Abstract
Right heart failure (RHF) is a frequent complication following left ventricular assist device (LVAD) implantation. The incidence of RHF complicates 20-50% (range, 9-44%) of cases and is a major factor of postoperative morbidity and mortality. Unfortunately, despite the fact that many risk factors contributing to the development of RHF after LVAD implantation have been identified, it seems to be extremely difficult to avoid them. Prevention of RHF consists of the management of the preload and the afterload of the right ventricle with optimum inotropic support. The administration of vasodilators designed to reduce pulmonary vascular resistance is standard practice in most centers. The surgical attempt of implantation of a right ventricular assist device does not always resolve the problem and is not available in all cardiac surgery centers.
KEYWORDS : Right heart failure (RHF), assist device, preload, afterload
Introduction
Implantable mechanical circulatory devices (MCDs), such as left ventricular assist device (LVAD), have emerged as a relevant option for improving quality of life and survival in patients with end-stage heart failure and are commonly utilized. The most common indications include bridge to transplant (BTT), bridge to candidacy (BTC), destination therapy (DT) and bridge to recovery (BTR) (1). Technological developments have led to the use of continuous flow devices which are improved compared to previous pulsatile models as far as efficiency, size, implantability, extended support, and overall patient outcomes are concerned. Results of the clinical practice led to an expanded role of LVAD clinical use (2-4). LVAD implantation improves exercise tolerance and end-organ dysfunction and can improve hemodynamics (5).
However, despite the excellent results, early right heart failure (RHF) or progressive decline of right ventricular function remains as major problems. RHF may lead to impaired LVAD flow, difficulty in weaning from cardio-pulmonary bypass (CPB), decreased tissue perfusion and multi-organ failure, which are associated with increased morbidity and mortality (6). Identifying LVAD patients at risk for RHF postoperatively still remains an unsolved problem.
This article, reviews the pathophysiology after LVAD implantation, as well as the management strategies for RHF. Patients with heart failure, who are candidates for LVAD implantation, may demonstrate a broad clinical spectrum of preoperative right ventricle (RV) dysfunction, from being relatively asymptomatic to developing fulminant right ventricular failure (RVF).
Assessment of RV function
The normal RV is the most anterior part of the heart right below the sternum. It is connected to a highly compliant pulmonary vascular system, so it acts as a volume pump (low pressure) rather than a pressure pump. RV’s stroke volume (SV) is equal to left ventricle’s (LV’s) SV, but at 25% of the stroke work. Right ventricle ejection fraction (RVEF) is less than the left ventricle ejection fraction (LVEF); 40-45% as opposed to 50-55%. Is very sensitive to a change in afterload, i.e., increased pulmonary artery pressure (PAP), but tolerates more easily volume overloading (in diastole). RV is more resistant to ischemia compared to LV due to lower coronary flow at rest and oxygen extraction.
Both ventricles are dependant to one other, thus any change in compliance, shape or size of one ventricle can affect the other (7).
Pre implantation heart failure
The presence of left heart failure (LHF) can affect RV function. Pulmonary hypertension in LHF is a frequent finding, which can lead to RV hypertrophy. RV contractility is affected, followed by RV dilatation to preserve cardiac output (CO). Over time, CO is reduced, tricuspid regurgitation (TR) ensues and hepatic venous hypertension followed by liver dysfunction may occur.
The presence of PAP >39 mmHg and RV dysfunction on heart failure patients are independent factors of mortality. Coronary ischemia [due to coronary artery disease (CAD) or due to reduced perfusion due to LHF], interventricular septum (IVS) dysfunction or cardiomyopathy, may lead to further RV deterioration. In LHF, RV preload is limited; therefore this can mask underlying RV dysfunction (7).
Post implantation heart failure
Post-successful LVAD implantation, the output of the right ventricle has to increase to match the LVAD work. This leads to increase of RV preload. Therefore, RV afterload has to be decreased in order to improve compliance. This generates pulmonary capillary wedge pressure (PCWP), PAP and right ventricle systolic pressure (RVSP) to reduce. However, leftward IVS shift and change in motion after LVAD implantation (especially in LV unloading) may impair RV contractility. TR peri-operatively may worsen due to the IVS position, increased pulmonary vascular resistance (PVR) during CPB, systemic inflammatory response syndrome (SIRS), increased preload and transfusion. High LVAD flows may lead to tricuspid annulus distortion (7).
RV function
Pre-operatively
Echocardiography remains the primary imaging modality for monitoring cardiac function in heart failure patients. Cardiac magnetic resonance imaging (MRI) has recently emerged as the gold standard but is not routinely used. Assessment of RV includes an evaluation of RV shape, size, volume, wall thickness, deviation of the septum towards the left or the right ventricle, evaluation of the dilatation of right atrium, right ventricle, of main pulmonary artery and branches, inferior vena cava dilatation and its respiratory alterations, tricuspid valve annulus, and TR degree (7).
Post implantation
Although in theory RV may benefit from a reduction of left atrium (LA) pressure, leftward IVS shift and increased venous return may lead to RV dysfunction (6). Echocardiography is the primary assessment tool for monitoring patients post LVAD implantation. Deterioration of RV function is suggested by increased RV size and TR degree compared to baseline measurements.
Reduced Tricuspid Annular Plane Systolic Excursion (TAPSE) may result from reduced RV afterload and increase in contractility to maintain a normal CO. However, an increase in RV size and a worsening of TR in conjunction with reduced TAPSE suggest worsening TR function. IVS position should be checked, as well as the pericardial space for possible effusion or thrombus which may compress the right heart (6,7).
Right heart failure
Pre-operatively, patients may present with a wide range of signs and symptoms; from being relatively asymptomatic to highly decompensated RHF. In these patients, RHF is defined as the inability of the right heart to be filled and eject normally or as the inability of the RV to provide the pulmonary circulation with adequate blood flow in the presence of a normal central venous pressure (CVP).
Post operatively, although there is a lack of a universal definition, RHF can be defined as the inability of the pulmonary circulation to fill LVAD despite maximal medical therapy; this is demonstrated as an right ventricular assist device (RVAD) implantation or extra-corporeal membrane oxygenation (ECMO) support (an extreme sign), the use of inotropic support for more than 14 days and/or inotropic support starting more than 14 days after implantation (1), inhaled nitric oxide (NO) (pulmonary vasodilator) given for more than 2-14 days post LVAD implantation, right-sided circulatory support (ECMO) or RVAD, or discharge from hospital on inotropes (8) with absence of other causes of circulatory failure (1,8,9).
In 2012, the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) applied criteria, which are presented in Table 1, for RHF post LVAD implantation in an attempt for a universal definition among different centres (9). RHF post LVAD implantation can also be classified according to the time of occurrence: intraoperatively, early or late if it occurs >14 days post-surgery (9). Potapov et al. (5) have utilized specific haemodynamic and inotropic criteria to define RHF but they not been widely used. These criteria are shown in Table 2.
Table 1. Diagnostic criteria for RVF and severity score of RVF.
| Diagnostic criteria for RV failure: |
| Symptoms and signs of persistent right ventricular dysfunction, CVP >18 mmHg with a CI <2.0 L/min/m2; |
| In the absence of elevated left atrial/pulmonary capillary wedge pressure >18 mmHg, tamponade, ventricular arrhythmias or pneumothorax; |
| Requiring RVAD implantation; or requiring inhaled nitric oxide or inotropic therapy for duration of more than one week at any time after LVAD implantation. |
| Severity scale: |
| Severe: RVAD implantation; |
| Moderate: inotropes or use of IV or inhaled pulmonary vasodilator (iNO or prostaglandin E); |
| Mild: 2 of the 4 following criteria: |
| CVP >18 mmHg or mean RA pressure >18 mmHg; |
| CI <2.3 L/min/m2 (using a pulmonary artery catheter); |
| Ascites or evidence of moderate to worse peripheral oedema; |
| Evidence of elevated CVP by echocardiogram (dilated inferior vena cava without collapse), and in physical exam (signs of increased jugular venous pressure). |
Abbreviations: RVF, right ventricular failure; RV, right ventricle; CVP, central venous pressure; CI, cardiac index; RVAD, right ventricular assist device; LVAD, left ventricular assist device.
Table 2. Potapov et al. criteria (5).
| RHF is diagnosed if any of the following: |
| Death; |
| Inability to wean from CPB. |
| Or any two of the following (sustained for 15 minutes after complete withdrawal from CPB): |
| Left ventricular flow rate index ≤2.0 liters/min/m2; |
| Administration of ≥20 IE: |
| 10 mcg/kg/min dopamine, dobutamine, enoximone, amrinone is equivalent to 10 IE; |
| 0.1 mcg/kg/min adrenaline or noradrenaline is equivalent to 10 IE; |
| 1 mcg/kg/min milrinone is equivalent to 15 IE; |
| 0.1 U/min vasopressin is equivalent to 10 IE; |
| MAP ≤55 mmHg; |
| CVP ≥16 mmHg; |
| SvO2 ≤55%. |
Abbreviations: RHF, Right heart failure; CPB, cardio-pulmonary bypass; IE, inotropic equivalents; MAP, mean arterial pressure; CVP, central venous pressure; SvO2, mixed venous oxygen saturation.
Risk factors
Most studies attempting to identify preoperative risk factors and to develop a risk scoring system are retrospective and include different models of VADs. Pre-operative risk factors for post-operative RHF are considered to be:
indication of LVAD (destination therapy being higher risk than bridge to recovery or transplantation) (4);
gender, with female being in higher risk than male gender;
existence of pre-operative circulatory failure: mechanical support (requirement of i.v. vasopressor agents, especially vasopressin and phenylephrine), pre-operative intra-aortic balloon pump, arrest at any time in the pre-operative period (8);
presence of end-organ dysfunction: pre-operative ventilator support (five times more likely to develop RVF) (7), liver dysfunction [aspartate aminotransferase (AST) ≥80 IU/L, bilirubin ≥2.0 mg/dL], renal impairment (manifested as serum creatinine ≥2.3 g/dL, or renal replacement therapy pre-operatively) (8) or malnutrition (blood urea nitrogen ≥48 mg/dL, albumin ≤3.0 g/dL) (1), coagulation abnormalities, white blood cell count ≥12.2 k/mm (1,3), platelets ≤120 k/mm (3), elevated pro-BNP, neopterin, procalcitonin, big entothelin-1, and raised C-reactive protein (CRP) (1,3,7,8);
severe RV systolic dysfunction and RV strain, as demonstrated on pre-operative TTE (10) (new emerging technique: two-dimensional global longitudinal RV strain imaging): RV end-diastolic diameter (RVEDD) >35 mm, RVEF <30%, and right atrial dimension >50 mm (11);
presence of pulmonary vascular disease; with haemodynamic parameters such as elevated CVP (≥15 mmHg) or CVP/PCWP (≥0.63) (1), low right ventricular stroke work index (RVSWI) ≥300 mmHg mL/m2, low PAP, low cardiac index (CI), low mean arterial pressure (MAP), high PVR (1,2,7,10,12);
other risk factors include: non-ischaemic cardiomyopathy, reoperation, presence of severe TR pre operatively (7). Moreover, the presence of pulmonary thrombi in patients pre LVAD implantation (venous thromboembolism—DVT and/or PE—has a higher incidence in congestive heart failure) increases significantly the risk for postoperative RHF (13).
A study by Raina et al., combined the RV fractional area change (RV FAC), which is estimated by the right atrial pressure (RAP) and the left atrial volume (LAV) index as shown on pre-operative echocardiogram, into a scoring system and suggested that low RV FAC, high RAP and low LAV index may predict RHF post LVAD implantation (14).
Kato et al. suggested that signs of dilated ventricles (LVED dimension, LA size relative to LVED dimension and LVEF) are more prone to IVS shift thus susceptible to RHF post op (15).
The optimal hemodynamic parameters of preoperatively RV function indicating a low likelihood of developing RVF are the followings:
CVP ≤8 mmHg;
PCWP ≤18 mmHg;
CVP/PCWP ≤0.66;
PVR <2 wood units;
RVSWI ≥400 mmHg mL/m2.
Risk scores
Risk scoring systems have been suggested by many authors; however none has been validated on prospective studies. Matthews et al. (8), having studied a population of 197 patients with LVAD implantation, identified the use of vasopressor, creatinine ≥2.3 mg/dL, bilirubin ≥2 mg/dL and AST ≥80 IU/L as independent risk factors and developed the following risk score (16):
| Matthews’ score =4 (vasopressor requirement) +2 (if AST ≥80 IU/L) +2.5 (if bilirubin ≥2.0 mg/dL) + 3 (creatinine ≥2.3 mg/dL or renal replacement therapy). |
Fitzpatrick et al. studied a population of 266 patients receiving different types of LVAD (17). Cardiac index ≤2.2 L/min/m2, RVSWI ≤0.25 mmHg mL/m2, severe RV dysfunction, Cr ≥1.9 mg/dL, previous cardiac surgery and systolic blood pressure (SBP) ≤96 mmHg were identified as risk factors for RHF post operatively, which was defined as the need for RVAD implantation. They developed a formula and a risk score, in which a calculated score more than 50 is prone for Bi-ventricular assist device (BiVAD) implantation, with a sensitivity of 83% and a specificity of 80% (16).
| Fitzpatrick’s score =18 (cardiac index, L/min) +18 (RV stroke work index, mmHg L/m2) +17 (creatinine, mg/dL) +16 (previous cardiac surgery) +16 (RV dysfunction) +13 (systolic blood pressure, mmHg). |
More recently, in 2010 Drakos et al., in a retrospective study of 175 patients receiving either pulsatile or continuous flow LVADs, identified the use of intra-aortic balloon pump (IABP), PVR value, inotropic dependency, obesity, angiotensin converting enzyme inhibitor (ACEi)/ARB and b-blocker use and destination therapy, as risk factors for RHF, which was defined as the need for inotropic support for more than 14 days, inhaled NO for more than 48 hours or RVAD implant (18). They developed a prediction model which divided patients in four risk groups. The incidence of RHF was 11% in the lowest risk group and 83% in the highest risk group (16).
| Drakos’ score =3.5 (destination therapy) +4 (intra-aortic balloon) +4 (pulmonary vascular resistance: 1 if PVR <1.7 Wood units, 2 if 1.8-2.7 Wood units, 3 if 2.8-4.2 Wood units, 4 if >4.3 Wood units) +2.5 (inotrope dependency) +2 (obesity) +2.5 (angiotensin converting enzyme inhibitor and/or angiotensin II receptor blocker) +2 (β-blocker). |
In 2012, Pettinari et al. published a retrospective study of 59 patients where the above three scores were calculated (16). They revealed that these RV failure scores failed to predict the actual need for RV support after LVAD implantation. By using multivariate analysis, they indicated that the presence of non-ischaemic (dilated) cardiomyopathy was the major predictor for RV failure. The incidence of RVAD implantation was 23% and BiVAD was more frequently required for female, young patients and in non-ischaemic cardiomyopathy. In 2009, a study using the INTERMACS data, compared INTERMACS levels I and II patients (sicker decompensation) with levels III and IV patients, in terms of postoperatively complications and mortality, but they were unable to specifically predict RHF (19).
On the Assessment of Right Ventricle before the Implantation of Left Ventricular Assist Device by Echocardiographic Parameters (ARVADE) study, Aissaoui et al. calculated FAC (%), Basal end-diastolic RV diameter (mm), RV Tissue Doppler Systolic Velocity and TAPSE and suggested that an ARVADE score >2 can predict the occurrence of RVF with 92% sensibility and 67% specificity (20).
RHF prevention
The need to optimize preload, contractility and afterload peri-operatively is the cornerstone for RHF prevention, especially in patients with pre-operative RV dysfunction. Adequate ventilation, acid-base balance, sinus rhythm (SR) or atrio-ventricular (AV) synchronicity, temperature and coagulopathy prevention should be maintained.
The maintenance of CVP <15 mmHg is mandatory to avoid RHF post implantation. Therefore, aggressive diuresis or continuous veno-venous hemodialysis (CVVHD) may be used to reduce preload if needed. Some researchers suggest preoperative management of raised PVR, by measuring PAP with Swan-Ganz catheters and advance pulmonary vasodilators if needed (21). Preoperative coagulopathy must to be corrected, because it predisposes to bleeding and increases the need for blood transfusion. Studies on first-generation LVADs have validated the administration of vitamin K preoperatively or aprotinin intraoperatively to reduce bleeding (22).
Although pre-operative use of IABP is considered a risk factor for RHF post implantation, some authors suggest using it, if LV function cannot be adequately supported by pharmacological therapy. The goal is to ultimately preserve RV function. In our department we have utilized IABP in decompensated cardiac failure and have found that it improves CI and corrects right heart pressures. MPAP, RA pressure and PCWP decreased, as well as RV base and mid RV diameter, while RVSm and RVSWI increased post IABP insertion. Also, biochemical markers like serum creatinine and total bilirubin decreased. In one selected patient we inserted IABP to the right subclavian artery via a graft for total mobilization, for a total period of 187 days.
Medication
Although beta-blockers or/and ACEi are used for LV dysfunction, they are not ideal medication for RV dysfunction. RV can be supported with inotropes like milrinone, levosimendan and doboutamine, which allow pulmonary vasodilation. Inhaled NO and sildenafil (phosphodiesterase inhibitor) can be used to reduce PVR. Adrenaline also can be used to maintain adequate SBP for coronary perfusion (7).
A prospective, randomized, double-blind, multicentre, placebo-controlled trial conducted in USA and Germany between 2003 and 2008, studied the effects of inhaled NO which was given prophylactically to prevent post-operative RHF in patients undergoing LVAD implantation. NO was initiated before weaning from CPB and continued until the patient was either extubated, reaching an end-point in the study or was treated for 48 hours. Inhaled NO was found to decrease MPAP and increase LVAD flow. However, this study did not statistically prove that iNO actually reduced RHF occurrence. There is a suggestion that patients most likely to benefit were those with high PAP or low pump flow rate during weaning from CPB (5,6).
Ideally, inotropes should be weaned as soon as possible, even on postoperative day 1, as mortality is strongly correlated with inotrope duration (23).
Heart rate must be maintained at 80-100 bpm. This can be achieved by using cardioversion, MgSO4 or digoxin if >100 bpm and DDD pacing, adrenaline or isoproterenol if heart rate is slow. Normal sinus rhythm can be maintained/restored by using MgSO4, amiodarone or lidocaine.
Surgical management
TR may worsen postoperative due to an IVS shift to the left. The decision to perform TV repair during LVAD implantation is correlated to: TV annulus >40 mm and moderate or severe TR. If TR is corrected this may help venous flow and renal perfusion and may improve postoperative morbidity (7).
There are reports indicating the significance of reducing RV overload in pulmonary hypertension. The creation of a right-to-left shunt by interposition of a pulmonary artery-LA graft with or without a lung assist device has shown significant improvement in RV function (24,25).
Myocardial ischemia, presence of RV thrombus, development of SIRS, mechanical compression of the PA, is some of the intra-operative factors that may contribute to RHF (12). In order to reduce the possibility of SIRS development, the amount of blood loss and also reduce the postoperative morbidity, researchers suggest procedures such as off-pump implantation of LVAD and minimal invasive approaches (7). Control of CBP time, meticulous surgical technique, adequate myocardial protection, continuous ventilation during CPB, careful de-airing using TOE guidance or CO2 insufflation in the pericardium are mandatory procedures for successful weaning from CPB. Careful must be taken in LV volume, which has to be adequate to prevent leftward IVS shift. The LVAD flow, can and must be adjusted (increased or decreased) under TEE guidance, in order to optimize RV function (7).
Hypoxia, hypercapnia and acidosis should be avoided by using low PEEP after weaning from CPB. Protamine should be given slowly only once the patient is hemodynamically stable (7).
If all the other interventions, have failed to improve RV function, then, mechanical means have to be utilized to restore blood flow to the pulmonary circulation and increase LV preload. In the early 1980s, pulmonary artery balloon pumps were used to support the failing RV. This method may be used for a shorter duration in patients with up to a 50% reduction in optimal RV performance and it is not suitable for prolonged use or as reliable RVAD (7,11,13).
Peripheral veno-arterial ECMO for RV support is an alternative. However, ECMO does not unload the ventricles as effectively as a ventricular assist device and has a high rate of complications like thromboembolism, hemolysis, and bleeding (7,11,13). The right atrium to pulmonary artery bypass using an ECMO circuit or paracorporeal devices are widely accepted (11). Experimentally, pulmonary artery bypass to LA may reduce RV overload and increase of LV preload (24,25).
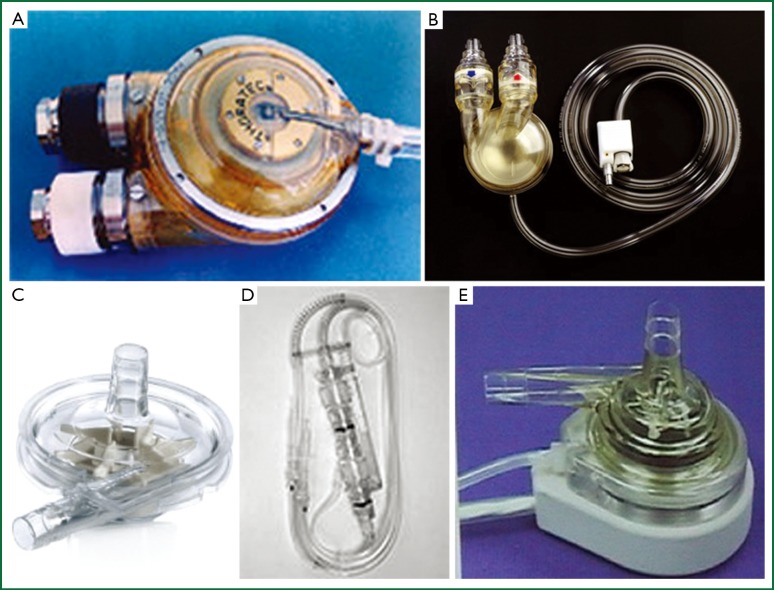
Intraoperative RHF is recognized when the cardiac index remains less than 2.0 L/min/m2 and CVP is greater than 20 mmHg. If this situation occurs and weaning from CBP is unfeasible, then a temporary RVAD may be considered, before leaving the operating theatre. The CentriMag (Levitronix, Waltham, Massachusetts, USA), the Abiomed (Abiomed, Danvers, Mass), the Tandem Heart (Cardiac Assist, Pittsburgh, Pa), and the paracorporeal Thoratec VAD (Thoratec Corp., Pleasanton, California, USA) are the most frequently assist devices used for temporary RV support (Figure 1); as a last solution when RHF does not respond to medical treatment (1,12).
Figure 1.
Ventricular assist devices used in right ventricular failure. (A) Thoratec® pVAD; (B) Abiomed AB5000TM VAD; (C) Thoratec Centrimag® Blood pump; (D) Abiomed BVS 5000TM VAD; (E) TandemHeartTM pVAD.
The ideal device for RV support should be one that is easy to implant and explant, provides adequate RV support, requires minimal anticoagulation, and is relatively inexpensive. Different minimally invasive approaches have been described for RVAD implantation: through vessel grafts, cannulation of the outflow graft through the right pulmonary artery between ascending aorta and superior vena cava (SVC) with Seldinger technique, left lateral thoracotomy and RVAD implantation, transcutaneous RVAD via sternotomy, temporary percutaneous RVAD using a centrifugal pump (11).
Some studies suggest that elective BiVAD implantation or early RVAD implantation at the time of surgery; have better survival rates than urgent implantation >24 h from surgery (1,10,26,27). Therefore, risk assessment for RHF should be performed preoperatively to assess the need for initial BiVAD implantation or total artificial heart.
In the last years, the need for RVAD during LVAD implantation has decreased significantly, as demonstrated on INTERMACS report of 2011. The implantation rate has decreased from 24.7% in 2006 to 5% in 2011 and 2.9% in 2012, for which responsible is better patient selection for LVAD (28).
Conclusions
RHF is the major cause of morbidity and mortality post LVAD implantation. Preoperative dysfunction and strain of the right ventricle are prone to postoperative RHF. Further studies are needed to create a universal risk score that includes clinical, hemodynamic and imaging parameters. The use of prophylactic inhaled NO or sildenafil is still needed to be investigated for its utility. Meticulous surgical techniques to minimize post CPB complications like SIRS are necessary in order to prevent RHF.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Kormos RL, Teuteberg JJ, Pagani FD, et al. Right ventricular failure in patients with the HeartMate II continuous-flow left ventricular assist device: incidence, risk factors, and effect on outcomes. J Thorac Cardiovasc Surg 2010;139:1316-24 [DOI] [PubMed] [Google Scholar]
- 2.Miller LW, Pagani FD, Russell SD, et al. Use of a continuous-flow device in patients awaiting heart transplantation. N Engl J Med 2007;357:885-96 [DOI] [PubMed] [Google Scholar]
- 3.Slaughter MS, Rogers JG, Milano CA, et al. Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med 2009;361:2241-51 [DOI] [PubMed] [Google Scholar]
- 4.Pagani FD, Miller LW, Russell SD, et al. Extended mechanical circulatory support with a continuous-flow rotary left ventricular assist device. J Am Coll Cardiol 2009;54:312-21 [DOI] [PubMed] [Google Scholar]
- 5.Potapov E, Meyer D, Swaminathan M, et al. Inhaled nitric oxide after left ventricular assist device implantation: a prospective, randomized, double-blind, multicenter, placebo-controlled trial. J Heart Lung Transplant 2011;30:870-8 [DOI] [PubMed] [Google Scholar]
- 6.Kukucka M, Potapov E, Stepanenko A, et al. Acute impact of left ventricular unloading by left ventricular assist device on the right ventricle geometry and function: effect of nitric oxide inhalation. J Thorac Cardiovasc Surg 2011;141:1009-14 [DOI] [PubMed] [Google Scholar]
- 7.Meineri M, Van Rensburg AE, Vegas A. Right ventricular failure after LVAD implantation: prevention and treatment. Best Pract Res Clin Anaesthesiol 2012;26:217-29 [DOI] [PubMed] [Google Scholar]
- 8.Matthews JC, Koelling TM, Pagani FD, et al. The right ventricular failure risk score a pre-operative tool for assessing the risk of right ventricular failure in left ventricular assist device candidates. J Am Coll Cardiol 2008;51:2163-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holman WL. Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS): what have we learned and what will we learn? Circulation 2012;126:1401-6 [DOI] [PubMed] [Google Scholar]
- 10.Grant AD, Smedira NG, Starling RC, et al. Independent and incremental role of quantitative right ventricular evaluation for the prediction of right ventricular failure after left ventricular assist device implantation. J Am Coll Cardiol 2012;60:521-8 [DOI] [PubMed] [Google Scholar]
- 11.Haneya A, Philipp A, Puehler T, et al. Temporary percutaneous right ventricular support using a centrifugal pump in patients with postoperative acute refractory right ventricular failure after left ventricular assist device implantation. Eur J Cardiothorac Surg 2012;41:219-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patlolla B, Beygui R, Haddad F.Right-ventricular failure following left ventricle assist device implantation. Curr Opin Cardiol 2013;28:223-33 [DOI] [PubMed] [Google Scholar]
- 13.Stepanenko A, Potapov EV, Krabatsch T, et al. Right ventricular failure after left ventricular assist device implantation with concomitant pulmonary embolectomy needing right ventricular assist device support in a patient with terminal heart failure and asymptomatic pulmonary thrombus. Interact Cardiovasc Thorac Surg 2010;10:154-5 [DOI] [PubMed] [Google Scholar]
- 14.Raina A, Seetha Rammohan HR, Gertz ZM, et al. Postoperative right ventricular failure after left ventricular assist device placement is predicted by preoperative echocardiographic structural, hemodynamic, and functional parameters. J Card Fail 2013;19:16-24 [DOI] [PubMed] [Google Scholar]
- 15.Kato TS, Farr M, Schulze PC, et al. Usefulness of two-dimensional echocardiographic parameters of the left side of the heart to predict right ventricular failure after left ventricular assist device implantation. Am J Cardiol 2012;109:246-51 [DOI] [PubMed] [Google Scholar]
- 16.Pettinari M, Jacobs S, Rega F, et al. Are right ventricular risk scores useful? Eur J Cardiothorac Surg 2012;42:621-6 [DOI] [PubMed] [Google Scholar]
- 17.Fitzpatrick JR, 3rd, Frederick JR, Hsu VM, et al. Risk score derived from pre-operative data analysis predicts the need for biventricular mechanical circulatory support. J Heart Lung Transplant 2008;27:1286-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drakos SG, Janicki L, Horne BD, et al. Risk factors predictive of right ventricular failure after left ventricular assist device implantation. Am J Cardiol 2010;105:1030-5 [DOI] [PubMed] [Google Scholar]
- 19.Alba AC, Rao V, Ivanov J, et al. Usefulness of the INTERMACS scale to predict outcomes after mechanical assist device implantation. J Heart Lung Transplant 2009;28:827-33 [DOI] [PubMed] [Google Scholar]
- 20.Aissaoui N, Paluszkiewicz L, Martin Gorria G, et al. Assessment of Right Ventricle before the Implantation of Left Ventricular Assist Device by Echocardiographic Parameters (ARVADE). J Heart Lung Transplant 2013;32:S234-5 [Google Scholar]
- 21.Van Meter CH., Jr Right heart failure: best treated by avoidance. Ann Thorac Surg 2001;71:S220-2 [DOI] [PubMed] [Google Scholar]
- 22.Kaplon RJ, Gillinov AM, Smedira NG, et al. Vitamin K reduces bleeding in left ventricular assist device recipients. J Heart Lung Transplant 1999;18:346-50 [DOI] [PubMed] [Google Scholar]
- 23.Schenk S, McCarthy PM, Blackstone EH, et al. Duration of inotropic support after left ventricular assist device implantation: risk factors and impact on outcome. J Thorac Cardiovasc Surg 2006;131:447-54 [DOI] [PubMed] [Google Scholar]
- 24.Spillner J, Amerini A, Hatam N, et al. Pulmono-atrial shunt and lung assist to treat right ventricular failure. Front Biosci (Landmark Ed)2011;16:2342-51 [DOI] [PubMed] [Google Scholar]
- 25.Argiriou M, Mikroulis D, Sakellaridis T, et al. Acute pressure overload of the right ventricle. Comparison of two models of right-left shunt. Pulmonary artery to left atrium and right atrium to left atrium: experimental study. J Cardiothorac Surg 2011;6:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fitzpatrick JR, 3rd, Frederick JR, Hiesinger W, et al. Early planned institution of biventricular mechanical circulatory support results in improved outcomes compared with delayed conversion of a left ventricular assist device to a biventricular assist device. J Thorac Cardiovasc Surg 2009;137:971-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morgan JA, John R, Lee BJ, et al. Is severe right ventricular failure in left ventricular assist device recipients a risk factor for unsuccessful bridging to transplant and post-transplant mortality. Ann Thorac Surg 2004;77:859-63 [DOI] [PubMed] [Google Scholar]
- 28.INTERMACS Interagency Registry for Mechanically Assisted Circulatory Support quarterly statistical report. Implant dates: June 23, 2006-March 31, 2011.