ABSTRACT
BACKGROUND
The risk of readmission varies among hospitals. This variation has led the Centers of Medicare and Medicaid services to reduce payments to hospitals with excess readmissions. The contribution of patient characteristics, hospital characteristics and provider type to the variation in risk of readmission among hospitals has not been determined.
OBJECTIVE
To describe the variation in risk of readmission among hospitals and partition it by patient characteristics, hospital characteristics and provider type.
DESIGN
Retrospective research design of 100 % Texas Medicare data using multilevel, multivariable models.
SUBJECTS
A total of 514,064 admissions of Medicare beneficiaries to 272 hospitals in Texas for medical diagnoses during the years 2008 and 2009.
MAIN MEASURES
Using hierarchical generalized linear models, we describe the hospital-specific variation in risk of readmission that is attributable to patients characteristics, hospital characteristics and provider type by measuring the variance and intraclass correlation coefficients.
KEY RESULTS
Of the total variation in risk of readmission, only a small amount (0.84 %) is attributed to hospitals. In further analyses modeling the components of this variation among hospitals, differences in patient characteristics in the hospitals explained 56.2 % of the variation. Hospital characteristics and the type of provider explained 9.3 % of the variation among hospitals and 0.08 % of the total variation in risk of readmission.
CONCLUSIONS
Patient characteristics are the largest contributor to variation in risk of readmission among hospitals. Measurable hospital characteristics and the type of inpatient provider contribute little to variation in risk of readmission among hospitals.
KEY WORDS: readmissions, hospitalist, variation
INTRODUCTION
Approximately 20 % of Medicare beneficiaries discharged from US hospitals are readmitted within 30 days of discharge, at an estimated cost of $17 billion.1 Additionally, the risk of readmission varies among hospitals.1–6 For example, Krumholz et al. have reported that readmission rates for Acute Myocardial Infarction (AMI) varied from 10.9 % to 24.9 % and those for Heart Failure (HF) varied from 6.6 % to 19.8 % among US hospitals.5 This variation in risk of readmission has led the Centers for Medicare and Medicaid services (CMS) to attempt to reduce readmissions by lowering payments to hospitals that have excess readmissions for AMI, HF and pneumonia.7 This program, known as the Hospital Readmissions Reduction Program (HRRP), took effect on 1 October 2012 in hospitals at risk for up to 1 % of total inpatient reimbursement.8 The plan is to add more diagnoses and also to increase the penalties over the next few years.7 The implicit rationale of the accountability for excess readmissions placed on hospitals by the HRRP is that variations in risk of readmissions are caused by correctable hospital systems of care or modifiable practice patterns of hospital providers. Yet, little is known about what contributes to the variation in risk of readmission among hospitals.
In this report, using 100 % Medicare data for the state of Texas, we first aim to quantify the part of the total variation in risk of readmission that is attributable to hospitals, in other words, the variation ‘among hospitals’. We then partition this variation in risk of readmission among hospitals into that related to differences among those hospitals in patient characteristics, hospital characteristics and the type of provider caring for the patient during the hospitalization.
METHODS
Source of Data
We used claims from the year 2007 to 2009 for 100 % of Texas Medicare beneficiaries, including Medicare beneficiary summary files, Medicare Provider Analysis and Review (MedPAR) files, Outpatient Standard Analytical Files (OutSAF), and Medicare Carrier files. We obtained diagnosis-related groups (DRG) associated information, including type (medical or surgical), weights, and Major Diagnostic Categories (MDC) from Centers for Medicare & Medicaid Services (https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html). We obtained hospital characteristics from the Provider of Service (POS) file.
Establishment of the Study Cohort
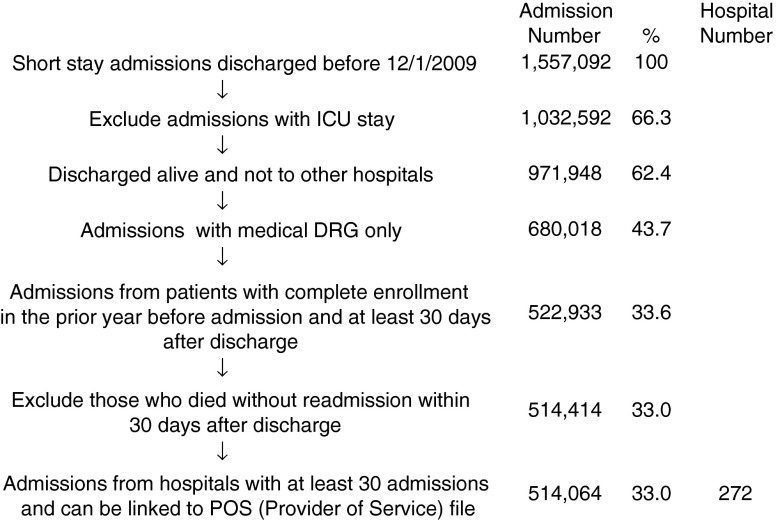
We outline this process in Figure 1. From 2008 and 2009 MedPAR files, we started with all admissions and then excluded those with intensive care unit services. We excluded those discharged dead or transferred to other hospitals. From the remaining, we selected admissions with a medical DRG. We further excluded patients who were enrolled in health maintenance organizations (HMOs), or did not have continuous Medicare Parts A and B coverage in the 12 months before and 1 month after the admission of interest, and those who died within 30 days of discharge without a readmission. We then selected admissions from hospitals with at least 30 admissions, resulting in 514,064 admissions and 272 hospitals in the final cohort.
Figure 1.
Cohort selection.
Measures
Patient Characteristics
We categorized patients by age, gender and ethnicity using Medicare beneficiary summary files. We used the Medicaid indicator as a proxy of low income and obtained information on weekday vs. weekend admission, emergent admission, and DRG from MedPAR files. We identified Elixhauser medical conditions using the claims from MedPAR, Carrier and OutSAF files in the year prior to the admission of interest.9 We determined residence in a nursing facility in the 3 months before the admission of interest from the MedPAR files and by identifying evaluation-and-management (E&M) billings using Current Procedural Terminology (CPT) codes 99304–99318 (nursing facility services) from Carrier files.10 We also assessed whether a patient had a primary care physician (PCP), defined as a generalist (general practitioner, family physician, internist or geriatrician) who saw the patient on three or more occasions in an outpatient setting (E&M codes 99201–99205 and 99211–99215) in the prior year.11 We identified total hospitalizations and outpatient visits in the prior year from MedPAR files and Carrier files, respectively.
Provider Type
We identified the treating physicians for each admission by linking inpatient evaluation and management (E&M) codes in the carrier files to the admission record in the MEDPAR files. Using specialty codes, we determined which physicians were specialists and generalists. We identified some generalists as ‘hospitalists,’ if they had at least 100 E&M billings in a given year and generated >90 % of these claims from care provided to hospitalized patients in that year.12 We thus could determine three types of physicians—specialists, hospitalists and non-hospitalist generalists.
If an inpatient stay did not have any E&M billings from generalists but only billings from specialists, the admission was classified as an admission cared for by specialists. If all the generalist billings during the hospitalization were from hospitalists, the admission was classified as an admission cared for by hospitalists. If none of the generalist billings were from hospitalists, the admission was classified as an admission cared for by non-hospitalist generalists. If only some of the generalist billings were from hospitalists, the admission was classified as cared for by both types of generalists.
Hospital Characteristics
We categorized hospitals by total bed number, financial status (Nonprofit, For-profit, or Government), and medical school affiliation using Provider of Service (POS) file.
Statistical Analyses
The unadjusted 30-day readmission rates for the 272 Texas hospitals were calculated and then plotted by rank from lowest to highest. The standard deviation of the unadjusted rate of each hospital was estimated by the normal approximation to the binomial distribution. We then used the hierarchical generalized linear model (multilevel logistic model), to account for the clustering of patients within a hospital and determined the intraclass correlation coefficient (ICC) of hospitals, representing the variation in readmission rates explained by hospitals.
In order to partition the sources of the variation among hospitals, we first built a null model without any adjustment to determine the ICC of hospitals, and then used Spearman-Brown prophecy formula13 to calculate reliability. The proportion of variation due to noise was calculated as 1-reliability.14 The reliability was higher and noise lower for hospitals with more admissions. The reliability was 93 % (noise 7 %) when we selected hospitals with at least 1,500 admissions of interest. These represented about half of the total of 272 hospitals in our study. We performed further analysis on this subgroup of hospitals with at least 1,500 admissions of interest, as with them we felt that we had the best balance between a large enough sample and low enough noise to get valid results. We then estimated the proportion of non-noise hospital variation attributed to differences in patient characteristics, hospital characteristics or provider type among the hospitals by comparing the variance of hospitals from adjusted models to that of the null model (Appendix 1, available online). We presented our findings in the form of a Venn diagram constructed using “eulerAPE version 2.0” (School of Computing, University of Kent, Canterbury, UK). All analyses were performed with SAS version 9.2 (SAS Inc., Cary, NC).
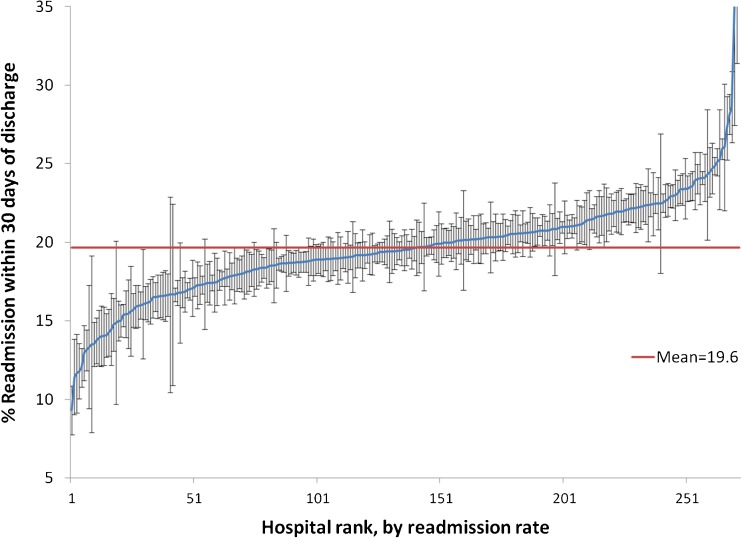
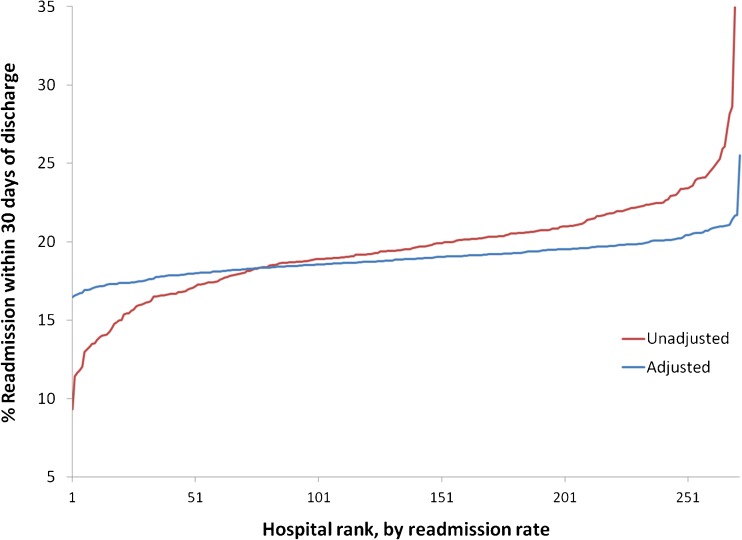
RESULTS
The cumulative distribution of the unadjusted 30-day readmission rates for medical discharges from the 272 Texas hospitals in 2008 and 2009 is presented graphically in Figure 2, and demonstrates the variation in risk of readmission. The unadjusted readmission rates for the top and bottom deciles of hospitals were 22.9 % and 15.9 %, respectively. Figure 3 shows the cumulative distribution of unadjusted 30-day readmission rates for the hospitals, along with the rates adjusted for patient characteristics. After adjustment for patient characteristics, the differences between the rates for the top and bottom deciles were greatly reduced, to 20.1 % and 17.5 %.
Figure 2.
Unadjusted 30-day readmission rates for the 272 Texas hospitals, by rank from lowest to highest. The horizontal line represents the overall mean. Error bars represent standard deviation estimated by the normal approximation to the binomial distribution.
Figure 3.
Unadjusted (red) and adjusted (blue) 30-day readmission rates for the 272 Texas hospitals, by rank from lowest to highest. The adjusted rates were estimated from a multilevel model adjusting for patient characteristics, including age, sex, race, Medicaid eligibility, ER admission, weekend admission, MDC, DRG weights, 29 comorbid conditions, any nursing home stay in the prior 90 days, number of hospitalizations, number of outpatient physician visits, and presence of an identifiable PCP in the prior year.
The results of the multivariable, multilevel analysis of patient and hospital factors associated with readmission are summarized in Table 1. Patient characteristics such as male gender, being poor, being sick and requiring more prior outpatient, inpatient or nursing home care were associated with higher odds of readmission. Non-white race had a protective effect against readmissions when controlling for all other factors. Patients who were cared for by specialists and those who were cared for by both hospitalists and non-hospitalist generalists during their hospitalization were at a higher risk for readmission. Not shown in the table but included in the analysis are the 22 major diagnostic categories for the index hospitalization and 29 specific comorbidities. This complete model is presented in Appendix 2, available online.
Table 1.
Multivariable Multilevel Analysis of the Impact of Patient and Hospital Characteristics on the Odds of Readmission Within 30 Days of Hospital Discharge
| Patient Characteristic | Odds Ratio (95 % CI) |
|---|---|
| Age, every 10y | 1.01 (1.00, 1.01) |
| Race | |
| White | 1.00 |
| Black | 0.98 (0.95, 1.00)* |
| Hispanic | 0.93 (0.91, 0.95)* |
| Other | 0.92 (0.87, 0.98)* |
| Sex, Male vs. Female | |
| Male | 1.10 (1.08, 1.11)* |
| Female | 1.00 |
| Medicaid eligible, Yes vs. No | 1.07 (1.06, 1.09)* |
| Emergency Admission, Yes vs. No | 0.99 (0.97, 1.00) |
| Weekend Admission, Yes vs. No | 0.99 (0.98, 1.01) |
| DRG weights | 1.38 (1.35, 1.41)* |
| Number of hospitalizations in the year prior | 1.18 (1.17, 1.18)* |
| Number of doctor visits in the year prior, every five visits | 1.02 (1.01, 1.02)* |
| Nursing home residence in prior 90 days, Yes vs. No | 1.07 (1.05, 1.09)* |
| Primary Care Physician in the year prior admission, Yes vs. No | 0.99 (0.97, 1.00) |
| Hospital characteristics | |
| Hospital type | |
| Nonprofit | 1.00 |
| Proprietary | 1.02 (0.99, 1.06) |
| Government | 1.02 (0.98, 1.06) |
| Hospital size | |
| ≤ 200 | 1.00 |
| 201–350 | 0.95 (0.92, 0.99)* |
| 351–500 | 0.96 (0.91, 1.00) |
| > 500 | 0.97 (0.92, 1.02) |
| Medical school affiliation | |
| No affiliation | 1.00 |
| Major | 1.04 (0.98, 1.11) |
| Limited | 0.99 (0.94, 1.04) |
| Type of care during hospitalization | |
| Non-Hospitalist Generalist | 1.00 |
| Hospitalist | 1.01 (0.99, 1.03) |
| Both of the above | 1.11 (1.07, 1.14)* |
| Specialist | 1.05 (1.03, 1.07)* |
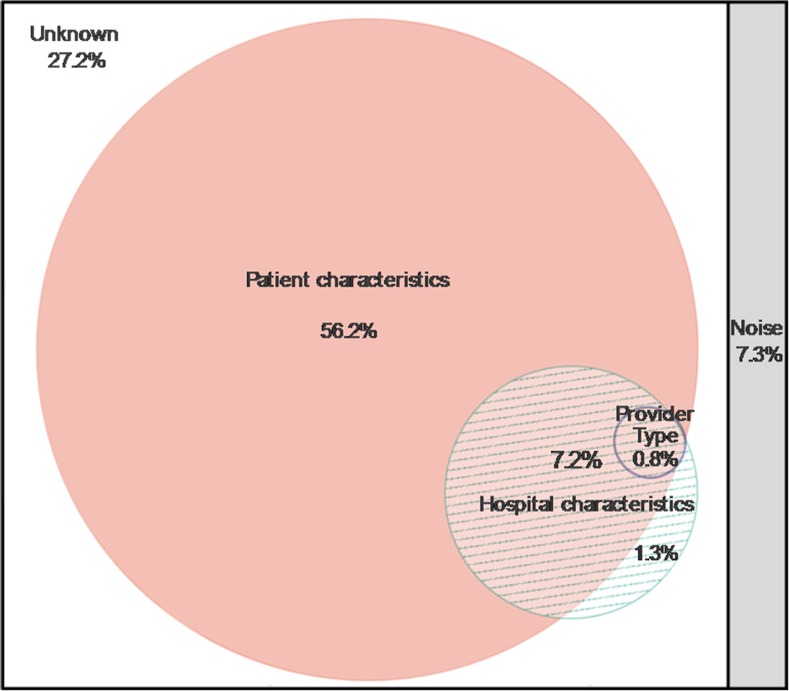
In a null multilevel model without any adjustment, the intraclass correlation coefficient (ICC) was 0.84 % for the hospital level. We then used models adjusting for the various hospital, patient and provider characteristics to assess the contribution of each to the variation among hospitals in 30-day readmission rate.
Figure 4 illustrates the apportioning of the variance in hospital readmission rates among patient characteristics, hospital characteristics, and the physician providing medical care while hospitalized, derived from multilevel models adjusting for patient, hospital characteristics, provider type, or combinations of them. The large square is the total variance in readmission rates explained by hospitals, and the sizes of the partitions within it are proportional to amount of this hospital specific variance explained by respective factors. The variation due to sampling error, or “noise,” depends on the number of admissions of a hospital. When there are more admissions in a hospital, the noise is smaller. In the model shown, 7.3 % of the variation is “noise”, shown as a grey bar at the right. The largest circle represents the contribution of measurable patient characteristics to variation among hospitals. The next smaller circle represents the contribution of measurable hospital characteristics, and the smallest circle represents the contribution of the provider type. When circles overlap, it means that the variance in proportion to the area of overlap is explained by multiple factors. Thus, measureable patient characteristics alone account for 56.2 % of the variation (area of large circle with no overlap). Another 7.2 % of variation is explained by patient characteristics and hospital characteristics (area of overlap between the two circles), and another 0.8 % of variation is explained by all three study factors—patient characteristics, hospital characteristics and provider type (area of overlap between all three circles). Measurable hospital characteristics account for 9.3 % of the variation, most of which (7.2 %) is the intersection of variance attributed to both patient and hospital characteristics. The provider type accounts for 0.8 % of the variation, which completely overlaps with what was attributed from patient or hospital characteristics. Another way of stating that is that 0.8 % of the variation in hospital readmission rates is due to the different types of physicians working in different hospitals taking care of different patients. Our models could not explain 27.2 % of the variation in risk of readmission among hospitals (un-partitioned white background in Fig. 4).
Figure 4.
Sources of variation in 30-day risk of readmission among hospitals with at least 1,500 admissions.
DISCUSSION
Among 514,064 hospitalizations of Medicare beneficiaries across 272 hospitals, we found that the proportion of total variation in risk of readmission that is explained by hospitals is less than 1 % (0.84 %). Upon further exploration of variation among hospitals, differences in patient characteristics explained over half of the variation. Measurable hospital characteristics and the type of provider caring for hospitalized patients each made a small contribution to the variation among hospitals.
Our finding of a low amount of total variation in readmission risk that can be explained by hospitals is consistent with a previous study, which found the proportion of total variation in risk of readmission explained by hospitals to be 1.5 % for acute myocardial infarction and 2.6 % for heart failure.5 The authors of that study commented that the low amount of variation explained by hospitals could represent a situation where all hospitals were performing poorly and might still represent a target for improvement. In the present study, upon partitioning the variation in the risk of readmission among hospitals, patient characteristics proved to be the largest contributor to this variation. To the best of our knowledge, this is the first investigation demonstrating the predominance of patient characteristics in determining hospital-specific variation in risk of readmission.
Others have shown that patient characteristics are important risk factors for an individual’s risk of readmission.15 In our study, we found that poorer patients and sicker patients and those who required greater outpatient, inpatient or nursing home care had a higher risk of readmission. Our finding of a protective effect of minority status is surprising, and contrasts with a recent report by Joynt et al. that showed that minorities are at increased risk for readmissions.16 We included Medicaid eligibility (as an indicator of poverty) as a covariate in our multivariable models, whereas Joynt et al. did not. Thus, if poverty is the main mechanism by which minorities are predisposed to an increased risk of readmission, our adjusting for Medicaid eligibility may explain the divergence in findings between our study and the study by Joynt et al.
The amount of total variation in risk of readmission explained by measurable hospital characteristics and inpatient provider type is 0.08 % (9.3 % of 0.84 %). This suggests that the locus of accountability for excess readmissions should not be the hospital. There is other evidence that supports this assertion. Vigorous quality improvement efforts have targeted readmissions, but rates have remained stable.17 Readmission rates have been stubbornly resistant to most carefully studied interventions (mostly hospital based) designed to reduce them.18,19 Additionally, the risk of readmission has no correlation with reported hospital performance on discharge planning in hospitals.20 Our findings, when combined with this emerging evidence, call into question CMS policies holding hospitals accountable for excess readmissions. Moreover, it is possible that the policies holding hospitals accountable for excess readmissions may not merely be ineffective, but may be harmful. Hospitals serving sicker, poorer and otherwise more disadvantaged patients will be financially penalized for the higher readmission rates resulting from the patient population they serve. This has a real potential to compromise the care of those most in need.21
Our study has limitations. We study patients with fee for service Medicare in a single large state in the US over a 2-year period. Our findings may not be generalizable to younger patient populations, other regions or other time periods. However, the fact that our cohort includes a large number of Medicare beneficiaries makes our study more relevant to CMS policies. We excluded patients who required an intensive care unit (ICU) stay and patients with surgical conditions, so our findings may not apply to those patient populations.
In summary, this study reveals that hospitals explain little of the variation in risk of readmission. Patient characteristics are the dominant contributor to the variation in risk of readmission among hospitals. Our findings add to the accumulating evidence that hospitals may not be the appropriate sole target for placing accountability for excess readmissions.17,22,23
Acknowledgments
Funders
Supported by grants from the National Institutes of Health: 1R01-AG033134, K05-CA134923, 5P30AG024832 and RP101207.
Prior Presentations
None.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
APPENDICES
Appendix 1
Detail on statistical analysis to partition the variation in risk of readmission among hospital between Patient characteristics, Hospital characteristics and provider type.
We estimated the proportion of non-noise hospital variation attributed to patient characteristics, provider type, or hospital characteristics by comparing the variance of hospitals from an adjusted model to that of the null model. For example, we ran the null model first and then a model including patient characteristics. The proportion of hospital variation due to patient characteristics is: (hospital variance of model0 – hospital variance of model1) / hospital variance of model0. We determined the proportions of non-noise hospital variation attributable to patient characteristics, provider type and hospital characteristics by comparing the following models to the null model.
Adjusted for patient characteristics
Adjusted for hospital characteristics
Adjusted for provider type
Adjusted for patient characteristics and hospital characteristics
Adjusted for patient characteristics and provider type
Adjusted for hospital characteristics and provider type
Adjusted for patient characteristics, hospital characteristics, and provider type
Let P, H, T be the proportions of non-noise variation attributable to patient, hospital characteristics, and provider type, respectively. From models 1 through 7, we obtained P, H, T, P∪H, P∪T, H∪T, and P∪H∪T. By applying the following equation,
 |
the intersection between each two proportions was identified, and these proportions were presented in a Venn diagram using “eulerAPE version 2.0” (School of Computing, University of Kent, Canterbury, UK). The proportion of non-noise variation attributable to unknown factors was calculated as 1-P∪H∪T.
Appendix 2
Table 2.
Multivariable Multilevel Analysis of the Impact of Patient and Hospital Characteristics on the Odds of Readmission Within 30 Days of Hospital Discharge
| Patient Characteristic | Odds Ratio (95 % CI) |
|---|---|
| Age, every 10y | 1.01 (1.00, 1.01) |
| Race | |
| White | 1.00 |
| Black | 0.98 (0.95, 1.00)* |
| Hispanic | 0.93 (0.91, 0.95)* |
| Other | 0.92 (0.87, 0.98)* |
| Sex, Male vs. Female | |
| Male | 1.10 (1.08, 1.11)* |
| Female | 1.00 |
| Medicaid eligible, Yes vs. No | 1.07 (1.06, 1.09)* |
| Emergency Admission, Yes vs. No | 0.99 (0.97, 1.00) |
| Weekend Admission, Yes vs. No | 0.99 (0.98, 1.01) |
| DRG weights | 1.38 (1.35, 1.41)* |
| Major Diagnostic Category | |
| Nervous System | 0.90 (0.88, 0.93)* |
| Eye | 0.73 (0.58, 0.93)* |
| Ear, Nose, Mouth And Throat | 0.66 (0.61, 0.72)* |
| Respiratory System | 0.91 (0.89, 0.93)* |
| Circulatory System | 1.00 |
| Digestive System | 0.99 (0.97, 1.02) |
| Hepatobiliary System And Pancreas | 1.33 (1.27, 1.39)* |
| Musculoskeletal System And Connective Tissue | 1.12 (1.08, 1.17)* |
| Skin, Subcutaneous Tissue And Breast | 0.78 (0.75, 0.81)* |
| Endocrine, Nutritional And Metabolic System | 1.06 (1.03, 1.10)* |
| Kidney And Urinary Tract | 0.99 (0.96, 1.02) |
| Male Reproductive System | 1.04 (0.91, 1.19) |
| Female Reproductive System | 1.77 (1.54, 2.03)* |
| Blood and Blood Forming Organs and Immunological Disorders | 1.19 (1.14, 1.24)* |
| Myeloproliferative Diseases and Poorly Differentiated Neoplasms | 3.06 (2.87, 3.26)* |
| Infectious and Parasitic Diseases and Disorders | 0.78 (0.75, 0.81)* |
| Mental Diseases and Disorders | 1.11 (1.06, 1.16)* |
| Alcohol/Drug Use or Induced Mental Disorders | 0.91 (0.80, 1.02) |
| Injuries, Poison And Toxic Effect of Drugs | 0.88 (0.81, 0.94)* |
| Burns | 0.84 (0.55, 1.29) |
| Factors Influencing Health Status | 1.05 (0.98, 1.14) |
| Human Immunodeficiency Virus Infection | 1.00 (0.84, 1.19) |
| Number of hospitalizations in the year prior | 1.18 (1.17, 1.18)* |
| Number of doctor visits in the year prior, every five visits | 1.02 (1.01, 1.02)* |
| Nursing home residence in prior 90 days, Yes vs. No | 1.07 (1.05, 1.09)* |
| PCP in the year prior admission, Yes vs. No | 0.99 (0.97, 1.00) |
| Comorbidity, Yes vs. No | |
| Congestive heart failure | 1.15 (1.13, 1.17)* |
| Valve disease | 1.04 (1.02, 1.06)* |
| Pulmonary circulation disease | 1.02 (0.99, 1.06) |
| Peripheral vascular disease | 1.02 (1.00, 1.04)* |
| Paralysis | 1.00 (0.97, 1.03) |
| Neurological disorder | 0.99 (0.97, 1.00) |
| Chronic pulmonary disease | 1.09 (1.07, 1.11)* |
| Diabetes mellitus without complication | 1.02 (1.00, 1.03) |
| Diabetes mellitus with complication | 1.06 (1.04, 1.08)* |
| Hypothyroidism | 0.98 (0.97, 1.00) |
| Renal failure | 1.10 (1.08, 1.13)* |
| Liver disease | 1.16 (1.12, 1.20)* |
| Peptic ulcer | 0.92 (0.76, 1.11) |
| AIDS | 1.03 (0.93, 1.14) |
| Lymphoma | 1.27 (1.21, 1.33)* |
| Metastatic cancer | 1.42 (1.37, 1.48)* |
| Solid tumor without metastasis | 1.12 (1.09, 1.15)* |
| Rheumatoid arthritis | 1.05 (1.02, 1.08)* |
| Coagulopathy | 1.07 (1.04, 1.10)* |
| Obesity | 0.97 (0.94, 0.99)* |
| Weight loss | 1.07 (1.04, 1.09)* |
| Fluid and electrolyte disorder | 1.09 (1.07, 1.11)* |
| Chronic blood loss anemia | 0.98 (0.94, 1.01) |
| Deficiency anemia | 1.08 (1.06, 1.10)* |
| Alcohol abuse | 1.02 (0.98, 1.07) |
| Drug abuse | 1.19 (1.14, 1.25)* |
| Psychosis | 1.02 (0.99, 1.04) |
| Depression | 0.99 (0.97, 1.01) |
| Hypertension | 1.00 (0.98, 1.02) |
| Hospital characteristics | |
| Hospital type | |
| Nonprofit | 1.00 |
| Proprietary | 1.02 (0.99, 1.06) |
| Government | 1.02 (0.98, 1.06) |
| Hospital size | |
| ≤ 200 | 1.00 |
| 201–350 | 0.95 (0.92, 0.99)* |
| 351–500 | 0.96 (0.91, 1.00) |
| > 500 | 0.97 (0.92, 1.02) |
| Medical school affiliation | |
| No affiliation | 1.00 |
| Major | 1.04 (0.98, 1.11) |
| Limited | 0.99 (0.94, 1.04) |
| Type of care during hospitalization | |
| Non-Hospitalist Generalist | 1.00 |
| Hospitalist | 1.01 (0.99, 1.03) |
| Both of the above | 1.11 (1.07, 1.14)* |
| Specialist | 1.05 (1.03, 1.07)* |
| Other | 1.00 (0.97, 1.03) |
*Statistically significant
REFERENCES
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare Fee-for-Service Program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Goodman, DC, Fisher ES, Chang C. After Hospitalization: A Dartmouth Atlas Report on Post-Acute Care for Medicare Beneficiaries. Dartmouth Atlas website. Available at: www.dartmouthatlas.org/downloads/reports/Post_discharge_events_092811.pdf. Accessed 11/10/13, 2013. [PubMed]
- 3.Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011;365(24):2287–2295. doi: 10.1056/NEJMsa1101942. [DOI] [PubMed] [Google Scholar]
- 4.Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why? Circ Cardiovasc Qual Outcomes. 2011;4(1):53–59. doi: 10.1161/CIRCOUTCOMES.110.950964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krumholz HM, Merrill AR, Schone EM, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009;2(5):407–413. doi: 10.1161/CIRCOUTCOMES.109.883256. [DOI] [PubMed] [Google Scholar]
- 6.Fisher ES, Wennberg JE, Stukel TA, Sharp SM. Hospital readmission rates for cohorts of Medicare beneficiaries in Boston and New Haven. N Engl J Med. 1994;331(15):989–995. doi: 10.1056/NEJM199410133311506. [DOI] [PubMed] [Google Scholar]
- 7.Readmissions Reduction Program 2012. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed 11/10/13, 2013.
- 8.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the hospital readmissions reduction program. JAMA. 2013;309(4):342–343. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 9.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Koroukian SM, Xu F, Murray P. Ability of Medicare claims data to identify nursing home patients: a validation study. Med Care. 2008;46(11):1184–1187. doi: 10.1097/MLR.0b013e31817925d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah BR, Hux JE, Laupacis A, Zinman B, Cauch-Dudek K, Booth GL. Administrative data algorithms can describe ambulatory physician utilization. Health Serv Res. 2007;42(4):1783–1796. doi: 10.1111/j.1475-6773.2006.00681.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuo Y-F, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360(11):1102–1112. doi: 10.1056/NEJMsa0802381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bravo G, Potvin L. Estimating the reliability of continuous measures with cronbach's alpha or the intraclass correlation coefficient: toward the integration of two traditions. J Clin Epidemiol. 1991;44(4–5):381–390. doi: 10.1016/0895-4356(91)90076-L. [DOI] [PubMed] [Google Scholar]
- 14.Kao LS, Ghaferi AA, Ko CY, Dimick JB. Reliability of superficial surgical site infections as a hospital quality measure. J Am Coll Surg. 2011;213(2):231–235. doi: 10.1016/j.jamcollsurg.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–1698. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joynt KE, Orav E, Jha AK. Thirty-day readmission rates for medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675–681. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Joynt KE, Jha AK. Thirty-day readmissions—truth and consequences. N Engl J Med. 2012;366(15):1366–1369. doi: 10.1056/NEJMp1201598. [DOI] [PubMed] [Google Scholar]
- 18.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 19.Benbassat J, Taragin MI. The effect of clinical interventions on hospital readmissions: a meta-review of published meta-analyses. Isr J Health Policy Res. 2013;2(1):1–15. doi: 10.1186/2045-4015-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med. 2009;361(27):2637–2645. doi: 10.1056/NEJMsa0904859. [DOI] [PubMed] [Google Scholar]
- 21.Bhalla R, Kalkut G. Could Medicare readmission policy exacerbate health care system inequity? Ann Intern Med. 2010;152(2):114–117. doi: 10.7326/0003-4819-152-2-201001190-00185. [DOI] [PubMed] [Google Scholar]
- 22.Fontanarosa PB, McNutt RA. Revisiting hospital readmissions. JAMA. 2013;309(4):398–400. doi: 10.1001/jama.2013.42. [DOI] [PubMed] [Google Scholar]
- 23.McCarthy D, Johnson MB, Audet AM. Recasting readmissions by placing the hospital role in community context. JAMA. 2013;309(4):351–352. doi: 10.1001/jama.2013.1. [DOI] [PubMed] [Google Scholar]