Abstract
Objective:
The purpose of this study was to evaluate associations between prescription drug misuse (PDM) and sexual risk behaviors (SRBs) among adolescents and emerging adults.
Method:
In a hospital emergency department, 2,127 sexually active 14- to 20-year-olds (61% female) reported on past-year alcohol use severity (using the Alcohol Use Disorders Identification Test–consumption [AUDIT-C]), cannabis use, PDM (n = 422), and SRBs (inconsistent condom use, multiple partners, intercourse following alcohol/other drug use).
Results:
Bivariately, AUDIT-C score, cannabis use, and PDM of stimulants, opioids, and sedatives were positively associated with each SRB. Because many participants reported PDM for multiple drug classes (i.e., sedatives, stimulants, opioids), participants were categorized as (a) no PDM (n = 1,705), (b) PDM of one class (n = 251), (c) PDM of two classes (n = 90), or (d) PDM of three classes (n = 81). Three hierarchical logistic regression models evaluated the associations of number of classes of PDM with SRBs separately, after accounting for demographics (age, gender, race), AUDIT-C score, and cannabis use. Adding PDM statistically improved each model beyond what was accounted for by demographics, alcohol, and cannabis use. For inconsistent condom use and substance use before sex, PDM of one, two, or three classes was significantly associated with increased odds of these SRBs. PDM of two or three classes was associated with increased odds of reporting multiple partners.
Conclusions:
Findings suggest that PDM, especially poly-PDM, may be a pertinent risk factor for SRBs among youth. Event-based research could further evaluate how PDM, as well as other substance use, is related to SRBs at the event level in order to inform interventions.
Sexual risk behaviors (SRBs; e.g., inconsistent condom use, multiple partners, substance use before sex) among adolescents (those approximately 12–17 years old) and emerging adults (those 18–25 years old) comprise an important public health concern in that they are related to increased risk of acquiring human immunodeficiency virus (HIV) and sexually transmitted infections (STIs) (Centers for Disease Control and Prevention [CDC], 2011; Kotchick et al., 2001). This is concerning given that 25% of new HIV infections occur in young people ages 13–24, with this age group representing the second highest annual incidence rate (CDC, 2012a, 2012b). Further, in 2009 those aged 15–29 accounted for 39% of new HIV infections while only comprising 21% of the U.S. population (CDC, 2011). Also concerning, 15- to 24-year-olds account for half of new STIs, and the incidence of both chlamydia and gonorrhea in this age group has increased in recent years (CDC, 2012a, 2012b).
National surveys of high school students indicate that one half have ever had sexual intercourse, about one third are currently sexually active, and of those sexually active, 60% did not use a condom during their last intercourse (CDC, 2010). In a national survey of young adults, 29% used condoms none of the time, 31% used condoms some of the time, and 40% used condoms most/all of the time in the past year (Gillmore et al., 2011). Rates of SRBs tend to peak during emerging adulthood (Arnett, 1992, 2000; Dariotis et al., 2008). Similarly, substance use is often initiated during adolescence and peaks during emerging adulthood (Arnett, 2000, 2005; Stone et al., 2012; Substance Abuse and Mental Health Services Administration [SAMHSA], 2011). Alcohol and other drug use have been associated with SRBs in samples of young people at both the global level, perhaps reflecting problem behavior theory (Donovan, 1996; Jessor, 1982) in which risk behaviors tend to cluster, and the event level (Bonar et al., in press; Brown and Vanable, 2007; Bryan et al., 2007, 2012; Ellickson et al., 2005; Hendershot et al., 2010; Kiene et al., 2009; Nkansah-Amankra et al., 2011), likely reflecting contextual influences and acute intoxication that may affect decision making related to SRBs.
Prescription drug misuse and sexual risk behaviors
Rising rates of prescription drug misuse (PDM) have created a recent public health concern among adolescents and young adults because many prescription drugs are used more frequently than other illicit drugs, except for marijuana (Johnston et al., 2012b). Although definitions vary across studies (Becker et al., 2008; Boyd et al., 2009; SAMHSA, 2010), in general (and as it is used in this research), PDM refers to using prescription substances to get high, taking others’ prescriptions, or taking more than what is prescribed to an individual. Recent data indicate that lifetime and past-year prevalence for PDM generally increases throughout adolescence and emerging adulthood, with past-year prevalence ranging from 6.7% for 14- to 15-year-olds to 12.4% for 21- to 25-year-olds (lifetime prevalence is 9.2% and 30.2% for these age groups, respectively; SAMHSA, 2012).
Further, in a review of studies of adolescents (generally ages 12–17, including some 18-year-olds in high school), the prevalence of PDM differs across samples and by drug classes; estimates range from 2% to 14% for “pain relievers,” 1% to 3% for stimulants, 1% to 3% for sedatives, and 0.4% to 3% for tranquilizers (Young et al., 2012). Similarly, data from Monitoring the Future also show variations in past-year PDM across substances for young adults (19–28 years old) and college students. For example, 9.8% of college students and 6.6% of young adults reported using Adderall in 2011, and 1.7% and 3.2%, respectively, reported sedative use (Johnston et al., 2012b). In line with theory and research, school, community-based, and national survey studies have begun to demonstrate that PDM among youth is associated with negative consequences (e.g., school dropout, decreased academic performance, and delinquency) and other substance-related risk behaviors (e.g., other substance use, co-ingestion of PDM and other drugs; McCabe et al., 2012; Young et al., 2012).
Very little is known about the role of PDM in SRBs among young people, and prior work in this area has focused on college students only. For example, among college students, PDM and lifetime sexual activity were associated (Ford and Arrastia, 2008; McCabe, 2005). Benotsch et al. (2011) reported that 35.6% of their college student sample endorsed lifetime PDM (defined as using a prescription medication without a doctor’s prescription), and 22.2% reported PDM in the past 3 months. Compared to those without lifetime PDM, those with lifetime PDM were significantly more likely to report having multiple sexual partners (23.2% vs. 10.1%), unprotected sex (51.3% vs. 22.2%), sex after “having too much to drink” (53.9% vs. 23.6%), and sex after using drugs (32.4% vs. 8.3%). On average, those with lifetime PDM reported significantly more sexual partners and unprotected sex acts during the past 3 months.
These previous studies provide a foundation for understanding the relationships between PDM and SRBs among college students; however, additional data from broader samples of adolescents and emerging adults are needed to understand this phenomenon and target intervention development and delivery for young people. Because most 18- to 24-year-olds are not enrolled in traditional colleges and many young people drop out of high school (National Center for Education Statistics, 2011, 2012), research and interventions must address young people in other settings. One promising venue to gain information about diverse populations of young people is the hospital emergency department (ED).
EDs are a common location of contact and intervention for young people who use substances (Bernstein et al., 2009; Ehrlich et al., 2010; Monti et al., 1999, 2007; Walton et al., 2010), and young people in the ED also have high rates of SRBs. For example, in 14- to 18-year-olds in the ED, Walton et al. (2011) found that among the 60% who were sexually active, 43% had multiple partners, 55% reported inconsistent condom use, and 15% used alcohol and/or other drugs before sex in the past year. Similarly, in an urban ED, among 14- to 24-year-olds with a history of drug use, Bonar et al. (in press) found that 95% were sexually active, 30% had a lifetime STI, and in the past month, 30% had multiple sexual partners, 55% reported inconsistent condom use with regular partners, and 27% reported inconsistent condom use with casual partners. Both of these studies also reported positive relationships between alcohol, cannabis, and other illicit drugs and SRBs but did not report on PDM.
Considering the dearth of knowledge regarding PDM and SRBs in young people, the present study addresses a gap in the literature by evaluating these relationships among 14- to 20-year-old patients presenting to an ED. We hypothesized that PDM would be associated with increased odds of reporting SRBs. We also expected that PDM would account for additional risk, beyond alcohol and cannabis use, adolescents’ two most frequently used substances (Johnston et al., 2012a). Given the varying pharmacology of these prescription drugs, we examined whether PDM from different classes (e.g., sedatives, opioids, stimulants) was differentially related to SRBs among youth. Further, we expected that use of multiple classes of prescription drugs would be associated with increased odds of SRBs.
Method
Study setting and design
The present study involves a secondary analysis of screening data collected in an ED-based randomized controlled trial of youth who engage in underage risky drinking. Recruitment and screening occurred at the University of Michigan, Department of Emergency Medicine, in Ann Arbor, MI. This academic level-1 trauma center has an annual census of approximately 85,000 patients and cares for a diverse population from the local community and the associated university. Study materials and procedures were approved by the Institutional Review Board at the University of Michigan. A Certificate of Confidentiality was obtained from the National Institutes of Health.
Patient sample and recruitment
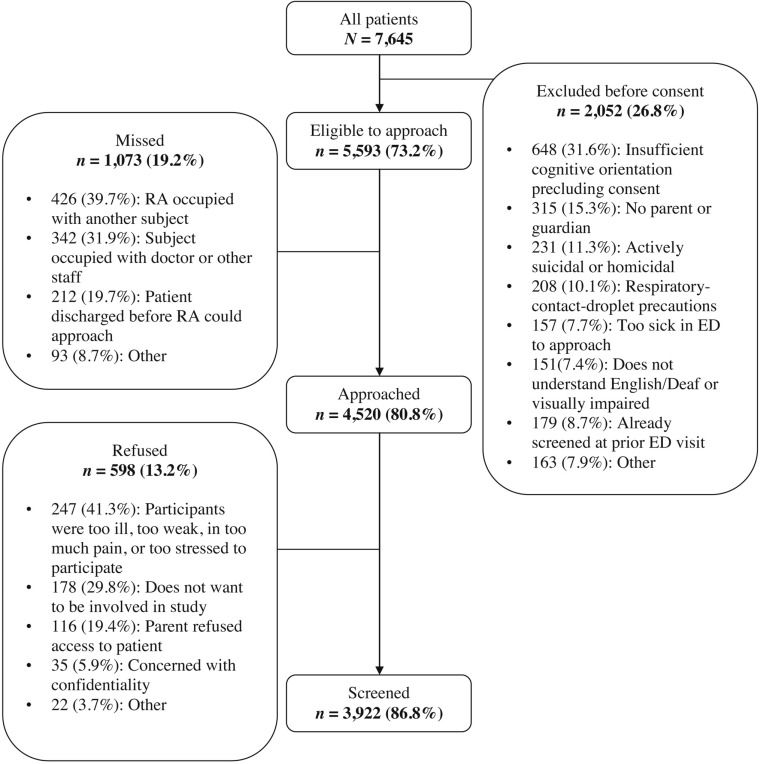
Youth ages 14–20 who presented to the medical ED were identified via an electronic medical record. Research assistants approached patients in waiting rooms or treatment spaces. Exclusion criteria, outlined in Figure 1, included insufficient cognitive orientation precluding informed consent, not having parent/guardian present if younger than 18 years old, having active suicidal/homicidal ideation, having respiratory-contact precautions, being too ill to approach, being deaf/visually impaired, being non–English speaking, and having already participated in this study on a prior visit. Patients who were too medically unstable to approach in the ED and who were admitted to the hospital were reached over the next 72 hours if they stabilized. Patients were recruited 7 days a week (except major holidays) over a 2-year period (September 2010 to September 2012) on evening shifts (triaged 2 p.m.–midnight). Day shifts (triaged 8 a.m.–2 p.m.) were randomly selected for sampling during this period (initially 7 days per week, reduced to 2 days per week); in addition, midnight shifts (triaged midnight–8 a.m.) were randomly selected for sampling twice a month initially but were eliminated because of low yield of participants.
Figure 1.
Flow chart detailing study recruitment, missed patients, and refusals. RA = research assistant; ED = emergency department.
Screening protocol
Written informed consent was obtained from the patient (or guardian). (If the patient was younger than age 18, assent was obtained.) Patients self-administered a 15-minute battery of surveys on a touch-screen tablet computer with audio headphones. Patients’ privacy was protected by asking accompanying guests to wait in another area. Research assistants paused the survey during medical evaluations and procedures. On completion, participants chose a gift ($1.00 value; e.g., pens, lip balm).
Measures
Sexual risk behaviors and sexual history.
Items assessing sexual activity and SRBs were adapted from the National Longitudinal Study of Adolescent Health (Bearman and Jones, 1997; Harris and Florey, 2003; Sieving et al., 2001). Participants first reported whether they ever had sexual intercourse by responding to the item, “Have you ever had sexual intercourse?” with a “yes” or “no” choice. Participants who responded “yes” were asked additional questions about SRBs. Number of sexual partners was assessed with the following: “During the past 12 months, with how many people did you have sexual intercourse?” Response options ranged from zero to six or more people. Condom use was measured with the following: “During the past 12 months, think of all the times you have had sexual intercourse, how much of the time have you or your partner used a condom?” Sexual intercourse following substance use was assessed with the following: “In the past 12 months, how often did you drink alcohol or use other drugs before you had sexual intercourse?” Response options for both items ranged from none of the time to all of the time. Because of low internal consistency when attempting to standardize and combine these three items into a cumulative measure of SRB, we examined each of these SRBs as a separate dependent measure.
Substance use.
To assess past-12-month alcohol use severity, we used a modified version of the three-item Alcohol Use Disorders Identification Test–consumption (AUDIT-C) questions (Bush et al., 1998) based on Chung et al.’s (2000) adaptation of the AUDIT for adolescents. Total scores on the three items assessing drinking frequency (never to four or more times a week), quantity (1 or 2 drinks to 10 or more drinks per drinking day), and frequency of five or more drinks on one occasion (never to daily/almost daily) ranged from 0 to 12. Other substance use was assessed using items from the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST; Humeniuk et al., 2008; WHO ASSIST Working Group, 2002). Specifically, participants indicated on a single item whether they had used cannabis (stated as “cannabis [marijuana, weed, pot, grass, hash, etc.]”) in the past 12 months (yes/ no). Three items measuring any misuse of prescription drugs in the past year were introduced with the statement, “In the past 12 months, have you used any of the following substances to get high, or taken them when they were prescribed to someone else, or taken more than what was prescribed to you?” Participants then responded “yes” or “no” for items representing three drug classes: prescription stimulants (Ritalin, Concerta, Dexedrine, Adderall, diet pills, etc.), sedatives or sleeping pills (Valium, Serepax, Ativan, Xanax, Librium, Rohypnol, gamma-hydroxybutyrate [GHB], etc.), and prescription pain medications/opioids (fentanyl, oxycodone [OxyContin, Percocet], hydrocodone [Vicodin], methadone, buprenorphine, Suboxone, etc.) separately.
Demographic measures.
Items from national surveys (Bearman and Jones, 1997; National Institute on Drug Abuse, 2008) were used to collect demographic information, including gender, age, and race (dichotomized as European American vs. African American/other for present analyses because of lack of variability in the sample).
Data analysis
Analyses were performed on the subset of patients (n = 2,127) who reported past-year sexual activity; this was determined using responses to the item assessing the number of past-year sexual partners. First, we calculated descriptive statistics (e.g., means, standard deviations, proportions) for the demographics, substance use, and SRBs (which were positively skewed). Of note, 84% of the sample reported any one of the three SRBs during the prior year, and the items assessing SRBs were not all highly correlated with each other (Spearman’s ρ ranging from .04 to .38), suggesting that these behaviors may be distinct from one another and should be examined separately. Further, given the public health concerns related to risk for HIV/STIs, we dichotomized responses on each SRB item to reflect any risk. Specifically, condom use was divided into “all the time” versus all other responses (i.e., inconsistent use), number of partners was divided into one versus two or more, and sex after alcohol/ other drug use was divided into none of the time versus all other responses.
Given the considerable overlap in proportions of the sample reporting PDM of sedatives, stimulants, and opioids (19% of PDM involved all three classes, 21% of PDM involved two classes) and correlations between PDM for each class (ranging from .40 to .50), we report descriptive information and bivariate analyses of relationships between each class of PDM with SRBs (see sample description below). For the primary multivariate analyses, we categorized participants based on the number of different classes of PDM (zero classes, one class, two classes, or three classes) and examined this categorical independent variable’s relationship with separate SRBs. Presumably, misuse of multiple classes of prescription drugs represents a higher level of risk behavior than a single class. As reported in the results, we examined drug classes with SRBs separately in supplementary analyses.
We conducted independent sample t tests (for continuous variables: age, AUDIT-C score) and chi-square analyses (for all other categorical variables) to test bivariate associations between independent variables and the three separate di-chotomous dependent measures of SRBs. Variance inflation factors for each of the independent variables were examined and were in the acceptable range. Three separate, parallel hierarchical logistic regression analyses were conducted to evaluate the relationships between each SRB and demographic information (age; gender: male/female; race: European American/African American and other), alcohol use severity (AUDIT-C total score), any past-12-month cannabis use (yes/no), and number of classes of prescription drugs misused. In Step 1, the demographics, alcohol, and cannabis use were entered; in Step 2, we added the number of different classes of PDM to evaluate whether PDM improved the model beyond what was accounted for in Step 1.
Results
Sample
A total of 7,645 patients 14–20 years old presented to the ED for a medical or injury complaint. Of those, 5,593 (73.2%) met eligibility criteria for screening, and 2,052 (26.8%) were excluded; the most common reasons for exclusion included insufficient cognitive orientation (31.6%) and not having a parent/guardian present if younger than 18 years old (15.3%). Among those eligible for screening, 1,073 (19.2%) were missed. Research assistants approached 4,520 (80.8%); 598 (13.2%) refused participation, and 3,922 (86.8%) completed the screening surveys (Figure 1). In comparing missed participants with screened participants on both gender and age group (14- to 17-year-olds vs. 18-to 20-year-olds), younger patients (23.6%) were more likely to be missed than older patients (19.7%), χ2(1) = 11.11, p < .001, and males (24.9%) were more likely to be missed than females (18.7%), χ2(1) = 27.99, p < .001. There were no significant gender or age differences between screened participants and patients who refused.
Of those screened, 2,198 (56.0%) reported ever having had sex, and 2,127 (54.2%) had at least one sexual partner in the past year and were included in further analyses. As displayed in Table 1, of those 2,127 participants, 60.7% were female, 69.0% were European American, and the mean age was 18.3 years (SD = 1.6); 9% reported having children. Most presented to the ED with a medical complaint (71%) rather than an injury. On average, participants scored a 3.03 (SD = 2.93) on the AUDIT-C, and 53.1% disclosed past-year cannabis use.
Table 1.
Bivariate associations of demographics, alcohol use, and prescription drug use with sexual risk behaviors among patients who were sexually active in the past yeara
| Inconsist. condom use |
|||||||
| Full sample, past-year sex (n = 2,127) | Always (n = 827) | None/inconsist. (n = 1,298) | Multiple partners |
Substance use before sex |
|||
| Variable | 1 partner (n = 1,001) | >1 partner (n = 1,126) | No (n = 1,072) | Yes (n = 1,053) | |||
| Female | 1,291 (60.7%) | 439 (53.1%)*** | 850 (65.5%) | 645 (64.4%)** | 646 (57.4%) | 688 (64.2%)** | 601 (57.1%) |
| Age | 18.34 (1.58) | 18.07 (1.68)*** | 18.51 (1.49) | 18.32 (1.63) | 18.36 (1.53) | 18.02 (1.71)*** | 18.67 (1.36) |
| European American | 1,468 (69.0%) | 620 (75.0%)*** | 846 (65.2%) | 685 (68.4%) | 783 (69.5%) | 673 (62.8%)*** | 793 (75.3%) |
| Stimulant PDM | 268 (12.6%) | 68 (8.2%)*** | 199 (15.3%) | 83 (8.3%)*** | 185 (16.4%) | 44 (4.1%)*** | 223 (21.2%) |
| Sedative PDM | 174 (8.2%) | 32 (3.9%)*** | 142 (10.9%) | 31 (3.1%)*** | 143 (12.7%) | 28 (2.6%)*** | 146 (13.9%) |
| Opioid PDM | 232 (10.9%) | 51 (6.2%)*** | 181(13.9%) | 63 (6.3%)*** | 169 (15.0%) | 51 (4.8%)*** | 181 (17.2%) |
| No PDM | 1,705 (80.2%) | 717 (86.7%)*** | 987 (76.0%) | 873 (87.2%)*** | 832 (73.9%) | 971 (90.6%)*** | 733 (69.6%) |
| One class | 251 (11.8%) | 81 (9.8%) | 169 (13.0%) | 94 (9.4%) | 157 (13.9%) | 82 (7.6%) | 168 (16.0%) |
| Two classes | 90 (4.2%) | 17 (2.1%) | 73 (5.6%) | 19 (1.9%) | 71 (6.3%) | 16 (1.5%) | 74 (7.0%) |
| Three classes | 81 (3.8%) | 12 (1.4%) | 69 (5.3%) | 15 (1.5%) | 66 (5.9%) | 3 (0.3%) | 78 (7.4%) |
| AUDIT-C score | 3.03 (2.93) | 2.58 (2.75)*** | 3.32 (3.01) | 2.19 (2.54)*** | 3.79 (3.06) | 1.40 (1.99)*** | 4.70 (2.80) |
| Cannabis use | 1,129 (53.1%) | 376 (45.5%)*** | 752 (57.9%) | 402 (40.2%)*** | 727 (64.6%) | 330 (30.8%)*** | 798 (75.8%) |
Notes: Data are n (%) or M (SD). Inconsist. = inconsistent; PDM = prescription drug misuse; AUDIT-C = Alcohol Use Disorders Identification Test–Consumption.
Reference groups for gender = male, for race = African American/other, for PDM and cannabis variables = no PDM or cannabis use.
p < .01;
p < .001.
Prevalence of prescription drug misuse and sexual risk behaviors
Among the 2,127 patients, 12.6% reported misuse of prescription stimulants, 10.9% reported misuse of prescription opioids, and 8.2% reported misuse of prescription sedatives. Of the 422 (19.8%) patients who reported any PDM, there was considerable overlap in use of different classes. For example, of the 232 patients who used prescription opioids/pain relievers, 63.4% also used stimulants and/or sedatives. Of the 174 patients who reported sedative use, 77.1% also used opioids/pain relievers and/or stimulants. Of those 268 patients with stimulant use, 53.0% used sedatives and/or opioids/pain relievers. Categorically, among those with any PDM, 59.4% reported one class of PDM, 21.3% reported two classes, and 19.2% reported three classes (in the full sample, 11.8% used one class, 4.2% used two classes, and 3.8% used three classes).
SRBs were relatively common in this sample. In the past year, 61.1% of participants engaged in inconsistent condom use, whereas the remaining 38.9% always used a condom (or their partner did) during sexual intercourse. About half (52.9%) had more than one partner in the past year and reported substance use before sexual intercourse (49.6%).
Bivariate associations of demographics and substance use with sexual risk behaviors
As displayed in Table 1, at the bivariate level, with a few exceptions, all independent variables of interest were significantly associated with each of the three SRBs. Significantly more females engaged in each SRB than males. Older age was significantly positively associated with SRBs (except for multiple partners). African American/other patients were more likely to report inconsistent condom use but less likely to report substance use before sex than European American youth. Higher levels of alcohol use and cannabis use were positively associated with each SRB. Examined separately, use of each prescription drug class was significantly positively associated with all three SRBs. In addition, the categorical variable reflecting number of classes of PDM was significantly associated with each SRB, with a larger proportion of participants engaging in SRBs reporting more classes of PDM than those who did not engage in SRBs.
Multivariate models evaluating correlates of sexual risk behaviors
In the model evaluating inconsistent condom use as the dependent measure (Table 2), Step 1 (gender, age, race, AUDIT-C score, cannabis use) was significant, with all independent variables significantly related to inconsistent condom use. The addition of PDM in Step 2 resulted in significant model improvement, Step χ2(3) = 35.70, p < .001, and the variables from Step 1 remained significant. Compared with the reference group who reported no PDM, use of one prescription drug class (adjusted odds ratio [adj. OR] = 1.42), two prescription drug classes (adj. OR = 2.90), and three prescription drug classes (adj. OR = 3.85) were associated with significantly higher odds of reporting inconsistent condom use.
Table 2.
Hierarchical logistic regression models evaluating correlates of sexual risk behaviorsa
| Inconsistent condom use |
Multiple partners |
Substance use before sex |
||||
| Variable | Step 1 Adj. OR [95% CI] | Step 2 Adj. OR [95% CI] | Step 1 Adj. OR [95% CI] | Step 2 Adj. OR [95% CI] | Step 1 Adj. OR [95% CI] | Step 2 Adj. OR [95% CI] |
| Female | 1.99 | 2.00 | 0.97 | 0.97 | 1.34 | 1.35 |
| [1.64, 2.41]*** | [1.65, 2.43]*** | [0.80, 1.17] | [0.80, 1.17] | [1.05, 1.69]* | [1.06, 1.71]* | |
| Age | 1.15 | 1.17 | 0.95 | 0.96 | 1.26 | 1.28 |
| [1.09, 1.22]*** | [1.10, 1.24]*** | [0.89, 1.01] | [0.90, 1.01] | [1.17, 1.35]*** | [1.18, 1.38]*** | |
| European American | 0.53 | 0.51 | 0.82 | 0.80 | 1.28 | 1.22 |
| [0.44, 0.66]*** | [0.42, 0.63]*** | [0.67, 1.00]* | [0.66, 0.97]* | [1.01, 1.63]* | [0.96, 1.55] | |
| AUDIT-C score | 1.10 | 1.07 | 1.19 | 1.17 | 1.57 | 1.55 |
| [1.06, 1.14]*** | [1.03, 1.11]** | [1.14, 1.23]*** | [1.13, 1.22]*** | [1.49, 1.66]*** | [1.47, 1.64]*** | |
| Cannabis use | 1.54 | 1.40 | 1.88 | 1.76 | 4.52 | 4.11 |
| [1.26, 1.89]*** | [1.14, 1.72]** | [1.55, 2.29]*** | [1.45, 2.15]*** | [3.60, 5.69]*** | [3.26, 5.18]*** | |
| No PDM | [reference] | [reference] | [reference] | |||
| One class | 1.42 | 1.25 | 1.44 | |||
| [1.05, 1.91]* | [0.93, 1.67] | [1.01, 2.05]* | ||||
| Two classes | 2.90 | 2.25 | 2.55 | |||
| [1.65, 5.07]*** | [1.31, 3.85]** | [1.31, 4.95]** | ||||
| Three classes | 3.85 | 2.10 | 8.66 | |||
| [2.02, 7.34]*** | [1.16, 3.81]* | [2.49, 30.04]*** | ||||
| Model χ2 | 160.68*** | 196.38*** | 216.30*** | 232.21*** | 992.10*** | 1,020.12*** |
| (5 df) | (8 df) | (5 df) | (8 df) | (5 df) | (8 df) | |
| Step χ2 | 35.70*** | 15.92** | 28.03*** | |||
| (3 df) | (3 df) | (3 df) | ||||
Notes: Adj. OR = adjusted odds ratio; CI = confidence interval; AUDIT-C = Alcohol Use Disorders Identification Test–consumption questions; PDM = prescription drug misuse.
Reference groups for gender = male, for race = African American/other, for PDM and cannabis variables = no PDM or cannabis use.
p < .05;
p < .01;
p < .001.
For the model evaluating multiple sexual partners as the dependent measure (Table 2), Step 1 was statistically significant. In this step, European American race was significantly associated with lower odds of reporting multiple partners, whereas AUDIT-C score and cannabis use were associated with increased odds of multiple partners. These associations persisted in Step 2 with the addition of the PDM variable, and Step 2 resulted in model improvement, Step χ2(3) = 15.92, p < .01. Compared with the no-PDM reference group, those who used two classes of prescription drugs (adj. OR = 2.25) and those who used three classes of prescription drugs (adj. OR = 2.10) had significantly higher odds of reporting multiple partners in the past year.
Finally, in the model including substance use before sexual intercourse as the dependent measure (Table 2), Step 1 was statistically significant such that female gender, older age, European American race, higher AUDIT-C score, and cannabis use were associated with increased odds of reporting substance use before sex. These associations remained (except that race became nonsignificant) when PDM was added in Step 2, and PDM significantly improved the model, Step χ2(3) = 28.03, p < .001. Compared with the reference group, use of one prescription drug class (adj. OR = 1.44), two prescription drug classes (adj. OR = 2.55), and three prescription drug classes (adj. OR = 8.66) were significantly associated with substance use before sex.
We also conducted supplemental multivariate analyses evaluating each drug class separately with each SRB. A total of nine hierarchical logistic regression models were created (3 prescription drugs × 3 SRBs), with the same demographic and substance use variables (Step 1: gender, age, race, AUDIT-C score, cannabis use) except that either sedative, opioid, or stimulant use (yes/no past-year) was entered in Step 2. In all but one model (prescription stimulant use and multiple partners), the addition of Step 2 statistically improved the model fit, and each PDM variable was positively associated with each SRB.
Discussion
Our findings showing significant relationships between PDM and SRBs among adolescents and emerging adults (ages 14–20) in the ED are novel and highlight an important public health concern. Individually, each class of drug (i.e., sedatives, stimulants, opioids/pain relievers) was positively associated with SRBs. Multivariate analyses indicated that relationships between the number of different classes of PDM and SRBs persisted after accounting for demographics and alcohol and cannabis use, two substances often associated with SRBs among young people (e.g., Bryan et al., 2007, 2012; Ellickson et al., 2005; Nkansah-Amankra et al., 2011). Additionally, when categorizing participants based on number of classes of PDM, those who reported multiple classes of PDM were significantly more likely to report each SRB, except that using one class of PDM was associated with substance use before sex and inconsistent condom use but not multiple partners. This may reflect the age range of our sample in that low levels of PDM are not necessarily correlated with what could be an arguably more normative behavior among youth (i.e., having more than one relationship in a year). However, it is important to note that variables assessing PDM were dichotomous, and future research that investigates the quantity and frequency of PDM across substance types could further characterize the relationships between PDM and SRBs. For example, it may be that a frequent user of one type of prescription drug may engage in a different pattern of sexual risk than an infrequent user of multiple classes of prescription drugs.
These results are consistent with prior research indicating that college students with lifetime PDM were more likely to report past-3-month SRBs (Benotsch et al., 2011). The current investigation builds on this important early work by evaluating prescription drug classes separately and cumulatively among a large sample of adolescents and young adults in a community setting. The finding that PDM from multiple classes was related to increased odds of SRBs suggests that polysubstance use, particularly with regard to PDM, may be a salient factor for identifying young people engaging in the highest levels of SRBs.
The prevalence of sexual activity and inconsistent condom use among the present sample reflects what has been reported among national samples of adolescents and young adults (CDC, 2010; Gillmore et al., 2011), although less is known about past-year prevalence of multiple partners and substance use before sexual intercourse in the larger population of adolescents and young adults. Rates of sexual activity, multiple partners, and condom use in this sample were relatively consistent with another ED-based study of 14- to 18-year-olds in an urban ED (Walton et al., 2011). However, a larger proportion in the current study reported sex after alcohol/other drug use in the past year (50% vs. 15%), which may reflect differences in the samples (e.g., older age in this study, ED location). Taken together, this and prior studies (Bonar et al., in press; Walton et al., 2011) suggest that the ED may be an appropriate venue to assess and intervene with regard to substance use and SRBs among young people. Further, research investigating the rates of other sexual risk behaviors (e.g., overlapping/concurrent partners, unprotected anal sex) and relationships with PDM can inform screening and intervention across settings.
The present investigation extends prior research, but it is not without limitations. First, because these data are cross-sectional, interpretations regarding causal relationships are not warranted. In addition, this study took place among young people 14–20 years old in a single ED at an academic medical center in the midwestern United States, where males (vs. females) and younger patients (vs. older patients) were more likely to be missed during recruitment. Thus, generalizability to other settings and the full population of adolescents and emerging adults may be limited. Although research supports the reliability and validity of adolescents’ reports of sensitive behaviors via computer (Brener et al., 2002, 2003; Buchan et al., 2002; Dennis et al., 2002; Harrison et al., 2007; Thornberry and Krohn, 2000; Turner et al., 1998; Webb et al., 1999), these data may still be subject to the limitations of self-report in addition to recall biases. The absence of data regarding the context of SRBs, such as whether inconsistent condom use occurred with a long-term, monogamous partner, potentially involving the use of other birth control methods, may overestimate the relationships identified in this study.
Another potential limitation of these data is the absence of information on which particular types of prescription sedatives/sleeping pills, stimulants, and opioids participants had used. For example, for sedatives, the ASSIST includes common prescription substances (e.g., Xanax) with GHB and Rohypnol; reasons and motives for use, in addition to how these drugs are acquired, may be different across substances within a drug class. Thus, future research should consider finer grained assessment of such medication use, which may be associated with higher or lower engagement in other risk behaviors.
This study assessed patterns of past-year substance use and SRBs. Given these significant findings, a more detailed longitudinal examination of PDM and SRBs at the daily or event level would further clarify whether PDM (or specific classes and/or drugs within a class) causally contributes to specific SRBs among young people. Similar to how interactive voice response technology and timeline followback interviews have been used to assess alcohol and cannabis use and SRBs (Carey et al., 2001; Simpson et al., 2011), these methods could also focus separately on specific substances, including different types of prescriptions, to further understand the context of substance use and SRBs. Future research using this methodology is also necessary given that SRBs such as lack of condom use can vary depending on contextual factors, such as whether the partner is a regular or casual partner (Kiene et al., 2009; Scott-Sheldon et al., 2010).
The findings of the current study are consistent with theories of risk behavior among adolescents and have implications for clinical research and healthcare. For example, that adolescents and emerging adults in the ED reported significant rates of SRBs suggests that the ED may be a potential venue for identifying young people outside of campus and school settings who are in further need of behavioral interventions as well as STI and/or HIV testing. Because a sizable proportion of sexually active youth in this study reported PDM (19.8%) and because PDM was significantly related to various SRBs, further research on these relationships is pertinent to the development of behavioral interventions in order to reduce the public health costs associated with both substance use and SRBs. Finally, that PDM of more than one drug class was significantly associated with SRBs beyond what was accounted for by alcohol and cannabis use further highlights the potential risks of PDM among young people and suggests the importance of assessing polysubstance use, including poly-PDM, in future research.
Footnotes
This study was funded by National Institute on Alcohol Abuse and Alcoholism (NIAAA) Grant AA018122. Erin E. Bonar’s work on this article was supported by NIAAA T32 training grant AA007477 awarded to the University of Michigan Addiction Research Center and National Institute on Drug Abuse K23 Grant DA036038.
References
- Arnett J. Reckless behavior in adolescence: A developmental perspective. Developmental Review. 1992;12:339–373. [Google Scholar]
- Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. The American Psychologist. 2000;55:469–480. [PubMed] [Google Scholar]
- Arnett JJ. The developmental context of substance use in emerging adulthood. Journal of Drug Issues. 2005;35:235–254. [Google Scholar]
- Bearman PS, Jones J. The National Longitudinal Study of Adolescent Health: Research design. 1997. Retrieved from http://www.cpc.unc.edu/projects/addhealth/codebooks/wave1. [DOI] [PubMed]
- Becker WC, Sullivan LE, Tetrault JM, Desai RA, Fiellin DA. Non-medical use, abuse and dependence on prescription opioids among U.S. adults: Psychiatric, medical and substance use correlates. Drug and Alcohol Dependence. 2008;94:38–47. doi: 10.1016/j.drugalcdep.2007.09.018. [DOI] [PubMed] [Google Scholar]
- Benotsch EG, Koester S, Luckman D, Martin AM, Cejka A. Non-medical use of prescription drugs and sexual risk behavior in young adults. Addictive Behaviors. 2011;36:152–155. doi: 10.1016/j.addbeh.2010.08.027. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Edwards E, Dorfman D, Heeren T, Bliss C, Bernstein J. Screening and brief intervention to reduce marijuana use among youth and young adults in a pediatric emergency department. Academic Emergency Medicine. 2009;16:1174–1185. doi: 10.1111/j.1553-2712.2009.00490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonar EE, Whiteside LK, Walton MA, Zimmerman MA, Booth BM, Blow FC, Cunningham RM. Prevalence and correlates of HIV risk among adolescents and young adults reporting drug use: Data from an urban emergency department in the U.S. Journal of HIV/AIDS & Social Services. in press. [PMC free article] [PubMed]
- Boyd CJ, Teter CJ, West BT, Morales M, McCabe SE. Non-medical use of prescription analgesics: A three-year national longitudinal study. Journal of Addictive Diseases. 2009;28:232–242. doi: 10.1080/10550880903028452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brener ND, Billy JOG, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: Evidence from the scientific literature. Journal of Adolescent Health. 2003;33:436–457. doi: 10.1016/s1054-139x(03)00052-1. [DOI] [PubMed] [Google Scholar]
- Brener ND, Kann L, McManus T, Kinchen SA, Sundberg EC, Ross JG. Reliability of the (1999) Youth Risk Behavior Survey questionnaires. Journal of Adolescent Health. 2002;31:336–342. doi: 10.1016/s1054-139x(02)00339-7. [DOI] [PubMed] [Google Scholar]
- Brown JL, Vanable PA. Alcohol use, partner type, and risky sexual behavior among college students: Findings from an event-level study. Addictive Behaviors. 2007;32:2940–2952. doi: 10.1016/j.addbeh.2007.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan A, Ray LA, Cooper ML. Alcohol use and protective sexual behaviors among high-risk adolescents. Journal of Studies on Alcohol and Drugs. 2007;68:327–335. doi: 10.15288/jsad.2007.68.327. [DOI] [PubMed] [Google Scholar]
- Bryan AD, Schmiege SJ, Magnan RE. Marijuana use and risky sexual behavior among high-risk adolescents: Trajectories, risk factors, and event-level relationships. Developmental Psychology. 2012;48:1429–1442. doi: 10.1037/a0027547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchan BJ, Dennis ML, Tims FM, Diamond GS. Cannabis use: Consistency and validity of self-report, on-site urine testing and laboratory testing. Addiction, 97, Supplement s1. 2002:98–108. doi: 10.1046/j.1360-0443.97.s01.1.x. [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Archives of Internal Medicine. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Carey MP, Carey KB, Maisto SA, Gordon CM, Weinhardt LS. Assessing sexual risk behaviour with the Timeline Followback (TLFB) approach: Continued development and psychometric evaluation with psychiatric outpatients. International Journal of STD & AIDS. 2001;12:365–375. doi: 10.1258/0956462011923309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance – United States, 2009. Surveillance Summaries, June 4, 2010. Morbidity and Mortality Weekly Report. 2010;59(SS-5):1–142. Retrieved from http://www.cdc.gov/mmwr/pdf/ss/ss5905.pdf. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV among youth. 2011. Retrieved from http://www.cdc.gov/hiv/pdf/library_factsheet_HIV_amongYouth.pdf.
- Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2011. 2012a. Retrieved from http://www.cdc.gov/std/stats11/Surv2011.pdf.
- Centers for Disease Control and Prevention. STD trends in the United States: 2011 National data for chlamydia, gonorrhea, and syphilis. 2012b. Retrieved from http://www.cdc.gov/std/stats11/trends-2011.pdf.
- Chung T, Colby SM, Barnett NP, Rohsenow DJ, Spirito A, Monti PM. Screening adolescents for problem drinking: performance of brief screens against DSM-IV alcohol diagnoses. Journal of Studies on Alcohol. 2000;61:579–587. doi: 10.15288/jsa.2000.61.579. [DOI] [PubMed] [Google Scholar]
- Dariotis JK, Sonenstein FL, Gates GJ, Capps R, Astone NM, Pleck JH, Zeger S. Changes in sexual risk behavior as young men transition to adulthood. Perspectives on Sexual and Reproductive Health. 2008;40:218–225. doi: 10.1363/4021808. [DOI] [PubMed] [Google Scholar]
- Dennis M, Titus JC, Diamond GS, Donaldson J, Godley SH, Tims FM, Scott CK, C. Y. T. Steering Committee Scott, C. K., & the C. Y. T. Steering Committee. The Cannabis Youth Treatment (CYT) experiment: Rationale, study design and analysis plans. Addiction, 97, Supplement s1. 2002:16–34. doi: 10.1046/j.1360-0443.97.s01.2.x. [DOI] [PubMed] [Google Scholar]
- Donovan JE. Problem-behavior theory and the explanation of adolescent marijuana use. Journal of Drug Issues. 1996;26:379–404. [Google Scholar]
- Ehrlich PF, Maio R, Drongowski R, Wagaman M, Cunningham R, Walton MA. Alcohol interventions for trauma patients are not just for adults: Justification for brief interventions for the injured adolescent at a pediatric trauma center. Journal of Trauma. 2010;69:202–210. doi: 10.1097/TA.0b013e3181df646a. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, Collins RL, Bogart LM, Klein DJ, Taylor SL. Scope of HIV risk and co-occurring psychosocial health problems among young adults: Violence, victimization, and substance use. Journal of Adolescent Health. 2005;36:401–409. doi: 10.1016/j.jadohealth.2004.06.008. [DOI] [PubMed] [Google Scholar]
- Ford JA, Arrastia MC. Pill-poppers and dopers: A comparison of non-medical prescription drug use and illicit/street drug use among college students. Addictive Behaviors. 2008;33:934–941. doi: 10.1016/j.addbeh.2008.02.016. [DOI] [PubMed] [Google Scholar]
- Gillmore MR, Chen AC, Haas SA, Kopak AM, Robillard AG. Do family and parenting factors in adolescence influence condom use in early adulthood in a multiethnic sample of young adults? Journal of Youth and Adolescence. 2011;40:1503–1518. doi: 10.1007/s10964-011-9631-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris K, Florey F. The national longitudinal study of adolescent health: Study design. 2003. Retrieved from http://www.cpc.unc.edu/projects/addhealth/design.
- Harrison LD, Martin SS, Enev T, Harrington D. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2007. Comparing drug testing and self-report of drug use among youths and young adults in the general population (DHHS Publication No. SMA 07–4249, Methodology Series M-7) Retrieved from http://www.samhsa.gov/data/nsduh/drugtest.pdf. [Google Scholar]
- Hendershot CS, Magnan RE, Bryan AD. Associations of marijuana use and sex-related marijuana expectancies with HIV/ STD risk behavior in high-risk adolescents. Psychology of Addictive Behaviors. 2010;24:404–414. doi: 10.1037/a0019844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, Simon S. Validation of the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) Addiction. 2008;103:1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- Jessor R. Problem behavior and developmental transition in adolescence. Journal of School Health. 1982;52:295–300. doi: 10.1111/j.1746-1561.1982.tb04626.x. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2011. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2012a. Retrieved from http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2011.pdf. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2011: Volume II, College students and adults ages 19–50. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2012b. [Google Scholar]
- Kiene SM, Barta WD, Tennen H, Armeli S. Alcohol, helping young adults to have unprotected sex with casual partners: Findings from a daily diary study of alcohol use and sexual behavior. Journal of Adolescent Health. 2009;44:73–80. doi: 10.1016/j.jadohealth.2008.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotchick BA, Shaffer A, Forehand R, Miller KS. Adolescent sexual risk behavior: A multi-system perspective. Clinical Psychology Review. 2001;21:493–519. doi: 10.1016/s0272-7358(99)00070-7. [DOI] [PubMed] [Google Scholar]
- McCabe SE. Correlates of nonmedical use of prescription benzodiazepine anxiolytics: Results from a national survey of U.S. college students. Drug and Alcohol Dependence. 2005;79:53–62. doi: 10.1016/j.drugalcdep.2004.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Teter CJ, Boyd CJ. Co-ingestion of prescription opioids and other drugs among high school seniors: Results from a national study. Drug and Alcohol Dependence. 2012;126:65–70. doi: 10.1016/j.drugalcdep.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monti PM, Barnett NP, Colby SM, Gwaltney CJ, Spirito A, Rohsenow DJ, Woolard R. Motivational interviewing versus feedback only in emergency care for young adult problem drinking. Addiction. 2007;102:1234–1243. doi: 10.1111/j.1360-0443.2007.01878.x. [DOI] [PubMed] [Google Scholar]
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, Lewander W. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- National Center for Education Statistics. Digest of Education Statistics. Table 213. 2011. Retrieved from http://nces.ed.gov/programs/digest/d11/tables/dt11_213.asp.
- National Center for Education Statistics. The Condition of Education 2012 (NCES 2012-045), Indicator 33. 2012. Retrieved from http://nces.ed.gov/pubs2012/2012045.pdf.
- National Institute on Drug Abuse. Drug Abuse Treatment Outcome Study—Adolescent (DATOS-A), 1993-1995: [United States]. (ICPSR03404-v3) Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 2008. Retrieved from http://www.icpsr.umich.edu/icpsrweb/SAMHSA/studies/3404. [Google Scholar]
- Nkansah-Amankra S, Diedhiou A, Agbanu HLK, Harrod C, Dhawan A. Correlates of sexual risk behaviors among high school students in Colorado: Analysis and implications for school-based HIV/ AIDS programs. Maternal and Child Health Journal. 2011;15:730–741. doi: 10.1007/s10995-010-0634-3. [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LAJ, Carey MP, Carey KB. Alcohol and risky sexual behavior among heavy drinking college students. AIDS and Behavior. 2010;14:845–853. doi: 10.1007/s10461-008-9426-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieving RE, Beuhring T, Resnick MD, Bearinger LH, Shew M, Ireland M, Blum RW. Development of adolescent self-report measures from the National Longitudinal Study of Adolescent Health. Journal of Adolescent Health. 2001;28:73–81. doi: 10.1016/s1054-139x(00)00155-5. [DOI] [PubMed] [Google Scholar]
- Simpson CA, Xie L, Blum ER, Tucker JA. Agreement between prospective interactive voice response telephone reporting and structured recall reports of risk behaviors in rural substance users living with HIV/AIDS. Psychology of Addictive Behaviors. 2011;25:185–190. doi: 10.1037/a0022725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone AL, Becker LG, Huber AM, Catalano RF. Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive Behaviors. 2012;37:747–775. doi: 10.1016/j.addbeh.2012.02.014. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Volume 1. Summary of National Findings (NSDUH Series H-38A, HHS Pub. No. SMA 10-4586) Rockville, MD: Author; 2010. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings (NSDUH Series H-41, HHS Publication No. SMA 11-4658) Rockville, MD: Author; 2011. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Mental health findings and detailed tables. 2012. Retrieved from http://www.samhsa.gov/data/NSDUH/2k11MH_FindingsandDetTables/Index.aspx.
- Thornberry TP, Krohn MD. The self-report method of measuring delinquency and crime. In: Duffee D, editor. Measurement and analysis of crime and justice: Criminal Justice 2000. Washington, DC: U.S. Department of Justice, Office of Justice Programs; 2000. [Google Scholar]
- Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: Increased reporting with computer survey technology. Science. 1998;280:867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, Cunningham RM. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: A randomized controlled trial. Journal of the American Medical Association. 2010;304:527–535. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Resko S, Whiteside L, Zimmerman MA, Chermack ST, Cunningham RM. Sexual risk behaviors among teens at an inner city emergency department: Relationship to violent behaviors and substance use. Journal of Adolescent Health. 2011;48:303–305. doi: 10.1016/j.jadohealth.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb PM, Zimet GD, Fortenberry JD, Blythe MJ. Comparability of a computer-assisted versus written method for collecting health behavior information from adolescent patients. Journal of Adolescent Health. 1999;24:383–388. doi: 10.1016/s1054-139x(99)00005-1. [DOI] [PubMed] [Google Scholar]
- WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability, and feasibility. Addiction. 2002;97:1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- Young AM, Glover N, Havens JR. Nonmedical use of prescription medications among adolescents in the United States: A systematic review. Journal of Adolescent Health. 2012;51:6–17. doi: 10.1016/j.jadohealth.2012.01.011. [DOI] [PubMed] [Google Scholar]