Abstract
Fragile X-associated tremor/ataxia syndrome (FXTAS) is an adult-onset neurodegenerative disorder associated with premutation alleles of the fragile X mental retardation 1 (FMR1) gene. Approximately 40% of older male premutation carriers, and a smaller proportion of females, are affected by FXTAS; due to the lower penetrance the characterization of the disorder in females is much less detailed. Core clinical features of FXTAS include intention tremor, cerebellar gait ataxia, and frequently parkinsonism, autonomic dysfunction, and cognitive deficits progressing to dementia in up to 50% of males.
Here, we report the clinical, molecular, and neuropathological findings of eight female premutation carriers. Significantly, four of these women had dementia; of the four, three had FXTAS plus dementia. Post mortem examination revealed the presence of intranuclear inclusions in all eight cases, which included one asymptomatic premutation carrier who died from cancer. Among the four subjects with dementia, three had sufficient number of cortical amyloid plaques and neurofibrillary tangles to make Alzheimer’s disease a highly likely cause of dementia and a fourth case had dementia with cortical Lewy bodies. Dementia appears to be more common than originally reported in females with FXTAS. Although further studies are required, our observation suggests that in a portion of FXTAS cases and Alzheimer pathologies a synergistic effect on the progression of the disease may occurs.
Keywords: FMR1 premutation, FXTAS, Alzheimer Disease, RNA toxicity, Activation Ratio
INTRODUCTION
The FMR1 gene is highly polymorphic for CGG trinucleotide repeats in its 5′ untranslated region. CGG expansions in the premutation range (55–200 repeats) give rise to the leading known single-gene cause of primary ovarian insufficiency (Oostra & Willemsen, 2009), and the late-onset neurodegenerative disorder, FXTAS (Hagerman et al., 2001). FXTAS is characterized by intention tremor and gait ataxia, with both age-of-onset and severity being associated with the number of CGG repeats (Tassone et al., 2007, Tassone & Berry-Kravis, 2010). Cerebral atrophy and white matter disease are prominent imaging findings in individuals with FXTAS (Adams et al., 2007, Adams et al., 2010). White matter MRI hyperintensities in the middle cerebellar peduncles (i.e., “MCP sign”) represent a major diagnostic criterion for FXTAS although observable in only 58% of males and 13% of female carriers (Adams et al., 2007, Brunberg et al., 2002). The pathological hallmark is the presence of intranuclear inclusions in neurons and astrocytes (Greco et al., 2002), in the neuroendocrine system (Louis et al., 2006), in the autonomic nervous system, and myocardial cells (Gokden et al., 2008, Greco et al., 2007, Hunsaker et al., 2011).
The pathogenesis of premutation-associated disorders, particularly FXTAS, is thought to involve an RNA toxic gain-of-function mechanism, mediated by elevated levels of premutation length FMR1 mRNA (Allen et al., 2004, Kenneson et al., 2001, Peprah et al., 2010, Tassone et al., 2000) which has been detected within the intranuclear inclusions present in the brain (Tassone et al., 2004). Although the role of these inclusions in the pathogenesis of FXTAS remains unclear, it is likely that they reflect, a much broader process of cellular sequestration of one or more proteins whose functions are thereby compromised (Raske & Hagerman, 2009, Sellier et al., 2010).
FXTAS occurs in approximately 40% of carrier males (Jacquemont et al., 2004a) with an increased likelihood of penetrance with age (Jacquemont et al., 2004b). A reduced FXTAS penetrance (between 8 and 17%) has been observed in female premutation carriers (Chonchaiya et al., 2010a, Coffey et al., 2008, Jacquemont et al., 2004b, Rodriguez-Revenga et al., 2009). This may be primarily due to the protective effect of the normal allele on the second X chromosome (Berry-Kravis et al., 2005, Jacquemont et al., 2005). Indeed, female premutation carriers show less frequent clinical and neuropathological features than male premutation carriers, both with and without FXTAS, but in some cases they may have symptoms that are as severe as those of their male counterparts (Adams et al., 2007). FXTAS females have a higher incidence of hypothyroidism, potentially autoimmune thyroid disease and fibromyalgia, than either age-matched controls or males with FXTAS (Coffey et al., 2008, Leehey et al., 2011, Rodriguez-Revenga et al., 2009). They also present hypertension, seizures, and peripheral neuropathy more often than controls (Chonchaiya et al., 2010b, Coffey et al, 2008, Hamlin et al., 2011). Co-occurrence of multiple sclerosis (MS) has been described in women carriers (Greco et al., 2008, Zhang et al., 2009). We have studied eight premutation females and here we report their neuropathological findings, molecular data, and clinical problems.
MATERIALS AND METHODS
Molecular measures
DNA analysis
Genomic DNA was isolated from peripheral blood leucocytes (5 ml of whole blood) obtained prior to death, and from post-mortem sections of approximately 500mg of brain tissue using standard methods (Puregene Kit; Gentra Inc.) and under informed consent according to Institutional Review Board approved protocols. Southern blot analysis, PCR analysis and calculation of the repeat size for both methods were performed as described in Tassone et al. (2008). The Activation Ratio (AR), which expresses the percent of cells carrying the normal allele on the active X chromosome, was measured using an Alpha Innotech FluorChem 8800 Image Detection System as previously described (Tassone et al., 1999).
FMR1 mRNA levels
Total RNA was isolated from peripheral blood leukocytes using Tempus tubes (Applied Biosystems, Foster City, CA). Reverse transcriptase reactions and quantifications of FMR1 mRNA were performed as described in Tassone et al. (2000).
Pathology
Formalin-fixed brain tissue for all cases was processed for paraffin sections, and histological and immunohistological staining in standard fashion as previous reported (Greco et al., 2006, Greco et al., 2002). Tissue blocks of frontal cortex and hippocampus were obtained from five age matched control female subjects (age range 60–76 years). Tissues were selected to be the same across all cases to facilitate comparisons among experimental cases. Control cases were obtained from pathology files at Department of Pathology at University of California, Davis according to UC Davis approved IRB protocol.
Evaluation of AD neuropathology
We evaluated the AD neuropathology, including the Braak and Braak stage and the CERAD plaque score, using the Diagnostic Criteria for the Neuropathological Assessment of Alzheimer’s Disease, following the recommendation by the National Institute on Aging and Reagan Institute Working Group (NIA-Reagan criteria) (1997).
Quantitative analysis of intranuclear inclusion number
Percentages of intranuclear inclusions in neurons and astrocytes were determined for frontal cortex, hippocampus, and middle superior temporal gyrus using protocols previously described (Greco et al., 2006, Greco et al., 2002, Greco et al., 2008). Tissue from blocks of frontal cortex and hippocampus were obtained for 8 female cases and middle superior temporal gyrus was obtained for 7 of these cases. Quantifications were compared to previously reported female control cases from Greco et al. (2006). These control cases matched the age range of the present female cases, and were free of gross neuropathological features or histological artifacts.
Brain tissues were blocked and sectioned in the same orientation to facilitate histological analysis. Tissues were paraffin embedded, sectioned at 10 μm, and stained with hematoxylin and eosin (H&E). Three sections separated by 50 μm were used for unbiased cell counting.
To estimate the number of intranuclear inclusions in females with the fragile X premutation both with and without FXTAS, regions of interest were outlined within the frontal cortex, superior medial temporal gyrus, and hippocampus, using the StereoInvestigator (v 8.0, MBI, Inc.; Williston, TN) software package and a Nikon E600 Eclipse microscope at 400x magnification. All parameters explicitly replicated those reported by Greco et al. (2006) quantifying inclusions presence in male FXTAS cases to facilitate comparison between the results of that study and the present report. To reduce bias in our samples, standard sections were taken from all control cases and premutation cases to allow direct comparisons among cases. Unbiased sampling techniques were used to collect and define a systematic, random sampling of the tissue to ensure an unbiased estimation of inclusion number, but no rigorous stereology was carried out in the present study and we are reporting the actual number of items counted, not estimated values provided by the software. Briefly, these techniques involved tracing the regions of interest at 40X magnification by an experimenter blinded to the identity of each case (i.e., slide blinded). Once the region of interest was traced, the software placed a regular grid of sampling frames across the region of interest using a randomized starting point. The size of the counting frame and spacing of the grids were the same as reported in Greco et al. (2006). This way, there was a rigorous, systematic sampling of the area contained within the region of interest, but the experimenter did not have control over precisely which areas of the region of interest were sampled. Counting of cells containing intranuclear inclusions was performed at 400X. Cell identification within the regions of interest was based on standard morphological criteria as previously described (Greco et al., 2006, Greco et al., 2002). The numbers obtained from these cell counts were converted to ratios (# of cell type with inclusions/total # of cell type counted).
RESULTS
Clinical Histories
Key clinical features and molecular characteristics of the eight cases included in this study are presented in Table 1.
Table 1.
Summary of the clinical, molecular and neuropathological features of the current cases
| Case | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | |
|---|---|---|---|---|---|---|---|---|---|
| Clinical | Age of death | 76 | 66 | 85 | 52 | 80 | 65 | 84 | 79 |
| Symptoms | Bell’s palsy, uterine cancer | Dementia | Slight intention tremor, cardiac arrhythmias | Cognitive decline; MS; neuropathy; tremor; ataxia | Dementia; tremor | Dementia; tremor, fibromyalgia, hyperthyroidis | DLB (2); intentional tremor, ataxia; neuropathy, hypertention; breast cancer | Intentional tremor; ataxia, neuropathy | |
| FXTAS | No | Yes | Yes | Yes | No | Yes | Yes | Yes | |
| Molecular | CGG repeats | 30,70 | 30, 80 | 29,87 | 36, 75 | 30, 63 | Premutation(1) | 27, 59 | 30, 78 |
| Activation Ratio | 0.80 | 0.30 | 0.53 | 0.44 | 0.28 | - | 0.63 | 0.21 | |
| FMR1 mRNA levels | 1.31 (0.11) | n/a | 2.31 (0.17) | 2.8 (0.12) | n/a | n/a | 1.83 (0.12) | 2.6 (0.04) | |
| Pathology | Intranuclear inclusions (FXTAS) | + | + | + | + | + | + | + | + |
| Braak & Braak staging (3) | 0 | Braak V–VI | Braak I–II | 0 | Braak V–VI | Braak V–VI | Braak I–II | Braak V–VI | |
| CERAD plaque score (4) | 0 | frequent | sparse | 0 | frequent | frequent | sparse | moderate | |
| Addl. significant histopathology | mild arteriolosclerosis | -- | -- | multiple sclerosis | -- | -- | Lewy bodies, | Severe arteriosclerosis |
Fixed tissues only; reported as premutation without allele sizes or AR (Yachnis et al., 2010)
DLB - Dementia with Lewy body disease
Case 1
Case 1 was an asymptomatic premutation carrier who had no neurological, behavioral, or cognitive symptoms by history. She had a 30 CGG repeat normal allele and 70 CGG repeat premutation allele with an activation ratio (AR) = 0.8. Her FMR1 mRNA levels were 1.31 (+/− 0.11) times normal. At age 40, she experienced an episode of Bell’s palsy. She had dry eyes resulting from cataract surgery in her early 70’s. At age 73, she developed uterine cancer and had a hysterectomy, followed by radiation treatment and chemotherapy. She died of uterine cancer at age 76, after a downhill course involving weakness and cognitive decline terminally.
Case 2
Case 2 experienced her first symptoms at the age of 56 years, presenting with expressive and receptive aphasia. The aphasia was not acute and there was no indication of a stroke. The detailed work up ruled out vascular infectious or inflammatory etiology. She had a normal and a premutation allele of 30 and 80 CGG repeats and an AR = 0.3. Her FMR1 mRNA levels were 6.06 (+/− 0.16) times normal. For this case, transcript levels were measured using frontal cortex as blood samples were not available. She subsequently developed hyperphagia, incontinence, and hallucinations. A positron emission tomography (PET) scan at age 61 showed hypoperfusion in left greater than right temporal lobes, and a brain MRI revealed mild cortical atrophy. Later, she experienced sudden falls and then swallowing difficulties. She died at 66 years of age after a progressive neurological and cognitive decline, and dementia.
Case 3
Case 3 had a history of mild FXTAS and was initially reported in Hagerman et al. (2004). She had a normal and a premutation allele of 29 and 87 CGG repeats, respectively, and an AR = 0.53. Her FMR1 mRNA level was 2.31 (+/− 0.17) times normal. She was a social worker who had 2 children with FXS. She had a long history of anxiety and she developed depression at age 75, which was treated with fluoxetine. Mild ataxia began at age 79, necessitating use of a cane. She developed an intention tremor and extremity weakness at age 82 years. She required a pacemaker in her 80s for cardiac arrhythmias. She fell and fractured her left hip at age 84. She did not have any significant cognitive deficits except for impaired memory a few months prior to death. She died at age 85 from complications related to gastrointestinal surgery for ileus.
Case 4
Case 4 was originally reported in 2008 (Greco et al., 2008), emphasizing the co-occurence diagnosis of FXTAS and multiple sclerosis (MS). The FMR1 alleles had 36 and 75 CGG repeats in size with an AR = 0.44. Her FMR1 mRNA levels were 2.80 (+/− 0.12) times normal. She died of MS at age 52, having been found to be a carrier just 2 weeks before her death after her daughter was diagnosed as a carrier by her OB/GYN physician on the basis of ovarian dysfunction. She developed neurological symptoms at age 32 years, with numbness in her arm and optic neuritis. By age 38 she had developed gait ataxia and loss of dexterity in the right hand. Her MRI demonstrated diffuse atrophy and multiple foci of increased T2 signal intensity in the periventricular and cerebellar white matter including the middle cerebellar peduncles (MCP sign). She was diagnosed with MS and treated with several regimens including methotrexate, but her symptoms gradually progressed. She developed an upper extremity intention tremor, progressive dysarthria, lower extremity numbness, and eventually spastic paraparesis and cognitive decline. She was unable to swallow and she became incontinent and bedridden before her death at age 52.
Case 5
Case 5 had normal and premutation alleles of 30 and 65 CGG repeats, respectively, and an AR = 0.28. No FMR1 mRNA levels are available. Her medical history was unremarkable beside AD later in life. Her psychiatric history included anxiety and depression. At 73 years of age she was diagnosed with AD by her neurologist and started taking donepezil. At age 77 years, she was placed in an assisted living setting and a year later she moved to an AD nursing home unit after a fall resulting in a broken ankle. She was unsteady in her walking and had tremor before death. Her downhill course was rapid. She did not have an MRI. She died as a result of AD at age 80 as result of AD.
Case 6
Case 6 was a premutation carrier; the mother of two sons with FXS, who died of FXTAS at age 65. This case has been previously described by Yachnis and colleagues (Yachnis et al., 2010). Her FMR1 mRNA levels and number of CGG repeats are unknown as only fixed tissues were available and results of previous genetic testing were unknown. She had a history of fibromyalgia symptoms starting at age 40 years with pain in her extremities, she also had hypothyroidism, and menopause at age 45. At age 58 she developed handwriting difficulties because of an intention tremor. At age 59 years her tremor worsened and involved hands and arms bilaterally. Her left hand would spasm and would close with increased tone. She also developed bladder incontinence and restless leg syndrome between age 59 and 60. She subsequently became physically weaker, with cognitive decline beginning at age 60 years, leading to a diagnosis of dementia, which was said to be rapidly progressive after age 60 (Yachnis et al., 2010). Her cognitive decline was characterized by getting lost, poor judgment and hygiene, eventually she lost the ability to converse. She required a walker at age 61 years due to ataxia, began using a wheelchair regularly at age 62, and by 63 years of age she was bedridden. Her MRI demonstrated white matter disease. She was hospitalized with aspiration pneumonia and died with respiratory failure.
Case 7
Case 7 died at age 84 years from FXTAS. She had two alleles, of 27 and 59 CGG repeats, and an AR = 0.63. Her FMR1 mRNA levels were 1.83 (+/− 0.12) times normal. She had two daughters and one son with the premutation, and three grandchildren with FXS. She was well until age 67 when she developed hypertension. She developed breast cancer in her 70s and was treated with a lumpectomy and radiation. She subsequently developed a hand tremor at age 78 with deteriorating handwriting; she was diagnosed with Parkinson’s disease and was treated with carbidopa/levodopa. Ataxia began at age 80 with frequent falling and cognitive decline that necessitated 24-hour care. By age 82 she did not recognize family members and spoke very little. She was diagnosed with dementia with Lewy Bodies (DLB); treatment with donepezil and memantine showed some clinical benefit. She gradually became weaker and was unable to walk independently after age 82 years; she then used a wheelchair consistently. On examination at age 83 she had an intention tremor, global weakness, and severe neuropathy with edema and absent vibration and pin prick sensation in her lower extremities. Her MRI demonstrated severe white matter disease in the pons, caudate, putamen, and thalamus, in addition to global cerebral atrophy. There were ischemic changes in her basal ganglia with iron deposits in her cerebellar dentate nuclei.
Case 8
Case 8 was originally reported in 2004 as the fifth case of the original case series of women with FXTAS (Hagerman et al., 2004). She had alleles of 30 CGG and 78 CGG repeats, and an AR = 0.21. Her FMR1 mRNA levels were 2.6 (+/− 0.04) times normal. She developed episodes of lightheadedness, unsteady gait, and frequent falls at age 71 years. She also developed an intention tremor of the hand that improved first with propranolol and then more markedly with primidone. Subsequently she developed numbness in her lower extremities. At age 74 she had bradykinesia, dystonia of the neck muscles, and upper extremity rigidity in addition to an intention tremor and ataxia. Her symptoms gradually worsened and she died of respiratory failure at the age of 79.
Gross and microscopic findings
Case 1
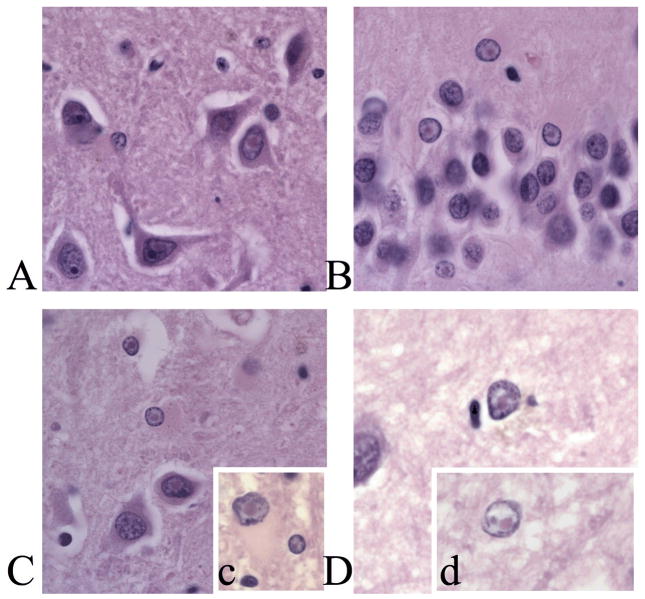
Fresh brain weight was 1231 g. Gross examination of the brain showed no pathological changes. Comprehensive microscopic examination of the brain identified intranuclear inclusions in neurons and astrocytes (Figure 1D), and mild vascular hyalinosis of white matter. Neither neurofibrillary tangles (NFTs) changes or plaque formation was seen on the modified Bielschowsky stain (Braak and CERAD stage 0).
Figure 1.
A. Intranuclear inclusions in pyramidal cells in CA3b of Case 2. B. Intranuclear inclusions in granule cells of the medial blade of the dentate gyrus of Case 2. C. Intranuclear infusions in pyramidal cells and neurons in the hilus of case 6. c. Inset, intranuclear inclusion in neuron and astrocyte in the white matter adjacent to layer VI of the frontal cortex of Case 6. D. Intranuclear inclusion in an astrocye in layer II if the frontal cortex of Case 1. d. Inset, granule cell from layer IV of the frontal cortex in Case 1. All plates are at 1000X magnification. Scale bar = 50μm.
Case 2
Total brain weight (fixed) was 1140 g. Gross examination showed global atrophy, and diffuse cerebrovascular atherosclerosis. Microscopic examination of the brain showed intranuclear inclusions as established for the histological diagnosis of FXTAS (Figure 1A,B). Loss of cortical neurons, occasional senile plaques, granulovacuolar degeneration (GVD), and NFTs were identified in frontal and temporal cortices. The hippocampus showed prominent formation of NFTs, GVD, and senile plaques in CA1. Bielschowsky stain showed abundant plaques and NFTs conforming to Braak and Braak Stage V–VI and CERAD plaque assessment as “frequent”.
Case 3
Fresh brain weight was 980 g. Gross examination showed cerebral edema, and small, scattered, atheromatous plaques in the circle of Willis. Neurons and astrocytes demonstrated intranuclear inclusions throughout the central nervous system. There was patchy pallor of subcortical, deep, and periventricular white matter evident on both H&E and myelin stains, and patchy myelin pallor involved arcuate fibers in a patchy distribution. Bielschowsky stain showed few NFTs, plaques and GVD in hippocampus, and only rare plaques in cortical sections, consistent with Braak and Braak Stage I–II and a “sparse” CERAD plaque score.
Case 4
A detailed neuropathological description was presented previously in Greco et al. (2008). In brief, gross examination showed cortical atrophy and scattered, discrete plaques of demyelination throughout the brain. Histological evaluation identified characteristic features seen with multiple sclerosis, and the intranuclear inclusions in neurons and astrocytes described in FXTAS. Bielschowsky stain showed no NFTs or plaque formation.
Case 5
Brain weight was unavailable. Gross examination of the brain showed moderate frontal lobe atrophy, ventricular enlargement, and cerebrovascular atherosclerosis. Gray matter was thinned to 3 mm in all lobes. Intranuclear inclusions were present in neurons and astrocytes. Histological features seen corresponded to Braak and Braak Stage V–VI. The CERAD plaque count showed “frequent density” of neuritic and cored plaques.
Case 6
The brain weighed 1040 gm., and showed mild cerebrovascular atherosclerosis. Mild cortical atrophy was present, favoring frontal, insular, and temporal cortices, with severe hippocampal atrophy. Neurons and astrocytes demonstrated intranuclear inclusions throughout the central nervous system (Figure 1C). Marked ventriculomegaly was seen, and some regions of white matter appeared almost translucent. Bielschowsky stain identified AD-like changes that corresponded to Braak and Braak Stage V–VI. According to CERAD criteria, plaques were “frequent” in density.
Case 7
Brain weight was unavailable. There was mild fronto-parietal cortical atrophy without ventriculomegaly, and mild spotty atherosclerosis in the Circle of Willis. Bielschowsky stain showed AD-like pathology that corresponded to Braak and Braak Stage I–II. Lewy bodies were seen in cortical areas and brainstem dopaminergic neurons.
Case 8
Brain weight was 930 gm., and showed moderate ventriculomegaly on cut section. The hippocampus was markedly atrophied. Histologic features as established for a post-mortem histological diagnosis of FXTAS were present. Bielschowsky stain identified AD-like pathological features corresponding to Braak and Braak Stage V–VI. “Moderate” numbers of plaques were present as per CERAD criteria. Severe arteriosclerosis was prominent in gray and white matter of frontal and temporal cortices.
Quantitative analysis of intranuclear inclusion number
The number of neurons and astrocytes with intranuclear inclusions (actual cell counts and percentages) are presented in Table 2 for frontal cortex, superior middle temporal gyrus, and hippocampus. No inclusions in neurons or astrocytes were observed for any of the similarly aged control subjects counted (n=6), and no inclusions were observed in the cytoplasm of neural cells in tissues from control or premutation cases. Intriguingly, the percentages of neurons and astrocytes with intranuclear inclusions were roughly equivalent in the female FXTAS cases, across all three areas evaluated (% +/− SEM) 9.03 +/− 1.62% neurons vs. 8.21 +/− 0.96% of astrocytes), which is in contrast to the findings previously reported in males (Greco et al., 2006). Importantly, there were no differences for number of cells counted among the experimental cases and control tissues counted using the same techniques.
Table 2.
Number of intranuclear inclusions (counts and percent) in neaurons and asytrocytes.
| A. Cortex
| ||||||||
|---|---|---|---|---|---|---|---|---|
| Subject | Gray Matter
|
White Matter
|
||||||
| Neurons | % | Astrocytes | % | Neurons | % | Astrocytes | % | |
| Case 1 | 24/265 | 9.06 | 25/680 | 3.68 | 3/26 | 11.54 | 30/346 | 8.67 |
| Case 2 | 16/190 | 8.40 | 2/117 | 1.80 | 1/57 | 1.75 | 21/615 | 3.41 |
| Case 3 | 2/231 | 0.80 | 5/200 | 2.50 | 3/5 | 60.00 | 19/333 | 5.71 |
| Case 4 | 0/370 | 0.00 | 14/504 | 2.80 | 6/19 | 31.58 | 12/662 | 1.81 |
| Case 5 | 6/251 | 0.02 | 10/403 | 0.02 | 1/7 | 0.14 | 9/501 | 0.02 |
| Case 6 | 62/456 | 13.60 | 240/1729 | 13.90 | 6/56 | 10.70 | 38/333 | 11.40 |
| Case 7 | 18/221 | 8.14 | 21/746 | 2.82 | 2/28 | 7.14 | 23/552 | 4.17 |
| Case 8 | 17/358 | 4.75 | 45/701 | 6.42 | 9/77 | 11.69 | 23/299 | 7.69 |
|
| ||||||||
| Mean | -- | 5.6 | -- | 4.24 | -- | 16.8 | -- | 5.36 |
| Controls | 0/361 | 0 | 0/251 | 0 | 0/16 | 0 | 0/303 | 0 |
| B. Hippocampus | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||
| Subject | Pyramidal Cell Layer (CA1–CA3)
|
Granule Cell Layer (DG)
|
Hilus
|
Superior Medial Temporal Gyrus
|
||||||||||||
| Neurons | % | Astrocytes | % | Neurons | % | Astrocytes | % | Neurons | % | Astrocytes | % | Neurons | % | Astrocytes | % | |
| Case 1 | 11/361 | 3.05 | 38/496 | 7.66 | 43/766 | 5.61 | 13/90 | 14.44 | 6/249 | 2.41 | 23/537 | 4.66 | 27/384 | 6.77 | 54/684 | 7.89 |
| Case 2 | 1/118 | 0.90 | 9/75 | 12.00 | 3/260 | 1.20 | 1/12 | 8.30 | 0/97 | 0.00 | 15/109 | 13.80 | -- | -- | ||
| Case 3 | 7/148 | 4.70 | 4/127 | 3.10 | 6/372 | 1.70 | 2/10 | 20.00 | 11/100 | 11.00 | 17/117 | 14.50 | 25/347 | 6.94 | 44/754 | 5.84 |
| Case 4 | 0/538 | 0.00 | 0/239 | 0.00 | 0/1094 | 0.00 | 0/85 | 0.00 | 0/251 | 0.00 | 0/462 | 0.00 | 26/298 | 8.72 | 82/730 | 11.23 |
| Case 5 | 8/289 | 2.77 | 17/364 | 4.67 | 28/806 | 3.47 | 17/199 | 4.26 | 3/155 | 1.94 | 6/332 | 1.81 | 16/316 | 5.06 | 44/326 | 6.06 |
| Case 6 | 79/332 | 24.00 | 157/698 | 22.00 | 100/899 | 11.00 | 12/46 | 26.00 | 97/265 | 37.00 | 205/831 | 25.00 | 46/234 | 20.00 | 146/774 | 19.00 |
| Case 7 | 36/486 | 7.41 | 9/123 | 7.32 | 27/486 | 5.56 | 13/107 | 12.15 | 14/160 | 8.75 | 14/209 | 6.70 | 20/297 | 6.73 | 61/599 | 10.18 |
| Case 8 | 26/263 | 9.89 | 72/514 | 14.01 | 68/777 | 8.75 | 6/82 | 7.32 | 54/305 | 17.70 | 101/901 | 11.21 | 52/236 | 22.03 | 50/722 | 6.93 |
|
| ||||||||||||||||
| Mean | -- | 6.59 | -- | 8.84 | -- | 4.66 | -- | 11.56 | -- | 9.85 | -- | 9.71 | -- | 11.59 | -- | 9.49 |
| Controls | 0/109 | 0.00 | 0/165 | 0.00 | 0/483 | 0.00 | 0/45 | 0.00 | 0/110 | 0.00 | 0/280 | 0.00 | ||||
DISCUSSION
The two most significant findings of this study are the presence of intranuclear inclusions in all cases and a high number of them presenting with AD neuropathological changes. Female carriers of the fragile X premutation, both with and without a FXTAS clinical diagnosis, show similar numbers of intranuclear inclusions in neurons in the cortex and hippocampus as do men with FXTAS. The number of intranuclear inclusions in astrocytes, however, was greatly reduced in female carriers relative to the levels observed in male FXTAS cases (Greco et al., 2006, Greco et al., 2002). Additionally, we found evidence of intranuclear inclusions in all cases, even though one woman (Case 1) was asymptomatic. To our knowledge this is the first report of intranuclear inclusions in a fragile X premutation female carrier that showed no clinical symptoms associated with FXTAS. There also appeared to be little to no contribution of co-morbid disorders to the number of intranuclear inclusions in any of the female premutation and FXTAS cases. Two other striking findings were the high number of women carriers with dementia (Cases 2, 5, 6, and 7), much higher than expected given previous reports, and the high level of AD-type plaque and tangle pathologies (Cases 2, 5, 6, and 8), with or without corresponding clinical AD signs.
Importantly, we have demonstrated that although the presence of intranuclear inclusions is considered a primary diagnostic criterion for FXTAS (Hagerman et al., 2004, Jacquemont et al., 2003), the presence of intranuclear inclusions may be necessary but not sufficient to lead to FXTAS symptoms. Two of the cases presented here did not have a FXTAS diagnosis at the time of death. Case 1 died of a uterine cancer for which she received radiation and chemotherapy. It is possible that the CNS trauma of the cancer treatment could have precipitated the formation of inclusions and FXTAS as was previously described in ODwyer et al. (2008) where chemotherapy lead to CNS white matter disease and clinical symptoms of FXTAS. However, the presence of the fragile X premutation appears to be sufficient for the presence of intranuclear inclusions, even when there are relatively normal levels of FMR1 mRNA, as demonstrated by the findings in Case 1. It is possible that genetic and environmental factors, including the genetic background and a favorable AR, may have played a role in the absence of FXTAS symptoms in Case 1. A high AR (0.8) was in fact measured in Case 1 in both peripheral blood leukocytes and also in brain tissue. Case 5 had a history of anxiety and depression, which are common in carriers (Bourgeois et al., 2009; Bourgeois et al., 2011; Roberts et al., 2009) and then presented with dementia with subsequent decline that included falling. Dementia has occasionally been a presenting sign of FXTAS and in Sevin et al. (2009) cognitive decline was more common in carriers compared to controls even in those without tremor and ataxia. Our cases demonstrate that the inclusions of FXTAS are more common than previously thought even in female carriers without classical symptoms of FXTAS.
Interestingly, cases 2, 5, 6, and 7 presented with dementia, which has only rarely been described in women with FXTAS. Only five women with FXTAS and dementia have been reported to date (Al-Hint et al., 2007; Karmon & Gadoth, 2008; Rodriguez-Revenga et al., 2009; Yachnis et al., 2010). Thus, the present case series greatly enriches the existing literature with these additional three cases (cases 2, 6, and 7). In three of the women we described (Cases 2, 5, and 6), there is a high likelihood that dementia was due to AD lesions according to the Diagnostic Criteria for the Neuropathological Assessment of Alzheimer’s Disease recommended by the National Institute on Aging and Reagan Institute Working Group (1997). The etiology of dementia in Case 7, who only had low levels of AD lesions, is not clear but the presence of Lewy bodies suggests a diagnosis of DLB (McKeith, 2006) or PD dementia. We have also seen the occurrence of FXTAS inclusions and Lewy bodies in one man with FXTAS (Greco et al., 2002). It is, in fact, possible that individuals with FXTAS who developed cognitive changes may get diagnosed as having AD, PD, or DLB, since dementia in FXTAS has an interesting cortical-subcortical picture which may partially mimic other neurodegenerative dementias (Seritan et al., 2008). Dementia associated with FXTAS has a characteristic profile different than other dementias, even though deficit severity may be of the order of the deficits encountered in AD (Bacalman et al., 2006, Seritan et al., 2008). Patients in more advanced stages of FXTAS (Gane et al., 2010) develop both cortical (apraxia, memory recall, visuospatial skills impairment) and subcortical (memory retrieval, bradyphrenia, latency of speech, mood and personality changes) cognitive deficits, in conjunction with the movement disorders described (ataxia, tremor, bradykinesia, parkinsonian features). Although aphasia may be present, language is typically spared early in FXTAS (Grigsby et al., 2007). Executive dysfunction is the most prominent deficit (Grigsby et al., 2008, Grigsby et al., 2007), it may occur prior to development of a full dementia and appears to mediate other cognitive deficits (Brega et al., 2008). These women described with FXTAS and neurocognitive changes presented with a variety of clinical features, making a specific dementia diagnosis difficult. It is not clear whether all the cognitively impaired women described here had FXTAS dementia, since one was also diagnosed with AD and another, with DLB. However, co-occurrence of FXTAS with other neurological disorders may exacerbate symptom severity and contribute to a faster decline.
Although further studies using a larger series are required, we hypothesize that a previously unrecognized association may exist between the FMR1 premutation and AD pathology. There may be a synergy of having both disorders because both have mitochondrial dysfunction and both have oxidative stress and these problems could be amplified when they occur together (Ross Inta et al., 2010; Napoli et al., 2011; Ye et al., 2011; Karbowski and Neutzner, 2012). However, this association could be independent of the development of FXTAS, as Case 5 developed AD without FXTAS. Because of the high frequency of female premutation carriers in the general population (1:110–259 females), the contribution of aberrant FMRP (FMR1 protein) metabolism to the development of AD should be evaluated. FMRP controls amyloid precursor protein (APP) through inhibition (Darnell et al., 2011) and FMRP may be somewhat lower in the brains of carriers (Handa et al., 2005, Qin et al., 2011) and if so APP levels may be higher in premutation carriers, as reported in Handa et al. (2005), possibly predisposing them to AD.
In summary, dementia is more common than had been previously observed in female premutation carriers, and the co-occurrence of AD-associated NFTs and plaques and FXTAS neuropathologic changes in this small series is a striking finding. Larger studies will be necessary to further substantiate this finding. The essential role of the premutation (even with normal FMR1 mRNA levels) in the inclusion formation is a cardinal finding, which will also need to be further explored in subsequent studies.
Acknowledgments
We would like to thank Dr. Anthony T. Yachnis for providing tissue from Case 6. This work was supported by National Institutes of Health grants HD036071; AG032115; UL1DE019583; AG03119; AD02274; National Center for Research Resources UL1RR024116.
Footnotes
This work is dedicated to the memory of Matteo.
References
- Consensus recommendations for the postmortem diagnosis of Alzheimer’s disease. The National Institute on Aging, and Reagan Institute Working Group on Diagnostic Criteria for the Neuropathological Assessment of Alzheimer’s Disease. Neurobiol Aging. 1997;18:S1–2. [PubMed] [Google Scholar]
- Adams JS, Adams PE, Nguyen D, Brunberg JA, Tassone F, Zhang W, Koldewyn K, Rivera SM, Grigsby J, Zhang L, DeCarli C, Hagerman PJ, Hagerman RJ. Volumetric brain changes in females with fragile X-associated tremor/ataxia syndrome (FXTAS) Neurology. 2007;69:851–859. doi: 10.1212/01.wnl.0000269781.10417.7b. [DOI] [PubMed] [Google Scholar]
- Adams PE, Adams JS, Nguyen DV, Hessl D, Brunberg JA, Tassone F, Zhang W, Koldewyn K, Rivera SM, Grigsby J, Zhang L, Decarli C, Hagerman PJ, Hagerman RJ. Psychological symptoms correlate with reduced hippocampal volume in fragile X premutation carriers. Am J Med Genet B Neuropsychiatr Genet. 2010;153B:775–785. doi: 10.1002/ajmg.b.31046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Hinti JT, Nagan N, Harik SI. Fragile X premutation in a woman with cognitive impairment, tremor, and history of premature ovarian failure. Alzheimer Dis Assoc Disord. 2007;21:262–264. doi: 10.1097/WAD.0b013e31811ec130. [DOI] [PubMed] [Google Scholar]
- Allen EG, He W, Yadav-Shah M, Sherman SL. A study of the distributional characteristics of FMR1 transcript levels in 238 individuals. Hum Genet. 2004;114:439–447. doi: 10.1007/s00439-004-1086-x. [DOI] [PubMed] [Google Scholar]
- Bacalman S, Farzin F, Bourgeois JA, Cogswell J, Goodlin-Jones BL, Gane LW, Grigsby J, Leehey MA, Tassone F, Hagerman RJ. Psychiatric phenotype of the fragile X-associated tremor/ataxia syndrome (FXTAS) in males: newly described fronto-subcortical dementia. J Clin Psychiatry. 2006;67:87–94. doi: 10.4088/jcp.v67n0112. [DOI] [PubMed] [Google Scholar]
- Berry-Kravis E, Potanos K, Weinberg D, Zhou L, Goetz CG. Fragile X-associated tremor/ataxia syndrome in sisters related to X-inactivation. Ann Neurol. 2005;57:144–147. doi: 10.1002/ana.20360. [DOI] [PubMed] [Google Scholar]
- Bourgeois JA, Coffey SM, Rivera SM, Hessl D, Gane LW, Tassone F, Greco C, Finucane B, Nelson L, Berry-Kravis E, Grigsby J, Hagerman PJ, Hagerman RJ. A review of fragile X premutation disorders: expanding the psychiatric perspective. J Clin Psychiatry. 2009;70:852–862. doi: 10.4088/JCP.08m04476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgeois JA, Seritan AL, Casillas EM, Hessl D, Schneider A, Yang Y, Kaur I, Cogswell JB, Nguyen DV, Hagerman RJ. Lifetime prevalence of mood and anxiety disorders in fragile X premutation carriers. J Clin Psychiatry. 2011;72:175–182. doi: 10.4088/JCP.09m05407blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brega AG, Goodrich G, Bennett RE, Hessl D, Engle K, Leehey MA, Bounds LS, Paulich MJ, Hagerman RJ, Hagerman PJ, Cogswell JB, Tassone F, Reynolds A, Kooken R, Kenny M, Grigsby J. The primary cognitive deficit among males with fragile X-associated tremor/ataxia syndrome (FXTAS) is a dysexecutive syndrome. J Clin Exp Neuropsychol. 2008;30:853–869. doi: 10.1080/13803390701819044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunberg JA, Jacquemont S, Hagerman RJ, Berry-Kravis E, Grigsby J, Leehey M, Tassone F, Brown WT, Greco C, Hagerman PJ. Fragile X premutation carriers: Characteristic MR imaging findings in adult males with progressive cerebellar and cognitive dysfunction. AJNR Am J Neuroradiol. 2002;23:1757–1766. [PMC free article] [PubMed] [Google Scholar]
- Chonchaiya W, Nguyen DV, Au J, Campos L, Berry-Kravis EM, Lohse K, Mu Y, Utari A, Hervey C, Wang L, Sorensen P, Cook K, Gane L, Tassone F, Hagerman RJ. Clinical involvement in daughters of men with fragile X-associated tremor ataxia syndrome. Clin Genet. 2010a;78:38–46. doi: 10.1111/j.1399-0004.2010.01448.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chonchaiya W, Tassone F, Ashwood P, Hessl D, Schneider A, Campos L, Nguyen DV, Hagerman RJ. Autoimmune disease in mothers with the FMR1 premutation is associated with seizures in their children with fragile X syndrome. Hum Genet. 2010b;128:539–548. doi: 10.1007/s00439-010-0882-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey SM, Cook K, Tartaglia N, Tassone F, Nguyen DV, Pan R, Bronsky HE, Yuhas J, Borodyanskaya M, Grigsby J, Doerflinger M, Hagerman PJ, RJH Expanded clinical phenotype of women with the FMR1 premutation. Am J Med Genet A. 2008;146A:1009–1016. doi: 10.1002/ajmg.a.32060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darnell JC, Van Driesche SJ, Zhang C, Hung KY, Mele A, Fraser CE, Stone EF, Chen C, Fak JJ, Chi SW, Licatalosi DD, Richter JD, Darnell RB. FMRP stalls ribosomal translocation on mRNAs linked to synaptic function and autism. Cell. 2011;146:247–261. doi: 10.1016/j.cell.2011.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gane LW, Iosif AM, Flynn-Wilson L, Venturino M, Hagerman RJ, Seritan AL. Assessment of patient and caregiver needs in fragile X-associated tremor/ataxia syndrome by utilizing Q-sort methodology. Aging Ment Health. 2010;14:1000–1007. doi: 10.1080/13607863.2010.501066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gokden M, Al-Hinti JT, Harik SI. Peripheral nervous system pathology in fragile X tremor/ataxia syndrome (FXTAS) Neuropathology. 2008;29:280–284. doi: 10.1111/j.1440-1789.2008.00948.x. [DOI] [PubMed] [Google Scholar]
- Greco CM, Berman RF, Martin RM, Tassone F, Schwartz PH, Chang A, Trapp BD, Iwahashi C, Brunberg J, Grigsby J, Hessl D, Becker EJ, Papazian J, Leehey MA, Hagerman RJ, Hagerman PJ. Neuropathology of fragile X-associated tremor/ataxia syndrome (FXTAS) Brain. 2006;129:243–255. doi: 10.1093/brain/awh683. [DOI] [PubMed] [Google Scholar]
- Greco CM, Hagerman RJ, Tassone F, Chudley A, Del Bigio MR, Jacquemont S, Leehey M, Hagerman PJ. Neuronal intranuclear inclusions in a new cerebellar tremor/ataxia syndrome among fragile X carriers. Brain. 2002;125:1760–1771. doi: 10.1093/brain/awf184. [DOI] [PubMed] [Google Scholar]
- Greco CM, Soontarapornchai K, Wirojanan J, Gould JE, Hagerman PJ, Hagerman RJ. Testicular and pituitary inclusion formation in fragile X associated tremor/ataxia syndrome. J Urol. 2007;177:1434–1437. doi: 10.1016/j.juro.2006.11.097. [DOI] [PubMed] [Google Scholar]
- Greco CM, Tassone F, Garcia-Arocena D, Tartaglia N, Coffey SM, Vartanian TK, Brunberg JA, Hagerman PJ, Hagerman RJ. Clinical and neuropathologic findings in a woman with the FMR1 premutation and multiple sclerosis. Arch Neurol. 2008;65:1114–1116. doi: 10.1001/archneur.65.8.1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigsby J, Brega AG, Engle K, Leehey MA, Hagerman RJ, Tassone F, Hessl D, Hagerman PJ, Cogswell JB, Bennett RE, Cook K, Hall DA, Bounds LS, Paulich MJ, Reynolds A. Cognitive profile of fragile X premutation carriers with and without fragile X-associated tremor/ataxia syndrome. Neuropsychology. 2008;22:48–60. doi: 10.1037/0894-4105.22.1.48. [DOI] [PubMed] [Google Scholar]
- Grigsby J, Brega AG, Leehey MA, Goodrich GK, Jacquemont S, Loesch DZ, Cogswell JB, Epstein J, Wilson R, Jardini T, Gould E, Bennett RE, Hessl D, Cohen S, Cook K, Tassone F, Hagerman PJ, Hagerman RJ. Impairment of executive cognitive functioning in males with fragile X-associated tremor/ataxia syndrome. Mov Disord. 2007;22:645–650. doi: 10.1002/mds.21359. [DOI] [PubMed] [Google Scholar]
- Hagerman RJ, Leavitt BR, Farzin F, Jacquemont S, Greco CM, Brunberg JA, Tassone F, Hessl D, Harris SW, Zhang L, Jardini T, Gane LW, Ferranti J, Ruiz L, Leehey MA, Grigsby J, Hagerman PJ. Fragile-X-associated tremor/ataxia syndrome (FXTAS) in females with the FMR1 premutation. Am J Hum Genet. 2004;74:1051–1056. doi: 10.1086/420700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagerman RJ, Leehey M, Heinrichs W, Tassone F, Wilson R, Hills J, Grigsby J, Gage B, Hagerman PJ. Intention tremor, parkinsonism, and generalized brain atrophy in male carriers of fragile X. Neurology. 2001;57:127–130. doi: 10.1212/wnl.57.1.127. [DOI] [PubMed] [Google Scholar]
- Hamlin A, Liu Y, Nguyen DV, Tassone F, Zhang L, Hagerman RJ. Sleep apnea in fragile X premutation carriers with and without FXTAS. Am J Med Genet B Neuropsychiatr Genet. 2011;156B:923–928. doi: 10.1002/ajmg.b.31237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handa V, Goldwater D, Stiles D, Cam M, Poy G, Kumari D, Usdin K. Long CGG-repeat tracts are toxic to human cells: implications for carriers of Fragile X premutation alleles. FEBS Letters. 2005;579:2702–2708. doi: 10.1016/j.febslet.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Harding AJ, Kril JJ, Halliday GM. Practical measures to simplify the Braak tangle staging method for routine pathological screening. Acta Neuropathol. 2000;99:199–208. doi: 10.1007/pl00007425. [DOI] [PubMed] [Google Scholar]
- Hunsaker MR, Greco CM, Spath MA, Smits AP, Navarro CS, Tassone F, Kros JM, Severijnen LA, Berry-Kravis EM, Berman RF, Hagerman PJ, Willemsen R, Hagerman RJ, Hukema RK. Widespread non-central nervous system organ pathology in fragile X premutation carriers with fragile X-associated tremor/ataxia syndrome and CGG knock-in mice. Acta Neuropathol. 2011;122:467–479. doi: 10.1007/s00401-011-0860-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacquemont S, Farzin F, Hall D, Leehey M, Tassone F, Gane L, Zhang L, Grigsby J, Jardini T, Lewin F, Berry-Kravis E, Hagerman PJ, Hagerman RJ. Aging in individuals with the FMR1 mutation. Am J Ment Retard. 2004a;109:154–164. doi: 10.1352/0895-8017(2004)109<154:AIIWTF>2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacquemont S, Hagerman RJ, Leehey M, Grigsby J, Zhang L, Brunberg JA, Greco C, Des Portes V, Jardini T, Levine R, Berry-Kravis E, Brown WT, Schaeffer S, Kissel J, Tassone F, Hagerman PJ. Fragile X premutation tremor/ataxia syndrome: molecular, clinical, and neuroimaging correlates. Am J Hum Genet. 2003;72:869–878. doi: 10.1086/374321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacquemont S, Hagerman RJ, Leehey MA, Hall DA, Levine RA, Brunberg JA, Zhang L, Jardini T, Gane LW, Harris SW, Herman K, Grigsby J, Greco CM, Berry-Kravis E, Tassone F, Hagerman PJ. Penetrance of the fragile X-associated tremor/ataxia syndrome in a premutation carrier population. JAMA. 2004b;291:460–469. doi: 10.1001/jama.291.4.460. [DOI] [PubMed] [Google Scholar]
- Jacquemont S, Orrico A, Galli L, Sahota PK, Brunberg JA, Anichini C, Leehey M, Schaeffer S, Hagerman RJ, Hagerman PJ, Tassone F. Spastic paraparesis, cerebellar ataxia, and intention tremor: a severe variant of FXTAS? J Med Genet. 2005;42:e14. doi: 10.1136/jmg.2004.024190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karbowski M, Neutzner A. Neurodegeneration as a consequence of failed mitochondrial maintenance. Acta Neuropathol. 2012;123:157–171. doi: 10.1007/s00401-011-0921-0. [DOI] [PubMed] [Google Scholar]
- Karmon Y, Gadoth N. Fragile X associated tremor/ataxia syndrome (FXTAS) with dementia in a female harbouring FMR1 premutation. J Neurol Neurosurg Psychiatry. 2008;79:738–739. doi: 10.1136/jnnp.2007.139642. [DOI] [PubMed] [Google Scholar]
- Kenneson A, Zhang F, Hagedorn CH, Warren ST. Reduced FMRP and increased FMR1 transcription is proportionally associated with CGG repeat number in intermediate-length and premutation carriers. Hum Mol Genet. 2001;10:1449–1454. doi: 10.1093/hmg/10.14.1449. [DOI] [PubMed] [Google Scholar]
- Leehey MA, Legg W, Tassone F, Hagerman R. Fibromyalgia in fragile X mental retardation 1 gene premutation carriers. Rheumatology (Oxford) 2011;50:2233–2236. doi: 10.1093/rheumatology/ker273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louis E, Moskowitz C, Friez M, Amaya M, Vonsattel JP. Parkinsonism, dysautonomia, and intranuclear inclusions in a fragile X carrier: a clinical-pathological study. Mov Disord. 2006;21:420–425. doi: 10.1002/mds.20753. [DOI] [PubMed] [Google Scholar]
- McKeith IG. Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the Consortium on DLB International Workshop. J Alzheimers Dis. 2006;9:417–423. doi: 10.3233/jad-2006-9s347. [DOI] [PubMed] [Google Scholar]
- Mendez MF, Cummings JL. Dementia: A Clinical Approach. Butterworth Heinemann; Philadelphia: 2003. [Google Scholar]
- Mirra SS, Heyman A, McKeel D, Sumi SM, Crain BJ, Brownlee LM, Vogel FS, Hughes JP, van Belle G, Berg L. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD) Part II. Standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology. 1991;41:479–486. doi: 10.1212/wnl.41.4.479. [DOI] [PubMed] [Google Scholar]
- Napoli E, Ross-Inta C, Wong S, Omanska-Klusek A, Barrow C, Iwahashi C, Garcia-Arocena D, Sakaguchi D, Berry-Kravis E, Hagerman R, Hagerman PJ, Giulivi C. Altered zinc transport disrupts mitochondrial protein processing/import in fragile X-associated tremor/ataxia syndrome. Hum Mol Genet. 2011;20:3079–3092. doi: 10.1093/hmg/ddr211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Dwyer JP, Clabby C, Crown J, Barton DE, Hutchinson M. Fragile X-associated tremor/ataxia syndrome presenting in a woman after chemotherapy. Neurology. 2005;65:331–332. doi: 10.1212/01.wnl.0000168865.36352.53. [DOI] [PubMed] [Google Scholar]
- Oostra BA, Willemsen R. FMR1: a gene with three faces. Biochim Biophys Acta. 2009;1790:467–477. doi: 10.1016/j.bbagen.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peprah E, He W, Allen E, Oliver T, Boyne A, Sherman SL. Examination of FMR1 transcript and protein levels among 74 premutation carriers. J Hum Genet. 2010;55:66–68. doi: 10.1038/jhg.2009.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin M, Entezam A, Usdin K, Huang T, Liu ZH, Hoffman GE, Smith CB. A mouse model of the fragile X premutation: effects on behavior, dendrite morphology, and regional rates of cerebral protein synthesis. Neurobiol Dis. 2011;42:85–98. doi: 10.1016/j.nbd.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raske C, Hagerman PJ. Molecular pathogenesis of fragile X-associated tremor/ataxia syndrome. J Investig Med. 2009;57:825–829. doi: 10.231/JIM.0b013e3181be329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JE, Bailey DB, Jr, Mankowski J, Ford A, Sideris J, Weisenfeld LA, Heath TM, Golden RN. Mood and anxiety disorders in females with the FMR1 premutation. Am J Med Genet B Neuropsychiatr Genet. 2009;150B:130–139. doi: 10.1002/ajmg.b.30786. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Revenga L, Madrigal I, Pagonabarraga J, Xuncla M, Badenas C, Kulisevsky J, Gomez B, Mila M. Penetrance of FMR1 premutation associated pathologies in fragile X syndrome families. Eur J Hum Genet. 2009;17:1359–1362. doi: 10.1038/ejhg.2009.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross-Inta C, Omanska-Klusek A, Wong S, Barrow C, Garcia-Arocena D, Iwahashi C, Berry-Kravis E, Hagerman RJ, Hagerman PJ, Giulivi C. Evidence of mitochondrial dysfunction in fragile X-associated tremor/ataxia syndrome. Biochemical J. 2010;429:545–552. doi: 10.1042/BJ20091960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellier C, Rau F, Liu Y, Tassone F, Hukema RK, Gattoni R, Schneider A, Richard S, Willemsen R, Elliott DJ, Adams JS. Sam68 sequestration and partial loss of function are associated with splicing alterations in FXTAS patients. EMBO J. 2010;29:1248–1261. doi: 10.1038/emboj.2010.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seritan AL, Nguyen DV, Farias ST, Hinton L, Grigsby J, Bourgeois JA, Hagerman RJ. Dementia in fragile X-associated tremor/ataxia syndrome (FXTAS): Comparison with Alzheimer’s disease. Am J Med Genet B Neuropsychiatr Genet. 2008;147B:1138–1144. doi: 10.1002/ajmg.b.30732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevin M, Kutalik Z, Bergman S, Vercelletto M, Renou P, Lamy E, Vingerhoets FJ, Di Virgilio G, Boisseau P, Bezieau S, Pasquier L, Rival JM, Beckmann JS, Damier P, Jacquemont S. Penetrance of marked cognitive impairment in older male carriers of the FMR1 gene premutation. J Med Genet. 2009;46:818–824. doi: 10.1136/jmg.2008.065953. [DOI] [PubMed] [Google Scholar]
- Tassone F, Adams J, Berry-Kravis EM, Cohen SS, Brusco A, Leehey MA, Li L, Hagerman RJ, Hagerman PJ. CGG repeat length correlates with age of onset of motor signs of the fragile X-associated tremor/ataxia syndrome (FXTAS) Am J Med Genet. 2007;144:566–569. doi: 10.1002/ajmg.b.30482. [DOI] [PubMed] [Google Scholar]
- Tassone F, Berry-Kravis EM. The Fragile X-Associated Tremor Ataxia Syndrome (FXTAS) Springer; 2010. [Google Scholar]
- Tassone F, Hagerman RJ, Garcia-Arocena D, Khandjian EW, Greco CM, Hagerman PJ. Intranuclear inclusions in neural cells with premutation alleles in fragile X associated tremor/ataxia syndrome. J Med Genet. 2004;41:e43. doi: 10.1136/jmg.2003.012518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tassone F, Hagerman RJ, Iklé DN, Dyer PN, Lampe M, Willemsen R, Oostra BA, Taylor AK. FMRP expression as a potential prognostic indicator in fragile X syndrome. Am J Med Genet. 1999;84:250–261. [PubMed] [Google Scholar]
- Tassone F, Hagerman RJ, Taylor AK, Gane LW, Godfrey TE, Hagerman PJ. Elevated levels of FMR1 mRNA in carrier males: a new mechanism of involvement in the fragile-X syndrome. Am J Hum Genet. 2000;66:6–15. doi: 10.1086/302720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tassone F, Pan R, Amiri K, Taylor AK, Hagerman PJ. A rapid polymerase chain reaction-based screening method for identification of all expanded alleles of the fragile X (FMR1) gene in newborn and high-risk populations. J Mol Diagn. 2008;10:43–49. doi: 10.2353/jmoldx.2008.070073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yachnis AT, Roth HL, Heilman KM. Fragile X dementia Parkinsonism Syndrome (FXDPS) Cogn Behav Neurol. 2010;23:39–43. doi: 10.1097/WNN.0b013e3181b6e1b9. [DOI] [PubMed] [Google Scholar]
- Ye X, Tai W, Zhang D. The early events of Alzheimer’s disease pathology: from mitochondrial dysfunction to BDNF axonal transport deficits. Neurobiol Aging. 2011 doi: 10.1016/j.neurobiolaging.2011.11.004. [DOI] [PubMed] [Google Scholar]
- Zhang L, Coffey S, Lua LL, Greco CM, Schafer JA, Brunberg J, Borodyanskaya M, Agius MA, Apperson M, Leehey M, Tartaglia N, Tassone F, Hagerman PJ, Hagerman RJ. FMR1 premutation in females diagnosed with multiple sclerosis. J Neurol Neurosurg Psychiatry. 2009;80:812–814. doi: 10.1136/jnnp.2008.160960. [DOI] [PubMed] [Google Scholar]