Abstract
Objective:
Conduct disorder and depression symptoms are well-established risk factors for substance use during adolescence. However, few investigations have examined whether early substance use increases adolescents’ risk of developing conduct disorder/depression symptoms.
Method:
Using the Developmental Pathways Project sample of 521 middle school students (51.6% male), we tested whether substance use (indicated by alcohol and marijuana use, and use-related impairment) in 8th and 9th grade increased risk of conduct disorder and depression symptoms in 9th and 12th grade over and above prior symptoms. We examined whether associations between substance use and conduct disorder/depression symptoms were consistent across self- or parent-reported symptoms and whether associations were moderated by gender.
Results:
Analyses indicated that, over and above prior symptoms, elevated substance use in 8th grade predicted elevated conduct disorder symptoms in 9th grade, and substance use in 9th grade predicted conduct disorder symptoms in 12th grade. In contrast, substance use failed to predict later depression symptoms independent of prior symptoms. These findings were consistent across self- and parent-reported conduct disorder/depression symptoms. With one exception (association between substance use in 8th grade and self-reported conduct disorder symptoms in 9th grade), relations between early substance use and later conduct disorder symptoms did not differ between boys and girls.
Conclusions:
Study findings underscore the unique contribution of substance use during early adolescence to the development of conduct disorder symptoms by late adolescence.
By 12th grade, most adolescents have used alcohol, a high proportion have used marijuana, and many have histories of conduct disorder or depression (Johnston et al., 2012; Merikangas et al., 2010). Developmental theorists have articulated both externalizing and internalizing pathways to alcohol and other drug use (e.g., Hussong et al., 2011; Zucker et al., 2011). Indeed, studies have demonstrated prospective associations between early conduct disorder and depression symptoms and alcohol and illicit drug use during adolescence (e.g., Loeber et al., 1999; McCarty et al., 2012). Fewer studies, however, have investigated whether early substance use contributes to the development of conduct disorder and depression symptoms, despite a number of plausible explanatory mechanisms.
Adolescent substance use and development of conduct disorder
Early substance use may play a role in the development, maintenance, and escalation of conduct disorder symptoms during adolescence. Substance use may “ensnare” adolescents into prolonged patterns of antisocial behavior (Hussong et al., 2004). The physiological effects of intoxication in conjunction with situational provocation could also facilitate risk of adolescents engaging in aggressive and antisocial behavior (Felson and Staff, 2010; Ito et al., 1996).
Although substantially more studies have examined conduct disorder as a risk factor for substance use, evidence does indicate that substance use predicts the development of conduct disorder symptoms. For example, early- to mid-adolescent alcohol use has been shown to increase risk of self-reported aggression (Huang et al., 2001), juvenile offending (Wells et al., 2004), and antisocial personality disorder (Brook et al., 1998) by late adolescence or emerging adulthood. Using the same data set as examined in the current study, McCarty and colleagues (2012) found that any alcohol use at ages 12–14 predicted parent-reported, but not self-reported, conduct disorder symptoms the following year, over and above prior conduct disorder symptoms.
Because some alcohol use is normative in adolescence, we might expect to see stronger associations between substance use and conduct disorder symptoms when less socially sanctioned substances (e.g., marijuana) are investigated. Indeed, early- to mid-adolescent marijuana use has been shown to increase risk for violence and juvenile of fending by late adolescence (Fergusson and Horwood, 1997; White et al., 1999) and antisocial personality disorder by emerging adulthood (Brook et al., 1998). Conversely, it may be that patterns of early use across substances are the best predictor of developing conduct disorder symptoms during adolescence. Use of multiple substances at early ages may be indicative of more severe substance use problems that could exacerbate the development of conduct disorder. To our knowledge, only one study has explored the association between broad substance use and conduct disorder symptoms: Mason and Windle (2002) demonstrated that substance use (alcohol and marijuana use frequencies) at age 15.5 years prospectively predicted greater self-reported delinquent behavior at age 16. Studies are warranted to extend this preliminary work by illustrating that early substance use patterns are a risk factor for developing conduct disorder symptoms over a longer period. Moreover, given that nearly all prior studies were conducted with self-report data for substance use and conduct disorder symptoms, there is a need for studies using data collected from additional informants in order to rule out measurement bias.
Adolescent substance use and development of depression
There are reasons to suggest that substance use could be linked with growth of depression symptoms during adolescence (in addition to the development of conduct disorder symptoms), although less research has addressed this association. Problematic alcohol or marijuana use may have physiological or psychological effects that take the form of depression symptoms (Schuckit, 2006), as has been found for adult heavy users (Fergusson et al., 2009). Excessive use is also associated with neurocognitive dysfunction and impairment in educational and interpersonal functioning (Sher et al., 2007; Tapert et al., 2004), which could worsen depression symptoms in adolescence.
Studies of alcohol use as a risk factor for later depression symptoms indicate that the strength of association varies depending on how alcohol use is measured. Frequency of alcohol use does not predict development of self-reported depression symptoms (Mason et al., 2008). Positive associations have been demonstrated, however, between heavy episodic drinking or alcohol-induced impairment and later depression symptoms during adolescence (Hallfors et al., 2005; Mason et al., 2008). Conversely, research suggests that marijuana use, regardless of how it is measured, increases risk of subsequent depression symptoms. For example, Brook and colleagues (2002) found that more frequent marijuana use by age 14 increased risk of self-reporting depression by age 26. Similarly, growth in illicit drug use frequency from early- to mid-adolescence was shown to predict more self-reported internalizing symptoms in emerging adulthood, independent of earlier adolescent internalizing symptoms (Trim et al., 2007).
Although alcohol and marijuana use may contribute individually to the development of depression symptoms during adolescence, patterns of early use across substances may be the most reliable risk factor for depression symptoms. Only one study has investigated whether broad substance use (including cigarette and alcohol use frequencies) prospectively predicted depression symptoms, with null results (Mason et al., 2009). More studies are needed to examine whether early patterns of substance use increase the development of depression symptoms. In addition, only one study (Trim et al., 2007) investigated whether substance use increased risk of depression symptoms while conduct disorder symptoms were controlled for. Because the association between early substance use and later depression symptoms may be driven by their association with conduct disorder symptoms, it is crucial to examine substance use as a unique predictor of depression symptoms over and above conduct disorder symptoms.
Gender differences
In light of gender differences in the prevalence of substance use, conduct disorder, and depression during adolescence, the strength of prospective associations also may vary between boys and girls. For example, relative to girls, adolescent boys are more likely to engage in substance use, particularly high-risk use (Johnston et al., 2012), and exhibit externalizing behavior problems (Merikangas et al., 2010). This may explain why Mason and Windle (2002) found that substance use predicted delinquency among boys but not girls. In contrast, adolescent girls are more likely than boys to experience depression (e.g., Merikangas et al., 2010). Still, studies exploring gender as a moderator of the association between adolescent substance use and depression symptoms have yielded mixed results. Patton and colleagues (2002) observed that prospective associations between marijuana use and depression symptoms were more likely among mid-adolescent girls compared with boys. Hallfors et al. (2005) found that mid-adolescent male, but not female, marijuana users were more likely to report elevated depression symptoms 1 year later compared with those who abstained from using marijuana. The same study also found that alcohol use predicted greater depression symptoms in girls but not boys. Other studies found no gender differences in associations between specific substances (Needham, 2007; Trim et al., 2007) or substance use patterns (Mason et al., 2009) in the prediction of depression symptoms. In sum, research is needed to clarify whether the strength of association between substance use and conduct disorder/depression symptoms differs for boys and girls.
Study goals and hypotheses
This study used structural equation modeling to investigate prospective associations between early adolescent substance use and the development of conduct disorder and depression symptoms by late adolescence. Prior studies mainly used simple linear regression or path analyses to assess for prospective associations between forms of adolescent substance use and either conduct disorder or depression symptoms. The chief drawback of those methods is that they do not allow for an evaluation of substance use patterns as a predictor of subsequent conduct disorder or depression symptoms. This is noteworthy, as it may be that levels of use across substances are more meaningful in the development of conduct disorder or depression symptoms than levels of specific substances. Studies testing models that include both conduct disorder and depression symptoms as outcomes are also needed to explicitly test whether the magnitude of these associations is different.
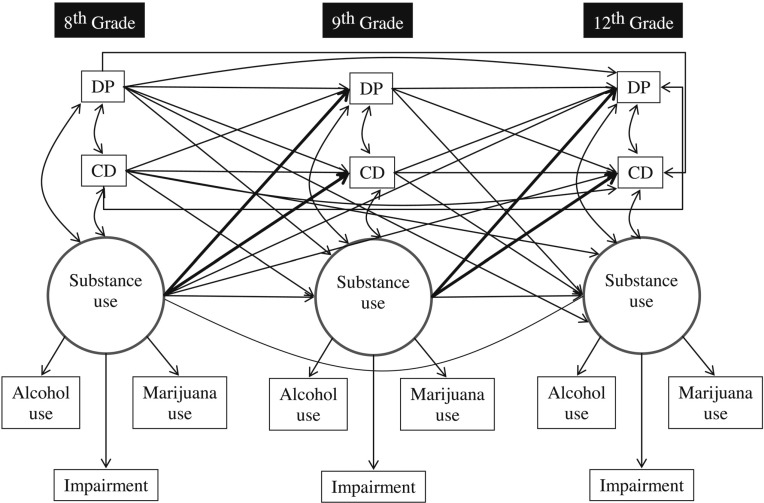
We tested whether substance use involvement in 8th and 9th grades, as indicated by self-reported alcohol and marijuana use and impairment caused by use of either substance, was prospectively associated with self- and parent-reported conduct disorder and depression symptoms in 9th and 12th grades, over and above prior symptoms (Figure 1). We hypothesized that greater patterns of substance use during 8th and 9th grades would be associated with greater conduct disorder and depression symptoms in 9th and 12th grades. Because early substance use is considered to be part of the broader “externalizing behaviors spectrum” (Krueger et al., 2002), we expected that early patterns of substance use would be more strongly associated with conduct disorder symptoms than with depression symptoms. We also examined whether youth-reported substance use would be differentially associated with self- and parent-reported conduct disorder and depression symptoms, with the hypothesis that more robust associations would be found for youth ratings of both substance use and conduct disorder/depression symptoms. Finally, as an exploratory aim, we tested whether gender moderated prospective associations between early substance use and later conduct disorder and depression symptoms.
Figure 1.
Model tested to examine latent substance use in 8th and 9th grade as risk factors for conduct disorder (CD) and depression (DP) symptoms in 12th grade. Residual errors for latent indicators and outcome variables were estimated but were omitted here to preserve space and enhance clarity. Regression paths of interest are bolded.
Method
Sample
The Developmental Pathways Project (DPP) is a community-based prospective cohort study designed to examine the antecedents, phenomenology, and outcomes of depression and conduct disorder in early adolescence. DPP participants were recruited from four Seattle-area public schools located in distinct areas within the city and together have a racial/ ethnic distribution that is nearly identical to the total enrolled student population of the school district. Universal emotional health screening was carried out with sixth-grade students at these schools in 4 consecutive years (2001–2004), details of which have been described elsewhere (Vander Stoep et al., 2005). Procedures were approved by the University of Washington Human Subjects Review Board and by the Seattle Public Schools Office of Research, Evaluation, and Assessment.
Students eligible for screening were sixth graders who had a third-grade reading comprehension level or higher. Of the 2,920 eligible students, 2,187 (74.9%) were screened. Following screening, a random sample of students, stratified by their scores on the Mood and Feelings Questionnaire for depression symptoms (Costello and Angold, 1988) and Youth Self Report externalizing scale for conduct disorder symptoms (Achenbach and Rescorla, 2001), were identified for participation in the longitudinal study.
A stratified random sample of 807 students was selected for longitudinal follow-up, with students scoring high (>0.5 SD above sample mean) on depression and/or conduct disorder symptoms oversampled according to a ratio of 1:1:1:2 from the four psychopathology screening groups (comorbid depression and conduct disorder, depression only, conduct disorder only, elevated on neither depression nor conduct disorder). This sample selection approach yielded an over-representation of children in the comorbid, depression, and conduct disorder groups relative to their distribution in the general population. Of those selected, 521 (64.6%) students and their parents/guardians consented to participate in the DPP (described in Vander Stoep et al., 2011). At baseline, participants were 12.0 years old on average (range: 11–13.6), and 51.6% were male. Of the total participants, 39.5% were White, 24.9% Black, 24.1% Asian/Pacific Islander, 10.1% Hispanic, and 1.4% Native American. Nearly half (48.1%) were raised in households with a total income less than $50,000.
In-home interviews were conducted with participating students and parents/guardians (76% biological mothers, 15% biological fathers, 9% other relatives) by two trained research interviewers who were blind to participants' psychopathology risk group status. Baseline interviews were conducted within 3 months of screening (fall 6th grade), and in-person follow-up interviews were conducted 6, 12, 18, 24, 36, and 72 months afterward (through fall 12th grade). Of the participants originally enrolled in DPP, 91% were retained through 12th grade. Data from 8th-, 9th-, and 12th-grade assessments were used in this study.
Measures
Substance use involvement.
The Customary Drinking and Drug Use Record (Brown et al., 1998) was administered in eighth and ninth grade to assess alcohol and marijuana use frequency in the past 6 months. Adolescent responses regarding alcohol and marijuana use ranged from 0 (never used) to 7 (used more than once per day). The Customary Drinking and Drug Use Record was validated in a community sample of adolescents, demonstrating good test–retest reliability over 1 week, convergent validity, and interrater reliability (Brown et al., 1998).
The Alcohol and Marijuana Abuse and Dependence modules from the young adult version of the Voice-Diagnostic Interview Schedule for Children (V-DISC) were administered in 12th grade to ascertain the level of adolescent alcohol and marijuana use. The V-DISC has comparable reliability with other versions of the DISC (Wasserman et al., 2002, 2004). In this study, symptoms of abuse and dependence endorsed as occurring within the past year were summed to form symptom counts for alcohol (range: 0–12) and marijuana use (range: 0–11).
A modified version of the 23-item Rutgers Alcohol Problem Index (White and Labouvie, 1989) was administered in 8th, 9th, and 12th grades to measure negative marijuana and alcohol use–related consequences within the past 6 months. Adolescents reported their level of use-related impairment in personal, social, and academic functioning domains on a 5-point Likert-type scale ranging from 0 (never) to 4 (>10 times). The Rutgers Alcohol Problem Index has demonstrated good test–retest reliability as well as discriminant and construct validity in general and clinical samples of adolescents (Miller et al., 2002; White and Labouvie, 1989), as well as reliability when assessing consequences of using substances other than alcohol (Ginzler et al., 2007).
Conduct disorder and depression symptoms.
As part of the 8th-, 9th-, and 12th-grade assessments, the DISC was administered (Shaffer et al., 2000). The DISC has well-established psychometric properties, including good test–retest reliability and concurrent validity for conduct disorder and depression diagnoses (Schwab-Stone et al., 1996). Adolescents and their parents completed the conduct disorder and depression DISC modules. Conduct disorder and depression symptoms endorsed as occurring within the past year were summed to form symptom counts for conduct disorder (range: 0–26) and depression (range: 0–22).
Analytic plan
First, a confirmatory factor analysis (CFA) model was conducted to examine the fit of the 8th-, 9th-, and 12th-grade latent substance use variables (indicators: alcohol use, marijuana use, and use-related impairment) while correlating them with 8th-, 9th-, and 12th-grade conduct disorder and depression symptom manifest variables. Next, within a structural equation model (SEM), we investigated whether latent substance use in 8th and 9th grades predicted conduct disorder and depression symptoms in 9th and 12th grades over and above prior symptoms (Figure 1). Models were run separately for adolescent- and parent-reported conduct disorder and depression symptoms. Next, we tested for model invariance for adolescent boys and girls using multiple group analyses. All structural paths were first allowed to vary across boys and girls. Then, in turn, only paths that were statistically significant in the pooled sample model (e.g., 9th-grade substance use → 12th-grade conduct disorder symptoms) were tested for invariance across gender. Chi-square difference tests compared the gender-nested model with the base model. If the constrained structural path (fixing pathways for boys and girls to be equivalent) did not cause model fit to worsen significantly over the base model, as evaluated by the Satorra-Bentler scaled chi-square difference test (Muthén and Muthén, 2010), then the strength of the association was considered to be the same for boys and girls. Conversely, if constraining the structural path of interest to be equal caused model fit to worsen significantly, then the strength of the association was considered different for boys and girls.
Model estimation was conducted with Mplus 6.1 (Muthén and Muthén, 2010) using the maximum likelihood estimator with robust standard errors. Model fit was assessed using χ2/df, root mean square error of approximation (RMSEA), and comparative fit index (CFI). All participants contributed at least some data to these analyses; full-information maximum likelihood estimates were used to account for missing data. Preliminary analyses indicated that participants with any missing data (n = 203) were more likely to be older, ethnic minorities, and to have lower family income compared with participants with no missing data (n = 318). These variables were included as covariates in all analyses.
Results
Descriptive statistics for substance use variables and conduct disorder and depression symptom counts are presented in Table 1. Although boys and girls reported similar levels of alcohol use, marijuana use, and use-related impairment in 8th and 9th grades, there were significant gender differences in 12th grade. Relative to girls, 12th-grade boys reported greater alcohol use, marijuana use, and use-related impairment. There also were gender differences in conduct disorder and depression symptoms. Girls reported more depression symptoms than boys across 8th, 9th, and 12th grades, whereas boys reported more conduct disorder symptoms than girls across 8th, 9th (marginal), and 12th grades. Parents also reported that boys exhibited significantly more conduct disorder symptoms across grades but did not report gender differences in depression symptoms in 8th, 9th, or 12th grades.
Table 1.
Descriptive statistics for substance use, conduct disorder, and depression variables
| Variable | Girls (n = 249) | Boys (n = 272) | p |
| M (SD) | M (SD) | ||
| Alcohol use, 8th grade | 0.21 (0.64) | 0.15 (0.68) | .34 |
| Marijuana use, 8th grade | 0.17(0.72) | 0.20 (0.94) | .66 |
| Use-related impairment, 8th grade | 0.62 (2.70) | 1.09(6.35) | .29 |
| Alcohol use, 9th grade | 0.56(1.00) | 0.40 (0.88) | .08 |
| Marijuana use, 9th grade | 0.42(1.19) | 0.49(1.26) | .60 |
| Use-related impairment, 9th grade | 2.31 (7.15) | 2.02 (5.52) | .64 |
| Alcohol use, 12th grade | 0.74 (2.01) | 1.15(2.17) | .03 |
| Marijuana use, 12th grade | 0.76(1.90) | 1.42(2.46) | <.01 |
| Use-related impairment, 12th grade | 3.35 (7.50) | 5.03 (8.48) | .02 |
| CD-self, 8th grade | 2.32 (3.05) | 2.96 (3.39) | .04 |
| DP-self, 8th grade | 5.96 (4.85) | 4.24 (3.82) | <.01 |
| CD-self, 9th grade | 3.24 (3.66) | 3.94 (3.68) | .06 |
| DP-self, 9th grade | 6.53 (4.76) | 4.55 (3.64) | <.01 |
| CD-self, 12th grade | 4.25 (3.71) | 6.09 (4.38) | <.01 |
| DP-self, 12th grade | 8.12(5.40) | 6.20 (4.44) | <.01 |
| CD-parent, 8th grade | 1.73 (2.41) | 2.56 (3.04) | <.01 |
| DP-parent, 8th grade | 3.64 (3.58) | 3.85 (3.45) | .53 |
| CD-parent, 9th grade | 1.92 (2.70) | 2.84(3.12) | <.01 |
| DP-parent, 9th grade | 3.81 (3.72) | 3.98 (3.59) | .65 |
| CD-parent, 12th grade | 3.13(3.35) | 4.16(3.90) | <.01 |
| DP-parent, 12th grade | 5.08 (4.10) | 4.56 (3.97) | .19 |
Notes: 8th- and 9th-grade alcohol and marijuana use were assessed using the Customary Drinking and Drug Use Record, with scores ranging from 0 (never used) to 7 (used more than once per day). 12th-grade alcohol and marijuana use were measured using the Diagnostic Interview Schedule for Children (DISC)–Young adult version, with scores ranging from 0 to 12. Use-related impairment scores ranged from 0 to 74. CD = DISC symptom count for adolescent conduct disorder; DP = DISC symptom count for adolescent depression.
Intercorrelations among substance use and symptom variables are presented in Table 2. Overall, early substance use tended to be more strongly associated with later conduct disorder symptoms than with depression symptoms. This pattern appears across gender and informant (self- vs. parent-report).
Table 2.
Intercorrelations among 9th-grade substance use predictors and conduct disorder/depression symptom counts
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | 17. | 18. | 19. | 20. | 21. |
| 1. Alcohol, 8th grade | – | .38** | .48** | .37** | .32** | .33** | .08 | .25** | .19** | .22** | .24** | .23** | .10 | .24** | .13 | .08 | .06 | .28** | .04 | .19** | .12 |
| 2. Marijuana, 8th grade | .48** | – | .73** | .31** | .62** | .24** | .09 | .41** | .18* | .45** | .19** | .37** | .06 | .35** | .15* | .14 | .03 | .19** | -.02 | .35** | .05 |
| 3. Impairment, 8th grade | .51** | .74** | – | .28** | .45** | .36** | .14* | .37** | .17* | .47** | .30** | .31** | .17* | .33** | .15* | .16* | .15* | .30** | .05 | .33** | .08 |
| 4. Alcohol, 9th grade | .19** | .10 | .06 | – | .49** | .52** | .19** | .32** | .28** | .24** | .10 | .29** | .04 | .27** | .07 | .10 | .04 | .17* | .09 | .22** | .06 |
| 5. Marijuana, 9th grade | .24** | .35** | .13 | .56** | – | .45** | .21** | .37** | .36** | .42** | .11 | .38** | .08 | .35** | .14* | .18* | .03 | .24** | .07 | .30** | .01 |
| 6. Impairment, 9th grade | .23** | .36** | .21** | .57** | .78** | – | .11 | .35** | .34** | .39** | .18* | .43** | .22** | .43** | .13 | .22** | .04 | .33** | .11 | .38** | .01 |
| 7. Alcohol, 12th grade | .09 | .05 | .05 | .19** | .32** | .35** | – | .33** | .63** | .08 | .08 | .14* | .14* | .31** | .18* | .06 | .08 | .08 | .07 | .22** | .14* |
| 8. Marijuana, 12th grade | .26** | .22** | .19** | .24** | .53** | .48** | .58** | – | .62** | .19** | .20** | .16* | .19** | .37** | .28** | .10 | .11 | .17* | .13 | .40** | .14* |
| 9. Impairment, 12th grade | .19** | .19** | .15* | .13 | .39** | .29** | .54** | .73** | – | .10 | .18* | .17* | .12 | .36** | .26** | .09 | .05 | .02 | .11 | .26** | .14* |
| 10. CD-self, 8th grade | .42** | .46** | .47** | .27** | .31** | .38** | .05 | .24** | .22** | – | .36** | .77** | .29** | .71** | .31** | .52** | .21** | .51** | .19** | .51** | .13 |
| 11. DP-self, 8th grade | .05 | .11 | .19** | .13 | .06 | .11 | -.03 | .08 | .06 | .35** | – | .40** | .71** | .33** | .58** | .17* | .26** | .12 | .16* | .24** | .21** |
| 12. CD-self, 9th grade | .32** | .44** | .36** | .31** | .34** | .36** | .19** | .20** | .31** | .73** | .28** | – | .40** | .76** | .31** | .53** | .16* | .49** | .17* | .56** | .12 |
| 13. DP-self, 9th grade | .10 | .21** | .24** | .16* | .15* | .24** | .14* | .10 | .16* | .22** | .65** | .39** | – | .32** | .58** | .15* | .23** | .13 | .18* | .19** | .10 |
| 14. CD-self, 12th grade | .23** | .29** | .22** | .23** | .36** | .25** | .37** | .46** | .46** | .49** | .07 | .64** | .19** | – | .42** | .52** | .24** | .59** | .32** | .68** | .22** |
| 15. DP-self, 12th grade | .11 | .09 | .10 | .02 | .02 | .01 | .17* | .16* | .30** | .14* | .38** | .27** | .43** | .41** | – | .17* | .32** | .13 | .28** | .28** | .39** |
| 16. CD-parent, 8th grade | .13 | .38** | .28** | .14* | .22** | .29** | .06 | .11 | .12 | .43** | .08 | .45** | .21** | .47** | .09 | – | .38** | .74** | .34** | .70** | .28** |
| 17. DP-parent, 8th grade | .08 | .17* | .17* | .02 | .02 | -.03 | .03 | .10 | .13 | .08 | .12 | .23** | .17* | .33** | .33** | .34** | – | .26** | .66** | .30** | .51** |
| 18. CD-parent, 9th grade | .31** | .42** | .36** | .09 | .30** | .23** | .15* | .29** | .28** | .44** | .09 | .48** | .16* | .56** | .19** | .67** | .31** | – | .32** | .79** | .22** |
| 19. DP-parent, 9th grade | .16* | .25** | .25** | .01 | .10 | -.01 | .02 | .09 | .15* | .11 | .16* | .27** | .30** | .34** | .27** | .25** | .64** | .41** | – | .40** | .60** |
| 20. CD-parent, 12th grade | .23** | .34** | .27** | .11 | .37** | .36** | .41** | .43** | .38** | .33** | .02 | .42** | .21** | .58** | .15* | .61** | .19** | .66** | .34** | – | .32** |
| 21. DP-parent, 12th grade | -.05 | .05 | .06 | -.03 | .07 | -.01 | .12 | .11 | .13 | -.05 | .12 | .11 | .22** | .15* | .31** | .24** | .54** | .27** | .53** | .34** | – |
Notes: Boys below diagonal, girls above diagonal. CD = Diagnostic Interview Schedule for Children (DISC) symptom count for adolescent conduct disorder; DP = DISC symptom count for adolescent depression.
p < .05;
p < .01.
Latent substance use and conduct disorder/depression symptoms
Adolescent-report data.
The CFA model fit the self-reported data adequately, χ2(60, N = 521) = 132.04, p < .001, χ2/df = 2.20, RMSEA = .05, CFI = .96. The indicators all loaded strongly on the latent substance use factor in 8th (βs > .63), 9th (βs > .62) and 12th (βs > .70) grades, and the variability of the latent variable was significant in 9th (variance = 0.34, SE = 0.08, p < .01) and 12th (variance = 2.27, SE = 0.68, p <.01) grades.
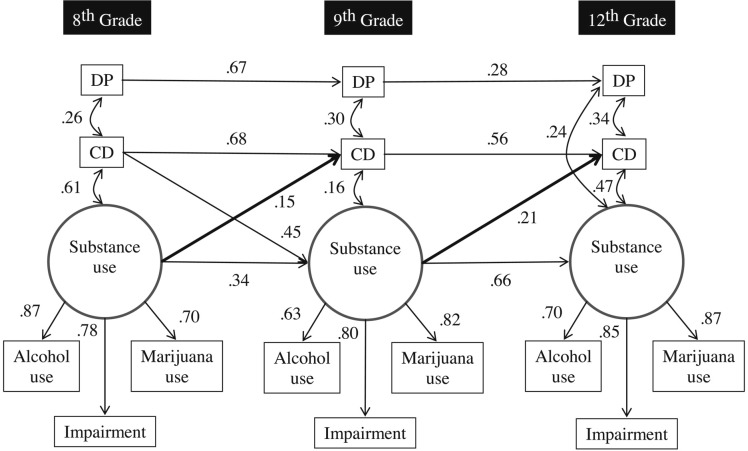
Next, regression paths from the latent variable to the outcomes were estimated. Because the SEM had the same number of regression paths as the CFA had correlational paths, the model fit was exactly the same. As shown in Figure 2, elevated substance use in 8th grade predicted greater self-reported conduct disorder symptoms in 9th grade over and above prior symptoms and within-time covariances. Similarly, substance use in 9th grade increased risk of self-reported conduct disorder symptoms in 12th grade over and above prior symptoms and within-time covariances. Substance use did not predict depression symptoms at either subsequent time point. It is notable that, because marijuana use in 8th and 9th grades had the strongest loading on the latent substance use variable, post hoc analyses explored 8th- and 9th-grade marijuana use as predictors of adolescent-reported conduct disorder symptoms in 9th and 12th grades holding constant all other paths in the model. This model fit very well, χ2(2, N = 506) = 2.18, p = .34, χ2/df = 1.09, RMSEA = .01, CFI = 1.00. In brief, we found that the strength of regression paths from 8th-grade marijuana use to 9th-grade conduct disorder symptoms (β = .15, p < .01) and from 9th-grade marijuana use to 12th-grade conduct disorder symptoms (β = .23, p < .01) were consistent with those found for latent substance use predicting conduct disorder symptoms (Figure 2).
Figure 2.
Latent substance use in 8th and 9th grade as risk factors for adolescent-reported conduct disorder (CD) and depression (DP) symptoms in 12th grade. Residual errors for latent indicators and outcome variables were estimated (and were significant) but were omitted here to preserve space and enhance clarity. Only significant paths (with standardized betas) and covariances are shown. Regression paths of interest are bolded.
Parent-report data.
The CFA model fit the data well when parent-reported conduct disorder and depression symptoms were included, χ2(60, N = 521) = 121.66, p < .01, χ2/df = 2.03, RMSEA = .04, CFI = .96. The indicators all loaded strongly on the latent substance use factor in 8th, 9th, and 12th grades (βs > .60), and the variability of the latent variable was significant in 9th (variance = 0.33, SE = 0.08, p < .01) and 12th (variance = 2.18, SE = 0.63,p < .01) grades.
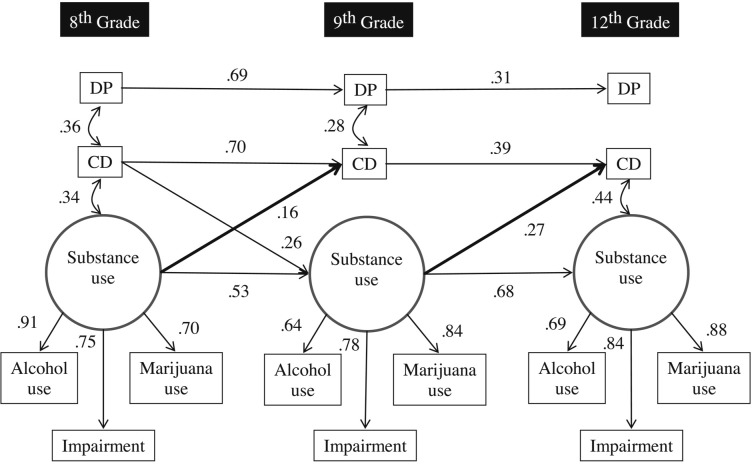
When regression paths from latent substance use to the outcomes were estimated as part of the SEM, elevated substance use in 8th and 9th grade was associated with increased parent-reported conduct disorder symptoms in 9th and 12th grades, respectively (Figure 3). As above, the fit of the SEM was identical to that of the CFA, and latent substance use did not predict later depression symptoms. Post hoc analyses explored 8th- and 9th-grade marijuana use as predictors of parent-reported conduct disorder symptoms in 9th and 12th grades. The model fit very well, χ2(2, N = 507) = 1.15, p = .56, χ2/df = 0.58, RMSEA = .00, CFI = 1.00, and showed that the strength of the path from 8th-grade marijuana use to 9th-grade conduct disorder symptoms (β = .11, p < .01) was consistent with the path from latent substance use to conduct disorder symptoms (Figure 3). However, the strength of the association between 9th-grade marijuana use and 12th-grade conduct disorder symptoms (β = .17, p < .01) was somewhat weaker than the association between latent substance use and conduct disorder symptoms.
Figure 3.
Latent substance use in 8th and 9th grade as risk factors for parent-reported conduct disorder (CD) and depression (DP) symptoms in 12th grade. Residual errors for latent indicators and outcome variables were estimated (and were significant) but were omitted here to preserve space and enhance clarity. Only significant paths (with standardized betas) and covariances are shown. Regression paths of interest are bolded.
Testing gender as moderator
Adolescent-report data.
The multiple-group model fit the adolescent-report data adequately, χ2(132, N = 521) = 275.88, p < .01, χ2/df = 2.09, RMSEA = .08, CFI = .94. Model fit worsened significantly when the path from substance use in 8th grade to self-reported conduct disorder symptoms in 9th grade was constrained to be equivalent across adolescent boys and girls, Δχ2(1) = 6.20, p < .05. Specifically, 8th-grade substance use was more strongly associated with 9th-grade conduct disorder symptoms in boys (β = .26, p < .01) than girls (β = -.01, p = .87). However, model fit did not worsen significantly when the path from 9th-grade substance use to 12th-grade parent-reported conduct disorder symptoms was constrained, Δχ2(1) = 1.13, p > .10), indicating no gender differences in associations between substance use in 9th grade and self-reported conduct disorder symptoms in 12th grade.
Parent-report data.
The multiple-group model fit the data well when parent-reported conduct disorder and depression symptoms were included, χ2(132, N = 521) = 261.86, p < .01, χ2/df = 1.98, RMSEA = .06, CFI = .93. Fit did not worsen significantly when the paths from substance use in 8th grade to parent-reported conduct disorder symptoms in 9th grade, Δχ2(1) = 2.00, p > .10, or from substance use in 9th grade to parent-reported conduct disorder symptoms in 12th grade, Δχ2(1) = 1.58, p > .10, were constrained to be equivalent across gender. Thus, the strength of prospective associations between substance use and later parent-reported conduct disorder symptoms did not differ between boys and girls.
Discussion
The current study examined early adolescent substance use as a risk factor for the development of conduct disorder and depression symptoms. We found that substance use involvement in 8th and 9th grades, as represented by latent factors including adolescent-reported alcohol and marijuana use and use-related impairment, increased risk of adolescent-and parent-reported conduct disorder symptoms in 9th and 12th grades over and above prior symptoms. Conversely, early substance use involvement did not uniquely predict later self- or parent-reported depression symptoms. Supplemental tests indicated that more frequent marijuana use might identify adolescents most likely to exhibit growth in conduct disorder symptoms over time. Tests of moderation by gender indicated that the association between substance use in 8th grade and self-reported conduct disorder symptoms in 9th grade was stronger in boys than in girls. Otherwise, the strength of the remaining associations between substance use and conduct disorder symptoms did not vary between boys and girls.
Given that substance use, particularly in early adolescence, is linked with other externalizing behaviors (Krueger et al., 2002), we were not surprised to find that substance use in 8th and 9th grades uniquely predicted greater conduct disorder symptoms in 9th and 12th grades, respectively. Yet, our study extends the research base in two ways. First, we built on work by Mason and Windle (2002), who conducted the only previous study demonstrating that patterns of substance use, including alcohol and marijuana, prospectively predicted the development of delinquent behavior during adolescence. Not only did we find that a broad measure of adolescent substance use predicted the development of conduct disorder symptoms, we also showed that substance use increased risk of conduct disorder symptoms at two time points (9th and 12th grades) and over a longer period (1 and 3 years). These results suggest that high-risk patterns of early use across multiple substances, rather than early use of any single substance, may play a key role in the development of conduct disorder symptoms by late adolescence. However, secondary tests demonstrated that marijuana use in 8th and 9th grades was as strong a predictor of 9th- and 12th-grade conduct disorder symptoms, at least those reported by adolescents, as was latent substance use. Therefore, use of less socially sanctioned substances (marijuana in particular) may be as likely to identify adolescents at risk for growth in conduct disorder symptoms as those exhibiting patterns of elevated use across substances.
Second, this was the first study to demonstrate prospective associations between early adolescent substance use and both self- and parent-reported conduct disorder symptoms in late adolescence. Prior studies in this age range only evaluated for associations between self-reported substance use and conduct disorder symptoms. This cross-informant consistency increases our confidence in the contribution of early substance use patterns to the maintenance and escalation of conduct disorder from early to late adolescence. However, we did not find that 9th-grade marijuana use was as strong a predictor of 12th-grade conduct disorder symptoms reported by parents as it was for predicting symptoms reported by adolescents.
Regardless of the informant, we found that early use did not increase risk of developing depression symptoms. Our results contrast with results from several other studies, which indicate prospective links between heavy alcohol use (Hallfors et al., 2005; Mason et al., 2008) and marijuana/illicit drug use (Brook et al., 2002; Trim et al., 2007) and later depression symptoms. It may be that our findings underscore the limited unique association between early substance use and depression independent of conduct disorder symptoms. Notably, one prior study (Trim et al., 2007) covaried baseline externalizing symptoms and found significant prospective associations between growth in illicit drug use and later internalizing symptoms. Trim and colleagues may have found an association, where we did not, because they used broader measures of substance use (including marijuana and seven other illicit drugs) and internalizing symptoms (depression and anxiety symptoms). Our sample did not endorse much use of illicit drugs beyond marijuana (e.g., only 1.8% of 8th graders and 1.8% of 9th graders, respectively), thereby prohibiting us from including additional illicit drugs as risk factors for psychopathology. Variability in use of illicit drugs may have been greater in the sample used by Trim et al.; it comprised children of alcoholics, whereas ours was a community sample. In addition, Trim and colleagues investigated prediction of internalizing symptoms in young adulthood, whereas we focused on prediction of depression by late adolescence.
It is notable that boys reporting elevated substance use involvement in 8th grade were more likely than girls reporting similar use patterns to self-report elevated conduct disorder symptoms in 9th grade. This finding replicates those of Mason and Windle (2002), who also found evidence that early adolescent substance use predicted greater conduct disorder symptoms in boys but not in girls. On the other hand, there was no difference between boys and girls in the strength of association between 9th-grade substance use and 12th-grade self-reported conduct disorder symptoms and paths to parent-reported conduct disorder symptoms in 9th and 12th grades. Thus, on the whole, the contribution of substance use toward the development of conduct disorder symptoms was not moderated by gender.
Although this study has many notable strengths (e.g., large, diverse sample; multiple informants; modeling latent substance use at multiple time points), several weaknesses limit the conclusions we draw. First, our sample comprises youths residing in the metropolitan area of Seattle, where substance use patterns may differ from those of youths in other parts of the country. Second, there was no external validation of adolescent self-reported substance use; however, other research indicates that self-report surveys assessing substance use like those used in this study are reliable and valid (Shillington and Clapp, 2000). Third, although our broad factor of substance use included two of the most frequently used substances in adolescence (alcohol and marijuana; Johnston et al., 2012), it did not include tobacco or illicit drugs, owing to low base rates in this sample and poor fit with the other substances we included. As such, our results may not generalize to studies including tobacco or other illicit drugs as indicators of latent substance use (e.g., Trim et al., 2007).
Fourth, because one of our research questions was to control for response bias by having different informants (adolescent and parents) rate predictor and outcome variables, and because we did not have multiple measures of conduct disorder or depression symptoms rated by each informant, we relied on manifest variables as outcomes in this study. Using manifest, and not latent, variables to represent conduct disorder and depression symptoms may have increased bias in our models due to measurement error and relying on the perceptions of a single rater. Fifth, associations between substance use and conduct disorder symptoms may be artificially increased because some conduct disorder behaviors could be consequences of drug use (e.g., stealing to money to buy drugs; see Brown et al., 1996). This could not be addressed in the current study because of the nature of the assessments. Sixth, other than including covariates associated with missing data in this sample that may also be associated with substance use, conduct disorder, and depression symptoms (e.g., household income), we did not control for antecedent factors that may be common among these variables across time. Thus, it is possible that our results are confounded by nonobserved third variables (e.g., family histories of alcoholism, conduct disorder, or depression). Last, we did not have any assessment points between 9th and 12th grades, which prohibited us from examining possible mechanisms explaining the prospective associations. For example, adolescents with elevated use patterns in 9th grade may have been more likely to associate with deviant peers over time (Kiesner et al., 2010), and these associations, not substance use, may have been the proximal risk factor exacerbating development of conduct disorder symptoms (Dishion et al., 2010).
Taken together, this study complements numerous studies that represent conduct disorder and depression symptoms as risk factors for substance use during adolescence by demonstrating risk in the reverse direction, specifically for conduct disorder symptoms. These data validate the importance of clinicians working with substance-using or conduct-disordered youths to assess and treat both of these behaviors concurrently (e.g., Henggeler and Schaeffer, 2010). This dual-pronged approach may be especially important for boys. In terms of prevention, delaying the initiation of alcohol and marijuana use should be important goals to reduce the incidence of conduct disorder and delinquency. Research is needed to examine potential moderators (e.g., clinical status) and mediators (e.g., peer deviance) of the longitudinal, bidirectional association between substance use and conduct disorder symptoms to determine best practices for future prevention and intervention efforts.
Footnotes
This research was supported by the National Institute on Alcohol Abuse and Alcoholism, National Institute of Mental Health, and National Institute on Drug Abuse under Award Numbers R01 AA018701 (to Carolyn A. McCarty) and R01 MH/DA63711 (to Ann Vander Stoep and Elizabeth McCauley). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work was also supported by Seattle Children's Hospital Steering Committee Grant and American Foundation for Suicide Prevention Grant (to Ann Vander Stoep) and UW Provost Bridge Funding (to Ann Vander Stoep and Elizabeth McCauley). Portions of the analyses were presented at the annual conference of the Research Society on Alcoholism, San Francisco, CA (June 2012).
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont; 2001. [Google Scholar]
- Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug use and the risk of major depressive disorder, alcohol dependence, and substance use disorders. Archives of General Psychiatry. 2002;59:1039–1044. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- Brook JS, Cohen P, Brook DW. Longitudinal study of co-occurring psychiatric disorders and substance use. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:322–330. doi: 10.1097/00004583-199803000-00018. [DOI] [PubMed] [Google Scholar]
- Brown SA, Gleghorn A, Schuckit MA, Myers MG, Mott MA. Conduct disorder among adolescent alcohol and drug abusers. Journal of Studies on Alcohol. 1996;57:314–324. doi: 10.15288/jsa.1996.57.314. [DOI] [PubMed] [Google Scholar]
- Brown SA, Myers MG, Lippke L, Tapert SF, Stewart DG, Vik PW. Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): A measure of adolescent alcohol and drug involvement. Journal of Studies on Alcohol. 1998;59:427–438. doi: 10.15288/jsa.1998.59.427. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Angold A. Scales to assess child and adolescent depression: Checklists, screens, and nets. Journal of the American Academy of Child and Adolescent Psychiatry. 1988;27:726–737. doi: 10.1097/00004583-198811000-00011. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Véronneau M-H, Myers MW. Cascading peer dynamics underlying the progression from problem behavior to violence in early to late adolescence. Development and Psychopathology. 2010;22:603–619. doi: 10.1017/S0954579410000313. [DOI] [PubMed] [Google Scholar]
- Felson RB, Staff J. The effects of alcohol intoxication on violent versus other offending. Criminal Justice and Behavior. 2010;37:1343–1360. [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. Tests of causal links between alcohol abuse or dependence and major depression. Archives of General Psychiatry. 2009;66:260–266. doi: 10.1001/archgenpsychiatry.2008.543. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ. Early onset cannabis use and psychosocial adjustment in young adults. Addiction. 1997;92:279–296. [PubMed] [Google Scholar]
- Ginzler JA, Garrett SB, Baer JS, Peterson PL. Measurement of negative consequences of substance use in street youth: An expanded use of the Rutgers Alcohol Problem Index. Addictive Behaviors. 2007;32:1519–1525. doi: 10.1016/j.addbeh.2006.11.004. [DOI] [PubMed] [Google Scholar]
- Hallfors DD, Waller MW, Bauer D, Ford CA, Halpern CT. Which comes first in adolescence—sex and drugs or depression? American Journal of Preventive Medicine. 2005;29:163–170. doi: 10.1016/j.amepre.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Schaeffer C. Treating serious antisocial behavior using multisystemic therapy. In: Weisz JR, Kazdin AE, editors. Evidence-based psychotherapies for children and adolescents. 2nd ed. New York, NY: Guilford Press; 2010. pp. 259–276. [Google Scholar]
- Huang B, White HR, Kosterman R, Catalano R, Hawkins JD. Developmental associations between alcohol and interpersonal aggression during adolescence. Journal of Research in Crime and Delinquency. 2001;38:64–83. [Google Scholar]
- Hussong AM, Curran PJ, Moffitt TE, Caspi A, Carrig MM. Substance abuse hinders desistance in young adults' antisocial behavior. Development and Psychopathology. 2004;16:1029–1046. doi: 10.1017/s095457940404012x. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychology of Addictive Behaviors. 2011;25:390–404. doi: 10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito TA, Miller N, Pollock VE. Alcohol and aggression: A meta-analysis on the moderating effects of inhibitory cues, triggering events, and self-focused attention. Psychological Bulletin. 1996;120:60–82. doi: 10.1037/0033-2909.120.1.60. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2011. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2012. [Google Scholar]
- Kiesner J, Poulin F, Dishion TJ. Adolescent substance use with friends: Moderating and mediating effects of parental monitoring and peer activity contexts. Merrill-Palmer Quarterly. 2010;56:529–556. doi: 10.1353/mpq.2010.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Loeber R, Stouthamer-Loeber M, White HR. Developmental aspects of delinquency and internalizing problems and their association with persistent juvenile substance use between ages 7 and 18. Journal of Clinical Child Psychology. 1999;28:322–332. doi: 10.1207/S15374424jccp280304. [DOI] [PubMed] [Google Scholar]
- Mason WA, Hitch JE, Spoth RL. Longitudinal relations among negative affect, substance use, and peer deviance during the transition from middle to late adolescence. Substance Use & Misuse. 2009;44:1142–1159. doi: 10.1080/10826080802495211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason WA, Kosterman R, Haggerty KP, Hawkins JD, Redmond C, Spoth RL, Shin C. Dimensions of adolescent alcohol involvement as predictors of young-adult major depression. Journal of Studies on Alcohol and Drugs. 2008;69:275–285. doi: 10.15288/jsad.2008.69.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason WA, Windle M. Reciprocal relations between adolescent substance use and delinquency: A longitudinal latent variable analysis. Journal of Abnormal Psychology. 2002;111:63–76. doi: 10.1037//0021-843x.111.1.63. [DOI] [PubMed] [Google Scholar]
- McCarty CA, Wymbs BT, King KM, Mason WA, Vander Stoep A, McCauley E, Baer J. Developmental consistency in associations between depressive symptoms and alcohol use in early adolescence. Journal of Studies on Alcohol and Drugs. 2012;73:444–453. doi: 10.15288/jsad.2012.73.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He J-P, Burstein M, Swanson SA, Avenevoli S, Cui L, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication—Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller ET, Neal DJ, Roberts LJ, Baer JS, Cressler SO, Metrik J, Marlatt GA. Test-retest reliability of alcohol measures: Is there a difference between internet-based assessment and traditional methods? Psychology of Addictive Behaviors. 2002;16:56–63. [PubMed] [Google Scholar]
- Muthén B, Muthén L. Mplus user's guide. sixth ed. Los Angeles, CA: Authors; 2010. [Google Scholar]
- Needham BL. Gender differences in trajectories of depressive symptomatology and substance use during the transition from adolescence to young adulthood. Social Science & Medicine. 2007;65:1166–1179. doi: 10.1016/j.socscimed.2007.04.037. [DOI] [PubMed] [Google Scholar]
- Patton GC, Coffey C, Carlin JB, Degenhardt L, Lynskey M, Hall W. Cannabis use and mental health in young people: Cohort study. BMJ. 2002;325:1195–1198. doi: 10.1136/bmj.325.7374.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction, 101, Supplement. 2006;1:76–88. doi: 10.1111/j.1360-0443.2006.01592.x. [DOI] [PubMed] [Google Scholar]
- Schwab-Stone ME, Shaffer D, Dulcan MK, Jensen PS, Fisher P, Bird HR, Rae DS. Criterion validity of the NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3) Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:878–888. doi: 10.1097/00004583-199607000-00013. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Grekin ER, Gross JJ. Alcohol and affect regulation. Handbook of emotion regulation. New York, NY: Guilford Press; 2007. pp. 560–580. [Google Scholar]
- Shillington AM, Clapp JD. Self-report stability of adolescent substance use: Are there differences for gender, ethnicity and age? Drug and Alcohol Dependence. 2000;60:19–27. doi: 10.1016/s0376-8716(99)00137-4. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Caldwell L, Burke C. Alcohol and the adolescent brain—Human studies. Alcohol Research & Health. 2004;28:205–212. [Google Scholar]
- Trim RS, Meehan BT, King KM, Chassin L. The relation between adolescent substance use and young adult internalizing symptoms: Findings from a high-risk longitudinal sample. Psychology of Addictive Behaviors. 2007;21:97–107. doi: 10.1037/0893-164X.21.1.97. [DOI] [PubMed] [Google Scholar]
- Vander Stoep A, Adrian M, McCauley E, Crowell SE, Stone A, Flynn C. Risk for suicidal ideation and suicide attempts associated with co-occurring depression and conduct problems in early adolescence. Suicide and Life-Threatening Behaviors. 2011;41:316–329. doi: 10.1111/j.1943-278X.2011.00031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vander Stoep A, McCauley E, Thompson KA, Herting JR, Kuo ES, Stewart DG, Kushner S. Universal emotional health screening at the middle school transition. Journal of Emotional and Behavioral Disorders. 2005;13:213–223. doi: 10.1177/10634266050130040301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman GA, McReynolds LS, Ko SJ, Katz LM, Cauffman E, Haxton W, Lucas CP. Screening for emergent risk and service needs among incarcerated youth: Comparing MAYSI-2 and Voice DISC-IV. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:629–639. doi: 10.1097/00004583-200405000-00017. [DOI] [PubMed] [Google Scholar]
- Wasserman GA, McReynolds LS, Lucas CP, Fisher PW, Santos L. The voice DISC-IV with incarcerated male youths: Prevalence of disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:314–321. doi: 10.1097/00004583-200203000-00011. [DOI] [PubMed] [Google Scholar]
- Wells JE, Horwood LJ, Fergusson DM. Drinking patterns in mid-adolescence and psychosocial outcomes in late adolescence and early adulthood. Addiction. 2004;99:1529–1541. doi: 10.1111/j.1360-0443.2004.00918.x. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- White HR, Loeber R, Stouthamer-Loeber M, Farrington DP. Developmental associations between substance use and violence. Development and Psychopathology. 1999;11:785–803. doi: 10.1017/s0954579499002321. [DOI] [PubMed] [Google Scholar]
- Zucker RA, Heitzeg MM, Nigg JT. Parsing the under-control–disinhibition pathway to substance use disorders: A multilevel developmental problem. Child Development Perspectives. 2011;5:248–255. doi: 10.1111/j.1750-8606.2011.00172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]