Abstract
Vulvar hematomas are uncommon outside of the obstetric population and may be the result of trauma to the perineum. Vulvar hematomas most often present with low abdominal pain and urologic and neurologic symptoms. The vulva has rich vascularization that is supplied by the pudendal artery, a branch of the anterior division of the internal iliac artery. We describe a rare case of a 15-cm-sized vulvar hematoma with the suggested rupture of a pseudoaneurysm of the left pudendal artery without trauma injury. A 14-year-old girl presented with sudden pain and swelling in her left labium and was successfully treated with selective arterial embolization and surgical evacuation. We provide a literature review and discuss patient treatment and management strategies.
Keywords: Aneurysm, false; Hematoma; Vulvar
Introduction
The vulva consists of elastin fibers, smooth muscle fibers, and connective tissue with many vessels, and is primarily supplied by the pudendal artery, a branch of the anterior division of the internal iliac artery that divides into the inferior rectal artery, posterior labial artery and transverse perineal branches [1].
Vulvar hematomas are uncommon; their reported incidence in obstetrics is 1 or 2 per 1,000 deliveries [2]. The vasculature commonly develops varicosities during pregnancy, especially in parous women, due to increased venous pressure created by the increasing weight of the uterus. Postpartum vulvar hematomas are most frequently accompanied by genital tract laceration. Non-obstetric genital hematomas constitute up to 0.8% of all gynecologic admissions [3], and may be the result of trauma to the perineum, such as straddle-type injuries, coitus, or physical assault. As vulvar tissue is crushed against the pelvic bone plane, it causes the vulva to be susceptible to frontal injuries with vascular lesions.
However, vulvar hematomas can rarely be caused by spontaneous injury to a blood vessel. The bleeding can be either arterial or venous in origin. Vessel ruptures result in various symptoms such as low abdomen pain and urologic and neurologic symptoms. This case report discusses a rare case of a 15-cm-sized vulvar hematoma with a suggested rupture of a pseudoaneurysm of the left pudendal artery without traumatic injury.
Case report
A 13-year-old female with gravida 0 and para 0 visited our emergency center and presented with sudden pain and swelling in the left labium. Her medical history included Rett syndrome and epilepsy, and she had used medication for this condition; however, the patient was not taking an anticoagulant medication upon admission. Because the patient was bedridden, a regular catheterization was performed by her mother to empty her bladder. A week before she presented in the emergency center, her parents found a 2×2-cm cystic mass on the left labium. Her pediatrician prescribed antibiotics and the mass size seemed to decrease daily with treatment. However, because the mass abruptly increased to 15×15 cm, her parents took her to the hospital.
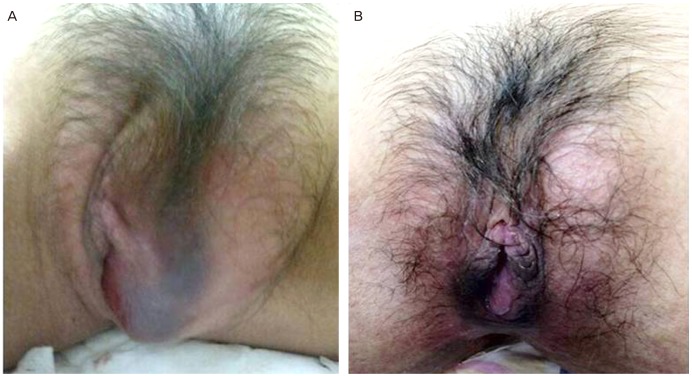
The patient was alert and anxious. Her vital signs were recorded and her blood pressure was 120/76 mmHg, heart rate was 132 beats per minute, respiratory rate was 32 breaths per minute, and temperature was 37.3℃. Palpation of her perineum revealed that the patient had severe tenderness in this area. A genital examination revealed that there was a tense, 15×7-cm hematoma of the left labia majora that significantly distorted the anatomy, along with redness but no laceration (Fig. 1). There was no history of sexual assault or trauma, especially related to catheterization. Laboratory analysis indicated that the patient had a hemoglobin level of 13.3 g/dL (reference range, 12-16 g/dL), a hematocrit of 41.9% (reference range, 36%-48%), a platelet count of 28.5×104/µL (reference range, 13-40×104/µL), and an international normalized ratio of 1.08 (reference range, 1.00-1.10).
Fig. 1.
Significantly distorted anatomy due to left vulvar hematoma (A). After resolution of hematoma (B).
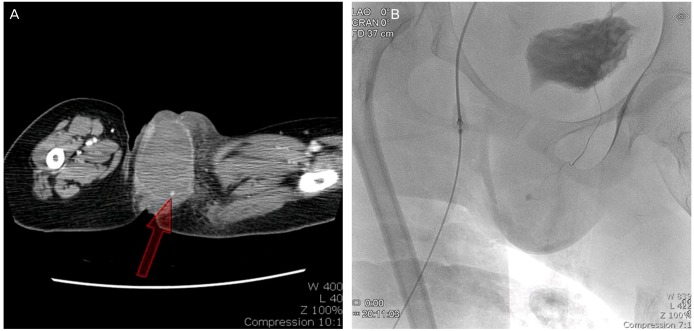
Computed tomography of the pelvis with angiography showed marked dilatation of the vagina (7.0×4.8 cm in size) and left vulvar area (7.5×4.4 cm, red arrow) (Fig. 2) and an abnormal, round high density in the left vulvar area, which was suspected to be a pseudoaneurysm. The radiologist confirmed extravasation of blood and active bleeding in the lower vagina and left anterior vulvar area. After evaluation and during urinary catheterization, the hematoma was opened. About 400 mL of bloody discharge was drained. The hemoglobin level dropped to 8.5 g/dL and the patient was given a transfusion of 3 units of packed red blood cells. Angiography subsequently confirmed the existence of a small pseudoaneurysm, and a branch of the internal pudendal artery and embolization were successfully adhered with a 1:5 mixture of lipidol (Fig. 2).
Fig. 2.
Computed tomography shows the hematoma on left vulvar area (red arrow) (A). Angiography confirmed rupture of internal pudendal artery (B).
There was no indication of further vulvar bleeding after embolization, but the hematoma was still present and we therefore opted for evacuation as treatment. Under local anesthesia, the hematoma was evacuated and no vessels were ligated. No further bleeding was noted after this procedure. During the first postoperative day, her vital signs were stable, and the hematoma resolved on the second day. She was discharged from the hospital on the fourth postoperative day.
Discussion
Vulvar hematoma caused by non-obstetric injuries is uncommon (incidence 3.7%) [4]. Although trauma is the major preceding cause, spontaneous vessel rupture is considered in the absence of evidence at examination.
Spontaneous rupture of the pudendal artery can occur exclusively at the site of an aneurysm and is generally related to atherosclerosis. Infection or connective tissue disease is rarely identified, but can occasionally cause aneurysms. The pudendal artery passes through the greater sciatic foramen and enters the ischioanal fossa through the external genitalia and perineum. Extension of a hematoma in this area is limited by the Colles fascia and the urogenital diaphragm, and is therefore directed toward the skin [5].
In this case, the patient did not present with symptoms due to her underlying condition, but common symptoms of internal iliac artery rupture include abdominal and groin pain as well as neurologic and urologic symptoms. In addition, the patient can be hemodynamically unstable and fluid replacement and blood transfusion may thus be necessary.
The management of vulvar hematoma remains controversial. However, imaging modality improvement has increased image clarity and allowed defined diagnoses based on imaging findings. Ultrasound, computed tomography, or magnetic resonance imaging may be appropriate for future studies to investigate the size, site, and expansion of the hematoma. Sherer et al. [6] described perineal sonography, which offers objective imaging assessment of the extent of vulvar hematoma at the bedside and negates the need for complex and more expensive imaging modalities. Butori et al. [7] proposed that computed tomography should be used as the principal diagnostic imaging modality because it is more specific in diagnosing aneurysms. Additionally, magnetic resonance imaging can provide a more detailed mapping of the lesion and exclude any retroperitoneal involvement [8].
The majority of vulvar hematomas are conservatively managed and usually progress satisfactorily with minimal treatment measures. However, large hematomas (>12 cm) accompanied by progressive expansion, decreased hematocrit, hemodynamic disorders, and the need for transfusion are more controversial. Currently, there is no established consensus regarding the optimal timing of an intervention. However, study reports have agreed that if the hematoma is large enough to cause urologic and neurologic symptoms or is expanding, then intervention is required immediately.
Blood clot evacuation and ligation of bleeding points with surgery may be performed to prevent pressure necrosis and infection. Brown et al. [9] first described uterine artery embolization to manage postpartum bleeding in 1979, and advanced selective angiography embolization can be used as an effective alternative to surgery for hemorrhage. In the past few years, this approach has been demonstrated to be a successful method for controlling intractable hemorrhage. Additionally, this approach has been used in obstetrics and gynecology to treat neoplastic disease of the genital tract, trauma to the pelvis, postpartum hemorrhage, and bleeding from an unknown origin without causing complications.
The vascular supply to the pelvic organs is characterized by a massive collateral blood supply that prevents necrosis of the organs after selective embolization of the feeding vessel [10]. Selective embolization can be performed in carefully selected patients, and can have more advantageous outcomes for these patients than surgery. Future comparison of the two methods should be conducted in a large or randomized trial and further study is necessary to determine the best interventional options for patients.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Palacios Jaraquemada JM, Garcia Monaco R, Barbosa NE, Ferle L, Iriarte H, Conesa HA. Lower uterine blood supply: extrauterine anastomotic system and its application in surgical devascularization techniques. Acta Obstet Gynecol Scand. 2007;86:228–234. doi: 10.1080/00016340601089875. [DOI] [PubMed] [Google Scholar]
- 2.Villella J, Garry D, Levine G, Glanz S, Figueroa R, Maulik D. Postpartum angiographic embolization for vulvovaginal hematoma: a report of two cases. J Reprod Med. 2001;46:65–67. [PubMed] [Google Scholar]
- 3.Rabinerson D, Fradin Z, Zeidman A, Horowitz E. Vulvar hematoma after cunnilingus in a teenager with essential thrombocythemia: a case report. J Reprod Med. 2007;52:458–459. [PubMed] [Google Scholar]
- 4.Jones IS, O'Connor A. Non-obstetric vulval trauma. Emerg Med Australas. 2013;25:36–39. doi: 10.1111/1742-6723.12016. [DOI] [PubMed] [Google Scholar]
- 5.Egan E, Dundee P, Lawrentschuk N. Vulvar hematoma secondary to spontaneous rupture of the internal iliac artery: clinical review. Am J Obstet Gynecol. 2009;200:e17–e18. doi: 10.1016/j.ajog.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 6.Sherer DM, Stimphil R, Hellmann M, Abdelmalek E, Zinn H, Abulafia O. Transperineal sonography of a large vulvar hematoma following blunt perineal trauma. J Clin Ultrasound. 2006;34:309–312. doi: 10.1002/jcu.20188. [DOI] [PubMed] [Google Scholar]
- 7.Butori N, Coulange L, Filipuzzi L, Krause D, Loffroy R. Pseudoaneurysm of the uterine artery after cesarean delivery: management with superselective arterial embolization. Obstet Gynecol. 2009;113:540–543. doi: 10.1097/AOG.0b013e318190a43a. [DOI] [PubMed] [Google Scholar]
- 8.Guerriero S, Ajossa S, Bargellini R, Amucano G, Marongiu D, Melis GB. Puerperal vulvovaginal hematoma: sonographic findings with MRI correlation. J Clin Ultrasound. 2004;32:415–418. doi: 10.1002/jcu.20053. [DOI] [PubMed] [Google Scholar]
- 9.Brown BJ, Heaston DK, Poulson AM, Gabert HA, Mineau DE, Miller FJ., Jr Uncontrollable postpartum bleeding: a new approach to hemostasis through angiographic arterial embolization. Obstet Gynecol. 1979;54:361–365. [PubMed] [Google Scholar]
- 10.Dehaeck CM. Transcatheter embolization of pelvic vessels to stop intractable hemorrhage. Gynecol Oncol. 1986;24:9–16. doi: 10.1016/0090-8258(86)90002-8. [DOI] [PubMed] [Google Scholar]