Abstract
This paper addresses the issue of how to target interventions to girls 15-19 and young women 20-24 in a resource poor setting of Hwange District, Zimbabwe. The Priorities for Local AIDS Control efforts (PLACE) methodology was used to understand where these young people socialize and also to understand whether age disparate relationships were a common occurrence. Findings indicated prevention efforts for those 15-19 would need to focus on “everyday” sites as these are the places where the majority of girls socialized. However the girls 15-19 with the riskiest sexual behaviors were found at venues affiliated with alcohol. Prevention efforts for those 20-24 would also need to largely focus on venues affiliated with alcohol. Women at such sites generally reported more risky behaviors than women in other types of venues. Reporting of a partner five or more years older was common across age groups and across venues. Tackling HIV in Zimbabwe will take a multifaceted approach targeted towards the places girls 15-19 and young women 20-24 are meeting new partners.
Keywords: HIV, Zimbabwe, sexual behavior, adolescents
Introduction
Young women are at high risk for acquiring HIV around the world. Young people 15-24, particularly girls and women, account for 45% of new HIV infections around the world. In sub-Saharan Africa women account for nearly 60% of HIV infections (UNAIDS 2008), and adolescent girls and young women 18-24 are at greater risk of acquiring HIV compared to their male counterparts (Macro International Inc. 2008). For example, in Cote d'Ivore and Kenya, for every infected young man there are five infected young women (UNAIDS 2006). Corresponding ratios are one to three in Botswana, Namibia, South Africa, and Zambia (UNAIDS 2006). Zimbabwe has been particularly hard hit by the HIV epidemic, and gender differentials are quite apparent. According to the Zimbabwe 2005/2006 Demographic and Health Survey (ZDHS), HIV prevalence is 21% for women 15-49 compared to 15% for males 15-49. Among those 15-19 the prevalence was 6.2% for females versus 3.1% for males. Among those 20-24 the prevalence was 16.3% for females and 5.8% for males (CSO and Macro International 2007). Life expectancy for women in Zimbabwe is only 34 years – the lowest life expectancy in the world (WHO 2006). Thus the urgency is targeting interventions towards adolescent girls and young women.
The ZDHS indicates that knowledge of prevention methods of condom use, abstinence and having one faithful partner is lower among adolescent girls 15-19 and young women 20-24 than women 25-29 and women 30-39. For example knowledge of condom usage as a preventive measure was 67.8% for adolescent girls 15-19, 77.5% for young women 20-24, 80.6% for women 25-29 and 80.2% for women 30-39.
Zimbabwe has been affected by both a political and severe economic crisis. Once one of the most developed countries in sub-Saharan Africa, Zimbabwe is suffering from hyper-inflation, out-migration and worsening health outcomes. According to data from the ZDHS under-five mortality, which is a key indicator of both health and socioeconomic status, is higher today at 82.5/1000 than it was in 1988 at 70.6/1000.
Despite the high HIV prevalence rate and a high and rising number of orphans (about 1.3 million out of an estimated total population of 12 million), Zimbabwe receives less donor aid than other neighboring countries due largely to political turmoil in the country. In Zimbabwe the average annual donor-spending-per-HIV –infected-person is only $4 compared to $319 for Uganda, $187 in Zambia and $802 for Eritrea (UNICEF 2005). In the face of limited resources there is a clear need to target interventions to the populations most vulnerable to acquiring HIV. There is also a need for a relatively quick and inexpensive study that can yield insights into local HIV epidemics and can help program planners and policymakers target interventions for the local context.
Epidemiological theory identifies that HIV transmission is most likely to occur in certain key areas (Wasserhert and Aral 1996, Grassly, N. et al. 2001, MEASURE Evaluation 2005). The Priorities for Local AIDS Control Effort (PLACE) method is a monitoring tool focused on identifying such areas called Priority Prevention Areas (PPAs) and specific public venues for subsequent HIV prevention programs. The objective is to identify where people meet new partners and thus where prevention interventions should be focused. The PLACE method focuses on sites where new sexual partnerships are formed because the pattern of new partnerships in a community shapes its HIV epidemic Individuals with newly acquired HIV are also more infectious which is another reason why new partnerships are so important (Anderson and May 1988, Anderson 1999). The advantages of taking prevention interventions to public places include reaching individuals who may be at risk of transmitting the infection (but who are asymptomatic) and for reaching large numbers of individuals (Weir et al. 2008).
The PLACE study has been conducted in over 40 countries around the world. For the PLACE study in Zimbabwe the methodology was adapted for a particular focus on adolescent girls 15-19 and young women 20-24. A detailed technical report for this study has been published focused on both men and women which includes over 50 data tables (Singh et al. 2008). This particular paper highlights how interventions can be targeted to women by age and type of venue because of the particular vulnerability of young women.
A key risk factor that will be explored is age-disparate relationships because they are believed to be a key factor in the disparity in HIV prevalence between adolescent girls and young women compared to adolescent boys and young men (i.e. Gregson et al. 2002; Kelly et al. 2003, Luke 2003, Katz and Low-Beer 2008). The term age-disparate relationship refers to a partnership between young women and men who are 5 or more years old (Madlala 2008). (Other terms such as age-mixing and intergenerational sex are also commonly used, however sometimes those terms refer only to age differences of 10 or more years. Therefore this paper will use the term age-disparate.) A review article of 25 studies concerning age-disparate and transactional sex in sub-Saharan Africa found that both age disparity and transactional sex were quite common and were associated with an increased risk of HIV (Luke 2003). The review found that in the studies between 27 to 50% of adolescent girls had partners at least 6 years older. The review also found that while girls might have some negotiating power over partnership formation and continuation, they had little control over practices within partnerships including condom usage. Girls’ motivations for engaging in sex with older partners were assistance with economic survival, a way to secure longer-term opportunities and a means of increasing status among one's peers.
There is evidence of age disparate sex being a risk factor for young women in Zimbabwe. According to the ZDHS ,women 15-24 who reported that their first partner was 10+ years older had a HIV prevalence of 23% compared to 16% for other women. A study in Manicaland, Zimbabwe found that older age of sexual partner was associated with HIV infection for both men and women. Women tended to have partnerships with men 5 to 10 years older (Gregson et al. 2002). A study of youth 15-21 sampled at drinking establishments in Harare found that women engaged in sex work had older partners than women not engaged in sex work. The mean age difference was 5.8 for those engaged in sex work versus 3.5 for those not engaged in sex work (Mataure et al. 2002). Qualitative research on adolescents aged 16-19 in Zimbabwe indicated that girls reported that having a boyfriend 5 or more years older was normal. They also indicated that older partners often become violent with the suggestion of condom usage or if sex is refused. The authors of the study indicated that the ability of girls to negotiate safe sex was inversely related to the age of their partner (Chinake et al. 2002).
Another key factor to be explored is the type of venue where individuals socialize, particularly venues that focus on serving alcohol compared to those that do not. The relationship between alcohol usage and HIV risks has been clearly established. A review and meta-analysis of research studies focused on Africa found a direct relationship between alcohol use and being HIV positive. Individuals who consumed alcohol had between 57% to 70% increased risk of being HIV positive than nondrinkers (Fisher et al. 2007). A review focused specifically in southern Africa found a consistent relationship between alcohol use and sexual risks for HIV (Kalichman et al. 2007). In terms of the importance of venue, a recently published study in South Africa found a higher risk for HIV infection among men and women who indicated that they had met sexual partners at informal drinking places, shebeens (Kalichman et al. 2008). In a PLACE study focused on South Africa, Weir et al. (2004) found that 85% of the venues where people met new sexual partners also served alcohol. In South Africa many venues serving alcohol also are places where sex occurs (Morojele et al. 2006). In Zimbabwe the importance of beerhalls has been documented as well. In rural Manicaland, researchers found that men and women who went to beer halls were more likely to be HIV positive than those that did not. Risks were also higher for women who did not attend beerhalls but whose partners did (Lewis et al. 2005) indicating the importance of understanding not only women's risk behaviors but also the risk behaviors of their partners. Having sex while intoxicated in the past sex months was strongly associated with HIV seroconversion among men attending beerhalls in Harare (Fritz et al. 2002). The study by Mataure et. al. (2003) of youth 15-21 sampled at drinking establishments in Harare found that 60% of the women sampled had met a partner at a drinking establishment, 42% of the women sampled had sex under the influence of alcohol in the last 90 says and 63% had received money for sex in the last 90 days.
Methods
The PLACE method has five steps. The first step is to select a PPA. During a national stakeholders meeting in Harare, Zimbabwe on August 26, 2006 stakeholders selected Hwange District due to the high HIV prevalence, large number of orphans and lack of data from this district. The 2005/6 DHS indicates that Matabeleand North Province, where Hwange District is located, has the highest HIV prevalence for women 15-24 at 13.3%.
According to the 2002 Zimbabwe Census, Hwange District has a population of about 132,459. The District comprises three communities – the towns of Hwange and Victoria Falls and also Hwange rural. The PLACE method was conducted in all three communities. Hwange Discrict is a major producer of coal and is also home to Victoria Falls and both draw many visitors to Hwange District.
Steps 2 through 4 were carried out from November-December 2006. Step 2 involves identifying venues/events where people meet new sexual partners. In Zimbabwe the focus was on where young people meet partners. In Zimbabwe interviewers approached potential community informants and asked them to list the public places and events where young people are believed to meet new sexual partners. Community informants were people believed to be knowledgeable about the community and included a variety of individuals including orphans, youth, teachers, street venders, community leaders, health care workers, taxi drivers etc. In the PLACE method community informants are selected by convenience sampling. A total of 429 community informants listed 334 unique sites and events.
In Step 3 each venue/event was verified and visited, mapped using GIS and characterized. Of the 334 unique sites and events that were mentioned by the community informants, 312 were found. In nine cases venues mentioned were permanently closed and in six cases they were temporarily closed. Four of the venues could not be found and in only two cases the venue was found but there was no willing respondent for the interviewer to speak with. At each of the 312 venues/events a representative was interviewed to obtain information about the venue, the people who socialize in the venue and about existing HIV prevention programs and willingness to have such programs. A representative was typically a manager or owner of the venue or someone who worked at the venue and was knowledgeable about the venue and about the individuals who typically socialize at the venue.
The venue verification revealed that a variety of venues and events were mentioned by community informants as places where young people meet new partners. Interviewers noted the type of venue or event for each site which was found. The most common type of venue mentioned was a bar or tavern at 20%. Also commonly mentioned were hotel/hostels at 10%, nearby to school 10%, boreholes at 7%, church (6%), store (6%) and mall/shopping center (4%). Twenty-two community informants mentioned events such as concerts, sporting events and weddings. Because such events are time specific interviewers had to visit such events that happened to be ongoing during the fieldwork. Though some events such as weddings and tea parties are typically private events, the interviewers were welcomed. Overall these results indicate that young people meet partners in a variety of settings.
In Step 4 the characteristics of the people socializing at the venues/events is described. In this step venues/events were randomly selected by using a systematic fixed interval sampling strategy with the probability of selection proportional to the size of the venue. The size of the venue was determined by the number of people socializing at the venue during a busy time as reported by venue representatives. Venues were listed by geographic code and by size. Large venues have the potential to be selected more than once if their cluster code number was larger than the selection interval. This systematic fixed interval sampling strategy produces a self-weighted sample which gives each individual socializing at eligible venues an equal probability of selection for an individual interview. This sampling strategy also allows venue to be geographically distributed within a priority prevention area (PPA).
In the PLACE method the target number of individual interviews is 24 per site at 40 sites to obtain about 960 interviews (MEASURE Evaluation 2005). However, researchers quickly realized that Hwange was different from other cities which had a PLACE study in that many sites were quite small. A number of sites had fewer than six persons even at the busiest times. So in Hwange more sites were selected to obtain the target number of individuals. These additional sites were selected using the same systematic fixed interval sampling strategy with probability of selection proportional to the size of the venue.
All individuals age 15 and above were eligible for interview. Interviewers were trained to determine if individuals were sober enough to be interviewed which fortunately turned out not to be an issue. For those sites with more than 24 individuals there was an effort to select males randomly and in most cases to interview all females present because males socializing at the venues generally outnumbered females at the larger sites. In this particular study there was a strong emphasis on interviewing females under age 24. To select the male respondents interviewers started at different corners of a room and approached people at evenly spaced points along an imaginary diagonal line.
Interviews were conducted at 132 sites over a period of 12 days. A total of 529 men and 511 women socializing at these venues were interviewed. All individuals approached for an interview agreed to participate. Persons interviewed nearby schools included students, persons affiliated with the school and also individuals who were socializing in the public space close to the schools Individuals were asked about their frequency of venue attendance, number of partners, condom use and participation in HIV/AIDS prevention programs, among other things. The key variables studied for this paper focus on number of partnerships (in the past 4 weeks and past 12 months) and number of new partnerships (in the past 4 weeks and past 12 months) and transactional sex as these are risk factors for HIV. Transactional sex was defined as having given or received money in exchange for sex in the past 12 months. Condom use is also studied because it is a fundamental prevention intervention. The particular variable studied was condom use at most recent sex which minimizes recall bias and gives a good cross-sectional picture of levels of condom use (UNAIDS 2000). Age of oldest partner was asked of respondents to understand if intergenerational sex was commonly reported.
Step 5 is using findings to inform interventions. The idea behind the PLACE method is that the data should be tied to interventions. In Zimbabwe this process was began with a local dissemination meeting held in Hwange District and publication of the final report. Efforts are still ongoing to ensure the data is utilized through dissemination of the report findings.
The PLACE method is described in full detail in the PLACE Manual (MEASURE Evaluation 2005) and also in publications (Weir et al 2003; Weir et al 2004).
Statistical Analysis
Chi-square tests of group differences were done to compare selected variables. Stratification was done by age and type of venue.
Results
Venues are classified into different categories in an effort to understand importance of type of venue. Also important is understanding what types of venues are frequently most commonly by young women.
Nightlife/Drinking: eating, drinking, dancing and sleeping sites
Open/Transport-Related: transportation, public, commercial areas
Events/Private or Hidden Sites: abandoned yard, field, bush, concerts, sports events, tea parties, weddings
The Nightlife/Drinking sites include places where alcohol is often consumed or places where people meet at night. The open/transport sites are typical community locations such as schools, boreholes, shops, churches etc. Transport-related sites were included because they are also considered public sites, and we did not have a big enough sample (19 venues) to analyze them separately. The events/private or hidden sites were classified as a group because they tend to occur in (or are) private locations and are not open to the public or are events which require the purchase of a ticket.
Table 1 presents type of venue and some socioeconomic variables stratified by age. Chi-square tests of group differences were done to check for statistical significance. All comparisons presented in this table were significant at p<0.01. The largest percentage of 15-19 year olds was found in the Open-Transport Related Sites at 78%, while 14% were found in the Events/Private or Hidden Sites and only 8% in the Nightlife/Drinking Sites. In contrast about a quarter of the 20-24 year olds and 25+ women were found in the Nightlife/Drinking Sites. Only 7% of the 15-19 year olds reported that they had ever been married while 57% of those 25+ indicated that they had ever been married. About 3% of those 15-19 indicated that they were employed full-time. The percentages were 27% and 28% for those 20-24 and 25+ years old, respectively. A large percentage, about 70%, of those 15-19 were currently in school. Over 60% of those 20-24 and 25+ had completed secondary school or a higher level of education.
Table 1.
Socioeconomic Factors by Age
| Number in Category | 15-19 | 20-24 | 25+ | X2(df) | |
|---|---|---|---|---|---|
| Venue | 511 | N=287 | N=135 | N=89 | 28** (4) |
| Nightlife/drinking | 287 | 8.0 | 23.7 | 24.7 | |
| Open/Transport-related | 135 | 77.7 | 59.3 | 65.2 | |
| Events/Private or Hidden Sites | 89 | 14.3 | 17.0 | 10.1 | |
| Respondent Has Ever Been Married | 503 | N=284 | N=131 | N=88 | 104** (2) |
| Yes | 105 | 7.0 | 26.7 | 56.8 | |
| No | 398 | 93.0 | 73.3 | 43.2 | |
| Employment Status | 504 | N=285 | N=132 | N=87 | 144** (6) |
| Employed full-time | 67 | 2.8 | 26.5 | 27.6 | |
| Employed part-time/occasional | 35 | 2.1 | 10.6 | 17.2 | |
| Unemployed, looking for work | 98 | 13.7 | 31.8 | 19.5 | |
| Unemployed, not looking for work | 304 | 81.4 | 31.1 | 35.6 | |
| Student Status for those under 24 | 418 | N=287 | N=131 | NA | 132** (1) |
| Currently in school | 212 | 69.7 | 9.2 | NA | |
| Not currently a student | 206 | 30.3 | 90.8 | NA | |
| Highest Level of Schooling Completed | 506 | N=287 | N=131 | N=88 | 88** (2) |
| None or Primary | 307 | 78.4 | 35.9 | 39.8 | |
| Secondary or Higher | 199 | 21.6 | 64.1 | 60.2 |
Chi-square test for group differences significant at p<0.01
Table 2 presents ever had sex stratified by both age and type of venue. Chi-square tests of group differences were done by age group to check for statistical significance. For adolescents 15-19 reporting of ever had sex was highest by those found in the Nightlife/Drinking Sites at 61%, followed by 32% for those interviewed at the Events/Private or Hidden Sites and 18% for those at the Open/Transport-Related Sites. These differences were significant at p<0.01 with a X2 value of 28 and df=2. In contrast for young women 20-24 reporting of ever had sex was highest at the Events/Private or Hidden Sites at 91%, followed by 87% at the Nightlife/Drinking Sites and 71% at the Open/Transport-Related Sites. These differences were significant at X2 value of 7, df=2 and p<0.05. Only a small number of women 25+ were interviewed at the Events/Private or Hidden Sites so comparisons for this age group could only be made between those interviewed at the Nightlife/Drinking Sites and the Open/Transport-Related Sites. Differences were not statistically significant.
Table 2.
Ever had Sex by Type of Venue
| Number in Category | Nightlife/Drinking Sites (N=75) | Open/Transport-Related Sites (N=360) | Events/Private or Hidden Sites (N=73) | X2(df) | |
|---|---|---|---|---|---|
| Ever had Sex 15-19 | 287 | 60.9 | 17.5 | 31.7 | 28**(2) |
| Ever had Sex 20-24 | 135 | 87.1 | 70.9 | 91.3 | 7*(2) |
| Ever had Sex 25+ | 89 | 95.2 | 93.1 | NA | 0.1(1) |
| Ever had Sex Total | 511 | 81.3 | 41.4 | 58.9 | 42**(2) |
Chi-square test for group differences significant at p<0.05
Chi-square test for group differences significant at p<0.01
Table 3 presents sexual risk behaviors stratified by both type of venue and age. Few women 25+ were found at the Events/Private or Hidden Sites so these women were not compared to their peers in the other sites. Chi-square tests of group comparisons were once again done to check for statistical significance. Respondents at the Nightlife/Drinking Sites had the riskiest sexual behaviors. Respondents 15-19 and 20-24 found at the Nightlife/Drinking Sites tended to have riskier sexual behaviors compared to their peers at the other sites. Reporting of 1+ partner in the past four weeks was 48% for 15-19 year olds in the Nightlife/Drinking Sites compared to 15% in the Events/Private or Hidden Sites and 8% for those found at the Open/Transport-Related Sites. This comparison was significant at X2 value of 33, df=2 and p<0.01. Over three-quarters of 20-24 year olds in the Nightlife/Drinking Sites reported a partner in the past four weeks compared to 48% at the Events/Private or Hidden Sites and 40% in the Open/Transport-Related Sites. This comparison was significant at X2 value of 13, df=2 and p<0.01. Likewise women 15-19 and 20-24 at the Nightlife/Drinking Sites were more likely to report a new partner in the past four weeks than their peers at the other sites. Comparisons for women 25+ were not significant for 1+ partner in the past 4 weeks and 1+ new partner in the past 4 weeks.
Table 3.
Comparison of Risk Behaviors By Venue
| Number in Category | Nightlife/Drinking Sites | Open/Transport-related Sites | Events/Private or Hidden Sites | X2(df) | |
|---|---|---|---|---|---|
| 1+ partner in past 4 weeks | |||||
| AGE | |||||
| 15-19 | 287 | 47.8 | 7.6 | 14.6 | 33**(2) |
| 20-24 | 135 | 78.1 | 40.0 | 47.8 | 13**(2) |
| 25+ | 89 | 68.2 | 53.4 | NA | 1 (1) |
| Total | 511 | 66.2 | 22.2 | 32.9 | 59**(2) |
| 1+ new partner in past 4 weeks | |||||
| AGE | |||||
| 15-19 | 287 | 30.4 | 2.7 | 4.9 | 32**(2) |
| 20-24 | 135 | 31.2 | 11.3 | 21.7 | 7*(2) |
| 25+ | 98 | 18.2 | 5.2 | NA | 3(1) |
| Total | 511 | 27.3 | 4.7 | 13.7 | 40**(2) |
| 2+ partners in past 12 months | |||||
| AGE | |||||
| 15-19 | 287 | 47.8 | 3.1 | 4.9 | 65** (2) |
| 20-24 | 135 | 34.4 | 11.3 | 17.4 | 8** (2) |
| 25+ | 89 | 22.7 | 6.9 | NA | 4*(1) |
| Total | 511 | 35.1 | 5.5 | 11.0 | 58**(2) |
| 1+ new partner in past 12 months | |||||
| AGE | |||||
| 15-19 | 287 | 43.5 | 9.9 | 17.1 | 21**(2) |
| 20-24 | 135 | 43.7 | 18.8 | 34.8 | 8*(2) |
| 25+ | 89 | 22.7 | 15.5 | NA | 0.6(1) |
| Total | 511 | 37.7 | 12.7 | 26.0 | 30**(2) |
| Condom use at last sex among sexually active | |||||
| AGE | |||||
| 15-19 | 67 | NA | 66.7 | NA | NA |
| 20-24 | 108 | 62.1 | 36.2 | 52.4 | 6(2) |
| 25+ | 87 | 38.1 | 17.5 | NA | 4(1) |
| Total | 262 | 53.9 | 37.0 | 60.5 | 10** (2) |
| Give or Received Money for Sex in Past 12 Months | |||||
| AGE | |||||
| 15-19 | 67 | NA | 15.4 | NA | NA |
| 20-24 | 108 | 27.6 | 12.1 | 19.1 | 3(2) |
| 25+ | 87 | 19.1 | 5.3 | NA | 4(1) |
| Total | 262 | 30.8 | 10.4 | 16.3 | 14**(2) |
Chi-square test for group differences significant at p<0.05
Chi-square test for group differences significant at p<0.01
Respondents were also asked about numbers of partners in the past 12 months. Women interviewed at the Nightlife/Drinking Sites were most likely to report two or more partners in the 12 months. The comparison was particularly striking for those 15-19 with 48% at the Nightlife/Drinking Sites reporting two or more partners in the past 12 months, 5% at the Events/Private or Hidden Sites and 3% at the Open/Transport Related Sites (X2=65, df=2 and p<0.01). More 15-19 year olds at the Nightlife/Drinking Sites reported 2 or more partners in the past 12 months than young women 20-24 (34%). Comparisons for women 20-24 were also significant at X2=8, df=2 and p<0.01 while they were significant at X2=4, df=2 and p<0.05 for women 25+. For women 15-19, reporting of 1+ new partner in the past 12 months was also strikingly higher for those interviewed at the Nightlife/Drinking Sites (44%) compared to the Events/Private or Hidden Sites (14%) and the Open/Transport-Related Sites (10%). This comparison was significant at X2=21, df=2 and p<0.01. About 44% of young women 20-24 at the Nightlife/Drinking Sites also reported one or more new partner in the past year. Comparisons for women 20-24 were significant at X2=8, df=2 and p<0.05.
Only respondents who reported ever had sex were asked about condom use at last sex and transactional sex in the past year. Because of small cell sizes comparisons can not be made across age groups. However comparisons by type of venue indicate that women at the Events/Private or Hidden Sites were most likely to have reported using a condom at last sex (61%), compared to 54% for those at the Nightlife/Drinking Sites and 37% for women at the Open or Transport Related Sites. This comparison was significant (X2=10, df=2 and p<0.01). Approximately 31% of women at the Nightlife/Drinking Sites reported transactional sex compared to 16% at the Events/Private or Hidden Sites and 10% at the Open or Transport Related Sites (X2=14, df=2 and p<0.01).
Sexually active respondents were also asked about the ages of their oldest partners in the past 12 months. Fifty-one percent of women 15-19 indicated having an oldest partner 5 or more years older. The percentages were 47% and 48% for women 20-24 and 25+, respectively. Differences by age were not statistically significant. This variable was also stratified by type of venue. The percentages reporting an oldest partner 5 or more years older 48% for the Nightlife/Drinking Sites and the Open/Transport-Related Sites and 53% at the Events/Private or Hidden Sites. Differences were not statistically significant. Cell sizes were too small to stratify by both age and type of venue.
Respondents were not asked where they meet each of their partners. However they were asked if they ever met a new partner at the venue where they were being interviewed. When stratified by age, the percentages were 27% for 15-19, 20% for 20-24 and 12% for 25+. These comparisons were significant at X2=8, df=2 and p<0.05. When stratified by type of venue the percentages were 30% for Nightlife/Drinking Sites, 13% for Open/Transport-Related Sites and 23% for Events/Private or Hidden Sites. This comparisons was significant at X2=9, df=2 and p<0.01.
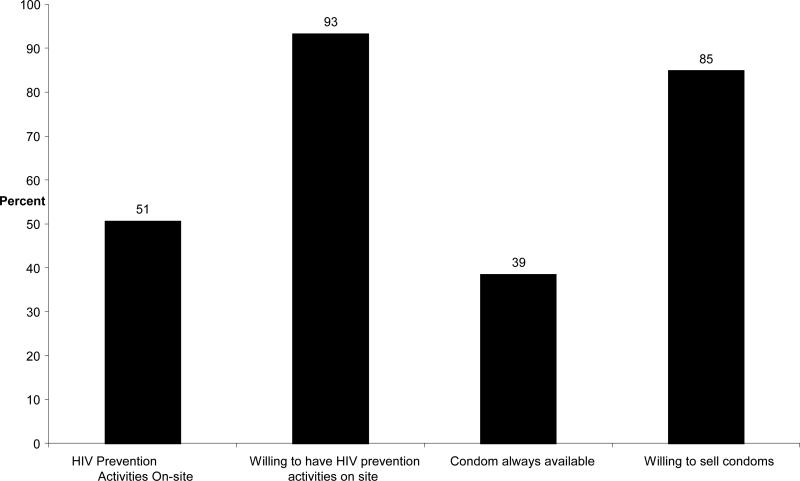
Figure 1 presents current HIV prevention efforts and willingness to participate in HIV prevention programs and condom distribution. Only 51% of venues currently had prevention activities and only 39% had condom distribution. However, willingness to participate in HIV prevention programs was high at 93% as was willingness to sell condoms at 85%. This represents an opportunity for prevention programs to link with these public sites and events. Such sites can be an important contributor in the fight against HIV. These variables were also stratified by type of venue. Willingness to have HIV prevention activities was 96% at the Open/Transport-Related Sites, 93% at the Nightlife/Drinking Sites and 82% at the Events/Private or Hidden Sites. Willingness to have condom sales or free distribution was 95% at the Nightlife/Drinking Sites and 84% at both other types of sites.
Figure 1.
HIV/AIDS prevention activities and condom availability on-site, Hwange District
Discussion
Facing limited resources, program planners and policymakers in Zimbabwe need to understand how best to target resources to the people most likely to acquire and transmit HIV. The PLACE method offers a relatively simple and quick methodology that yields valuable information about a local HIV epidemic – the places where HIV transmission is most likely to acquire.
The PLACE method yielded valuable information about where adolescent girls 15-19 and young women 20-24 socialize and potentially meet new sexual partners. Girls, 15-19, tend to socialize in everyday sorts of sites. Interventions solely targeted at bars and nightclubs which are known to be common meeting places, would completely miss the majority of those 15-19. About 92% of the 15-19 year olds were found at the everyday sites. However the 8% of the 15-19 year olds at the Nightlife/Drinking Sites had significantly more risky behaviors than 15-19 year olds found at the other sites. Interventions would need to be designed with differing aims 1) reaching the largest number of adolescents and 2) reaching those with the riskiest behaviors. These interventions thus would differ by type of venue for those 15-19
Women 20-24 at the Nightlife/Drinking Sites also had more risky sexual behaviors than their peers at the other sites. Women of this age also comprised the largest age group found at such sites. Respondents at the Nightlife/Drinking sites had significantly riskier sexual behavior than women at the Open/Transport-Related Sites and Events/Private or Hidden Sites. This finding is not surprising. Other studies have found that persons who frequent sites associated with alcohol use have riskier sexual behavior than those who do not (Lewis et al. 2005, Kalichman et al. 2008). Alcohol use and risky sexual behavior has also been well-documented (Fisher et al. 2007, Kalichman et al. 2007).
Evidence of age-disparate sex was apparent from the data for all age groups. Just over half of adolescent girls reported a partner 5 or more years older. Intergenerational sex was also commonly reported by respondents in all three types of venues. Thus it is important for prevention messages aimed at addressing this issue to be placed in all three types of venues.
The venues listed as places where young people meet new partners included “nearby to schools” and at churches. It would be important to incorporate school officials and church leaders into prevention efforts. Media campaigns can also be targeted nearby such places. Unfortunately in the past many church leaders in Zimbabwe have promoted only abstinence until marriage and have not endorsed the use of condoms (Marindo et al. 2003). A good sign from the PLACE study in Zimbabwe is that 93% of venue representatives indicated a willingness to participate in HIV prevention and 85% indicated a willingness to sell condoms.
Sexual behavior is typically difficult to measure. A study in Zimbabwe found that there was little correlation between questionnaire responses and biological evidence concerning sexual experience (Cowan et al. 2002). Other studies have indicated the difficulty in measuring sexual behavior in household surveys T(i.e. Huygens et al. 1996; Fenton et al. 2001; Cleland et al. 2004). The PLACE method takes measures to reduce such bias by using verbal, anonymous consent, assuring confidentiality and designing simple, close ended questions. In addition only individuals socializing at the venues are asked questions about their own sexual behavior. These individuals likely would feel more open to answering such questions than those in a household survey. This was the case for the comparison of the PLACE method and a household survey in Zambia (Tate et al. 2007).
Limitations of the PLACE method include community informants not mentioning important key meeting places and individuals “hiding” from interviewers in the venues. It is also possible that individuals over-report sexual partners in some venues such as the relaxed settings of bar, nightclubs etc. However in Zimbabwe individuals were interviewed in a variety of settings including some very ordinary types of sites so it could be that under-reporting would be more of an issue. Another limitation is that it is proposed that implementing interventions at venues where people meet partners would be an important strategy for prevention, but as of yet there have been no studies to document this (Weir et al. 2004).
In situations of limited resources it is important to strategize HIV intervention efforts so that they reach the people most at risk of acquiring HIV. In Zimbabwe adolescent girls and young women are most at risk for HIV and interventions to reach them must be targeted by age and by type of venue where they socialize and meet new partners. Adolescents and young women with the riskiest behaviors were found in the Nightlife/Drinking Sites thus the most cost-effective strategy would be to focus on those sites. However, given that the largest numbers of adolescents socialize in everyday sites it is still important to have prevention messages in such sites to reach the largest numbers. It would thus make sense to incorporate education messages into such sites but perhaps saving the most intensive efforts such as condom distribution for those venues frequented by individuals with the highest risk behaviors.
Acknowledgements
This study was funded by the U.S. Agency for International Development (USAID) under the terms of Cooperative Agreement GPO-A-00-03-00003-00. UNICEF Zimbabwe also provided funding for this study. The authors wish to thanks the study participants, Ilene Speizer for her helpful comments and Elizabeth Jackson for her assistance during the fieldwork.
Contributor Information
Kavita Singh, MEASURE Evaluation, UNC-Chapel Hill, CB# 8120, Chapel Hill, NC 27516, USA.
William Sambisa, MEASURE Evaluation, UNC-Chapel Hill, CB# 8120, Chapel Hill, NC 27516, USA.
Shungu Munyati, Biomedical Research and Training Institute (BRTI), Harare, Zimbabwe.
Brian Chandiwana, Biomedical Research and Training Institute (BRTI), Harare, Zimbabwe.
Alfred Chingono, University of Zimbabwe, Harare, Zimbabwe.
Roeland Monash, UNICEF Zimbabwe, Harare, Zimbabwe.
Sharon Weir, MEASURE Evaluation, UNC-Chapel Hill, CB# 8120, Chapel Hill, NC 27516, USA.
References
- Anderson R, May R. Epidemiological parameters of HIV transmission. Nature. 1998;333:514–519. doi: 10.1038/333514a0. [DOI] [PubMed] [Google Scholar]
- Anderson R. Transmission dynamics of sexually transmitted infections. In: Holmes K, Mardh P, Sparling P, editors. Sexually transmitted diseases. McGraw-Hill; New York: 1999. pp. 25–37. [Google Scholar]
- Central Statistical Office (CSO) of Zimbabwe and Macro International Inc. Zimbabwe Demographic and Health Survey 2005-06. Author; Calverton, Maryland: 2007. [Google Scholar]
- Chinake H, Dunbar M, van der Straten A, Esim S, Makunike B, Padian N. Intergenerational sex among adolescents in Zimbabwe.. Paper presented at the Fourteenth International AIDS Conference; Barcelona. 7-12 July.2002. [Google Scholar]
- Cleland J, Boerma J, Carael M, Weir S. Monitoring sexual behavior in general populations: A synthesis of lessons of the past decade. Sexually Transmitted Infections. 2004;78(Suppl 11):ii1–ii7. doi: 10.1136/sti.2004.013151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowan FM, Langhaug L, Mashungupa GP, Nyamurera T, Hargive J, Jaffar S, Peeling RW, Brown DW, Power R, Johnson AM, Stephenson JM, Bassett MT, Hayes RJ, Regai Dzive Shiri Project School-based HIV prevention in Zimbabwe: Feasibility and acceptability of evaluation trials using biological outcomes. AIDS. 2002;16(12):1673–1678. doi: 10.1097/00002030-200208160-00013. [DOI] [PubMed] [Google Scholar]
- Fenton K, Johnson A, McManus S, Erens B. Measuring sexual behavior: Methodological challenges in survey research. Sexually Transmitted Infections. 2001;77:84–92. doi: 10.1136/sti.77.2.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher J, Bang H, Kapiga S. The association between HIV infection and alcohol use: A systematic review and meta-analysis of African studies. Sexually Transmitted Disease. 2007;11:856–63. doi: 10.1097/OLQ.0b013e318067b4fd. [DOI] [PubMed] [Google Scholar]
- Fritz KE, Woelk GB, Bassett M, McFarland WC, Routh JA, Tobaiwa O, Stall RD. The association between alcohol use, sexual risk behavior and HIV infection among men attending beerhalls in Harare, Zimbabwe. AIDS and Behavior. 2007;6(3):221–228. [Google Scholar]
- Grassly N, Garnett G, Schwartlander B, Gregson S, Anderson R. The effectiveness of HIV prevention and the epidemiologic context. Bulletin of the World Health Organization. 2001;79:1121–32. [PMC free article] [PubMed] [Google Scholar]
- Gregson S, Nyamukapa CA, Garnett GP, Wambe M, Lewis JJC, Mason PR, Chandiwana SK, Anderson RM. Sexual mixing patterns and sex-differentials in teenage exposure to HIV infection in rural Zimbabwe. The Lancet. 2002;359(9321):1896–1903. doi: 10.1016/S0140-6736(02)08780-9. [DOI] [PubMed] [Google Scholar]
- Hope R. Addressing Cross-Generational Sex: A Desk Review of Research and Programs. Population Reference Bureau; Washington, D.C: 2007. [Google Scholar]
- Huygens P, Kajura E, Seeley J, Barton T. Rethinking methods for the study of sexual behavior. Social Science and Medicine. 1996;42:221–231. doi: 10.1016/0277-9536(95)00088-7. [DOI] [PubMed] [Google Scholar]
- Katz I, Low-Beer D. Why has HIV stabilized in South Africa, yet not declined further? Age and sexual behavior patterns among youth. Sexually Transmitted Diseases. 2008;35(10):837–842. doi: 10.1097/OLQ.0b013e31817c0be5. [DOI] [PubMed] [Google Scholar]
- Kalichman S, Simbayi L, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: Systematic review of empirical findings. Prevention Science. 2007;8:141–151. doi: 10.1007/s11121-006-0061-2. [DOI] [PubMed] [Google Scholar]
- Kalichman S, Simbayi L, Vermaak R, Jooste S, Cain D. HIV/AIDS Risks among men and women who drink at informal alcohol serving establishments (shebeens) in Cape Town, South Africa. Prevention Science. 2008;9:55–62. doi: 10.1007/s11121-008-0085-x. [DOI] [PubMed] [Google Scholar]
- Kelly R, Gray R, Sewankambo N, Serwadda D, Wabwirre-Mangen F, Lutalo F, Wawer M. Age differences in sexual partners and risk of HIV-1 infection in rural Uganda. Journal of Acquired Immune Deficiency Syndromes. 2003;32(4):446–451. doi: 10.1097/00126334-200304010-00016. [DOI] [PubMed] [Google Scholar]
- Lewis JJ, Garnett GP, Mhlanga S, Nyamukapa CA, Donnelly CA, Gregson S. Beer halls as a focus for HIV prevention activities in rural Zimbabwe. Sexually Transmitted Disease. 2005;32:364–369. doi: 10.1097/01.olq.0000154506.84492.61. [DOI] [PubMed] [Google Scholar]
- Luke N. Age and economic asymmetries in the sexual relationships of adolescent girls in sub-Saharan Africa. Studies in Family Planning. 2003;34(2):67–86. doi: 10.1111/j.1728-4465.2003.00067.x. [DOI] [PubMed] [Google Scholar]
- Madlala S. Age-disparate and intergenerational sex in southern Africa: The dynamics of hypervulnerability. AIDS. 2008;22(Suppl 4):S17–S25. doi: 10.1097/01.aids.0000341774.86500.53. [DOI] [PubMed] [Google Scholar]
- Marindi R, Pearson S, Casterline J. Condom Use and Abstinence Among Unmarried Young People in Zimbabwe: Which Strategy, Whose Agenda? Population Council; New York: 2003. [Google Scholar]
- MACRO International Inc. HIV Prevalence Estimates from the Demographic and Health Surveys. Macro International Inc.; Calverton, Maryland: 2008. [Google Scholar]
- MEASURE Evaluation Project . Priorities for Local AIDS Control Efforts (2005) A Manual for Implementing the PLACE Method. MEASURE Evaluation Project: University of North Carolina at Chapel Hill; Chapel Hill, NC: 2005. [Google Scholar]
- Mataure P, McFarland W, Fritz K, Kim A, Woelk G, Ray S, Rutherford G. Alcohol use and high-risk sexual behavior among adolescents and young adults in Harare, Zimbabwe. AIDS and Behavior. 2002;6(3):211–219. [Google Scholar]
- Morojele NK, Kachieng'a MA, Mokoko E, Nkoko MA, Parry CDH, Nkowane AM, Moshia KM, Saxena S. Alcohol use and sexual behavior among risky drinkers and bar and shebeen patrons in Gauteng province, South Africa. Social Science & Medicine. 2006;62:217–227. doi: 10.1016/j.socscimed.2005.05.031. [DOI] [PubMed] [Google Scholar]
- Singh K, Sambisa W, Munyati S, Chandiwana B, Chingono A, Mahati, Mashange W. PLACE in Zimbabwe: Identifying Gaps in HIV Prevention Among Young People in Hwange District. MEASURE Evaluation Project: Univerisyt of North Carolina at Chapel Hill; Chapel Hill, NC: 2008. 2006. [Google Scholar]
- Tate J, Singh K, Ndubani P, Kwmwanga J, Buckner B. Measurement of HIV Prevention Indicators: A Comparison of the PLACE Method and a Household Survey in Zambia. AIDS and Behavior. 2008 doi: 10.1007/s10461-008-9505-y. DOI 10.1007/s10461-008-9505-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS . National AIDS Programmes: A Guide to Monitoring and Evaluation. Author; Geneva: 2000. [Google Scholar]
- UNAIDS . 2006 Report on the Global AIDS Epidemic. Author; Geneva: May, 2006. 2006. [Google Scholar]
- UNAIDS . 2008 Report on the Global AIDS Epidemic. Author; Geneva: Aug, 2008. 2008. [Google Scholar]
- UNICEF [December 10, 2008];Zimbabwe's Forgotten Children. 2005 (from http://www.unicef.org/media/media_25617.html)
- Wasserheit J, Aral S. The dynamic topology of sexually transmitted disease epidemics: implications for prevention strategies. Journal of Infectious Diseases. 1996;174(Suppl 2):S201–S213. doi: 10.1093/infdis/174.supplement_2.s201. [DOI] [PubMed] [Google Scholar]
- Weir S, Pailman C, Mahlalela X, Coetzee N, Meidany F, Boerma J. From people to places: focusing AIDS prevention efforts where it matters most. AIDS. 2003;17(6):895–903. doi: 10.1097/01.aids.0000050809.06065.e0. [DOI] [PubMed] [Google Scholar]
- WHO [December 10, 2008];Country Health System Fact Sheet 2006 Zimbabwe. 2006 (from http://www.who.int/countries/zwe/en/)
- Weir SS, Tate JE, Zhusupov B, Boerma JT. Where the action is: monitoring local trends in sexual behavior. Sexually Transmitted Infections. 2004;80(Suppl 2):63–68. doi: 10.1136/sti.2004.012336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir S, Figueroa J, Byfield L, Hall A, Cummings S, Suchindran C. A randomized controlled trial to investigate impact of site-based safer sex programs in Kingston, Jamaica: Trial design, methods and baseline findings. Tropical Medicine & International Health. 2008;13(6):801–813. doi: 10.1111/j.1365-3156.2008.02057.x. [DOI] [PubMed] [Google Scholar]