Abstract
Objective:
The purpose of this study was to examine the relations between drinking (mean quantity and heavy drinking patterns) and alcohol use disorders (AUDs) in the U.S. general population.
Method:
Data from three telephone National Alcohol Surveys (in 2000, 2005, and 2010) were pooled, with separate analyses for men and women restricted to current drinkers (ns = 5,922 men, 6,270 women). Predictors were 12-month volume (mean drinks per day), rates of heavy drinking (5+/4+ drinks in a day for men/women), and very heavy drinking (8+, 12+, and 24+ drinks in a day). Outcomes were negative alcohol-related consequences constituting abuse (1+ of 4 DSM-IV–based domains assessed by 13 items) and alcohol dependence (symptoms in 3+ of 7 DSM-IV–based domains), together taken to indicate an AUD. Segmentation analyses were used to model risks of problem outcomes from drinking patterns separately by gender.
Results:
In the general population, men and women who consumed ≤1 drink/day on average with no heavy drinking days did not incur substantial risks of an AUD (<10%). Men who drank from 1 to 2 drinks/day on average but never 5+ incurred a 16% risk of reporting an AUD (3.5% alcohol dependence). At higher volumes, men and women who indicated higher rates of drinking larger amounts per day and/or involving 8+ and 12+ drinks/day (and even 24+ drinks/day for men) showed much higher risks of experiencing AUDs.
Conclusions:
The findings provide quantitative guidance for primary care practitioners who wish to make population-based recommendations to patients who might benefit by reducing both overall intake and amounts per occasion in an effort to lower their risks of developing AUDs.
Low-risk or “moderate” drinking guidelines for the U.S. general population (Bradley et al., 1993; Dufour, 2001; Rehm and Bondy, 1996) have been based on expert opinions (Dietary Guidelines Advisory Committee, 2000) and limited empirical findings (Dawson, 2000; Dawson et al., 2012). These include the U.S. Department of Agriculture’s (USDA’s) Dietary Guidelines (USDA, 2005; USDA and U.S. Department of Health and Human Services, 2010) and the National Institute on Alcoholism and Alcohol Abuse’s (NIAAA’s) updated Rethinking Drinking (NIAAA, 2009) (men’s weekly amount ≤14 drinks, ≤4 drinks in a day; women’s weekly amount ≤7 drinks, ≤3 drinks in a day). These guidelines emphasize recommendations for the general public or patients seen in general practice. The present study was intended to inform the discussion of low-risk drinking guidelines for the adult population as a whole, going beyond the emphasis on drinking patterns defined by the 5+ (men) and 4+ (women) thresholds.
Because the same average volume (mean drinks per day in the reference period) may be obtained by either “massed” or “spaced” drinking (Cahalan and Cisin, 1968), measures of heavy drinking have long helped to define drinking patterns. Average intake can result from a few high-quantity occasions (heavy episodic drinking) or many days of lighter “spaced” drinking (Cahalan et al., 1969).
Although other levels of intake (e.g., 8+ drinks/occasion) have also been considered as problem-drinking indicators (Knupfer, 1984), epidemiological studies have converged on 5+ drinking on an occasion (or alternately, in a day) as a risk measure because it is associated with many harms (Greenfield, 1998; Rehm et al., 1996; World Health Organization, 2000). The number of 5+ drinking days is strongly associated with nonfatal injury (Cherpitel et al., 1995), drinking and driving (Greenfield and Rogers, 1999a), arguments and fights (Nyaronga et al., 2009), and criminal behavior (Greenfield, 1998), as well as morbidity (Greenfield, 2001) and mortality (Rehm et al., 2006). Even chronic harms, such as alcohol dependence (Caetano et al., 1997), show a dose-response relationship with 5+ drinking days.
However, for drinkers with high average volume, 5+ does not adequately distinguish massed versus spaced drinking patterns, because people with high volumes report this daily amount frequently. Indeed, in clinical samples, this is the rule rather than the exception. Measuring the maximum quantity consumed (Greenfield et al., 2006) better distinguishes massed versus spaced patterns among high-volume groups, as well as low-volume groups (Greenfield and Kerr, 2008). Greenfield (1986) found that, even for heavy drinkers at a given volume, those with a higher maximum show more alcohol-related problems than do more-frequent but lower maximum drinkers. Maximum consumption has appeared as an outcome measure in clinical trials and as a phenotype for genetic studies (Malone et al., 2002; Saccone et al., 2000).
A promising method of measuring consumption patterns, the graduated-frequency (GF) approach (Greenfield, 2000), both assesses maximum consumption and provides the frequency of drinking at various quantity levels. Standardized since 1990 (Room, 1990) in the 5-yearly National Alcohol Survey, GF has been validated through comparison with drinking diaries (Greenfield et al., 2009; Hilton, 1989) and recommended by international expert groups (Dawson and Room, 2000; World Health Organization, 2000). It captures unusually large—not just typical—quantities and therefore better identifies risks for acute and chronic alcohol problems (Rehm et al., 1999).
The present study used U.S. general population data to estimate the risks of current (past-12-month) DSM-IV alcohol abuse and dependence (together, alcohol use disorder [AUD]) among current-drinker subgroups that differed on average volume and maximum number of drinks in a day. We hypothesized that, at higher volumes, higher quantity cutoffs and more-frequent heavy drinking would distinguish risks of alcohol dependence and AUD. One aim was to compare the risk levels in the empirically derived subgroups of individuals in the spectrum of drinking levels, defined both by mean volume and by frequencies of drinking at each of a series of amount-per-day levels (i.e., 5+, 8+, etc., based on the GF measure). In addition, we anticipated gender differences (Keyes et al., 2008).
Method
Study samples
We pooled data from three National Alcohol Surveys with needed, nearly identical survey items: the 2000 National Alcohol Survey (N10; n = 7,612), the 2005 National Alcohol Survey (N11; n = 6,919), and the 2010 National Alcohol Survey (N12; n = 6,855). All telephone interviews were gathered with informed consent. This yielded 12,980 current drinkers (ns for analyses vary based on complete data). Although the percentages given are weighted, unweighted ns are given in tables. Details on the survey methods are provided in Kerr et al. (2006) and Korcha et al. (2013).
Variables
Heavy-alcohol-consumption variables.
Twelve-month estimates of the frequency of heavy drinking at several levels were ascertained from the GF measure (Greenfield, 2000; Greenfield and Rogers, 1999b; Hilton, 1989). The GF yields a combined-beverage quantity-frequency series with up to six quantity levels. NIAAA (1995, 2005, 2009) defines heavy episodic drinking as >4 drinks/day for men and >3 drinks/day for women, which we ascertained. For both genders, frequencies of 8+ and 12+ drinks in a day were also available from the GF. Note that frequency categories for these quantity levels are not mutually exclusive (e.g., respondents reporting 12+ drinks/day at least monthly are also 8+ monthly drinkers). See Greenfield (2000) for additional details.
Indicators of drinking patterns were frequencies of drinking in three categorical threshold levels—12+, 8+, and 5+ (4+ for women) drinks in a day—each with four frequency levels: (a) never (in prior 12 months), (b) at least yearly but less than monthly, (c) monthly but less than weekly, and (d) weekly or more often; 24+ drinks (from the maximum) was retained as yearly or not. Because preliminary analyses indicated no empirical distinctions between at least weekly and at least monthly, final analyses used a three-level partition of frequency: never (in the last 12 months), at least yearly but less than monthly, and at least monthly.
Outcomes: Alcohol use disorders (alcohol dependence and abuse).
Alcohol dependence (12 months) was assessed using seven symptom subscales of 2—4 items each, totaling 17 items (Caetano and Greenfield, 1997). Alcohol dependence required any symptom in each of three or more of the seven areas identified, consistent with the DSM-IV diagnosis (American Psychiatric Association, 2000).
Alcohol abuse was defined using the standard one or more 12-month alcohol-related consequences involving workplace problems (three items), trouble with the law (three items), aggression and interpersonal problems (four items), and drunk driving and accidents (three items) (Greenfield et al., 2002; Midanik and Greenfield, 2000). Item content was reflective of the DSM-IV definition of alcohol abuse (significant drinking-related failure to fulfill major obligations at work, school, or home; interpersonal problems; legal problems; and drinking in hazardous situations). In the present analysis, as in the DSM-IV, alcohol dependence took precedence, and we treated (a) dependence only and (b) dependence or abuse (AUD) as outcomes.
Analysis
Segmentation analyses.
To investigate how rates of dependence diagnoses and/or abuse varied with drinking pattern, we used a segmentation technique that partitions the sample into multiple groups using the set of drinking measures. The categorical-analysis strategy maximizes differences in prevalence of the outcome and selects significantly different groups. The average volume of consumption was categorized with nine logically chosen initial levels.
Segmentation analyses used CHAID (Chi-squared Automatic Interaction Detector) implemented in AnswerTree (SPSS Inc., 2001a, 2001b), a tool for “tree growing” (Kass, 1980), successfully used in earlier alcohol studies (Greenfield, 1997). In addition, as an exploratory tool, the method has also been widely used in recent years for survey weighting adjustment (Wun et al., 2007). The CHAID algorithm examines the relationship between an outcome variable and a series of predictors and their interactions, thus progressively splitting a data set via a classification-tree structure by choosing from a set of specified variables, the one maximizing a chi-square criterion in each split. A Bonferroni-type adjustment is used to correct for the number of different ways a single predictor can be split. This is a suitable strategy for determining empirically separable drinking patterns ordered by risk outcomes, in this case quantifying the likelihood, for each pattern, of experiencing alcohol dependence or AUD.
Current analyses were conducted separately by gender. Two outcome variables were considered in separate analyses: (a) DSM-IV alcohol dependence and (b) dependence or abuse (i.e., AUD).
(a) Level 1 segmentation: Volume emerged as the first segmentation variable. At Stage 1, CHAID estimates the rate of the problem outcome within each volume category and statistically compares it with rates in neighboring volume groups. If one or more of these comparisons resulted in nonsignificant differences in rates, CHAID merged the respective volume categories (combining groups to yield a wider volume range, with no nonadjacent groups joined). The process was repeated until outcome rates in all remaining adjacent volume groups differed significantly (final categorization). Although separate analyses of the two outcome variables (dependence and AUD) could result in different segmentation of the volume variable, in our analyses there were only small differences in the final volume segmentation for the two outcomes, differing somewhat for men and women. Thus, a single, optimal partition solution was chosen, primarily based on the dependence outcome, but appropriate for AUD outcome as well, although each was allowed to differ by gender.
(b) Level 2 segmentation: Conditional on the fewer empirically distinct volume levels identified at Stage 1, drinking-pattern variables (frequency of 4+/5+, 8+, 12+ [for men and women], and 24+ [for men only]) were next added to the segmentation. At Stage 2, CHAID selects the most effectively discriminating pattern variable in regard to the outcome (e.g., frequencies of 4+/5+, 8+, etc.), for each remaining volume level, when a split is empirically viable.
(C) Higher level segmentations: Each node identified in Level 2 was considered for further segmentation using remaining pattern variables. Rates of the outcome variable under consideration were estimated for each of the categories of the remaining quantity threshold variables, and categories were again merged for nonsignificant rates among adjacent groups. The drinking-pattern variable chosen to partition the specific volume subgroup under consideration is the one with the smallest adjusted p value (≤.05). Level 3 segmentation could occur if a volume-pattern group could be empirically split by a different pattern variable (e.g., for male AUD, the ≤1 drink/week and 5+ yearly group was segmented into never 8+ and at least yearly 8+). If no drinking-pattern variable produced such an adjusted p value, then the volume-pattern subgroup was not segmented further.
Results
Segmentation analysis
Tables 1 (men) and 2 (women) provide characteristics of the resultant segmentation groups among current drinkers in the population. For men (Table 1)—taking alcohol dependence as the outcome but also displaying levels of AUD—in the first two volume groups (those up to 1 drink/day), the Level 2 empirical cut point was never versus ever consuming 5+ drinks in a day in the past 12 months.
Table 1.
Volume and pattern segmentation analysis summary based on DSM-IV alcohol dependence for mena
| Mean depend. criteria counts (0–7) |
Mean abuse and depend. criteria counts (0–11) |
|||||||||||
| Average volume (in drinks) (Level 1) | Heavy drinking threshold measure (Level 2) | Heavy drinking threshold measure (Level 3) | % among drinkers (n = 5,922) | Mean volume (drinks/week) | % depend. | % depend. or abuse | All | Pos.b | Neg.b | All | Pos.c | Neg.c |
| No more than | Never 5+ | – | 30.4 | 0.3 | 0.3 | 3.0 | 0.06 | 3.97 | 0.05 | 0.09 | 1.91 | 0.04 |
| 1/week | Any 5+*** | Never 8+ | 3.5 | 0.5 | 0.9 | 10.3 | 0.25 | 4.00 | 0.21 | 0.35 | 2.22 | 0.14 |
| Any 8+* | 0.7 | 0.6 | 6.3 | 14.7 | 0.52 | 3.80 | 0.30 | 0.75 | 3.59 | 0.26 | ||
| No more than | Never 5+ | – | 17.0 | 2.9 | 1.1 | 6.0 | 0.13 | 4.54 | 0.08 | 0.20 | 2.26 | 0.07 |
| 1/day | Any 5+*** | Never 8+ | 9.9 | 3.3 | 2.8 | 16.8 | 0.29 | 3.26 | 0.21 | 0.46 | 1.90 | 0.17 |
| Any 8+** | 8.2 | 3.6 | 6.7 | 33.5 | 0.66 | 3.60 | 0.45 | 1.08 | 2.59 | 0.32 | ||
| No more than | 5+ <monthly | – | 8.9 | 9.8 | 2.8 | 17.0 | 0.34 | 3.91 | 0.24 | 0.54 | 2.44 | 0.15 |
| 2/day | 5+ ≥monthly*** | 8+ <monthly | 2.8 | 10.3 | 4.3 | 39.8 | 0.54 | 4.19 | 0.38 | 1.01 | 2.33 | 0.14 |
| 8+ ≥monthly** | 2.1 | 9.7 | 13.4 | 49.8 | 1.09 | 3.75 | 0.67 | 1.65 | 2.83 | 0.48 | ||
| No more than | 8+ <monthly | – | 4.7 | 19.0 | 9.3 | 33.4 | 0.88 | 4.27 | 0.53 | 1.25 | 2.92 | 0.42 |
| 4/day | 8+ ≥monthly*** | 12+ <monthly | 2.4 | 21.1 | 15.6 | 52.5 | 1.17 | 3.72 | 0.70 | 1.82 | 2.91 | 0.61 |
| 12+ ≥monthly** | 1.2 | 21.0 | 33.9 | 70.0 | 1.84 | 3.36 | 1.06 | 2.78 | 3.63 | 0.78 | ||
| More than | 8+ <monthly | – | 0.7 | 33.5 | 15.4 | 41.7 | 1.23 | 4.70 | 0.59 | 1.69 | 3.62 | 0.31 |
| 4/day | 8+ ≥monthly** | Never 24+ | 4.9 | 47.7 | 32.9 | 70.1 | 2.14 | 4.89 | 0.79 | 3.21 | 4.38 | 0.47 |
| Any 24+*** | 2.4 | 62.7 | 50.3 | 82.5 | 2.79 | 4.45 | 1.11 | 4.33 | 5.13 | 0.58 | ||
Notes: Chi-square test with Bonferroni-type adjustment using Chi-squared Automatic Interaction Detection (CHAID) algorithm. DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; depend. = dependence; pos. = positive; neg. = negative.
Weighted percentages given in table; total percentage of last-12-month DSM-IV alcohol dependence among men drinkers: 6.0%; equivalent alcohol use disorder total: 20.0%;
count is of symptoms in each of 7 DSM-IV domains (pos.: only for those positive for dependence; neg.: only for those negative for dependence); ccount is of 7 dependence domains and 4 abuse domains (pos.: only for those positive for abuse or dependence; neg.: only for those negative for abuse or dependence).
p < .05;
p < .01;
p < .001.
In the lowest volume groups averaging ≤1 drink/week, CHAID chose a two-pattern split, adding a Level 3 split of any versus no prior-year 8+ days. Although this intake volume is low, men who indicated heavy episodic drinking at the 5+ threshold level (only) had significantly elevated rates of alcohol dependence (0.9% vs. 0.3%) and especially dependence or abuse (AUD): above 10% (weighted percentage). The effect was greater for the intermittent heavy drinkers having an 8+ maximum: about 6% alcohol dependence and 15% AUD. Only 3% of men never reporting 5+ drinks in any day last year met the criteria for an AUD. Thus, among male current drinkers, even at low volume levels, defining heavy drinking not only as 5+ days but also by the higher level of 8+ had utility for risk estimation. For the next two volume groups, from 2 drinks/week to 2 drinks/day (i.e., ≤14 drinks/week, the average volume component of low-risk guidelines), the frequency of 5+ (never vs. ever in 12 months up to 1 drink/day and less than monthly vs. more often for >1 to 2 drinks/day) distinguished between levels of alcohol problems. In addition, never versus ever drinking 8+ (for up to 1 drink/day) and monthly versus more often 8+ (for 1-2 drinks/day) also added to risks of both alcohol dependence and AUD. Thus, rates of dependence in the greater than weekly but up to 1 drink/day volume group ranged from 1% (never 5+) to 7% (with some 8+ drinking), whereas for AUD the range was from 6% with no 5+ to a third (33.5%) with some 8+ drinking. At the >1 drink/day but up to 2 drinks/day volume level, the similar ranges for dependence were 3% to 13% and for AUD were 17% to almost half (49.8%). In the fourth volume group (≤4 drinks/ day average), the rates of dependence ranged higher, 9% to a third (34%), and for AUD from a third (33%) to 70%, depending on whether 8+ drinking was <monthly or monthly or more, and depending on whether there was also 12+ drinking <monthly or monthly or more. Finally, at the highest volumes, >4 drinks/day average 8+ monthly or more, and in this case never versus ever indicating 24 or more/day, yielded a dependence range from 15% to a half (50%) and yielded an AUD range from 42% to 83%. Therefore, men’s results for the segmentation analysis indicate both volume and drinking-pattern effects, as hypothesized. At successively higher volumes, higher maximum drinking patterns (and higher rates of high-threshold drinking) progressively come into play in determining risks of both alcohol dependence and AUD. At lower volumes and for “less risky” low-quantity patterns, abuse and dependence are uncommon. However, at the highest volumes and with higher quantity patterns, more than half the group is dependent, and AUD is present for more than three quarters.
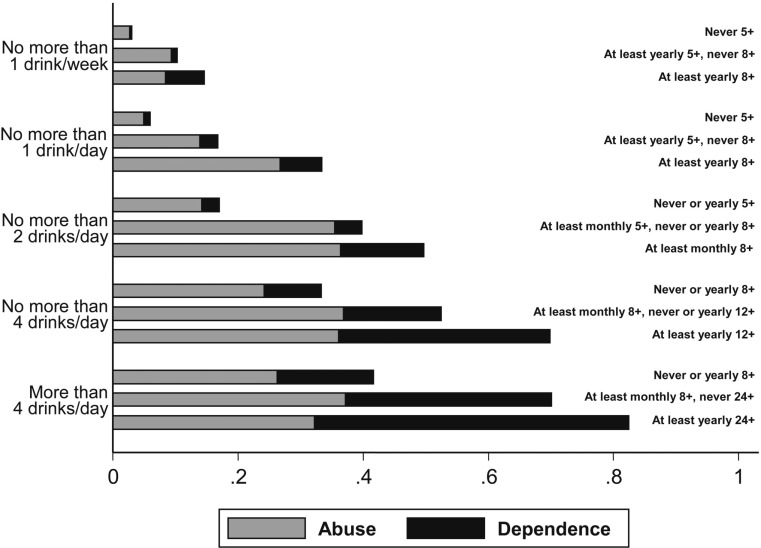
When instead of dependence, AUD is taken as the empirical outcome of the segmentation analyses (but again looking at dependence prevalence also), a slightly different solution but with extremely similar overall characteristics emerged (table not shown but available from the first author on request). Never versus ever drinking 5+ was an important determinant at lower volumes; 8+ played an additional distinguishing role in the intermediate and higher levels of volume and, additionally, 12+ at the highest volume levels. In this case, 24+ did not enter as a discriminating pattern variable at the >4 drinks/day volume level, no doubt because AUD involves a broader classification inclusive of consequences, whereas alcohol dependence, although less prevalent, is in essence more severe. We prefer the dependence-based analysis (Table 1) because, at the highest level of risk (volume >4 drinks/day, some 24+ drinking), 50% indicated alcohol dependence (40% in the AUD-based analysis), with AUD prevalences generally being similar, but the outcome more concentrated in the dependence-based analysis (83% vs. 79%). To aid the reader, we present a graph displaying results for the dependence-based solution (Figure 1).
Figure 1.
Proportions of alcohol abuse and dependence by volume and heavy drinking, for male drinkers
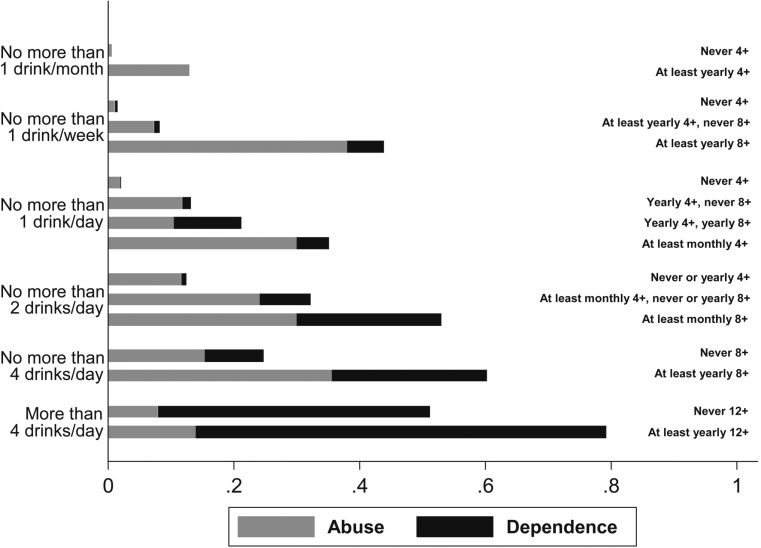
For women (Table 2), the best empirical segmentation of volume differed from that found for men, distinguishing a sizable group (35.4% of current drinkers, reflecting low intake of many U.S. women) of very-low-volume drinkers (≤1 drink/month average) with very low rates of alcohol dependence. The top four groups were similar to the men’s solution and were set to be identical to simplify comparisons (see also Figure 2).
Table 2.
Volume and pattern segmentation analysis summary based on DSM-IV alcohol dependence for womena
| Mean depend. criteria counts (0–7) |
Mean abuse and depend. criteria counts (0–11) |
|||||||||||
| Average volume (in drinks) (Level 1) | Heavy drinking threshold measure (Level 2) | Heavy drinking threshold measure (Level 3) | % among drinkers (n = 6,270) | Mean volume (drinks/week) | % depend. | % depend. or abuse | All | Pos.b | Neg.b | All | Pos.c | Neg.c |
| No more than | Never 4+ | – | 33.4 | 0.1 | 0.1 | 0.7 | 0.02 | 3.96 | 0.02 | 0.03 | 1.97 | 0.02 |
| 1/month | Any 4+d | – | 1.0 | 0.2 | 0.0 | 13.0 | 0.30 | n.a. | 0.30 | 0.46 | 2.11 | 0.21 |
| No more than | Never 4+ | – | 15.6 | 0.5 | 0.3 | 1.5 | 0.06 | 3.15 | 0.05 | 0.07 | 2.00 | 0.04 |
| 1/week | Any 4+* | Never 8+ | 5.8 | 0.6 | 0.9 | 8.3 | 0.23 | 4.94 | 0.19 | 0.32 | 2.26 | 0.14 |
| Any 8+* | 0.5 | 0.6 | 5.8 | 43.9 | 0.63 | 3.77 | 0.43 | 1.01 | 2.08 | 0.17 | ||
| Never 4+ | – | 15.1 | 2.9 | 0.1 | 2.1 | 0.08 | 3.00 | 0.08 | 0.10 | 2.04 | 0.06 | |
| No more than | 4+ <monthly | Never 8+ | 10.4 | 2.8 | 1.5 | 13.3 | 0.37 | 3.43 | 0.32 | 0.49 | 1.78 | 0.30 |
| 1/day | Any 8+*** | 1.5 | 2.3 | 10.8 | 21.3 | 0.64 | 3.26 | 0.33 | 0.85 | 2.86 | 0.30 | |
| 4+ ≥monthly*** | – | 4.5 | 4.4 | 5.1 | 35.1 | 0.78 | 3.63 | 0.62 | 1.19 | 2.52 | 0.46 | |
| No more than | 4+ <monthly | – | 4.5 | 9.8 | 0.8 | 12.5 | 0.23 | 5.85 | 0.19 | 0.36 | 1.75 | 0.16 |
| 2/day | 4+ ≥monthly*** | 8+ <monthly | 2.3 | 10.1 | 8.2 | 32.3 | 0.68 | 3.83 | 0.40 | 1.03 | 2.50 | 0.33 |
| 8+ ≥monthly** | 1.2 | 10.4 | 23.1 | 53.1 | 1.56 | 4.30 | 0.74 | 2.25 | 3.82 | 0.46 | ||
| No more than | Never 8+ | – | 2.6 | 18.5 | 9.5 | 24.9 | 0.72 | 4.16 | 0.36 | 1.04 | 3.30 | 0.29 |
| 4/day | Any 8+** | – | 1.3 | 19.2 | 24.8 | 60.3 | 1.57 | 3.58 | 0.90 | 2.31 | 3.27 | 0.86 |
| More than | Never 12+ | – | 0.8 | 43.2 | 43.3 | 51.2 | 2.55 | 5.27 | 0.48 | 3.30 | 6.05 | 0.42 |
| 4/day | Any 12+e | – | 0.6 | 56.0 | 65.3 | 79.2 | 3.24 | 4.39 | 1.07 | 4.39 | 5.31 | 0.91 |
Notes: Chi-square test with Bonferroni-type adjustment using Chi-squared Automatic Interaction Detection (CHAID) algorithm. DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; depend. = dependence; pos. = positive; neg. = negative; n.a. = not applicable.
Weighted percentages given in table; total percentage of last-12-month DSM-IV alcohol dependence among women drinkers: 2.5%; equivalent alcohol use disorder total: 9.1%;
count is of symptoms in each of 7 DSM-IV domains (pos.: only for those positive for dependence; neg.: only for those negative for dependence);
count is of 7 dependence and 4 abuse domains (pos.: only for those positive for abuse or dependence; neg.: only for those negative for abuse or dependence);
CHAID fails to split this volume category predicting dependence; this pattern split is based on significantly predicting abuse or dependence;
CHAID fails to split this volume category predicting dependence (p = .17); this pattern split is based on significantly predicting abuse or dependence.
p < .05;
p < .01;
p < .001.
Figure 2.
Proportions of alcohol abuse and dependence by volume and heavy drinking, for female drinkers
One striking feature of the CHAID analysis that focused on dependence for all female drinkers is that for volumes up to an average of 1 drink/day (within the NIAAA weekly low-risk drinking limit; NIAAA, 2009), when no 4+ drinks are reported in any day, the risk of alcohol dependence (<1%) and even AUD (1%-2%) appears minimal. However, importantly, 24% (1,486 of 6,270) of women in these three lowest risk volumes do exceed the 3 drinks/day quantity limit (4+), and 2% (125) of women indicate some 8+ drinking episodes, thus carrying substantially higher risks of from 6% to 11% of alcohol dependence (21%-44% risk of AUD). Of women drinking at the 1-2 drinks/day volume, 3.5% report 4+ at least monthly and 1.2% indicate 8+ drinking episodes, with both groups carrying elevated risks of alcohol dependence (8% and 23%, respectively). This reinforces other U.S. findings (true also for men) that even low-volume drinking more often than not involves occasional hazardous quantities (Greenfield et al., 2003).
Figures 1 (for men) and 2 (for women) provide results of CHAID analyses based on the alcohol dependence outcome. The stacked bars for the volume pattern levels allow demarcation for each volume by pattern group and indicate what proportion reported DSM-IV alcohol dependence and what proportion indicated abuse only (the total being AUD). In the analyses shown for men and women, the four volume levels from more than 1 drink/week but no more than 1 drink/ day, up to more than 4 drinks/day, are the same for men and women, thus simplifying comparison. There is some evidence, comparing the two figures (see also Tables 1 and 2), that women with heavy drinking patterns carry greater risks of alcohol dependence than men at equivalent volumes. Although the pattern specifics differ in the CHAID analyses of men and women, higher risk pattern measures segmenting women’s dependence were at a lower threshold than men’s for given volume levels. For example, at average volumes of 2-4 drinks/week, the empirical pattern cut point for women was never versus ever 8+, with risks of alcohol dependence of 10% and 25%, respectively; at the same volume level, cut points for men were never 8+ monthly versus at least monthly 8+, further divided by never 12+ monthly versus 12+ monthly (with a risk range from 9% to 34% of being alcohol dependent). At the mean volume of >4 drinks/day levels, the highest risk for women for those ever having 12+ drinks ever in the year was 65%, whereas for men—even for those drinking 24 drinks in a day—it was 50%. Thus, at this high volume, women tend to be at risk for alcohol dependence at a lower frequency and quantity of heavy drinking than are men.
Discussion
Risks for current drinkers in general
For current drinkers in the U.S. general population, both average volume and frequency of drinking larger-than-usual quantities in a day are important determinants of the risk of DSM-IV alcohol dependence and AUD. Although the often-reported 5+ (for men) and 4+ (for women) drinks/day are important problem indicators at modest levels of intake, at mid- to high-average (moderate) volume, the frequency of 8+ episodes (whether reported at all or at least monthly in the prior year) becomes a major discriminator of individuals with alcohol abuse and/or alcohol dependence for both women and men. This was so at regular intake levels from as low as 1 drink/week to as high as 2-4 drinks/day for women, and from <1 drink/week and <2 drinks/day for men. For both genders, at the highest volumes (>4 drinks/day on average), surprisingly high amounts in any day last year (i.e., a maximum of 12+ for women and 24+ for men) distinguished the likelihood of experiencing alcohol dependence from those with a less variable pattern. For high-volume men, frequent 8+ days (at least monthly) were also important. Empirically higher rates of AUD were seen for those with a variable pattern (higher maximum) at all volumes. Pattern played a less important role at the higher volumes (where many people have heavy drinking days) but remained influential.
At an intermediate intake level, averaging 2-4 drinks/ day, men’s risk for alcohol dependence increased if they drank 8 or more drinks in a day ever in the previous year compared with never, from 8% to 13% and increasing again to a quarter meeting criteria if they drank 12+ ever. For women at the same volume range, reporting any 8+ episode in the preceding year was the discriminating feature, with a quarter found dependent in contrast to a tenth among those never drinking 8+ drinks. Empirically, at this volume range, 5+ (or 4+ for women) was not an effective pattern measure because most regularly drank this amount. However, at lower volume levels, the standard 5+/4+ measures distinguished massed (or “heavy episodic”) versus spaced drinking patterns. Using the large U.S. sample from the three national surveys, we replicated a finding result noted for university students (Greenfield, 1986) showing that different pattern indicators are essential to identify patterns of drinking that are meaningful at high, middle, and low volumes. The overall results are not surprising given the common-sense logic that a higher maximum of heavy drinking is needed to separate relative heavy episodic drinkers and spacers at high volumes of intake and lower ones at low volumes of intake.
For the adult drinking population, groups with considerably different relative (or absolute) risk for alcohol problems can be identified using the segmentation analyses at all average consumption volume levels. Importantly, however, for both dependence and AUD, it is possible to incur lower risks while drinking at a higher volume when there were no heavy drinking occasions than at a lower volume of consumption that includes heavy drinking occasions, as can be observed for men and women in Figures 1 and 2, respectively.
Limitations
An acknowledged limitation of the results is their cross-sectional, correlational nature and that they are based on self-report summary measures. The measures used assume standard drinks and do not take account of actual drink sizes, which may be larger for many people at home (Kerr et al., 2005) and in bars (Kerr et al., 2008). In this light, it is interesting how effective the volume and threshold measures are at distinguishing different levels of AUD risks. One important limitation is that volume and pattern as defined here are not entirely independent, as can be seen from the mean-volume column for each volume heavy drinking category in the tables. In some cases, the volume-pattern level—including some heavier occasions—has a lower mean volume than the less variable low-threshold volume. However, especially when a Level 3 pattern involves frequent very high amounts in a day, the mean volume may also be somewhat larger.
The analyses pool data from three recent U.S. national surveys with identical measures, all using random-digit-dialed telephone interviewing. An important asset of the analysis is its use of extensive U.S. probability samples, making it likely that the results are generalizable to the nation. These empirical findings are based on well-conducted, large-scale population surveys that included substantial numbers of heavy drinkers. Therefore, we deem it plausible to consider this evidence among other data to guide the advice of primary care clinician to their patients regarding drinking.
For those in the U.S. general population who choose to drink rather than abstain, the NIAAA-recommended amounts of no more than 3 drinks for a woman and 4 drinks on any occasion for a man (as borne out by the empirical study of other health outcomes by Dawson, 2000) appear for the most part serviceable and “protective.”
Conclusions
Where drinking does not exceed an average of 1 drink/ day, and the quantities never exceed 4 drinks for a man and 3 drinks for a woman, the associated 12-month risks of AUD are less than 10%. Where the individual mean consumption is from 1 to 2 drinks/day for a man, within the 4 drinks or less quantity limits, the risks of experiencing an AUD are less than 20%.
The findings may have particular relevance for brief interventions targeting heavy drinkers seen in primary care settings. Providing an evidence base for advice regarding low-risk drinking patterns for the general population is the immediate contribution of our study. Future research will investigate the low-risk guidelines more suited to key population subgroups such as those recovering from alcohol dependence who may wish to resume drinking, for whom these general guidelines (as indicated in Rethinking Drinking, NIAAA, 2009) are likely not to be appropriate.
Footnotes
This research was supported by Center Grant P50 AA005595 (to the Public Health Institute, Alcohol Research Group), including a supplement from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and Grant K24 AA13736 to Dr. Kranzler. Dr. Litten’s contribution was supported by NIAAA. Drs. Anton and Kranzler performed this work in conjunction with their affiliation with the Alcohol Clinical Trials Initiative (ACTIVE) sponsored by the American Society of Clinical Psychopharmacology and funded in part by the following pharmaceutical companies: Eli Lilly, Alkermes, Lundbeck, and AbbVie (formerly Abbott Laboratories). In addition, Dr. Anton in the last 12 months was a member of the Scientific Advisory Board for Lundbeck and acted as a consultant for GlaxoSmithKline. In the last 12 months, Dr. Kranzler was a consultant to Alkermes, Lilly, Lundbeck, Pfizer, and Roche. Opinions are those of the authors and not the sponsoring institutions. Pharmaceutical companies listed herein have not reviewed or commented on the research.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, text revision. 4th ed. Washington, DC: Author; 2000. [Google Scholar]
- Bradley KA, Donovan DM, Larson EB. How much is too much? Advising patients about safe levels of alcohol consumption. Archives of Internal Medicine. 1993;153:2734–2740. doi: 10.1001/archinte.153.24.2734. [DOI] [PubMed] [Google Scholar]
- Caetano R, Greenfield TK. Trends in DSM-IV alcohol dependence: 1990 and 1995 U.S. national alcohol surveys. Berkeley, CA: Alcohol Research Group, Public Health Institute; 1997. [Working paper] [Google Scholar]
- Caetano R, Tam TW, Greenfield TK, Cherpitel CJ, Midanik LT. DSM-IV alcohol dependence and drinking in the U.S. population: A risk analysis. Annals of Epidemiology. 1997;7:542–549. doi: 10.1016/s1047-2797(97)00114-2. [DOI] [PubMed] [Google Scholar]
- Cahalan D, Cisin IH. American drinking practices: Summary of findings from a national probability sample. II. Measurement of massed versus spaced drinking. Quarterly Journal of Studies on Alcohol. 1968;29:642–656. [PubMed] [Google Scholar]
- Cahalan D, Cisin IH, Crossley HM. American Drinking Practices: A national survey of drinking behavior and attitudes (Monograph No. 6) New Brunswick, NJ: Rutgers Center of Alcohol Studies; 1969. [Google Scholar]
- Cherpitel CJ, Tam TW, Midanik LT, Caetano R, Greenfield TK. Alcohol and non-fatal injury in the U.S. general population: A risk function analysis. Accident Analysis and Prevention. 1995;27:651–661. doi: 10.1016/0001-4575(95)00011-n. [DOI] [PubMed] [Google Scholar]
- Dawson DA. US low-risk drinking guidelines: An examination of four alternatives. Alcoholism: Clinical and Experimental Research. 2000;24:1820–1829. [PubMed] [Google Scholar]
- Dawson DA, Room R. Towards agreement on ways to measure and report drinking patterns and alcohol-related problems in adult general population surveys: The Skarpö conference overview. Journal of Substance Abuse. 2000;12:1–21. doi: 10.1016/s0899-3289(00)00037-7. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Smith SM, Pickering RP, Grant BF. An empirical approach to evaluating the validity of alternative low-risk drinking guidelines. Drug and Alcohol Review. 2012;31:141–150. doi: 10.1111/j.1465-3362.2011.00335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietary Guidelines Advisory Committee. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2000. 2000 [Archived by WebCite® at http://www.webcitation.org/69EgpsvDZ]. Washington, DC: U.S. Department of Agriculture Human Nutrition Information Service. [Google Scholar]
- Dufour MC. If you drink alcoholic beverages, do so in moderation: What does this mean? Journal of Nutrition. 2001;131:552s–561s. doi: 10.1093/jn/131.2.552S. [DOI] [PubMed] [Google Scholar]
- Greenfield TK. Quantity per occasion and consequences of drinking: A reconsideration and recommendation. International Journal of the Addictions. 1986;21:1059–1079. doi: 10.3109/10826088609077255. [DOI] [PubMed] [Google Scholar]
- Greenfield TK. Warning labels: Evidence of harm reduction from long-term American surveys. In: Plant M, Single E, Stockwell T, editors. Alcohol: Minimizing the harm. London, England: Free Association Books; 1997. pp. 105–125. [Google Scholar]
- Greenfield TK. Evaluating competing models of alcohol-related harm. Alcoholism: Clinical and Experimental Research, 22, Supplement s2. 1998:52s–62s. doi: 10.1097/00000374-199802001-00008. [DOI] [PubMed] [Google Scholar]
- Greenfield TK. Ways of measuring drinking patterns and the difference they make: Experience with graduated frequencies. Journal of Substance Abuse. 2000;12:33–49. doi: 10.1016/s0899-3289(00)00039-0. [DOI] [PubMed] [Google Scholar]
- Greenfield TK. Individual risk of alcohol-related disease and problems. In: Heather N, Peters TJ, Stockwell T, editors. International handbook of alcohol problems and dependence. New York, NY: John Wiley; 2001. pp. 413–437. [Google Scholar]
- Greenfield TK, Bond J, Midanik LT, Cherpitel CJ, Kerr WC. How drinking patterns affect alcohol dependence and consequences: A risk-curve analysis from a multi-ethnic national sample. Philadelphia, PA: Presented at the American Public Health Association Annual Meeting; 2002. [Google Scholar]
- Greenfield TK, Kerr WC. Alcohol measurement methodology in epidemiology: Recent advances and opportunities. Addiction. 2008;103:1082–1099. doi: 10.1111/j.1360-0443.2008.02197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield TK, Kerr WC, Bond J, Ye Y, Stockwell T. Improving graduated frequencies alcohol measures for monitoring consumption patterns: Results from an Australian national survey and a US diary validity study. Contemporary Drug Problems. 2009;36(3/4):705–733. doi: 10.1177/009145090903600320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield TK, Nayak MB, Bond J, Ye Y, Midanik LT. Maximum quantity consumed and alcohol-related problems: Assessing the most alcohol drunk with two measures. Alcoholism: Clinical and Experimental Research. 2006;30:1576–1582. doi: 10.1111/j.1530-0277.2006.00189.x. [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Rogers JD. Alcoholic beverage choice, risk perception and self-reported drunk driving: Effects of measurement on risk analysis. Addiction. 1999a;94:1735–1743. doi: 10.1046/j.1360-0443.1999.9411173510.x. [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Rogers JD. Who drinks most of the alcohol in the U.S.? The policy implications. Journal of Studies on Alcohol. 1999b;60:78–89. doi: 10.15288/jsa.1999.60.78. [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Ye Y, Bond J, Kerr WC, Rehm J, Nayak MB. Most of the alcohol consumed in the U.S. is not drunk safely: The health policy implications. San Francisco, CA: Presented at the American Public Health Association Annual Meeting; 2003. [Google Scholar]
- Hilton ME. A comparison of a prospective diary and two summary recall techniques for recording alcohol consumption. British Journal of Addiction. 1989;84:1085–1092. doi: 10.1111/j.1360-0443.1989.tb00792.x. [DOI] [PubMed] [Google Scholar]
- Kass GV. An exploratory technique for investigating large quantities of categorical data. Applied Statistics. 1980;29:119–127. [Google Scholar]
- Kerr WC, Greenfield TK, Midanik LT. How many drinks does it take you to feel drunk? Trends and predictors for subjective drunkenness. Addiction. 2006;101:1428–1437. doi: 10.1111/j.1360-0443.2006.01533.x. [DOI] [PubMed] [Google Scholar]
- Kerr WC, Greenfield TK, Tujague J, Brown SE. A drink is a drink? Variation in the amount of alcohol contained in beer, wine and spirits drinks in a US methodological sample. Alcoholism: Clinical and Experimental Research. 2005;29:2015–2021. doi: 10.1097/01.alc.0000187596.92804.bd. [DOI] [PubMed] [Google Scholar]
- Kerr WC, Patterson D, Koenen MA, Greenfield TK. Alcohol content variation of bar and restaurant drinks in Northern California. Alcoholism: Clinical and Experimental Research. 2008;32:1623–1629. doi: 10.1111/j.1530-0277.2008.00741.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Grant BF, Hasin DS. Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug and Alcohol Dependence. 2008;93:21–29. doi: 10.1016/j.drugalcdep.2007.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knupfer G. The risks of drunkenness (or ebrietas resurrecta). A comparison of frequent intoxication indices and of population subgroups as to problem risks. British Journal of Addiction. 1984;79:185–196. doi: 10.1111/j.1360-0443.1984.tb00261.x. [DOI] [PubMed] [Google Scholar]
- Korcha RA, Polcin DL, Kerr WC, Greenfield TK, Bond J. Pressure and help seeking for alcohol problems: Trends and correlates from 1984 to 2005. Addictive Behaviors. 2013;38:1740–1746. doi: 10.1016/j.addbeh.2012.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malone SM, Iacono WG, McGue M. Drinks of the father: Father’s maximum number of drinks consumed predicts externalizing disorders, substance use, and substance use disorders in preadolescent and adolescent offspring. Alcoholism: Clinical and Experimental Research. 2002;26:1823–1832. doi: 10.1097/01.ALC.0000042222.59908.F9. [DOI] [PubMed] [Google Scholar]
- Midanik LT, Greenfield TK. Trends in social consequences and dependence symptoms in the United States: The National Alcohol Surveys, 1984-1995. American Journal of Public Health. 2000;90:53–56. doi: 10.2105/ajph.90.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. The physician’s guide to helping patients with alcohol problems. [NIH Publication No. 95–3769] Rockville, MD: Author; 1995. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: A clinician s guide. Rockville, MD: Author; 2005. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Rethinking drinking: Alcohol and your health. 2009 [Archived by WebCite® at http://www.webcitation.org/5wtRANlQ7]. Bethesda, MD: Author. [Google Scholar]
- Nyaronga D, Greenfield TK, McDaniel PA. Drinking context and drinking problems among Black, White, and Hispanic men and women in the 1984, 1995, and 2005 U.S. National Alcohol Surveys. Journal of Studies on Alcohol and Drugs. 2009;70:16–26. doi: 10.15288/jsad.2009.70.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Ashley MJ, Room R, Single E, Bondy SJ, Ferrence RG, Giesbrecht N. On the emerging paradigm of drinking patterns and their social and health consequences. Addiction. 1996;91:1615–1621. [PubMed] [Google Scholar]
- Rehm J, Bondy S. Risk functions, low risk drinking guidelines, and the benefits of moderate drinking. Addiction. 1996;91:1439–1441. [Google Scholar]
- Rehm J, Greenfield TK, Kerr W. Patterns of drinking and mortality from different diseases—An overview. Contemporary Drug Problems. 2006;33:205–235. [Google Scholar]
- Rehm J, Greenfield TK, Walsh G, Xie X, Robson L, Single E. Assessment methods for alcohol consumption, prevalence of high risk drinking and harm: A sensitivity analysis. International Journal of Epidemiology. 1999;28:219–224. doi: 10.1093/ije/28.2.219. [DOI] [PubMed] [Google Scholar]
- Room R. Measuring alcohol consumption in the United States: Methods and rationales. In: Kozlowski LT, Annis HM, Cappell HD, Glaser FB, Goodstadt MS, Israel Y, Kalant H, Sellers EM, Vingilis ER, editors. Research advances in alcohol and drug problems. Vol. 10. New York, NY: Plenum Press; 1990. pp. 39–80. [Google Scholar]
- Saccone NL, Kwon JM, Corbett J, Goate A, Rochberg N, Edenberg HJ, Rice JP. A genome screen of maximum number of drinks as an alcoholism phenotype. American Journal of Medical Genetics. 2000;96:632–637. doi: 10.1002/1096-8628(20001009)96:5<632::aid-ajmg8>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- SPSS Inc. AnswerTree 3.0. Chicago, IL: Author; 2001a. [Google Scholar]
- SPSS Inc. AnswerTree user’s guide. Chicago, IL: Author; 2001b. [Google Scholar]
- U.SDepartment of Agriculture. Dietary guidelines for Americans. 6th ed. Washington, DC: Author; 2005. [Google Scholar]
- U.S. Department of Agriculture & U.S. Department of Health and Human Services. Dietary guidelines for Americans, 2010. (7th ed.) 2010 [Archived by WebCite® at http://www.webcitation.org/5wM9GjvZ3]. Washington, DC: U.S. Government Printing Office. [Google Scholar]
- World Health Organization. International guide for monitoring alcohol consumption and related harm. Copenhagen, Denmark: World Health Organization, Department of Mental Health and Substance Dependence, Noncommunicable Diseases and Mental Health Cluster; 2000. [Google Scholar]
- Wun L-M, Ezzati-Rice TM, Diaz-Tena N, Greenblatt J. On modeling response propensity for dwelling unit (DU) level non-response adjustment in the Medical Expenditure Panel Survey (MEPS) Statistics in Medicine. 2007;26:1875–1884. doi: 10.1002/sim.2809. [DOI] [PubMed] [Google Scholar]