Abstract
Reducing tobacco use among adolescents in China represents a significant challenge for global tobacco control. Existing behavioral theories developed in the West – such as the Protection Motivation Theory (PMT) – may be useful tools to help tackle this challenge. We examined the relationships between PMT factors and self-reported cigarette smoking behavior and intention among a random sample of vocational high school students (N = 553) in Wuhan, China. Tobacco-related perceptions were assessed using the PMT Scale for Adolescent Smoking. Among the total sample, 45% had initiated cigarette smoking, and 25% smoked in the past month. Among those who never smoked, 15% indicated being likely or very likely to smoke in a year. Multiple regression modeling analysis indicated the significance of the seven PMT constructs, the four PMT perceptions and the two PMT pathways in predicting intention to smoke and actual smoking behavior. Overall, perceived rewards of smoking, especially intrinsic rewards, were consistently positively related to smoking intentions and behavior, and self-efficacy to avoid smoking was negatively related to smoking. The current study suggests the utility of PMT for further research examining adolescent smoking. PMT-based smoking prevention and clinical smoking cessation intervention programs should focus more on adolescents’ perceived rewards from smoking and perceived efficacy of not smoking to reduce their intention to and actual use of tobacco.
Keywords: Protection Motivation Theory, Adolescents, Cigarette smoking, China
1. Introduction
Tobacco control in developing countries presents a pressing global public health challenge (Giovino et al, 2012; World Health Organization [WHO], 2011). More than 80% of smokers are in developing countries. Smokers in China alone account for a third of the world total (Giovino et al, 2012). Despite the high rates of smoking in China and other developing countries, few evidence-based tobacco prevention and intervention studies have been conducted (Shek & Yu, 2011). Moreover, most studies that have been conducted are not guided by an established behavioral theory (see Guo et al., 2007 for a notable exception). Most behavioral theories are developed in the West. Promoting the application of Western-developed behavioral theories in China and other developing countries may advance the understanding of tobacco use for more effective tobacco control across the globe.
1.1 Theory-Based Behavioral Research
Contemporary medical and health behavior research has become increasingly grounded in and guided by theory (Glanz, Rimer, & Viswanath, 2008; National Research Council, 2001; Otten, Bricker, Liu, Comstock, & Peterson, 2011). A large number of theories and models have been developed and used to guide behavioral research including the Information-Motivation-Behavioral Theory (Fisher & Fisher, 1992; Fisher, Fisher, Misovich, Kimble, & Malloy, 1996), the Theory of Reasoned Action and Planned Behavior (Ajzen, 1985; Ajzen & Fishbein, 1980; Fishbein & Ajzen, 1975), the Transtheoretical Model of Change (Prochaska & Velicer, 1997), Social Cognitive (Learning) Theory (Bandura, 1989), and Protection Motivation Theory (Boer & Seydel, 1996; Rogers, 1975). With the guidance of a theory or a conceptual framework, a researcher can better investigate and understand smoking behaviors, supporting more effective tobacco use prevention and smoking cessation. In addition, data derived from a theory-guided study will help theorists to refine the proposed theory. To date, little research on smoking in China has been conducted and only a small subset is theory-based.
1.1.1 Protection Motivation Theory and Health Behavior
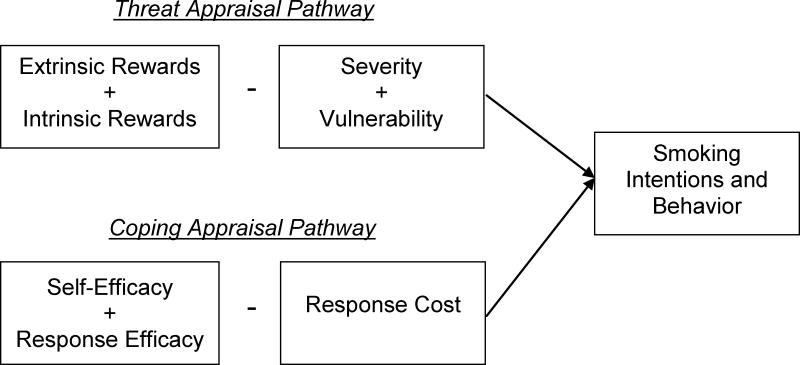
Among the various theories that are frequently used to guide behavior research, the Protection Motivation Theory (PMT) may be particularly well-suited for understanding and addressing smoking behavior (Floyd, Prentice-Dunn, & Rogers, 2000; Milne, Sheeran, & Orbell, 2000). First elucidated by Rogers (1975), PMT in its current format posits two closely related pathways, Threat Appraisal and Coping Appraisal, which link environmental influences to a behavior through a series of cognitive processes (Figure 1).
Figure 1.
Schematic representation of the Protection Motivation Theory (PMT) components.
The balance between the two appraisal pathways determines the likelihood for a risk behavior, such as smoking, to occur (Boer & Seydel, 1996; Rogers, 1975). The threat appraisal pathway involves comparing perceived rewards (intrinsic and extrinsic) of a maladaptive health-related behavior (e.g., smoking) with perceived threats (severity and vulnerability) that the behavior poses. For example, adolescents might weigh feelings of relaxation and better concentration (potential perceived intrinsic rewards of smoking) and beliefs that happier and more popular smoke (potential perceived extrinsic rewards of smoking), against their knowledge that smoking causes cancer and other diseases (potential severity of smoking-related risk) and concerns that smoking may lead to an earlier death (potential vulnerability to smoking-related risk). The coping appraisal pathway involves comparing coping efficacy (self-efficacy and response efficacy) of an adaptive variant of the health-related behavior (e.g., avoiding smoking) with perceived response costs of such adaptive behavior. For example, adolescents might consider the health benefits that nonsmokers may enjoy (perceived response efficacy of not smoking) and how well they think they could decline a cigarette offered by friend (self-efficacy for not smoking), as compared with their concerns about social isolation if they do not smoke (perceived cost of not smoking).
Application of PMT to research has advanced our understanding of a number of health behaviors, including alcohol consumption (Gibbons, Houlihan, Gerrard, 2010), substance use and abuse (Feigelman, Li, & Stanton, 1995; Stanton & Galbraith, 1994), and sexual risk behavior for HIV infection (Chen et al., 2009; Chen et al., 2010; Gong et al., 2009). As described in the next section, PMT has been used as a framework for tobacco research in the United States. We propose to extend the application of PMT to smoking behavior in China. The approach commonly seen in the reported studies to examine the utility of a PMT model is either to treat it as a whole or to focus on certain significant constructs (e.g., self-efficacy, response cost) (Chen et al., 2009). In this study, we will investigate PMT constructs hierarchically. Our intention is to provide data on the role of individual PMT constructs, perceptions, and appraisal pathways as an integrative system in predicting smoking behavior.
1.1.2 PMT and Adolescent Tobacco Use Research
As an integrative conceptual framework, PMT has also been used in tobacco research among adolescents in the United States and other developed countries (Costa, Jessor, & Turbin, 2007; Greening, 1997; Ho, 1998). For example, guided by PMT, one early epidemiological study demonstrated the significance of cognition and appraisal in predicting adolescents’ smoking behavior (Greening, 1997). In this sample of 690 American high school students, a logistic regression controlling for age and gender revealed that smokers were more likely to acknowledge the vulnerability to smoking-related diseases, perceived less severity of smoking risks, viewed male smokers as popular (an indicator of extrinsic rewards of smoking, an effect stronger for boys than for girls), and perceived lower response efficacy for not smoking than did nonsmokers.
Anti-tobacco intervention programs based on PMT have also shown significant effects in discouraging tobacco use among adolescents in developed countries (Pechman, Zhao, Goldberg, & Reibling, 2003; Smith & Stutts, 2003). For example, perceived social disapproval increased adolescents’ intentions to abstain from smoking (Pechman et al., 2003). The successful application of PMT in tobacco research in developed countries suggests the potential utility of the theory to guide tobacco research in developing countries such as China. However, few such studies can be found in the published literature in China.
1.2 Need for Theory-Based Tobacco Research in China
As part of the global tobacco control effort, reducing tobacco use in China represents a critical challenge. China is the world’s largest tobacco producer and consumer, and is home to approximately one-third of the world’s smokers (Han, Chen, & Stanton, 2013; WHO, 2011). Despite much progress in tobacco control in China, data from diverse sources indicate little decline in the prevalence of tobacco use, particularly tobacco use among adolescents (Chen, Stanton, et al., 2006; Cheng, 2008; Han et al, 2013; Zhang, Ou, & Bai, 2011). Every day, approximately 80,000–90,000 Chinese adolescents 12–17 years of age become new smokers and 11–12 million adolescents smoked in the past month (Grenard et al., 2006; Han et al., 2013; Weiss, Palmer, Chou, Mouttapa, & Johnson, 2008). Thus, it is a significant and timely challenge for tobacco researchers in China and across the globe to curb the high rates of tobacco use among young Chinese.
There have been notable tobacco control efforts in China, but very few studies or intervention programs have been grounded in specific theory. This lack of theory-based research could be one potential explanation for the persistently high levels of tobacco use among young Chinese after several decades of tobacco control efforts. A search of the published literature in Chinese and English revealed that few studies on tobacco use in Chinese adolescents were theory-guided, and all were conducted by the same research team (e.g., Guo et al., 2007; Guo, Unger, Azen, MacKinnon, & Johnson, 2012; Guo, Unger, Palmer, Chou, & Johnson, 2013). In addition, theories were mentioned in only three reported smoking prevention intervention trials conducted in China (Chen, Fang, Li, Stanton, & Lin, 2006; Chou et al., 2006; Wen et al., 2010). Furthermore, even in these intervention trials, no detailed information was provided about integrating the theories into the intervention programs, and no evaluation data (e.g., mediation effect analysis) were reported to support the role that the theory played in supporting the observed intervention effect.
1.3 Purposes and Hypotheses of this Study
In the present study, we were guided by the PMT to predict tobacco use intention and behavior among adolescents in China. The purpose of this study is to demonstrate the utility of PMT, a Western-based and empirically tested behavioral theory, to advance our understanding of tobacco use behavior among Chinese adolescents. In addition, findings of this study will provide data supporting tobacco use prevention in China, with potential to extend to other developing countries, further facilitating global tobacco control efforts. As suggested by PMT principles, we hypothesized that smoking would be negatively associated with perceived threat (i.e., severity and vulnerability) of smoking effects and perceived efficacy (i.e., self-efficacy and response efficacy) of not smoking. Further, we hypothesized that smoking would be positively associated with perceived rewards (i.e., intrinsic and extrinsic rewards) of smoking and perceived costs of not smoking.
2. Method
2.1 Participants
Participants were vocational high school students recruited in Wuhan, China. Vocational high school education in China is a three-year, employment oriented, and technical skills training program. Chinese vocational high schools enroll students who either elect not to advance to academic high schools or fail the entrance exam necessary to advance to these high schools after completing the Nine-Year Compulsory Education program. Students in grades 1 and 2 were included, but students in grade 3 were excluded because of the time commitment to preparations for graduation and employment. We elected to target vocational high schools rather than academic high schools because of the higher prevalence of health risk behaviors (e.g., 26–30% smoked cigarettes in the past month) among students in these schools (compared with 8% of academic high school students who reported smoking in the past month) (Johnson et al., 2006; Corcoran & Allegrante, 1989).
The study was conducted in 2011 in Wuhan, China. Wuhan is the provincial Capital of Hubei Province located in central China with a total population of more than nine million and an average level of economic development for China (National Bureau of Statistics China, 2011). Students were randomly selected by class to participate in the study. We first compiled a list of typical vocational high schools in Wuhan with regard to several key factors, including school size, diversity of training programs offered, and time to reach to the school within one hour. After contacting the listed schools, we selected one for which the school administration agreed to participate. Among the total 35 separate eligible classes in the school, 17 were randomly selected using the random digit method. Students in the selected classes who were present on the day when the survey was administered were invited to participate, and those who provided parental consent and participant assent were administered the survey. Among the total 556 students invited to participate, three refused, yielding a final sample of 553 (99.46%).
Participants were 278 girls (50% of the sample) and 275 boys aged 15–18 years old (M = 16.28, SD = 0.98). Just over half (n = 300, 54%) of the sample were grade 1 students. School performance was self-reported as 1, among the lowest 10% (n = 17), 2, below average (n = 84), 3, about average (n = 275), 4, above average (n =120), and 5, among the top 10% (n = 54). Most students’ mothers (n = 372) and fathers (n = 422) attained at least middle school/technical secondary school education level. The most common family income reported was in the 1000–1999 RMB per month (approximately USD $161–322, based on conversion from https://www.google.com/finance/converter on March 12, 2013). There were no significant gender differences in age, grade, parents’ education level, or family income.
2.2 Data Collection Procedure
Trained data collectors from Wuhan Centers for Disease Prevention and Control completed data collection. Data collectors were required to have at least a college degree and three or more years of related experience, or have a graduate degree in a medical or health-related field. Data collection was conducted in classroom settings using the “Chinese Student Health Behavior Questionnaire.” Data collectors distributed the questionnaire to individual students in the classroom; participating students completed the survey by themselves with instruction and supervision only by the trained data collector. This questionnaire was developed and used in previous research with adolescent students in China (Chen, Tang, Li, Stanton, & Li, 2008). Participants completed the questionnaire in approximately 25 to 35 minutes. Approval of the study protocol was obtained from the Human Investigation Committee at Wayne State University, the United States, and the Institutional Review Board at Wuhan Center for Diseases Prevention and Control, China.
2.3 Materials
2.3.1 PMT Scores
PMT constructs were assessed using the PMT Scale for Adolescent Smoking (MacDonell et al., 2013). The PMT Scale consists of 21 items using a 7-point Likert-type response scale anchored by 1, definitely disagree, and 7, definitely agree. Items were specifically devised to assess smoking related perceptions. The PMT items (in English) are shown in the Appendix.
The PMT Scale for Adolescent Smoking has seven construct subscales: vulnerability to smoking-related health problems (calculated α = .48), severity of smoking-related health problems (α = .76), extrinsic rewards of smoking (α = .61), intrinsic rewards of smoking (α = .80), response efficacy of not smoking (α = .68), self-efficacy of not smoking (α = .72), and response cost of not smoking (α = .59). Each construct subscale includes three items, and we computed the mean as the subscale score.
From the scores of the seven PMT constructs, four PMT Perceptions scores were created: perceived threat from smoking (score computed as the mean of vulnerability and severity items, α = .74), perceived rewards of smoking (score computed as the mean of extrinsic rewards and intrinsic rewards items, α = .80), perceived efficacy of not smoking (score computed as the mean of response efficacy and self-efficacy items, α = .74), perceived cost of not smoking (score being equal to that of the response cost construct score with the same α coefficient). From the scores of the four PMT Perceptions described above, two PMT Pathway scores were computed. The threat appraisal pathway was computed as the difference between perceived rewards and perceived threat (i.e., threat appraisal score = perceived rewards score – perceived threat score), and coping appraisal pathway was computed as the difference between the perceived efficacy and perceived cost (i.e., coping appraisal score = perceived efficacy score – perceived cost score). Reliability of the pathway scores and the overall scale was assessed after the items for perceived threat and perceived efficacy were reversed so that all items would correlate positively. Cronbach’s α = .75, .71 and .81 for the threat appraisal pathway, the coping appraisal pathway, and the overall PMT scale respectively.
2.3.2 Smoking Behavior
Three measures were used to assess smoking behavior. Smoking intention was assessed using the question, “How likely is it that you will smoke in a year?” with response options ranging from 1, very unlikely, to 4, very likely. Smoking in the past 30 days was determined in a 2-step process. First, students were asked if they had ever smoked in their lifetime. Second, among those who reported having ever smoked, smoking in the past month was assessed using the question: “Please think about the past 30 days (one month), including today, have you smoked any cigarettes during this period?” Response options were 1, never, 2, occasionally, 3, weekly but not every day, and 4, every day or almost every day. Participants who had never smoked in their lives were coded as never smoking in the past month. The number of cigarettes smoked per day was asked to those who smoked in the past 30 days with the question, “During the past 30 days, on the days you smoked, how many cigarettes on average did you smoke per day?” For analyses, responses were coded as 1, 1 cigarette, 2, 2–5 cigarettes, and 3, more than 5 cigarettes. This categorization of the number of cigarettes was determined with reference to the Youth Risk Behavior Survey (Eaton et al., 2006).
2.4 Data Processing and Statistical Analysis
Survey data were manually entered into computer using the 100% double-entry protocol. The associations between PMT constructs and dependent variables (i.e., smoking intention and actual smoking behavior measures) were first assessed using Pearson correlations, and then with multiple linear regression to account for age and gender . Three sets of regression models were constructed and used in the analysis: (1) Model 1 included the seven PMT constructs simultaneously; (2) Model 2 contained the four PMT perceptions at the same time; and (3) Model 3 involved the two PMT pathways simultaneously. Age and gender were included as covariates because of significant differences in cigarette smoking by gender and age among adolescents in China (Chen, Fang, et al, 2006; Wen et al., 2010). In these modeling analyses, the standardized regression coefficients were reported with type-I error set at p < 0.05 level (two-sided). Data processing and statistical analyses were conducted on a personal computer using SAS version 9.2 (SAS Institute, Cary, NC).1
3. Results
3.1 Preliminary Analyses
Just under half (45%, n = 251) of students indicated that they had ever smoked.2 In the past month, 74% (n = 393) of students indicated not smoking, 12% (n = 63) reported smoking occasionally, 7% (n = 39) indicated weekly smoking, and 6% (n = 33) reported daily/near daily smoking. Of the approximately one-quarter of students who smoked in the past month, 35% (n = 46) smoked one cigarette, 52% (n = 69) smoked 2–5 cigarettes, and 14% (n = 18) smoked more than five cigarettes per day that they smoked. Further, 17% of students (n = 94) believed it likely and 5% (n = 25) believed it very likely that they would be smoking in one year.
3.2 Correlation Analyses
3.2.1 Demographic Relationships
Table 1 includes descriptive statistics and correlations among study variables. Boys were significantly more likely than girls to intend to smoke in one year and to have smoked in the past month; among past-month smokers, boys also smoked more cigarettes per day than girls. Girls indicated higher vulnerability and severity of smoking-related health issues, lower rewards for smoking, higher efficacy for not smoking, and lower costs of not smoking than boys. Neither age nor school performance was significantly associated with any of the smoking measures nor with the PMT constructs, with the exception of the significant association between younger age and higher response efficacy.
Table 1.
Descriptive Statistics of and Correlations among Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | -- | ||||||||||||
| 2. Age | −.07 | -- | |||||||||||
| 3. School performance | .02 | .21*** | -- | ||||||||||
| 4. Smoking intention | −.31*** | −.06 | −.08 | -- | |||||||||
| 5. Frequency smoked in past month | −.43*** | .02 | −.11* | .57*** | -- | ||||||||
| 6. Number cigarettes per day | −.23** | .02 | −.08 | .25** | .61*** | -- | |||||||
| 7. Vulnerability | .08* | −.03 | .01 | −.16*** | −.10* | −.02 | -- | ||||||
| 8. Severity | .14*** | .04 | −.01 | −.23*** | −.20*** | −.06 | .52*** | -- | |||||
| 9. Extrinsic rewards | −.26*** | .01 | −.03 | .24*** | .36*** | .13 | −.05 | −.11** | -- | ||||
| 10. Intrinsic rewards | −.22*** | .01 | −.07 | .31*** | .37*** | .29*** | −.08* | −.22*** | .61*** | -- | |||
| 11. Response efficacy | .12** | −.09* | .01 | −.07 | −.14** | .02 | .24*** | .28*** | −.15*** | −.11* | -- | ||
| 12. Self-efficacy | .17*** | −.01 | .08 | −.19*** | −.29*** | −.10 | .18*** | .29*** | −.17*** | −.23*** | .41*** | -- | |
| 13. Response cost | −.28*** | .06 | −.01 | .24*** | .25*** | .15 | −.12** | −.23*** | .42*** | .44*** | −.12** | −.27*** | -- |
|
| |||||||||||||
| N | 553 | 553 | 550 | 538 | 528 | 133 | 551 | 551 | 551 | 550 | 550 | 550 | 550 |
| M | 1.50 | 16.28 | 3.20 | 1.61 | 1.45 | 1.79 | 4.76 | 5.88 | 2.71 | 2.36 | 5.14 | 5.94 | 2.58 |
| SD | .50 | .98 | .92 | .93 | .88 | .66 | 1.37 | 1.36 | 1.42 | 1.44 | 1.70 | 1.40 | 1.41 |
Notes. Gender was coded as 1 = boys, 2 = girls. Number of cigarettes smoked per day was restricted to students who had smoked in the past month (n = 133).
p < .05.
p < .01.
p < .001.
3.2.1 Relationships of Smoking Measures with PMT Variables
Stronger smoking intentions were significantly associated with more frequent past-month smoking, smoking more cigarettes per day, lower vulnerability and severity, higher extrinsic and intrinsic rewards, lower self-efficacy, and higher response cost. Past month smoking frequency was associated with PMT constructs in the same manner, and frequency was also significantly associated with lower response efficacy of not smoking. Number of cigarettes smoked only included those who indicated smoking in the past month (n = 133); more cigarettes smoked was significantly associated with stronger intrinsic rewards for smoking.
PMT constructs were moderately intercorrelated. Most of the strongest relationships were among pairs of variables forming perception scores (i.e., r = 0.52 for vulnerability and severity, r = 0.61 for extrinsic and intrinsic rewards, and r = 0.41 for self-efficacy and response efficacy).
3.3 Multiple Regression Models
Table 2 contains the standardized estimates for multiple regression models predicting smoking intentions and behaviors from PMT variables. Gender and age were included as control variables in all models.
Table 2.
Regression Models of Smoking Variables Regressed on PMT Variables
| Smoking Intentions | Frequency Smoked in Past Month | Number of Cigarettes Per Day | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PMT Constructs | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 |
| Threat Appraisal | .27*** | .25*** | .15 | ||||||
| Perceived Threat | −.15*** | −.04 | .01 | ||||||
| Vulnerability | −.08 | .01 | −.00 | ||||||
| Severity | −.10* | −.05 | .08 | ||||||
| Perceived Rewards | .20*** | .30** | .21* | ||||||
| Extrinsic Rewards | .04 | .14** | −.07 | ||||||
| Intrinsic Rewards | .18*** | .18*** | .32** | ||||||
| Coping Appraisal | .05 | −.09* | −.03 | ||||||
| Perceived Efficacy | −.01 | −.12** | −.02 | ||||||
| Response Efficacy | .05 | .02 | −.00 | ||||||
| Self-Efficacy | −.07 | −.17*** | −.06 | ||||||
| Perceived Cost | .05 | −.01 | .03 | ||||||
| Response Cost | .04 | −.03 | .02 | ||||||
|
| |||||||||
| R2 | 0.19 | 0.18 | 0.18 | 0.31 | 0.29 | 0.27 | 0.13 | 0.10 | 0.08 |
Notes. Multiple linear regression was used. Models for number of cigarettes per day were restricted to students who had smoked in the past 30 days (n = 133). Model 1 includes the 7 PMT construct scores. Model 2 includes the 4 PMT perception scores. Model 3 includes the 2 PMT pathway scores. All models controlled for age and gender.
p < .05.
p < .01.
p < .001.
3.3.1 Smoking Intentions
The first set of results in Table 2 shows the standardized estimates of the multiple linear regression models predicting intention to smoke in one year. Model 1, in which all seven PMT constructs were entered, was significant, F(9, 525) = 14.09, p < .001. Stronger intentions were significantly associated with higher intrinsic rewards for smoking and lower perceived severity of health issues from smoking. Model 2, in which the four PMT perceptions were entered, was also significant, F(6, 528) = 19.87, p < .001. The greater the perceived rewards from smoking and the lower the perceived threat that smoking poses, the greater the intention to smoke. Model 3, with smoking intentions regressed onto the two appraisal pathways, was significant, F(4, 530) = 29.64, p < .001. Greater intentions to smoke were significantly associated with higher threat appraisals (more rewards than threats). The estimated R2 indicated that these models accounted for 18–19% of the variance in smoking intentions.
3.3.2 Frequency of Smoking in the Past Month
The second set of models shown in Table 2 provides estimates of the multiple linear regression models predicting past-month smoking. Model 1, in which all seven PMT constructs were entered, was significant, F(9, 515) = 25.46, p < .001. More frequent smoking in the past month was significantly associated with higher perceived intrinsic and extrinsic rewards of smoking and lower self-efficacy for not smoking. Model 2, in which the four PMT perceptions were entered, was also significant, F(6, 518) = 35.85, p < .001. Similar to the construct model (Model 1), more frequent past-month smoking was significantly associated with higher perceived rewards of smoking and lower perceived efficacy for not smoking. Model 3, with smoking intentions regressed onto the two appraisal pathways, was significant, F(4, 520) = 47.68, p < .001. Smoking more often was associated with significantly higher threat appraisals and lower coping appraisals. Model 3 suggests that smoking more frequently is related to believing more strongly that the rewards from smoking outweigh the potential risks. Further, more frequent recent smoking was associated with higher costs of not smoking outweighing perceived efficacy of not smoking. These models accounted for 27–31% of the variance in past-month smoking frequency.
3.3.3 Number of Cigarettes Smoked per Day
The last set of models shown in Table 2 provides estimates of the multiple linear regression models predicting the number of cigarettes smoked per day among past-month smokers. Model 1, in which all seven PMT constructs were entered, was significant, F(9, 122) = 2.11, p < .05. The stronger the intrinsic rewards from smoking, the more cigarettes smoked per day. Model 2, in which the four PMT perceptions were entered, was also significant, F(6, 125) = 2.31, p < .05. The greater the perceived rewards from smoking, the more cigarettes smoked. Model 3, with smoking intentions regressed onto the two appraisal pathways, was significant, F(4, 127) = 2.70, p < .05. Although the model as a whole was significant, neither pathway reached significance. These models accounted for 8–13% of the variance in daily cigarette consumption.
4. Discussion
In this study, we applied the Protection Motivation Theory (PMT) to understand cigarette smoking behavior among youth in a random sample of vocational high school students in Wuhan, China. This study is among only a few that utilized a theory-based approach to understand smoking behavior in youth in China (e.g., Guo et al., 2007, 2012, 2013). PMT constructs were measured using a newly developed instrument, the PMT Scale for Adolescent Smoking (MacDonell et al., 2013). The association of all PMT measures with intention to smoke and actual smoking behavior was assessed. To the best of our knowledge, this is the first research study focusing on the application of PMT, a Western-developed theory, in examining adolescent smoking in China. This study provides new evidence supporting the utility of behavioral theories developed in West to advance tobacco research in China and other developing countries, where 80% of all smokers in the world reside (Giovino et al., 2012; WHO, 2011).
4.1 PMT Significantly Predicted Smoking among Chinese Adolescents
Smoking intention and recent smoking were both related to PMT factors. We used multiple conceptualizations of PMT aspects, including the seven PMT constructs (severity, vulnerability, intrinsic rewards, extrinsic rewards, self-efficacy, response efficacy, and response cost), the four PMT perceptions (threat, rewards, efficacy, and cost), and the two PMT pathways (threat appraisal and coping appraisal). Findings of our study are consistent with those summarized through meta-analysis of a number of related studies conducted in the United States and other developed countries in several decades (Floyd et al., 2000; Gwaltney, Metrik, Kahler, & Shiffman, 2009; Milne et al., 2000). PMT theorists explain that perceiving greater severity of and vulnerability to health risks, and having more self-efficacy and response efficacy for avoiding such health risks, encourage adaptive intentions and/or behaviors. At the same time, perceiving more rewards from the behavior and higher costs associated with avoiding the behavior facilitate maladaptive intentions or behaviors.
4.2 Differences in Significance of Individual PMT Components
Consistent with findings reported by others (Floyd et al., 2000; Ho, 1998; Milne et al., 2000), not all PMT measures had the same strength in predicting behavior. When all the PMT measures were analyzed individually, most PMT components were significantly related to smoking intention and behavior, but the strength of the relationships differed for different PMT constructs. For example, smoking intentions were significantly correlated with all PMT constructs except response efficacy. However, when considered simultaneously along with gender and age, only intrinsic rewards positively predicted intentions and severity negatively predicted intentions. Likewise, all seven PMT constructs were significantly correlated with past month smoking frequency. When considered simultaneously, those who perceived higher intrinsic and extrinsic rewards for smoking and lower self-efficacy for not smoking reported smoking more frequently. This finding implies that differential attention should be directed to the more influential PMT constructs in devising and delivering behavioral intervention program in order to achieve better effects. Specifically, for tobacco use prevention among adolescents in China, more attention should be paid to perceived rewards (including intrinsic and extrinsic rewards) and perceived efficacy (including self-efficacy and response efficacy).
Supporting research findings from other countries (Floyd et al., 2000), perceived rewards from smoking, including the intrinsic bio-psychological responses and extrinsic social reactions were the most significant and consistent predictors for adolescent smoking behavior for youth in China. Even when our power to detect effects was reduced because we only included recent smokers, intrinsic rewards specifically and rewards more generally were positively related to cigarette consumption. Consequently, assisting adolescents in identifying and correcting their misperceptions of the rewards from smoking will need to be a priority task for behavioral interventionists. This may be more challenging than educating adolescents on the potential harms from smoking (Cecil, Evans, & Stanley, 1996; Romer & Jamieson, 2001); however, the payoff may be greater than for simply educating students on the dangers of smoking. Data from the present study indicated that similar to youth in the West, many Chinese youth do feel that “smoking makes people feel comfortable” and “smoking is good for social networking.” These perceptions related to intrinsic and extrinsic rewards of smoking should be specifically addressed in tobacco prevention and intervention programs targeting youth.
Notably, self-efficacy has been recognized as one of the most important components for effective intervention to discourage health risk behaviors and to encourage health protective behaviors (Chen et al., 2010; Floyd et al., 2000; Lwin & Saw, 2007; Wurtele & Maddux, 1987). Published studies outside of China have documented the effect of self-efficacy in predicting smoking behavior (Gwaltney et al., 2009). In our study, we found that perceived efficacy, particularly self-efficacy for avoiding cigarettes, among the strongest predictors of recent smoking behavior for adolescents in China. This suggests the importance of promoting self-efficacy in tobacco prevention and treatment efforts for Chinese adolescents. In the United States, current clinical recommendation for treatment of tobacco use and dependence from the Public Health Service specifically includes strategies to promote self-efficacy in patients (Fiore et al., 2008).
It is worth noting that emphasis on some PMT constructs does not mean that we should ignore other constructs to achieve synergetic effect. Behavioral interventionists have long recognized that it is often easier, and frequently effective, to educate youth regarding the immediate negative health consequences of tobacco use (Flay, Hu, & Richardson, 1998), as well as the long-term health implications (e.g., the dangers of smoking included getting cancer, cardiovascular diseases, or other chronic health problems). However, although it may present a challenge to stress to young adolescents the long-term negative health impacts of smoking (Smith & Stutts, 2003), we cannot ignore the significance of this strategy in tobacco use prevention. Rather, our study implies that modifying perceived rewards and adding promotion of self-efficacy and other key PMT constructs may strengthen prevention intervention programs to achieve sustainable effects, as has been reported in intervention studies to reduce HIV risk behavior (Chen et al., 2010).
4.3 Limitations
There are several limitations to this study. First, data used in this analysis were collected through a cross-sectional design. Although we took several technical measures to enhance the efficacy of the association analysis, such as using recent smoking as the outcome measure (to avoid reverse impact of smoking on perception), longitudinal data are needed to verify the results observed in this study. Second, even though participants of this study were randomly selected, they all came from one school. Although a number of key factors were considered to ensure the representativeness of the study sample, including school size, and the diversity of the training programs, caution should be used if the results of this study are to be generalized to other parts of China. Lastly, the reliability was low for several of the three-item constructs, especially vulnerability. Therefore, the perceived vulnerability to tobacco smoking may not be adequately assessed. Additional research is needed to continue refining the scale.
4.4 Conclusions
Despite the limitations described above, this study was the first to apply PMT as a theoretical framework to predict adolescent smoking in China. In addition, findings of this study provide needed data supporting the development of theory-based behavioral prevention interventions to curb the high rates of adolescent tobacco use in China. Lastly, the success of this study implies that the US-developed PMT may also be used as guide to investigate tobacco use among adolescents in other developing countries as well.
Highlights.
Little theory-guided research previously conducted on Chinese youth smoking
Components of PMT were associated with smoking intention and behavior
Perceived rewards increased smoking intention and behavior
Recent smokers indicated lower self-efficacy to avoid smoking
Acknowledgments
Role of Funding Sources
This study is supported in part by NIH grant #: R01-MH086322 and by the Wuhan Centers for Disease Prevention and Control (CDC). Neither organization played a role in the study design, collection, analysis, or interpretation of data, writing the manuscript, or the decision to submit the manuscript for publication.
We are thankful for the teachers and students for their participating and cooperation in the questionnaire survey. We are also thankful for the data collectors from Wuhan CDC for their assistance in data collection, checking and cleaning.
Appendix
| PMT Scale For Adolescent Smoking |
|---|
Severity
Vulnerability
Extrinsic Rewards
Intrinsic Rewards
Response Efficacy
Self-Efficacy
Response Cost
|
Footnotes
The outcome variables (e.g., the three smoking measures) were continuous, but their distributions were skewed. To ensure valid results, we analyzed the data using both multiple linear regression and multinomial logistic regressions for all the three models. The pattern of results was the same; for effective communication, we report the more straightforward results of the multiple linear regressions.
To verify self-reported smoking in the past month, participants were asked to breathe through the instrument PiCO+™ (Smokerlyzer carbon monoxide monitor, USA) to assess Carbon Monoxide (CO) levels in the exhaled air after completing the survey. This measurement was conducted individually for each student. The half-life of CO in the body is approximately 6–9 hours (Jatlow, Toll, Leary, Krishnan-Sarin, & O’Malley, 1993), so the CO measure has been recommended as a verification measure of self-reported smoking data (Jatlow et al., 1993; Wozniak, Moes, Chadzynski, & Domagala-Lulawick, 2009). Of the total sample, 550 participants (99.5%) provided valid CO data. Providing confirmation of recent smoking behavior, self-reported past-month smoking frequency was significantly correlated with breath CO level, r = .49, p < .001.
Contributors
YY, XC, and GJ initiated the study. AJT, NX, JC, NY, and KKM participated in reshaping the analytical plan and manuscript development by providing feedback. GJ, NY, JC, NY and YY organized the data collection in the field. YY conducted data processing, started the analysis and drafted the first version of the manuscript. AJT furthered the analysis and finalized the manuscript with XC’s guidance. All authors approved the final version of the manuscript.
Conflict of Interest
No authors have conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Yaqiong Yan, Email: samwhcdc@hotmail.com.
Angela J. Jacques-Tiura, Email: atiura@med.wayne.edu.
Xinguang Chen, Email: jimax.chen@ufl.edu.
Nianhua Xie, Email: xienh@163.com.
Jing Chen, Email: cj540@163.com.
Niannian Yang, Email: niannianyang@yahoo.com.cn.
Jie Gong, Email: jiegong322@hotmail.com.
Karen Kolmodin MacDonell, Email: kkolmodin@med.wayne.edu.
References
- Ajzen I. From intentions to actions: A theory of planned behavior. In: Kuhl J, Beckman J, editors. Action-control: From cognition to behavior. New York: Springer Verlag; 1985. pp. 11–39. [Google Scholar]
- Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980. [Google Scholar]
- Bandura A. Social cognitive theory. In: Vasta R, editor. Annals of child development, Vol.6. Six theories of child development. Greenwich, CT: JAI Press; 1989. pp. 1–60. [Google Scholar]
- Boer H, Seydel ER. Protection Motivation Theory. In: Conner M, Norman P, editors. Predicting health behaviour. Buckingham, UK: Open University Press; 1996. pp. 95–120. [Google Scholar]
- Cecil H, Evans RI, Stanley MA. Perceived believability among adolescents of health warning labels on cigarette packs. Journal of Applied Social Psychology. 1996;26:502–519. doi: 10.1111/j.1559-1816.1996.tb02728.x. [DOI] [Google Scholar]
- Chen X, Fang X, Li X, Stanton B, Lin D. Stay away from tobacco: A pilot trial of a school-based adolescent smoking prevention program in Beijing, China. Nicotine & Tobacco Research. 2006;8:227–237. doi: 10.1080/14622200600576479. [DOI] [PubMed] [Google Scholar]
- Chen X, Lunn S, Deveaux L, Li X, Brathwaite N, Cottrell L, Stanton B. A cluster randomized controlled trial of an adolescent HIV prevention program among Bahamian youth: Effect at 12 months post-intervention. AIDS and Behavior. 2009;13:499–508. doi: 10.1007/s10461-008-9511-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Stanton B, Fang X, Li X, Lin D, Zhang J, Yang H. Perceived smoking norms, socioenvironmental factors, personal attitudes and adolescent smoking in China: A mediation analysis with longitudinal data. Journal of Adolescent Health. 2006;38:359–368. doi: 10.1016/j.jadohealth.2005.03.010. [DOI] [PubMed] [Google Scholar]
- Chen X, Stanton B, Gomez P, Lunn S, Deveaux L, Brathwaite N, Harris C. Effects on condom use of an HIV prevention programme 36 months postintervention: A cluster randomized controlled trial among Bahamian youth. International Journal of STD & AIDS. 2010;21:622–630. doi: 10.1258/ijsa.2010.010039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Tang X, Li X, Stanton B, Li H. Core human values and their interactions with pro-tobacco factors on cigarette smoking: The role of factors not explicitly related to a risk behavior. California Journal of Health Promotion. 2008;6:23–39. [Google Scholar]
- Cheng TO. Adolescent smoking in China. International Journal of Cardiology. 2008;126:1–2. doi: 10.1016/j.ijcard.2007.04.168. [DOI] [PubMed] [Google Scholar]
- Chou CP, Li Y, Unger JB, Xia J, Sun P, Guo Q, Johnson CA. A randomized intervention of smoking for adolescents in urban Wuhan, China. Preventive Medicine. 2006;42:280–285. doi: 10.1016/j.ypmed.2006.01.002. [DOI] [PubMed] [Google Scholar]
- Corcoran RD, Allegrante JP. Vocational education students: A difficult-to-reach population at risk for smoking-related cancer. Journal of School Health. 1989;59:195–198. doi: 10.1111/j.1746-1561.1989.tb04701.x. [DOI] [PubMed] [Google Scholar]
- Costa FM, Jessor R, Turbin MS. College student involvement in cigarette smoking: The role of psychosocial and behavioral protection and risk. Nicotine & Tobacco Research. 2007;9:213–224. doi: 10.1080/14622200601078558. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Ross J, Hawkins J, Harris WA, Weschler H. Youth risk behavior surveillance – United States, 2005. Journal of School Health. 2006;76:353–372. doi: 10.1111/j.1746-1561.2006.00127.x. [DOI] [PubMed] [Google Scholar]
- Feigelman S, Li X, Stanton B. Perceived risks and benefits of alcohol, cigarette, and drug use among urban low-income African-American early adolescents. Bulletin of the New York Academy of Medicine. 1995;72:57–75. [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Jaén CR, Baker TB, Bailey WC, Benowitz NL, Wewers ME. Treating tobacco use and dependence: 2008 update. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2008. [Google Scholar]
- Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: An introduction to theory and research. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Misovich SJ, Kimble DL, Malloy TE. Changing AIDS risk behavior: Effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychology. 1996;15:114–123. doi: 10.1037/0278-6133.15.2.114. [DOI] [PubMed] [Google Scholar]
- Flay BR, Hu FB, Richardson J. Psychosocial predictors of different stages of cigarette smoking among high school students. Preventive Medicine. 1998;27(5 Pt B):A9–A18. doi: 10.1006/pmed.1998.0380. [DOI] [PubMed] [Google Scholar]
- Floyd DL, Prentice-Dunn S, Rogers RW. A meta-analysis of research on protection motivation theory. Journal of Applied Social Psychology. 2000;30:407–429. doi: 10.1111/j.1559-1816.2000.tb02323.x. [DOI] [Google Scholar]
- Gibbons FX, Houlihan AL, Gerrard M. Reason and reaction: The utility of a dual-focus, dual-processing perspective on promotion and prevention of adolescent health risk behavior. British Journal of Health Psychology. 2010;14:231–248. doi: 10.1348/135910708X376640. [DOI] [PubMed] [Google Scholar]
- Giovino GA, Mirza SA, Samet JM, Gupta PC, Jarvis MJ, Bhala N GATS Collaborative Group. Tobacco use in 3 billion individuals from 16 countries: An analysis of nationally representative cross-sectional household surveys. Lancet. 2012;18:668–79. doi: 10.1016/S0140-6736(12)61085-X. [DOI] [PubMed] [Google Scholar]
- Glanz K, Rimer BK, Viswananth K, editors. Health behavior and health education: Theory, research and practice. San Francisco, CA: Jossey-Bass; 2008. [Google Scholar]
- Gong J, Stanton B, Lunn S, Deveaux L, Li X, Marshall S, Chen X. Effects through 24 months of an HIV/AIDS prevention intervention program based on protection motivation theory among preadolescents in the Bahamas. Pediatrics. 2009;123:e917–e928. doi: 10.1542/peds.2008-2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greening L. Adolescents’ cognitive appraisals of cigarette smoking: An application of the protection motivation theory. Journal of Applied Social Psychology. 1997;27:1972–1985. doi: 10.1111/j.1559-1816.1997.tb01635.x. [DOI] [Google Scholar]
- Grenard JL, Guo Q, Jasuja GK, Unger JB, Chou CP, Gallaher PE, Johnson CA. Influences affecting adolescent smoking behavior in China. Nicotine & Tobacco Research. 2006;8:245–255. doi: 10.1080/14622200600576610. [DOI] [PubMed] [Google Scholar]
- Guo Q, Johnson CA, Unger JB, Lee L, Xie B, Chou CP, Pentz M. Utility of the theory of reasoned action and theory of planned behavior for predicting Chinese adolescent smoking. Addictive Behaviors. 2007;32:1066–81. doi: 10.1016/j.addbeh.2006.07.015. [DOI] [PubMed] [Google Scholar]
- Guo Q, Unger JB, Azen SP, MacKinnon DP, Johnson CA. Do cognitive attributions for smoking predict subsequent smoking development. Addictive Behaviors. 2012;37:273–279. doi: 10.1016/j.addbeh.2011.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Q, Unger JB, Palmer PH, Chou CP, Johnson CA. The role of cognitive attributions for smoking in subsequent smoking progression and regression among adolescents in China. Addictive Behaviors. 2013;38:1493–1498. doi: 10.1016/j.addbeh.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwaltney CJ, Metrik J, Kahler CW, Shiffman S. Self-efficacy and smoking cessation: A meta-analysis. Psychology of Addictive Behaviors. 2009;23:56–66. doi: 10.1037/a0013529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han J, Chen X, Stanton B. Prevalence of cigarette smoking among adolescents in China 1981–2010: A meta-analysis and review. Plos Medicine. 2013 Manuscript in press. [Google Scholar]
- Ho R. The intention to give up smoking: Disease versus social dimensions. The Journal of Social Psychology. 1998;138:368–380. doi: 10.1080/00224549809600389. [DOI] [PubMed] [Google Scholar]
- Jatlow P, Toll BA, Leary V, Krishnan-Sarin S, O’Malley SS. Comparison of expired carbon monoxide and plasma cotinine as markers of cigarette abstinence. Drug and Alcohol Dependence. 2008;98:203–209. doi: 10.1016/j.drugalcdep.2008.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson CA, Palmer PH, Chou CP, Pang Z, Zhou D, Dong L, Unger JB. Tobacco use among youth and adults in mainland China: The China seven cities study. Public Health. 2006;120:1156–1169. doi: 10.1016/j.puhe.2006.07.023. [DOI] [PubMed] [Google Scholar]
- Lwin MO, Saw SM. Protecting children from myopia: A PMT perspective for improving health marketing communications. Journal of Health Communication. 2007;12:251–268. doi: 10.1080/10810730701266299. [DOI] [PubMed] [Google Scholar]
- MacDonell K, Chen X, Yan Y, Li F, Gong J, Sun H, Stanton B. A protection motivation theory-based scale for tobacco research among Chinese youth. Journal of Addiction Research & Therapy. 2013;4(3):154. doi: 10.4172/2155-6105.1000154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milne S, Sheeran P, Orbell S. Prediction and intervention in health-related behavior: A meta-analytic review of protection motivation theory. Journal of Applied Social Psychology. 2000;30:106–143. doi: 10.1111/j.1559-1816.2000.tb02308.x. [DOI] [Google Scholar]
- National Bureau of Statistics of China. 2010 China Statistical Yearbook. Beijing: China Statistics Press; 2011. [Google Scholar]
- National Research Council. Health and behavior: The interplay of biological, behavioral, and societal influences. Washington, DC: The National Academies Press; 2001. [PubMed] [Google Scholar]
- Otten R, Bricker J, Liu JM, Comstock BA, Peterson AV. Adolescent psychological and social predictors of young adult smoking acquisition and cessation: A 10-year longitudinal study. Health Psychology. 2011;30:163–170. doi: 10.1037/a0022352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pechmann C, Zhao G, Goldberg ME, Reibling ET. What to convey in antismoking advertisements for adolescents: The use of protection motivation theory to identify effective message themes. Journal of Marketing. 2003;67(2):1–18. doi: 10.1509/jmkg.67.2.1.18607. [DOI] [Google Scholar]
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. American Journal of Health Promotion. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- Rogers RW. A protection motivation theory of fear appeals and attitude change. The Journal of Psychology. 1975;91:93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- Romer D, Jamieson P. Do adolescents appreciate the risks of smoking? Evidence from a national survey. Journal of Adolescent Health. 2001;29:12–21. doi: 10.1016/S1054-139X(01)00209-9. [DOI] [PubMed] [Google Scholar]
- Shek DTL, Yu L. A review of validated youth prevention and positive youth development programs in Asia. International Journal of Adolescent Medicine and Health. 2011;23:317–324. doi: 10.1515/IJAMH.2011.028. [DOI] [PubMed] [Google Scholar]
- Smith KH, Stutts MA. Effects of short-term cosmetic versus long-term health fear appeals in anti-smoking advertisements on the smoking behaviour of adolescents. Journal of Consumer Behaviour. 2003;3:157–77. doi: 10.1002/cb.130. [DOI] [Google Scholar]
- Stanton B, Galbraith J. Drug trafficking among African-American early adolescents: Prevalence, consequences, and associated behaviors and beliefs. Pediatrics. 1994;93:1039–1043. [PubMed] [Google Scholar]
- Weiss JW, Palmer PH, Chou CP, Mouttapa M, Johnson CA. Association between psychological factors and adolescent smoking in seven cities in China. International Journal of Behavioral Medicine. 2008;15:149–156. doi: 10.1080/10705500801929825. [DOI] [PubMed] [Google Scholar]
- Wen X, Chen W, Gans KM, Colby SM, Lu C, Liang C, Ling W. Two-year effects of a school-based prevention programme on adolescent cigarette smoking in Guangzhou, China: A cluster randomized trial. International Journal of Epidemiology. 2010;39:860–876. doi: 10.1093/ije/dyq001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. WHO report on the global tobacco epidemic, 2011: Warning about the dangers of tobacco. Geneva, Switzerland: World Health Organization; 2011. http://whqlibdoc.who.int/publications/2011/9789240687813_eng.pdf. [Google Scholar]
- Wozniak K, Moes A, Chadzynski R, Domagala-Kulawik J. Evaluation of the indication of carbon monoxide in exhaled air. Przeglad Lekarski [Evaluation Studies] 2009;66:632–635. [PubMed] [Google Scholar]
- Wurtele SK, Maddux JE. Relative contributions of protection motivation theory components in predicting exercise intentions and behavior. Health Psychology. 1987;6:453–466. doi: 10.1037/0278-6133.6.5.453. [DOI] [PubMed] [Google Scholar]
- Zhang J, Ou JX, Bai CX. Tobacco smoking in China: Prevalence, disease burden, challenges and future strategies. Respirology. 2011;16:1165–72. doi: 10.1111/j.1440-1843.2011.02062.x. [DOI] [PubMed] [Google Scholar]