ABSTRACT
BACKGROUND
We evaluated the effectiveness and cost-effectiveness of alternative interventions designed to promote mammography in safety-net settings.
METHODS
A three-arm, quasi-experimental evaluation was conducted among eight federally qualified health clinics in predominately rural Louisiana. Mammography screening efforts included: 1) enhanced care, 2) health literacy-informed education of patients, and 3) education plus nurse support. Outcomes included mammography screening completion within 6 months and incremental cost-effectiveness.
RESULTS
Overall, 1,181 female patients ages 40 and over who were eligible for routine mammography were recruited. Baseline screening rates were < 10 %. Post intervention screening rates were 55.7 % with enhanced care, 51.8 % with health literacy-informed education and 65.8 % with education and nurse support. After adjusting for race, marital status, self-efficacy and literacy, patients receiving health-literacy informed education were not more likely to complete mammographic screening than those receiving enhanced care; those additionally receiving nurse support were 1.37-fold more likely to complete mammographic screening than those receiving the brief education (95 % Confidence Interval 1.08–1.74, p = 0.01). The incremental cost per additional women screened was $2,457 for literacy-informed education with nurse support over literacy-informed education alone.
CONCLUSIONS
Mammography rates were increased substantially over existing baseline rates in all three arms with the educational initiative, with nurse support and follow-up being the most effective option. However, it is not likely to be cost-effective or affordable in resource-limited clinics.
KEY WORDS: cancer screening, mammography, community clinics, health literacy, underserved populations
INTRODUCTION
Breast cancer screening in safety-net settings remains underutilized in the United States. Breast cancer is the second leading cause of cancer-related death among women in the United States.1 National efforts to reduce breast cancer-related mortality have emphasized early detection through mammography.1 While mammography rates have increased dramatically over the last 30 years, they remain persistently lower among disadvantaged populations, including low-income women, those with no health insurance, lower health literacy,2,3 fewer years of education, and racial/ethnic minorities.4–15 Reducing these disparities in mammography screening is a national public health priority.16
Numerous studies have identified patient and system barriers that impact breast cancer screening rates among disadvantaged populations. These include: poorer knowledge about screening, fear of finding cancer, lack of motivation, embarrassment, inadequate transportation, lack of health insurance, lack of physician screening recommendation, and poor availability of screening facilities.1,5,17–27 Limited health literacy is another barrier that has been linked to lower levels of breast cancer knowledge, attitudes on breast cancer screening, understanding of screening benefits, lower self-efficacy and a lesser likelihood of completing screening mammography.2,3,13,27–29 To help address this problem, the Department of Health and Human Services “National Action Plan to Improve Health Literacy” 30 has called for the development and dissemination of health information and services that are accurate, accessible, understandable and actionable. However, few health literacy interventions have evaluated mammography in safety net settings.31
Our team developed and evaluated an intervention for a population at higher risk for not undergoing mammography: patients cared for in rural and inner-city Federally Qualified Health Centers (FQHCs). FQHCs are government-supported clinics that are required to provide services to patients regardless of insurance status. Strategically located in areas designated as medically underserved, FQHCS provide care to over 20 million individuals in the U.S.32 Identifying practices that can improve mammography rates in community clinics disproportionately caring for vulnerable populations has the potential to advance public health preventive practices and potentially reduce screening disparities among disproportionately affected groups.
The purpose of this quasi-experimental study was to evaluate the effectiveness and cost-effectiveness of three alternative strategies designed to improve mammography screening rates: 1) enhanced care that provided assurance that patients received a screening recommendation and had access to mammography; 2) the use of literacy-informed educational materials with accompanying ‘teach back’ to confirm comprehension; 33 or 3) utilization of this education strategy with support and follow-up by a nurse. Given the resource-constrained FQHCs environment, we evaluated not only the effectiveness of our interventions, but also cost-effectiveness of the interventions.
METHODS
Study Design and Sample
A three-arm, quasi-experimental (i.e. based on randomization of sites, but not patients within sites) comparative effectiveness evaluation was conducted among three Louisiana FQHC networks between May 2008 and August 2011. Louisiana ranks third among states in breast cancer death rates.34
The study team determined that randomizing patients within an FQHC network was not an optimal study design, as was case in our prior studies of screening for colorectal cancer,35,36 because of the diffuse nature of interventions and concern of contamination among patients who belonged in a network FQHC that shared providers and staff. The target population was the five FQHC networks in predominantly rural north Louisiana. Three networks participated in this study; the other two were involved in cancer screening programs. The study statistician used computer-generated random numbers to allocate each network to an arm. Each participating FQHC parent network was affiliated with multiple clinics, which were assigned to the same study arm as their parent network. This resulted in two clinics in the enhanced care arm, two in the education arm, and three in the nurse support arm. After the first year of the study, one additional clinic was enrolled in the enhanced care arm due to limited patient recruitment in this arm. The three parent networks each served between 1,162 and 2,386 female patients aged 40 and over.
The eight study clinics were located in eight towns in seven parishes across the state. Six clinics were located in rural towns, with populations ranging from 450 to 13,000; and two clinics were in low-income areas of cities with populations of 63,000 and 199,000, respectively. Clinic personnel included on average one to two physicians, two nurse practitioners, one registered nurse, and one to three licensed practical nurses (LPNs), a medical technician and a receptionist. Baseline rates of screening mammograms at each clinic ranged from 5 to 9 %.
Due to ethical concerns and to ensure all patients had access to mammography, the grant provided free mammograms to those without insurance. The parent FQHCs were randomized to one of three arms: 1) enhanced care; 2) a literacy informed educational intervention; or 3) nurse support.
Participants
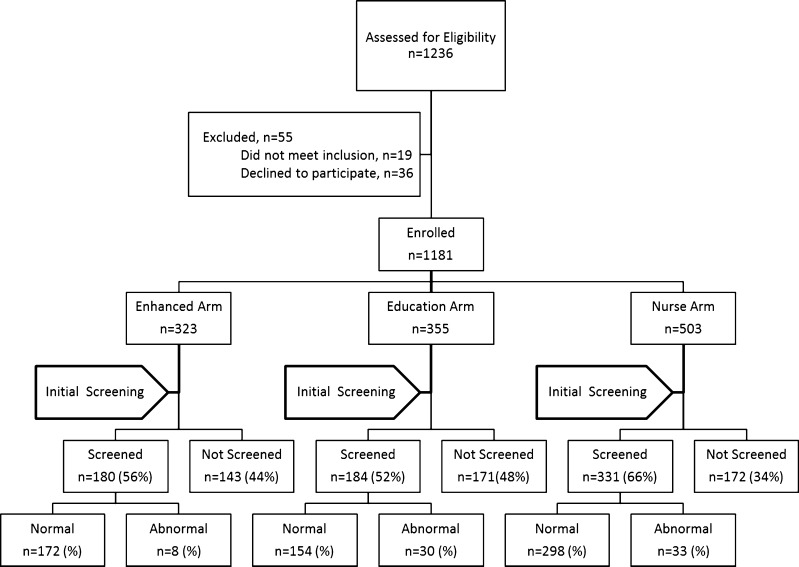
Patients were recruited through a multi-step process. First, while taking patient vital signs, a medical assistant at each clinic identified potentially eligible female patients by age (≥ 40 years old) and asked if they would be willing to talk to a research assistant (RA) on site about participating in a cancer screening study prior to their physician encounter. Those interested met with the RA, who screened them for further eligibility: 1) English-speaking, 2) current clinic patient, 3) not requiring screening at an earlier age according to American Cancer Society (ACS) guidelines,1 4) not up-to-date with United States Preventive Services Task Force 37 screening mammography recommendations (i.e. mammogram every other year), and 5) not having an acute medical concern. In all, 1,236 patients were identified, 36 (3 %) refused to participate and 19 (2 %) were found to be ineligible (see Fig. 1). This left 1,181 enrolled patients with a determined cooperation rate of 96 %. All patients were consented prior to data collection. The Louisiana State University Health Sciences Center–Shreveport Institutional Review Board approved the study. Each patient received $10 for their participation in the baseline survey.
Figure 1.
Flowchart of initial screening.
Structured Survey
The study interview included demographic, breast cancer and screening mammography items from validated questionnaires38 used previously by the authors and conceptually guided by the Health Belief Model (HBM)39–42 and Social Cognitive Theory (SCT).41,42 A detailed description of the survey, which was written on a fourth-grade level and administered orally, has been reported previously.43 Literacy was assessed using the Rapid Estimate of Adult Literacy in Medicine (REALM).44 The REALM is highly correlated with the Test of Functional Health Literacy in Adults (TOFHLA), and is an indicator of functional health literacy. Raw REALM scores (0–66) can be converted into reading grade levels that correlate with literacy skills. Raw scores of ≤ 60 indicate a reading grade level of eighth grade or below, or limited literacy; scores > 61 indicate at least a ninth-grade reading level or adequate literacy.
Clinic In-Service and Training of Research Assistants and Nurses
Staff and providers in each clinic attended a 2-hour in-service on mammography screening guidelines and an orientation to the study during a quarterly clinic meeting. RA training in the enhanced care arm included practice interviewing patients and administrating the survey and literacy test. Each clinic RA (who was a part-time clinic staff member) was given a script for recommending screening. For the educational strategy, RAs were given additional training in using health literacy techniques.32,33 For the nurse support arm, the nurse training also included motivational interviewing techniques,45 use of a tracking system, and a protocol for contacting patients and assisting them with navigation if a test was positive.
The Three Study Arms
Enhanced Care Arm
At enrollment, after completing the structured interview, the RA gave patients a recommendation to get a mammogram, and suggested they talk with their primary care provider about screening during their visit that day. Before patients left the clinic, the clinic nurse scheduled the mammograms at the closest community hospital with which the clinic had a contract, or the closest state public hospital. Mammography was provided at no cost to those who lacked adequate insurance. Regular clinic protocol was followed for abnormal mammogram results and if there was a need for diagnostic testing.
Health-Literacy Informed Education Arm
At enrollment, after completing the structure interview, the RA followed the enhanced care protocol and additionally provided brief education using health literacy best practices, such as using plain language and teach back to confirm understanding.29,37 As in the enhanced care arm, the clinic nurse scheduled mammograms before patients left the clinic. The education included the RA using a pamphlet and brief video as teaching tools. The materials were created by the authors, a video production team, and input from focus groups of FQHC patients and clinic providers. The video captured actual FQHC patients discussing barriers and facilitators to screening. It showed women encouraging each other to get screened, a physician recommending screening, and one woman getting a mammogram. The pamphlet, written on a fifth-grade level, highlighted risk factors for breast cancer, benefits of regular mammography and a brief explanation and illustration of the test. It included culturally appropriate pictures, text and testimonials to convey empowering messages to encourage mammography. Iterative cognitive interviews of FQHC patients ensured appeal and cultural and literacy appropriateness of the text and pictures.
Both materials incorporated evidence-based practices for the design of multimedia tools, guided by the theory of health learning capacity.46 The Health Belief Model and Social Cognitive Theory guided the inclusion and framing of content to address the salience of mammogram screening and the need to take action.41,42 The strategies were targeted at overcoming patient barriers to mammography, such as access to tests, limited knowledge, negative beliefs, poor self-efficacy and lack of motivation.5,17–27 Regular clinic protocol was followed for abnormal mammogram results.
Nurse Support Arm
At enrollment after the structured interview by the RA, the registered nurse gave participants the educational intervention, brief counseling and a screening recommendation, and the suggestion to talk to their primary care provider about screening. This nurse scheduled the mammogram, and followed up with patients to remind them of their mammogram appointment and ensure that they knew how to locate the clinic. This strategy was designed to extend the educational intervention by adding an ongoing supportive relationship and follow-up reminder calls to help identify and problem-solve barriers and motivate patients to complete mammography. If the patient missed her appointment, the nurse called to reschedule. If the patient had obtained the mammogram, the nurse entered the results in the tracking system and clinic chart. If results were negative, the nurse sent a letter informing patients that their mammogram was normal. If results were positive, the nurse called the patient to discuss results and facilitate scheduling of an appointment for a diagnostic mammogram.
Outcomes
Eligible patient mammogram completion at six months post enrollment was the primary outcome measure, as documented by the clinic nurse (enhanced care and education arms) or the nurse (nurse support arm) when mammography results were returned to the clinic.
Statistical Analysis
Mammography completion rates were defined as the percentage of mammogram results returned to the clinic. To examine whether patients in the study arms differed on baseline age and the self-efficacy and barrier indices, analysis of variance was used. Chi-square tests were performed to compare categorical factors across study arms. Screening ratios were defined as the ratio of mammogram completion rates between two groups. Screening ratios and pairwise tests for mammogram were calculated using logistic regression, which accounted for clustering by clinic. Factors found to be significantly different between arms (race, marital status, literacy level, self-efficacy) were included in a multivariate analysis.
Cost and Cost Effectiveness Analysis
Cost data were collected from purchase orders, receipts, and questioning research staff. Incremental costs and additional number of persons screened were calculated for the education arm over the enhanced care arm. Costs included a video ($5,000), pamphlets ($2,000) and research assistant ($1,098). Costs for the nurse arm over the education arm included 65 % of two registered nurses ($172,705). Comparison arm costs and number screened were normalized to the reference arm to account for differences in sample size. The incremental cost effectiveness (ICER) was calculated as the total incremental cost of a comparison arm relative to the reference arm divided by the total number of additional persons screened, as was done in our prior studies of cost-effectiveness of cancer screening interventions.36
RESULTS
Baseline participant characteristics, stratified by study arm, are presented in Table 1. While almost all (88 %) reported seeing a doctor in the past 12 months, none reported receiving a mammogram in the last 2 years, despite a high reported recommendation rate (82 %) and screening history (77 %). There were significant differences across groups for race/ethnicity, marital status, and literacy.
Table 1.
Characteristics of Study Sample at Baseline, Stratified by Study Arm
| Characteristic | All patients (n = 1181) | Study arm | p value | ||
|---|---|---|---|---|---|
| Enhanced care (n = 323) | Education (n = 355) | Nurse (n = 503) | |||
| Age, mean (sd) | 53.3 (9.0) | 53.2 (8.9) | 52.9 (8.1) | 53.7 (9.5) | 0.66 |
| Self-Efficacy Index*, mean (sd) | 28.2 (2.4) | 27.8 (2.5) | 29.0 (2.7) | 27.8 (1.9) | 0.007 |
| Barrier Index*, MEAN (sd) | 14.3 (3.0) | 14.4 (3.1) | 14.4 (3.2) | 14.1 (2.8) | 0.60 |
| N (%) | N (%) | N (%) | N (%) | ||
| Age categories | |||||
| 40–49 | 437 (37) | 113 (35) | 131 (37) | 193 (38) | 0.44 |
| 50–59 | 475 (40) | 143 (44) | 146 (41) | 186 (37) | |
| 60–69 | 203 (17) | 50 (15) | 65 (18) | 88 (17) | |
| 70+ | 66 (6) | 17 (5) | 13 (4) | 36 (7) | |
| Years of education | |||||
| Less than high school | 346 (29) | 103 (32) | 107 (30) | 136 (27) | 0.22 |
| High school grad | 544 (46) | 135 (42) | 175 (49) | 234 (46) | |
| Some college | 214 (18) | 62 (19) | 54 (15) | 98 (19) | |
| ≥ College graduate | 77 (7) | 23 (7) | 19 (5) | 35 (7) | |
| Race | |||||
| African-American | 766 (65) | 208 (64) | 164 (46) | 394 (78) | < 0.001 |
| Caucasian/Hispanic | 416 (35) | 115 (36) | 191 (54) | 109 (22) | |
| Marital status | |||||
| Single | 370 (31) | 85 (26) | 87 (24) | 198 (39) | 0.04 |
| Married | 369 (31) | 106 (33) | 145 (41) | 118 (23) | |
| Separated | 93 (8) | 29 (9) | 29 (8) | 35 (7) | |
| Divorced | 207 (18) | 54 (17) | 63 (18) | 90 (18) | |
| Widowed | 142 (12) | 49 (15) | 31 (9) | 62 (12) | |
| Marital status | |||||
| Married | 369 (31) | 106 (33) | 145 (41) | 118 (23) | < 0.001 |
| Not married | 812 (69) | 217 (67) | 210 (59) | 385 (77) | |
| Literacy level | |||||
| Limited: < 9th grade | 536 (45) | 173 (54) | 105 (30) | 258 (51) | 0.01 |
| Adequate: ≥ 9th grade | 645 (55) | 150 (46) | 250 (70) | 245 (49) | |
| Seen doctor in past 12 months | 1041 (88) | 284 (88) | 322 (91) | 435 (86) | 0.13 |
| Prior recommendation | 922 (82) | 249 (80) | 307 (86) | 366 (80) | 0.40 |
| Ever had a mammogram | 850 (77) | 233 (75) | 260 (73) | 357 (78) | 0.34 |
| Want to know if had cancer | 1034 (92) | 288 (93) | 326 (92) | 420 (92) | 0.77 |
*The Self-Efficacy Index ranges from 17 to 35, where low numbers mean low self-efficacy and high numbers mean high self-efficacy. The Barrier Index ranges from 6 to 26, where low numbers indicate a low barrier level to obtaining a mammogram and high numbers indicate a high barrier level
The overall mammogram completion rate was 59.9 %, 55.7 % in the enhanced care arm, 51.8 % in the education arm and 65.8 % in the nurse support arm (p = 0.037). Adjusting for race, marital status, literacy and self-efficacy, participants in the education arm were 0.87 times more likely to be screened (95 % CI 0.62–1.22, p = 0.42) compared to participants in the enhanced care arm (Table 2). Those in the nurse support arm were 1.19 times more likely to be screened (95 % CI 0.85–1.65, p = 0.31) compared to those in the enhanced care arm and 1.37 times more likely to be screened (95 % CI 1.08–1.74, p < 0.0001) compared to those in the education arm.
Table 2.
Primary Outcome Measure—Mammogram (Screened) Within 12 Months
| Study arm | |||||
|---|---|---|---|---|---|
| All patients (n = 1181) | Enhanced care (n = 323) | Education (n = 355) | Nurse (n = 503) | p value | |
| N (%) | N (%) | N (%) | N (%) | ||
| Mammogram (screened) | 695 (59.9) | 180 (55.7) | 184 (51.8) | 331 (65.8) | 0.037 |
| No mammogram | 486 (41.1) | 143 (44.3) | 171 (48.2) | 172 (34.2) | |
| Screening ratio | 1.00 | 0.87 | 1.19 | ||
| 95 % Confidence Interval | (0.62–1.22) | (0.85–1.65) | |||
| p value | 0.42 | 0.31 | |||
| Screening ratio | – | 1.00 | 1.37 | ||
| 95 % Confidence Interval | (1.08–1.74) | ||||
| p value | 0.01 | ||||
Multivariate analyses controlling for race (African American vs. Caucasian and Hispanic), marital status (married vs. not married), literacy (two categories) and self-efficacy
Table 3 presents the differences in mammography completion rates among study arms for each of the two literacy groups. There were significant differences across arms for the adequate literacy group, but not for the limited literacy group; among those with adequate literacy screening, completion rates were highest in the nurse support arm. An interaction term for study arm and literacy level was entered into the final model and was statistically significant (p < 0.0001), indicating significantly different levels of effectiveness for the two literacy categories.
Table 3.
Primary Outcome Measure—Mammogram (Screened) Within 12 months, by Literacy Level
| All patients | Study arm | p value | |||
|---|---|---|---|---|---|
| Enhanced care | Education | Nurse | |||
| N (%) | N (%) | N (%) | N (%) | ||
| Limited literacy | N = 536 | N = 173 | N = 105 | N = 258 | |
| Mammogram (screened) | 309 (58) | 102 (59.0) | 58 (55.2) | 149 (57.7) | 0.17 |
| No mammogram | 227 (42) | 71 (41.0) | 47 (44.8) | 109 (42.3) | |
| Adequate literacy | N = 645 | N = 150 | N = 250 | N = 245 | |
| Mammogram (screened) | 386 (60) | 78 (52.0) | 126 (50.4) | 182 (74.3) | 0.039* |
| No mammogram | 259 (40) | 72 (48.0) | 124 (49.6) | 63 (25.7) | |
Multivariate analyses controlling for race (African American vs. Caucasian and Hispanic), marital status (married vs. not married), literacy (two categories) and self-efficacy
* p = 0.016, Nurse versus Education
The incremental cost effectiveness of the health literacy informed education, with or without nurse support is presented in Table 4. After adjustment for sample size, more people were screened in the enhanced care arm than in the education arm. Therefore, an incremental cost-effectiveness ratio was not calculated for education over enhanced care. The incremental cost of the nurse support intervention per additional person screened compared with the education arm was $2,457.
Table 4.
Cost-Effectiveness Analysis
| Education (comparison arm) vs. EUC (reference arm) | Nurse (comparison arm) vs. Education (reference arm) | ||
|---|---|---|---|
| Additional people screened in comparison arm | |||
| A | Sample size in reference arm | 323 | 355 |
| B | Number screened in reference arm | 180 | 184 |
| C | Sample size in comparison arm | 355 | 503 |
| D | Number screened in comparison arm | 184 | 331 |
| E | Number screened in comparison arm normalized to size of reference arm | 167.4 | 233.6 |
| F | Additional number screened in comparison arm normalized to size of reference arm = E – B | -12.6 | 49.6 |
| Incremental costs of comparison arm | |||
| G | Personnel | $1,098 | $172,705 |
| H | Non-personnel | $7,000 | $0 |
| I | Total incremental costs | $8,098 | $172,705 |
| J | Total incremental costs normalized to size of reference arm | $7,368 | $121,889 |
| Incremental cost-effectiveness ratio = row J/row F | * | $2,457 | |
*Incremental cost-effectiveness ratio of Education vs EUC was not calculated, since after adjusting for different group sample sizes, more people were screened in the EUC arm
DISCUSSION
Among urban and rural southern FQHC patients, our study documented extremely low baseline screening mammography rates. Our results indicate that mammography rates increased substantially over baseline in the three study strategies, although the nurse support arm was clinically and statistically superior to the other two arms. Of interest, we found giving low-income women a recommendation and scheduling a mammogram that required no out-of-pocket cost increased screening rates dramatically; however, additionally providing literacy and culturally appropriate education did not result in improvement in mammography rates over enhanced care. The addition of the nurse support and telephone follow-up significantly increased mammogram screening completion, but this arm was at substantially greater cost per patient.
Prior studies in safety-net clinics cite provider and system barriers, such as low rates of physician recommendation and inadequate insurance, as causes of lower mammography screening rates.12,14,47,48 Overcoming these barriers may be a reason for substantial improvement in the enhanced care arm, where non-medical staff gave patients a recommendation and suggestion to talk with their provider during their routine office visit and mammography was provided at no cost to those who lacked adequate insurance. The literature also cites personal barriers, such as limited knowledge and self-efficacy and faulty beliefs.5,17–27 However, in our study, although no patients were up-to-date and three-fourths had previously had a mammogram, the literacy-informed education intervention did not improve mammography completion over enhanced care. This may suggest that the education needs to be aimed at enhancing motivation and emphasizing the importance of regular mammography screening.
In our study, two-thirds of women who received brief education by a nurse with telephone follow-up, along with a free mammogram to those who lacked adequate insurance, completed screening. This is consistent with a meta-analysis that found the most effective programs for women with historically lower rates of mammography incorporated multifaceted–leveraging access-enhancement as well as individuallydirected strategies.49 Previous studies using personal telephone calls by an outreach specialist or patient navigator with women patients enrolled in privately and publically insured programs found significant improvement in mammography completion.47–52 In our study, when the nurses called patients, the most common barrier was being unable to make the appointment, rather than additional decision-making or cancer-related anxiety. Providing telephone follow-up reminders, and if needed, rescheduling assistance for no cost mammograms, may reduce key barriers for mammography completion for low income women. Given the cost of the nurse, other strategies to prompt patients, such as reminder calls and rescheduling help by a less-costly medical assistant, should be investigated. Even though use of a medical assistant would reduce cost by 80 %, this may still be cost-prohibitive among FQHCs. With the recent federal requirement for community health centers to have electronic health records (EHRs), amount of staff time dedicated to identifying and tracking patients could be substantially reduced. None of the FQHCs in this study had an integrated EHR system at the time of this study. Future studies should consider coupling reminder letters generated from the EHR with outreach calls and use of mobile mammography units, particularly in rural areas. FQHC networks could also consider structuring a collaborative outreach program, using a designated medical assistant to provide follow-up reminder calls for patients from multiple clinics.
Our study has limitations. Differences were noted between arms in sociodemographic characteristics, and self-efficacy, but not for the primary outcome of screening rates. Adjustments for key variables were therefore made in statistical analyses. Other limitations relate to generalizability of our results; we included predominantly African American and female patients receiving care from FQHCs in one state. However, this is generally representative of FQHC populations in the southern United States.
Strategies are needed to overcome limited resources for patient reminders, continued outreach, and scheduling assistance in FQHCs.30 Future research should explore leveraging less expensive clinic staff, distributing the workload over multiple clinics, and using EHR technology and possibly automated phone calls or text messages to offset some of the costs that may likely be necessary to maintain the success of a screening program that requires regular follow-up.
Acknowledgements
The authors would like to thank Ivory Davis, MSN and Cara Pugh, BSN, for their commitment to helping patients complete screening. This research was funded by the National Cancer Institute (R01- CA115869-05).
Conflict of Interest
The study authors have no potential conflicts of interest.
REFERENCES
- 1.Cancer facts & figures 2011–2012. Atlanta: ACS; 2012. [Google Scholar]
- 2.Cho Y, Lee S, Arozullah A, et al. Effects of health literacy on health status and health service utilization amongst the elderly. Soc Sci Med. 2008;66:1809–1816. doi: 10.1016/j.socscimed.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 3.White S, Chen J, Atchinson R. Relationship of Preventive Health Practices and Health Literacy: A National Study. Am J Health Behav. 2008;32(3):227–242. doi: 10.5993/AJHB.32.3.1. [DOI] [PubMed] [Google Scholar]
- 4.Alexandraki I, Mooradian AD. Barriers related to mammography use for breast cancer screening among minority women. J Natl Med Assoc. 2010;102(3):206–218. doi: 10.1016/s0027-9684(15)30527-7. [DOI] [PubMed] [Google Scholar]
- 5.Kagawa-Singer M, Valdez Dadia A, Yu MC, et al. Cancer, culture, and health disparities: Time to chart a new course? CA: A Cancer Journal for Clinicians. 2010;60(1):12–39. doi: 10.3322/caac.20051. [DOI] [PubMed] [Google Scholar]
- 6.Rayman KM, Edwards J. Rural primary care providers’ perceptions of their role in the breast cancer care continuum. J Rural Health. 2010;26(2):189–195. doi: 10.1111/j.1748-0361.2010.00281.x. [DOI] [PubMed] [Google Scholar]
- 7.Edwards JB, Tudiver F. Women’s preventive screening in rural health clinics. Women’s Health Issues. 2008;18(3):155–166. doi: 10.1016/j.whi.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 8.American Cancer Society. Breast Cancer Facts & Figures 2009-2010. Atlanta: American Cancer Society.
- 9.Brown KC, Fitzhugh EC, Neutens JJ, et al. Screening mammography utilization in Tennessee women: the association with residence. J Rural Health. 2009;25(2):167–173. doi: 10.1111/j.1748-0361.2009.00213.x. [DOI] [PubMed] [Google Scholar]
- 10.Cummings DM, Whetstone LM, Earp JA, et al. Disparities in mammography screening in rural areas: analysis of county differences in North Carolina. J Rural Health. 2002;18(1):77–83. doi: 10.1111/j.1748-0361.2002.tb00879.x. [DOI] [PubMed] [Google Scholar]
- 11.Harris DM, Miller JE, Davis DM. Racial differences in breast cancer screening, knowledge and compliance. J Nat Med Assoc. 2003;95(8):693–701. [PMC free article] [PubMed] [Google Scholar]
- 12.Cronan T, Villalta I, Gottfried E, et al. Predictors of mammography screening among ethnically diverse low-income women. Journal of Women’s Health. 2008;17(4):527–537. doi: 10.1089/jwh.2007.0331. [DOI] [PubMed] [Google Scholar]
- 13.Davis TC, Arnold C, Berkel HJ, et al. Knowledge and attitude on screening mammography among low literate, low income women. Cancer. 1996;78(9):1912–1920. doi: 10.1002/(SICI)1097-0142(19961101)78:9<1912::AID-CNCR11>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 14.Eheman C, Benard V, Blackman D, et al. Breast Cancer Screening among Low-Income or Uninsured Women: Results from the National Breast and Cervical Cancer Early Detection Program, July 1995 to March 2002 (United States) Canc Causes Contr. 2006;17(1):29–38. doi: 10.1007/s10552-005-4558-y. [DOI] [PubMed] [Google Scholar]
- 15.U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020. Washington, DC. Available at http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=5 Accessed December 4, 2013.
- 16.Agency for Healthcare Research and Quality. National Health Disparities Report 2011.
- 17.Champion V, Skinner C, Menon U. Development of a self efficacy scale for mammography. Res Nurse Health. 2005;28(4):329–336. doi: 10.1002/nur.20088. [DOI] [PubMed] [Google Scholar]
- 18.Clark M, Rakowski W, Bonacore L. Repeat mammography: Prevalence estimates and considerations for assessment. Ann Behav Med. 2003;26(3):201–211. doi: 10.1207/S15324796ABM2603_05. [DOI] [PubMed] [Google Scholar]
- 19.Elting LS, Cooksley CD, Bekele BN, et al. Mammography capacity: impact on screening rates and breast cancer stage at diagnosis. Am J Prev Med. 2009;37(2):102–108. doi: 10.1016/j.amepre.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 20.Ogedegbe G, Cassells AN, Robinson CM, et al. Perceptions of barriers and facilitators of cancer early detection among low-income minority women in community health centers. J Natl Med Assoc. 2005;97(2):162–170. [PMC free article] [PubMed] [Google Scholar]
- 21.Rauscher GH, Hawley ST, Earp JAL. Baseline predictors of initiation vs. maintenance of regular mammography use among rural women. Prev Med. 2005;40(6):822–830. doi: 10.1016/j.ypmed.2004.09.029. [DOI] [PubMed] [Google Scholar]
- 22.O’Malley AS, Forrest CB, Mandelblatt J. Adherence of low-income women to cancer screening recommendations. J Gen Intern Med. 2002;17(2):144–155. doi: 10.1046/j.1525-1497.2002.10431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Engelman KK, Ellerbeck EF, Perpich D, et al. Office systems and their influence on mammography use in rural and urban primary care. J Rural Health. 2004;20(1):36–42. doi: 10.1111/j.1748-0361.2004.tb00005.x. [DOI] [PubMed] [Google Scholar]
- 24.Lyttle NL, Stadelman K. Assessing awareness and knowledge of breast and cervical cancer among Appalachian women. Prev Chronic Dis. 2006;3(4):A125. [PMC free article] [PubMed] [Google Scholar]
- 25.Lopez EDS, Khoury AJ, Dailey AB, et al. Screening mammography: A cross-sectional study to compare characteristics of women aged 40 and older from the deep south who are current, overdue, and never screeners. Women’s Health Issues. 2009;19(6):434–445. doi: 10.1016/j.whi.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 26.Tejeda S, Thompson B, Coronado GD, et al. Predisposing and enabling factors associated with mammography use among Hispanic and non-Hispanic white women living in a rural area. J Rural Health. 2009;25(1):85–92. doi: 10.1111/j.1748-0361.2009.00203.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McAlearney AS, Reeves K, Tatum C, et al. Cost as a barrier to screening mammography among underserved women. Ethn Health. 2007;12(2):189–203. doi: 10.1080/13557850601002387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bennett I, Chen J, Soroui J, et al. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann Fam Med. 2009;7:204–211. doi: 10.1370/afm.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guerra C, Krumholz M, Shea J. Literacy and knowledge, attitudes and behavior about mammography in Latinas. J Health Care Poor Underserved. 2005;16:152–166. doi: 10.1353/hpu.2005.0012. [DOI] [PubMed] [Google Scholar]
- 30.U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion: National Action Plan to Improve Health Literacy. Washington, D.C.: U.S. Department of Health and Human Services, 2010.
- 31.Davis TC, Berkel HJ, Arnold CL, et al. Intervention to increase mammography utilization in a public hospital. J Gen Intern Med. 1998;13(4):230–233. doi: 10.1046/j.1525-1497.1998.00072.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Health Resources and Services Administration. www.hrsa.gov/. Accessed December 4, 2013.
- 33.Weiss B, Schwartzberg J, Davis T, et al. Health literacy and patient safety: Help patients understand: manual for clinicians. AMA Foundation, 2007.
- 34.U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999-2009 Incidence and Mortality Web-based Report. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2013. Available at: www.cdc.gov/uscs. Accessed December 4, 2013.
- 35.Ferreira MR, Dolan NC, Fitzgibbon ML, et al. Health care provider-directed intervention to increase colorectal cancer screening among veterans: Results of a randomized controlled trial. J Clin Oncol. 2005;23:1548–1554. doi: 10.1200/JCO.2005.07.049. [DOI] [PubMed] [Google Scholar]
- 36.Davis T, Arnold C, Rademaker A, et al. Improving colon cancer screening in community clinics. Cancer. 2013;119(21):3879–3886. doi: 10.1002/cncr.28272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.US Preventive Services Task Force Screening for breast cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2009;151:716–726. doi: 10.7326/0003-4819-151-10-200911170-00008. [DOI] [PubMed] [Google Scholar]
- 38.Champion V, Skinner C, Menon U. Development of a self-efficacy scale for mammography. Res Nurs Health. 2005;28:329–336. doi: 10.1002/nur.20088. [DOI] [PubMed] [Google Scholar]
- 39.Janz NK, Champion VL, Strecher VJ. The health belief model. In: Glanz K, Lewis F, Rimer B (eds.), Health Education Behavior, San Francisco: Jossey-Bass.
- 40.Rosenstock I. The health belief model: origins and correlates. Health Educ Monogr. 1974;2:336–353. [Google Scholar]
- 41.Rosenstock I, Strecher V, Becker M. Social learning theory and the health belief model. Health Educ Q. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 42.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 43.Davis TC, Arnold CL, Rademaker A, et al. Differences in Barriers to Mammography between Rural and Urban Women. Journal of Women’s Health. July 2012; 748-55. [DOI] [PMC free article] [PubMed]
- 44.Davis T, Long S, Jackson R, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25(6):391. [PubMed] [Google Scholar]
- 45.Hecht J, Borrelli B, Breger R, et al. Motivational interviewing in community-based research: Experiences from the field. Ann Behav Med. 2005;9(2):29–34. doi: 10.1207/s15324796abm2902s_6. [DOI] [PubMed] [Google Scholar]
- 46.Wolf MS, Wilson EA, Rapp DN, et al. Literacy and learning in health care. Pediatrics. 2009;124(Suppl 3):S275–S281. doi: 10.1542/peds.2009-1162C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Phillips C, Rothstein J, Beaver K, et al. Patient navigation to increase mammography screening among inner city women. J Gen Intern Med. 2011;26(2):123–129. doi: 10.1007/s11606-010-1527-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lipkus I, Rimer B, Halabi S, et al. Can tailored interventions increase mammography use among HMO women? Am J Prev Med. 2000;18(1):1–10. doi: 10.1016/S0749-3797(99)00106-3. [DOI] [PubMed] [Google Scholar]
- 49.Legler J, Meissner H, Coyne C, et al. The effectiveness of interventions to promote mammography among women with historically lower rates of screening. Cancer Epidemiol Biomarkers Prev. 2002;11(1):59–71. [PubMed] [Google Scholar]
- 50.Dietrich A, Tobin J, Cassells A, et al. Translation of an efficacious cancer-screening intervention to women enrolled in a Medicaid managed care organization. Ann of Fam Med. 2007;5(4):320–327. doi: 10.1370/afm.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Saywell R, Champion V, Skinner C, et al. A cost-effectiveness comparison of three tailored interventions to increase mammography screening. J Womens Health. 2004;13(8):909–918. doi: 10.1089/jwh.2004.13.909. [DOI] [PubMed] [Google Scholar]
- 52.Saywell R, Champion V, Zollinger T, et al. The cost effectiveness of 5 interventions to increase mammography adherence in a managed care population. Am J Manag Care. 2003;9(1):33–44. [PubMed] [Google Scholar]