Abezoar is an indigestible mass of material—such as hair, food, seeds, or another ingested substance—found in the gastrointestinal tract.1 A phytobezoar, the most common type of bezoar, is composed of indigestible fruit and vegetable fibers, such as cellulose, hemicellulose, lignin, or tannins. Most phytobezoars occur in patients who have impaired gastric motility or digestion, usually following gastric surgery (such as a Billroth I or II gastrectomy) or as a consequence of impaired motility in patients with diabetic gastroparesis, mixed connective tissue disease, or hypothyroidism.2,3 Impaired gastric peristalsis, low gastric acidity, and loss of normal pyloric function can all contribute to phytobezoar formation.4 Patients with phytobezoars may experience epigastric pain or discomfort, nausea, vomiting, early satiety, weight loss, diarrhea, dysphagia, or upper gastrointestinal ulcerations and hemorrhage.1,2
Prior to the 1960s, phytobezoars were often treated with surgery; however, a wide variety of therapeutic options have since been reported, including medical treatment with cellulase, papain, metoclopramide, or N-acetylcysteine.1,2,4-6 Surgical intervention is still sometimes necessary, and endoscopic removal has also been used.7-9 Recently, the carbonated beverage Coca-Cola (The Coca-Cola Company) has been successfully used to dissolve bezoars.3 We report 3 patients with gastric phytobezoars who were successfully treated with a combination of Diet Coke (The Coca-Cola Company) and cellulase.
Case series
Over the course of several months, 3 patients presented to our institution with endoscopically documented phytobezoars. These patients included 2 men and 1 woman, and all of the patients had 1 or more factors that predisposed them to bezoar formation. Patient #1 was a 68-year-old man with diabetic gastroparesis who had undergone an esophagectomy with gastric pull-up for treatment of esophageal cancer. He presented with postprandial bloating, nausea, and vomiting of several months’ duration. Patient #2 was a 76-year-old diabetic man who presented with postprandial dysphagia and belching. Patient #3 was an 83-year-old woman who had undergone a Billroth I gastrectomy 45 years earlier for treatment of peptic ulcer disease. Tis patient presented with a 2-month history of intermittent postprandial nausea and vomiting, as well as decreased appetite and weight loss. All of these patients were referred for treatment of the symptoms described above and were diagnosed with a phytobezoar during an esophagogastroduodenoscopy. At the time of diagnosis, no attempt was made to remove or mechanically disrupt the bezoar.
After diagnosis of the phytobezoar, each patient was instructed to drink one 12-oz can of Diet Coke twice daily. Additionally, each patient started treatment with cellulase. As cellulase is not readily available by prescription in US pharmacies, the patients were told to visit a local health food store to find the enzymatic supplement that contained the largest amount of cellulase. Cellulase is only available in combination with other enzymes, and the amount of cellulase in each tablet varies depending on the manufacturer. The patients were told to take 1 cellulase tablet twice daily in addition to the Diet Coke. Patient #1 also received 5 injections (of 20 units each) of onabotulinumtoxin A (Botox, Allergan) to the pylorus for treatment of gastroparesis. All of the patients were treated until resolution of the phytobezoar could be documented via endoscopy (Figure 1); therefore, the treatment time varied among the patients. The interval of time from the initiation of treatment to endoscopic confirmation of bezoar resolution was 8 weeks for Patient #1, 6 weeks for Patient #2, and 8 weeks for Patient #3 (Table 1).
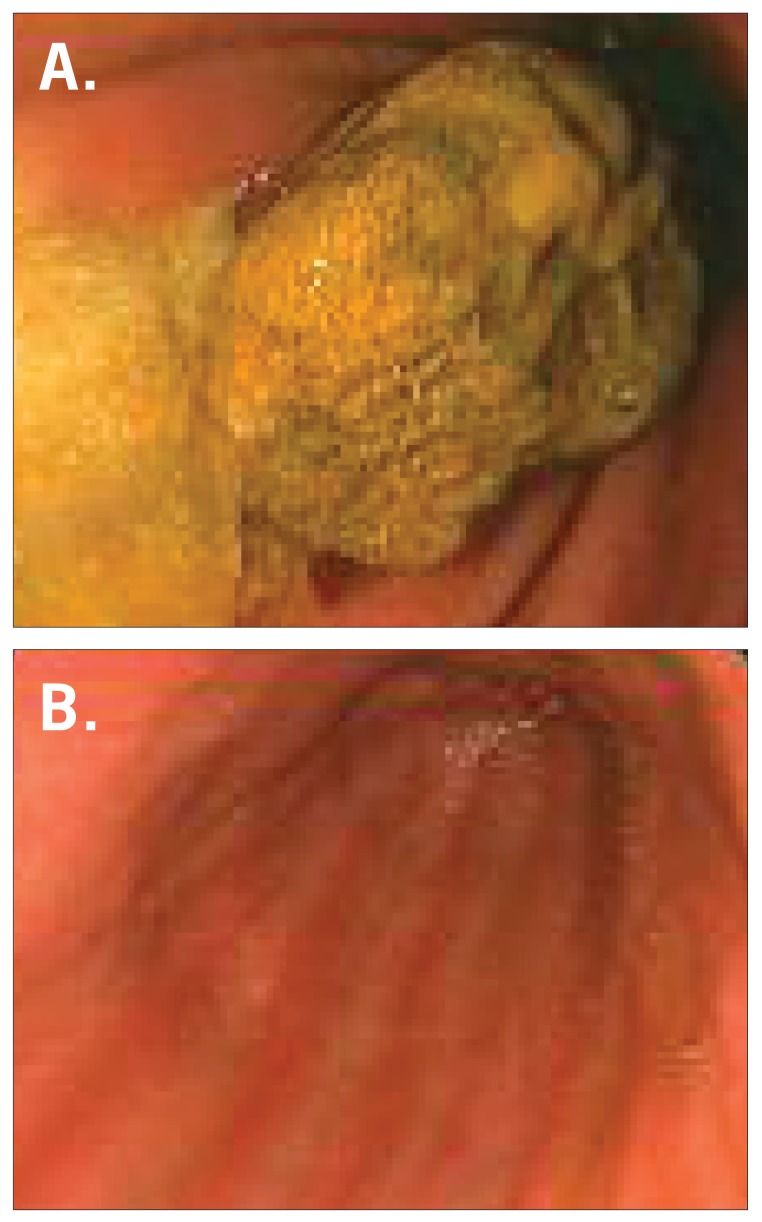
Figure 1.
An endoscopic view of the gastric phytobezoar in Patient #3 before treatment (A). After treatment, there was complete resolution of the phytobezoar (B).
Table 1.
Summary of Patient Characteristics
| Age (years) | Gender | Risk factors | Presenting symptoms | Length of treatment (weeks) | |
|---|---|---|---|---|---|
| Patient #1* | 68 | Male | Diabetic gastroparesis and prior esophagectomy with gastric pull-up | Postprandial bloating, nausea, and vomiting | 8 |
| Patient #2 | 76 | Male | Diabetes mellitus | Postprandial dysphagia and belching | 6 |
| Patient #3 | 83 | Female | Billroth I gastrectomy | Postprandial nausea and vomiting, decreased appetite, and weight loss | 8 |
* The patient also received onabotulinumtoxin A (Botox, Allergan) injections to the pylorus for treatment of diabetic gastroparesis.
Since anecdotal reports had previously suggested the possible efficacy of Coca-Cola and cellulase for treatment of bezoars and there is no known significant toxicity for either of these agents, institutional review board approval was deemed to be unnecessary.
Discussion
In the past, phytobezoars have been medically treated using cellulase (an enzyme that digests cellulose) or papain (a proteolytic enzyme currently found in Adolph’s Meat Tenderizer [Lawry’s]).4-6 Other medical agents that have been used include metoclopramide, N-acetylcysteine, and combination therapy consisting of cellulase, cysteine, and metoclopramide.1,2,10 Surgical removal of phytobezoars may be necessary, and laparoscopic surgery has recently been used for gastric bezoar removal.7,11 Endoscopic options that have been attempted include endoscopic suction and mechanical fragmentation of the bezoar using a pulsating jet of water with subsequent extraction.8,9 Coca-Cola has recently been used to dissolve phytobezoars with administration via nasogastric lavage, intrabezoar injection during endoscopy, ingestion, or a combination of these approaches.3,12-16
This case series documents the successful treatment of phytobezoars in 3 patients using ingestion of Diet Coke and cellulase for 1–2 months. Tis case series is the first to report the combined use of cellulase and Diet Coke for phytobezoar dissolution. The simple ingestion of Diet Coke eliminated the need for nasogastric tube placement or complicated endoscopic procedures in these patients.
As cellulose is a major component of phytobezoars, it is logical that the enzyme cellulase could help to dissolve the concretions. The specific mechanism of action of cellulase is thought to consist of an attack on the leucoanthocyanidin-hemicellulose-cellulose bonds of the bezoar, resulting in the bezoar’s dissolution.1 As a pure form of cellulase is not available by prescription in the United States, the patients in this case series were told to obtain an oral enzymatic supplement that contained the largest amount of cellulase that they could find. The first 2 patients used Enzymedica Digest Gold (Enzymedica), which contains 3,000 units of cellulase per capsule. Tis preparation also contains glucoamylase, alpha-galactosidase, phytase/ pectinase, xylanase, hemicellulase, and beta-glucanase. As phytobezoars may be composed of fruit and vegetable materials other than cellulose, it is reasonable to speculate that the other enzymes (eg, hemicellulase) in these capsules may have contributed to the dissolution of the bezoars. Unfortunately, we were unable to identify the exact brand of the cellulase supplement used by the third patient.
The mechanism of action of Coca-Cola for the dissolution of phytobezoars is less certain. It is believed that the sodium bicarbonate found in Coca-Cola has a mucolytic effect, and the penetration of carbon dioxide bubbles into the bezoar is thought to digest the fibers of the concretion.14 Additionally, Coca-Cola has a pH of 2.6 and contains both phosphoric and carbonic acids. Tis pH is close to that of normal gastric secretions (pH of 1–2). Since acid is important for digesting fiber, it has been suggested that Coca-Cola exerts its effect by acidifying gastric contents.3 Tis mechanism of action is consistent with the fact that low gastric acidity is associated with phytobezoar formation.4 Diet Coke would presumably have the same mechanism of action because it is also made from carbonated water and phosphoric acid. It appears that substituting Diet Coke for Coca-Cola did not adversely affect bezoar dissolution; however, this observation is complicated by the fact that cellulase supplements were also used in this case series. Diet Coke is preferable to nondiet Coca-Cola, as many patients with bezoars have underlying diabetes mellitus and, thus, need to limit intake of dietary sugar. It is unknown to what extent the positive results of this case series could be attributed to the use of Diet Coke, cellulase, or other enzymes in the cellulase supplement. Other case reports have shown similar success rates for the dissolution of bezoars with cellulase ingestion, and Coca-Cola ingestion has been successful for bezoar dissolution in a case report.5,6,14
A limitation of this treatment approach is the lack of readily available, standardized-dose cellulase capsules without other digestive enzymes. To fully elucidate whether any of the other enzymes in the supplement contributed toward bezoar resolution in this case series, it would be necessary to use a pure form of cellulase in a standard dose. Unfortunately, such a preparation is not commercially available at the present time. Another limitation of this case series is that 1 patient was also treated with onabotulinumtoxin A, which is a potential confounding variable.
Additionally, it is important to determine whether both cellulase and Diet Coke need to be used together, as it is possible that equally successful results could occur with only 1 of the 2 agents. In previous case reports, successful phytobezoar dissolution has been reported with cellulase or Coca-Cola ingestion alone in a very small number of patients.
Summary
The findings of this case series support the combined use of cellulase and Diet Coke as a simple, noninvasive, and efective treatment for gastric phytobezoars. Future evaluation is necessary to assess and compare the efficacy of each agent as monotherapy as well as to evaluate the combination therapy in more patients.
Footnotes
The authors have no conflicts of interest to report.
References
- 1.Walker-Renard P. Update on the medicinal management of phytobezoars. Am J Gastroenterol. 1993;88:1663–1666. [PubMed] [Google Scholar]
- 2.Andrus CH, Ponsky JL. Bezoars: classification, pathophysiology, and treatment. Am J Gastroenterol. 1988;83:476–478. [PubMed] [Google Scholar]
- 3.Ladas SD, Triantafyllou K, Tzathas C, Tassios P, Rokkas T, Raptis SA. Gastric phytobezoars may be treated by nasogastric coca-cola lavage. Eur J Gastroenterol Hepatol. 2002;14:801–803. doi: 10.1097/00042737-200207000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Rider JA, Foresti-Lorente RF, Garrido J, et al. Gastric bezoars: treatment and prevention. Am J Gastroenterol. 1984;79:357–359. [PubMed] [Google Scholar]
- 5.Pollard HB, Block GE. Rapid dissolution of phytobezoar by cellulase enzyme. Am J Surg. 1968;116:933–936. doi: 10.1016/0002-9610(68)90470-4. [DOI] [PubMed] [Google Scholar]
- 6.Smith BH, Mollot M, Berk JE. Use of cellulase for phytobezoar dissolution. Am J Gastroenterol. 1980;73:257–259. [PubMed] [Google Scholar]
- 7.Krausz MM, Moriel EZ, Ayalon A, Pode D, Durst AL. Surgical aspects of gastrointestinal persimmon phytobezoar treatment. Am J Surg. 1986;152:526–530. doi: 10.1016/0002-9610(86)90221-7. [DOI] [PubMed] [Google Scholar]
- 8.Madsen R, Skibba RM, Galvan A, Striplin C, Scott P. Gastric bezoars: a technique of endoscopic removal. Am J Dig Dis. 1978;23:717–719. doi: 10.1007/BF01072358. [DOI] [PubMed] [Google Scholar]
- 9.Blam ME, Lichtenstein GR. A new endoscopic technique for the removal of gastric phytobezoars. Gastrointest Endosc. 2000;52:404–408. doi: 10.1067/mge.2000.108407. [DOI] [PubMed] [Google Scholar]
- 10.Gayà J, Barranco L, Llompart A, Reyes J, Obrador A. Persimmon bezoars: a successful combined therapy. Gastrointest Endosc. 2002;55:581–583. doi: 10.1067/mge.2002.122332. [DOI] [PubMed] [Google Scholar]
- 11.Song KY, Choi BJ, Kim SN, Park CH. Laparoscopic removal of gastric bezoar. Surg Laparosc Endosc Percutan Tech. 2007;17:42–44. doi: 10.1097/01.sle.0000213765.86170.77. [DOI] [PubMed] [Google Scholar]
- 12.Kato H, Nakamura M, Orito E, Ueda R, Mizokami M. The first report of successful nasogastric coca-cola lavage treatment for bitter persimmon phytobezoars in Japan. Am J Gastroenterol. 2003;98:1662–1663. doi: 10.1111/j.1572-0241.2003.07563.x. [DOI] [PubMed] [Google Scholar]
- 13.Sechopoulos P, Robotis JF, Rokkas T. Gastric bezoar treated endoscopically with a carbonated beverage: case report. Gastrointest Endosc. 2004;60:662–664. doi: 10.1016/s0016-5107(04)01872-3. [DOI] [PubMed] [Google Scholar]
- 14.Okamoto Y, Yamauchi M, Sugihara K, Kato H, Nagao M. Is coca-cola effective for dissolving phytobezoars? Eur J Gastroenterol Hepatol. 2007;19:611–612. doi: 10.1097/01.meg.0000252638.18915.45. [DOI] [PubMed] [Google Scholar]
- 15.Chung YW, Han DS, Park YK, et al. Huge gastric diospyrobezoars successfully treated by oral intake and endoscopic injection of coca-cola. Dig Liver Dis. 2006;38:515–517. doi: 10.1016/j.dld.2005.10.024. [DOI] [PubMed] [Google Scholar]
- 16.Harikumar R, Kunnel P, Sunilraj R. Dissolution of pharmacobezoar using carbonated beverage. Indian J Gastroenterol. 2008;27:245–246. [PubMed] [Google Scholar]