Abstract
Objective:
We used motor vehicle traffic (MVT) crash fatalities as an example to examine the extent of underreporting of alcohol involvement on death certificates and state variations.
Method:
We compared MVT-related death certificates identified from national mortality data (Multiple Cause of Death [MCoD] data) with deaths in national traffic census data from the Fatality Analysis Reporting System (FARS). Because MCoD data were not individually linked to FARS data, the comparisons were at the aggregate level. Reporting ratio of alcohol involvement on death certificates was thus computed as the prevalence of any mention of alcohol-related conditions among MVT deaths in MCoD, divided by the prevalence of decedents with blood alcohol concentration (BAC) test results (not imputed) of .08% or greater in FARS. Through bivariate analysis and multiple regression, we explored state characteristics correlated with state reporting ratios.
Results:
Both MCoD and FARS identified about 450,000 MVT deaths in 1999–2009. Reporting ratio was only 0.16 for all traffic deaths and 0.18 for driver deaths nationally, reflecting that death certificates captured only a small percentage of MVT deaths involving BAC of .08% or more. Reporting ratio did not improve over time, even though FARS indicated that the prevalence of BAC of at least .08% in MVT deaths increased from 19.9% in 1999 to 24.2% in 2009. State reporting ratios varied widely, from 0.02 (Nevada and New Jersey) to 0.81 (Delaware).
Conclusions:
The comparison of MCoD with FARS revealed a large discrepancy in reporting alcohol involvement in MVT deaths and considerable state variation in the magnitude of underreporting. We suspect similar underreporting and state variations in alcohol involvement in other types of injury deaths.
Death certificates have been the preferred source for mortality statistics because they contain demographic information and (most important) cause-of-death information certified by a physician, coroner, or medical examiner. The cause-of-death information represents the medicolegal opinions on “the chain of events—diseases, injuries, or complications—that directly caused the death” and “other significant conditions contributing to death” (National Center for Health Statistics [NCHS], 2004a, 2004b). In the United States, all the death certificates filed in the states and the District of Columbia are submitted to NCHS, Centers for Disease Control and Prevention (CDC). NCHS processes the cause-of-death information in accordance with the World Health Organization (WHO) regulations and the International Classification of Diseases (10th Revision [ICD-10], since 1999) (Kochanek et al., 2011). NCHS developed multiple computer programs—the Mortality Medical Indexing, Classification, and Retrieval (MICAR) system; SuperMICAR; Automated Classification of Medical Entities (ACME); and Translation of Axes (TRANSAX)—to automatically code the literal entry of cause-of-death information, systematically select the underlying cause of death, and methodically generate the list of multiple causes of death (Kochanek et al., 2011). Manual coding is applied when the automated process is not executable. This process results in the Multiple Cause of Death (MCoD) data, in which each record contains one underlying cause and up to 20 multiple causes.
The quality and details of the information recorded on death certificates determine the accuracy of mortality statistics and the validity of research findings based on mortality data. Since the early 1980s, underreporting of alcohol involvement on death certificates has been documented by a number of studies (Hanzlick, 1988; Kircher et al., 1985; Nashold and Naor, 1981; Nelson et al., 1993; Petersson et al., 1982; Pollock et al., 1987; Romelsjö et al., 1993). In their sampled populations, the ratio of alcohol involvement determined by death certificates to that determined by the designated reference standard (e.g., autopsy, medical panel review, case file review, and blood alcohol testing program reports) ranged from 0:30 to 1:3, varying by study method or by cause and manner of death. The reasons for underreporting included the following: avoiding distressing relatives and/or social stigma, omitting information on elevated blood alcohol concentrations (BACs), having difficulty obtaining accurate information on alcohol involvement within time limits, and lacking sufficient training in death certification (Bell and Cremona, 1989; Carter, 1985; Comstock and Markush, 1986; Maudsley and Williams, 1993; Nashold and Naor, 1981; Pollock et al., 1987). The long history of questioning death certificate accuracy has fostered efforts to improve its quality and completeness. For example, an NCHS-published handbook (2003, p. 12) encourages reporting alcohol use on death certificates when it is believed to be a contributory cause.
The objective of the present study was to reexamine the underreporting of alcohol involvement on death certificates. To our knowledge, none of the previous studies investigated this question at the national level and examined state variations. Considering the plausibility of recent alcohol consumption contributing to deaths and the availability of data on BACs of all decedents in all states, we chose motor vehicle traffic (MVT) crash fatalities as our study objects to explore the extent of the underreporting problem and state variations.
Alcohol consumption’s contribution to MVT crashes has been well known for years (Hingson and Winter, 2003). A person with a BAC of .08% is likely to show impairments in the tasks of driving performance, sustained attention, divided attention, tracking, and contrast sensitivity (Moskowitz and Fiorentino, 2000). An increased BAC increases the risk of a driver being involved in or dying from a fatal crash (Zador et al., 2000). A meta-analysis of five case-control studies suggested a pooled odds ratio of 1.60 (95% confidence interval [CI] [1.17, 2.20]) for fatal motor vehicle injury per .02% increase in BAC (Taylor and Rehm, 2012). Fatally injured drivers with BACs of .10% or more, compared with those with zero BAC, were more likely to be convicted of driving under the influence of alcohol during the 3 years before the fatal crashes, to be perceived as a problem drinker during the last month of life, and to have engaged in heavy episodic drinking and drunk driving at least monthly during the last year of life (Baker et al., 2002). Since 2005, .08% BAC illegal per se laws have been in effect in all states and the District of Columbia (National Highway Traffic Safety Administration [NHTSA], 2011); these laws make it a violation to operate a noncommercial motor vehicle at a BAC of .08% or above. Therefore, alcohol involvement is undoubtedly a medicolegally contributory cause of MVT crash fatalities and should be reported in the cause-of-death section of the death certificate, especially for drunk drivers who were killed in crashes.
The Fatality Analysis Reporting System (FARS), maintained by NHTSA, is a national traffic census in the United States covering all MVT crashes occurring on public roads and causing at least one death within 30 days (NHTSA, 2013). FARS contains information on the BACs of those who died from MVT crashes in all states, enabling us to compare the prevalence of BAC of .08% or more (i.e., legally drunk) in crash deaths with the prevalence of alcohol involvement reported on the death certificates. The comparisons offer insights into whether or to what extent alcohol involvement in MVT crash deaths was underreported on death certificates at the national level. In addition, we examined how the underreporting varied by state and which state characteristics were correlated with the state variation.
Method
Data sources
Death certificate: The Multiple Cause of Death data, 1999–2009.
The MCoD data for 1999–2009 are available to the public through the CDC WONDER (Wide-ranging Online Data for Epidemiologic Research) online databases (NCHS, 2012). The online system is menu driven and allows users to query mortality statistics based on the underlying cause of death as well as on multiple causes of death. The statistics can be stratified by demographics and by geographic area. Deaths included in this study were selected based on whether the underlying cause was categorized as MVT related according to the External Cause of Injury Mortality Matrix (NCHS, 2002). The detailed list of ICD-10 codes for MVT deaths can be found on the NCHS website (NCHS, 2002). The decedent’s role in crashes was determined by the fourth digit of the ICD-10 codes for the underlying cause of death (Kochanek et al., 2011) and categorized into seven groups—vehicle driver, vehicle passenger, unknown vehicle occupant, motorcyclist, pedestrian, pedalcyclist, and other/unspecified. Alcohol involvement was identified by the presence of any of the following codes in the listed multiple causes of death: F10 (mental and behavioral disorders due to use of alcohol), R78.0 (finding of alcohol in blood), T51 (toxic effect of alcohol), X45 (accidental poisoning by and exposure to alcohol), X65 (intentional self-poisoning/suicide by and exposure to alcohol), and Y15 (poisoning by and exposure to alcohol, undetermined intent). This identification covered more than just acute alcohol intoxication, as we strove to broadly capture any types of alcohol involvement as reported on the death certificate.
Blood alcohol concentration of decedents in motor vehicle traffic crashes: The Fatality Analysis Reporting System data, 1999–2009.
The FARS data are collected and coded by state agencies under cooperative agreements with NHTSA. Annual meetings and standardized protocol and coding manuals ensure uniform coding across states. We used actual BAC test results reported to FARS to determine alcohol involvement in the MVT deaths in FARS. Decedents with reported (not imputed) BACs of .08% or more (i.e., the legal limit of intoxication in the United States) were counted as intoxicated deaths. Decedents without alcohol test results were counted as not intoxicated because it is very likely that the certifiers also did not have such information to record intoxication on the death certificates. Additionally, BAC level of .30% or more (i.e., serious intoxication and likely blackout) (International Center for Alcohol Policies, 2011) was examined as a cut point for severe alcohol involvement. We categorized the decedent’s role described in FARS in the same way as for MCoD.
According to previous publications, NHTSA maintains a linked FARS–MCoD database; however, it is accessible only by the agency’s internal users (Briggs et al., 2005; Subramanian, 2007; R. Subramanian, personal communication, May 24, 2012). Therefore, in our study, the MVT deaths identified from the MCoD and FARS data were not individually linked. Rather, the comparisons between these two data sets were based on aggregate measures at the national or state level.
Statistical analysis
Because MVT deaths from the MCoD and FARS data were not individually linked, we compared the prevalence of alcohol involvement estimated from these two data sets at the national and state levels instead. Both data sources covered all MVT deaths in the United States; therefore, they both should identify similar, if not the same, MVT deaths. The degree of reporting of alcohol involvement on death certificates compared with that in FARS, referred to below as “reporting ratio” (RR), was computed as the prevalence of any mention of alcohol-related conditions among MVT deaths in MCoD divided by the prevalence of decedents with reported BACs of .08% or more in FARS. If all intoxicated MVT decedents in FARS were reported as such on their death certificates, the RR should reach 1.00. Because our identification of alcohol involvement on death certificates was based on a broader definition than just intoxication, it is possible that the RR is greater than 1.00.
The RR was estimated as the national average, by sex, race (White, Black, Asian or Pacific Islander, American Indian or Alaska Native, and other/unknown), Hispanic origin, age (0–15, 16–20, 21–34, 35–54, and ≥55 years), year of death, state, and decedent’s role in the crash. Because of confidentiality constraints, the WONDER system suppresses any subnational death counts representing fewer than 10 persons; therefore, the RRs subsequently cannot be calculated for such cases. We plotted 5-year moving averages of state RRs from 1999 to 2009 to examine changes in RRs over time and across states. Five-year moving averages were used to stabilize the pattern and reduce the number of states that had too few cases.
The analysis also explored the extent to which state variation in the average of RRs in 1999–2009 could be explained by state characteristics, including the following: the death investigation system, status of the Uniform Accident and Sickness Policy Provision Law (UPPL), year when .08% BAC illegal per se laws were in effect (before 1999 vs. in 1999 or after), prevalence of driving after drinking too much alcohol at least once during the past month, per capita alcohol consumption among ages 14 years and older (gallons of ethanol per 10,000 capita), BAC testing rate for all MVT deaths or for all vehicle drivers killed in MVT crashes, and population rate of all MVT crash deaths or of drivers killed in MVT crashes. The data sources for each state characteristic are listed in Table 1; detailed descriptions of the data sources can be found on their respective websites. The state death investigation system was dichotomized as a centralized state medical examiner system (16 states) versus any other coroner/medical examiner systems (34 states). The UPPL, if enacted by states, allowed insurers to decline coverage for claims “in consequence of the insured’s being intoxicated or under the influence of any narcotic unless administered on the advice of a physician” (National Association of Insurance Commissioners, 1950, p. 399). In recent years, several states started repealing the UPPL and enacted new legislation that prohibits the denial of coverage (Chezem, 2004). In our analysis, the status of the UPPL was determined by which law was in effect for half or more of the study period and then dichotomized as denial prohibited (5 states) versus permitted or no law (45 states).
Table 1.
State characteristics examined in the analysis
| Characteristic | Data source |
| Death investigation system (as of 2004) | Hickman et al., 2007. Medical Examiners and Coroners Offices, 2004. Bureau of Justice Statistics Special Report NCJ 216756. Washington, DC: U.S. Department of Justice, Office of Justice Programs. (http://bjs.ojp.usdoj.gov/content/pub/pdf/meco04.pdf) |
| Status of Uniform Accident and Sickness Policy Provision Law (effective for half or more of the study period) | Alcohol Policy Information System (www.alcoholpolicy.niaaa.nih.gov) |
| Year when .08% blood alcohol concentration illegal per se laws were in effect (before 1999 vs. 1999 or after) | National Highway Traffic Safety Administration, 2011. Traffic Safety Facts 2009. Report No. DOT HS 811 402. Washington, DC: National Highway Traffic Safety Administration. (www-nrd.nhtsa.dot.gov/Pubs/811402.pdf) |
| Prevalence of driving after drinking too much alcohol at least once during the past month (average of 1999–2009) | Behavioral Risk Factor Surveillance System (www.cdc.gov/brfss) |
| Per capita alcohol consumption among those ages 14 years and older (average of 1999–2009) | LaVallee et al., 2011. Apparent per capita alcohol consumption: National, state, and regional trends, 1977–2009. Surveillance Report #92. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism. (http://pubs.niaaa.nih.gov/publications/surveillance91/Underage09.htm) |
| Blood alcohol concentration testing rates for all people and for vehicle drivers killed in motor vehicle traffic (MVT) crashes (average of 1999–2009) | Fatality Analysis Reporting System |
| Rate of MVT crash deaths and rate of vehicle drivers killed in MVT crashes (average of 1999–2009) | Fatality Analysis Reporting System (Population estimates retrieved from U.S. Census Bureau, Population Division) |
All the analyses were conducted using PC-SAS (Version 9.3; SAS Institute Inc., Cary, NC). Bivariate analysis was used to assess the difference in RRs by each state characteristic. Spearman’s rank correlation coefficient (rs) was used to examine the strength of associations between RRs and continuous measures of the state characteristics. Simple linear regression was conducted to examine unadjusted associations between each state characteristic and RR. Multiple linear regression with forward selection was used to select state characteristics that best explained state variation in RRs. The significance level for entry into the model was set at .50. After the state characteristics were selected, robust multiple linear regression with least trimmed squares estimation was conducted to identify outlier states and control their impact on parameter estimates (Chen, 2002). Because RR has a right-skewed distribution, it was transformed by the natural logarithm before analyses.
Results
The total MVT deaths reported in the MCoD and FARS data for 1999–2009 were 458,071 and 452,318, respectively. This indicated that the inclusion criteria of the MCoD data captured 1.3% more MVT deaths than the FARS (Table 2). In MCoD, 3.3% of MVT deaths were reported as alcohol involved, whereas in FARS, 21.1% of MVT deaths had BACs of .08% or more. This indicated an RR of 0.16 (i.e., overall, alcohol involvement is only 0.16 times as likely to be reported on the death certificate as in FARS). Alcohol involvement in decedents who were American Indian or Alaska Native, non-Hispanic, and ages 0–15 years was more likely to be reported as such on their death certificates than other subpopulations. Although Hispanics had a higher percentage of BACs of .08% or more than non-Hispanics in FARS data, the MCoD data showed a reverse ethnic difference in alcohol involvement. Over time, no improvement in reporting was observed at the national level.
Table 2.
Comparison of motor vehicle traffic (MVT) deaths indicated as alcohol involved between the Multiple Cause of Death (MCoD) data and the Fatality Analysis Reporting System (FARS) data, by selected factors: United States, 1999–2009
| MCoD dataa |
FARS data |
|||||
| Variable | Deaths n | Alcohol-involvedb n (prevalence) | Deaths n | BAC ≥ .08% n (prevalence) | RRc | |
| Total | 458,071 | 15,179 (3.3%) | 452,318 | 95,220 (21.1%) | 0.16 | |
| Sex | ||||||
| Male | 315,069 | 12,655 (4.0%) | 312,915 | 79,768 (25.5%) | 0.16 | |
| Female | 143,002 | 2,524 (1.8%) | 139,217 | 15,440 (11.1%) | 0.16 | |
| Unknown | 94 | 12 (12.8%) | ||||
| Race | ||||||
| White | 381,567 | 12,845 (3.4%) | 326,300 | 71,869 (22.0%) | 0.15 | |
| Black | 57,974 | 1,500 (2.6%) | 49,484 | 9,601 (19.4%) | 0.13 | |
| Asian or Pacific Islander | 10,215 | 177 (1.7%) | 8,899 | 983 (11.0%) | 0.16 | |
| American Indian or Alaska Native | 8,315 | 657 (7.9%) | 7,439 | 2,728 (36.7%) | 0.22 | |
| Other/unknown | 60,196 | 10,039 (16.7%) | ||||
| Hispanic origin | ||||||
| Yes | 58,311 | 1,501 (2.6%) | 50,228 | 13,115 (26.1%) | 0.10 | |
| No | 398,250 | 13,626 (3.4%) | 332,717 | 70,077 (21.1%) | 0.16 | |
| Unknown | 1,510 | 52 (3.4%) | 69,373 | 12,028 (17.3%) | ||
| Age, in years | ||||||
| 0–15 | 25,954 | 59 (0.2%) | 25,826 | 253 (1.0%) | 0.23 | |
| 16–20 | 60,944 | 1,515 (2.5%) | 61,267 | 9,955 (16.2%) | 0.15 | |
| 21–34 | 119,546 | 5,952 (5.0%) | 120,716 | 39,111 (32.4%) | 0.15 | |
| 35–54 | 133,006 | 6,060 (4.6%) | 132,408 | 37,344 (28.2%) | 0.16 | |
| 55 and older | 118,414 | 1,586 (1.3%) | 110,983 | 8,356 (7.5%) | 0.18 | |
| Unknown | 207 | 7 (3.4%) | 1,118 | 201 (18.0%) | ||
| Year of death | ||||||
| 1999 | 40,965 | 1,326 (3.2%) | 41,681 | 8,282 (19.9%) | 0.16 | |
| 2000 | 41,994 | 1,482 (3.5%) | 41,864 | 8,360 (20.0%) | 0.18 | |
| 2001 | 42,443 | 1,471 (3.5%) | 41,775 | 8,427 (20.2%) | 0.17 | |
| 2002 | 44,065 | 1,528 (3.5%) | 42,914 | 8,981 (20.9%) | 0.17 | |
| 2003 | 43,340 | 1,346 (3.1%) | 42,729 | 8,684 (20.3%) | 0.15 | |
| 2004 | 43,432 | 1,254 (2.9%) | 42,747 | 8,336 (19.5%) | 0.15 | |
| 2005 | 43,667 | 1,443 (3.3%) | 43,429 | 8,866 (20.4%) | 0.16 | |
| 2006 | 43,664 | 1,359 (3.1%) | 42,717 | 8,817 (20.6%) | 0.15 | |
| 2007 | 42,031 | 1,406 (3.3%) | 41,212 | 9,280 (22.5%) | 0.15 | |
| 2008 | 37,985 | 1,287 (3.4%) | 37,432 | 9,010 (24.1%) | 0.14 | |
| 2009 | 34,485 | 1,277 (3.7%) | 33,818 | 8,177 (24.2%) | 0.15 | |
| Decedent’s role | ||||||
| Vehicle driver | 113,061 | 5,111 (4.5%) | 243,084 | 61,187 (25.2%) | 0.18 | |
| Vehicle passenger | 48,675 | 741 (1.5%) | 103,216 | 10,122 (9.8%) | 0.16 | |
| Unknown vehicle occupant | 36,526 | 964 (2.6%) | 983 | 291 (29.6%) | ||
| Motorcyclist | 41,782 | 1,504 (3.6%) | 43,868 | 9,702 (22.1%) | 0.16 | |
| Pedestrian | 52,152 | 1,730 (3.3%) | 51,720 | 12,655 (24.5%) | 0.14 | |
| Pedalcyclist | 6,608 | 154 (2.3%) | 7,785 | 1,140 (14.6%) | 0.16 | |
| Other/unspecified | 159,267 | 4,975 (3.1%) | 1,662 | 123 (7.4%) | ||
| State | ||||||
| Alabama | 11,983 | 189 (1.6%) | 11,586 | 1,456 (12.6%) | 0.13 | |
| Alaska | 931 | 25 (2.7%) | 918 | 193 (21.0%) | 0.13 | |
| Arizona | 11,183 | 142 (1.3%) | 11,794 | 2,204 (18.7%) | 0.07 | |
| Arkansas | 7,281 | 113 (1.6%) | 7,011 | 1,408 (20.1%) | 0.08 | |
| California | 42,996 | 912 (2.1%) | 42,789 | 10,225 (23.9%) | 0.09 | |
| Colorado | 7,059 | 663 (9.4%) | 6,809 | 1,752 (25.7%) | 0.37 | |
| Connecticut | 3,395 | 441 (13.0%) | 3,273 | 908 (27.7%) | 0.47 | |
| Delaware | 1,325 | 276 (20.8%) | 1,393 | 360 (25.8%) | 0.81 | |
| Florida | 33,824 | 489 (1.4%) | 34,105 | 7,300 (21.4%) | 0.07 | |
| Georgia | 16,672 | 138 (0.8%) | 17,307 | 2,691 (15.5%) | 0.05 | |
| Hawaii | 1,362 | 115 (8.4%) | 1,412 | 418 (29.6%) | 0.29 | |
| Idaho | 2,803 | 90 (3.2%) | 2,879 | 588 (20.4%) | 0.16 | |
| Illinois | 15,187 | 714 (4.7%) | 14,336 | 4,064 (28.3%) | 0.17 | |
| Indiana | 9,877 | 261 (2.6%) | 9,174 | 1,568 (17.1%) | 0.15 | |
| Iowa | 4,703 | 325 (6.9%) | 4,699 | 628 (13.4%) | 0.52 | |
| Kansas | 5,264 | 520 (9.9%) | 5,006 | 821 (16.4%) | 0.60 | |
| Kentucky | 9,320 | 249 (2.7%) | 9,660 | 1,526 (15.8%) | 0.17 | |
| Louisiana | 10,445 | 522 (5.0%) | 10,273 | 1,802 (17.5%) | 0.28 | |
| Maine | 1,963 | 32 (1.6%) | 2,013 | 406 (20.2%) | 0.08 | |
| Maryland | 7,125 | 49 (0.7%) | 6,813 | 1,643 (24.1%) | 0.03 | |
| Massachusetts | 5,062 | 84 (1.7%) | 4,711 | 907 (19.3%) | 0.09 | |
| Michigan | 13,439 | 398 (3.0%) | 12,967 | 2,536 (19.6%) | 0.15 | |
| Minnesota | 6,474 | 872 (13.5%) | 6,136 | 1,496 (24.4%) | 0.55 | |
| Mississippi | 9,428 | 221 (2.3%) | 9,525 | 1,731 (18.2%) | 0.13 | |
| Missouri | 11,748 | 1,015 (8.6%) | 12,099 | 2,876 (23.8%) | 0.36 | |
| Montana | 2,499 | 363 (14.5%) | 2,688 | 816 (30.4%) | 0.48 | |
| Nebraska | 2,956 | 62 (2.1%) | 2,904 | 610 (21.0%) | 0.10 | |
| Nevada | 3,885 | 15 (0.4%) | 3,929 | 908 (23.1%) | 0.02 | |
| New Hampshire | 1,439 | 12 (0.8%) | 1,500 | 385 (25.7%) | 0.03 | |
| New Jersey | 7,801 | 29 (0.4%) | 7,843 | 1,688 (21.5%) | 0.02 | |
| New Mexico | 4,502 | 64 (1.4%) | 4,875 | 1,344 (27.6%) | 0.05 | |
| New York | 16,408 | 195 (1.2%) | 15,762 | 2,226 (14.1%) | 0.08 | |
| North Carolina | 17,633 | 1,218 (6.9%) | 16,419 | 3,594 (21.9%) | 0.32 | |
| North Dakota | 1,230 | 34 (2.8%) | 1,201 | 407 (33.9%) | 0.08 | |
| Ohio | 14,584 | 929 (6.4%) | 14,136 | 3,449 (24.4%) | 0.26 | |
| Oklahoma | 7,925 | 259 (3.3%) | 8,077 | 1,709 (21.2%) | 0.15 | |
| Oregon | 5,013 | 229 (4.6%) | 4,971 | 1,353 (27.2%) | 0.17 | |
| Pennsylvania | 17,046 | 180 (1.1%) | 16,633 | 3,998 (24.0%) | 0.04 | |
| Rhode Island | 962 | 125 (13.0%) | 904 | 318 (35.2%) | 0.37 | |
| South Carolina | 10,814 | 399 (3.7%) | 11,286 | 2,930 (26.0%) | 0.14 | |
| South Dakota | 1,784 | 160 (9.0%) | 1,849 | 507 (27.4%) | 0.33 | |
| Tennessee | 13,770 | 195 (1.4%) | 13,363 | 2,089 (15.6%) | 0.09 | |
| Texas | 40,990 | 569 (1.4%) | 39,488 | 6,528 (16.5%) | 0.08 | |
| Utah | 3,324 | 45 (1.4%) | 3,348 | 292 (8.7%) | 0.16 | |
| Vermont | 836 | 12 (1.4%) | 876 | 234 (26.7%) | 0.05 | |
| Virginia | 10,190 | 165 (1.6%) | 10,038 | 1,957 (19.5%) | 0.08 | |
| Washington | 7,375 | 355 (4.8%) | 6,608 | 2,011 (30.4%) | 0.16 | |
| West Virginia | 4,098 | 181 (4.4%) | 4,376 | 1,178 (26.9%) | 0.16 | |
| Wisconsin | 8,210 | 444 (5.4%) | 8,211 | 2,636 (32.1%) | 0.17 | |
| Wyoming | 1,425 | 80 (5.6%) | 1,839 | 489 (26.6%) | 0.21 | |
Notes: Data sources: MCoD data—Centers for Disease Control and Prevention (CDC), National Center for Health Statistics. Multiple Cause of Death, 1999–2009 on CDC WONDER online database, released 2012. Retrieved from http://wonder.cdc.gov/mcd-icd10.html. FARS data—National Highway Traffic Safety Administration, Department of Transportation. Fatality Analysis Reporting System, 1999–2009. Retrieved from http://www.nhtsa.gov/FARS. BAC = blood alcohol concentration; RR = reporting ratio; ICD-10 = International Classification of Diseases, 10th Revision; WONDER = Wide-ranging Online Data for Epidemiologic Research.
MVT crash deaths in the MCoD data were identified by injury mechanism—MVT as the underlying cause of death. For the detailed list of ICD-10 codes, see http://www.cdc.gov/nchs/injury/ice/matrix10.htm;
identification was based on multiple cause of death, in which any of the following codes were listed: F10.0–F10.9, R78.0, T51 , X45, X65, and/or Y15;
RR was calculated as the prevalence of alcohol involvement in MVT deaths in the MCoD data divided by the prevalence of decedents with BACs ≥ .08% in the FARS data.
Death certificates are much less specific about the decedent’s role than the FARS. For example, MCoD data identified 113,061 MVT decedents as vehicle drivers, which is less than half of those identified by the FARS data (243,084 deaths) (Table 2). Assuming alcohol involvement in the drivers identified in MCoD was similar to those not identified in MCoD, we estimated the prevalence of alcohol involvement among drivers as 4.5%. Comparing this estimate with the prevalence of BACs of .08% or more in FARS (i.e., 25.2%), we arrived at an estimated 0.18 RR for vehicle drivers, not much higher than the RR for all MVT decedents (i.e., 0.16).
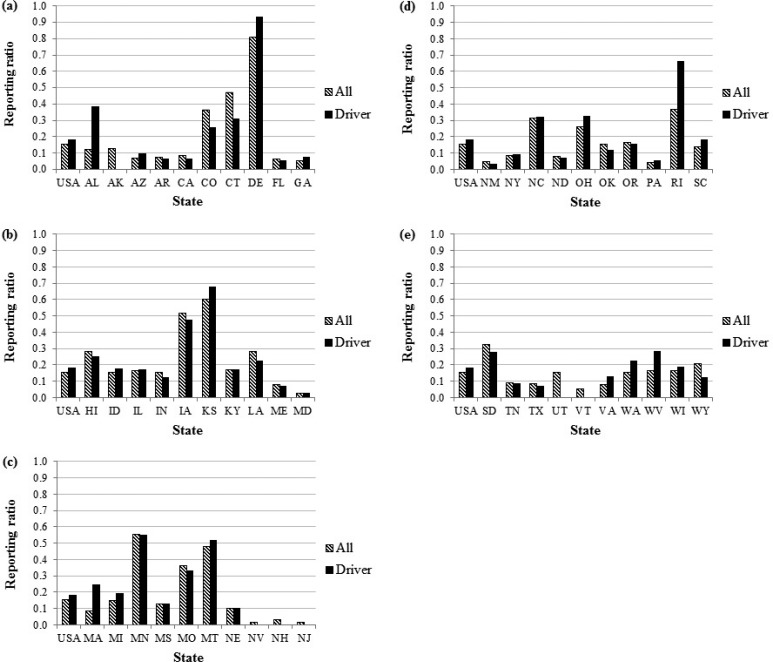
We observed a large state variation in reporting alcohol involvement in MVT deaths. The RR ranged from 0.02 in Nevada and New Jersey to 0.81 in Delaware (Table 2). Similar state variation was observed in the RRs for vehicle drivers (Figure 1). In Alabama, Massachusetts, Rhode Island, Virginia, and West Virginia, the RRs for drivers were more than 50% higher than those for all MVT decedents; conversely, in Connecticut, New Mexico, and Wyoming, the RRs for all MVT decedents were higher. Because six states (Alaska, Nevada, New Hampshire, New Jersey, Utah, and Vermont) had too few alcohol-involved driver deaths (i.e., <10, by CDC WONDER’s data suppression rule) to be reported from the MCoD data, their RRs for drivers cannot be determined.
Figure 1.
Reporting ratio in 1999–2009 by state among all motor vehicle traffic crash deaths and among all identified drivers killed in crashes. Six states (AK, NV, NH, NJ, UT, and VT) did not have reporting ratios for identified drivers because their numbers of alcohol-involved drivers were too few (<10 deaths) to be reported in the Multiple Cause of Death data.
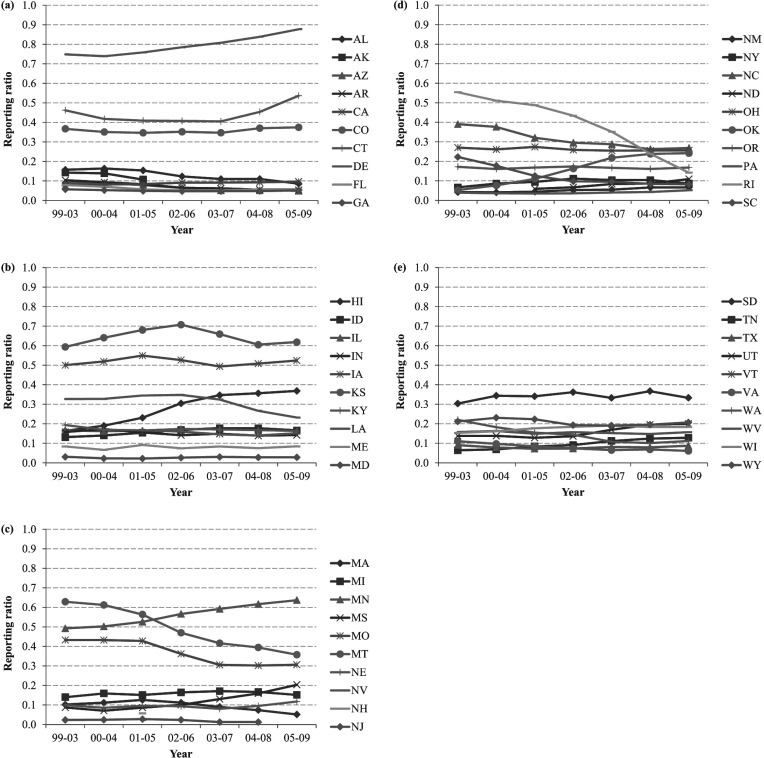
The 5-year moving averages showed that most states had consistent RRs for all MVT deaths over time, whereas others showed patterns of increasing (e.g., Delaware, Hawaii, Minnesota, and Oklahoma) or decreasing (e.g., Louisiana, Missouri, Montana, Rhode Island, and South Carolina) (Figure 2). Alaska, Nevada, New Hampshire, and Vermont were missing on four, six, six, and all seven data points, respectively, because their numbers of MVT deaths with alcohol involvement in MCoD were too small to be reported. Therefore, their trends cannot be determined.
Figure 2.
Five-year moving average of reporting ratios by state, 1999–2009. Six states’ numbers of motor vehicle traffic crash deaths with alcohol involvement in the Multiple Cause of Death data were too small to be reported, so these states did not have all valid data points: AK (missing 4 data points), NV (missing 6 data points), NH (missing 6 data points), NJ (missing 1 data point), ND (missing 1 data point), and VT (missing all 7 data points).
No statistically significant difference in RR was observed by the death investigation system, status of UPPL, and the year that illegal per se laws went into effect (Table 3). This could be attributable to the large intra-group variations. On one hand, among states that had a centralized state medical examiner system, Maryland and New Hampshire had the lowest RR at 0.03, whereas Delaware had the highest at 0.81, followed by Connecticut at 0.47. On the other hand, Kansas (county coroner system) achieved an RR of 0.60 without a centralized state medical examiner system, followed by Minnesota (mixed county medical examiner and coroner system) at 0.55, and then Iowa (county medical examiner system) at 0.52. States that prohibited insurers from declining coverage because of alcohol involvement showed higher (but not statistically significant) RRs than those without the law or those that permitted the exclusion. States where .08% BAC illegal per se laws were in effect before 1999 did not have higher RRs than states where the laws were in effect in 1999 or later.
Table 3.
Median and range of state reporting ratios by death investigation system, status of Uniform Accident and Sickness Policy Provision Law, and year when .08% blood alcohol concentration illegal per se laws were in effect
| Variable | No. of states | Median | Lowest (state) | Highest (state) | pa |
| Death investigation system | .64 | ||||
| Centralized state medical examiner system | 16 | 0.14 | 0.03 (MD, NH) | 0.81 (DE) | |
| Any other systems | 34 | 0.15 | 0.02 (NV, NJ) | 0.60 (KS) | |
| Uniform Policy Provision Law | .29 | ||||
| Prohibited | 5 | 0.32 | 0.03 (MD) | 0.52 (IA) | |
| Permitted or no law | 45 | 0.14 | 0.02 (NV, NJ) | 0.81 (DE) | |
| Year illegal per se laws in effect | .47 | ||||
| Before 1999 | 15 | 0.13 | 0.03 (NH) | 0.60 (KS) | |
| 1999 or after | 35 | 0.15 | 0.02 (NV, NJ) | 0.81 (DE) |
Notes: No. = number.
p value of the Wilcoxon rank-sum test of equality of medians between two subgroups.
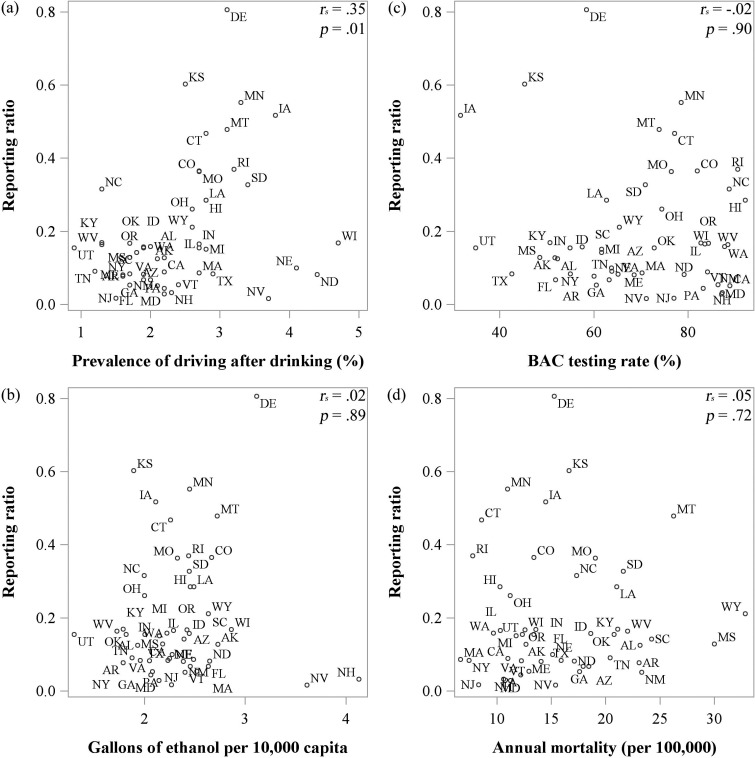
Figure 3a shows a significant positive correlation between RR and the prevalence of driving after drinking too much at least once in the past month (rs = .35, p = .01). Per capita alcohol consumption among individuals ages 14 years and older, BAC testing rate, and rate of MVT crash deaths were not correlated with state RR (Figures 3b–3d).
Figure 3.
Scatter plots of reporting ratio by (a) prevalence of driving after drinking too much alcohol at least once during the past month, (b) per capita alcohol consumption among individuals ages 14 years and older, (c) blood alcohol concentration (BAC) testing rate, and (d) rate of motor vehicle traffic crash deaths. Spearman’s rank correlation coefficients (rs) and p values are shown in the top-right corner of each chart.
In simple linear regression models, only the prevalence of driving after drinking showed a marginally significant association in the models for all MVT deaths and for vehicle driver deaths specifically (Table 4). A forward-selection procedure for multiple linear regression determined that certain state characteristics—death investigation system (p = .30), prevalence of driving after drinking too much (p < .01), per capita alcohol consumption (p = .02), and rate of MVT deaths (p = .18)—explained 20% of the variability in state RRs for all MVT deaths. Another group of state characteristics—death investigation system (p = .32), prevalence of driving after drinking (p = .03), and BAC testing rates among drivers killed in crashes (p = .32)—explained 12% of the variability in state RRs for vehicle drivers specifically. Robust multiple linear regression identified Nevada as the outlier state in the model for all MVT deaths and identified Maryland, North Dakota, and New Mexico as outlier states in the model for driver deaths. The observed values of RR in these states were much lower than the expected values, given the values of their state characteristics. After we controlled for the impact of outliers, parameter estimates in the model for all MVT deaths did not change much, but per capita alcohol consumption became nonsignificant. As for drivers, the associations of death investigation and the prevalence of driving after drinking with RRs became stronger, and the parameter estimate of death investigation became significant. Overall, the prevalence of driving after drinking was the only state characteristic that was robustly positively associated with state RRs for all MVT crash deaths as well as for driver deaths.
Table 4.
Parameter estimates (b) for state characteristics from simple linear regression, forward-selection multiple linear regression, and robust multiple linear regression models, in which the dependent variable is the natural log of the reporting ratio in 1999–2009
| Variable | Simple |
Multipleb |
Robust multiple |
|||||||||
| Exp(b) | [95% CI] | p | Exp(b) | [95% CI] | p | Exp(b) | [95% CI] | p | ||||
| All MVT deaths (50 states) | ||||||||||||
| Centralized state medical examiner system | 0.91 | [0.53, 1.56] | .74 | 1.34 | [0.77, 2.32] | .30 | 1.24 | [0.73, 2.09] | .43 | |||
| UPPL – Prohibited | 1.43 | [0.63, 3.27] | .40 | |||||||||
| .08% BAC illegal per se laws in effect before 1999 | 0.84 | [0.49, 1.44] | .52 | |||||||||
| Prevalence of driving after drinking (%) | 1.31 | [0.98, 1.76] | .08 | 1.72 | [1.22, 2.42] | <.01 | 1.71 | [1.24, 2.38] | <.01 | |||
| Gallons of ethanol (per 10,000 capita) | 0.74 | [0.43, 1.27] | .28 | 0.47 | [0.26, 0.84] | .02 | 0.61 | [0.34, 1.12] | .11 | |||
| BAC testing rate among all decedents (%) | 0.99 | [0.98, 1.01] | .42 | |||||||||
| Rate of MVT deaths (per 100,000) | 1.02 | [0.97, 1.06] | .43 | 1.03 | [0.99, 1.07] | .18 | 1.03 | [0.99, 1.07] | .16 | |||
| R2 | .2042 | .3089 | ||||||||||
| Outlier state | NV | |||||||||||
| Vehicle drivers killed in crashes (44 states)a | ||||||||||||
| Centralized state medical examiner system | 1.07 | [0.61, 1.87] | .81 | 1.35 | [0.75, 2.43] | .32 | 1.78 | [1.06, 2.99] | .03 | |||
| UPPL – Prohibited | 1.20 | [0.55, 2.64] | .65 | |||||||||
| .08% BAC illegal per se laws in effect before 1999 | 0.84 | [0.48, 1.46] | .53 | |||||||||
| Prevalence of driving after drinking (%) | 1.34 | [1.00, 1.80] | .05 | 1.42 | [1.04, 1.93] | .03 | 1.56 | [1.18, 2.05] | <.01 | |||
| Gallons of ethanol (per 10,000 capita) | 1.60 | [0.71, 3.60] | .26 | |||||||||
| BAC testing rate among drivers killed in crashes (%) | 1.00 | [0.97, 1.02] | .64 | 0.99 | [0.97, 1.01] | .32 | 1.00 | [0.98, 1.01] | .62 | |||
| Rate of drivers killed in MVT crashes (per 100,000) | 0.99 | [0.93, 1.06] | .85 | |||||||||
| R2 | .1188 | .2789 | ||||||||||
| Outlier state | MD, ND, NM | |||||||||||
Notes: BAC = blood alcohol concentration; CI = confidence interval; MVT = motor vehicle traffic; UPPL = Uniform Accident and Sickness Policy Provision Law.
Six states (AK, NV, NH, NJ, UT, and VT) did not have reporting ratios for identified drivers because their numbers of alcohol-involved drivers were too small to be reported in the Multiple Cause of Death data;
the significance level for entry into the model was set at .50.
When using BAC of .30% or more to define severe alcohol involvement in the FARS data, the prevalence of alcohol involvement reported in the MCoD data at the national level became higher than the prevalence of BAC of .30% or more in the FARS data. This implied that most of the severely intoxicated cases were reported on death certificates. However, this was not always the case at the state level. For 14 states (Arizona, Arkansas, California, Florida, Georgia, Maryland, Nevada, New Hampshire, New Jersey, New Mexico, North Dakota, Pennsylvania, Texas, and Virginia), the prevalence of alcohol involvement in MCoD was still lower than the prevalence of BAC of .30% or more in FARS. Their RRs (based on BAC ≥ .30%) ranged from 0.14 in Nevada and New Jersey to 0.90 in Arkansas (data not shown).
Discussion
Our findings show that the underreporting of alcohol involvement on death certificates remained substantial during the past 11 years. Based on the comparison of MCoD and FARS data, alcohol involvement is 84% less likely to be reported on death certificates than in FARS. The reporting practice did not improve over time, whereas the prevalence of reported BAC of .08% or more in MVT deaths increased slightly from 19.9% in 1999 to 24.2% in 2009. Even when focusing on vehicle drivers, whose alcohol involvement contributed more directly to MVT crashes, the RR was still low at 0.18.
The magnitude of underreporting estimated in our study at the aggregate level is similar to that reported at the individual level. Nashold and Naor (1981) observed that, in Wisconsin in 1975–1977, alcohol involvement was reported on an average of 10% of the death certificates of drivers, motorcyclists, and pedestrians whose BACs were .05% or more. The difference is that they found the highest reporting for decedents ages 45–64 years, whereas our results showed the highest for those ages 0–15 years. Pollock et al. (1987) requested a medical panel to review 426 veteran postservice deaths in the 1970s and 1980s. The panel determined that 40.2% of deaths caused by motor vehicle injury were alcohol related, whereas only 5.4% of the death certificates had any alcohol-related ICD-9 codes, yielding an RR of 0.13. In a more recent study, Daula and Hanzlick (2006) compared investigative case files and death certificates issued by the Fulton County, GA, Medical Examiner in 2004. They found that for 137 traffic accident deaths, only 1 death certificate indicated alcohol involvement, whereas 6 case files mentioned BAC of .10% or more, which is equivalent to an RR of 0.17.
Our study is the first, to our knowledge, to show a wide range of state variation in death certification regarding alcohol involvement in MVT crashes. RR ranged from 0.02 (Nevada and New Jersey) to 0.81 (Delaware). This could have resulted from the state differences in death investigation systems, the prevalence of drunk-driving behavior, BAC testing rates, timing of receiving toxicology test results, office general practice, or a combination of all the factors. In the United States, MVT crash deaths are investigated and certified by medical examiners or coroners in a given jurisdiction. Although a medical examiner system was recommended over a coroner system (Committee on Identifying the Needs of the Forensic Science Community et al., 2009), and a centralized system provides uniform guidelines statewide, our study showed that a centralized statewide medical examiner system did not ensure higher reporting of alcohol involvement than other systems. Romano and McLoughlin (1992) also pointed out that in California, the county variation in reporting was not related to autopsy rates or a medical examiner system but rather coroners’ or medical examiners’ preference.
In our study, state prevalence of self-reported drunk-driving behavior shows a robust positive association with state RR. In other words, alcohol involvement in traffic crashes was more likely to be reported on death certificates in states with a higher prevalence of self-reported drunk driving. Self-reported drunk-driving behavior was highly associated with heavy episodic drinking and driving without always using a seatbelt (CDC, 2011). Romelsjö et al. (1993) also found that decedents’ previous drunk-driving experience was associated with a high BAC at death (by any cause) and with any mention of alcoholism, alcohol psychosis, alcohol intoxication, liver cirrhosis, or cardiac enlargement or suspected cardiomyopathy on the death certificate. Drunk-driving behavior seems to be a proxy for acute as well as chronic drinking problems. The positive correlation between state prevalence of drunk-driving behavior and state RR of alcohol involvement may indicate that death certifiers tended to record alcohol involvement when the decedent had other alcohol-related problems rather than just one-time intoxication at the time of the crash.
As of 2009, 25 states implemented policies requiring BAC testing for drivers killed in vehicle crashes (Casanova et al., 2012). On average, states with mandatory testing laws had BAC testing rates 15 percentage points higher than the states without a law, although some states without a law did achieve high BAC testing rates (Casanova et al., 2012). Mandatory testing laws for fatally injured drivers may enhance the coroners’ or medical examiners’ awareness of alcohol involvement by increasing BAC testing rates and, consequently, enhance the accuracy of death certification. However, our results showed that BAC testing rates were not correlated with reporting alcohol involvement on death certificates (Figure 3c and Table 4). This may have been because of the long turnaround time of toxicology tests in some offices (Daula and Hanzlick, 2006). Coroners or medical examiners generally are required to complete and file a death certificate within 3–5 days after a death occurs (Warner and Chen, 2012, p. 4). If a toxicology test takes longer, the BAC result, even when known, will not be documented unless the medical examiner or coroner files a supplemental report or amends the death certificate. Another reason for underreporting suggested by Daula and Hanzlick (2006) is that sometimes the medical examiners are unsure whether high BAC contributed to MVT crash deaths. They may choose not to report alcohol intoxication on death certificates even when the BAC exceeds the legal intoxication level. This may have been the practice in certain areas only given our findings of a large variation in reporting across states. The .08% illegal per se law could be a legal ground for documenting high BAC; but in our study, states with the law in effect for a long time did not consistently show higher RRs than states with the law in effect for a short time (Tables 3 and 4).
The BAC of injured persons is critical for determining the scope of alcohol-related problems and developing dose–response relationships between alcohol consumption and injuries. In the 1980s, researchers at the National Institute on Alcohol Abuse and Alcoholism realized that the ninth revision of the ICD lacked specific codes for alcohol involvement in casualties. They collaborated with other federal agencies, experts, and consultants to propose two supplementary codes to quantitatively or qualitatively record alcohol consumption leading or contributing to a disease condition or death (Grant et al., 1987). These two codes were later included in the ICD-10 as optional codes—Y90, evidence of alcohol involvement determined by BAC; and Y91, evidence of alcohol involvement determined by level of intoxication (WHO, 1992). By using Y90, the known BACs of decedents can be reported as one of the following categories: <.02% (Y90.0), .02%–<.04% (Y90.1), .04%–<.06% (Y90.2), .06%–<.08% (Y90.3), .08%–<.10% (Y90.4), .10%–<.12% (Y90.5), .12%–<.20% (Y90.6), .20%–<.24% (Y90.7), ≥.24% (Y90.8), or unspecified level (Y90.9). Code Y91 can be used to record the clinical observation of intoxication severity. This information, if collected, could enhance the use of death data to monitor alcohol-involved injuries. Unfortunately, these two codes were not adopted in the United States for death certificate coding. FARS thus becomes the sole source for tracking BACs of MVT deaths, and no other national injury surveillance systems collect detailed BAC information.
The major limitation of our study was that the analysis could be conducted only at aggregate levels. This was because, due to the confidentiality issue, the linked decedent records of the FARS and MCoD are not available to the public. We could not determine how discrepancies occurred at the individual level. It is possible that the decedents had alcohol-related ICD-10 codes on death certificates but were not reported as having BACs of .08% or more in FARS data and vice versa. Nonetheless, our results provide a general assessment of underreporting at the national and state levels, and they indicate wide state variation in death certification, which cannot be easily accomplished by reviewing records at the individual level.
Another study limitation is that in MCoD data, many decedents’ roles in the crashes are missing or cannot be determined, even though this information must be reported (NCHS, 2003, p. 19). It can be argued that alcohol intoxication of passengers is less likely to contribute to MVT deaths than that of drivers, motorcyclists, or pedestrians. Including passengers in the analysis may overestimate the magnitude of underreporting. However, in our study, the reporting practice did not differ much by role of decedents, given the RR at 0.18 for vehicle drivers versus 0.16 for all MVT crash decedents. The argument about the causal contribution of alcohol involvement may not be the sole reason for underreporting.
The comparison in this study is based on known BAC values in FARS because the certifiers can only report known conditions on the death certificates. At the national average, more than a quarter of fatally injured drivers were not tested for alcohol (Casanova et al., 2012). If the unknown BAC values were imputed by the method developed by NHTSA (Subramanian, 2002), the percentage of drivers killed in MVT crashes in 2011 who had BACs of .08% or more could increase from 25.2% (95% CI [24.6%, 25.8%]) to 31.4% (95% CI [30.7%, 32.0%]) (Chen, 2013). Therefore, the magnitude of underestimation of alcohol involvement based on death certificates could be even larger than our underreporting estimates. In addition, if blood samples were collected long after the injury occurred, the testing results could underestimate the true BACs, leading to another source of underestimation.
The comparison of MCoD with FARS data shows a great degree of state variation in reporting alcohol involvement on death certificates. We suspect similar state variations in other types of injury deaths. Caution is merited when comparing state alcohol-related mortalities using MCoD data. The Alcohol-Related Disease Impact (ARDI) software, developed by the CDC and supported by the Robert Wood Johnson Foundation (Princeton, NJ), may be used as an alternative source for state comparisons in alcohol-attributable deaths. ARDI provides state average estimates of alcohol-attributable deaths for 2001–2005 using cause- and gender-specific alcohol-attributable fractions derived from observational studies or systematic reviews. However, ARDI’s estimates did not take into account the racial or age differences in alcohol involvement in deaths or state differences in population composition. This could lead to over- or underestimating alcohol-related deaths. For example, Native Americans and Hispanics have higher proportions of alcohol-related MVT fatalities than non-Hispanic Whites (Keyes et al., 2012; NHTSA, 2009). Applying the averaged alcohol-attributable fractions of MVT crashes to Alaska, where American Indians and Alaska Natives account for 14.8% of the state population (U.S. Census Bureau, n.d.), and to California, where Hispanics or Latinos account for 37.6% of the state population (U.S. Census Bureau, n.d.), could result in underestimates of alcohol-attributable MVT deaths in these two states.
Despite the growing recognition of alcohol use as an important risk factor for public health, the reporting of alcohol involvement on death certificates does not seem to have improved much over the years. Medical examiners, coroners, and physicians serving as death certifiers are the key to accurate and complete cause-of-death information. Federal and state government agencies should continue to encourage or perhaps start to require death certifiers to report alcohol involvement when it contributes to death. One way to raise general awareness would be to emphasize the importance of reporting alcohol involvement during death certification training. By communicating with the local offices that had low RRs, we may better understand the hurdles. MCoD is a very important data source for injury surveillance and public health research. New approaches are needed to increase data accuracy and completeness because these approaches have not improved in past decades.
Acknowledgments
The authors thank Chiung M. Chen (CSR, Incorporated) for providing data on state prevalence of driving after drinking too much alcohol and percentages of MVT deaths that had imputed BACs of .08% or more.
Footnotes
This article is based on a study conducted for the Alcohol Epidemiologic Data System project funded by the National Institute on Alcohol Abuse and Alcoholism through Contract No. HHSN267200800023C to CSR, Incorporated. The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of the sponsoring agency or the federal government.
References
- Baker SP, Braver ER, Chen LH, Li G, Williams AF. Drinking histories of fatally injured drivers. Injury Prevention. 2002;8:221–226. doi: 10.1136/ip.8.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell G, Cremona A. Alcohol and death certification: Influencing current practice and attitudes. British Journal of Addiction. 1989;84:1523–1525. doi: 10.1111/j.1360-0443.1989.tb03935.x. [DOI] [PubMed] [Google Scholar]
- Briggs NC, Levine RS, Haliburton WP, Schlundt DG, Goldzweig I, Warren RC. The Fatality Analysis Reporting System as a tool for investigating racial and ethnic determinants of motor vehicle crash fatalities. Accident Analysis and Prevention. 2005;37:641–649. doi: 10.1016/j.aap.2005.03.006. [DOI] [PubMed] [Google Scholar]
- Carter JR. The problematic death certificate. [Editorial] New England Journal of Medicine. 1985;313:1285–1286. doi: 10.1056/NEJM198511143132009. [DOI] [PubMed] [Google Scholar]
- Casanova T, Hedlund J, Tison J. Washington, DC: National Highway Traffic Safety Administration; 2012. State blood alcohol concentration (BAC) testing and reporting for drivers involved in fatal crashes: Current practices, results, and strategies, 1997–2009. (Report No. DOT HS 811 661) Retrieved from www.nhtsa.gov/staticfiles/nti/pdf/811661.pdf. [Google Scholar]
- Centers for Disease Control and Prevention. Vital signs: Alcohol-impaired driving among adults—United States, 2010. Morbidity and Mortality Weekly Report. 2011;60:1351–1356. [PubMed] [Google Scholar]
- Chen C. Robust regression and outlier detection with the ROBUSTREG procedure. SAS Users Group International Conference. Paper. 2002;265-27:1–12. Retrieved from http://www2.sas.com/proceedings/sugi27/p265-27.pdf. [Google Scholar]
- Chen CM. 2013 Unpublished report. [Google Scholar]
- Chezem L. Legal barriers to alcohol screening in emergency departments and trauma centers. Alcohol Research and Health. 2004;28:73–79. [PMC free article] [PubMed] [Google Scholar]
- Committee on Identifying the Needs of the Forensic Sciences Community; Committee on Science. Strengthening forensic science in the United States: A path forward. Washington, DC: National Academies Press; 2009. Technology, and Law Policy and Global Affairs; Committee on Applied and Theoretical Statistics Division on Engineering and Physical Sciences; & National Research Council of the National Academies; pp. 241–268. Medical examiner and coroner systems: Current and future needs. Retrieved from https://www.ncjrs.gov/pdffiles1/nij/grants/228091.pdf. [Google Scholar]
- Comstock GW, Markush RE. Further comments on problems in death certification. American Journal of Epidemiology. 1986;124:180–181. doi: 10.1093/oxfordjournals.aje.a114376. [DOI] [PubMed] [Google Scholar]
- Daula M, Hanzlick R. American Journal of Forensic Medicine and Pathology. Vol. 27. Atlanta: Georgia, 2004; 2006. Evaluation of certifier practices regarding alcohol-related deaths Fulton County Medical Examiner’s Center; pp. 355–358. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dufour M, Stinson F, Towle LH, Bertolucci D. Proposed coding of alcohol’s role in casualties. Alcohol Health and Research World. 1987;12:48–50. [Google Scholar]
- Hanzlick R. Death certificates, natural death, and alcohol. The problem of underreporting. American Journal of Forensic Medicine and Pathology. 1988;9:149–150. doi: 10.1097/00000433-198806000-00011. [DOI] [PubMed] [Google Scholar]
- Hickman MJ, Hughes KA, Strom KJ, Ropero-Miller JD. Bureau of Justice Statistics Special Report NCJ 216756: Medical Examiners and Coroners’ Offices, 2004. Washington, DC: U.S. Department of Justice; 2007. Office of Justice Programs. Retrieved from http://bjs.ojp.usdoj.gov/content/pub/pdf/meco04.pdf. [Google Scholar]
- Hingson R, Winter M. Epidemiology and consequences of drinking and driving. Alcohol Research and Health. 2003;27:63–78. [PMC free article] [PubMed] [Google Scholar]
- International Center for Alcohol Policies. ICAP Blue Book: Practical guides for alcohol policy and prevention approaches. Washington, DC: Author; 2011. Annex 1. The basics about alcohol. Retrieved from http://www.icap.org/PolicyTools/ICAPBlueBook/Annex1TheBasicsaboutAlcohol/tabid/116/Default.aspx. [Google Scholar]
- Keyes KM, Liu XC, Cerda M. The role of race/ethnicity in alcohol-attributable injury in the United States. Epidemiology Review. 2012;34:89–102. doi: 10.1093/epirev/mxr018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kircher T, Nelson J, Burdo H. The autopsy as a measure of accuracy of the death certificate. New England Journal of Medicine. 1985;313:1263–1269. doi: 10.1056/NEJM198511143132005. [DOI] [PubMed] [Google Scholar]
- Kochanek KD, Xu J, Murphy SL, Miniño AM, Kung H-C. National Vital Statistics Reports, 60. 2011. http://www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_03.pdf. Deaths: Final data for 2009. Retrieved from. [PubMed]
- LaVallee RA, Yi H. Surveillance Report #92: Apparent per capita alcohol consumption: National, state, and regional trends, 1977–2009. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2011. Retrieved from http://pubs.niaaa.nih.gov/publications/Surveillance92/CONS09.pdf. [Google Scholar]
- Maudsley G, Williams EM. Death certification by house officers and general practitioners—Practice and performance. Journal of Public Health Medicine. 1993;15:192–201. [PubMed] [Google Scholar]
- Moskowitz H, Fiorentino D. A review of the literature on the effects of low doses of alcohol on driving related skills. 2000 (Pub. No. DOT HS-809–028). Springfield, VA: U.S. Department of Transportation, National Highway Traffic Safety Administration. [Google Scholar]
- Nashold RD, Naor EM. Alcohol-related deaths in Wisconsin: The impact of alcohol on mortality. American Journal of Public Health. 1981;71:1237–1241. doi: 10.2105/ajph.71.11.1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association of Insurance Commissioners. 161. 1950-2. Kansas City, MO: National Association of Insurance Commissioners; 1950. Proceedings of the National Association of Insurance Commissioners, 81st Annual Session, June 13, 1950; Québec, Canada. (1950 NAIC Proc. 398) p. 950. [Google Scholar]
- National Center for Health Statistics. ICD framework: External cause of injury mortality matrix. 2002. Retrieved from http://www.cdc.gov/nchs/injury/ice/matrix10.htm.
- National Center for Health Statistics. Medical examiners’ and coroners’ handbook on death registration and fetal death reporting. 2003. Retrieved from http://www.cdc.gov/nchs/data/misc/hb_me.pdf.
- National Center for Health Statistics. Instructions for completing the cause-of-death section of the death certificate. 2004a. Retrieved from http://www.cdc.gov/nchs/data/dvs/blue_form.pdf.
- National Center for Health Statistics. Instructions for completing the cause-of-death section of the death certificate for injury and poisoning. 2004b. Retrieved from http://www.cdc.gov/nchs/data/dvs/red_form.pdf.
- National Center for Health Statistics. About multiple cause of death 1999–2010. CDC WONDER online database. 2012. Retrieved from http://wonder.cdc.gov/mcd-icd10.html.
- National Highway Traffic Safety Administration. (Report No. DOT HS 810 995) Washington, DC: Author; 2009. Traffic safety facts 2006 data: Race and ethnicity. Retrieved from http://www-nrd.nhtsa.dot.gov/Pubs/810995.pdf. [Google Scholar]
- National Highway Traffic Safety Administration. (Report No. DOT HS 811 402) Washington, DC: Author; 2011. Traffic safety facts 2009: A compilation of motor vehicle crash data from the Fatality Analysis Reporting System and the General Estimates System. Retrieved from http://www-nrd.nhtsa.dot.gov/Pubs/811402.pdf. [Google Scholar]
- National Highway Traffic Safety Administration. Fatality Analysis Reporting System (FARS): Analytical users manual 1975–2010. (Report No. DOT HS 811 529) 2013. Retrieved from http://www-nrd.nhtsa.dot.gov/Pubs/811529.pdf.
- Nelson DE, Sacks JJ, Parrish RG, Sosin DM, McFeeley P, Smith SM. Sensitivity of multiple-cause mortality data for surveillance of deaths associated with head or neck injuries. MMWR CDC Surveillance Summaries. 1993;42(5):29–35. [PubMed] [Google Scholar]
- Petersson B, Krantz P, Kristensson H, Trell E, Sternby NH. Alcohol-related death: A major contributor to mortality in urban middle-aged men. The Lancet. 1982;320:1088–1090. doi: 10.1016/s0140-6736(82)90015-0. [DOI] [PubMed] [Google Scholar]
- Pollock DA, Boyle CA, DeStefano F, Moyer LA, Kirk ML. Underreporting of alcohol-related mortality on death certificates of young US Army veterans. Journal of the American Medical Association. 1987;258:345–348. [PubMed] [Google Scholar]
- Romano PS, McLoughlin E. Unspecified injuries on death certificates: A source of bias in injury research. American Journal of Epidemiology. 1992;136:863–872. doi: 10.1093/aje/136.7.863. [DOI] [PubMed] [Google Scholar]
- Romelsjö A, Karlsson G, Henningsohn L, Jakobsson SW. The prevalence of alcohol-related mortality in both sexes: Variation between indicators, Stockholm, 1987. American Journal of Public Health. 1993;83:838–844. doi: 10.2105/ajph.83.6.838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian R. Washington, DC: National Highway Traffic Safety Administration; 2002. Transitioning to multiple imputation—A new method to impute missing blood alcohol concentration (BAC) values in FARS. (Report No. DOT HS 809 403) Retrieved from http://www-nrd.nhtsa.dot.gov/Pubs/809-403.PDF. [Google Scholar]
- Subramanian R. Washington, DC: National Center for Statistics and Analysis; 2007. Traffic safety facts: Bodily injury locations in fatally injured motorcycle riders (DOT HS 810 856) National Highway Traffic Safety Administration. Retrieved from http://www-nrd.nhtsa.dot.gov/Pubs/810856.pdf. [Google Scholar]
- Taylor B, Rehm J. The relationship between alcohol consumption and fatal motor vehicle injury: High risk at low alcohol levels. Alcoholism: Clinical and Experimental Research. 2012;36:1827–1834. doi: 10.1111/j.1530-0277.2012.01785.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau (nd.) 2010 Census Interactive Population Search. Retrieved from http://www.census.gov/2010census/
- Warner M, Chen L-H. Surveillance of injury mortality. In: Li G, Baker SP, editors. Injury research: Theories, methods, and approaches. New York, NY: Springer; 2012. pp. 3–21. [Google Scholar]
- World Health Organization. Geneva, Switzerland: Author; 1992. International Statistical Classification of Diseases and Related Health Problems (10th ed., revisedVol. 1) [Google Scholar]
- Zador PL, Krawchuk SA, Voas RB. Alcohol-related relative risk of driver fatalities and driver involvement in fatal crashes in relation to driver age and gender: An update using 1996 data. Journal of Studies on Alcohol. 2000;61:387–395. doi: 10.15288/jsa.2000.61.387. [DOI] [PubMed] [Google Scholar]