Abstract
A Pancoast tumor, also called a pulmonary sulcus tumor or superior sulcus tumor, is a tumor of the pulmonary apex. It is a type of lung cancer defined primarily by its location situated at the top end of either the right or left lung. It typically spreads to nearby tissues such as the ribs and vertebrae. Most Pancoast tumors are non-small cell cancers. The growing tumor can cause compression of a brachiocephalic vein, subclavian artery, phrenic nerve, recurrent laryngeal nerve, vagus nerve, or, characteristically, compression of a sympathetic ganglion resulting in a range of symptoms known as Horner’s syndrome. Pancoast tumors are named for Henry Pancoast, a US radiologist, who described them in 1924 and 1932.The treatment of a Pancoast lung cancer may differ from that of other types of non-small cell lung cancer (NSCLC). Its position and close proximity to vital structures may make surgery difficult. As a result, and depending on the stage of the cancer, treatment may involve radiation and chemotherapy given prior to surgery. Surgery may consist of the removal of the upper lobe of a lung together with its associated structures as well as mediastinal lymphadenectomy. Surgical access may be via thoracotomy from the back or the front of the chest and modification. Careful patient selection, improvements in imaging such as the role of PET-CT in restaging of tumors, radiotherapy and surgical advances, the management of previously inoperable lesions by a combined experienced thoracic-neurosurgical team and prompt recognition and therapy of postoperative complications has greatly increased local control and overall survival for patients with these tumors.
KEYWORDS : Pancoast, lung cancer, therapy
Historical approach-evolution of therapy
In the early era, before 1950, Pancoast tumors were considered unresectable, until 1956 when Chardack and MacCallum (1) reported a cure of Pancoast tumor by performing resection followed by 65 Gy of irradiation. Five-years later, Shaw and Paulson (2) approached superior sulcus tumors by using preoperative radiation therapy followed by a posterior surgical approach. This combined approach shortly became the treatment of choice with superior 5-year survival and disease control than the preexisting treatment modalities. As a result, a dose of 30 Gy induction radiotherapy given over two week period followed by en-bloc resection through a posterolateral incision became a clear alternative in relation to radiotherapy alone. In this second era of management of Pancoast tumors, which lasted for more than 30 years, the treatment of Pancoast tumors had been based on a bimodality regimen which mainly consisted of preoperative external beam radiotherapy followed by surgery (3). Numerous preoperative radiotherapy schedules were proposed, however the basic therapeutic strategy remained unchanged.
Over the last decade, various novel techniques have been developed, offering safer and more effective resection of Pancoast tumors, particularly those invading subclavian vessels, brachial plexus, and vertebral bodies (4).
However, apart from this important evolution in surgical techniques, the most significant advancement in the treatment of Pancoast tumors has been the addition of chemotherapy to the traditional induction radiotherapy. The recognition that induction chemoradiation may substantially improve the response of patients underwent complete resection, and may offer a better long-term survival was a significant step in the treatment of these tumors (4).
Trimodality treatment with the addition of platinum based chemotherapy regimens has nowadays become the standard treatment (3). Wright et al. (5) suggested that induction of chemoradiotherapy can be safely administered with low morbidity, offering a higher complete resection rate, a high pathologic response rate, a reduced locoregional recurrence rate and better survival.
Chemoradiation treatment could offer a possible complete resection of the tumor and in some cases even sterilise it. Higher doses of radiotherapy have been proposed in order to increase the efficiency of the treatment. On the other hand, this strategy could also induce higher toxicity and increase the complications of chemoradiotherapy followed by surgical excision (6-8).
The best possible local control of the disease is a matter of high concern, since local recurrence usually causes intense pain and discomfort. Accelerated concurrent schemes of 66 Gy radiotherapy with daily cisplatin offer a promising high rate of pathologic complete response. However, surgery is essential in at least 40% of these patients in order to achieve local disease control (9).
Additionally, many centers introduced sandwich radiotherapy tumors with controversial results. Shahian and associates (10) reported improved loco-regional control and survival with sandwich external irradiation in 14 patients with lymph node involvement, tumor at the resection margin, or both. The 5-year survival rate was 50%. Ginsberg and colleagues (11) administered sandwich radiation treatment to few patients in order to assess its effectiveness but only four of them reached a long term survival. Moreover they also studied 102 patients receiving brachytherapy in addition to surgical resection. Forty-nine out of 69 patients received brachytherapy with a 5-year survival rate of 41%. Loco-regional recurrence or survival rates seemed not to be influenced by intraoperative brachytherapy, in patients who underwent complete tumor resection. In addition, they noticed a low survival rate in 55 patients who had incomplete or no resection. Intraoperative brachytherapy was administered to 53 of 55 patients. In 24 patients tumor resection was not performed and they only received brachytherapy combined with preoperative radiotherapy as primary local control treatment. Ginsberg et al. reached the point to question the role of combined surgical resection and intraoperative brachytherapy, since it did not seem to improve overall survival compared with external radiation alone.
Furthermore Hilaris et al. (12) reported improved survival with 5-year survival rate of 25% and better loco-regional control in a significant number of patients treated with intraoperative brachytherapy combined with surgical resection. Hagan et al. (13) reported an overall 5-year survival rate of 33% in patients who received irradiation followed by surgery, with prolonged survival in those who could tolerate high-dose radiation treatment.
In several reports comparing combined radio-surgical treatment for Pancoast tumors, a mean 5-year survival rate of (36.5±12.7)% (mean ± SD) was described which was much higher than the results reported with radiation treatment alone (14). Since there is no randomized trial comparing radiotherapy alone on the one hand and bimodality therapy (15) on the other, the existing evidence that outcome is better with combined radio-surgical than with high-dose radiotherapy alone (16) still remains controversial. Retrospective studies (17,18) using radiotherapy alone cannot be adequately evaluated since staging in these non-operable patients is only clinical and the mode of therapy differs among them. Survival at five years ranged from 0% to 40% depending on T stage, total radiation dose, and other prognostic factors such as weight loss. Nevertheless, survival in these series was shorter than in surgical series.
Moreover, variations in the literature exist in relation to the administered radiation dose in these patients. Whereas Paulson (19) adopted a low-dose preoperative radiation scheme administering 30 Gy over a 2-week period, resulting in a 5-year survival rate of 35%; others such as Attar and Miller (20) initially have used preoperative doses of between 40 to 60 Gy but later abandoned this scheme due increased postoperative morbidity and mortality which led them to lowering the dose to 30 Gy. Finally, others (18) did not demonstrate any significant advantage in the outcome of patients by adopting higher preoperative radiation schemes.
Kappers et al. (9) evaluated the efficacy and safety of a 66 Gy dose of radiotherapy combined with cisplatinum. Induction therapy with high-dose radiation and concurrent cisplatinum was proved to safe and highly effective in fit patients.
The approach of Shaw and Paulson is completely satisfactory in dealing with posteriorly located tumors. It is not fully adequate in the presence of invasion of anterior tumors. The third era, in the management of Pancoast tumors, between late 1980’s and 1990’s introduced the development of new surgical techniques that enabled the R0 resection of lesions involving the subclavian vessels and the vertebral bodies, which until then considered inoperable. Anterior approaches were introduced and other various methods developed by many surgeons as it will be detail further, but Dartevelle et al. (21) were the pioneer who provided adequate access to this complex anatomical region, by popularizing the anterior transcervical approach for tumors infiltrating the subclavian vessels. The reported a 5-year survival rate was 30%. Since then various modifications of this technique have been developed (22,23). Rusch et al. (24) reported that those who were managed predominantly with preoperative radiotherapy followed by surgery, the complete resection rate was 56% and 5-year survival was 46% for IIB disease, 0% for IIIA disease and 13% for IIIB disease.
These modest results offered by the bimodality approach stressed out the need for new treatment protocols. By the late 90s’ changes in the treatment of non-small cell lung cancer (NSCLC) resulted in the introduction of induction chemo-radiotherapy followed by radical surgical resection. This period started the fourth era in the treatment of superior sulcus tumors; leading to the development of a large, prospective, multicentre, phase II trial (Southwest Oncology Group 9416, INT 0160) (25). In this study eligible patients with mediastinoscopy negative, clinical T3-4, N0-1 superior sulcus tumors underwent initially induction treatment with two cycles of etoposide and cisplatin and 45 Gy of concurrent radiotherapy. This induction chemo-radiotherapy protocol could sterilize the primary lesion. Those with stable disease or tumor regression underwent thoracotomy and anatomical pulmonary resection followed by two additional cycles of chemotherapy with cisplatin and etoposide. Results were very promising since 75% of those enrolled initially, ultimately underwent thoracotomy. Additionally, 91% of participants with T3 and 87% with T4 tumors had complete R0 resection. Finally, the number of postoperative complications was not greatly increased after induction chemo-radiotherapy compared with historical experience with radiotherapy. Updated results of this phase II trial were published in 2003 (26) and long-term results in 2007 (27). They reported a 41% 5-year survival for all patients and 53% for those with complete resection. Of those patients who relapsed, only 12% recurred locally, compared to 40% of previous reports (28). This phase II trial was the beginning of others to follow that led many in the lung cancer community to accept induction chemo-radiation followed by surgery as standard of care for selected operable and borderline inoperable Pancoast tumors.
Prognosis after the above treatments were presented seems fairly divergent depending on the special features of each tumor. A 5-year survival rate has generally been 30% to 40% in patients with negative lymph nodes and complete resection of the lesion, but it has been less than 10% for patients with incomplete resection or with T4 vertebral infiltration (29). The presence of positive mediastinal lymph node is an extremely poor prognostic sign. However, metastases to the ipsilateral supraclavicular lymph nodes may be a sign of local extension of the disease, and the prognosis may be better than for N2 mediastinal lymph node metastases (29). In any case, a lobectomy seems to have superior results compared to wedge resection of the tumor (11,30). The most common cause of mortality is systemic metastases, especially to the brain. Cranial irradiation has been therefore suggested as a prophylactic measure (4,31).
Surgical indications
Detterbeck argued that the unique feature of Pancoast tumors appears not to lie in the tumor biology but rather in the anatomy of the region in which these tumors occur (32). Because these tumors involve the chest wall by definition, it is logical that these patients usually present with local rather than systemic manifestations of lung cancer. Furthermore, the local extension of these tumors involves structures that are technically difficult to approach and limit the extent of resection if major long term disability is to be avoided. Therefore, it is difficult to accomplish a complete resection (R0 resection) of these tumors (32).
Throughout the years different surgical approaches have been described, all of which should be included in the armamentarium of the thoracic surgeon since the ultimate hope for cure depends on whether a complete resection is accomplished. As a general rule, superior sulcus tumors not invading the thoracic inlet are completely resectable through the classical posterior Shaw-Paulson approach alone, although this approach does not allow a direct and safe visualization, manipulation and complete oncological clearance of all anatomical structures composing the thoracic inlet. This restricted access may be one of the reasons for the high rate of incomplete resections (33) and high surgical morbidity and mortality using this approach. The anterior transcervical approach (22) proved to be the answer to the problem of limited exposure since it appears to be the optimal method to anterior lung apex or first rib lesions (34). Over the last years, this last approach is being increasingly accepted as standard method or all benign and malignant lesions of the thoracic inlet structures other than bronchogenic cancers, as well, osteosarcomas of the first rib, or tumors of the brachial plexus.
Absolute surgical contraindications are the presence of extrathoracic sites of metastasis, N2 (mediastinal) or N3 (contralateral supraclavicular) nodal disease, invasion of the brachial plexus above T1 and invasion of the spinal canal. Histologically confirmed mediastinal N1 or N3 ipsilateral lymph node involvement is a relative contraindication. Invasion of the brachial plexus above Tl as supported by sensitive or, even worse, motor deficits in the nerve distribution of the median and radial nerves, indicate inoperability. The same stands for tumor invasion of the trachea or esophagus. Extensive involvement of the subclavian vessels is not an absolute contraindication, provided a complete surgical resection may be anticipated. Patients whose tumors invade the vertebral body should not be deemed inoperable unless there is certified invasion of the spinal canal through the intervertebral foramina. Based on preoperative imaging findings, Bruzzi et al. (35) have proposed relative and absolute criteria that contraindicate surgical excision. Thus, in terms of the TNM classification, selected patients with T3-4, N0-1 Pancoast tumors are potentially resectable. The latest version of TNM classification based on the recommendations of the International Association for the Study of Lung Cancer (IASLC) has not altered the situation much in the case of Pancoast tumors (36). According to contemporary staging principles satellite nodules in the same primary tumor lobe are referred to as T3 disease, whereas it was previously staged as T4. Even though there have been no significant changes to nodal staging, however, a nodule in a different ipsilateral lobe is now classified as T4, whereas it was previously classified as M1. Regarding operability in these patients, this change seems to be positive, as a nodule could represent a synchronous lesion rather than a metastasis and each patient should be evaluated individually. The role of palliative incomplete resection is highly questionable and without any individual benefit.
Operative techniques
The goal of operation is resection of the upper lobe along with the invaded ribs and transverse processes and all invaded structures such as the lower trunk of the brachial plexus, stellate ganglion and upper dorsal sympathetic chain. Any apical tumor without invasion of the thoracic inlet can be completely resected through the posterior Shaw-Paulson approach alone. Lesions with a high suspicion of invading the thoracic inlet should be first explored by an anterior transclavicular approach and possibly followed by the Shaw-Paulson approach. The different approaches will be described thoroughly in the following text.
Posterolateral approach (Shaw-Paulson)
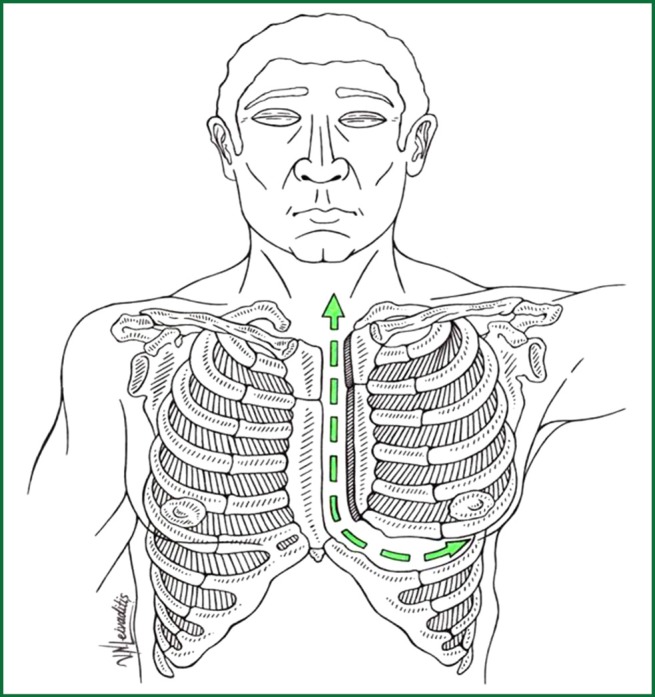
The patient is placed in the standard lateral decubitus position. The skin preparation is carried out from the base of the skull down to the iliac crest and past the mid-line posteriorly and the midline anteriorly. A long posterior thoracotomy incision is made starting superiorly midway between the spinous process of the seventh cervical vertebra and the posterior aspect of the scapula, extending downward 2 cm below the inferior angle of the scapula, ending 2 cm beyond it or just lateral to the breast in women (Figure 1). Anteriorly, the latissimusdorsi and the fascia posterior to the serratus anterior muscle are incised along their posterior edge; the serratus anterior muscle is then divided toward the lower margin of the incision. Posteriorly, the trapezius muscle is divided along the full length of the incision. Below the trapezius muscle, the levator scapulae and rhomboideus minor and major muscles are then divided in the line of the incision. This maneuver allows the scapula to be completely mobilized from the chest wall. The rhomboid muscles insert into the medial border of the scapula; Care should be taken at this stage to identify and preserve the dorsal scapular nerve and artery, which run posterior to the rhomboid muscles. Although With the scapula fully mobilized from the chest wall, upward and forward retraction is further achieved by placing a scapula retractor on its inferior angle. The next step to be determined is the relationship of the tumor to critical structures in the thoracic inlet; in other words assess its resectability. To do so, the attachments of the anterior and middle scalene muscles on the first rib and the posterior scalene muscle on the second rib are divided. The thorax is then entered through the intercostal space below the lowest rib to be resected, as determined by preoperative CT scan or MRI (usually the third intercostal space). Once the selected interspace is opened, resectability is assessed by inspection of the pleural cavity and thoracic inlet and evaluation of the extension of the tumorous process on the chest wall. Chest wall infiltration is resected primarily. Once resected, it can be released into the pleural cavity permitting a safer pulmonary resection.
Figure 1.
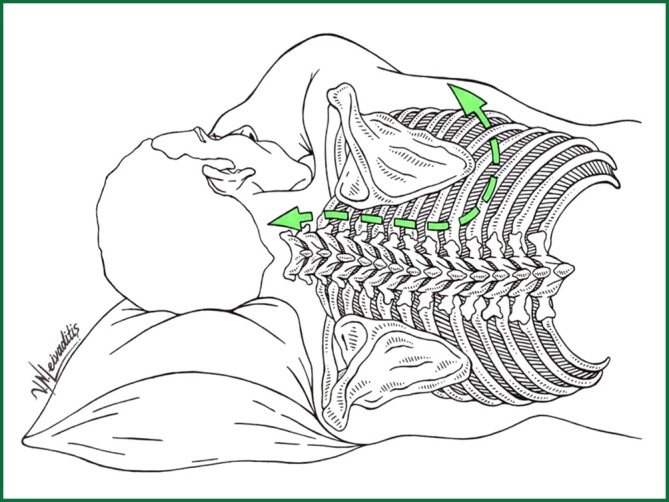
Posterolateral-Shaw-Paulson incision.
Chest wall resection
If the tumor does not involve neurovascular structures in the thoracic inlet, the chest wall resection is then performed. Once resectability has been determined, the previously made intercostal incision is extended posteriorly towards the angle of the rib, taking care to keep the incision 2-3 cm away from the costovertebral angle. The anterior border of the resection specimen is divided allowing for a 5-cm margin from the tumor. Completing the previous procedure, resection of the posterior chest wall is begun. The erector spinae muscle is incised along its anterior border and retracted laterally and posteriorly from the first to the fifth thoracic vertebrae, allowing the costovertebral gutter to be exposed. All involved ribs should be resected en bloc. Extrapleural dissection without rib removal may lead to incomplete procedures and therefore is not recommended. The division of the ribs is started anteriorly along the previously established margins of resection beginning with the healthy rib. The intercostal muscles and ribs are divided anteriorly in successive manner beginning cephalad and extending caudally as the anterior margin of the resection. Consequently the intervening intercostal neurovascular pedicles are sutured-ligated and finally divided. The anterior and middle scalenus anterior muscles are then divided with cautery, either at their insertion on the first rib or above the level of the tumor; the scalenus posterior muscle is divided where it crosses the outer border of the first rib. The superior margin of the first rib is then freed in tumor-free margins. Thereafter the relation of the apical tumor with this inlet structure is outlined and the operation continues posteriorly. After having dissected the angle of the invaded ribs, they are either disarticulated or transected at the costotransverse or transverse level, respectively. If only the parietal pleura are invaded the invaded head of the ribs are disarticulated from the transverse process without transaction. On the other hand, if the tumor erodes the ribs posteriorly, the transverse processes are transected along with the lateral cortex of the vertebrae. A crucial step at this point is the identification of the adjacent intercostal nerve and ligation with clips, since potentially devastating cerebrospinal fluid leakage may result in meningitis or tension pneumocephalus. Bleeding control at the costovertebral angle by means of electrocauteryor other hemostatic material should be avoided since potential debris may migrate into the spinal cord or occlude the anterior spinal artery. Subsequently the posterior margin is then carried superiorly until the first rib is reached.
Dissection of the brachial plexus
At this point the surgeon taking into consideration the extent of tumorous process should decide whether or not must sacrifice the nerve roots of the brachial plexus which join to form the lower trunk. The root of the 8th cervical nerve is seen above and that of 1st thoracic nerve below the neck of the first rib. Usually, the tumorous invasion is limited to the 1st thoracic nerve root; in this case, it should be divided as it emerges from the intervertebral foramen while keeping intact the 8th cervical nerve. Resection of the T1 root may result in diffuse hand weakness, but the hand remains functional. If the lesions also involve the eighth cervical nerve, then the lower trunk of the brachial plexus should be divided after its invasion. Sacrifice of the C8 nerve root or lower trunk of the brachial plexus results in permanent paralysis of the hand and its intrinsic muscles. As already mentioned, the nerve roots should be transected as they exit the intervertebral foramen and ligated in order to prevent cerebral fluid leakage.
Dissection of subclavian vessels
Although vascular involvement was once considered as relative contraindication to resection, nowadays with advances in surgical techniques and the introduction of multimodality induction therapy, tumors once characterized as unresectable can now be effectively removed. Careful dissection of the subclavian artery can usually be done following a sub adventitial plane. When the subclavian artery is encased by the tumor it should be cross-clamped, the tumorous mass removed and the vessel reconstructed with the use of an 8 mm polytetrafluoroethylene (PTFE) graft. However, in some cases invasion extends beyond the subclavian vessels into the planes of the scalene muscles and phrenic nerve. In these cases mobilization and reconstruction of subclavian vessels is very risky, therefore modification of the surgical procedure and consideration of an anterior approach can be performed. Involvement of regional branches of subclavian artery by the tumor, such as the internal mammary and the thyrocervical trunk are identified and transected if necessary.
Vertebral body resection
Vertebral column invasion by the tumor was in the past considered as contraindication for a curative surgery because of the extended nature of the process and the inability to perform a R0 resection. In addition the lack of multimodal induction therapy made many cases to remain inoperable. These procedures can be performed today by a specialized team including an orthopedic or a neurosurgeon. These techniques include laminectomy, partial and hemi-vertebrectomy involving one or more vertebral bodies, as well as resection of whole vertebral bodies. With the adoption of such curative methods, 2-year survival rates of 52% have been reported for radically resected cases in contrast to only 13% in partially resected tumors (37). Additionally, with the introduction of trimodality therapy protocols increase the rate of R0 resection above 85% (38). For tumors invading only the vertebral body, posterolateral thoracotomy with en bloc chest wall resection is accomplished. The vertebral bodies are resected with a high-speed drill and curettage of the lytic soft tissue tumor (39). Tumors involving both the vertebral body and posterior elements (spinous process, laminae, and pedicles),or extensive epidural tumors are most often resected by means of a posterior approach with posterior cervicothoracic spinal fixation followed by anterior resection and reconstruction. Posterior segmental fixation remains a challenge at the cervicothoracic junction. Its basic principle is to maintain sagittal and coronal balance and add fixation points at least two levels above and below the resected vertebral bodies.
Pulmonary resection
After resection of the chest wall the specimen is allowed to drop into the chest cavity. Upper lobectomy is the preferred procedure of choice and is performed usually through the defect of the chest wall. Mediastinal lymph node dissection is concurrently performed.
Chest wall reconstruction depends upon the site and extent of the defect. Small defects of the first three ribs or under the scapula usually remain unreconstructed, since the scapula and clavicle will cover the bony defect of the thorax. For larger defects or defects on the lower angle of the scapula which may cause impingement of the inferior tip, require chest wall reconstruction. We use a 2 mm thickness Gore-Tex patch (W.L. Gore and Associates, Arizona, USA) to reconstruct the defect.
Anterior approaches
According to Machiarini et al. (40) the introduction of anterior approaches for resection has been one of the most important advances in the surgical treatment of Pancoast tumors, allowing resection of tumors that were previously considered unresectable (41). Several anterior approaches have been described for management of superior sulcus carcinomas, but Dartevelle and colleagues (21,22) provided adequate access to this complex anatomical region, by popularizing the anterior transcervical approach for tumors infiltrating the subclavian vessels. This approach offers satisfactory visualization of the region’s major structures such as the subclavian artery, the superior vena cava, the brachial plexus, sympathetic chain, and stellate ganglion (3,42). It also allows the surgeon to perform a hemi-vertebrectomy if the anterior body of the vertebrae is infiltrated. Anterior approaches are considered to be ideal for resection of the chest wall. The morbidity of anterior approaches is less than the posterior approach (3). Moreover the postoperative stay is less in patients undergoing an anterior approach (3-6 days). It also allows extension as per Grunenwald (43), or by a high anterior thoracotomy if needed.
In the following text the proposed anterior approaches for superior sulcus lesions will be analyzed in chronological order.
The trans-sternal approach
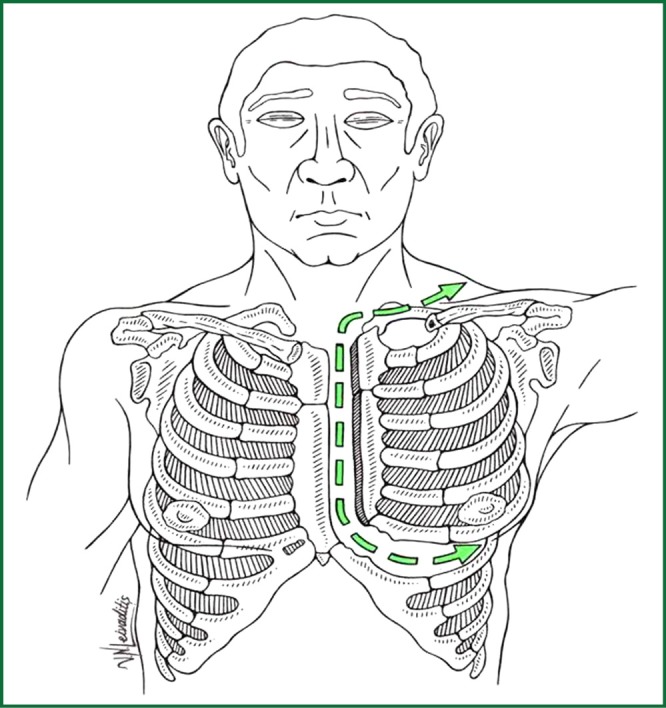
In 1979 Masaoka and colleagues (44) described and anterior approach for managing the superior sulcus tumors invading the thoracic inlet involving the vascular compartment. The patient is placed in a supine position with the neck extended and the thorax is brought forward with the aid of a pillow between the shoulders. A lateral transverse incision on the base of the neck on the affected side is continued to an upper median sternotomy and extended through the anterior 4th intercostal space (Figure 2). After division of the muscles of the neck (sternocleidomastoid, sternohyoid and sternothyroid) the chest wall is retracted and access to vascular and nervous structures of the inlet is accomplished. After resection of the chest wall and lung tissue the sternum is re-approximated and the divided muscles of the neck and thorax are sutured. Disadvantages of this incision are the potential for sternal dehiscence and resulting flail chest and the depth of exposure, particularly in obese patients. Additionally, although this approach was effective for resection of anterior tumors, adequate access to more posterior lesions, involving the head of the ribs and transverse processes of the vertebrae was difficult. For this reason in 1993 the Masaoka group proposed a variation of their initial incision the so-called “hook approach” (45), performed with a long periscapular skin incision around the axilla from the level of the 7th cervical vertebra to the midclavicular line above the nipple. In their study they concluded that the lesions of the sternum and subclavian vessels and ipsilateral supraclavicular lymph nodes were resected by the anterior approach. Lesions of the vertebrae, brachial plexus, subclavian vessels and ipsilateral supraclavicular lymph nodes could be resected by the hook approach. The anterior approach was suited for lesions in the anterior portion or middle portion and the hook approach for lesions in the middle or posterior portion. However, the “hook approach” did not receive great popularity because of the enormous extension of the incision, leading to serious wound closure complications.
Figure 2.
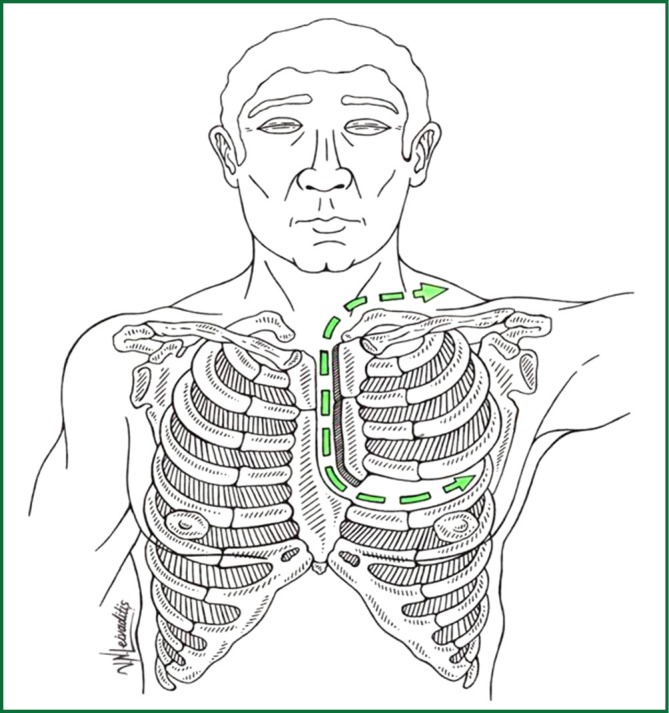
Tthetransternal-Masaoka incision.
Transcervical-thoracic approach (transclavicular)
As already mentioned in 1993, Dartevelle and colleagues popularized the anterior transcervical-thoracic approach (21). The patient is placed in the supine position with the neck hyperextended and head turned away from the involved side. A pillow is placed behind the shoulder to elevate the operative field. The skin preparation extends from the mastoid process downward to the xiphoid process and from the middle axillary line laterally to the hemiclavicular line. An L-shaped incision starting along the anterior border of the sternocleidomastoid muscle is extended horizontally below, parallel to the clavicle at the level of the second intercostal space up to the deltopectoral groove (Figure 3). Division of the sternal attachment of the sternocleidomastoid muscle is made and the cleidomastoid muscle along with the upper digitations of the ipsilateral pectoralis major muscle are dissected away from the clavicle and a myocutaneous flap is folded back to expose the thoracic inlet. Once the inferior belly of the omohyoid muscle is divided the scalene fat pad is examined to rule out lymph node metastases. Inspection of the ipsilateral superior mediastinum is then made after division of the sternothyroid and sternohyoid muscles. Additionally, the extent of infiltration of the tumor into the thoracic inlet is assessed by opening the intercostal space below the tumorous lesion. The medial half of the clavicle is removed only if the lesion is considered resectable. The distal part of the internal, external, and anterior jugular veins is divided to expose the subclavian and innominate veins. If the subclavian vein is affected then it is resected. On the left side, ligation of the thoracic duct is usually required.
Figure 3.
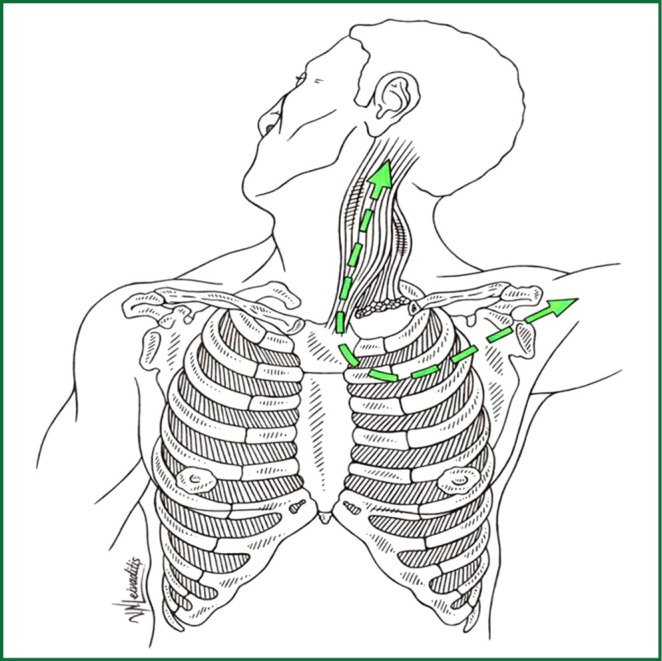
Transclavicular-Dartevelle approach.
The next step is the division of scalenus anterior muscle either on its insertion on the scalene tubercle on the first ribor in tumor-free margin. If the tumor has invaded the upper part of this muscle, it needs to be divided at the insertion on the anterior tubercles of the transverse processes of C3 through C6. The phrenic nerve should be identified and preserved, if not invaded whenever possible, since phrenic nerve dissection may result in undesirable respiratory postoperative complications. The subclavian artery is then dissected. To improve its mobilization, its branches are divided; the vertebral artery is resected only if invaded and provided that no substantial extracranial occlusive disease was detected on preoperative Doppler ultrasound. In case of artery invasion the vessel should be resected on tumor-free margins. Reconstruction of vessel lumen is performed with a 6 or 8 mm PTFE vascular graft anastomosed in an end-to-end fashion. The pleural space is usually opened by dividing Sibson’s fascia. The middle scalenus muscle is divided above its insertion on the first rib or higher according to tumorous extension. The nerve roots of C8 and Tl are identified and dissected from outwards proceeding inwards until their confluence forms the lower trunk of the brachial plexus. The ipsilateral prevertebral muscles are resected along with the paravertebral sympathetic chain and stellate ganglion from the anterior surface of the vertebral bodies of C7 and Tl. The Tl nerve root is usually divided just lateral to the T1 intervertebral foramen.
The next step in the procedure is chest wall resection followed by upper lobectomy. The anterolateral arch of the first rib is divided at the costochondral junction while the second rib is divided at the level of its middle arch and the third rib is scraped on the superior border toward the costovertebral angle. The first ribs are then disarticulated from the transverse processes of the first two or three thoracic vertebrae. Through this cavity an upper lobectomy can be performed to complete the operation. With increasing surgical experience, additional posterior thoracotomy becomes unnecessary, so that upper lobectomy and chest wall resection can be performed through the transcervical approach only.
Although this approach accounts for lower morbidity than the posterior approach, the transection of the clavicle causes postoperative alterations in the shoulder mobility and cervical posture (46). The indications to preserve and reconstruct the clavicle are limited to the combined resection of the serratus anterior muscle and long thoracic nerve. When this occurs, the scapula rotates and draws forward (scapula alata) and in combination with the resection of the internal half of the clavicle, the shoulder is pushed anteriorly and medially leading to severe aesthetic and functional discomfort. This complication led to the development of the transmanubrial L-shaped incision.
The transmanubrial approach
In 1997, Grunenwald and Spaggiari (43) introduced the transmanubrial approach (Figure 4). A manubrial L-shaped transection and first cartilage resection allow retraction of an osteomuscular flap including but sparing the clavicle and its insertion. This approach allows excellent access to the subclavicular region with safe resection of neurovascular outlet structures during the resection of apical chest tumors. Thus, the functional and cosmetic complications of clavicle resection are avoided and the postoperative morbidity is decreased.
Figure 4.
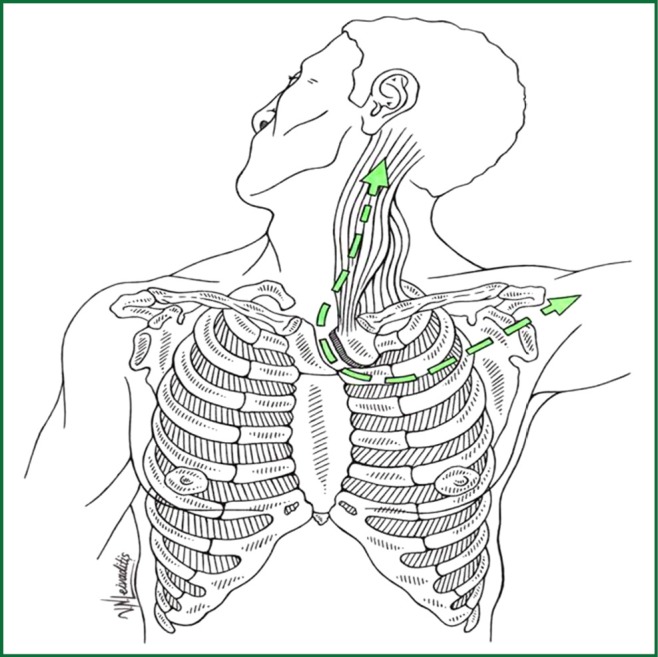
The transmanubrial approach.
Hemiclamshell and trapdoor incisions
Hemiclamshell (Figure 5) and trapdoor (Figure 6) incisions were originally applied for management of mediastinal tumors or trauma of subclavian vessels. In 1994 Bains et al. (47) of the Memorial Sloan-Kettering Cancer Center thoracic unit, followed later by Korst et al. in 1998 (48) published their results using the hemiclamshell approach for the resection of the cervico-thoracic lesions including superior sulcus tumors. Depending on the location of the tumor posterior extension of the thoracotomy may be needed. The patient is placed in a supine position with the ipsilateral side elevated. A submammary incision is continued to a partial median sternotomy up to the jugular notch. The chest wall is elevated superiorly and laterally, allowing an excellent exposure of lesions infiltrating the superior mediastinum and lung apex. The sternoclavicular junction is left untouched. The hemiclamshell incision can be diverted into a “trapdoor” incision (49) by extending the upper border of the median sternotomy towards the neck; from the median margin on the sternocleidomastoid muscle to the middle of the sternum as far as the thoracotomy. The hemiclamshell approach is closed by using sternal wires and pericostal sutures. Rarely an accessory anterior approach may be required to radically resect the infiltrated structures of the thoracic inlet, such as the distal portion of the subclavian artery. In these cases we add the hemi clamshell approach, to the transmanubrial one.
Figure 5.
Hemiclasmshell incision.
Figure 6.
The trapdoor incision.
The use of video-assisted thoracic surgery (VATS) in the management of Pancoast tumors
Nowadays the use of VATS has gradually been introduced in the diagnosis and treatment of Pancoast tumors. Candidates for surgical resection and the type of surgical approach to be chosen are usually selected and evaluated by the results provided by CT and MRI scanning tests. VATS has lately been a useful diagnostic tool to examine the extent of the tumor on the thoracic chest-wall, the thoracic inlet, the lung, the mediastinum, and the level of subclavian vessels involvement. Very few reports have been published about the usefulness of VATS in the treatment of Pancoast tumors. Vallieres et al. (29) reported the possible use of thoracoscopy for the staging and assessment of resectability only of Pancoast tumors. Roviaro et al. (50) suggested routine use of VATS as intraoperative staging for lung cancer and confirmation of resectability of the lesion.
Beshay et al. (51) obtained the diagnosis in a patient with Pancoast tumor using a biopsy through thoracoscopy. Koshiko et al. (52) announced a case of an en bloc resection of a Pancoast tumor using VATS. The patient was treated with an anterior transcervical approach and assisted by thoracoscopy in the supine position, which was then converted to a posterior thoracotomy to complete the operation without video-assistance.
Caronia et al. (53) presented a novel use of VATS as an adjunct to the surgical management of Pancoast tumors which allowed a reduction in the size of the thoracotomy, sparing the latissimusdorsi muscle without the need to perform a thoracotomy through the fourth or fifth intercostal space to explore the chest cavity. Combined anterior and posterior approaches wave been performed entirely with video-assistance and without changing the position of the patient. VATS offers excellent visualization of anatomical structures of thoracic inlet. This allows all members of the surgical team to follow in detail the surgical steps. Finally observing the chest-wall invasion through VATS helps the surgeon to confirm or change the surgical strategy intraoperatively (53).
Surgical complications
Hemothorax and exploratory reoperation due to extensive chest wall resection or pleural adhesion by the tumor may be encounter in the immediate postoperative period.
Resection of Pancoast tumors is often accompanied by thoracic instability due to chest wall resection. Moreover, inadequate postoperative analgesia and inefficient chest physiotherapy with concomitant immobilization may lead to accumulation of pulmonary secretions and lung atelectasis. Postoperative pneumonia, possibly complicated by empyema, constitutes a large proportion of the serious complications encountered. Epidural analgesia and prompt aggressive chest physiotherapy alleviates the routine need for such an approach. Fluid overload should be avoided and diuretics judiciously used to avoid ARDS.
Partial claviculectomy or hemiclaviculectomy as required by the Dartevelle approach may result in shoulder girdle instability and esthetic or functional discomfort that affects the free end of the clavicle. These led to modifications of Dartevelle approach to spare the clavicular head. Potential phrenic nerve injuries are also particular to anterior approaches and can result in significant disability. Postoperative reintubation and prolonged ventilatory support may be the end result of all of the above situations.
Vascular complications, as a consequence of subclavian arterial resection and reconstruction, may lead to severe morbidity. Intraoperative injuries or tears from traction are more likely to occur with a posterior approach to tumors with vascular involvement and may be fatal. Subclavian artery involvement is reconstructed after tumor resection with a 6-8 mm ringed PTFE graft as already proposed to minimize the risk of thrombosis and amputation. Subclavian vein thrombosis even when the vein is not involved may occur as a result of the combination of radiation therapy and surgical resection. Division of the subclavian vein without revascularization is associated with ipsilateral edema therefore; elevation of the ipsilateral arm should be encouraged.
Neurologic function may be minimally affected in case of division of T1 nerve root but severely affected in C8 root tumor invasion leading to forearm and intrinsic hand muscle weakness with paralysis of the cervical sympathetic system (Klumpke-Dejerine syndrome).
Air embolism into the subarachnoid space although rare, may be the result in case of spinal fluid leakage.
An infrequent complication due to tumorous invasion or resection of the thoracic duct at the venous angle is chylothorax. An experienced surgeon should be alert for this complication and recognize it intraoperatively. This can be managed by ligation of thoracic duct or cervical and intrathoracic lymphatics.
Prognostic factors and tumor recurrence
Various studies have been published considering the factors contributing to the prognosis of Pancoast tumors. Before the onset of the 4th era and introduction of trimodality therapy Rusch et al. have already recognized as prognostic factors for tumor recurrence the completeness of resection, and the T and N status of the tumor (24). Completeness of resection and particularly tumor invasion to the brachial plexus was also proposed by Okubo et al. (33) as indicator for prognosis. In the beginning of the new millennium and with the introduction of trimodality therapy the SWOG trial stressed the importance of achieving R0 resection margins (25). Additionally, nodal disease (N2 disease) is a poor indicator as suggested by many authors (24,54,55). Nodal status was the only significant predictor of death in multivariate analysis in the series from the Massachusetts General Hospital (13). In addition to N2 disease, Sartori (54) suggested that T4 status (vertebral body and subclavian vessel invasion) is a poor prognostic factor. Anderson et al. (55) also considered vertebral body invasion as an ominous sign and also stressed out the importance of R0 resections margins. Tumor stage predicts survival in some reports. T4 tumor was a significant predictor of death in multivariate analysis. Additionally, patients with T3 tumors had a 73% possibility to receive a complete resection in comparison to those with T4 disease (only 15%) (24).
It is obvious that incomplete resection margins are associated with high locally recurrence rates whereas R0 resection with distant metastasis. Since trimodality treatment facilitates better R0 resection one would expect a shift of clinical recurrences towards distant metastasis. Although bimodality protocols were associated with local recurrence rates with to be as high as 70% (56,57) the incidence was found to be reduced to approximately 30-40% after concurrent chemoradiotherapy (56) and after trimodality therapy is reduced even below 30% (27,38,58). Rusch et al. (26) reported a local recurrence of 12% which is considerably less compared to 40% of previous reports (28).Thus these improvements achieved in survival of Pancoast patients with the introduction of trimodality therapy are synchronously paralleled by a decrease in local recurrence.
Despite the advances in therapeutic modalities local recurrence rates are found to be significantly high (59); this high rates can be explained merely by the fact that complete resection can be achieved in less than 50% of the patients with clinical T4 disease. As already mentioned complete resection rate was achieved in only 64% of T3N0 and 39% ofT4N0 tumors.
In patients with locally advanced NSCLC who undergo induction treatment followed by surgery, the pattern of failure however shifts towards distant recurrence, particularly the brain. Pourel et al. (58) suggested the brain as the most frequent site of relapse and found a 66% rate of distant metastasis, with only an 18% of loco-regional recurrence. Komaki et al. (60) located the brain as the first site of tumor recurrence in a rate of approximately 24%.
Since brain metastases comprise a significant entity in patients with Pancoast tumors, a question is raised of whether prophylactic cranial irradiation (PCI) should be offered to patients with completely resected lesions. The negative impact of brain metastasis on survival has to be weighed against the risks benefits ration of the impact of prophylaxis with radiation to the brain until phase III trials in NSCLC with PCI are completed. However, at present there is no evidence to support the routine use of PCI in Pancoast tumours (61).
Survival and long-term outcome
From the surgeons prospective and following the oncological guidelines as with NSCLC surgery, lobectomy was associated with a better overall survival than limited pulmonary resection in patients with Pancoast tumors. Moreover, the addition of intraoperative brachytherapy to resection did not improve survival (11).
In 1994, Martinez-Monge et al. (62) published a small series of patients using preoperative chemoradiation. They reported a 56% 4-year survival rate and a 76% R0 resection rate. The treatment-related mortality of 17% although was very high.
Rusch et al. in 2000 reported an overall postoperative 5-year survival of 46% for T3N0, 13% for T4N0, and 0% for N2 lesions (24). In 2003 the updated results (25) of the initial SWOG phase II trial using trimodality therapy were reported with 41% 5-year survival for all patients and 53% for those with R0 resection; followed four years later by the publication of the long-term results of this study (27). Five-year survival was 44% for all patients and 54% after complete resection, with no difference between T3 and T4 tumors. Pathologic complete response led to better survival than when any residual disease was present. Local control and overall survival seem markedly improved relative to previous studies of radiation plus resection. In 2008 Kunitoh et al. published the JCOG trial (38) reproducing these favorable results and reporting a 56% 5-year survival, which were clearly superior to the historical value of 30%.
Moreover Tamura et al. (14) comparing the outcomes in terms of 5-year survival rates of the trimodality versus bimodality approach, reported 5-year survival rates between 44% to 59% for trimodality protocols compared to a mean of 36.5% for bimodality studies. Complete resection rates also seem better, varying from 76% to 97% compared with an average of 62% for bimodality approaches. Pathological complete response rates vary from 16% to 40.5%. Local recurrence rates of less than 30% also compare favorably with historical bimodality series.
In 2005, Kwong et al. (63) reported upon 37 patients who were treated with the trimodality protocol. They used a combination therapy of platinum-based chemotherapy concurrent with 45 Gy large-field radiotherapy to the tumor and mediastinum; followed by 14.2 Gy small-field boost radiotherapy only to the primary lesion. In their study they even enrolled patients with advanced tumorous process such as N3 disease and solitary brain metastasis. In their results, R0 surgical resection was achieved in 97.3% of patients. However, complete response was seen in 40% only and the 5-year survival of the population was 50%, despite the advanced stage of the patients. Interestingly, the occurrence or absence of recurrence in the brain did not have any influence on survival.
Future directions
Although the understanding of the biology and treat¬ment of Pancoast tumors has evolved significantly, it is clear that more progress is needed. It is always difficult to guess the direction in which further developments will take us. However some significant issues have to be stressed out: (I) the role of more aggressive surgery in cases of more extensive involvement of the brachial plexus; supportive care or treatment with radiotherapy alone often eventually lead to a functionless arm as a result of further tumor growth. Advancements in surgical techniques for Pancoast tumors now permit resection of subclavian vessels and even vertebral bodies, but extensive involvement of the brachial plexus remains a contraindication to resection. It is possible that the morbidity of such an operation is compensate by the eventual morbidity of further tumor growth if this is not doneas well as by a chance of cure; (II) the inclusion of patients with N2 disease into the pool of surgical candidates after chemo-radiation to downstage the disease. Although studies with N2 disease have clearly demonstrated a worse outcomethan those with N0-1 disease, as mentioned previously, Kwong et al. (63) included in their study patients with advanced nodal disease and after trimodality therapy depicted a 50% rate of 5-year survival; (III) the consideration of N3 ipsilateral supraclavicular lymph nodes, located in the vicinity of the lesion as local nodes with a biological behavior prognostic significance similar to that of N1 disease; (IV) the benefit of delivering high dose irradiation to T4 tumors; since in less than half of those can an R0 resection be accomplished. Additionally, despite the fact that brachial plexus can tolerate higher doses of irradiation (than the spinal cord), spinal cord tolerance deserves significant consideration when planning radiotherapy to Pancoast tumors. Today most departments recommend radiation doses between 60 and 74 Gy for the treatment of NSCLC, but limit the dose in case of the spinal cord or brachial plexus involvement. Considering that most Pancoast tumors are located in the posterior compartment the ability of delivering an adequate radiation dose to many Pancoast tumors may be impaired. Since pathological complete response rates are about 30% after induction chemo-radiation and are associated with increased survival, it may be hypothesized that dose escalation above the ‘standard’ 45 Gy in 25 fractions may increase pathological complete response and improve outcomes further (63). However, higher induction radiotherapy doses in combination with chemotherapy have been associated with an increased risk of bronchopleural fistula and air leaks (64); (V) since the incidence of brain metastasis as a first site of recurrence of these tumors is between 15-30% (60,65) the role of PCI must be examined in addition to preoperative chemo-radiotherapy in Pancoast tumors. Generally PCI is well tolerated, and it could be given postoperatively to patients with a Pancoast tumor after a complete resection has been accomplished; (VI) the experience with preoperative concurrent chemo-radiotherapy and resection has demonstrated that the majority of relapses with this approach involve distant sites, in contrast to the experience with preoperative radiotherapy alone. Thus the concurrent chemo-radiotherapy has resulted in the expected improvement in local control, and further improvements in survival must involve attempts to decrease the incidence of distant recurrences. The addition of postoperative systemic chemotherapy is supported by randomized studies of patients with non-Pancoast (66) demonstrating that systemic chemotherapy decreases the incidence of distant recurrences with a 5-15% survival benefit at five years of adjuvant chemotherapy in patients with radically resected NSCLC (66). This observation is in contrast with Martinod et al. (28) who did not demonstrated any improvement in survival benefit after addition of postoperative chemotherapy whereas they observe significant survival benefit with the addition of preoperative radiotherapy in stages IIB-IIIA. Furthermore, the ability to deliver adjuvant chemotherapy after resection of a tumorous lesion has consistently been poor since patients with Pancoast tumors may not tolerate more extensive treatment. Therefore it may be best to add several cycles of chemotherapy either before or after the concurrent chemo-radiotherapy, although this would delay resection of the Pancoast tumor; (VII) studies have shown that in patients with pulmonary adenocarcinoma who had a base-pair deletion at exon 19 (del746A750) or a point mutation at exon 21 (L858R), the tumors were highly responsive to epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (67). Additional studies with these agents showed significant response rates and progression-free survival among patients with these mutations (68,69). Since most Pancoast tumors are adenocarcinomas, this evidence associates Pancoast tumors with the EGFR. Mutation of the EGFR gene is a strong predictor of a better prognosis in adenocarcinomas treated with EGFR inhibitors such as gefitinib. Thus gefitinib may be superior to carboplatin-paclitaxel as an initial treatment for pulmonary adenocarcinoma and may be used in control of distant metastases.
Conclusions
Although the understanding of the biology and treatment of Pancoast tumors has evolved significantly, it is clear that additional studies and progress is required since they represent a small percentage of lung cancer population and impose great challenge to the lung cancer multidisciplinary team.
One of the major advances in therapy of these tumors during the last decades from the surgical aspect was the introduction of anterior approaches. These approaches increase the likelihood of complete resection and permit resection of tumors that were previously considered inoperable. Furthermore, there is no clear consensus as to the optimal standard of care due to the heterogeneity of Pancoast tumors and the subsequent lack of clinical trials. Controversy exists of whether trimodality approach should be the accepted standard therapy. In comparison to historical series; recent prospective phase II trials adopting the trimodality approach have produced promising complete resection and significant 5-year survival rates. Confirmation of these results by other studies proposes trimodality approach as a widely accepted treatment paradigm and is recommended by NCCN and ACCP guidelines (70). In addition ACCP stated that the best survival is achieved by pre-operative chemoradiotherapy followed by surgical resection in carefully selected patients (71).
Careful patient selection, improvements in imaging such as the role of PET-CT in restaging of tumors, radiotherapy and surgical advances, the management of previously inoperable lesions by a combined experienced thoracic-neurosurgical team and prompt recognition and therapy of postoperative complications has greatly increased local control and overall survival for patients with these tumors. Moreover due to the puzzling and heterogeneous nature of those tumors further prospective studies are needed to address the continuing difficulties of systemic relapse after surgery, especially in the brain.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Chardack WM, Maccallum JD. Pancoast syndrome due to bronchiogenic carcinoma: successful surgical removal and postoperative irradiation; a case report. J Thorac Surg 1953;25:402-12 [PubMed] [Google Scholar]
- 2.Shaw RR, Paulson DL, Kee JL. Treatment of superior sulcus tumor by irradiation followed by resection. Ann Surg 1961;154:29-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parissis H, Young V.Treatment of pancoast tumors from the surgeons prospective: re-appraisal of the anteriormanubrial sternal approach. J Cardiothorac Surg 2010;5:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shahian DM. Contemporary management of superior pulmonary sulcus (Pancoast) lung tumors. Curr Opin Pulm Med 2003;9:327-31 [DOI] [PubMed] [Google Scholar]
- 5.Wright CD, Menard MT, Wain JC, et al. Induction chemoradiation compared with induction radiation for lung cancer involving the superior sulcus. Ann Thorac Surg 2002;73:1541-4 [DOI] [PubMed] [Google Scholar]
- 6.Matsubara Y, Takeda S, Mashimo T.Risk stratification for lung cancer surgery: impact of induction therapy and extended resection. Chest 2005;128:3519-25 [DOI] [PubMed] [Google Scholar]
- 7.Stamatis G, Djuric D, Eberhardt W, et al. Postoperative morbidity and mortality after induction chemoradiotherapy for locally advanced lung cancer: an analysis of 350 operated patients. Eur J Cardiothorac Surg 2002;22:292-7 [DOI] [PubMed] [Google Scholar]
- 8.Venuta F, Anile M, Diso D, et al. Operative complications and early mortality after induction therapy for lung cancer. Eur J Cardiothorac Surg 2007;31:714-7 [DOI] [PubMed] [Google Scholar]
- 9.Kappers I, van Sandick JW, Burgers JA, et al. Results of combined modality treatment in patients with non-small-cell lung cancer of the superior sulcus and the rationale for surgical resection. Eur J Cardiothorac Surg 2009;36:741-6 [DOI] [PubMed] [Google Scholar]
- 10.Shahian DM, Neptune WB, Ellis FH. Pancoast tumors: improved survival with preoperative and postoperative radiotherapy. Ann Thorac Surg 1987;43:32-8 [DOI] [PubMed] [Google Scholar]
- 11.Ginsberg RJ, Martini N, Zaman M, et al. Influence of surgical resection and brachytherapy in the management of superior sulcus tumor. Ann Thorac Surg 1994;57:1440-5 [DOI] [PubMed] [Google Scholar]
- 12.Hilaris BS, Martini N, Wong GY, et al. Treatment of superior sulcus tumor (Pancoast tumor). Surg Clin North Am 1987;67:965-77 [DOI] [PubMed] [Google Scholar]
- 13.Hagan MP, Choi NC, Mathisen DJ, et al. Superior sulcus lung tumors: impact of local control on survival. J Thorac Cardiovasc Surg 1999;117:1086-94 [DOI] [PubMed] [Google Scholar]
- 14.Tamura M, Hoda MA, Klepetko W. Current treatment paradigms of superior sulcus tumours. Eur J Cardiothorac Surg 2009;36:747-53 [DOI] [PubMed] [Google Scholar]
- 15.Attar S, Krasna MJ, Sonett JR, et al. Superior sulcus (Pancoast) tumor: experience with 105 patients. Ann Thorac Surg 1998;66:193-8 [DOI] [PubMed] [Google Scholar]
- 16.Paulson DL. Carcinomas in the superior pulmonary sulcus. J Thorac Cardiovasc Surg 1975;70:1095-104 [PubMed] [Google Scholar]
- 17.Herbert SH, Curran WJ, Stafford PM, et al. Comparison of outcome between clinically staged, unresected superior sulcus tumors and other stage III non-small cell lung carcinomas treated with radiation therapy alone. Cancer 1992;69:363-9 [DOI] [PubMed] [Google Scholar]
- 18.Fuller DB, Chambers JS. Superior sulcus tumors: combined modality. Ann Thorac Surg 1994;57:1133-9 [DOI] [PubMed] [Google Scholar]
- 19.Paulson DL. Superior sulcus tumors; results of combined therapy. N Y State J Med 1971;71:2050-7 [PubMed] [Google Scholar]
- 20.Attar S, Miller JE, Satterfield J, et al. Pancoast’s tumor: irradiation or surgery? Ann Thorac Surg 1979;28:578-86 [DOI] [PubMed] [Google Scholar]
- 21.Dartevelle PG, Chapelier AR, Macchiarini P, et al. Anterior transcervical-thoracic approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 1993;105:1025-34 [PubMed] [Google Scholar]
- 22.Dartevelle PG. Herbert Sloan Lecture. Extended operations for the treatment of lung cancer. Ann Thorac Surg 1997;63:12-9 [DOI] [PubMed] [Google Scholar]
- 23.Fadel E, Missenard G, Chapelier A, et al. En bloc resection of non-small cell lung cancer invading the thoracic inlet and intervertebral foramina. J Thorac Cardiovasc Surg 2002;123:676-85 [DOI] [PubMed] [Google Scholar]
- 24.Rusch VW, Parekh KR, Leon L, et al. Factors determining outcome after surgical resection of T3 and T4 lung cancers of the superior sulcus. J Thorac Cardiovasc Surg 2000;119:1147-53 [DOI] [PubMed] [Google Scholar]
- 25.Rusch VW, Giroux DJ, Kraut MJ, et al. Induction chemoradiation and surgical resection for non-small cell lung carcinomas of the superior sulcus: Initial results of Southwest Oncology Group Trial 9416 (Intergroup Trial 0160). J Thorac Cardiovasc Surg 2001;121:472-83 [DOI] [PubMed] [Google Scholar]
- 26.Rusch VW, Giroux D, Kraut MJ, et al. Induction chemoradiotherapy and surgical resection for non-small cell lung carcinomas of the superior sulcus: prediction and impact of pathologic complete response. Lung Cancer 2003;41:S78 [Google Scholar]
- 27.Rusch VW, Giroux DJ, Kraut MJ, et al. Induction chemoradiation and surgical resection for superior sulcus non-small-cell lung carcinomas: long-term results of Southwest Oncology Group Trial 9416 (Intergroup Trial 0160). J Clin Oncol 2007;25:313-8 [DOI] [PubMed] [Google Scholar]
- 28.Martinod E, D’audiffret A, Thomas P, et al. Management of superior sulcus tumors: experience with 139 cases treated by surgical resection. Ann Thorac Surg 2002;73;1534-9; discussion 1539-40 [DOI] [PubMed] [Google Scholar]
- 29.Vallières E, Karmy-Jones R, Mulligan MS, et al. Pancoast tumors. Curr Probl Surg 2001;38:293-376 [DOI] [PubMed] [Google Scholar]
- 30.Ginsberg RJ. Resection of a superior sulcus tumor. Chest Surg Clin N Am 1995;5:315-31 [PubMed] [Google Scholar]
- 31.Komaki R, Roth JA, Walsh GL, et al. Outcome predictors for 143 patients with superior sulcus tumors treated by multidisciplinary approach at the University of Texas M.D. Anderson Cancer Center. Int J Radiat Oncol Biol Phys 2000;48:347-54 [DOI] [PubMed] [Google Scholar]
- 32.Detterbeck FC. Changes in the treatment of Pancoast tumors. Ann Thorac Surg 2003;75:1990-7 [DOI] [PubMed] [Google Scholar]
- 33.Okubo K, Wada H, Fukuse T, et al. Treatment of Pancoast tumors. Combined irradiation and radical resection. Thorac Cardiovasc Surg 1995;43:284-6 [DOI] [PubMed] [Google Scholar]
- 34.Ducic Y, Crepeau A, Ducic L, et al. A logical approach to the thoracic inlet: the Dartevelle approach revisited. Head Neck 1999;21:767-71 [DOI] [PubMed] [Google Scholar]
- 35.Bruzzi JF, Komaki R, Walsh GL, et al. Imaging of non-small cell lung cancer of the superior sulcus. Part 2: initial staging and assessment of resectability and therapeutic response. Radiographics 2008;28:561-72 [DOI] [PubMed] [Google Scholar]
- 36.Goldstraw P. eds. International Association for the Study of Lung Cancer. Staging handbook in thoracic oncology. Florida: Orange Park, 2009. [Google Scholar]
- 37.Mazel Ch, Grunenwald D, Laudrin P, et al. Radical excision in the management of thoracic and cervicothoracic tumors involving the spine: results in a series of 36 cases. Spine (Phila Pa 1976) 2003;28:782-92; discussion792. [DOI] [PubMed]
- 38.Kunitoh H, Kato H, Tsuboi M, et al. Phase II trial of preoperative chemoradiotherapy followed by surgical resection in patients with superior sulcus non-small-cell lung cancers: report of Japan Clinical Oncology Group trial 9806. J Clin Oncol 2008;26:644-9 [DOI] [PubMed] [Google Scholar]
- 39.Kent MS, Bilsky MH, Rusch VW. Resection of superior sulcus tumors (posterior approach). Thorac Surg Clin 2004;14:217-28 [DOI] [PubMed] [Google Scholar]
- 40.Macchiarini P.Resection of superior sulcus carcinomas (anterior approach). Thorac Surg Clin 2004;14:229-40 [DOI] [PubMed] [Google Scholar]
- 41.Tamura M, Hoda MA, Klepetko W. Current treatment paradigms of superior sulcus tumours. Eur J Cardiothorac Surg 2009;36:747-53 [DOI] [PubMed] [Google Scholar]
- 42.Vanakesa T, Goldstraw P.Antero-superior approaches in the practice of thoracic surgery. Eur J Cardiothorac Surg 1999;15:774-80 [DOI] [PubMed] [Google Scholar]
- 43.Grunenwald D, Spaggiari L.Transmanubrial osteomuscular sparing approach for apical chest tumors. Ann Thorac Surg 1997;63:563-6 [DOI] [PubMed] [Google Scholar]
- 44.Masaoka A, Ito Y, Yasumitsu T.Anterior approach for tumor of the superior sulcus. J Thorac Cardiovasc Surg 1979;78:413-5 [PubMed] [Google Scholar]
- 45.Niwa H, Masaoka A, Yamakawa Y, et al. Surgical therapy for apical invasive lung Cancer: different approaches according to tumor location. Lung Cancer 1993;10:63-71 [DOI] [PubMed] [Google Scholar]
- 46.Pitz CC, de la Rivière AB, van Swieten HA, et al. Surgical treatment of Pancoast tumors. Eur J Cardiothorac Surg 2004;26:202-8 [DOI] [PubMed] [Google Scholar]
- 47.Bains MS, Ginsberg RJ, Jones WG, et al. The clamshell incision: an improved approach to bilateral pulmonary and mediastinal tumor. Ann Thorac Surg 1994;58:30-2; discussion33. [DOI] [PubMed]
- 48.Korst RJ, Burt ME. Cervicothoracic tumors: results of resection by the “hemi-clamshell” approach. J Thorac Cardiovasc Surg 1998;115:286-94; discussion 294-5 [DOI] [PubMed] [Google Scholar]
- 49.Nazzaro JM, Arbit E, Burt M. ‘‘Trap-door’’ exposure of the cervicothoracic junction (technical note). J Neurosurg 1994;80:338-41 [DOI] [PubMed] [Google Scholar]
- 50.Roviaro G, Varoli F, Rebuffat C, et al. Videothoracoscopic staging and treatment of lung cancer. Ann Thorac Surg 1995;59:971-4 [DOI] [PubMed] [Google Scholar]
- 51.Beshay M, Roth T, Stein RM, et al. Tuberculosis presenting as Pancoast tumor. Ann Thorac Surg 2003;76:1733-5 [DOI] [PubMed] [Google Scholar]
- 52.Koshiko S, Inaba M, Uchida H, et al. En bloc resection for apical invading lung cancer under anterior transcervical approach and assisted thoracoscopic procedure. Kyobu Geka 2008;61:379-82 [PubMed] [Google Scholar]
- 53.Caronia FP, Ruffini E, Lo Monte AI. The use of video-assisted thoracic surgery in the management of Pancoast tumors. Interact Cardiovasc Thorac Surg 2010;11:721-6 [DOI] [PubMed] [Google Scholar]
- 54.Sartori F, Rea F, Calabrò F, et al. Carcinoma of the superior pulmonary sulcus. J Thorac Cardiovasc Surg 1992;104:679-83 [PubMed] [Google Scholar]
- 55.Anderson TM, Moy PM, Holmes EC. Factors affecting survival in superior sulcus tumors. J Clin Oncol 1986;4:1598-603 [DOI] [PubMed] [Google Scholar]
- 56.Kappers I, Belderbos JS, Burgers JA, et al. Non-small cell lung carcinoma of the superior sulcus: favourable outcomes of combined modality treatment in carefully selected patients. Lung Cancer 2008;59:385-90 [DOI] [PubMed] [Google Scholar]
- 57.Wright CD, Moncure AC, Shepard JA, et al. Superior sulcus lung tumors. Results of combined treatment (irradiation and radical resection). J Thorac Cardiovasc Surg 1987;94:69-74 [PubMed] [Google Scholar]
- 58.Pourel N, Santelmo N, Naafa N, et al. Concurrent cisplatin/etoposide plus 3D-conformal radiotherapy followed by surgery for stage IIB (superior sulcus T3N0)/III non-small cell lung cancer yields a high rate of pathological complete response. Eur J Cardiothorac Surg 2008;33:829-36 [DOI] [PubMed] [Google Scholar]
- 59.Pfannschmidt J, Kugler C, Muley T, et al. Non-small cell superior sulcus tumor: results of en bloc resection in fifty-six patients. Thorac Cardiovasc Surg 2003;51:332-7 [DOI] [PubMed] [Google Scholar]
- 60.Komaki R, Derus SB, Perez-Tamayo C, et al. Brain metastasis in patients with superior sulcus tumors. Cancer 1987;59:1649-53 [DOI] [PubMed] [Google Scholar]
- 61.Shah H, Anker CJ, Bogart J, et al. Brain: the common site of relapse in patients with pancoast or superior sulcus tumors. J Thorac Oncol 2006;1:1020-2 [PubMed] [Google Scholar]
- 62.Martínez-Monge R, Herreros J, Aristu JJ, et al. Combined treatment in superior sulcus tumors. Am J Clin Oncol 1994;17:317-22 [DOI] [PubMed] [Google Scholar]
- 63.Kwong KF, Edelman MJ, Suntharalingam M, et al. High-dose radiotherapy in trimodality treatment of Pancoast tumors results in high pathologic complete response rates and excellent long-term survival. J Thorac Cardiovasc Surg 2005;129:1250-7 [DOI] [PubMed] [Google Scholar]
- 64.Fujita S, Katakami N, Takahashi Y, et al. Postoperative complications after induction chemoradiotherapy in patients with non-small-cell lung cancer. Eur J Cardiothorac Surg 2006;29:896-901 [DOI] [PubMed] [Google Scholar]
- 65.Marra A, Eberhardt W, Pöttgen C, et al. Induction chemotherapy, concurrent chemoradiation and surgery for Pancoast tumour. Eur Respir J 2007;29:117-26 [DOI] [PubMed] [Google Scholar]
- 66.Arriagada R, Bergman B, Dunant A, et al. Cisplatin-based adjuvant chemotherapy in patients with completely resected non-small-cell lung cancer. N Engl J Med 2004;350:351-60 [DOI] [PubMed] [Google Scholar]
- 67.Paez JG, Jänne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 2004;304:1497-500 [DOI] [PubMed] [Google Scholar]
- 68.Inoue A, Suzuki T, Fukuhara T, et al. Prospective phase II study of gefitinib for chemotherapy-naive patients with advanced non-small-cell lung cancer with epidermal growth factor receptor gene mutations. J Clin Oncol 2006;24:3340-6 [DOI] [PubMed] [Google Scholar]
- 69.Rosell R, Moran T, Queralt C, et al. Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med 2009;361:958-67 [DOI] [PubMed] [Google Scholar]
- 70.NCCN Clinical Practice Guidelines in Oncology. Non-small cell lung cancer. Available online: http://www.nccn.org/professionals/physician gls/f guidelines.asp; 2007.
- 71.Shen KR, Meyers BF, Larner JM, et al. Special treatment issues in lung cancer. ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007;132:290S-305S. [DOI] [PubMed] [Google Scholar]


