Abstract
Objective
To characterize safety hazards related to e-prescribing in community pharmacies.
Methods
The Sociotechnical Systems (STS) framework was used to investigate the e-prescribing technology interface in community pharmacies by taking into consideration the social, technical and environmental work elements of a user’s interaction with technology. This study focused specifically on aspects of the social subsystem.
Study Design and Setting
The study employed a cross-sectional qualitative design and was conducted in seven community pharmacies in Wisconsin. Direct observations, think aloud protocols, and group interviews were conducted with 14 pharmacists and 16 technicians, and audio-recorded. Recordings were transcribed and subjected to thematic content analysis guided by the sociotechnical systems theoretical framework.
Results
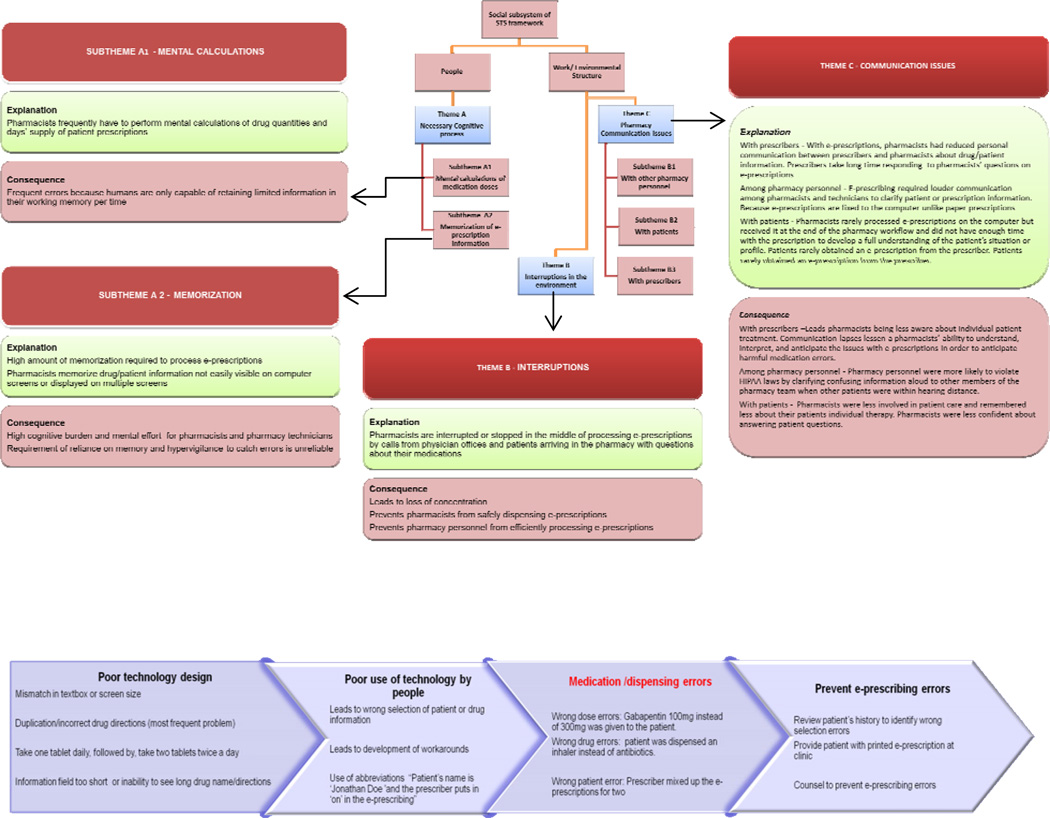
Three major themes that may increase the potential for medication errors with e-prescribing were identified and described. The three themes included: (1) increased cognitive burden on pharmacy staff, such as having to memorize parts of e-prescriptions or having to perform dosage calculations mentally; (2) interruptions during the e-prescription dispensing process; and (3) communication issues with prescribers, patients, and among pharmacy staff. Pharmacy staff reported these consequences of e-prescribing increased the likelihood of medication errors.
Conclusions
This study is the first of its kind to identify patient safety risks related to e-prescribing in community pharmacies using a sociotechnical systems framework. The findings shed light on potential interventions that may enhance patient safety in pharmacies and facilitate improved e-prescribing use. Future studies should confirm patient safety hazards reported and identify ways to utilize e-prescribing effectively and safely in community pharmacies.
Keywords: Electronic Prescribing, Pharmacy, Health Information Technology, Patient Safety, Sociotechnical Systems
INTRODUCTION
Federal government efforts to encourage adoption of various components of electronic health records have led to increasing adoption of health information technology (health IT) in healthcare settings to improve the safety in the medication use process.1 One type of health IT that is being mandated for use in primary and secondary healthcare settings in the United States is electronic prescribing.2, 3 Electronic prescribing (e-prescribing) is a type of health IT that allows prescribers to electronically send prescriptions (e-prescriptions) to community pharmacies via a secure pharmacy information network.4 E-prescribing has received significant attention for its potential to improve patient safety by reducing medication errors in primary care settings.5 However, several years of using e-prescribing has shown that this health IT may introduce new kinds of medication errors in community pharmacies that threaten patient safety.6, 7 One study on e-prescribing in community pharmacies reported that pharmacists intervene on 11.7% of e-prescriptions and 15.4% of handwritten prescriptions; however, there was no statistical difference in pharmacist intervention rates between e-prescriptions and handwritten prescriptions.6 Researchers in this study concluded that pharmacists must intervene on e-prescriptions as they do with handwritten prescriptions.
Community pharmacies are located within the community and typically have no direct affiliation with hospitals or clinics and therefore have no access to electronic health records of patients. Prevention of medication errors is a priority for community pharmacists. Pharmacists routinely screen prescriptions for potential problems, including prescribing errors to ensure that medication errors do not reach patients and cause harm.8 As use of e-prescribing becomes more common, examining the types of problems encountered in community pharmacies using e-prescribing is important in preventing medication errors. A primary reason for adopting e-prescribing is to reduce medication errors associated with illegible handwritten prescriptions. It has become essential to examine, understand and mitigate the safety risks related to e-prescribing that may result in medication errors. This is important in moving forward with enhancing e-prescribing systems to improve patient safety and overall quality of care. Thus far, there has been limited research to identify patient safety issues related to e-prescribing in community pharmacies.
In order to understand these safety concerns, this study employs human factors engineering (HFE) concepts and techniques, a science that deals with discovering and applying information about human behavior, abilities, limitations and other characteristics to the design of systems, tasks, tools, jobs, and environments for productive, safe, comfortable and effective human use.9 The application of the HFE approach has been found to be useful in understanding health IT safety issues, and designing and implementing interventions to improve quality and safety in patient care.10–15 HFE researchers and patient safety experts have conducted multiple studies aimed at examining patient safety issues that arise with health IT in hospital settings.9, 16 Such studies report that use of health IT such as e-prescribing or computerized order entry can introduce new kinds of medication errors.17, 18 Safety experts have recommended the adoption of HFE concepts to understand why these safety risks exist and how to mitigate these risks in healthcare settings.19 However, few studies have employed HFE approaches to examine patient safety and health IT in community pharmacies. In practice, applying of HFE concepts involves designing technology or systems with appropriate fit between individuals, products, and the environment.
For this study, a HFE conceptual model called the sociotechnical system (STS) framework was applied as the guiding framework for this research. The STS framework was developed to characterize, evaluate, and improve human-technology interactions.20 A sociotechnical theoretical approach assumes a systems perspective which takes into consideration the social, technical, and environmental work elements of a user’s interaction with technology.21 For example, the social element includes the people in the work systems such as healthcare professionals and the technical elements includes tools and technologies used by the healthcare professional within a specific physical environment. The interactions of the various elements of a sociotechnical system produce different outcomes on performance and safety and this can positively or negatively contribute to causes of medication errors.11 The objectives of this study were to understand pharmacy concerns with e-prescribing safety and to identify social aspects of pharmacy staff interaction with e-prescribing that create the potential for medication errors that can lead to patient harm. This study focused on a human factors analysis of the social subsystem of the STS framework; a previous study has reported on the technical aspects of using e-prescribing in community pharmacies.22 This study identified hazards to patients associated with differences between e-prescribing interfaces used by pharmacists and prescribers, differences that increased the risk of errors such as selection of the wrong patient or drug (name, directions, dose, strength, formulation, package sizes).
METHODS
Participants
The targeted sample size was 30 participants from a broad spectrum of demographical characteristics and variability in types of e-prescribing systems used. Community pharmacies in Wisconsin were selected for participation in the study if they processed at least 10 e-prescriptions daily. Three pharmacies were recruited through the Pharmacy Society of Wisconsin listserv in December 2010. An additional four pharmacies were identified by snowball sampling techniques. In total, 14 pharmacists and 16 technicians from seven community pharmacies were recruited for participation in the study, out of a total of 40 pharmacy staff (17 pharmacists and 23 technicians). Human subjects’ approval for the study was granted by the University of Wisconsin-Madison IRB. Written informed consent forms were obtained from all participants.
Data Collection Procedures
Data collection took place between January and March, 2011. The study design involved a systematic qualitative examination of e-prescription processing in community pharmacies using a combination of data collection methods (direct observations, think aloud protocols, and pharmacy team interviews). In community pharmacies in the United States, prescription are typically processed in the following order: 1) receive the prescription electronically, by fax, via telephone, or as a typed or handwritten paper prescription; 2) pharmacists and/or technicians input the prescription information into the pharmacy computer system; 3) pharmacists verify that the prescription is appropriate for the patient by reviewing the patient and medication profile; 4) technicians fill the prescription; 5) pharmacists reviews the prescription filled by the technician; and 6) pharmacist counsels the patient on how to use the medications.23 For purposes of the study, the e-prescription process began with the receipt of the e-prescription in the pharmacy, through the review of the prescription by the pharmacist prior to patient counseling.
Direct Observations and Think Aloud Protocols
The purpose of conducting direct observations was to understand how e-prescriptions are handled in real-time. Data were first obtained using direct observations and think aloud protocols. Think aloud protocol is a method used by human factors researchers to provide information on tasks by having participants verbalize task performance to yield insight into cognitive components of the task.24, 25 Think aloud protocol combined with direct observation was used to elucidate the stepwise processing of an e-prescription, and to identify cognitive and informational needs of pharmacists and technicians. As an e-prescription was transmitted to the pharmacy, the pharmacist or pharmacy technician was observed and questioned about their interactions with the pharmacy e-prescribing system used for processing the e-prescription. During think aloud sessions, participants were instructed to verbalize their thoughts as they process at least five consecutive e-prescriptions and to highlight the patient safety issues with using the technology that could easily lead to a medication error. The duration of direct observations and think aloud protocols ranged from two to five hours. Sixteen pharmacy staff (seven pharmacists and nine technicians) took part in this phase of data collection. Responses from the think aloud protocols were audio taped and digitally recorded. Additional information was collected by the researcher using field notes from observations to contribute to participants’ responses during think aloud protocols. Field notes were transcribed.
Pharmacy Team Interviews
The second phase of the project involved semi-structured group interviews with the pharmacy staff. These group interviews were conducted with two pharmacists and two technicians from each pharmacy and were referred to as “team interviews”. The team interviews involved participants from the same pharmacy. During the pilot test of this project, it was observed that conducting pharmacy team interviews, rather than individual interviews or traditional focus groups with homogenous participants, was more effective in generating information on the aspects of the e-prescription that presented patient safety hazards. In addition, participants were more comfortable sharing about e-prescribing problems when they were with other pharmacists or technicians from the same pharmacy.
A semi-structured interview guide was developed (appendix A). The development of interview questions was guided by the objective of the study and previous studies on e-prescribing in community pharmacies.7, 26 The interview questions consisted of neutral and open-ended questions, carefully constructed to avoid eliciting socially desirable responses. Scripted and unscripted follow-up probes were used to elicit further information. The first part of the team interview was guided by the Critical Incident Technique (CIT). CIT involves using participants’ past experiences to elicit information. CIT is an HFE technique whereby participants are asked about unusual incidents (positive and negative experiences). 10, 17 This method was used to provide information on the aspects of e-prescribing that could negatively affect patient safety. The use of the CIT involved eliciting information on pharmacists’ and technicians’ account of past and recent experiences or events with e-prescribing that proved challenging in the pharmacy.
The team meetings with pharmacists and technicians who frequently processed e-prescriptions were scheduled shortly after the direct observations and think aloud protocols, so that specific scenarios or issues that came up during observations could be clarified. The team meetings were moderated by the researcher and conducted in a quiet location chosen by pharmacy team members. Six interviews were conducted within the pharmacies and one interview took place at a restaurant. Each team meeting took about one hour. The interviewer used the semi-structured interview instrument to elicit a wide range of pharmacists’ and technicians’ perceptions about e-prescribing.
Interviews were audio recorded with permission of participants using a digital tape recorder, and then transferred immediately to a computer. Audio recorded team interviews were transcribed verbatim by a transcription company, while recordings from the think aloud protocol were transcribed verbatim by the researcher. Data saturation was reached by participation of all seven pharmacies. Interview transcripts were verified for accuracy and detail. Each pharmacy team interview was assigned a number code to identify the transcripts for subsequent analysis.
Data Analysis
All transcripts were cross-checked with the original recording to ensure accuracy. The primary researcher (OO) analyzed all field notes and transcripts using thematic analysis. Each transcript was coded by one researcher (OO) with background in pharmacy and human factors engineering. The research identified themes relevant to the social subsystem of the STS framework. Figure 1 depicts the constructs of the STS framework that guided the pre-specified theme structure that guided data analysis. The two main constructs (people and structure) as outlined in the social subsystem of the STS framework were found to be most useful in categorizing emergent themes. A second researcher (MC) reviewed all themes and verified their accuracy and interpretation by reading sections of the transcripts. Finally, both researchers met to discuss any inconsistencies and reached a consensus on the description and interpretation of each theme. Methodological triangulation was conducted to validate the data obtained from each data collection. Triangulation of data from multiple sources enabled researchers to obtain an in-depth understanding of patient safety issues related to use of e-prescribing in pharmacies.
Figure 1.
Sociotechnical Systems Analysis of E-prescribing Safety Issues in Pharmacies
RESULTS
Of the seven pharmacies that participated in the study, three were chain pharmacies and four were independently owned pharmacies. The pharmacies were staffed with one to three pharmacists and one to five technicians. The pharmacies’ experience with e-prescribing ranged from six months to three years. On average, a third of prescriptions dispensed daily in these pharmacies were e-prescriptions (33 to 90 e-prescriptions). For processing e-prescriptions, three of the pharmacies used the PDX pharmacy dispensing computer system, two pharmacies used the QS/1 pharmacy dispensing computer system, and two used the Pharmaserv pharmacy dispensing computer system. Pharmacy staff characteristics are shown in Table 1.
Table 1.
Description of Participants
| Pharmacists | Technicians | |
|---|---|---|
| Men | 6 | 1 |
| Women | 8 | 15 |
| Years of experience | 2 – 43 | 1 – 30 |
| Age (in years) | 25 – 67 | 21 – 54 |
The two main constructs (people and structure) as outlined in the social subsystem of the STS framework were found to be most useful in categorizing emergent themes. Table 2 contains a summary explanation of themes identified and Table 3 includes verbatim quotes from participants that relate to the themes identified. Participants reported receiving erroneous e-prescriptions daily because prescribers had entered incorrect information. Examples of erroneous e-prescriptions discussed by participants during data collection are provided in Table 4.
Table 2.
Summary of Themes
| Theme | Explanation | Consequence |
|---|---|---|
| Themes Related to the “People” Component of the Sociotechnical Systems Framework | ||
| Cognitive burden | ||
| Memorization | High amount of memorization required to process e-prescriptions | High cognitive burden for pharmacists |
| Pharmacists memorize drug/patient information not easily visible on computer screens or displayed on multiple screens | Requirement of reliance on memory and hypervigilance to catch errors is unreliable | |
| Perform mental calculations | Pharmacists frequently have to perform mental calculations of drug quantities and days’ supply of patient prescriptions | Increases mental workload for pharmacists |
| Themes Related to the “Structure” Component of the Sociotechnical Systems Framework | ||
| Communication issues | ||
| With prescribers | With e-prescriptions, pharmacists reduced personal communication between prescribers and pharmacists about drug/patient information | Leads to pharmacists being less aware about individual patient treatment |
| Prescribers take long time responding to pharmacists’ questions on e-prescriptions | Communication lapses lessen a pharmacist’s ability to understand, interpret, and anticipate the issues with e-prescriptions in order to anticipate harmful medication errors. | |
| Among pharmacy personnel | E-prescribing required louder communication among pharmacists and technicians to clarify patient or prescription information | Pharmacy personnel were more likely to violate HIPAA [Health Insurance Portability and Accountability Act]. laws by clarifying confusing information aloud to other members of the pharmacy team when other patients were within hearing distance. |
| With patients | Pharmacists rarely processed e-prescriptions on the computer, but received it at the end of the pharmacy workflow and did not have enough time with the prescription to develop a full understanding of the patient’s situation or profile | Pharmacists were less involved in patient care and remembered less about their patients’ individual therapy |
| Pharmacists were less confident about answering patient questions | ||
| Patients rarely obtained an e-prescription from the prescriber | Patients are less aware of what drugs were prescribed or were not familiar with the workings of the e-prescribing process; this lead to additional confusion during patient counseling. | |
| Interruptions | Pharmacists were interrupted or stopped in the middle of processing e-prescriptions by calls from physician offices and patients arriving in the pharmacy with questions about their medications | Leads to loss of concentration |
| Prevent pharmacists from safely dispensing e-prescriptions | ||
| Prevents pharmacy personnel from efficiently processing e-prescriptions | ||
| With interruptions pharmacists frequently forgot what part of the e-prescriptions they were processing and often have to start over | ||
Table 3.
Sample Quotes from Participants Related to Identified Themes
| Theme | Quote from Participants |
|---|---|
| Memorization | “I don’t like when the drug names are too long to fit in and the sigs [drug directions] are too long to fit in too…That’s a potential for our error because try to remember what you saw. Who wants to fill a prescription based on memory? That’s not safe…Are you going to remember it correctly? That’s an opportunity for error for sure.” |
| Performing mental calculations | “The quantity they are looking for is 120 units. In other words 2 boxes of 60… If it’s 3 mL each then 12 times 5 is 60. Ours then is 360, because we are going by the number of milliliters. So this is actually 2 boxes.” |
| Communicating with prescribers | “It’s less about ‘I can’t read what this is. What is it?’ but it’s more just, ‘Are you sure this is what you [prescriber] meant?’ So it’s really focusing more on clarification of what they [prescriber] intended, rather than trying to decipher what they actually wrote.” “There is another concern in that it doesn’t always print the information of the doctor where they’re currently at. If you have a doctor working a walk-in or an E.R. [emergency room] and you get a prescription from them, it sometimes lists their office phone number. Then if you have a question on it and you try to call the phone number that’s on the e-prescription sometimes they’re like, ‘Oh, well they’re not here today.’ Then you have to call around or they have to bounce you around from person to person until you can find where they actually are practicing. So it makes it harder to track them down. |
| Communicating with patients | “I can see part of it. If they’re giving you [paper] prescriptions, you know they’ve given you three prescriptions. If they say, ‘Oh, the doctor just sent down an e-prescription for me,’ Okay, well did they send down one prescription or did they send down four prescriptions? Sometimes patients know and sometimes they don’t. Even just for telling them a time of how long it’s going to take, if I can see they have three prescriptions here, in my mind I can do that. Whereas with e-prescriptions I’m not entirely sure how many have come down, so I say, ‘Oh, yeah, it will be ten minutes,’ because I thought it was one prescription, but ‘Oh, wait there are four prescriptions. Okay, it’s going to be 20 minutes now.’ “A lot of times when a patient comes down, they expect the prescription to be ready already because it was sent down electronically. Whereas when they bring it in with a paper prescription, they know that this is where it starts, right there. With an e-prescription it started 20 minutes ago, when the doctor sent it down. ‘I’m here to pick up a prescription.’ That’s how they come in. ‘Well, did you call it in or did the doctor send it?’ ‘The doctor sent it. It was 10 minutes ago.’ …That doesn’t take in to account the fact that three other doctors also sent prescriptions down all at the same time, so we’ve got four people coming down all for prescriptions at the same time, that all think they’re the only one. Then you’ve got four people waiting all of the sudden.” |
| Communicating in the pharmacy | “There is more potential to break HIPAA [U.S. Health Insurance Portability and Accountability Act, a legislative act that protects patients’ health information]. Because we have a small pharmacy, I’ll be over here [pointing to opposite side of pharmacy] and I’ll say, ‘Hey, can you pull a prescription for [John Doe],’ or whomever the patient may be. I’ll say it across the pharmacy, so the other patients know who the person is. Whereas with the paper prescription, it’s there and you don’t even have to say anything.” |
| Interruptions | “Sometimes when you are doing e-prescriptions you have to stop if someone comes to the window or they ask for something else, you know… if I got half way through the prescription and checking stuff. I won’t process it. I will just exit out of it and have to start all over” |
Table 4.
E-prescriptions Errors Identified in Community Pharmacies
| Type of Error Detected |
Quote from Participants |
|---|---|
| Wrong drug strength | “Gabapentin 100mg prescribed instead of 300mg” |
| Wrong drug duration | “Here’s an error with Levaquin 500 [levofloxacin, an antibiotic], [Directions were] one every 24 hours for a quantity of 30. So that’s not right. It should have been ten days [e.g., quantity of 10 instead of 30]” |
| Wrong drug name | “They [prescribers] can pick the wrong drug. That’s why you counsel the patient. Like I had one maybe two months ago. It was a mom, and I had said, ‘Here are 2 inhalers for your children’. And she’s like, ‘inhalers? They are not getting inhalers.’ So the doctor had picked the wrong, I can’t remember what it was, an antibiotic or cream or something totally differently.” |
| Wrong drug formulation | “For example Wellbutrin [bupropion] SR versus XL [SR formulation taken twice daily whereas XL formulation taken once daily], when we’ve called back to the doctor, we’ve found that it’s actually changed the drug that they wrote. They’ve put in Wellbutrin [bupropion] SR and then somehow in the system it comes in here at XL or the other way around.” |
| Wrong patient | A patient came down looking for an EpiPen [epinephrine autoinjector]. ‘We don’t have it. We have an EpiPen[epinephrine autoinjector] from the same doctor for somebody else.’ We call up and they said, ‘Oh, yeah, that was an error. Wrong patient.’ So if they have multiple patient charts up, sometimes they prescribe drugs for the wrong patient, which are errors that are kind of hard to fish through sometimes.” |
Themes Related to the “People” Component of the STS Framework
Theme 1 – Cognitive burden
Memorizing prescription information
The information on a prescription includes patient name, drug name, formulation, strength, directions for use, quantity, and prescriber name. All of the prescription information is presented together on a paper prescription. However, for an e-prescription, information can be presented on different screens. As participants processed e-prescriptions, they memorized information needed to process the prescription that was not easily visible on the computer screen. For example, participants frequently memorized patient information on e-prescriptions when they needed to search for drug information on multiple screens, and vice versa. When the drug name was too long for the textbox, participants had to search for the drug name on one screen, memorize the drug name and input it into another screen containing the original e-prescription. Participants memorized in-house pharmacy “sig codes” which were used to populate drug directions on the e-prescriptions. Participants in pharmacies with dispensing robots memorized which e-prescription drugs were filled by the robot and those to be filled from the stock shelf. Participants also memorized how many e-prescriptions a patient was to receive if the patient was to receive prescriptions by multiple avenues (e-prescriptions and faxed prescriptions –mainly for controlled substances).
In order to save time during dispensing, participants memorized e-prescription information such as patient name, drug name, and insurance issues that were known to be predictably problematic. For example, participants memorized irregular drug package sizes so as to detect mistakes in drug quantities sent from physician offices so the pharmacy could be billed correctly for the medication.
Performing mental calculations
A frequently noted cognitive burden performed by participants was the mental calculation of drug quantities and days’ supply based on memorized drug package size. This was done to ensure that the pharmacy was billed correctly by insurance companies. This was common for drugs with dosage forms that were not easy measured, such as inhalers, creams, and eye drops. For example, an inhaler that contains 8.5 grams could be e-prescribed by the prescriber as 8 grams. This would be inadvertently missed by pharmacy staff and result in the pharmacy being reimbursed incorrectly by the insurance company.
Themes Related to the “Structure” Component of the STS Framework
Theme 2 - Communication issues with e-prescribing use
Several communication issues were identified with e-prescriptions which are discussed below.
Communicating with prescribers
The use of e-prescribing resulted in several changes to communication with prescribers. First, e-prescribing led to fewer phone calls and therefore less conversation between the pharmacy and the prescriber’s office. Pharmacy personnel reported that frequent conversations with the prescriber had previously allowed them to be more informed about their patients. Second, the nature of conversations with the advent of e-prescribing was not as constructive as previously, as pharmacists and prescribers were now more focused on fixing problems with e-prescriptions rather than addressing other important patient care related issues. Third, pharmacy staff also perceived that prescribers took longer in responding to their questions with e-prescriptions than with paper prescriptions, because the prescriber had to send an entirely new e-prescription even if issues were clarified verbally.
Communicating with patients
Unlike paper prescriptions brought into the pharmacy by patients and handed directly to the pharmacist, pharmacists typically did not see the e-prescription until it was about to be dispensed to the patient. E-prescriptions in the pharmacy were typically initially processed on the computer by the technician and the pharmacist only reviewed the e-prescription at the end of the workflow before it was given to the patient. Participants explained that having a paper prescription handed to them by a patient immediately alerted them that the patient had a prescription. In addition, being handed a paper prescription allowed the pharmacist to start thinking through the prescription and probe for information while the prescription was being processed; this encouraged immediate communication with the patient, instead of trying to create a plan of action at the very end of the workflow. As a result, pharmacists perceived that they were less involved with patient care and remembered less about their patients. Two pharmacists reported feeling less confident about answering patient questions because they rarely processed e-prescriptions and only received the prescription at the end of the pharmacy workflow, where they ultimately did not have enough time with the prescription to develop a full understanding of the patient’s situation or profile.
Unlike paper prescriptions which can be read by the patient can read as they are being brought from the prescriber’s office to the pharmacy, participants reported that since e-prescriptions were sent directly to pharmacies, patients did not have a visible artifact that reminded them of how many prescriptions or what medications they were being prescribed; this led to additional confusion at the pharmacy during patient counseling.
Communicating in the pharmacy
When filling prescriptions, technicians frequently clarify information with pharmacists. With paper prescriptions, technicians typically walk across the pharmacy with the paper prescription in hand to obtain clarification quietly from the pharmacist. This allows both the pharmacist and technician to view the paper prescription while discussing and clarifying. This is not possible with e-prescriptions, because the prescription information is only viewable on the pharmacy computer and cannot be easy carried around the pharmacy like a paper prescription. In fact, one participant stated that in her pharmacy, computer terminals were placed at both ends of the dispensing process. Pharmacy personnel, locked into viewing and filling e-prescriptions directly from the computer, were more likely to violate HIPAA (Health Insurance Portability and Accountability Act – federal law that protects patient information) laws by clarifying confusing information aloud to other members of the pharmacy team when other patients were within hearing distance.
Theme 3 – Interruptions
Interruptions take place whether pharmacy staff is handling paper or e-prescriptions. However, when handling a paper prescription, the participants appeared better able to accommodate interruptions more fluidly than with e-prescriptions. For example, a pharmacist who was filling a paper prescription was able to carry the paper around the pharmacy while talking to a technician about a different prescription or answering the telephone. As a result, the paper prescription served as a memory aid and stayed in the foremost mind of the pharmacist; hence, the pharmacist was less likely to forget about the prescription. An e-prescription is locked onto the computer monitor and is not portable or mobile in the pharmacy. This led to participants having to stop mid-way in filling the e-prescriptions to attend to other pressing issues in another part of the pharmacy. Participants frequently forgot where they were in the process of dispensing the e-prescription and had to start over again. Sometimes the participant completely forgot about the outstanding e-prescription when distracted by another issue.
DISCUSSION
The number of e-prescriptions received in community pharmacies is increasing and is currently estimated to grow by about 70% annually.27 This exponential increase has significant implications on patient safety in community pharmacies. Our findings are consistent with one study that found that one in 10 computer generated prescriptions included at least one medication error, and a third of these errors were potentially harmful.28 Study participants reported receiving erroneous e-prescriptions daily because prescribers had input or selected incorrect information. Prescribers selected the wrong drug, the wrong patient, the wrong dosage form or strength. If such inaccuracies in e-prescriptions are not detected in the pharmacy, patients could receive the wrong medication or incorrect dose of their current medication therapy. It is therefore important to consider the factors that contribute to e-prescription errors in community pharmacies to prevent and resolve similar errors in the future.
For instance, there is still need for verbal communication between prescribers and pharmacists to clarify e-prescription information; however, there are no processes in place to facilitate direct and easy communication between prescribers and pharmacists. This is particularly important, as pharmacies are able to receive prescriptions faster than previously possible due to tighter coupling between the prescriber and pharmacy computer systems. Communication lapses further lessen a pharmacists’ ability to understand and interpret the issues with e-prescriptions in order to anticipate harmful medication errors. Indeed, previous research has found that reduction in communication among clinicians increases the likelihood of errors resulting from miscommunication and poor coordination of patient care.29
Poor communication between prescribers and pharmacists may negatively influence patient care and health outcomes by resulting in medication errors.30 Communication issues arise from using e-prescribing that present additional patient safety hazards in the pharmacy. Prescribers may verbally interact less frequently with pharmacists about patient information needed to process e-prescriptions, as interactions between prescribers and pharmacists have become more electronic in nature rather than verbal. Likewise, pharmacists who encountered e-prescribing errors felt less compelled to contact prescribers for clarifications on problematic e-prescriptions because of delays in directly reaching the prescribers. This is consistent with scientific literature that suggests that technologies such as e-prescribing have the potential to reduce human relationships among clinicians and this is important for patient care.31 Another study found that hospital pharmacists independently corrected errors in e-prescriptions if they identified that it was a common error from the prescriber.18
Communication issues that might have resulted from e-prescribing also affected pharmacists’ interaction with patients. Participants observed that patients appeared confused about workings of e-prescribing between the physician office and the pharmacy. These findings are consistent with a previous study evaluating e-prescribing in chain community pharmacies in which 68 respondents reported that e-prescribing use reduced communication with patients.26 Pharmacists also reported being less confident in communicating with patients about their prescriptions received electronically. Pharmacists stated that with this technology, they had to remember less about individual patients, making them feel less confident in communicating with patients. This finding suggests that there is reduced situation awareness for pharmacists when handling e-prescriptions. Situation awareness, which is the ability to quickly and effectively integrate relevant information from multiple sources in order to develop an accurate understanding of the environment32, is known to be a key factor in enhancing patient safety.33 Additionally, findings from this study indicated that the interaction between pharmacy personnel and e-prescribing technology impacted pharmacists’ cognitive performance, needing higher memory requirements and increased mental calculations. This is consistent with the literature that suggests that health IT’s effect on patient safety is related to its ability to affect clinicians’ cognitive performance.34
Memory lapses easily occur when clinicians have to juggle multiple tasks, and this is affected by the number of steps each task requires. Reliance on memory could lead clinicians to inadvertently make errors when processing e-prescriptions. Indeed, memory lapses have been found to significantly cause errors due to the limits of short term memory, caused by memory overload.35 The goal of health IT technology such as e-prescribing should be to reduce a healthcare professional’s reliance on memory and eliminate the need to perform mental calculations, to lower the probability of errors of omission. Another important factor found by this study is that interruptions from other staff during medication preparation and dispensing occur when processing e-prescriptions. Multiple interruptions and distractions are common in community pharmacies and the presence of such distractions has been demonstrated to contribute to medication errors when handling prescriptions.36 In addition, significant evidence in human factors literature shows that reliance on vigilance to catch errors is unreliable when users perform tasks that require high cognitive load in a busy and chaotic work environment.35 This is because humans are only capable of retaining a limited amount of information in their working memory at a given time. Pharmacy personnel face similar burdens with current e-prescribing systems, which require high cognitive effort to prevent and catch medication errors. With e-prescribing, pharmacists and technicians need to be more hyper vigilance than with traditional prescriptions. Interruptions reported in the pharmacy environment also limit pharmacists’ and technicians’ ability to meet the required vigilance when processing e-prescriptions. Furthermore, it has been shown that humans have very limited insight into their own performance when using health IT such as e-prescribing technology. Participants indicated that they were unaware of the high amount of memorization required to process e-prescriptions.
There are several limitations to this study that must be noted. First, pharmacies that participated in this study were from only one state in the United States, which may limit generalizability of findings. Second, the use of think aloud protocols during observations may have resulted in interruptions for pharmacy staff during their usual workflow. Although having participants think aloud and attend to a task at the same time can be a challenge, the strength of using think aloud as a data collection method outweighs this limitation.37 Third, the use of pharmacy team interviews for data collection was a modified focus group in which participants were not homogeneous (included pharmacists and technicians) and were not unknown to each other as is typical of a focus group. This method of data collection was chosen because it was found to be more effective in helping participants open up about e-prescribing problems during intial piloting of the data collection methods.
CONCLUSION
Findings from this study have important implications. Inappropriate use of e-prescribing can lead to medication errors, and patient harm. This could results in more healthcare complications and extra expenditures in treating adverse drug events and hospitalizations. In addition, pharmacists and technicians must be aware of patient safety hazards due to using e-prescribing in order to be proactive in addressing erroneous e-prescriptions to prevent patient harm.
Poor design of e-prescribing may lead to poor utilization by pharmacists and prescribers. A possible reason for poor design of e-prescribing is developers’ lack of understanding of actual pharmacy workflow and day-to-day practice. A consequence of this is a poor fit of the technology with clinic workflow, which can lead to medication errors. For future studies, researchers and pharmacy organizations should examine the impact of interruptions, miscommunication between users in different healthcare settings, and cognitive burden on safety when using e-prescribing technology. In this study, pharmacists highlighted safety issues that arise when using e-prescribing technology that may easily lead to patient harm or injury. It is also important to evaluate how design of current e-prescribing systems impact patient safety in order to ensure that patients do not receive incorrect medication regimens in community pharmacies.
Acknowledgments
ACKNOWLEDGEMENTS AND FUNDING
This project was funded by the Community Pharmacy Foundation and the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
APPENDIX A
Interview Protocol
Thank you for participating in this interview.
Anyone can choose to respond to each question and contribute to other people’s responses.
Use of critical interview technique
-
1
Can anyone give a description of a bad experience you had when processing an electronic prescription?
-
2
Please provide additional details such as: what happened, at what time or when it happened, why it was bad, and what could have been made better.
Assessing design of electronic prescriptions
-
3
Can you describe to me some weaknesses of the design of electronic prescriptions?
-
4
Are there any gaps in the design that may pose a risk to safe dispensing of the prescription?
Medication safety
-
5
In the last 30 days, how frequently have you received electronic prescriptions with errors?
-
6
Briefly described these errors and why you think they occurred?
Communication patterns
-
7
When handling e-prescriptions, what differences have you observed when communicating with a prescriber, patient or pharmacy staff when compared to handling paper prescriptions?
Feedback about the interview
-
8
Thank you for participating in this interview. What feedback do you have for us about the interview?
Footnotes
COMPETING INTERESTS: None to declare.
Contributor Information
Olufunmilola K. Odukoya, Institution: University of Wisconsin, Department: Social & Administrative Sciences, School of Pharmacy, Postal address: 777 Highland Avenue, Madison Wisconsin 53705, USA, odukoya@wisc.edu, Telephone: 608-698-5054, Fax: 608-262-5262
Michelle A. Chui, Institution: University of Wisconsin, Department: Social & Administrative Sciences, School of Pharmacy, Postal address: 777 Highland Avenue, Madison Wisconsin 53705, USA, mchui@pharmacy.wisc.edu, Telephone: 608-262-0452, Fax: 608-262-5262
REFERENCES
- 1.Buntin MB, Burke MF, Hoaglin MC, et al. The benefits of health information technology: A review of the recent literature shows predominantly positive results. Health Aff (Millwood) 2011;30(3):464–471. doi: 10.1377/hlthaff.2011.0178. [DOI] [PubMed] [Google Scholar]
- 2.Hersh W. Health care information technology: Progress and barriers. JAMA. 2004;292(18):2273–2274. doi: 10.1001/jama.292.18.2273. [DOI] [PubMed] [Google Scholar]
- 3.Siska MH, Tribble DA. Opportunities and challenges related to technology in supporting optimal pharmacy practice models in hospitals and health systems. Am J Health Syst Pharm. 2011;68(12):1116–1126. doi: 10.2146/ajhp110059. [DOI] [PubMed] [Google Scholar]
- 4.Moniz TT, Seger AC, Keohane CA, et al. Addition of electronic prescription transmission to computerized prescriber order entry: Effect on dispensing errors in community pharmacies. Am J Health Syst Pharm. 2011;68(2):158–163. doi: 10.2146/ajhp080298. [DOI] [PubMed] [Google Scholar]
- 5.Kaushal R, Kern LM, Barron Y, et al. Electronic prescribing improves medication safety in community-based office practices. J Gen Intern Med. 2010;25(6):530–536. doi: 10.1007/s11606-009-1238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gilligan AM, Miller K, Mohney A, et al. Analysis of pharmacists’ interventions on electronic versus traditional prescriptions in 2 community pharmacies. Research in Social and Administrative Pharmacy. 2012 doi: 10.1016/j.sapharm.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Warholak TL, Rupp MT. Analysis of community chain pharmacists' interventions on electronic prescriptions. J Am Pharm Assoc (2003) 2009;49(1):59–64. doi: 10.1331/JAPhA.2009.08013. [DOI] [PubMed] [Google Scholar]
- 8.Chen YF, Neil KE, Avery AJ, et al. Prescribing errors and other problems reported by community pharmacists. Therapeutics and clinical risk management. 2005;1(4):333. [PMC free article] [PubMed] [Google Scholar]
- 9.Carayon P. Human factors in patient safety as an innovation. Appl Ergon. 2010;41(5):657–665. doi: 10.1016/j.apergo.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carayon P. Sociotechnical systems approach to healthcare quality and patient safety. Work: A Journal of Prevention, Assessment and Rehabilitation. 2012;41:3850–3854. doi: 10.3233/WOR-2012-0091-3850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carayon P, Schoofs Hundt A, Karsh BT, et al. Work system design for patient safety: The SEIPS model. Qual Saf Health Care. 2006;15(Suppl 1):i50–i58. doi: 10.1136/qshc.2005.015842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karsh BT, Holden RJ, Alper SJ, et al. A human factors engineering paradigm for patient safety: Designing to support the performance of the healthcare professional. Qual Saf Health Care. 2006;15(Suppl 1):i59–i65. doi: 10.1136/qshc.2005.015974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wetterneck TB, Walker JM, Blosky MA, et al. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. Journal of the American Medical Informatics Association. 2011;18(6):774–782. doi: 10.1136/amiajnl-2011-000255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carayon P, Wetterneck T, Hundt A, et al. Assessing nurse interaction with medication administration technologies: The development of observation methodologies. Work With Computing Systems. 2004:319–324. [Google Scholar]
- 15.Carayon P, Wetterneck TB, Hundt AS, et al. Observing nurse interaction with infusion pump technologies. In: Henriksen K, Battles JB, Marks ES, Lewin DI, editors. Advances in patient safety: From research to implementation (volume 2: Concepts and methodology) Rockville (MD): 2005. [Google Scholar]
- 16.Carayon P. Human factors and ergonomics in health care and patient safety. In: Carayon P, editor. Handbook of human factors and ergonomics in healthcare and patient safety. Mahwah, NJ: 2006. pp. 699–700. [Google Scholar]
- 17.Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293(10):1197–1203. doi: 10.1001/jama.293.10.1197. [DOI] [PubMed] [Google Scholar]
- 18.Abdel-Qader DH, Harper L, Cantrill JA, et al. Pharmacists' interventions in prescribing errors at hospital discharge: An observational study in the context of an electronic prescribing system in a UK teaching hospital. Drug Saf. 2010;33(11):1027–1044. doi: 10.2165/11538310-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 19.Gurses AP, Ozok AA, Pronovost PJ. Time to accelerate integration of human factors and ergonomics in patient safety. BMJ Quality & Safety. 2011 doi: 10.1136/bmjqs-2011-000421. [DOI] [PubMed] [Google Scholar]
- 20.Carayon P. Human factors of complex sociotechnical systems. Appl Ergon. 2006;37(4):525–535. doi: 10.1016/j.apergo.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 21.Holden RJ, Karsh BT. A theoretical model of health information technology usage behaviour with implications for patient safety. Behaviour & Information Technology. 2009;28(1):21–38. [Google Scholar]
- 22.Odukoya OK, Chui MA. Retail pharmacy staff perceptions of design strengths and weaknesses of electronic prescribing. JAMIA. 2012;19(6):1059–1065. doi: 10.1136/amiajnl-2011-000779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Odukoya OK, Chui MA. Relationship between E-prescriptions and community pharmacy workflow. Journal of American Pharmacists Association, JAPhA. 2012 Nov-Dec;:185–190. doi: 10.1331/JAPhA.2012.12066. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lundgren-Laine H, Salantera S. Think-aloud technique and protocol analysis in clinical decision-making research. Qual Health Res. 2010;20(4):565–575. doi: 10.1177/1049732309354278. [DOI] [PubMed] [Google Scholar]
- 25.Odukoya OK, Chui MA. Using think aloud protocols to assess E-prescribing in community pharmacies. INNOVATIONS in Pharmacy. 2012;3(3) doi: 10.24926/iip.v3i3.270. Article 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rupp MT, Warholak TL. Evaluation of e-prescribing in chain community pharmacy: Best-practice recommendations. J Am Pharm Assoc (2003) 2008;48(3):364–370. doi: 10.1331/JAPhA.2008.07031. [DOI] [PubMed] [Google Scholar]
- 27.Surescripts. The national progress report on E-prescribing and interoperable healthcare. About E-prescribing Web site. [Accessed 07/12, 2012]. Updated 2011. [Google Scholar]
- 28.Nanji KC, Rothschild JM, Salzberg C, et al. Errors associated with outpatient computerized prescribing systems. J Am Med Inform Assoc. 2011 doi: 10.1136/amiajnl-2011-000205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Campbell EM, Sittig DF, Ash JS, et al. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc. 2006;13(5):547–556. doi: 10.1197/jamia.M2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gallagher RM, Gallagher HC. Improving the working relationship between doctors and pharmacists: Is inter-professional education the answer? Adv Health Sci Educ Theory Pract. 2010 doi: 10.1007/s10459-010-9260-5. [DOI] [PubMed] [Google Scholar]
- 31.Bodenheimer T, Grumbach K. Electronic technology: A spark to revitalize primary care? JAMA. 2003;290(2):259–264. doi: 10.1001/jama.290.2.259. [DOI] [PubMed] [Google Scholar]
- 32.Endsley MR. Toward a theory of situation awareness in dynamic systems. Human Factors: The Journal of the Human Factors and Ergonomics Society. 1995;37(1):32–64. [Google Scholar]
- 33.Leonard M, Graham S, Bonacum D. The human factor: The critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care. 2004;13(Suppl 1):i85–i90. doi: 10.1136/qshc.2004.010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holden RJ. Cognitive performance-altering effects of electronic medical records: An application of the human factors paradigm for patient safety. Cogn Technol Work. 2011;13(1):11–29. doi: 10.1007/s10111-010-0141-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Porto GG. Safety by design: Ten lessons from human factors research. J Healthc Risk Manag. 2001;21(4):43–50. doi: 10.1002/jhrm.5600210408. [DOI] [PubMed] [Google Scholar]
- 36.Flynn EA, Barker KN, Gibson JT, et al. Impact of interruptions and distractions on dispensing errors in an ambulatory care pharmacy. American Journal of Health System Pharmacy. 1999;56:1319–1325. doi: 10.1093/ajhp/56.13.1319. [DOI] [PubMed] [Google Scholar]
- 37.Young KA. Direct from the source: The value of ‘think-aloud’data in understanding learning. Journal of Educational Enquiry. 2005;6(1):19–33. [Google Scholar]