Abstract
Objective. To compare the accuracy of medication lists obtained by student pharmacists, nurses, and physicians, and quantify the number of discrepancies identified as part of the medication reconciliation process.
Methods. Between May and July 2012, patients admitted to an internal medicine team at a 350-bed tertiary academic medical center were assessed for inclusion in the study. Physicians and/or nurses conducted medication reviews for these patients at the time of admission, while student pharmacists conducted medication reconciliation.
Results. Eighty-six patients were assessed, and 52 met all inclusion criteria. A total of 268 discrepancies were identified as part of the medication reconciliation performed by the student pharmacists, approximating 5 discrepancies per patient (range 0-13). Student pharmacists identified 532 preadmission medications, significantly more than did nurses (355) or physicians (368), p=0.006.
Conclusion. Student pharmacists, with appropriate oversight, can be used in several tasks that previously may have been designated to pharmacists only, such as medication reconciliation.
Keywords: medication reconciliation, pharmacy, student pharmacist
INTRODUCTION
An extensive body of published literature exists on the importance of medication reconciliation within the hospital setting, including the 2013 National Patient Safety Goals put forth by The Joint Commission.1 Additionally, several studies have reported that high-quality medication reconciliation improves the overall care provided to hospitalized patients.2-5 Up to a quarter of all prescription medications taken by patients prior to admission are not accurately recorded within the medical record.4 Patients who are taking 7 or more medications are more likely to experience 1 or more medication-related discrepancies.6 These discrepancies have been categorized as omission of prescription or nonprescription medications; differing dosage form, dose, or route recorded; and/or therapeutic substitutions; among others. Furthermore, the impact of these discrepancies can be great, with up to 40% of noted discrepancies having the potential to cause “moderate to severe” patient discomfort and/or a decline in patient clinical status.2
Aside from the literature regarding the impact of pharmacists in providing medication reconciliation, 3 publications have evaluated the impact of student pharmacists in providing medication reconciliation services at community hospitals.6-8 Lubowski and colleagues demonstrated that, when student pharmacists performed medication reconciliation in over 300 patients, approximately 1000 discrepancies were identified.6 These discrepancies largely consisted of omitted prescription medications. Furthermore, Lubowski and colleagues demonstrated that discrepancies were directly associated with the number of medications patients were taking prior to admission. From this study the authors determined that patients whose admission medication list included 1 or more discrepancies contained on average 8±4 medications as compared with 5±4 medications for patients whose lists did not have discrepancies (p=0.05).6 Pardiyara demonstrated similar outcomes in her study in which student pharmacists identified approximately 3 discrepancies per patient, with a similar number of omissions as identified in the study by Lubowski.7 Walker and colleagues evaluated the impact that student pharmacists can have on clinical interventions within a transition of care setting, with results similar to those from the other studies noted.8 These studies show that student pharmacists can have a positive impact on patient care that is similar to that of licensed pharmacists. As the role of student pharmacists continues to expand, particularly as part of their clinical advanced pharmacy practice experiences, they are being asked to participate in a number of patient care areas previously limited to pharmacists, including medication reconciliation. It is important for pharmacy educators to provide students with appropriate activities that not only ensure they receive high impact, meaningful, experiences as part of their training, but also positively impact patient care.
A thorough literature search failed to identify any studies evaluating the accuracy of admission medication lists obtained by pharmacy students as part of a medication reconciliation process compared to those lists obtained by nurses and physicians. Thus, pharmacy faculty members at Northeastern University and Massachusetts College of Pharmacy and Health Sciences University undertook a study to evaluate the role of student pharmacists within the medication reconciliation process and to compare the accuracy of the medication list obtained by student pharmacists with that of nurses and physicians caring for the same patients. The objectives of this study were to: (1) compare and contrast the accuracy of medication lists obtained by student pharmacists with those obtained by nurses and physicians for inpatients admitted to a tertiary academic medical center, and (2) categorize and quantify the type and nature of any interventions made as a result of performing medication reconciliation.
METHODS
This study was exempted by the Lahey Hospital & Medical Center Institutional Review Board. During a 12-week period between May and July 2012, consecutive patients admitted to 1 of 4 inpatient internal medicine teams at the Lahey Hospital & Medical Center, a 350-bed tertiary academic medical facility in Burlington, Massachusetts, were assessed for inclusion in this study. Patients were included if they were English-speaking, aged 18 years or older, had a primary care provider affiliated with our institution, and were admitted from a non-institutional place of residence within the United States. Patients were included only if they were taking 7 or more medications at the time of admission, and/or had at least 1 of the following health conditions documented in their medical record: arrhythmia, asthma, coronary artery disease, chronic obstruction pulmonary disease, diabetes mellitus, drug/alcohol abuse, end stage renal disease, gastrointestinal bleeding, heart failure, myocardial infarction, pancreatitis, stroke, syncope, and/or venous thromboembolism. The requirement that patients were taking at least 7 medications and/or had one of the specified conditions was adapted from previously published literature and preexisting hospital criteria for high-risk medical conditions as these patients were most at risk for medication errors.6 Only patients admitted to the hospital from non-institutional settings were included because accurate medication lists are typically readily available for patients coming from these facilities. Exclusion criteria included: (1) admission duration anticipated to be less than 24 hours; (2) limitation of care or death within 24 hours of admission; or (3) unresponsive and/or noncommunicative.
Using a computer-generated list, student pharmacists completing a 6-week (Monday through Friday) APPE at this institution evaluated patients admitted to 1 of the hospital’s inpatient general medicine teams for eligibility. Student pharmacists were trained by their preceptor, a pharmacy practice faculty member with an active practice site at the institution, to conduct patient interviews and obtain detailed medication histories. The students assessed each patient for inclusion in the study within 72 hours of admission. If the patient met the inclusion criteria, the student performed medication reconciliation. Medication reconciliation, for the purposes of this study, was defined as reviewing the preadmission medication list(s) obtained by the nurse and/or medical provider, interviewing the patient and/or designated healthcare proxy, and contacting the appropriate outpatient pharmacy(ies) to obtain the most accurate preadmission medication list. All patients, regardless of their inclusion in this study, had standard-of-care medication reconciliation performed by the hospital nursing and medical staff as part of their admission to the institution. When obtaining home medication lists, nurses and physicians used their judgment to determine how to interview patients and the best sources of information to identify home medications, eg, patient or family members, drug bottles or medication lists brought from home, the patient’s pharmacist or physicians.
Any discrepancies between the nurse- and physician-obtained medication lists were discussed directly with the pharmacist preceptor prior to presentation to the medical provider(s) caring for the patient. Discrepancies were defined as any deviation between the student pharmacist-obtained admission medication list and that obtained by the nurses and/or physicians, including omissions and transcription errors. A discrepancy was classified as an omission if a medication was not included within the nurse or physician-obtained medication reconciliation list, either in whole or in part (eg, omission of dosage form, route, strength, or frequency). Any newly started medication(s) related to admission were excluded from this count. Additionally, students were responsible for reviewing the complete medication list, including newly initiated medications, and for making appropriate recommendations after consultation with their preceptor. Drug-related problems, or interventions, were categorized using the ranking system developed by Hatoum and colleagues.9
A one-way analysis of variance (ANOVA) was used to identify significant differences in the number of medications identified by nurses, physicians, and student pharmacists. A p value of less than or equal to 0.05 was considered significant. Statistical analysis was performed using SPSS, version 18 (SPSS Inc, Chicago, IL).
RESULTS
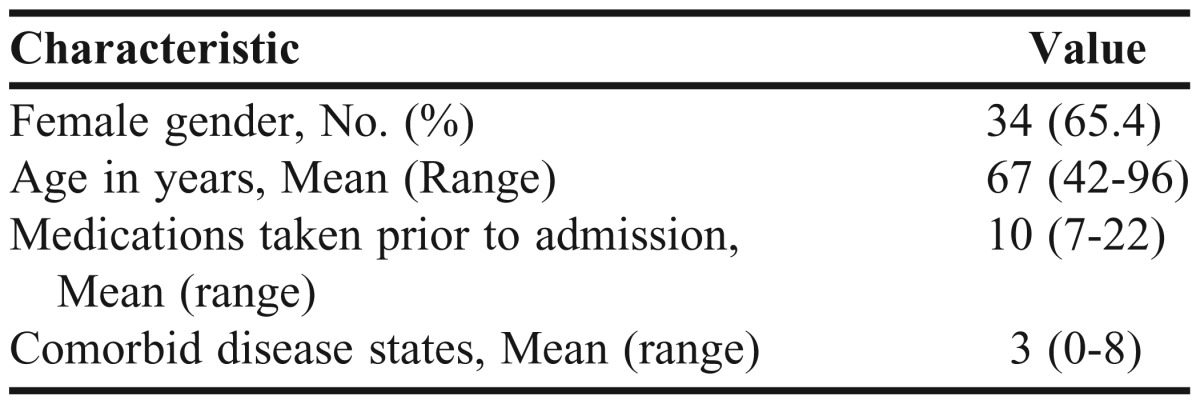
Over the course of two 6-week APPEs, 8 student pharmacists participated in this study. During the 3-month time period, 86 patients were assessed, and 52 met all inclusion criteria. The most common reason for exclusion from the study were: patients taking less than 7 medications prior to admission, 43 (50%); admission from an institutional place of residence, 20 (23.3%); and/or admission lasting less than 24 hours, 18 (20.9%). Table 1 details the patient demographics for those meeting inclusion criteria for this study. The patient population was largely comprised of elderly patients with several comorbid disease states who were taking a large number of medications prior to admission.
Table 1.
Demographics of Patients Enrolled in a Study to Compare the Accuracy of Medication Lists Obtained by Students Pharmacists With That Obtained by Nurses and Physicians
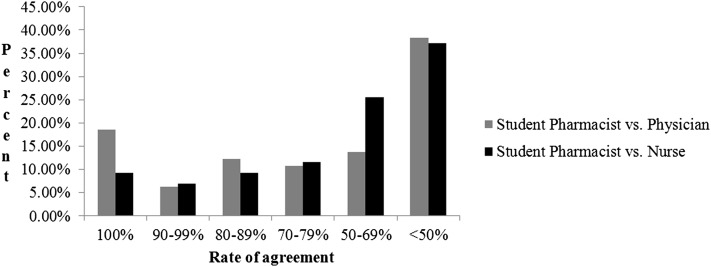
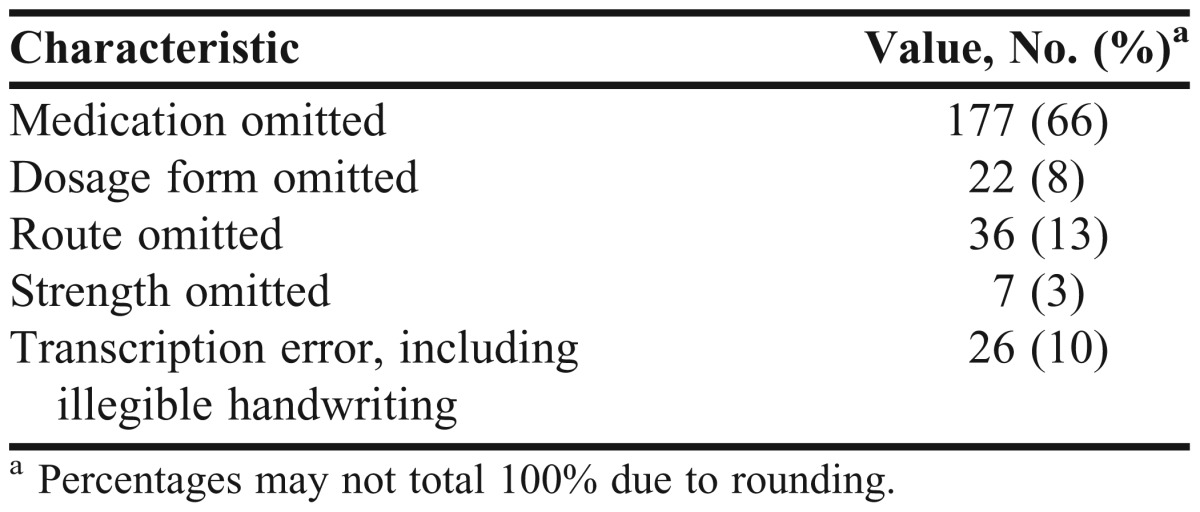
When student pharmacists’ medication lists were compared to medication lists obtained by nurses or physicians, 268 discrepancies were identified. On average, 5 discrepancies were identified per patient; however, the number of discrepancies per patient ranged from 0 to 13. Figure 1 illustrates the level of agreement between the 3 medication lists obtained. Wide discrepancies were found between the medication lists obtained by the student pharmacists and those compiled by the nurses and physicians. However, the physician and nurses performed similarly to one another in terms of total medications identified during the medication reconciliation process. Only in 20% of the cases was there 100% agreement among all 3 medication lists; the average agreement rate among the lists was 57.6%. Ninety percent of all discrepancies were related to complete medication omission or omission of dosage form, strength, and/or frequency (Table 2).
Figure 1.
Percent agreement between medication lists obtained by student pharmacists, nurses, and physicians.
Table 2.
Description of Discrepancies Identified by Student Pharmacists
Student pharmacists identified 532 prescription and nonprescription medications during medication reconciliation compared with 355 identified by nurses and 368 identified by physicians. Student pharmacists also identified significantly more medications per patient (10.2) as compared with nurses (6.8) and physicians (7.1), p=0.006. Of the medications identified by student pharmacists that were not identified by nurses and/or physicians, 68% (N=105) were nonprescription medications.
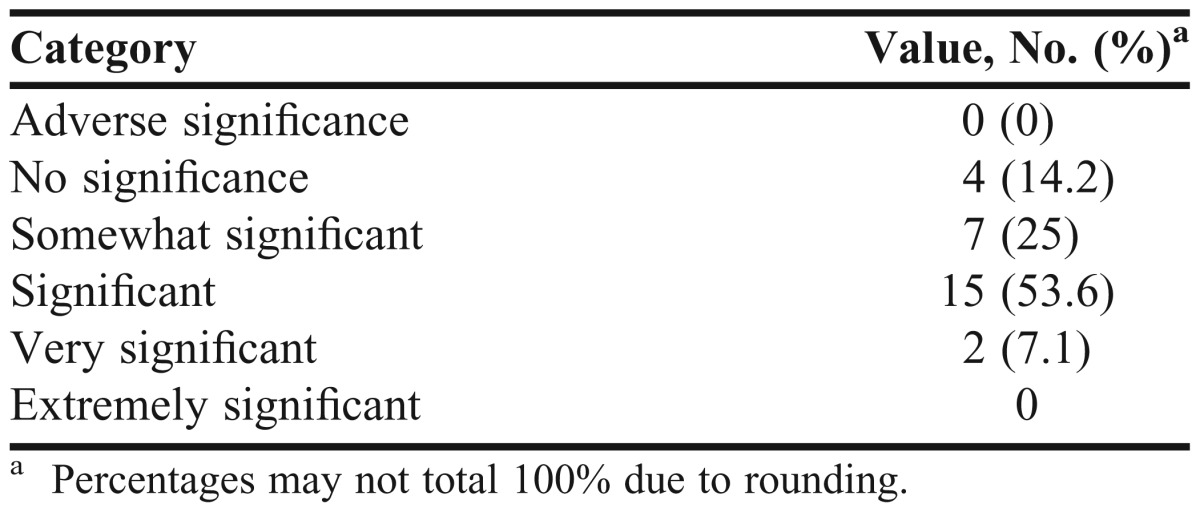
A total of 28 interventions in 18 patients were recorded during the study period. Table 3 delineates the results of the student interventions. More than 50% of the student interventions were significant, meaning that they would “bring care to a more acceptable and appropriate level” as previously defined by Hatoum and colleagues.9
Table 3.
Assessed Importance of Student Pharmacists’ Intervention
DISCUSSION
The role of the pharmacist within the medication reconciliation process has been explored by others, with Mergenhagen and colleagues demonstrating the superiority of pharmacist-performed medication reconciliation compared to physician-performed medication reconciliation.9 The results of our study demonstrate the important role that student pharmacists can have in performing medication reconciliation, especially for hospitalized patients.
Many of the reported medication list discrepancies identified by the student pharmacists were based on recognition of nonprescription medications that were not listed as part of the patients’ admission medication lists compiled by nurses and physicians. This runs counter to previous publications by Lubowski and colleagues, where a majority of noted discrepancies were related to prescription medications.6 This discrepancy may have occurred if nurses and physicians in this study focused on documenting comprehensive prescription drug medication lists but placed less emphasis on obtaining thorough histories of nonprescription product use. Inclusion of nonprescription medications can be critical in complicated clinical situations and may assist in the identification and management of conditions that occur secondary to their use. Pharmacists and student pharmacists are uniquely trained to comprehensively identify all home medications, including nonprescription products. Regardless of the classification of medication, our study and others have consistently demonstrated the positive impact pharmacists and student pharmacists have on providing the most accurate and complete medication list possible for hospitalized patients. Notably, half of the interventions made as a result of the student pharmacists’ medication reconciliation were considered to be significant.
Our study has some limitations. The nurses and physicians in this study did not receive formal training on how to obtain a medication history and did not follow a uniform method for interviewing patients. The number of different physicians and nurses who obtained medication lists for the patients included in this study cannot be determined, but many more nurses and physicians were involved than student pharmacists. This lack of formalized training coupled with the variability in the methods the nurses and physicians used to obtain the medication list may limit the external validity of our findings for institutions where nurses and physicians receive comprehensive training in obtaining medication histories. We did not evaluate to what degree the identification of these discrepancies impacted care, nor whether the medical providers altered the patient medication lists based on the identified medication discrepancies. Nonetheless, we do not feel that the absence of this data lessens the impact of our study given that a majority of the omitted medications were nonprescription products, which may not have been continued as part of the regular care for patients admitted to our institution.
There are several differences between our study and others reported in the literature; namely, our study included subjects who were taking 7 or more medications prior to admission, whereas Lubowski and colleagues did not specify a minimum number of medications as part of their inclusion criteria.3,6-8,10 However, Gleason and and Lubowski both identified that, for patients taking 7 or more medications prior to admission, the total number of discrepancies was higher than for those patients taking 6 or less medications.3,6 Furthermore, several authors have published data comparing the accuracy of medication lists obtained by student pharmacists to physicians, or pharmacists to physicians, whereas our study compared lists obtained by student pharmacists vs those obtained by nurses and/or physicians.6,7,10,11
Given the emphasis and clinical impact of accurate admission medication histories and these data showing that student pharmacists more consistently document complete medication lists as compared with nurses and physicians, institutional APPE sites and colleges and schools of pharmacy may have added interest in developing APPEs that use student pharmacists in this role. In addition to the patient care benefits, institutions could satisfy some Joint Commission and other regulatory needs by using student pharmacists for medication reconciliation. Student pharmacists gain meaningful skills interviewing patients, critically evaluating medication lists, and working with multidisciplinary teams through these efforts. Perhaps limited roles for student pharmacists in earlier professional years could be explored in properly structured, selected situations so that they could also assist with medication reconciliation and develop key skills.
While our data demonstrate the positive impact student pharmacists can have on the delivery of care relative to medication reconciliation for hospitalized patients, these findings should not be seen as a recommendation to remove the pharmacist from this process. One of the important factors of any medication reconciliation program is the ability to provide such a program on an ongoing basis; thus, involvement of a variety of pharmacy personnel may be appropriate.
CONCLUSIONS
This study demonstrates an expanded role for student pharmacists within the delivery of healthcare as medication reconciliation specialists. Student pharmacists, with appropriate oversight, can be used to complete this and other tasks that previously may have been designated only for pharmacists. Pharmacy educators and those involved in the training of student pharmacists within advanced practice experiences should develop opportunities to fully involve student pharmacists in these types of activities, as high-quality medication reconciliation positively impacts patient care, provides benefits to the experiential site, and provides a strong learning experience for the student.
REFERENCES
- 1.Joint Commission on Accreditation of Healthcare Organizations. 2014 hospitals’ national patient safety goals. http://www.jointcommission.org/standards_information/npsgs.aspx. Accessed January 28, 2014. [PubMed]
- 2.Cornish PL, Knowles SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165(4):424–429. doi: 10.1001/archinte.165.4.424. [DOI] [PubMed] [Google Scholar]
- 3.Gleason KM, Groszek JM, Sullivan C, Rooney D, Barnard C, Noskin GA. Reconciliation of discrepancies in medication histories and admission orders of newly hospitalized patients. Am J Health-Syst Pharm. 2004;61(16):1689–1695. doi: 10.1093/ajhp/61.16.1689. [DOI] [PubMed] [Google Scholar]
- 4.Lau HS, Florax C, Porsius AJ, De Boer A. The completeness of medication histories in hospital medical records of patients admitted to general internal medicine wards. Br J Clin Pharmacol. 2000;49(6):597–603. doi: 10.1046/j.1365-2125.2000.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pippins JR, Gandhi TK, Hamann C, et al. Classifying and predicting errors of inpatient medication reconciliation. J Gen Intern Med. 2008;23(9):1414–1422. doi: 10.1007/s11606-008-0687-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lubowski TJ, Cronin LM, Pavelka RW, Briscoe-Dwyer LA, Briceland LL, Hamilton RA. Effectiveness of a medication reconciliation project conducted by PharmD students. Am J Pharm Educ. 2007;71(5):Article 94. doi: 10.5688/aj710594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Padiyara RS. Student pharmacists and medication reconciliation upon hospital admission: proposing a way to meet ASHP 2015 objective 1.1. J Am Pharm Assoc (2003) 2008;48(6):701. doi: 10.1331/japha.2008.08106. [DOI] [PubMed] [Google Scholar]
- 8.Walker PC, Tucker Jones JN, Mason NA. An advanced pharmacy practice experience in translational care. Am J Pharm Educ. 2010;74(2):Article 20. doi: 10.5688/aj740220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hatoum HT, Hutchinson RA, Witte KW, Newby GP. Evaluation of the contribution of clinical pharmacists: inpatient care and cost reduction. Drug Intell Clin Pharm. 1988;22(3):252–259. doi: 10.1177/106002808802200318. [DOI] [PubMed] [Google Scholar]
- 10.Mergenhagen KA, Blum SS, Kugler A, et al. Pharmacist- versus physician-initiated admission medication reconciliation: impact on adverse drug events. Am J Geriatr Pharmacother. 2012;10(4):242–250. doi: 10.1016/j.amjopharm.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Nester TM, Hale LS. Effectiveness of a pharmacist-acquired medication history in promoting patient safety. Am J Health-Syst Pharm. 2002;59(22):2221–2225. doi: 10.1093/ajhp/59.22.2221. [DOI] [PubMed] [Google Scholar]