in continuing education programs to address the needs of future and current practitioners in addiction and substance abuse. These recommendations are intended to improve the education of students, faculty and staff members, and practitioners to provide them with the necessary tools to identify and assist others who may need help with addiction and substance abuse. Therefore, colleges and schools of pharmacy must develop or modify alcohol abuse education programs to address both short-term and long-term alcohol use issues.
Nearly 1 in 4 pharmacy students has exhibited hazardous alcohol use.3,5 These students also exhibited behaviors that negatively affected grades and school work, and some even reported participating in patient care under the influence of alcohol. Because substance use by pharmacy students is a strong predictor of future abuse, understanding the prevalence of alcohol use and reasons for using alcohol during a pharmacy program may help prevent students from long-term alcohol abuse.6 Long-term alcohol abuse among pharmacists is concerning as pharmacists misuse alcohol at rates that exceed the general population.7 Pharmacists who have experienced addiction have indicated that more intensive early education and prevention programs are needed.8 Educational programs that address drinking motives should be established in colleges and schools of pharmacy to prevent long-term abuse.
Few publications have reported the motives for drinking among pharmacy students.5,9 Because drinking motives have not been primary study objectives or assessed with validated measures, additional research examining drinking motives is still needed. Studies in other student populations have yielded promising data to inform prevention and intervention efforts. Drinking motives represent a subjectively derived decisional framework for alcohol consumption that is based on an individual’s personal experience, current environment or situation, and alcohol expectancies.10,11 Social enhancement motives are the most commonly indicated reasons for consuming alcohol among college students.12,13 Although drinking to enhance social experiences may be common, drinking to cope with negative affect or enhance positive affect is more likely to be associated with increased alcohol consumption and alcohol-related problems.13-15 Our study investigated self-reported alcohol use and identified reasons for drinking alcohol among doctor of pharmacy (PharmD) students at 1 institution. The study objectives were to identify reasons for drinking, determine the patterns of alcohol abuse, and explore the relationships between drinking motives and alcohol abuse patterns while controlling for demographic differences.
METHODS
The Auburn University Institutional Review Board approved this study. This cross-sectional study used an anonymous, voluntary, self-administered paper survey. Participants included P1 through P3 students from the Auburn University Harrison School of Pharmacy. Fourth-year students were not included because the study took place during their advanced pharmacy practice experiences off campus, making it difficult to gather appropriate and anonymous data. There were 441 potential participants who were required to attend weekly professional seminars.
The survey instrument was self-administered in-class during a 1-hour weekly professional seminar. On the day of survey administration, the topic was alcohol abuse among college students and the use of brief interventions to address alcohol abuse. At the beginning of the seminar, the invitation letter approved by the university’s Institutional Review Board and the survey instrument were distributed to the students. At that time, the study’s benefits, potential risks, and participant rights were explained to the students. They were allowed approximately 15 minutes to complete the survey instrument. An attendance count was taken to assess response rate. The survey instruments were distributed and returned in opaque envelopes to maintain anonymous responses. All envelopes were collected immediately before the speaker started the session.
The survey instrument was separated into 3 sections: participant characteristics, drinking motives (reasons for drinking), and alcohol use patterns. Participant demographics were collected, including age, sex, marital status, race, highest degree attained after high school, current class year, cumulative grade point average, campus (either main or satellite campus), and hours of work per week.
The Drinking Motives Questionnaire-Revised (DMQ-R), a 20-item validated survey instrument, was used to measure reasons why students might be motivated to drink alcoholic beverages.10 Although originally developed for adolescents, the DMQ-R has been used extensively and validated for use with samples of college-age young adults.16 The DMQ-R measures reasons in 4 primary areas: social, coping, conformity, and enhancement.10 The DMQ-R asks participants to remember all the times they used alcohol and how often they used alcohol for each of the 20 items. Response categories include “almost never or never,” “some of the time,” “half of the time,” “most of the time,” and, “almost always or always.” Examples of items included, “I use alcohol so I won't feel left out,” and, “I use alcohol to get high.”
The alcohol use patterns were assessed using the Alcohol Use Disorders Identification Test (AUDIT), a standardized tool developed by the World Health Organization.17,18 The AUDIT consists of 10 questions which ask about the quantity and frequency of alcohol use as well as the consequences of alcohol use, eg, “How many drinks do you have on a typical day?” “Do you have 6 or more on 1 occasion?” “Have you or someone else been injured as a result of your drinking?” Each of the questions has a set of responses to choose from, and each response has a score ranging from 0 to 4. Based on participants’ responses, they were categorized into presence or absence of hazardous or harmful alcohol use, hazardous alcohol use, dependence symptoms, and alcohol-related harm experienced. For example, out of a possible 40 points, students with an AUDIT score of 8 or greater would be categorized as having hazardous or harmful alcohol use.17,18
Data were analyzed using SPSS for Mac, version 21 (SPSS Inc, Cary, NC). Descriptive statistics were used to describe participant characteristics, drinking motives, and patterns of alcohol use. Psychometric properties of DMQ-R were assessed; reliability coefficients and item and scale statistics were calculated. Bivariate analyses were conducted to examine relationships between participant characteristics and the dependent variable (hazardous or harmful alcohol use); this was to determine what characteristics were associated with presence of hazardous or harmful alcohol use. Relationships between drinking motives and presence of hazardous or harmful alcohol use were explored using logistic regression analysis. In the logistic regression model, participant characteristics that had significant relationships with hazardous or harmful alcohol use were entered as control variables. An a priori alpha of <0.05 was chosen for significance testing.
RESULTS
On the day the survey was administered, there were 364 pharmacy students present on both campuses. Of those students, 349 completed the survey instrument, which gave an overall response rate of 82.5% and a cooperation rate of 95.9%. No data were collected from students who were absent or who refused to participate.
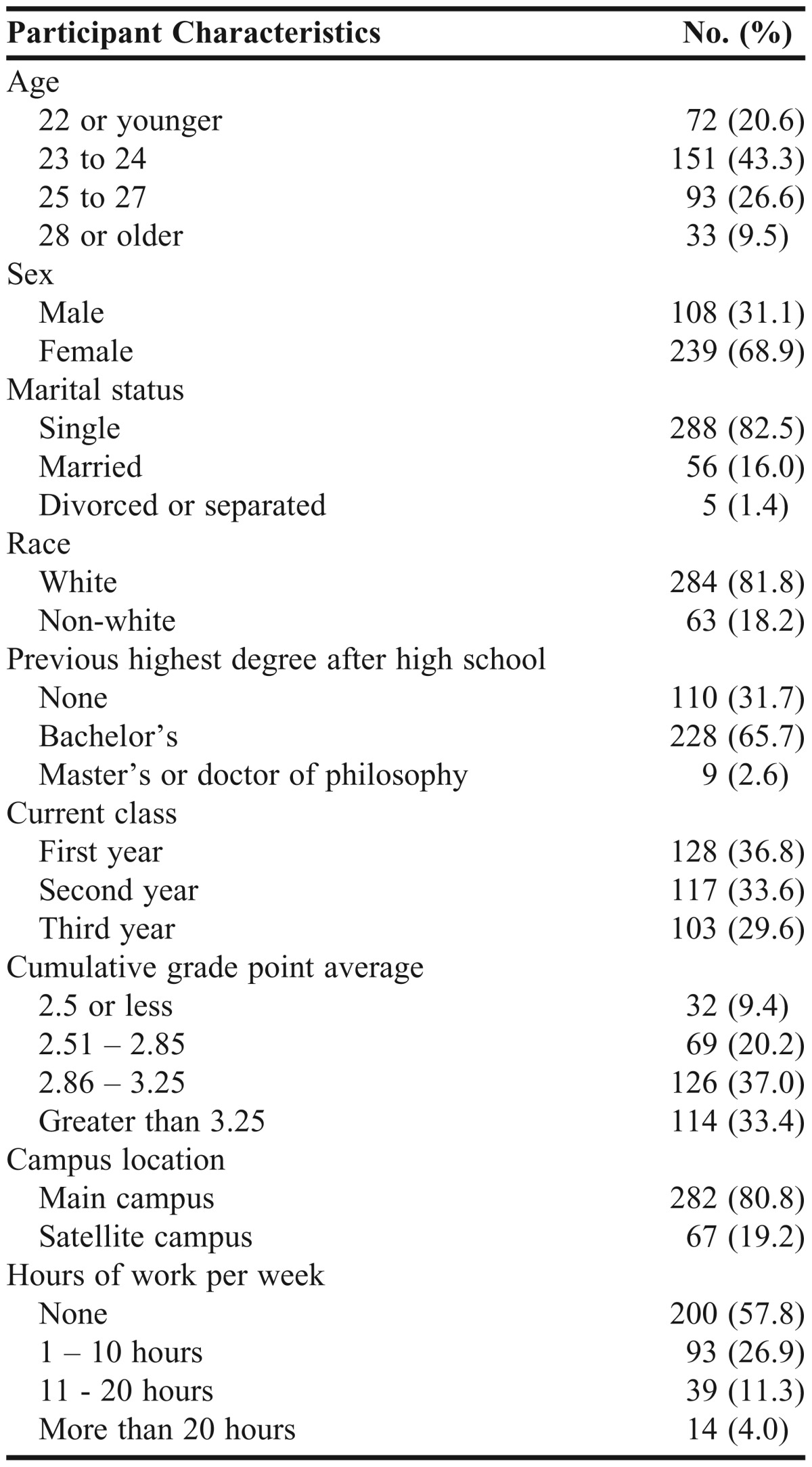
The largest percentages of participants were within the age range of 23 to 24 years of age (43.3%), female (68.9%), single (82.5%), and white (81.8%) (Table 1). Most students held a bachelor’s degree (65.7%) and most participants were from the main campus (80.8%) vs the satellite campus (19.2%).
Table 1.
Characteristics of Pharmacy Students Who Participated in a Survey of Alcohol Use Behaviors (N=349)
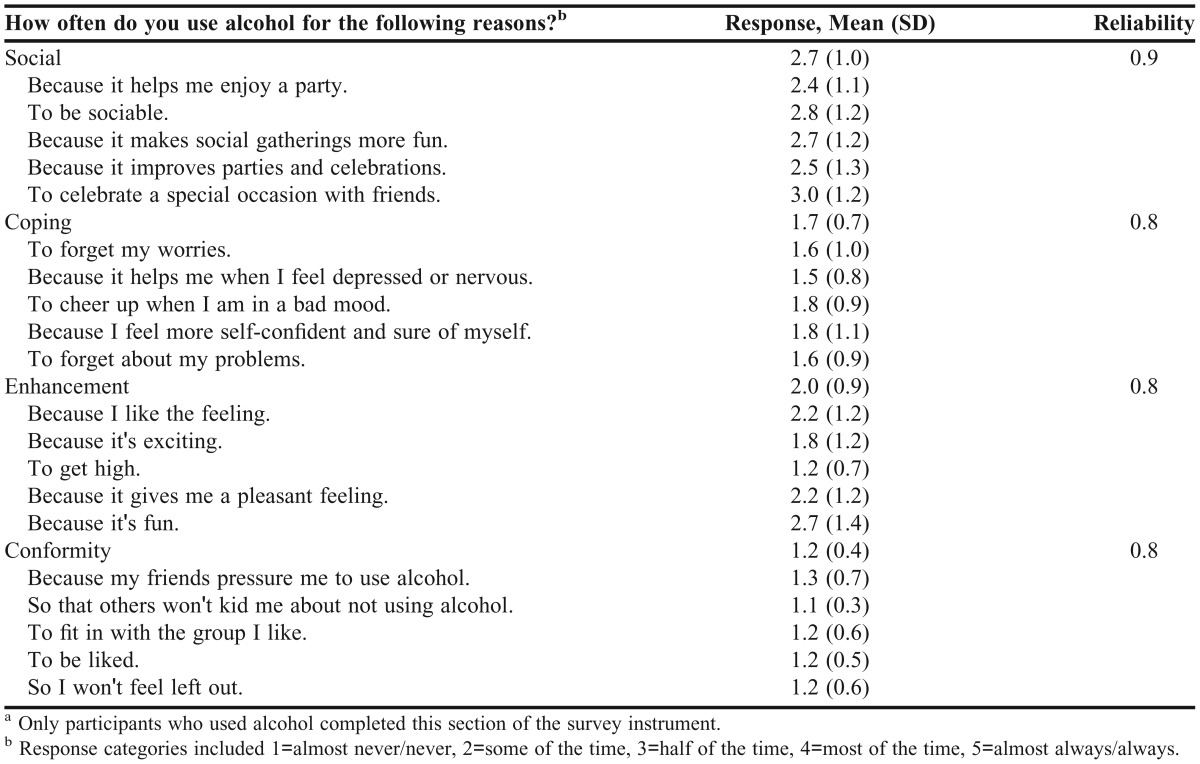
Participants who reported drinking during the last year answered 20 questions from the DMQ-R (Table 2). The mean score for social motives (2.7) was greater than enhancement motives (2.0), coping motives (1.7), and conformity motives (1.2). Each motive scale had 5 items and all scales had an acceptable reliability coefficient (>0.75).
Table 2.
Frequency of Drinking Motivesa of Pharmacy Students (N=302)
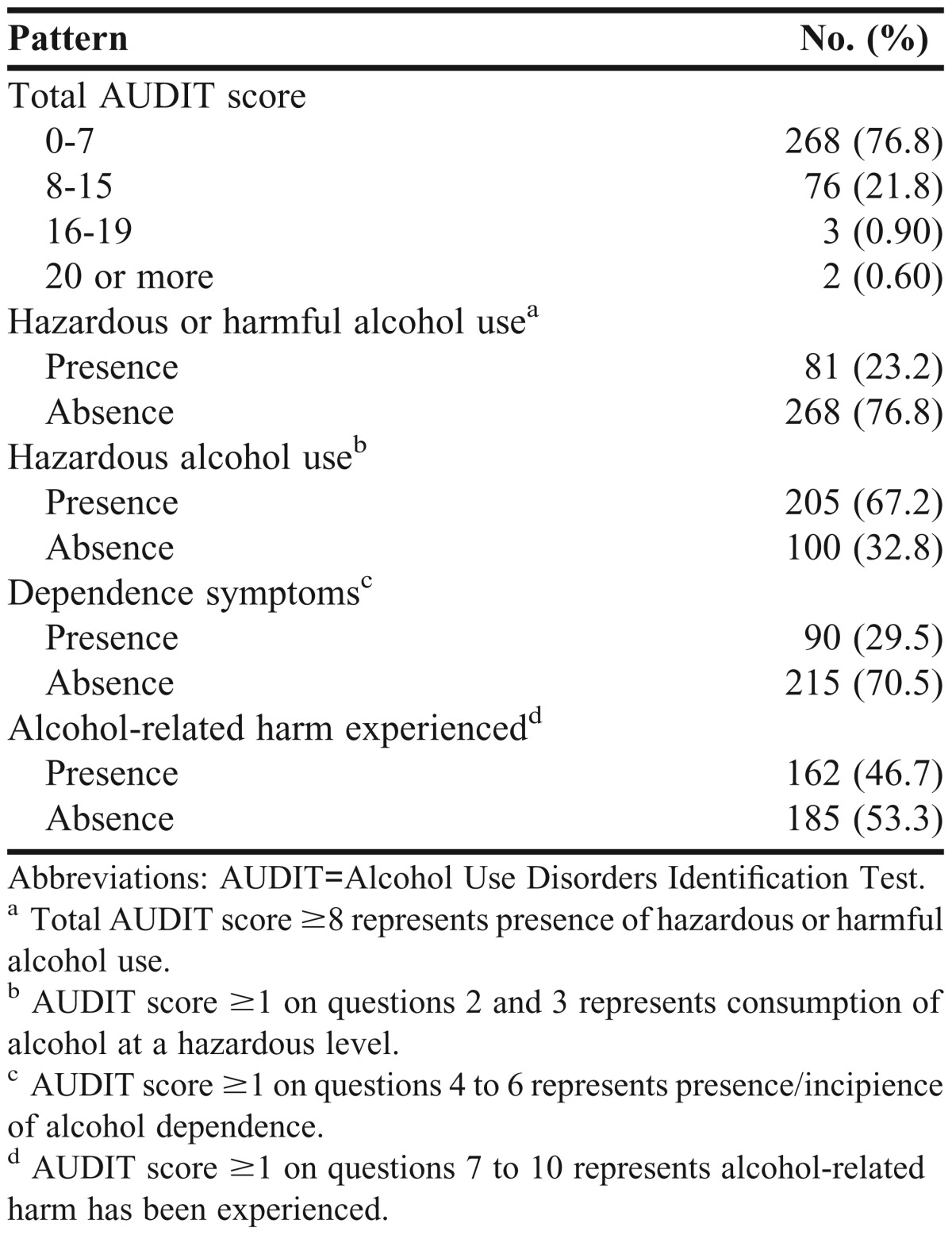
In terms of alcohol use patterns, of the students who completed the survey instrument, 23.2% had a total AUDIT score ≥8, which indicated hazardous or harmful alcohol use (Table 3). During the previous 12 months, 67.2% of respondents had consumed alcohol at hazardous levels, 29.5% had experienced symptoms suggestive of alcohol dependence, and 46.7% had experienced alcohol-related harm.
Table 3.
Patterns of Alcohol Use Based on Alcohol Use Disorders Identification Test Scores (N=349)
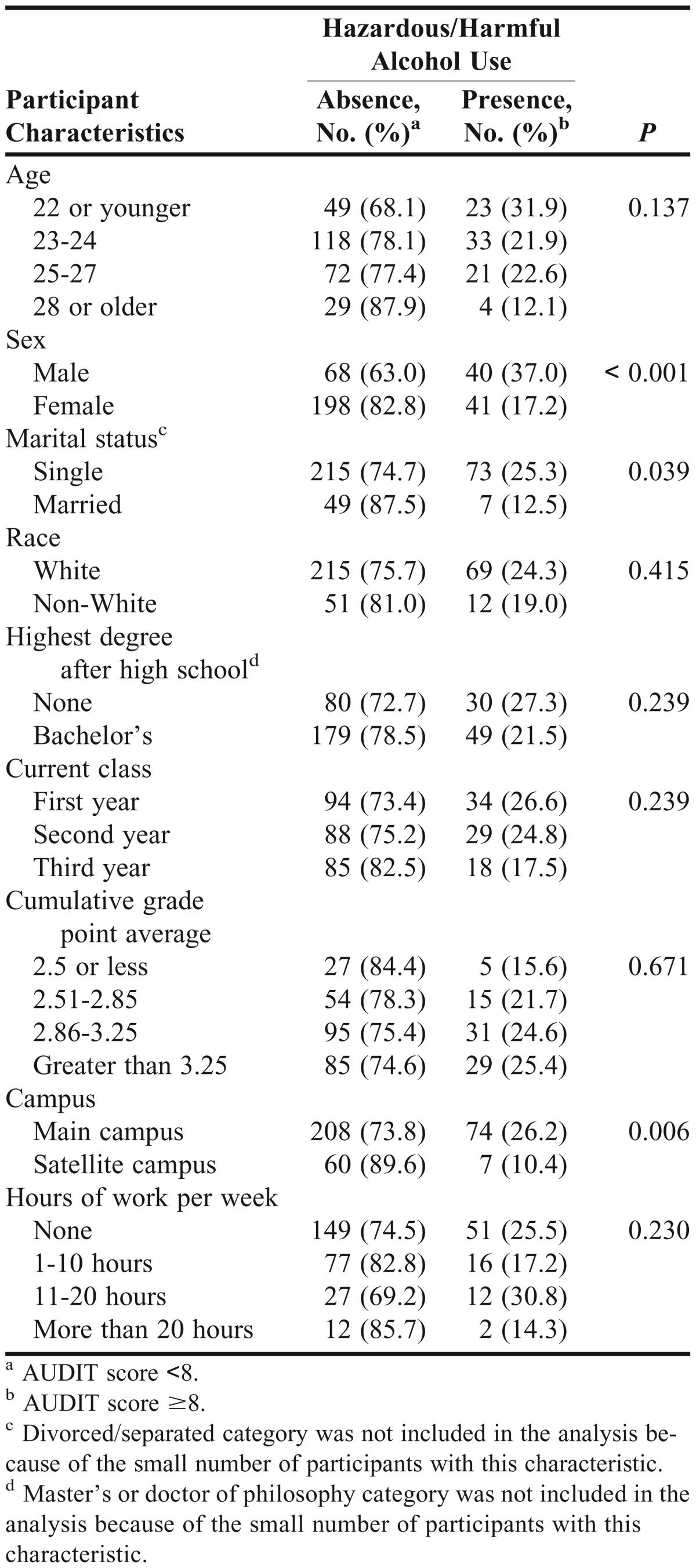
The associations between participant characteristics and status of hazardous or harmful alcohol use were assessed (Table 4). Students who were male, single, and attended classes on the main campus were more likely than their counterparts to report hazardous or harmful alcohol use. These 3 variables were later entered into the logistic regression model as control variables.
Table 4.
Relationship Between Pharmacy Student Characteristics and Hazardous or Harmful Alcohol Use (N=349)
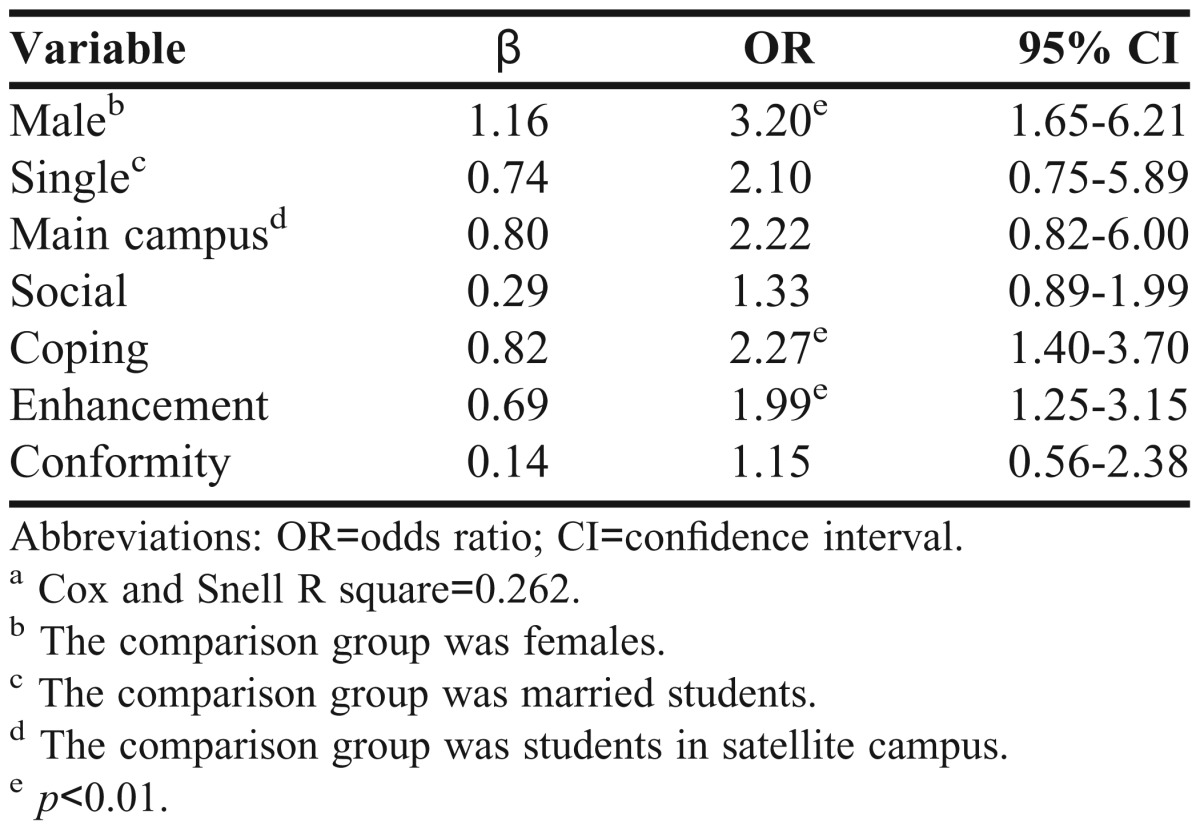
Next, a multiple logistic regression model was used to identify which drinking motives were associated with hazardous or harmful alcohol use when controlling for sex, marital status, and campus location (Table 5). The model indicated that the 4 drinking motives and 3 control variables accounted for 26.2% of variance in the harmful or hazardous alcohol use. The odds of a male student reporting harmful or hazardous alcohol use were 3.2 times greater than for a female student. However, marital status and campus location were not significant in the model. When examining the effect of drinking motives, coping and enhancement motives were significantly associated with hazardous or harmful alcohol use. A 1-unit change in coping motives or enhancement motives increased the odds of self-reported hazardous or harmful alcohol use by 2.3 and 2.0 times, respectively. Social and conformity motives neither significantly increased nor decreased the odds of hazardous or harmful alcohol use.
Table 5.
Odds Ratio and 95% Confidence Interval From Logistic Regression Analysis With Presence/Absence of Hazardous or Harmful Alcohol Use as the Dependent Variable (N=295)a
DISCUSSION
Using a standardized tool (AUDIT) to assess and categorize hazardous and harmful patterns of alcohol consumption strengthened our study Approximately 1 in 4 students (23.2%) had hazardous or harmful alcohol use, which was similar to the 25.2% of students among 9 colleges and schools of pharmacy reported by English and colleagues.3 Comparing this rate with other existing studies posed some challenges because other studies did not use the AUDIT tool. Most studies conducted in colleges and schools of pharmacy reported binge drinking percentage (5 or more drinks in 1 occasion) with varying reference timeframes. For example, 29% of students reported binge drinking in the preceding 2 weeks in the study by Baldwin and colleagues;5 36% of students reported binge drinking in the previous 2 weeks in the study by Kenna and Wood;6 and 29% to 44% of students reported binge drinking in the past year in the study by Murawski and colleagues.19 One theme is consistent across all of these studies: alcohol use among pharmacy students is concerning. Because of this, it is important to identify reasons for drinking, as it may allow colleges and schools of pharmacy to design interventions to focus on the areas affecting hazardous or harmful alcohol use.
Our study also intended to identify key reasons for harmful or hazardous alcohol use by using the DMQ-R, a validated questionnaire, to assess drinking motives. All 4 motives scales were internally reliable. Social motives were reported as the most frequently endorsed reasons for drinking. After controlling for demographics, coping and enhancement motives were found to increase the odds of harmful or hazardous alcohol use. These results were consistent with studies that investigated the role drinking motives play in alcohol use and alcohol-related problems. This suggests that the DMQ-R is suitable for use with pharmacy students, and that drinking motives play a similar role with this population of students.
Our findings have implications related to screening pharmacy students for potential alcohol problems and, when indicated, matching students to an appropriate intervention. Given the prevalence of alcohol use and misuse among pharmacy students, each college and school of pharmacy should have a system in place that can readily detect alcohol use problems and offer treatment recommendations. The AUDIT is designed to serve this purpose. Students with an AUDIT score of 8 to 15 are recommended to receive simple advice and alcohol education, those with an AUDIT score of 16 to 19 are recommended to receive simple advice plus brief counseling and continued monitoring, and those with an AUDIT score of ≥20 are recommended for referral to a specialist for diagnostic evaluation and treatment.10
A large percentage of students exhibiting hazardous alcohol use are recommended for simple advice and alcohol education. Therefore, improving the alcohol abuse education within colleges and schools of pharmacy could be sufficient to decrease the hazardous alcohol use behaviors in some of these students. Topics to be discussed in the alcohol educational programs should include, but are not limited to, drinking norms among pharmacy students, alcohol abuse among healthcare professionals, and consequences of binge drinking.9,20-22 Programs that offer information tailored to an individual student are more effective than general educational seminars and programs.23,24 Strategies for delivering alcohol education have been identified and garnered empirical support when used with college students. Examples include a variety of commercially available computer-delivered interventions (eg, AlcoholEdu (EVERFI, Washington, DC) and College Drinker’s Check-up (Behavior Therapy Associates, LLC, Albuquerque, NM)) and brief motivational interventions (eg, Brief Alcohol Screening Interventions for College Student Drinkers [BASICS]).24-26 Both interventions use personalized feedback on quantity and/or frequency of alcohol use, perceptions of normative behaviors among peer groups, and the personal and social consequences of alcohol use. These interventions may already be available on campus for pharmacy students. Because these interventions have not been tested among pharmacy students, additional research is needed to determine how effective these interventions will be when used with pharmacy students. Once effective strategies have been identified, colleges and schools of pharmacy will need to determine how to make these services available to students. Students with more severe problems and in need of more intensive interventions should be referred to pharmacy recovery networks, which operate in many states to assist pharmacists and pharmacy students. These networks typically provide treatment and recovery services that are directed toward the needs of healthcare professionals. In states without pharmacy recovery networks, colleges and schools of pharmacy will need to partner with mental health and substance abuse practitioners with the requisite training to provide for the needs of health professions students.
This study has several limitations. Recall bias may have occurred because of the 12-month time period over which students were asked to recall their alcohol use behavior. Also, first-year pharmacy students were asked to recall behaviors during the time they were in undergraduate studies; thus, alcohol use behaviors during undergraduate studies could have been included. Next, social desirability bias may have underestimated the true alcohol use. Given that the survey was anonymous in nature and opaque envelopes were used to return completed survey instruments, this bias may have been reduced. There may have also been differences in alcohol consumption among survey participants, those who refused to participate, and those who were absent from the seminar. Specifically, refusals and absent students may have consumed more alcohol than survey participants, which would have biased the results. It is unclear as to why the response rate among P3 students was lower than that for other classes. Fewer P3 students could have been in attendance or many of them who were in attendance could have chosen not to complete the survey instrument. Given the anonymous nature of the survey, the reason for lower response among the P3 students remains unclear. Lastly, the study was conducted at a single institution, making it difficult to generalize results to all pharmacy students, especially colleges and schools of pharmacy in different environments or other regions of the country.
CONCLUSION
Pharmacy students reported that social motives were the most common reasons for drinking, while coping and enhancement motives were more predictive of hazardous alcohol use. General alcohol education and tailored programs should be implemented in colleges and schools of pharmacy. Use of a standardized questionnaire like the DMQ-R is a simple way for colleges and schools to identify those students who need help and begin a dialogue about the dangers of alcohol abuse the role of pharmacists as health promoters/advocates.
ACKNOWLEDGEMENTS
Preliminary results of this study were presented at the Alabama Public Health Association Conference in Birmingham, AL, in April 2013.
REFERENCES
- 1.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Washington, DC: 2013. Healthy People 2020. [PubMed] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. Results from the 2011 National Survey on Drug Use and Health: summary of national findings, NSDUH Series H-44, HHS Publication No. (SMA) 12-4713. [Google Scholar]
- 3.English C, Rey JA, Schlesselman LS. Prevalence of hazardous alcohol use among pharmacy students at nine US schools of pharmacy. Pharm Pract. 2011;9(3):162–168. [PMC free article] [PubMed] [Google Scholar]
- 4.Jungnickel PW, Desimone EM, Kissack JC, et al. Report of the AACP Special Committee on Substance Abuse and Pharmacy Education. Am J Pharm Educ. 2010;74(10):Article S11. doi: 10.5688/aj7410s11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baldwin JN, Scott DM, DeSimone EM, 2nd, Forrester JH, Fankhauser MP. Substance use attitudes and behaviors at three pharmacy colleges. Subst Abus. 2011;32(1):27–35. doi: 10.1080/08897077.2011.540470. [DOI] [PubMed] [Google Scholar]
- 6.Kenna GA, Wood MD. Substance use by pharmacy and nursing practitioners and students in a northeastern state. Am J Health Syst Pharm. 2004;61(9):921–930. doi: 10.1093/ajhp/61.9.921. [DOI] [PubMed] [Google Scholar]
- 7.Kenna GA, Wood MD. Prevalence of substance use by pharmacists and other health professionals. J Am Pharm Assoc. 2004;44(6):684–693. doi: 10.1331/1544345042467281. [DOI] [PubMed] [Google Scholar]
- 8.Merlo LJ, Cummings SM, Cottler LB. Recovering substance-impaired pharmacists' views regarding occupational risks for addiction. J Am Pharm Assoc. 2012;52(4):480–491. doi: 10.1331/JAPhA.2012.10214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baldwin JN, Scott DM, Agrawal S, et al. Assessment of alcohol and other drug use behaviors in health professions students. Subst Abus. 2006;27(3):27–37. doi: 10.1300/J465v27n03_05. [DOI] [PubMed] [Google Scholar]
- 10.Cooper ML. Motivations for alcohol use among adolescents: development and validation of a four-factor model. Psychol Assess. 1994;6(2):117–128. [Google Scholar]
- 11.Cox WM, Klinger E. A motivational model of alcohol use. J Abnorm Psychol. 1988;97(2):168–180. doi: 10.1037//0021-843x.97.2.168. [DOI] [PubMed] [Google Scholar]
- 12.Stewart SH, Zeitlin SB, Samoluk SB. Examination of a three-dimensional drinking motives questionnaire in a young adult university student sample. Behav Res Ther. 1996;34(1):61–71. doi: 10.1016/0005-7967(95)00036-w. [DOI] [PubMed] [Google Scholar]
- 13.Simons JS, Correia CJ, Carey KB. A comparison of motives for marijuana and alcohol use among experienced users. Addict Behav. 2000;25(1):153–160. doi: 10.1016/s0306-4603(98)00104-x. [DOI] [PubMed] [Google Scholar]
- 14.Park CL, Levenson MR. Drinking to cope among college students: prevalence, preblems, and coping processes. J Stud Alcohol. 2002;63(4):486–497. doi: 10.15288/jsa.2002.63.486. [DOI] [PubMed] [Google Scholar]
- 15.Simons J, Gaher R, Correia C. An affective-motivational model of marijuana and alcohol problems among college students. Psychol Addict Behav. 2005;19(3):326–334. doi: 10.1037/0893-164X.19.3.326. [DOI] [PubMed] [Google Scholar]
- 16.Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clin Psychol Rev. 2005;25(7):841–861. doi: 10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Saunders JB, Aasland OG, Babor TF, De La Fuente KR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 2006;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 18.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The AUDIT, The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. 2nd edition. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 19.Murawski MM, Juergens JP. Analysis of longitudinal pharmacy student alcohol and other drug use survey data. Am J Pharm Educ. 2001;65(Spring):20–29. [Google Scholar]
- 20.Perkins HW. Social norms and the prevention of alcohol misuse in collegiate contexts. J Stud Alcohol Drugs. 2002;14:164–172. doi: 10.15288/jsas.2002.s14.164. [DOI] [PubMed] [Google Scholar]
- 21.Perkins HW, Haines MP, Rice R. Misperceiving the college drinking norm and related problems: a nationwide study of exposure to prevention information, perceived norms and student alcohol misuse. J Stud Alcohol Drugs. 2005;66(4):470–478. doi: 10.15288/jsa.2005.66.470. [DOI] [PubMed] [Google Scholar]
- 22.Brewer RD, Swahn MH. Binge drinking and violence. JAMA. 2005;294(5):616–618. doi: 10.1001/jama.294.5.616. [DOI] [PubMed] [Google Scholar]
- 23.Walters ST, Miller E, Chiauzzi E. Wired for wellness: e-interventions for addressing college drinking. J Subst Abuse Treat. 2005;29(2):139–145. doi: 10.1016/j.jsat.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 24.Carey KB. Brief motivational interventions. In: Correia CJ, Murphy JG, Barnett NP, editors. College Student Alcohol Abuse: A Guide to Assessment, Intervention, and Prevention. Hoboken, NJ: Wiley; 2013. pp. 218–245. [Google Scholar]
- 25.Campbell W, Hester RK. Computerized interventions. In: Correia C, Murphy J, Barnett N, editors. College Student Alcohol Abuse: A Guide to Assessment, Intervention, and Prevention. Hoboken, NJ: Wiley; 2013. pp. 246–267. [Google Scholar]
- 26.Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief Alcohol Screening and Intervention for College Students: A Harm Reduction Approach. New York: Guilford Press; 1999. [Google Scholar]


