Abstract
Pertussis toxin from the gram-negative bacterium Bordetella pertussis is an ADP-ribosylase that modifies Gi proteins in mammalian lymphocytes and inhibits their capacity to traffic from blood into lymphoid tissues. We used this compound to induce lymphocytosis in rhesus macaques and to study its effects on SIV infection. Pertussis toxin injected at 25 μg/kg induced a transient lymphocytosis that peaked 3–8 days after administration and caused a rapid, transient decrease in the frequency of infectious cells in blood as judged by in vitro virus isolation assays. Lymphocyte subsets were altered during the lymphocytosis interval and sustained changes in CD8+ T cell levels were noted as long as 53 days after pertussis toxin injection. In situ hybridization studies showed that pertussis toxin altered the distribution of viral RNA in lymph nodes during the interval of lymphocytosis, and caused long-term changes with decreased virus replication in some tissue specimens.
Introduction
Lymphoid organs including spleen, lymph nodes, thymus and mucosal-associated lymphoid tissues are primary sites for infection with human immunodeficiency virus type 1 (HIV-1) in humans1–5 and for simian immunodeficiency virus in nonhuman primates.6,7 Chronic SIV or HIV-1 infection promotes the conversion in lymphoid tissues from follicular hyperplasia to follicular involution; these changes are associated with functional loss of primary and memory immune responses (reviewed in Refs. 8 and 9). The highly organized architecture, conjunction of blood and lymph circulation, and specific cell-trafficking mechanisms are unique features of lymph nodes that both generate immune responses and support active HIV-1 or SIV replication. We are using a bacterial toxin that modifies heterotrimeric G proteins in an effort to assess how lymphocyte functions controlled by these regulatory molecules might be affecting viral pathogenesis. In this article our goal is to assess the effects of this toxin on virus replication and lymphocyte distribution in SIV-infected rhesus macaques.
The pertussis toxin (PTx) is a surface protein of Bordetella pertussis and the causative agent for lymphocytosis in children with whooping cough.10 The PTx binds to mammalian cells and modifies G proteins via an ADP-ribosylation activity.11 In murine models, low doses of intraperitoneal pertussis toxin induced a prominent lymphocytosis.12 Increased peripheral blood lymphocyte counts were attributed to PTx inhibition of lymphocyte extravasation across the endothelium and were not due to accelerated rates of cell exit from lymphoid tissues or increased levels of new cell synthesis.13 Pertussis toxin-treated lymphocytes leave lymph nodes in normal numbers and subsequently accumulate in blood because of a block in the pathway for returning to lymphoid tissues. It is also known from rodent model experiments that cells treated ex vivo with PTx fail to enter lymphoid tissues when reinjected into the animal and that enzymatically active pertussis toxin is required to affect lymphocyte distribution.9
Murine lymphocytes treated ex vivo with pertussis toxin retained the ability to roll along endothelial surfaces but failed to engage in the firm attachment process necessary for extravasation.14 Pertussis toxin treatment also prevented calcium changes normally associated with binding to the N-formyl peptide receptor on neutrophils.15 Both of these effects required enzymatically active pertussis toxin that could modify Gi proteins16 and it was assumed that interference with cell surface receptor activity was key to changing lymphocyte and neutrophil phenotypes. More recently, studies of HIV infection in vitro implicated chemokine receptors17,18 and cell surface fusin molecules19 as accessory factors for virus entry. These cell surface molecules believed to be coreceptors for HIV-1 entry and membrane fusion are known to be G protein-coupled receptors and are, thus, targets for pertussis toxin inactivation. Another G protein-coupled receptor for tumor necrosis factor α (TNF-α) was implicated as part of the mechanism explaining an inhibitory effect of pertussis toxin on HIV replication in the U.1 latently infected cell line.16 The increasing relationship between G protein-coupled cell surface receptors and HIV-1 replication encourages exploration of drugs, such as pertussis toxin, that might interfere with these aspects of the virus life cycle.
Materials and Methods
Animals and virus infection
Male rhesus macaques were selected from the Wisconsin Regional Primate Research Center (Madison, WI) breeding colony; all animals were 3 to 4 years old when the pertussis toxin study was initiated. The animals were enrolled previously in studies of virus transmission or pathogenesis and were infected with SIV (SIVmac251 biological isolate kindly provided by R. C. Desrosiers, New England Primate Research Center, Southborough, MA). Animals 90019 and 90047 had a chronic infection after intrarectal inoculation for 2 years prior to PTx injection. Animals 90054, 90061, and 90072 were infected by intravenous injection of SIV 4 months prior to PTx treatment. Animals 90100 and 90090 were inoculated intravenously 3 months prior to study and did not receive pertussis toxin injections.
SIV viral DNA levels
Quantitative polymerase chain reaction assays to detect viral long terminal repeat (LTR) were described previously for HIV-1.20 Oligonucleotide primers and reaction conditions for detecting SIV LTR DNA were described previously.21
Titration of virus and infectious cell numbers
Monkey peripheral blood mononuclear cells (PBMCs) were purified by Ficoll-Hypaque density gradients and stimulated overnight with phytohemagglutinin (PHA-M; GIBCO-BRL, Gaithersburg, MD). Serial 10-fold dilutions of PBMCs, beginning with 106 cells, were mixed with 2×105 CEM×174 cells; cultures were examined every 3 to 4 days for up to 30 days, and fresh medium and CEM×174 cells were added when necessary. The presence of virus was confirmed by cytopathic effects in the culture, by reverse transcriptase assay (Boehringer GmbH, Mannheim, Germany), and by p27 antigen capture assay (Coulter, Hialeah, FL). PBMC samples with less than 1 infectious cell in 106 PBMCs were considered negative.
Pertussis toxin administration
We determined previously21a that leukocytosis was induced in uninfected juvenile rhesus monkeys by intravenous injection of PTx (25 μg/kg). Sterile, lyophilized toxin (List Biological Laboratories, Inc., Campbell, CA) was aseptically reconstituted with injectable sterile water (Abbott Laboratories, North Chicago, IL) to a final concentration of 100 μg/ml. Toxin was injected into the saphenous vein of each animal at the rate of approximately 1 ml/min. The site of injection was observed for injury on the day of injection and for the following 2 weeks. There were no signs of local inflammation or necrosis at the site of injection.
Hematology data
Complete blood counts were performed by a commercial clinical laboratory (General Medical Laboratories, Madison, WI) starting with 2 ml of blood collected in EDTA-anticoagulant tubes. In addition to automated analysis, smear slides were prepared and checked routinely by the authors to confirm changes in leukocyte subpopulations.
Flow cytometry
The percentages of CD2+, CD4+, CD8+, and CD20+ cells in PBMCs were determined by flow cytometry using Lysys II software on a FACScan flow cytometer (Becton Dickinson, San Jose, CA). Purified PBMCs were pelleted by low-speed centrifugation and washed with phosphate-buffered saline before further treatment with 1% paraformaldehyde for 30 min at room temperature, followed by blocking and washing to remove the paraformaldehyde. Cells were incubated with antibodies (generally 5 μl/106 cells) for 30 min at 4°C. All stainings were direct. Phycoerythrin-conjugated anti-CD4, -CD8, and -CD2 (pan T cell marker) were purchased from Antigenix America, Inc. (Franklin Square, NY). Fluorescein-conjugated anti-CD20 (B cell marker) was purchased from Becton Dickinson. Labeled isotype controls were included in each flow cytometry experiment.
In situ hybridization for viral RNA
Lymph node biopsies were fixed in buffered formaldehyde for 5 hr, then embedded in 60°C paraffin. Sectioning and in situ hybridization were performed by Molecular Histology, Inc. (Gaithersburg, MD). The sections were treated with protease and then hybridized with radiolabeled antisense gag-specific probes. The sections were photographed with epifluorescent light. Control specimens were routinely negative when hybridized with sense-strand gag-specific probes.
Results
Clinical observations after pertussis toxin treatment
Five SIV-infected rhesus monkeys were injected, each with 25 μg of pertussis toxin per kilogram. Transiently elevated liver enzymes and reduced serum iron levels were noted in clinical chemistries (not shown); these changes were similar in magnitude and duration to those noted previously for uninfected rhesus macaques.21a Daily observations of animals showed no obvious changes in behavior, feeding pattern, appearance of stools, fluid intake, or urine output. All animals gained weight subsequent to pertussis toxin injection at the rates expected for age- and sex-matched rhesus macaques. There were no signs of local inflammation or necrosis at the site of injection. Intravenous PTx injection (25 μg/kg) appears relatively safe for investigations in either uninfected or SIV-infected rhesus macaques in the sense that exotic precautions or supportive treatments were not required.
Lymphocytosis induced by pertussis toxin
The temporal pattern of increasing lymphocyte count (Fig. 1) was consistent among five SIV-infected, PTx-treated animals, with maximum levels occurring on day 3 after injection. The mean increase in absolute lymphocyte count was 26,490 cells/μl of blood (range, 16,203 to 43,329 cells/μl) or 9.1 times (range, from 20.2 to 3.7 times). The magnitude of increased lymphocyte counts for all SIV-infected, PTx-injected animals exceeded the mean for uninfected rhesus of 4.2 times.21a The total white blood cell count was linearly related to the absolute lymphocyte count in blood at all times before and after PTx treatment (correlation coefficient 0.88). There were no significant correlations between lymphocyte count and absolute numbers of metamyelocytes or monocytes in peripheral blood.
FIG. 1.
Absolute lymphocyte counts in peripheral blood from SIV-infected animals after pertussis toxin injection. Lymphocyte counts were obtained by automated analysis of venous blood samples collected in EDTA-anticoagulant tubes; data are represented as lymphocytes per microliter of whole blood. The time scale indicates the day of toxin administration as day 0. Negative time values are samples prior to pertussis toxin treatment. Bars indicate the standard error of the mean.
Flow cytometry was used to quantitate the CD4+ lymphocyte subset in four of the PTx-treated animals and two untreated controls (Table 1). The CD4+ cell count increased from a mean of 913 cells/μl in blood to a mean of 5451 cells/μl, using the peak levels for each animal (a mean increase of 7.6 times). Maximum levels of total blood lymphocytes were reached on day 3 after PTx injection, in contrast to maximum levels of CD4+ cells being reached by 14 days after PTx injection. Despite the delayed pattern for increased blood count of CD4+ cells, the mean increase was 7.6 times compared to the 9.1 times increase in total lymphocyte count after PTx injection. By 53 days after PTx injection, the CD4+ cell count in blood was slightly higher than starting levels (1156 CD4+ cells/μl on day 53 compared to 913 cells/μl on day 0). The differences between CD4+ cell increases and total lymphocyte increases are partially explained by the rapid increases in CD8+ cells after PTx injection (Table 1). The maximum levels of CD8+ cells were reached by day 2 or 7 after PTx injection and the mean increase (for the maximum level) was 9966 cells/μl (range, from 12,828 cells/μl to 8148 cells/μl increase) and the mean increase in CD8+ cells was 9.0 times. There were no consistent changes in CD20+ B cells in SIV-infected, PTx-treated animals. The percentages of CD4+ cells were relatively constant over a similar sampling interval in untreated rhesus (not shown).
Table 1.
Lymphocyte Subpopulations in Peripheral Blood Mononuclear Cells from Animals before and after Pertussis Toxin Treatment
| Animal No. | Days after PTx treatment | % CD2+ | % CD4+ (cells/μl) | % CD8+ (cells/μl) | % CD20+ | % CD4+% CD8 |
|---|---|---|---|---|---|---|
| 90054 | (0) | 61 | 22 (472) | 38 (815) | 41 | 0.58 |
| 90054 | (2) | nd | 14 (5,056) | 24 (8,670) | 37 | 0.58 |
| 90054 | (7) | 81.4 | 13 (4,345) | 30 (10,027) | 11 | 0.43 |
| 90054 | (14) | 85 | 35 (7,739) | 32 (7,075) | 15 | 1.1 |
| 90054 | (28) | 82 | 6.5 (677) | 57 (5,937) | 17 | 0.11 |
| 90054 | (53) | 70 | 7.7 (418) | 49 (2,660) | 27 | 0.16 |
| 90061 | (0) | 68 | 31 (1,488) | 32 (1,536) | 38 | 0.97 |
| 90061 | (2) | nd | 30 (4,836) | 32 (5,159) | 29 | 0.94 |
| 90061 | (7) | 76.4 | 18 (3,195) | 35 (6,213) | 17 | 0.51 |
| 90061 | (14) | 81 | 38 (6,384) | 35 (5,880) | 20 | 1.1 |
| 90061 | (28) | 64 | 15 (1,669) | 48 (5,339) | 22 | 0.31 |
| 90061 | (53) | 62 | 14 (932) | 53 (3,528) | 30 | 0.26 |
| 90072 | (0) | 81 | 36 (1,047) | 47 (1,366) | 30 | 0.77 |
| 90072 | (2) | nd | 24 (6,680) | 51 (14,194) | 18 | 0.47 |
| 90072 | (7) | 83.3 | 15 (2,402) | 35 (5,605) | 14 | 0.43 |
| 90072 | (14) | 89 | 29 (3,989) | 44 (6,052) | 8.8 | 0.66 |
| 90072 | (28) | 82 | 8.1 (973) | 63 (4,226) | 16 | 0.23 |
| 90072 | (53) | 81 | 8.8 (707) | 65 (3,315) | 16 | 0.21 |
| 90047 | (0) | nd | 32 (645) | 33 (665) | nd | 1.0 |
| 90047 | (2) | nd | 19 (4,651) | 36 (8,813) | nd | 0.53 |
| 90047 | (7) | nd | 11 (1,694) | 35 (5,390) | nd | 0.31 |
| 90047 | (14) | nd | 31 (2,567) | 42 (3,478) | nd | 0.74 |
| 90019a | (0) | nd | 33 | 35 | nd | 0.94 |
| 90019a | (7) | nd | 34 | 31 | nd | 1.1 |
| 90019a | (28) | nd | 26 | 25 | nd | 1.0 |
| 90100a | (0) | nd | 52 | 22 | nd | 2.4 |
| 90100a | (7) | nd | 48 | 23 | nd | 2.1 |
| 90100a | (28) | nd | 44 | 25 | nd | 1.8 |
SIV-infected animals that did not receive pertussis toxin.
Abbreviations: nd, not determined.
Peripheral blood virus load and antibody levels after pertussis toxin treatment
We measured the minimum number of PBMCs required for detection of virus in vitro and expressed these data as the number of infectious cells in 106 PBMCs (Fig. 2). The responses of individual animals were distinct. The largest consistent changes in frequency of infectious cells were noted for animals 90019, 90061, and 90047. Lesser changes were noted for animals 90072 and 90054. In the case of animal 90072, the virus isolation assay at days 2 and 7 were negative before rising sharply to the value of 1000 infectious cells in 106 PBMCs by 14 days after PTx injection. The profile for animal 90054 showed a drop for infectious cell frequency between day 0 and day 7 (the day 14 assay was not performed owing to poor cell recovery); however, the overall pattern for this animal may be consistent with poor response to PTx injection. For two blood samples prior to PTx injection, an average of 441 infectious cells were present in 106 PBMCs. The greatest change for frequency of infectious cells in PBMCs was noted at 7 days after PTx injection (4 infectious cells in 106 PBMCs). This time point is after the peak of lymphocytosis but just prior to the maximum increase in CD4+ cells. For two blood samples after the interval of lymphocytosis (days 28 and 53), an average of 32 infectious cells were present in 106 PBMCs. This represents a 14 times decrease in the frequency of infectious mononuclear cells in peripheral blood by 1 to 2 months after a single injection of PTx compared to the average values for two pretreatment time points. Samples from untreated, SIV-infected rhesus macaques showed either an increasing frequency of infectious cells (in the rapidly progressing, animal 90090, which survived for 4 months after intravenous SIV inoculation) or changes of ≤10 times for animal 90100, which survived 11.5 months after SIV inoculation.
FIG. 2.

Infectious cell assay with PBMCs from pertussis toxin-treated, SIVmac-infected rhesus monkeys. The minimum number of PBMCs required for positive virus isolation in vitro is indicated at the left. Mitogen-stimulated PBMCs were co-cultured with CEM×174 cells for a maximum of 30 days. Infection was confirmed by the appearance of viral cytopathic effects or accumulation of reverse transcriptase activity in cell-free culture fluids. The day of pertussis toxin administration is indicated as day 0; negative time values are for samples prior to toxin administration. (A) Data for SIV-infected pertussis toxin-treated animals. (B) Similar time course for SIV-infected, untreated animals.
In vitro experiments have not demonstrated PTx inhibition of exogenous or endogenous SIV replication. These experiments tested PTx concentrations up to 2.5 μg/ml using CEM×174 cells infected in vitro with SIV, or using mitogen-stimulated PBMCs from uninfected animals that were infected in vitro with SIV, or using mitogen-stimulated PBMCs from SIV-infected rhesus (not shown). We estimate the final concentration of PTx in the rhesus monkey to be approximately 0.15 μg/ml (assuming a blood volume of approximately 650 ml). The half-life of the drug after intravenous injection has not been established. Overall, the amounts we used in vivo are well within the range we tested in vitro for direct affects on virus replication.
Viral DNA load in peripheral blood mononuclear cells after pertussis toxin treatment
Quantitative polymerase chain reaction assays were used to measure the number of SIV long terminal repeat (LTR) copies in DNA samples extracted from PBMCs. The copies of SIV DNA per CD4+ cell were calculated using the content of viral DNA in 250 ng of template DNA and the known proportion of CD4+ cells in PBMC samples. There were no distinct correlations for the numbers of CD4+ cells in blood and either total viral DNA copies in PBMCs or viral DNA copies per CD4+ cell (Table 2). A pattern of increased viral DNA copies per CD4+ cell was noted in animals treated with pertussis toxin. There was no comparable change in untreated, SIV-infected animals.
Table 2.
Viral DNA in CD4+ Lymphocytes from Peripheral Blood before and after Pertussis Toxin Treatment
| Animal No. | Days after PTx treatment | SIV copies in 250 ng DNA | SIV copies/CD4+ cell |
|---|---|---|---|
| 90054 | (0) | 9,000 | 0.41 |
| 90054 | (2) | 11,250 | 0.80 |
| 90054 | (7) | 2,100 | 0.16 |
| 90054 | (14) | 3,300 | 0.09 |
| 90061 | (0) | 150 | 0.005 |
| 90061 | (2) | 450 | 0.018 |
| 90061 | (7) | 1,200 | 0.07 |
| 90061 | (14) | 1,350 | 0.04 |
| 90072 | (0) | 900 | 0.025 |
| 90072 | (2) | 450 | 0.019 |
| 90072 | (7) | 1,350 | 0.09 |
| 90072 | (14) | 1,500 | 0.05 |
| 90047 | (0) | 11,550 | 0.36 |
| 90047 | (2) | 9,450 | 0.50 |
| 90047 | (7) | 1,800 | 0.16 |
| 90047 | (14) | 1,800 | 0.16 |
| 90019a | (0) | 8,450 | 0.26 |
| 90019a | (2) | nd | nd |
| 90019a | (7) | 9,300 | 0.27 |
| 90019a | (14) | 14,300 | 0.55 |
| 90100a | (0) | 3,300 | 0.06 |
| 90100a | (2) | nd | nd |
| 90100a | (7) | 2,700 | 0.06 |
| 90100a | (14) | 1,900 | 0.04 |
SIV-infected animals that did not receive pertussis toxin.
Abbreviations: nd, not determined.
Microscopic pathology and in situ hybridization
Lymph node biopsy and microscopic analysis showed the effect of PTx on lymph node architecture (Fig. 3). The image in Fig. 3A shows the normal appearance of a highly proliferative lymph node during SIV infection. The extent of proliferation is such that germinal centers are not easily defined. The specimen in Fig. 3B was taken 7 days after PTx treatment at the peak of lymphocytosis. Note the presence of intact germinal centers and the absence of paracortical lymphocytes in the spaces now occupied by lymph.
FIG. 3.
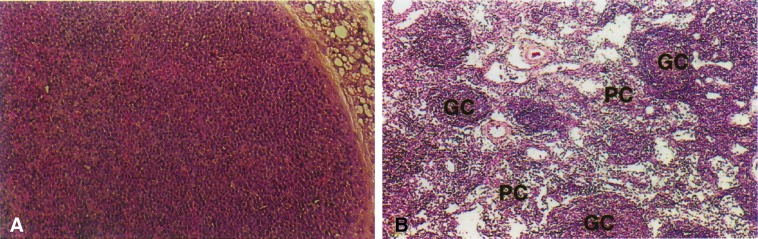
Microscopic anatomy of lymph node tissues from SIV-infected rhesus before and after pertussis toxin injection. Inguinal lymph node biopsies were performed and samples were fixed in buffered formalin before embedding in paraffin. Similar sections were compared for the pretreatment (A) and 7 days post-pertussis injection (B) samples. The labeling in (B) shows the position of germinal centers (GC) and paracortical regions (PC).
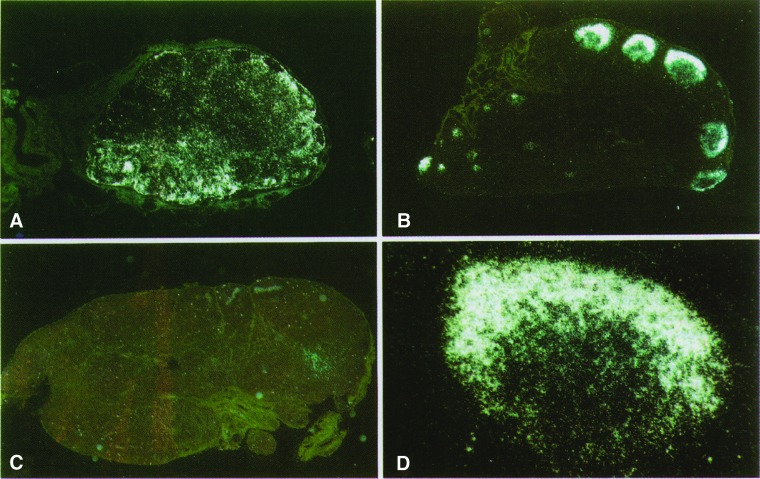
Lymph node biopsies were collected for in situ hybridization from SIV-infected animals before and after PTx treatment (Fig. 4). A pattern of dispersed viral RNA was observed in an active inguinal lymph node prior to PTx treatment (Fig. 4A). At the peak of lymphocytosis (Fig. 4B), a localized pattern of hybridization was observed; this pattern is consistent with virus particles being retained in germinal centers and there is little sign of active virus replication. The specimen in Fig. 4C is a popliteal lymph node from animal 90061 at 45 days after PTx treatment and shows little evidence of viral RNA. Figure 4D is an enlarged view of the specimen in Fig. 4B; this photomicrograph emphasizes the intact germinal center organization despite depletion of paracortical lymphocytes.
FIG. 4.
In situ hybridization analysis of pertussis toxin effects on SIV RNA in lymph nodes. Sections are photographed under epifluorescent light and hybridization to viral RNA appears white on the dark background. (A) Inguinal lymph node prior to pertussis toxin administration. (B) Popliteal fossis lymph node removed 7 days after pertussis toxin injection. (C) Popliteal fossis lymph node removed 45 days after pertussis toxin injection. (D) Enlarged view of a single germinal center from the specimen shown in (B).
Discussion
Pathogenesis of SIV in rhesus macaques is similar to HIV infection in humans. Peripheral lymphadenopathy is an early and sustained diagnosis following virus infection. The lymphadenopathy reflects active infection of superficial lymph nodes and active host immune responses (reviewed in Ref. 22). Viral pathogenesis in AIDS is associated with infection of cells in solid lymphoid tissues and the consequent virus replication, apoptosis, and immune-mediated mechanisms for cellular destruction that underlie the progressive loss of host immunity. Most importantly, HIV disease in humans reflects a dynamic process with high rates of spreading infection.23,24 Virus entry for primary isolates of HIV-1 proceeds via coreceptors for virus infection and these cell surface proteins are coupled to heterotrimeric G proteins.17–19 Thus, compounds known to affect G protein activity should be explored for their effects on HIV-1 and SIV infection.
Pertussis toxin enzymatically modifies heterotrimeric G proteins by an ADP-ribosylation of the α subunit25 and has many effects on lymphocyte activity. An early step in the pathway for lymphocyte invasion through endothelial venules is pertussis toxin sensitive, implying a G protein-coupled signal that converts the rolling lymphocyte to a firmly attached cell ready for extravasation.14 This molecular mechanism accounts for the ability of pertussis toxin to induce lymphocytosis in rodent models12,13,26–28 and for the lymphocytosis observed during natural Bordetella pertussis infection.10 Lymphocytes treated ex vivo with pertussis toxin fail to move rapidly from blood to lymphoid tissues9 and fail to reconstitute antigen-specific contact hypersensitivity responses after adoptive transfer.29 In the context of SIV or HIV disease, pertussis toxin has the potential to affect lymphadenopathy (by inducing lymphocytosis) and to alter the pattern of immune responses all through the action of this toxin on G proteins.
The peak for total lymphocytes in rhesus peripheral blood occurred 3 days after PTx injection. The maximum levels of CD4+ cells in peripheral blood were not reached until 14 days after injection; CD8+ cell counts peaked by 2 to 7 days after PTx injection. The absolute CD4+ cell counts at 53 days after PTx injection were slightly decreased, but within the range of starting values in each of the four animals tested. In the four cases studied with flow cytometry, the CD4/CD8 ratio was smaller on day 8 than the values observed prior to treatment for infected animals. Preliminary studies using monoclonal antibody detection of PCNA (proliferating cell nuclear antigen) in lymphocytes before and after pertussis toxin treatment in vivo showed that increases in CD4+ or CD8+ T cell populations were not the result of cellular proliferation, as the percentage of PCNA-positive cells in either subset did not change (K. K. Steger and C. D. Pauza, unpublished). Although pertussis toxin can be an effective mitogen for rhesus cells when used at concentrations above 1 μg/ml in vitro,21a we do not see effects on cell proliferation rates during in vivo treatments.
The CD4+ cell counts were increased significantly at their peak levels when compared to pretreatment or day 53 samples (p=0.005); however, the pretreatment and day 53 samples were not significantly different. We did note increases in CD8+ cells at 28 and 53 days after PTx injection. Pairwise statistical comparisons between pretreatment and day 53 samples showed a significant (p=0.005) increased in CD8+ cells. Thus, by 53 days after PTx injection the CD4 counts remained at pretreatment levels and CD8 cells were increased. We cannot be sure whether this is a direct effect of PTx on lymphocyte distribution or whether this reflects a change in virus replication that indirectly influences lymphocyte populations.
Our data showed a change in the efficiency of virus isolation from rhesus PBMCs after PTx treatment in vivo; however, we did not detect decreased levels of viral DNA in these same lymphocyte populations. Changes in the mean for infectious cells in PBMCs showed a drop by day 7 after PTx injection. This change coincided with the peak of lymphocytosis and a proportional increase in CD8+ cells. By 28 or 56 days after PTx treatment, the mean infectious cell values were around 10 times lower than the pretreatment levels and three of the five animals showed a decrease in the frequency of infectious cells in PBMCs relative to pretreatment points. Some animals, particularly 90019 and 90061, showed a sustained decrease for infectious cells after PTx injection. We were unable to recover virus from peripheral blood or lymph node biopsies of 90019 until 175 days after PTx injection (not shown); a biopsy of retroperitoneal lymph node from 90061 at 45 days after PTx was negative by in situ hybridization.
We do not yet know the mechanisms responsible for changes in infectious cell frequencies in peripheral blood after pertussis toxin treatment. Studies with PTx in vitro show a modest antiviral effect with compound in the range of 10 ng/ml (A. R. Schenkel and C. D. Pauza, unpublished), but this mechanism is probably insufficient to explain the virus isolation data presented here. It seems more likely that infected cells recovered from PTx-treated macaques are less efficiently detected in the virus isolation assay owing to unidentified changes in cell surface receptors (coupled to G proteins) or other changes. Studies are in progress to understand the relationships between in vitro and in vivo effects of PTx.
Our studies represent a unique approach to studying AIDS pathogenesis in the macaque model. Pertussis toxin affects lymphocyte circulation through its ability to modify heterotrimeric G proteins; the drug caused lymphocytosis with changes in virus distribution within lymph nodes and temporary decreases in virus isolation efficiency after injection into SIV-infected macaques. On the basis of the adoptive transfer experiments in rodents,29 PTx is known to have potential for altering cellular immune responses and may decrease the extent of lymphocyte activation in solid lymphoid tissues. The complex interplay of immune responses that limit virus spread and cytopathogenicity, versus those responses that promote virus replication through activation of target cells, is poorly characterized partly owing to a lack of effective approaches for studying these problems in animal models. Pertussis toxin affects the process of lymphocyte recruitment into lymphoid tissues that is essential for high-level virus replication, has the potential to alter patterns of immune responses, and may affect virus entry occurring via G protein-coupled coreceptors. Further study of PTx mechanisms in vivo has the potential to explain better the role of these reactions in AIDS pathogenesis.
Acknowledgments
These studies were supported by PHS Grants AI24591 (C.D.P.) and RR00167 (base grant support for the primate center). The authors are especially grateful to Dr. Greg Milman for his advice and support. We thank Dr. Miroslav Malkovsky, Dr. Pierre Lalouette, and Dr. Cecil Fox for helpful discussions and Dr. Dan Kurtycz for assistance in computer imaging of microscopic specimens.
References
- 1.Tenner-Racz K. Racz P. Dietrich M. Kern P. Altered follicular dendritic cells and virus-like particles in AIDS and AIDS-related lymphadenopathy. Lancet. 1985;i:105–106. doi: 10.1016/s0140-6736(85)91994-4. [DOI] [PubMed] [Google Scholar]
- 2.Pallesen G. Gerstoft J. Mathiesen L. Stages in LAV/HTLV-III lymphadenitis I. Histological and immunological classification. Scand J Immunol. 1987;25:83–91. doi: 10.1111/j.1365-3083.1987.tb01049.x. [DOI] [PubMed] [Google Scholar]
- 3.Pantaleo G. Graziosi C. Demarest JF. Butini L. Montroni M. Fox CH. Orenstein JM. Kotler DP. Fauci A. HIV infection is active and progressive in lymphoid tissue during the clinically latent stage of disease. Nature (London) 1993;362:355–359. doi: 10.1038/362355a0. [DOI] [PubMed] [Google Scholar]
- 4.Embretson J. Zupancic M. Ribas JL. Burke A. Racz P. Tenner-Racz K. Haase AT. Massive covert infection of helper T lymphocytes and macrophages by HIV during the incubation period of AIDS. Nature (London) 1993;362:359–362. doi: 10.1038/362359a0. [DOI] [PubMed] [Google Scholar]
- 5.Pantaleo G. Graziosi C. Butini L. Pizzo PA. Schnittman S. Kotler DP. Fauci AS. Lymphoid organs function as major reservoirs for human immunodeficiency virus. Proc Natl Acad Sci USA. 1991;88:9838. doi: 10.1073/pnas.88.21.9838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lackner AL. Vogel P. Ramos RA. Kluge JD. Marthas M. Early events in tissues during infection with pathogenic (SIVmac239) and nonpathogenic (SIVmac1A11) molecular clones of simian immunodeficiency virus. Am J Pathol. 1994;145:428–439. [PMC free article] [PubMed] [Google Scholar]
- 7.Reimann KA. Tenner-Racz K. Racz P. Montefiori DC. Yasutomi Y. Lin W. Ransil BJ. Letvin NL. Immunopathogenic events in acute infection of rhesus monkeys with simian immunodeficiency virus of macaques. J Virol. 1994;68:2362–2370. doi: 10.1128/jvi.68.4.2362-2370.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pantaleo G. Graziosi C. Demarest JF. Cohen OJ. Vaccarezza M. Gantt K. Muro-Cacho C. Fauci AS. Role of lymphoid organs in the pathogenesis of human immunodeficiency virus (HIV) infection. Immunol Rev. 1994;140:105–130. doi: 10.1111/j.1600-065x.1994.tb00867.x. [DOI] [PubMed] [Google Scholar]
- 9.Cyster JG. Goodnow CC. Pertussis toxin inhibits migration of B and T lymphocytes into splenic white pulp cords. J Exp Med. 1995;182:581–586. doi: 10.1084/jem.182.2.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith A. In: Bordetella Pertussis and Whooping Cough. Schaechter M, editor; Medoff G, editor; Schlessinger EG, editor. Williams & Wilkins; Baltimore: 1989. pp. 283–291. [Google Scholar]
- 11.Huang K. Im SY. Samlowski WE. Daynes RA. Molecular mechanisms of lymphocyte extravasation. III. The loss of lymphocyte extravasation potential induced by pertussis toxin is not mediated via the activation of protein kinase C. J Immunol. 1989;143:229–238. [PubMed] [Google Scholar]
- 12.Morse SI. Lymphocytosis-promoting factor of Bordetella pertussis: Isolation, characterization, and biological activity. J Infect Dis. 1977;136:S234–S238. doi: 10.1093/infdis/136.supplement.s234. [DOI] [PubMed] [Google Scholar]
- 13.Sewell WA. Andrews P. Inhibition of lymphocyte circulation in mice by pertussis toxin. Immunol Cell Biol. 1989;67:291–296. doi: 10.1038/icb.1989.43. [DOI] [PubMed] [Google Scholar]
- 14.Bargatze RF. Butcher EC. Rapid G protein-regulated activation event involved in lymphocyte binding to high endothelial venules. J Exp Med. 1993;178:367–372. doi: 10.1084/jem.178.1.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Honda S. Campbell JJ. Andrew DP. Engelhardt B. Butcher BA. Warnock RA. Ye RD. Butcher EC. Ligand-induced adhesion to activated endothelium and to vascular cell adhesion molecule-1 in lymphocytes transfected with the N-formyl peptide receptor. J Immunol. 1994;152:4026–4035. [PubMed] [Google Scholar]
- 16.Chowdhury IH. Koyanagi Y. Hazeki O. Ui M. Yamato N. Pertussis toxin inhibits induction of human immunodeficiency virus type 1 in infected monocytes. Virology. 1994;203:378–383. doi: 10.1006/viro.1994.1497. [DOI] [PubMed] [Google Scholar]
- 17.Dragic T. Litwin V. Allaway GP. Martin SR. Huang Y. Nagashima KA. Cayanan C. Maddon PJ. Koup RA. Moore JP. Paxton WA. HIV-1 entry into CD4+ cells is mediated by the chemokine receptor CC-CKR-5. Nature (London) 1996;381:667–673. doi: 10.1038/381667a0. [DOI] [PubMed] [Google Scholar]
- 18.Deng H. Liu R. Ellmeier W. Choe S. Unumatz D. Burkhart M. Di Marzio P. Marmon S. Sutton RE. Hill CM. Davis CB. Peiper SC. Schall TJ. Littman DR. Landau NR. Identification of a major co-receptor for primary isolates of HIV-1. Nature (London) 1996;381:661–666. doi: 10.1038/381661a0. [DOI] [PubMed] [Google Scholar]
- 19.Feng Y. Broder CC. Kennedy PE. Berger EA. HIV-1 entry cofactor: Functional cDNA cloning of a seven-transmembrane, G protein-coupled receptor. Science. 1996;272:872–877. doi: 10.1126/science.272.5263.872. [DOI] [PubMed] [Google Scholar]
- 20.Pauza CD. Trivedi P. McKechnie TS. Richman DD. Graziano FM. 2-LTR circular viral DNA as a marker for human immunodeficiency virus type 1 infection in vivo. Virology. 1994;205:470–478. doi: 10.1006/viro.1994.1667. [DOI] [PubMed] [Google Scholar]
- 21.Trivedi P. Meyer KK. Streblow DN. Preuninger BL. Schultz KT. Pauza CD. Selective amplification of simian immunodeficiency virus genotypes after intrarectal inoculation of rhesus monkeys. J Virol. 1994;62:7649–7653. doi: 10.1128/jvi.68.11.7649-7653.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21a.Hinds PW., II Yin C. Salvato MS. Pauza CD. Pertussis toxin induces lymphocytosis in rhesus macaques. 1997. submitted. [DOI] [PubMed]
- 22.Pantaleo G. Fauci AS. New concepts in the immunopathogenesis of HIV infection. Annu Rev Immunol. 1995;13:487–512. doi: 10.1146/annurev.iy.13.040195.002415. . [Review] [DOI] [PubMed] [Google Scholar]
- 23.Ho DD. Neumann AU. Perelson AS. Chen W. Leonard JM. Markowitz M. Rapid turnover of plasma virions and CD4 lymphocytes in HIV-1 infection. Nature (London) 1995;373:123–126. doi: 10.1038/373123a0. [DOI] [PubMed] [Google Scholar]
- 24.Wei X. Ghosh SK. Taylor ME. Johnson VA. Emini EA. Deutsch P. Lifson JD. Bonhoeffer S. Nowak MA. Hahn BH. Saag MS. Shaw GM. Viral dynamics in human immunodeficiency virus type 1 infection. Nature (London) 1995;373:117–122. doi: 10.1038/373117a0. [DOI] [PubMed] [Google Scholar]
- 25.Ui M. In: Pertussis as a Valuable Probe for G-Protein Involvement in Signal Transduction. Moss J, editor; Vaughan M, editor. American Society for Microbiology; Washington, D.C.: 1990. pp. 45–78. [Google Scholar]
- 26.Huang K. Im SY. Samlowski WE. Daynes RA. Molecular mechanisms of lymphocyte extravasation. III. The loss of lymphocyte extravasation potential induced by pertussis toxin is not mediated via the activation of protein kinase C. J Immunol. 1989;143:229–238. [PubMed] [Google Scholar]
- 27.Morse S. Barron B. Studies on the leukocytosis and lymphocytosis induced by Bordetella pertussis. III. The distribution of transfused lymphocytes in pertussis treated and normal mice. J Exp Med. 1970;132:663–672. doi: 10.1084/jem.132.4.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rai KR. Chanana AD. Cronkite EP. Joel DD. Stevens JB. Studies on lymphocytes. XVIII. Mechanism of lymphocytosis induced by supernatant fluids of Bordetella pertussis cultures. Blood. 1971;38:49–59. [PubMed] [Google Scholar]
- 29.Spangrude GJ. Araneo BA. Daynes RA. Site-selective homing of antigen-primed lymphocyte populations can play a crucial role in the efferent limb of cell-mediated immune responses in vivo. J Immunol. 1985;134:2900–2907. [PubMed] [Google Scholar]