Abstract
Objective
The purpose of this study was to evaluate risk factors of vaginal cuff dehiscence or evisceration according to the type of operation.
Methods
Medical records of 604 women who underwent hysterectomies at Korea University Anam Hospital between June 2007 and June 2011 were reviewed. They were allocated to six groups. The six types of hysterectomies included robotic hysterectomy (n = 7), robotic radical hysterectomy and node dissection (RRHND, n = 9), total laparoscopic hysterectomy (TLH, n = 274), laparoscopy assisted vaginal hysterectomy (LAVH, n = 238), laparoscopic radical hysterectomy and node dissection (n = 11), and abdominal radical hysterectomy (ARH, n = 63). The characteristics and outcomes of each groups were compared.
Results
There was no difference in the characteristics of patients between 6 groups. In total of 604 hysterectomies, 3 evisceration (0.49%) and 21 dehiscences (3.47%) occurred. Evisceration were found in RRHND (1/9, 11.1%), TLH (1/276, 0.36%), and ARH (1/63, 1.56%). Dehiscences occurred in TLH (15/274, 5.42%), LAVH (4/238, 1.68%), and ARH (2/63, 3.17%). In 169 cases of TLH with intra-corporeal continuous suture, 1 evisceration and 4 dehiscences occurred, whereas 11 dehiscences occurred in 105 TLH cases with vaginal continuous locking suture (2.96% vs. 10.47%, P = 0.02).
Conclusion
The incidence of vaginal cuff dehiscenceand eviscerationwas significantly higher in TLH than LAVH. The intra-corporeal cuff suture was superior to the vaginal suture to prevent the vaginal cuff complications in TLH.
Keywords: Complications, Hysterectomy, Surgical wound dehiscence, Suture techniques
Introduction
Hysterectomy is one of the most common gynecological surgeries performed in Korea. A variety of complication can occur with hysterectomies including bladder injury, ureteral injury, gastrointestinal injury, hemorrhage, postoperative fever, and vaginal vault prolapsed [1]. Vaginal cuff dehiscence or evisceration (VCDE) are rare but serious complication of hysterectomy. Vaginal cuff dehiscence has been defined as a full thickness separation, partial or total, of the anterior and posterior edges of the vaginal cuff with or without bowel evisceration [2]. The distal ileum is the most frequent eviscerating organ when vaginal evisceration is observed although prolapse of the omentum, appendix and fallopian tubes have also been reported [3]. When it occurs, prompt surgical and medical intervention is required to ensure optimal care.
Hysterectomy can now be performed utilizing minimally invasive surgical techniques such as laparoscopy. Previous studies suggest that the rate of VCDE seems to have been shown to increase after laparoscopic surgeries compared with that after the open approach [3,4,5]. The report postulated that the use of thermal energy in addition to other factors unique to laparoscopic surgery may be responsible for and increased risk of vaginal cuff dehiscence compared with other modes of total hysterectomy. As surgical equipment and techniques continue to improve, hysterectomies are increasingly performed with laparoscopy and related complications have been decreased. Possibly owing to this improvement, recently several authors have reported different surgical approaches between abdominal or vaginal and laparoscopic without substantial differences. Iaco et al. [6] reported that although the incidence of dehiscence is highest among total laparoscopic hysterectomies, it is not as high as previously reported. As a way of minimally invasive surgical techniques, robotic surgery is becoming common practice for hysterectomy recently. Kho et al. [7] revealed that robotic hysterectomy is feasible with minimal complications noted through the 6-week postoperative recovery time. But, in another report comparing robotic surgery to other mode of operation, the robotic surgery showed worse postoperative prognosis [8].
Not only surgical modality but also type of hysterectomy affects the incidence of vaginal cuff complication. Nick et al. [9] reported that radical hysterectomy was associated with a 9-fold increase in vaginal cuff complication. Also, special consideration should be given to the colpotomy incision and vault closure concerning vaginal dehiscence during total laparoscopic hysterectomy (TLH) [10]. Concerning about the technical difficulty of laparoscopic surgery, this study provides suggestions for prevention of vaginal cuff problems in terms of the type of suture techniques during TLH.
This study compared the incidence of vaginal cuff problems from different approaches to hysterectomy to assess which mode of hysterectomy poses a lesser risk for vaginal cuff problems and described the patient characteristics of those with VCDE after hysterectomy to identify potential risk factors for this complication. This study has great significance because of the fact that there is a dearth of well-conducted studies on vaginal cuff dehiscence after hysterectomy in Korea.
Materials and methods
We retrospectively analyzed medical reviews of 604 women who underwent hysterectomies at Korea University Anam Hospital in the period of June 2007 until June 2011. Vaginal cuff dehiscence was defined as partial or total full thickness opening of the anterior and posterior edges of vaginal cuff without protruding bowels. Vaginal cuff evisceration was defined as separation with protruding bowel [2].
Data extracted from the medical record included patient's age, body mass index (BMI), obstetrical history and indication for surgery. Operative reports were reviewed and operative times, estimated blood loss (EBL) and techniques of vaginal cuff closure were recorded. EBL was estimated by the gap between the amount of the fluid suctioned and that used on irrigation in laparoscopic or robotic surgery. In the cases of laparotomy, we counted the number of used gauzes to calculate the EBL. Postoperative records were also reviewed. These included postoperative fever, period of hospitalization, transfusion, hemoglobin (Hb), white blood cell (WBC), erythrocyte sedimentation rate, C-reactive protein, use of antibiotics and post-op complications other than VCDE. We also collected additional data from those who developed VCDE including history of operation, stage, lympho-vascular invasion and resection margin.
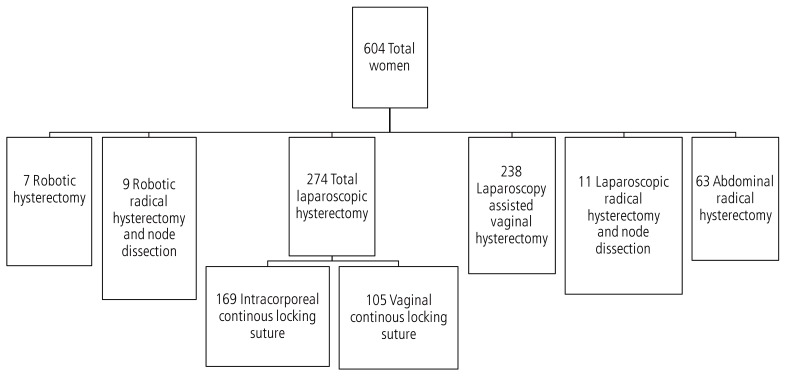
The main details considered for the analysis were surgical methods and suture techniques. A total of 604 women were allocated to six groups. The six types of hysterectomies included robotic hysterectomy (n=7), robotic radical hysterectomy and node dissection (RRHND, n=9), TLH (n=274), laparoscopy assisted vaginal hysterectomy (LAVH, n=238), laparoscopic radical hysterectomy and node dissection (LRHND, n=11), and abdominal radical hysterectomy (ARH, n=63) (Fig. 1). The da Vinci Surgical System has been used for robotic hysterectomy at our institution.
Fig. 1.
Flowchart of the trial population.
Three subcategories of laparoscopic hysterectomy (LH) have been described [11]. In LAVH, the procedure is done partially with laparoscopy and partly vaginally, but the laparoscopic component does not involve uterine vessel ligation. In uterine vessel ligation LH, although the uterine vessels are ligated with laparoscopy, part of the operation is donevaginally. In our study, including node dissection, LH is subclassified as LRHND. In TLH, the entire operation (including suture of the vaginal vault) is performed with laparoscopy.
In patients undergoing TLH, two methods for vaginal cuff closure were used, either intracorporeal continuous suture 169 (61%) or vaginal continuous locking suture 105 (38%) according to the single surgeon's decision (Fig. 1). Only intracorporeal continuous suture was performed in robotic surgery, while vaginal continuous suture was performed in LAVH. Five-point suture with figure of eight was performed in total abdominal hysterectomy. Subanalysis included age, BMI, operation time, parity, EBL, postoperative fever, and use of postoperative antibiotics.
Data were analyzed using SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA), with a significance set at P<0.05. Comparisons of baseline characteristics between groups were drawn using ANOVA test. Two different vaginal cuff suture techniques used in hysterectomy were compared with two tailed chi-square test. Associations between categorical variables and VCDE were determined using Kruskal-Wallis test.
Results
The baseline characteristics were shown in Table 1. Age, BMI, parity, operation time, EBL, hospitalized days, initial serum Hb and WBC level were compared between 6 different groups according to the operation type. There was some heterogeneity between groups in age, parity, operation time, EBL, hospitalized days (P-value was shown in Table 1). BMI, initial serum Hb and WBC were not significantly different between groups (P = 0.38, P = 0.36, P = 0.24, respectively).
Table 1.
Baseline characteristics of all participants according to operation types
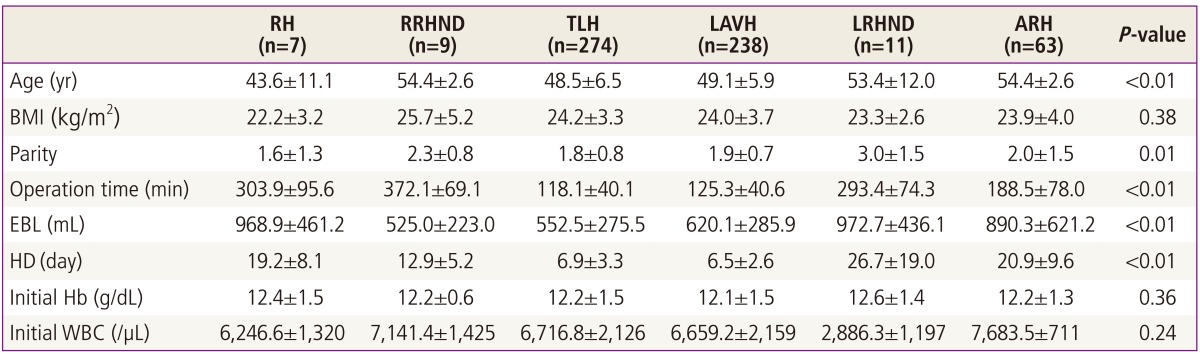
Values are presented as mean±standard deviation except P-values.
RH, robotic hysterectomy; RRHND, robotic radical hysterectomy and node dissection; TLH, total laparoscopic hysterectomy; LAVH, laparoscopy assisted vaginal hysterectomy; LRHND, laparoscopic radical hysterectomy and node dissection; ARH, abdominal radical hysterectomy; BMI, body mass index; EBL, estimated blood loss; HD, hospitalized days; Hb, hemoglobin; WBC, white blood cell.
In total of 604 hysterectomies, 3 eviscerations (0.49%) and 21 dehiscences (3.47%) occurred. Eviscerations were found in RRHND (1/9, 11.1%), TLH (1/274, 0.36%), and ARH (1/64, 1.56%). Dehiscences occurred in TLH (15/274, 5.43%), LAVH (4/238, 1.68%), and ARH (2/63, 3.17%) (Table 2). We analyzed patient and surgical characteristics of vaginal cuff dehiscence with or without evisceration by mode of hysterectomy (Tables 3, 4).
Table 2.
Incidence of vaginal cuff complications by mode of hysterectomy
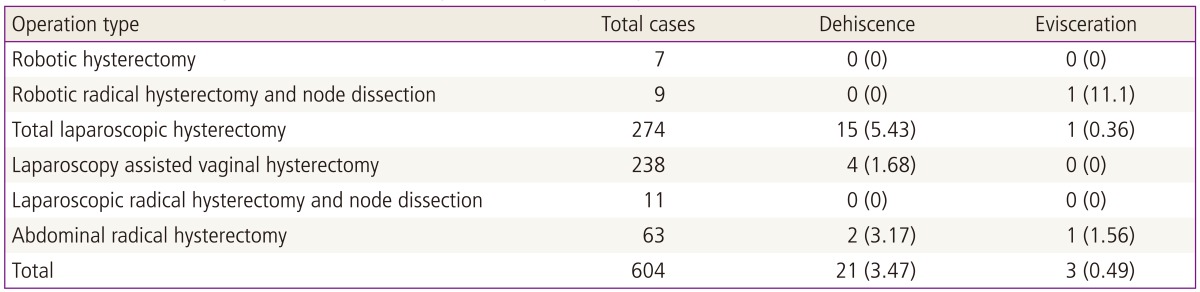
Values are presented as number or number (%).
Table 3.
Clinical data of the patients complicated by vaginal cuff problems
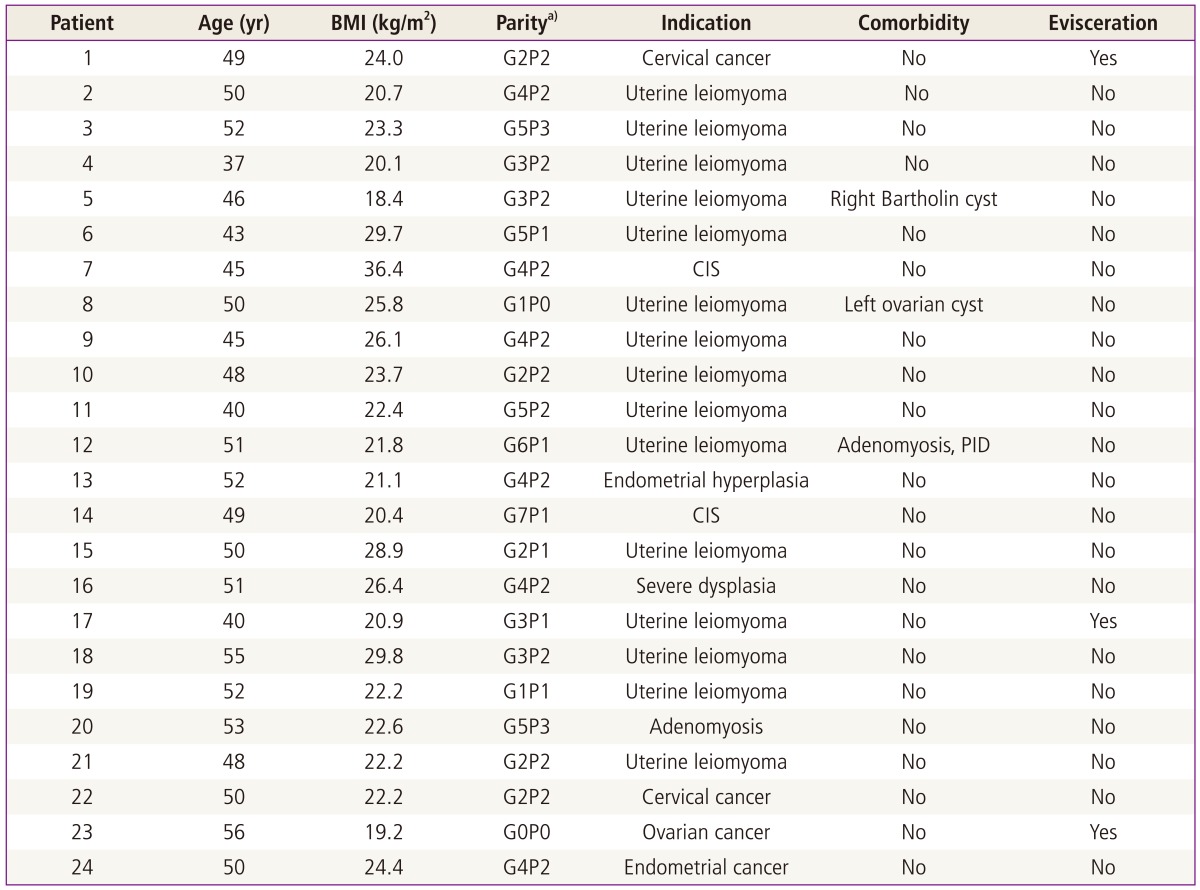
BMI, body mass index; CIS, squamous cell carcinoma in situ of cervix; PID, pelvic inflammatory disease.
a)Parity was shown with G (gravida) and P (para).
Table 4.
Surgical data of the patients complicated by vaginal cuff problems
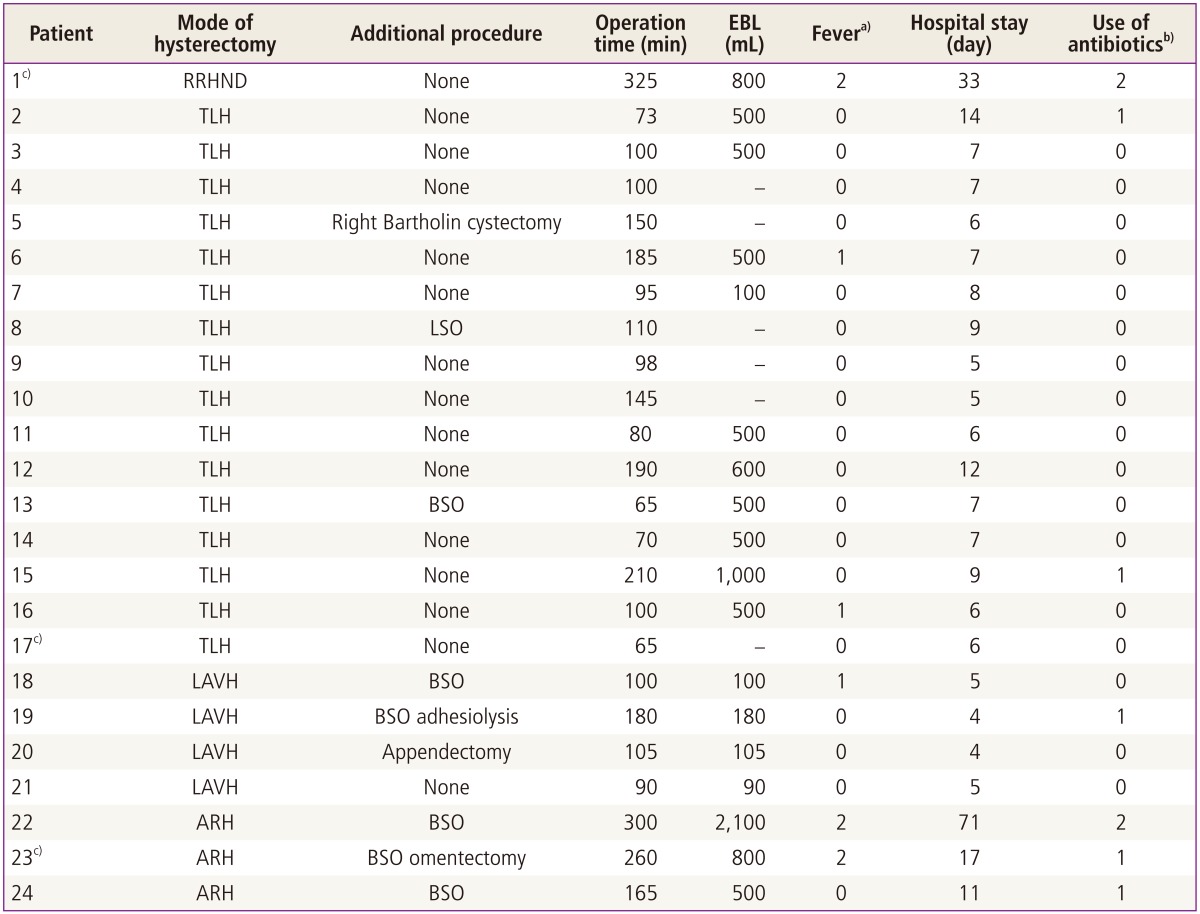
EBL, estimated blood loss; RRHND, robotic radical hysterectomy and node dissection; TLH, total laparoscopic hysterectomy; LSO, left salpingo-oophorectomy; BSO, bilateral salpingo-oophorectomy; LAVH, laparoscopy assisted vaginal hysterectomy; ARH, abdominal radical hysterectomy.
a)No fever (0), fever due to atelectasis (1), and fever due to other infectious condition (2); b)No use (0), use (1), and use after fever developed (2); c)Dehiscence with evisceration.
As a subgroup analysis, we compared the characteristics and VCDE occurrence rate between the TLH and LAVH groups. Age, BMI, parity, operation time, EBL, hospitalized days, initial serum Hb level, postoperation day-1 serum Hb level, initial serum WBC level, and post-operation day-1 WBC level were not significantly different between two groups. The VCDE occurrence rate was 5.79% in TLH group and 1.68% in LAVH group, and it was significantly higher in TLH group (P = 0.016).
In the cases of TLH, there was a significant difference in vaginal cuff problems depending on the suture method of vaginal cuff (Table 5). In 169 cases of TLH with intracorporeal continuous suture, 1 evisceration and 4 dehiscences (2.96%) occurred, whereas 11 dehiscences (10.47%) occurred in 105 TLH cases with vaginal continuous locking suture. Durations between the day of operation and VCDE in the cases of intra-corporeal suture and vaginal suture were 72.8 and 23.6 days respectively, and it took significantly longer time in intra-corporeal suture than in vaginal suture (P = 0.01).
Table 5.
Comparison of two different vaginal cuff suture techniques used in total laparoscopic hysterectomy
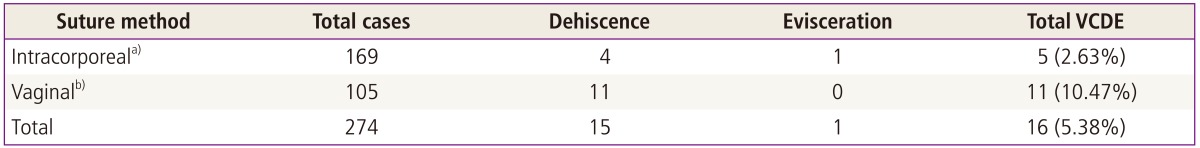
The intracorporeal continuous suture was superior than vaginal continuous locking suture in prevention of vaginal cuff complications (P=0.02).
VCDE, vaginal cuff dehiscence or evisceration.
a)Intracorporeal continuous suture; b)Vaginal approach continuous locking suture.
Subanalysis was performed to analyze the risk factors associated with VCDE, including age, BMI, operation time, EBL, postoperative fever, use of postoperative antibiotics, and none of these factors had correlation with VCDE (Table 6).
Table 6.
Evaluation of risk factors for vaginal cuff problems
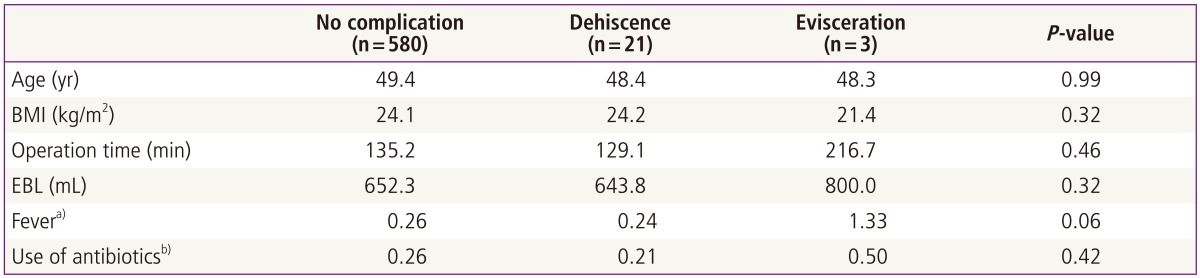
BMI, body mass index; EBL, estimated blood loss.
a)No fever (0), fever due to atelectasis (1), and fever due to other infectious condition (2); b)No use (0), use (1), and use after fever developed (2).
Discussion
Vaginal cuff dehiscence after hysterectomy is a rare, but potentially devastating complication. If it is not corrected in a rapid fashion, there is significant potential for morbidity and mortality. The incidence of this condition is not clear, ranging in the literature between 0% and 7.5% [12]. A review of records from 1970 to 2001 at the Mayo Clinic Rochester revealed a low incidence (0.032%) of vaginal evisceration after pelvic operation via abdominal and vaginal approach [13]. At a single, large, referral institution, TLH was associated with an increased incidence of vaginal cuff dehiscence compared with other approaches (4.93% compared with 0.29% total vaginal hysterectomy, and 0.12% total abdominal hysterectomy) [5]. In 2006, Iaco et al. [6] published a 0.28% incidence of evisceration after 3,593 hysterectomies. Although a greater rate of evisceration after laparoscopic hysterectomies was reported (0.26% abdominal, 0.25% vaginal, and 0.79% laparoscopic), the authors concluded that route of surgery does not influence risk of dehiscence because the difference was not statistically significant. In this study, the overall incidence of dehiscence without and with evisceration was 3.47% and 0.49% respectively. The overall incidence is low, but not negligible; therefore, the diagnosis and therapy of this post-hysterectomy complication must be kept in mind. However, it should be noted that this study is limited by the small number of robotic hysterectomies and only three vaginal evisceration was reported among RRHND, TLH, and ARH together (one case by each). In subgroup analysis, the VCDE occurrence rate was significantly higher in TLH group than LAVH group. This is supported by several previous studies [4,5].
We also hypothesized that the vaginal cuff suture method could influence the occurrence of VCDE. In this study, there was a significant difference in vaginal cuff problems depending on the suture method of vaginal cuff. Intracorporeal continuous suture was superior to vaginal approach continuous locking suture in TLH performed in our institution. This result could be regarded ironic because of the higher VCDE incidence in TLH than in LAVH, in which the vaginal cuff is almost always closed by vaginal suture. But the cut surface of vaginal cuff is not similar between two surgeries. In LAVH, the cut level of vaginal cuff is very close to cervix, so the cut surface is curved toward inside the vagina. However, in TLH, the cuff is mostly made at the level of vesico-vaginal junction and recto-vaginal junction, and the vaginal cuff is not so curved as in LAVH. In this point of view, the anterior and posterior cut surfaces of vaginal cuff would not attach properly with vaginal suture technique, because the closest layer between anterior and posterior surface is vaginal mucosa, not the pelvic serosa. Consequently, intracorporeal suture would give less tension to vaginal cuff than vaginal suture in cuff closure after TLH. However, Uccella et al. [8] reported that transvaginal colporrhaphy after TLH is associated with a reduction in risk of VCDE compared with laparoscopic suture, and Hwang et al. [14] found no difference between two groups. This heterogeneity between studies could be come from the difference of suture technique of the surgeons, or the development in suture materials may act as a bias. Thus, further study is needed about this correlation.
Besides surgical factors, some potential underlying patient-related risk factors are associated with VCDE incidence. Somkuti et al. [15] described 10 risk factors for apical vaginal rupture after an abdominal or vaginal hysterectomy: poor technique, postoperative infection, hematoma, coitus before healing, age, radiotherapy, corticosteroid therapy, trauma or rape, previous vaginoplasty, and use of the Valsalva maneuver. Furthermore the causes of vaginal cuff dehiscence and evisceration differ between premenopausal and postmenopausal women. Vaginal evisceration was associated with chronic pelvic prolapse, atrophic vaginal tissue associated with a sudden increase in abdominal pressure for postmenopausal women. In the elderly, the evisceration was usually a spontaneous event and happened quite late [16]. In young patients, sexual intercourse before complete healing of the vaginal cuff is considered the main trigger event. In this group of patients, the complication had an early onset [17]. Unfortunately, we did not collect data for several postoperative triggering events that could have had an impact on the incidence of vaginal dehiscence. Although our study was not designed to determine the causes of vaginal cuff dehiscence after hysterectomy this time, we hope to address this clinically important question with follow-up prospective studies.
We acknowledge limitations of the current study. First, a significant heterogeneity in cuff complication rates was found between studies, likely attributable to variation in sample size, patient selection. Second, in our study, we have missed data of total abdominal hysterectomy cases. We recognize that these missing data could potentially have had an influence on our results. Third, the retrospective nature of this study lacks the randomization of mode of hysterectomy. Last, the rarity of the event required a large study population to properly assess the actual complication rate after stratification for surgical approach, and such a large number of cases could only be achieved with a multicenter retrospective study.
Although there are some limitation in our recent study, this study has great significance in the aspect of comparing the incidence of vaginal cuff problems from different approaches to hysterectomy including minimally invasive surgery at the same time to assess which mode of hysterectomy poses a lesser risk for vaginal cuff problems and described the surgical and the patient characteristics of those with VCDE after hysterectomy to identify potential risk factors for this complication.
In conclusion, the incidence of vaginal cuff dehiscence and evisceration was significantly higher in TLH than LAVH. The intra-corporeal cuff suture was superior to the vaginal suture to prevent the vaginal cuff complications in TLH.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Ramirez PT, Klemer DP. Vaginal evisceration after hysterectomy: a literature review. Obstet Gynecol Surv. 2002;57:462–467. doi: 10.1097/00006254-200207000-00023. [DOI] [PubMed] [Google Scholar]
- 2.Kho RM, Akl MN, Cornella JL, Magtibay PM, Wechter ME, Magrina JF. Incidence and characteristics of patients with vaginal cuff dehiscence after robotic procedures. Obstet Gynecol. 2009;114(2 Pt 1):231–235. doi: 10.1097/AOG.0b013e3181af36e3. [DOI] [PubMed] [Google Scholar]
- 3.Ceccaroni M, Berretta R, Malzoni M, Scioscia M, Roviglione G, Spagnolo E, et al. Vaginal cuff dehiscence after hysterectomy: a multicenter retrospective study. Eur J Obstet Gynecol Reprod Biol. 2011;158:308–313. doi: 10.1016/j.ejogrb.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 4.Hur HC, Donnellan N, Mansuria S, Barber RE, Guido R, Lee T. Vaginal cuff dehiscence after different modes of hysterectomy. Obstet Gynecol. 2011;118:794–801. doi: 10.1097/AOG.0b013e31822f1c92. [DOI] [PubMed] [Google Scholar]
- 5.Hur HC, Guido RS, Mansuria SM, Hacker MR, Sanfilippo JS, Lee TT. Incidence and patient characteristics of vaginal cuff dehiscence after different modes of hysterectomies. J Minim Invasive Gynecol. 2007;14:311–317. doi: 10.1016/j.jmig.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Iaco PD, Ceccaroni M, Alboni C, Roset B, Sansovini M, D'Alessandro L, et al. Transvaginal evisceration after hysterectomy: is vaginal cuff closure associated with a reduced risk. Eur J Obstet Gynecol Reprod Biol. 2006;125:134–138. doi: 10.1016/j.ejogrb.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Kho RM, Hilger WS, Hentz JG, Magtibay PM, Magrina JF. Robotic hysterectomy: technique and initial outcomes. Am J Obstet Gynecol. 2007;197:113.e1–113.e4. doi: 10.1016/j.ajog.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 8.Uccella S, Ghezzi F, Mariani A, Cromi A, Bogani G, Serati M, et al. Vaginal cuff closure after minimally invasive hysterectomy: our experience and systematic review of the literature. Am J Obstet Gynecol. 2011;205:119.e1–119.e12. doi: 10.1016/j.ajog.2011.03.024. [DOI] [PubMed] [Google Scholar]
- 9.Nick AM, Lange J, Frumovitz M, Soliman PT, Schmeler KM, Schlumbrecht MP, et al. Rate of vaginal cuff separation following laparoscopic or robotic hysterectomy. Gynecol Oncol. 2011;120:47–51. doi: 10.1016/j.ygyno.2010.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeung IC, Baek JM, Park EK, Lee HN, Kim CJ, Park TC, et al. A prospective comparison of vaginal stump suturing techniques during total laparoscopic hysterectomy. Arch Gynecol Obstet. 2010;282:631–638. doi: 10.1007/s00404-009-1300-0. [DOI] [PubMed] [Google Scholar]
- 11.Reich H, Roberts L. Laparoscopic hysterectomy in current gynecological practice. Rev Gynaecol Pract. 2003;3:32–40. [Google Scholar]
- 12.DeNardis SA, Holloway RW, Bigsby GE, 4th, Pikaart DP, Ahmad S, Finkler NJ. Robotically assisted laparoscopic hysterectomy versus total abdominal hysterectomy and lymphadenectomy for endometrial cancer. Gynecol Oncol. 2008;111:412–417. doi: 10.1016/j.ygyno.2008.08.025. [DOI] [PubMed] [Google Scholar]
- 13.Croak AJ, Gebhart JB, Klingele CJ, Schroeder G, Lee RA, Podratz KC. Characteristics of patients with vaginal rupture and evisceration. Obstet Gynecol. 2004;103:572–576. doi: 10.1097/01.AOG.0000115507.26155.45. [DOI] [PubMed] [Google Scholar]
- 14.Hwang JH, Lee JK, Lee NW, Lee KW. Vaginal cuff closure: a comparison between the vaginal route and laparoscopic suture in patients undergoing total laparoscopic hysterectomy. Gynecol Obstet Invest. 2011;71:163–169. doi: 10.1159/000316052. [DOI] [PubMed] [Google Scholar]
- 15.Somkuti SG, Vieta PA, Daugherty JF, Hartley LW, Blackmon EB., Jr Transvaginal evisceration after hysterectomy in premenopausal women: a presentation of three cases. Am J Obstet Gynecol. 1994;171:567–568. doi: 10.1016/0002-9378(94)90306-9. [DOI] [PubMed] [Google Scholar]
- 16.Kowalski LD, Seski JC, Timmins PF, Kanbour AI, Kunschner AJ, Kanbour-Shakir A. Vaginal evisceration: presentation and management in postmenopausal women. J Am Coll Surg. 1996;183:225–229. [PubMed] [Google Scholar]
- 17.Alessandri F, Remorgida V, Venturini PL, Ferrero S. Unidirectional barbed suture versus continuous suture with intracorporeal knots in laparoscopic myomectomy: a randomized study. J Minim Invasive Gynecol. 2010;17:725–729. doi: 10.1016/j.jmig.2010.06.007. [DOI] [PubMed] [Google Scholar]