Sir,
There are few reports of anterior uveal non-Hodgkin lymphomas (NHL), which mainly involve the iris.1, 2, 3, 4, 5 Uveal lymphomas affecting almost exclusively the ciliary body (CB) are extremely rare. We describe a case of B-NHL with 360° infiltration of the CB without significant iris or choroidal involvement. To our knowledge, such a case of CB lymphoma with a ‘ring-like' pattern mimicking a melanoma has not been described previously.
Case report
An asymptomatic 76-year-old man was referred to our hospital with a suspected amelanotic melanoma of the CB of the right eye after a routine eye check-up. Vision was 6/12 in the affected eye and 6/6 in the fellow eye.
Anterior segment examination of the right eye revealed the presence of a small hyphema with raised intraocular pressure (IOP: 31 mm Hg) (Figure 1a). Gonioscopy showed a closed angle inferiorly without any evidence of iris neovascularization. Fundus examination showed a few scattered retinal haemorrhages associated with white chorioretinal infiltrates. Ultrasound showed 360° infiltration of the CB with acoustic solidity but low internal reflectivity (Figure 1b). The tumour had a maximum thickness of 1.5 mm and antero-posterior diameter of 1.3 mm. Examination of the fellow eye was unremarkable and IOP was within normal limits.
Figure 1.
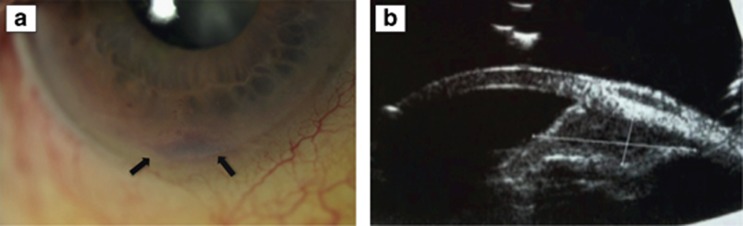
An otherwise healthy 76-year-old man with 2-year history of blurred vision and increased intraocular pressure in the right eye. (a) Anterior segment photograph shows a small hyphema (arrowheads) without visible tumour. (b) B-scan ultrasonography reveals 360° infiltration of the ciliary body with acoustic solidity but low internal reflectivity.
CB biopsy was performed through a limited cyclectomy at the thickest tumour area at 6 o'clock that was measuring 1.5 mm on U/S. Limited cyclectomy was chosen instead of fine needle aspiration biopsy to assure an adequate tissue sample for histologic evaluation.
The histological and immunohistological features disclosed an extranodal marginal zone B-cell lymphoma (Figure 2). This diagnosis was confirmed using PCR for both the heavy and light immunoglobulin chains.
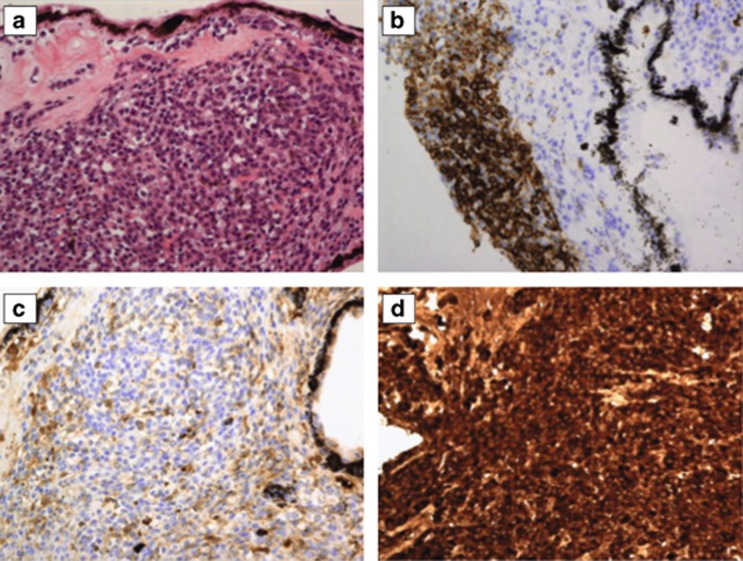
Figure 2.
Histopathological examination was performed on a trans-scleral incisional biopsy specimen of the ciliary body tumour. (a) Hematoxylin–eosin-stained section showing a diffuse infiltrate of small plasma cells and lymphocytes. (b) Immunohistochemical stain for CD20 showing that the infiltrate consists predominantly of B cells. (c, d) Immunohistochemical stain for immunoglobulin light chains showing monotypical expression for kappa; monoclonality was confirmed using IgKappa-PCR. Taken together these features are consistent with extranodal marginal zone B-cell lymphoma of the ciliary body.
Staging investigations—for example, brain MRI, CT chest, abdomen, iliac crest, and spinal tap—were negative for malignancy. The patient received a low dose external beam radiotherapy (EBR) to the right eye over 12 days. On review 3 months later, the tumour had regressed completely. At the 6-months follow-up, there were no signs of tumour, while the visual acuity of the affected eye was 6/48 as the result of a moderate cataract.
Comment
The majority of reported cases of B-cell uveal NHL were either mainly choroidal or iridal tumours, with secondary involvement of the CB.1 In 2004, Ahmed et al1 reported a case of 360° iris-CB B-cell lymphoma masquerading as post-cataract uveitis. However, there was significant involvement of the iris, which would actually suggest that the iris was the primary site of the tumour. In 2012, Mashayekhi et al2 reported three cases of primary iris-CB B-cell lymphoma. One case had significant choroidal involvement, whereas in the other two cases histological analysis revealed a high-grade large B-cell NHL, in contrast to the tumour in our patient.
In conclusion, the differential diagnosis of a CB tumour should include lymphoma even in the absence of significant iris and/or choroidal involvement. Ultrasound shows low acoustic reflectivity. Biopsy with histomorphological examination is necessary to establish the diagnosis. EBR may induce rapid and complete regression.
The authors declare no conflict of interest.
References
- Ahmed M, Androudi S, Brazitikos P, Paredes I, Foster CS. 360 degrees iris-ciliary body B-cell lymphoma masquerading as post-cataract uveitis. Semin Ophthalmol. 2004;19 (3-4:127–129. doi: 10.1080/08820530490882706. [DOI] [PubMed] [Google Scholar]
- Mashayekhi A, Shields CL, Shields JA. Iris involvement by lymphoma: a review of 13 cases. Clin Experiment Ophthalmol. 2013;41 (1:19–26. doi: 10.1111/j.1442-9071.2012.02811.x. [DOI] [PubMed] [Google Scholar]
- Yamada K, Hirata A, Kimura A, Tanihara H. A case of primary B-cell type non-Hodgkin lymphoma originating in the iris. Am J Ophthalmol. 2003;136 (2:380–382. doi: 10.1016/s0002-9394(03)00324-6. [DOI] [PubMed] [Google Scholar]
- Raju VK, Green WR. Reticulum cell sarcoma of the uvea. Ann Ophthalmol. 1982;14 (6:555–560. [PubMed] [Google Scholar]
- Coupland SE, Damato B. Understanding intraocular lymphomas. Clin Experiment Ophthalmol. 2008;36 (6:564–578. doi: 10.1111/j.1442-9071.2008.01843.x. [DOI] [PubMed] [Google Scholar]