Abstract
Aims
To investigate the characteristics and prognoses of golf ball-related ocular injuries (GROIs) using standardized terminology, classification, and scoring systems.
Methods
Twenty-two GROI patients were assessed using the Birmingham Eye Trauma Terminology, Ocular Trauma Classification Group (OTCG) classification, and Ocular Trauma Score. Globe preservation and final visual acuity (FVA) were assessed according to the injury severity categorical designation.
Results
Fourteen patients were injured on golf courses and eight on driving ranges. Nine patients (40.9%) had open-globe injuries (five ruptures (22.7%), four penetrating injuries (18.2%)). All rupture cases required enucleation, whereas penetrating injury cases did not (the FVA ranged from 20/100 to no light perception). In open-globe injuries, wearing glasses protected against rupture (P=0.008). Thirteen patients sustained closed-globe injuries that were accompanied by lens subluxation (38.5%), choroidal rupture (30.8%), macular commotio retinae (38.5%), and traumatic optic neuropathy (7.7%). Twelve (54.5%) patients had orbital wall fractures. The mean number of related surgeries required was 1.5±1.7 across all patients.
Conclusion
Eyes with GROIs had devastating FVA and globe preservation status, especially those with open-globe injuries. Observing golf rules and improving driving-range facilities are essential for preventing GROIs. Protective eyewear may reduce ocular damage from GROIs, especially globe rupture.
Keywords: golf, ocular injury, terminology, visual outcome, anatomic outcome
Introduction
Golf is a popular sport among people of all ages in many countries, including Korea. According to the report from the Korea Golf Association, about 3 million golfers in Korea played approximately 26 million games in 2012. Although golf-related ocular injuries (GROIs) were uncommon and accounted for only 1.5–5.6% of sports-related ocular traumas,1, 2, 3, 4, 5 GROIs are often devastating, requiring enucleation in numerous cases.4, 5, 6, 7, 8, 9, 10, 11, 12 Although previous studies provided informative results regarding clinical courses and prognosis of GROIs, the injury definition terms were not standardized (eg, rupture injury, penetrating injury) and were used ambiguously between studies.13, 14, 15 In addition, no study has assessed and/or categorized GROIs in a way that is predictive of visual and anatomical prognoses. Here, we examined both characteristics and prognoses of GROIs by using the Birmingham Eye Trauma Terminology (BETT),14 the Ocular Trauma Classification Group (OTCG) classification,13 and the Ocular Trauma Score (OTS) system16to assess injury severity and predict visual outcomes. We found 22 patients who experienced GROIs during the past 10 years and underwent treatments in Korea. To our knowledge, the present study is the largest GROI case series reported and is the first to report in an East Asian country, one of the most populated regions in the world.
Materials and methods
This retrospective observational study included patients with GROIs who presented at either of two tertiary referral hospitals (Seoul National University Hospital and Seoul National University Bundang Hospital) between 2004 and 2013. This study was approved by the institutional review boards of both hospitals and adhered to the tenets of the Declaration of Helsinki. Demographics, trauma characteristics (ie, injury mechanism, size, location, and extent), initial visual acuity (VA), eyewear use at the time of injury, and the presence of a GROI-related ocular/adnexal injury (eg, retinal detachment, choroidal rupture, eyelid injury, orbital wall fracture, canalicular injury, etc.) or afferent pupillary defect were evaluated. Related surgical procedures, follow-up duration, and final visual acuity (FVA) were also recorded. Ocular injuries were classified in accordance with the BETT as open- and closed-globe injuries. Closed-globe injuries were further categorized into contusion and lamellar laceration, whereas open-globe injuries were further classified into laceration and rupture. Last, lacerations were categorized into three subgroups: penetrating, perforating, and intraocular foreign body.14 The location of open-globe injuries was categorized in accordance with OTCG classifications as follows: zone I injuries were limited to the cornea, zone II injuries involved the eyewall (BETT defines the eyewall as the sclera and cornea) no more than 5 mm posterior to the limbus, and zone III injuries involved the eyewall posterior to zone II.13The OTS was calculated in all patients, in accordance with the OTS study.16 The OTS variables have numerical values, and include initial vision, rupture, endophthalmitis, perforating or penetrating injury, retinal detachment, and afferent pupillary defect (Table 1). Totalling these individual values at presentation determined the overall OTS and OTS category. The categorical distribution and the conventional OTS were compared using the Fisher's exact test in our study. Statistical significance was defined as P<0.05.
Table 1. Calculation of the ocular trauma score: variables and raw scores.
| Raw points | |
|---|---|
| Initial visual acuity | |
| NLP | 60 |
| LP/HM | 70 |
| 1/200–19/200 | 80 |
| 20/200–20/50 | 90 |
| ≥20/40 | 100 |
| Rupture | −23 |
| Endophthalmitis | −17 |
| Perforating or penetrating injury | −14 |
| Retinal detachment | −11 |
| Afferent pupillary defect | −10 |
Abbreviations: HM, hand motion; LP, light perception; NLP, no light perception.
Results
A total of 22 patients (16 men (72.7%) and 6 women (27.3%)) were enrolled. All patients had unilateral GROIs and the mean age was 48.5±15.0 years (range: 26–72 years). Fourteen patients (63.6%) were injured on golf courses. Of these, nine patients (64.3%) were players, three patients (21.4%) were caddies, and two patients (14.3%) were lawn-care-service employees. The other eight patients (36.4%) were injured on driving ranges (seven players and one employee). Seven patients were injured when their own golf balls ricocheted off a column or wall on driving ranges and one was hit after a ball ricocheted off a nearby tree on the golf course.
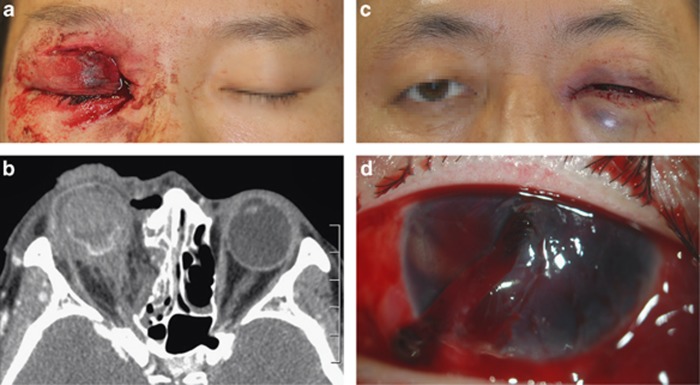
The injury was an open-globe injury in nine patients (40.9%), five (22.7%) of whom were classified as rupture injuries in zone III. Five cases experienced a rupture by direct impact of the golf ball, and they were not wearing glasses at the time of injury. The remaining four cases (18.2%) were classified as penetrating injuries in varying zones (one case with zone I injury, one case with zone II injury, and two cases with zone III injuries). All penetrating injuries occurred while the patient was wearing glasses. The eyewear broke on impact, which caused the penetrating injuries. In cases with open-globe injuries, wearing glasses was associated with preventing globe rupture (P=0.008 by the Fisher exact test). Two open-globe injury cases are shown in Figure 1, one (Case 1) with a rupture injury (Figures 1a and b) and the other (Case 6) with a penetrating injury (Figures 1c and d). All patients with an open-globe injury underwent the surgical repair of eyewall injuries.14 One patient (Case 2) had a failed primary rupture repair and the surgery was converted to a primary evisceration. All patients with a rupture injury also eventually underwent evisceration despite vitreoretinal surgeries to treat posterior complications. All patients with penetrating injuries had a preserved globe, but two eyes with zone III injuries developed phthisis bulbi. The FVA of patients with penetrating injuries ranged between 20/100 and no light perception.
Figure 1.
Images of two open-globe injuries (Cases 1 and 6). (a, b) Images of Case 1, a rupture injury that occurred without the use of eyewear. (c, d) Images of Case 6, a penetrating injury that occurred with the use of eyewear. (a) Eyelid photo showing a laceration and injury to the canaliculus. (b) Orbit computed tomography showing a ruptured globe and medial orbital wall fractures. (c) Eyelid photo showing bruising. (d) Anterior segment photography showing a full thickness corneoscleral laceration with iris prolapse. The injury was caused by broken glasses.
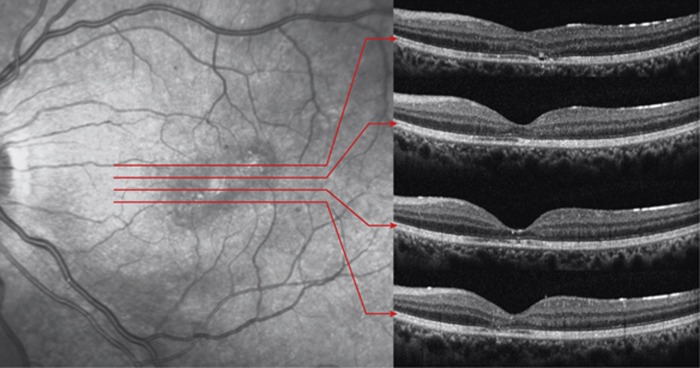
The remaining 13 patients (59.1%) sustained closed-globe injuries with contusion, and the globe could be preserved. All contusion cases had a hyphema of varying severity at the time of presentation. Four patients had choroidal ruptures, five had commotio retinae, and one patient had traumatic optic neuropathy. Five patients had a crystalline lens subluxation and underwent intraocular lens scleral fixation surgery with vitrectomy. Crystalline lens subluxation did not influence the FVA, but the FVA was dependent upon posterior segment status. The disrupted retinal photoreceptor layer after the patient experienced commotio retinae in the injured eye is shown in Figure 2 (Case 14). Injured patients with contusions had a FVA ranging between 20/20 and hand motion. In cases with closed-globe injuries, wearing glasses was not associated with either visual or anatomic outcome.
Figure 2.
Infrared reflectance (IR) image and corresponding optical coherence tomography (OCT) images of a contusion injury and subsequent commotion retinae (Case 14). The IR image showed diffuse macular hypo-reflectance and focal hyper-reflective lesions therein. The OCT images revealed the following: (1) the cone outer segment tip (COST) defects corresponded to hypo-reflective areas on the IR image and (2) the reflectivity loss of multi-layers in the COST, inner and outer segment junction, and external limiting membrane corresponded to hyper-reflective lesions on IR image.
Orbital wall fractures were observed in 12 patients (54.5%), 5 (41.7%) of whom underwent reduction surgery for orbital wall fractures. The use of eyewear was not associated with orbital wall fractures or the need for reduction surgery. Four patients (18.2%) experienced canalicular injuries and underwent necessary reduction surgeries.
The mean number of related surgeries required was 1.5±1.7 across all patients. Surgeries included primary eyewall repair, eyelid laceration repair, vitreoretinal surgery, orbital wall fracture reduction, and canalicular injury repair. Patients with open-globe injuries underwent an average of 3.00±1.6 surgeries, and patients with closed-globe injuries underwent an average of 0.5±0.7 surgeries (P=0.008). Wearing glasses was not associated with the number of surgeries (P=0.343). If patients underwent two or more procedures in a single surgery, the number of surgeries was counted as 1.
The OTS scores and OTS categories were calculated and these are presented in Table 2. When the FVAs were striated according to OTS categories (Table 3), the results of the present study were similar to those reported in the OTS study.16
Table 2. Characteristics of patients with golf ball-related ocular injuries.
| No. | Initial VA | Eyewear | BETT | Open-globe injurya | OTS (cat.) | Place | Self-injuryb | Eyeball preservationc | Final VA | Final FU (weeks) | OWF/reduction surgery | Can. injury | Sx | Notes | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F/35 | NLP | No | Rup. | ZoneIII | 26 (1) | Fieldd | No | Failed (105D) | — | 47 | Yes/yes | Yes | 5 | |
| 2 | M/47 | NLP | No | Rup. | ZoneIII | 37 (1) | Field | No | Failed (0D) | — | 68 | Yes/yes | Yes | 2 | |
| 3 | F/62 | NLP | No | Rup. | ZoneIII | 37 (1) | Field | No | Failed (99D) | — | 25 | Yes/yes | No | 5 | |
| 4 | F/54 | NLP | No | Rup. | ZoneIII | 37 (1) | Field | No | Failed (2D) | — | 19 | Yes/no | No | 2 | |
| 5 | M/37 | NLP | No | Rup. | ZoneIII | 37 (1) | Rangee | Yes | Failed (56D) | — | 14 | Yes/no | No | 2 | |
| 6 | M/58 | NLP | Yes | Penet. | ZoneIII | 46 (2) | Range | Yes | Preserved | NLP | 54 | Yes/no | No | 3 | Phthisis bulbi at last FU |
| 7 | F/30 | NLP | Yes | Penet. | ZoneIII | 46 (2) | Field | No | Preserved | NLP | 45 | Yes/yes | No | 4 | Phthisis bulbi at last FU |
| 8 | F/27 | HM | No | Contu. | — | 49 (2) | Field | No | Preserved | HM | 63 | No | No | 1 | RD, subfoveal choroidal rup. |
| 9 | M/27 | HM | Yes | Penet. | ZoneI | 56 (2) | Range | No | Preserved | 20/200 | 48 | Yes/yes | No | 4 | Traumatic macular hole |
| 10 | M/64 | HM | No | Contu. | — | 59 (2) | Range | Yes | Preserved | 20/100 | 6 | No | No | 1 | RD, SRH |
| 11 | M/68 | HM | Yes | Contu. | — | 70 (3) | Field | No | Preserved | 20/20 | 26 | No | No | 1 | Lens subluxation |
| 12 | M/46 | HM | No | Contu. | — | 70 (3) | Field | Yes | Preserved | 20/20 | 1 | No | No | 0 | |
| 13 | M/64 | HM | No | Contu. | — | 70 (3) | Field | No | Preserved | 20/40 | 47 | Yes/no | No | 1 | Lens subluxation, commotio retinae |
| 14 | M/30 | HM | No | Contu. | — | 70 (3) | Range | Yes | Preserved | 20/100 | 13 | Yes/no | Yes | 2 | Lens subluxation, commotio retinae |
| 15 | M/56 | 20/250 | No | Contu. | — | 70 (3) | Field | No | Preserved | 20/250 | 56 | No | No | 0 | Traumatic optic neuropathy |
| 16 | M/26 | 20/80 | Yes | Penet. | ZoneII | 76 (3) | Range | Yes | Preserved | 20/100 | 20 | No | Yes | 0 | |
| 17 | M/72 | 20/500 | No | Contu. | — | 80 (3) | Field | No | Preserved | 20/20 | 8 | No | No | 0 | |
| 18 | M/67 | 20/63 | Yes | Contu. | — | 90 (4) | Field | No | Preserved | 20/20 | 1 | No | No | 1 | Lens subluxation |
| 19 | F/42 | 20/20 | No | Contu. | — | 100 (5) | Field | No | Preserved | 20/20 | 6 | Yes/no | No | 0 | Peripheral choroidal rup. |
| 20 | M/56 | 20/20 | No | Contu | — | 100 (5) | Range | Yes | Preserved | 20/20 | 23 | Yes/no | No | 1 | Lens subluxation, Nasal choroidal rup. |
| 21 | M/56 | 20/40 | Yes | Contu | — | 100 (5) | Field | No | Preserved | 20/40 | 2 | No | No | 0 | Parafoveal choroidal rup. |
| 22 | M/42 | 20/32 | Yes | Contu | — | 100 (5) | Range | Yes | Preserved | 20/20 | 7 | No | No | 0 |
Abbreviations: BETT, Birmingham Eye Trauma Terminology classification; Can., canalicular; Contu., contusion; Cat., category; FU, follow-up; HM, hand motion; NLP, no light perception; OTS, Ocular Trauma Score; OWF, orbital wall fracture; Penet., penetrating injury; RD, retinal detachment; Rup., rupture; SRH, subretinal hemorrhage; Sx, number of surgeries required; VA, visual acuity.
The injury location according to the Ocular Trauma Classification Group.
Patients injured by their own golf ball that ricocheted off a column, wall, or tree.
The number in parentheses indicates the number of days that elapsed after presentation that evisceration was performed.
Golf course.
Golf driving range.
Table 3. Final visual acuity, as assessed with the Ocular Trauma Score (OTS): comparison with OTS study results.
| OTS category | Number (present study/OTS study) | Final visual acuity % in the present study/% in the OTS studya (number in the present study) | P valueb | ||||
|---|---|---|---|---|---|---|---|
| |
|
NLP |
LP/HM |
1/200–19/200 |
20/200–20/50 |
≥20/40 |
|
| 1 | 5/215 | 100/74 (n=5) | 0/15 | 0/7 | 0/3 | 0/1 | P=1.000 |
| 2 | 5/374 | 40/27 (n=2) | 20/26 (n=1) | 0/18 | 40/15 (n=2) | 0/15 | P=0.460 |
| 3 | 7/808 | 0/2 | 0/11 | 14/15 (n=1) | 2 (28.6%) | 57/41 (n=4) | P=0.910 |
| 4 | 1/378 | 0/1 | 0/2 | 0/3 | 0/22 | 100/73 (n=1) | P=1.000 |
| 5 | 4/376 | 0/0 | 0/1 | 0/1 | 0/5 | 100/94 (n=4) | P=1.000 |
Abbreviations: HM, hand motion; LP, light perception; NLP, no light perception.
The percentage in each column may not equal 100% because of rounding.
P values were calculated using the Fisher's exact test to compare the likelihood of final visual acuities between the present study and the OTS study.
Discussion
The present study showed devastating results of GROIs, similar to previous reports.4, 5, 6, 7, 8, 9, 10, 11, 12 Of the 22 patients described herein, 40.9% had open-globe injuries and 22.7% eventually underwent enucleation. The BETT provided a simple, comprehensive, and unambiguous method for describing GROIs. Although rupture was often defined as any type of open-globe injury in many studies, open-globe injuries can be classified as either a rupture or a laceration according to the BETT. A rupture is defined as a full-thickness wound of the eyewall caused by a blunt object, and a laceration is defined as a full-thickness wound of the eyewall caused by a sharp object.14 Among the open-globe injuries in our study, all rupture cases eventually underwent enucleation, whereas no cases of penetrating injury required enucleation. In addition, 50% (2 cases) of penetrating cases had preserved vision, with the VA ranging between 20/100 and 20/200. Eyewear, which broke in all cases, may have absorbed some of the travelling-golf ball's energy, and helped protect the eye and preserve the globe, even though the broken glasses caused the penetrating injuries. Burnstine and Elner8 stated that eyes with long wounds (≥10mm in length) were more likely to require enucleation, but we did not find this. Three of our cases with penetrating injuries (Cases 6, 7, and 16) had full-thickness lacerations well over 10 mm in length (19, 26, and 11 mm, respectively) and enucleation was avoided in all three cases. In addition, the OGCT classification system provided an easy, simple method for describing both the location and the extent of an open-globe injury. The severity of the open-globe injury could be assessed without a verbose laceration length and location description. In the present study, vision could not be preserved in zone III open-globe injuries and 71.4% (5 of 7 cases) of zone III cases underwent enucleation. The remaining two cases eventually developed phthisis bulbi.
At 42.67 mm in diameter, the golf ball is 3–8 mm larger than the orbital entrance, and the corneal apex is 13–18.5 mm anterior to the orbital rim.17, 18, 19 A golf ball is hard and dense and travels at high velocities. If ocular injury occurs by direct impact while the golf ball is traveling at a high velocity, globe rupture is hard to avoid.7, 8, 9, 10, 11 Even in penetrating injuries caused by broken glasses, the direct impact may result in extensive eyewall injuries, as occurred in Cases 6 and 7. These explanations could also account for the mechanism of orbital wall fracture in GROIs. Orbital wall fractures were only observed in 54.5% (12 cases) of cases, but among patients with open-globe injuries 88.9% (eight out of nine cases) had orbital wall fractures. In addition, patients with open-globe injuries tended to have more ocular adnexal injuries requiring surgeries than patients with a contusion injury. The direct impact of the golf ball may increase ocular adnexal injuries.
The FVA in cases with contusion injuries depended on the severity of injury to the posterior segment, including commotio retinae, choroidal rupture, and macular hole. Optical coherence tomography may be useful in evaluating the posterior segment of eyes with a decreased VA following a GROI.
Our VA results, which were categorized by the OTS, were comparable to those of the OTS study (Table 3).16 Unfortunately, our study had only 22 cases and did not have sufficient statistical power to be compared with the OTS study. Han and Yu20 reported that the OTS system had predictive value in open-globe injuries occurring in Asian population, and that the VA following an open-globe injury in the OTS category 1 or 2 was significantly better than that reported in the OTS study. In contrast, all of our OTS category 1 cases required enucleation.
Observing the rules and etiquette of golf is important for preventing GROIs, especially on golf courses. In addition, the social and/or legal policies for safety regulations on driving ranges should be discussed because GROIs should not occur when golf balls ricochet off driving range columns or walls. In addition, we showed that eyewear might reduce ocular damage from a golf ball, even though broken glasses caused injury to the eyewall, eyelid, and canaliculus. Unlike ordinary glasses, the protective eyewear may not scatter on impact and may additionally absorb the energy of impact. Hence, the use of protective eyewear can prevent devastating GROIs both the rupture and penetrating types.
The present study had several limitations. The number of cases was not quite large enough to evaluate classification systems for prognosis prediction. In addition, mild cases might have been missed because of referral bias, inherent to a tertiary hospital's patient population. Multicenter, large-scale, prospective trials are needed to evaluate the classifications for prognostic predictive value properly.
In conclusion, the present study demonstrated that using the BETT, OTCG, and OTS classification systems is useful for describing and evaluating GROIs. Consistent with previous studies,1, 2, 4, 7, 9, 10, 11, 14, 19 we showed that GROIs generally have devastating results for VA as well as for globe preservation. Observing the rules of golf is essential and social policies for safety regulation are needed. The use of protective eyewear may help to prevent devastating GROIs.
Acknowledgments
This study was partly supported by the Translational Research Program (A111161) funded by the Korea Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea.
The authors declare no conflict of interest.
References
- Jeffers JB. The role of organized ophthalmology in preventing ocular injuries. Int Ophthalmol Clin. 1988;28 (3:255–258. doi: 10.1097/00004397-198802830-00019. [DOI] [PubMed] [Google Scholar]
- Schein OD, Hibberd PL, Shingleton BJ, Kunzweiler T, Frambach DA, Seddon JM, et al. The spectrum and burden of ocular injury. Ophthalmology. 1988;95 (3:300–305. doi: 10.1016/s0161-6420(88)33183-0. [DOI] [PubMed] [Google Scholar]
- Macewen CJ. Eye injuries: a prospective survey of 5671 cases. Br J Ophthalmol. 1989;73 (11:888–894. doi: 10.1136/bjo.73.11.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayasundera T, Vote B, Joondeph B. Golf-related ocular injuries. Clin Experiment Ophthalmol. 2003;31 (2:110–113. doi: 10.1046/j.1442-9071.2003.00615.x. [DOI] [PubMed] [Google Scholar]
- Weitgasser U, Wackernagel W, Oetsch K. Visual outcome and ocular survival after sports related ocular trauma in playing golf. J Trauma. 2004;56 (3:648–650. doi: 10.1097/01.ta.0000062970.91139.05. [DOI] [PubMed] [Google Scholar]
- Millar GT. Golfing eye injuries. Am J Ophthalmol. 1967;64 (4:741–742. doi: 10.1016/0002-9394(67)92859-0. [DOI] [PubMed] [Google Scholar]
- Mieler WF, Nanda SK, Wolf MD, Harman J. Golf-related ocular injuries. Arch Ophthalmol. 1995;113 (11:1410–1413. doi: 10.1001/archopht.1995.01100110070027. [DOI] [PubMed] [Google Scholar]
- Burnstine MA, Elner VM. Golf-related ocular injuries. Am J Ophthalmol. 1996;121 (4:437–438. doi: 10.1016/s0002-9394(14)70441-6. [DOI] [PubMed] [Google Scholar]
- Pollack JS, Mieler WF, Mittra RA. Golf-related ocular injuries. Curr Opin Ophthalmol. 1997;8 (3:15–18. doi: 10.1097/00055735-199706000-00004. [DOI] [PubMed] [Google Scholar]
- Roth DB, Warman R. Optic nerve avulsion from a golfing injury. Am J Ophthalmol. 1999;128 (5:657–658. doi: 10.1016/s0002-9394(99)00220-2. [DOI] [PubMed] [Google Scholar]
- Hink EM, Oliver SC, Drack AV, Hawes MJ, Wojno TH, On AV, et al. Pediatric golf-related ophthalmic injuries. Arch Ophthalmol. 2008;126 (9:1252–1256. doi: 10.1001/archopht.126.9.1252. [DOI] [PubMed] [Google Scholar]
- Townley D, Kirwan C, O'Keefe M. Golf—recognising the risk of severe eye injury. Ir Med J. 2008;101 (6:167–169. [PubMed] [Google Scholar]
- Pieramici DJ, Sternberg P, Jr, Aaberg TM, Sr, Bridges WZ, Jr, Capone A, Jr, Cardillo JA, et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol. 1997;123 (6:820–831. doi: 10.1016/s0002-9394(14)71132-8. [DOI] [PubMed] [Google Scholar]
- Kuhn F, Morris R, Witherspoon CD.Birmingham Eye Trauma Terminology (BETT): terminology and classification of mechanical eye injuries Ophthalmol Clin North Am 200215(2139–143.v. [DOI] [PubMed] [Google Scholar]
- Kuhn F, Morris R, Witherspoon CD, Mester V. The Birmingham Eye Trauma Terminology system (BETT) J Fr Ophtalmol. 2004;27 (2:206–210. doi: 10.1016/s0181-5512(04)96122-0. [DOI] [PubMed] [Google Scholar]
- Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD.The Ocular Trauma Score (OTS) Ophthalmol Clin North Am 200215(2163–165.vi. [DOI] [PubMed] [Google Scholar]
- Whitnall SE.The Anatomy of the Human Orbit and Accessory Organs of Vision2nd edn.Humphrey Milford, Oxford University Press: London; New York; 1932 [Google Scholar]
- Cui M, Zhang C, Liang S. Measurements and observations of Chinese orbits. Chin J Ophthalmol. 1959;4:208–211. [Google Scholar]
- Migliori ME, Gladstone GJ. Determination of the normal range of exophthalmometric values for black and white adults. Am J Ophthalmol. 1984;98 (4:438–442. doi: 10.1016/0002-9394(84)90127-2. [DOI] [PubMed] [Google Scholar]
- Han SB, Yu HG. Visual outcome after open globe injury and its predictive factors in Korea. J Trauma. 2010;69 (5:E66–E72. doi: 10.1097/TA.0b013e3181cc8461. [DOI] [PubMed] [Google Scholar]