Abstract
Introduction
To analyze the correlation between the many different emergency department (ED) treatment metric intervals and determine if the metrics directly impacted by the physician correlate to the “door to room” interval in an ED (interval determined by ED bed availability). Our null hypothesis was that the cause of the variation in delay to receiving a room was multifactorial and does not correlate to any one metric interval.
Methods
We collected daily interval averages from the ED information system, Meditech©. Patient flow metrics were collected on a 24-hour basis. We analyzed the relationship between the time intervals that make up an ED visit and the “arrival to room” interval using simple correlation (Pearson Correlation coefficients). Summary statistics of industry standard metrics were also done by dividing the intervals into 2 groups, based on the average ED length of stay (LOS) from the National Hospital Ambulatory Medical Care Survey: 2008 Emergency Department Summary.
Results
Simple correlation analysis showed that the doctor-to-discharge time interval had no correlation to the interval of “door to room (waiting room time)”, correlation coefficient (CC) (CC=0.000, p=0.96). “Room to doctor” had a low correlation to “door to room” CC=0.143, while “decision to admitted patients departing the ED time” had a moderate correlation of 0.29 (p <0.001). “New arrivals” (daily patient census) had a strong correlation to longer “door to room” times, 0.657, p<0.001. The “door to discharge” times had a very strong correlation CC=0.804 (p<0.001), to the extended “door to room” time.
Conclusion
Physician-dependent intervals had minimal correlation to the variation in arrival to room time. The “door to room” interval was a significant component to the variation in “door to discharge” i.e. LOS. The hospital-influenced “admit decision to hospital bed” i.e. hospital inpatient capacity, interval had a correlation to delayed “door to room” time. The other major factor affecting department bed availability was the “total patients per day.” The correlation to the increasing “door to room” time also reflects the effect of availability of ED resources (beds) on the patient evaluation time. The time that it took for a patient to receive a room appeared more dependent on the system resources, for example, beds in the ED, as well as in the hospital, than on the physician.
INTRODUCTION
Emergency departments (ED) nationwide are encountering extended delays in evaluating patients.2–5 The following attempts have been made to improve the ED patient evaluation process: additional ED beds, additional hospital beds, and improved patient through-put and discharges. Hoffenberg et al6 evaluated 291 EDs, and assessed 386,837 patient visits within a 19-month period. A significant improvement with length of stay (LOS) was noted within the slowest EDs. By using “best demonstrated processes,” the slowest EDs decreased their average LOS by only 29 minutes.6 Kyriacou et al conducted a 5-year study using time intervals to analyze the ED patient care efficiency.7 When an ED bed was immediately available, LOS was decreased by 36 minutes.7 The most successful process changes addressed external factors to the ED.8 These factors included increased flexibility of inpatient resources, float nurses who responded to acute care needs in the ED, and a transition team (mid-level provider along with registered nurse) who cared for inpatients boarded in the ED.8 Other factors are an integrated admission service across affiliated hospitals/systems, an early alert system that notified key personnel before “critical bed” criteria were met, and a multi-disciplinary team to round in the ED and analyze resource needs.
With the increasing number of patient visits, decreasing numbers of EDs9 and the diminishing availability of ED care as a resource, efficiency has become an important issue in providing emergency patient care and is driving hospital administration to encourage emergency physicians (EP) to improve ED metrics. The ED is a complex system. Understanding the contributions to the total time a patient spends in the department are keys to improving patient flow. The factors that affect ED flow include department size, the staffing of physicians, nursing, and the numerous ancillary services. EPs are one part of the equation in the evaluation process. They directly affect the evaluation interval by how long it takes the physician to assess the patient once the patient receives a room. Physicians determine the patient evaluation time based on the time to complete their directed evaluation, and discharge the patient. We used typical ED metric variation to try and quantify the effect of each interval of ED patient flow. The goal of the investigation was to analyze the relationship of ED metrics, to the time it took for a patient to receive an available ED treatment room (“door to room” time). We also wanted to evaluate the correlations between physician-controlled factors within the process and ED flow, to provide valuable insights into whether management efforts should focus at the level of the individual physician or larger hospital-based factors.
MATERIALS AND METHODS
Study Design
The design was to analyze the correlation between several different ED treatments intervals by collecting interval data of the average daily time for a 1-year period. With this information we used the intervals directly impacted by the EP and what effects they have on the “door to room” interval (bed availability) in an ED. Our null hypothesis was that the foundation of the delay in a patient being placed in an ED room for treatment correlates to multiple factors, not just any one interval in the process of ED evaluation.
Study Setting and Population
We conducted this study at an urban county hospital facility. The hospital was a designated level 2 trauma center by the American College of Surgeons for a 12-county region, as well as having emergent cardiac catheterization capability. This facility saw 41,000 patients annually, with an admission rate of 18%. Twenty-five percent of those admissions were admitted to the intensive care units. The ED had 2 major resuscitation/trauma rooms, with an additional 15 rooms in the main department and 6 rooms for evaluation of lower acuity patients. The main part of the ED was essentially divided into 2 nursing patient care teams. The room assignments were staffed as the following: 2 registered nurses and a technician to a major resuscitation room and 6 acute care rooms. Physician staffing in the main part of the ED was an attending physician and two emergency medicine residents (of variable levels of training) for a 24-hour period. The radiology department, which was located directly behind the ED, was equipped with a CT, ultrasound, as well as MRI capabilities.
Study Process
The ED had a typical evaluation process. All walk-in patients checked in at the triage window, which was staffed by an ED technician. The patient signed in on a triage complaint form with their name, time of arrival, and chief complaint (time of arrival started the ED intervals). Then a registered nurse evaluated the patient. A vast majority of the patients received an evaluation using the Emergency Severity Index (ESI) index based on the stability of the patient as well as need for evaluation.10 If their complaint had potential severity, and/ or if a room was available, the patient would be immediately assigned to an ED room. If no beds were available, the triage nurse asked the patient to wait in the lobby until a room was available for further evaluation (arrival to room interval). A vast majority of the patients that arrived by ambulance were immediately taken to a room for evaluation (in that situation, time of nurses initial triage started the ED intervals). The EP (or physician extender) then assessed the patient to determine if further evaluation or consultation was necessary. The EP determined if the patient needed to be admitted to the hospital for further treatment, or discharged home with discharge instructions for care at home. If a patient was admitted to the hospital, the time that the order was given was used to determine the beginning of ED “boarding” (admit decision to hospital bed). Boarding occurred only after a physician (a hospitalist or patient physician) had accepted and agreed to treat and follow the patient during their hospital stay.
Method of Measurement
Average daily time interval data was collected from the ED tracking system, Meditech©. This was a dynamic tracking system that required the staff to time mark the following events: when the patient received a room (room), when the physician assessed the patient (doctor), physician order to admit patient to the hospital for further treatment (admit) and when the patient was discharged from the ED (dismiss). The intervals collected included classic ED measures as defined by Welch et al11 (Table 1). We chose the intervals as they represented the separate event points entered in every visit, and represented the distinct steps in the flow of a patient through-put in an ED related to the physicians’ care (Figure 1). The data collected were the average of the interval for each 24-hour day during a year covering the period from November 2008 to November 2009. April 2009 was used as a representative month for Figures 2, 3, and 4, which visually represented the pattern of relationships of ED intervals. April 2009 was chosen because of the very similar correlation coefficients to the results for the entire year.
Table 1.
Emergency department (ED) intervals (determine the variables used for correlation analysis for linear relationships) address independent variable comments(8), as well as why intervals attributed to the physician(6), corresponding Meditech intervals and definitions:
| ED interval | Meditech interval | Definitions |
|---|---|---|
| Door to room | Received to room | Time it takes for the patient to be placed back into a room i.e. bed availability for evaluation, waiting room time |
| Room to doctor (LIP) | Room to provider | Time it takes for a physician to see the patient in the room after the patient is placed in the room, interval directly impacted by physician getting into the room |
| ED length of stay for discharged patients | Received to dismiss | The time interval in minutes between arrival time and discharge time |
| Admit decision to depart ED time | Admit to dirty bed | The time interval in minutes between the decision to admit and the physical departure of the patient from the ED treatment area, ED boarding time |
| Doctor to discharge time | Provider to dismiss | The time interval in minutes between MD contact with the patient and doctor orders discharge time. Time determined by the physician directed evaluation. |
| Total patients per day | New arrivals | Total number of patients that signed up for triage that day. |
Definitions from a consensus group created to address standardization of performance measures in emergency medicine. 11
Figure 1.
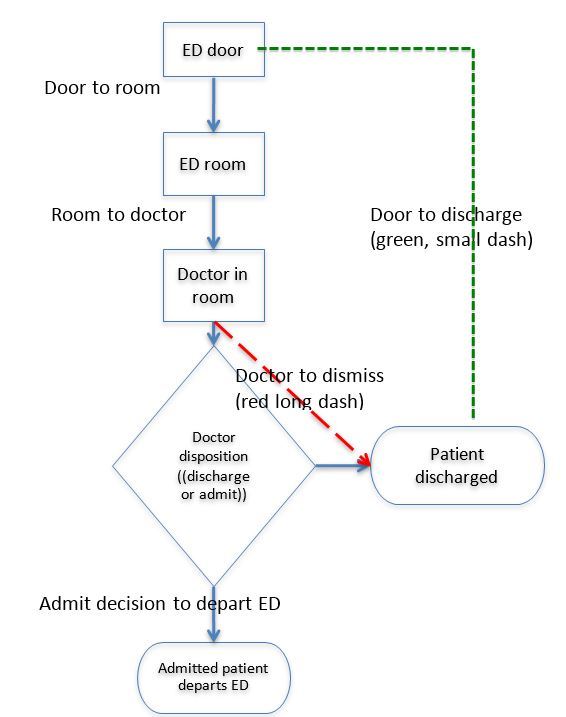
Emergency department (ED) intervals.
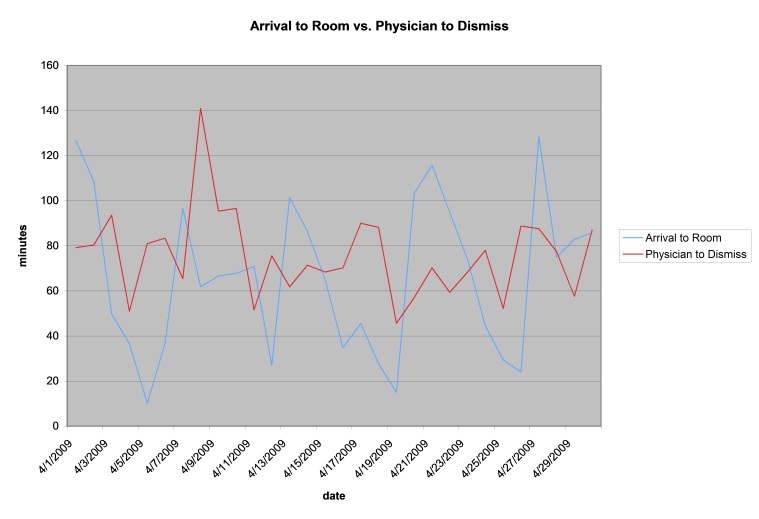
Figure 2.
Door (arrival) to room versus doctor (physician) to discharge time (correlation coefficient 0.00, April correlation coefficient −0.065) reviewer d.
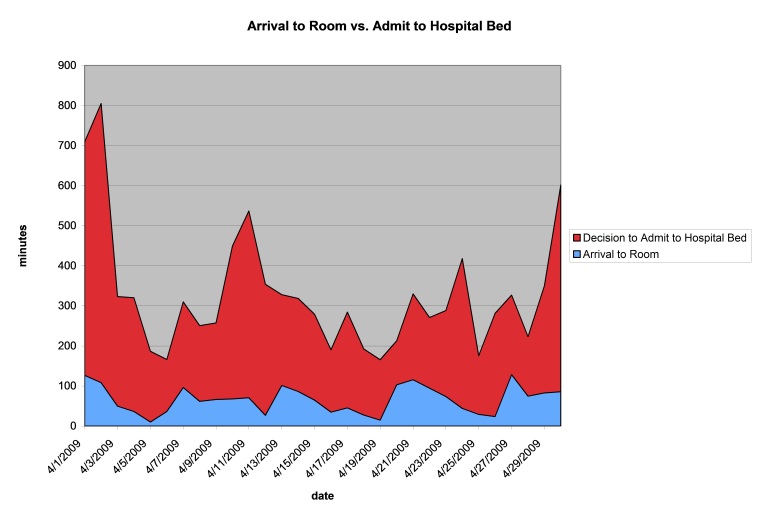
Figure 3.
Door (arrival) to room versus decision to left emergency department time (correlation coefficient 0.29, April correlation coefficient 0.24).
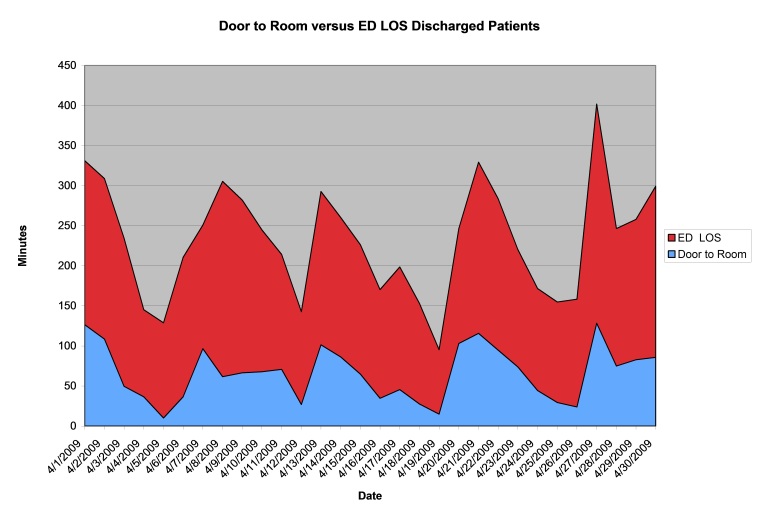
Figure 4.
Door to room versus emergency department (ED) length of stay (LOS) for discharged patients (correlation coefficient 0.804, April correlation coefficient 0.73).
Primary Data Analysis
We divided the intervals based on if the physician had any direct impacts on the majority of the time in the interval. The time it took the physician to get into the room to evaluate the patient was directly controlled by the priority the physician placed on getting into the room to see the patient. The physician determines the duration of the “room to dismiss interval,” based on the complaint dictating the duration of the patient evaluation. We analyzed the relationship of each interval using simple correlation (Pearson Correlation coefficients) to the “arrival to room” interval. We felt that variation in the arrival to room time was the primary determinant of extended evaluation times within the department and wanted to understand what intervals correlated best to extending the time the patients spent in the waiting room. We also divided data by intervals based on the average ED length of stay published by Centers for Disease Control on 2008 Emergency Department Statistics.1 The 2008 average ED LOS was divided into the following two groups – less than average LOS and greater than average LOS. The information was presented to demonstrate the change in interval times based on the extended LOS (Table 2.) We performed statistical analysis using SPSS Version 16, Chicago Illinois. The Institutional Review Board approved this study as exempt.
Table 2.
Study emergency department (ED) intervals divided, based on median length of stay (LOS) of 154 minutes.
| Interval: (median) | LOS ≤ 154 (SD) | LOS > 154 (SD) | Difference |
|---|---|---|---|
| Door to room (minutes) | 38.4 (21) | 88.8 (31.5) | 50.4 (131%) |
| Room to doctor (LIP) (minutes) | 28.2 (8) | 33 (8) | 4.8 (17%) |
| ED LOS for discharged patients (minutes) | 132 (17.5) | 199 (33) | 67.0 (51%) |
| Decision to left ED time (minutes) | 199 (99.7) | 237 (141) | 38.0 (19%) |
| Doctor to discharge time | 69.6 (16) | 82 (17) | 12.4 (18%) |
| Total patients per day | 114 (14) | 131 (16) | 17.0 (15%) |
RESULTS
We divided ED median interval times (Table 2) into 2 groups based on the CDC reports of national median LOS in 2008 (154 minutes),1 to compare “good” days to days with delays in patient progress through the department. When the LOS extended beyond the CDC-reported median, the following intervals were increased: room to doctor 17%, doctor to discharge 18%, ED LOS for discharged patient 51%, and door to room 131% (Table 2). Delays with patients receiving a “room” within the ED had no effect on “room to doctor” intervals” (Table 3). “Door to room” interval correlation coefficients (CC) show a low CC of 0.143 for “room to doctor” interval. The “doctor to discharge” time interval demonstrates no correlation to the variation with the “door to room” (see Figure 2). Variation within the physician-directed components of the evaluation and acuity of the treatment did not have a correlation with the delay in time it took for a patient to receive an ED “room.” “Admit decision time to depart ED time” had a moderate correlation to the “door to room” interval. The “door to room” component of the “door to discharge” interval had a strong correlation (see Figure 4) to delays in a patient receiving a room. Another major factor in department function was the “total patients per day,” with a strong correlation of 0.657 to the variation in the “door to room” time interval.
Table 3.
Summary “Door to Room” interval correlation coefficients to the following intervals
| Interval: | Pearson Correlation | p-value |
|---|---|---|
| Room to doctor (LIP) | 0.143 (low) | p=0.006 |
| Emergency department (ED) length of stay for discharged patients | 0.804 (Very strong) | p<0.001 |
| Decision to left ED time | 0.290 (Medium) | p<0.001 |
| Doctor to discharge time | 0.000 (None) | p=0.996 |
| Total patients per day | 0.657 (Strong) | p<0.001 |
DISCUSSION
Patient evaluation within the ED is part of a very complex system that involves both the ED and additional departments/systems within the hospital. Literature review supports no impact on the LOS interval by improving ED process within 2/3 of hospitals with best practices.6 This institution used several best practice methods that included triage orders. This best practice method alone has been shown to save 37 minutes of time that a patient occupies an ED bed.12,13 We also evaluated lower acuity complaints in a separate area in the department.14 Physicians controlled the evaluation time of the patient, but the actual evaluation was dictated by the complaint complexity and the critical nature of the complaint. The “physician to dismiss” had no correlation to the variation.
“Door to discharge” interval had a very significant correlation of 0.804 (p<0.001) to the variation in the “door to room” interval, which showed the component effects on the “door to room” interval on total LOS for the ED. Dividing the data based on the CDC median LOS from 2008 showed an average of 14.3 more patients per day seen, as the LOS in the ED increased beyond the 154 minutes. “Total patients per day” correlation with the “door to room” interval supported the effect of increasing the number of patients with delays in patients receiving a room. Indirectly, it supported the effect of availability of ED beds within the department and the impact it had on ED LOS. Ding et al noted that higher ED occupancy rates had a much greater effect on increasing “door to room” time or waiting room time.15 Asaro et al showed that an increase from the 20th to the 80th percentile in ED arrivals increased the wait room (“door to room”) time by 42 minutes and the LOS by 49 minutes.16 There was no direct evaluation of the causes for the delay in receiving a room. The lack of room availability was an obvious factor that caused the delay, thus supporting the need for ED space to properly evaluate patients. The Kyriacou et al study showed that when an ED bed was immediately available, LOS was decreased by 36 minutes.7 The time that it took for a patient to get into a room appeared more dependent on the ED system resources than on the physician.
The interval in ED LOS directly impacted by the hospital was the time it took for an admission to be transferred to an inpatient bed for care (boarding time). The Institute of Medicine identified boarding in the ED as one of the major issues in ED flow.17 “Admit decision to depart ED” had a moderate correlation to the variation of the “door to room” interval. This variation demonstrated the effect that inpatient hospital bed availability independently has on ED LOS. McCarthy also identified ED crowding as delaying treatment and LOS.18 Previous evaluation of hospital bed occupancy in the literature showed attempts to optimize inpatient hospital bed utilization, resulting in 85–100% hospital occupancy.19 Bagust et al discussed the subsequent difficulty of transferring patients from the ED to inpatient beds.19 Modeling of the dynamics for such a hospital system supports the occurrence of bed shortages and crisis at these occupancy levels.19 An example includes the Toronto area: area hospitals closed 30%(2,890) of their acute care beds through 1997 resulting in minimum crowding. When 943 beds were closed between 1998 and 2000 and occupancy rates exceeded 90%, with a peak at 96% for acute care beds in the region, ED crowding became a frequent occurrence.20 Vicellio et al has shown that placing admitted patients in inpatient hallways decreases those patients’ LOS within the ED and available ED beds. By doing this, it also removed the additional workload from the ED staff. Thus, showing the effect of non-physician staffing, whether within the hospital or in the department, can have on ED efficiency.21 The moderate correlation of “door to room” to “admit decision to left ED” demonstrates the large effect the inpatient hospital resource availability can have upon the ED patients’ LOS. Rathlev et al showed that for every additional surgical elective admission, it prolonged the ED LOS by 0.21 minutes per ED patient, 2.2 minute for each additional ED admission, and 4.1 minutes for every increase in hospital occupancy.22 Lucas et al concluded very similar correlations with the number of admissions as well as occupancies using 5 facilities varying from 30,000 census up to 99,280 census.23 Continued financial drivers to maintain high occupancies will result in the need for the hospital care system to be more efficient when evaluating patients, transferring patients from the ED to a hospital bed, and discharging patients from the hospital.
Overall, EPs infrequently have direct responsibility for other personnel, staffing, and management. They can advocate, encourage and set the examples to increase patient flow within the ED. However they need the support and recognition of hospital administration to maintain the necessary workforce and available beds to accomplish that goal. Incentivizing the physician outside the “room to doctor” interval, specifically the arrival (“door”) to physician interval, will only lead to individual physician frustration with the entire system given the lack of direct ability to affect patient movement through the system and complicated workforce system issues throughout the hospital. Managing the ED is complex and requires significant partnering between the hospital staff, emergency staff, and the physicians to optimize patient care.
LIMITATIONS
The information was from a single institution and only applies to that institution. Every institution has variable methods of triage, as well as handling ambulances, registrations, and their own focuses on patient evaluation. This makes the actual intervals difficult to compare between institutions, but the evaluation of the entire system remains pertinent to understanding the overall ED process.
Another major consideration in interpreting the information was in the mechanism of tracking the status of the patient. The individual staff had to mark the status of the patients in the system, and we continue to use paper charts as a visual queue of patients waiting to be seen. Both can contribute to variation in the intervals being recorded, but the large sample size should minimize the potential for error.
Third, there was no direct evaluation for the specific causes of daily variation in intervals or in individual patients as they processed through the ED. The study used average daily interval data with correlation, which shows linear relationships. (It does not analyze for specific factors.) We did not analyze specific complaints, and surges, or specific causes of the delays.
We performed statistical analysis using simple correlation of the intervals, to demonstrate a linear relationship between the various intervals. The outside, confounding variables, radiographs, laboratory or acuity markers were not included in the data collected (in simple correlation, we could miss their contribution or be the cause of the correlation). This study looked at how each interval affected the time a patients waited for an ED room. While the above confounders exist as part of the intervals’ daily variation in presentation complaint and evaluation, even with this daily variation, the simple correlation remained, demonstrating the significant component effect of time to receive a room in the patients’ LOS.
CONCLUSION
Physician-dependent intervals had minimal correlation to the variation in the “door to room” time. The average “doctor to discharge” time required to evaluate the patient remains relatively consistent and does not correlate to variation in “door to room” times. The “door to room” interval was a significant component to the variation in “door to discharge,” i.e. LOS, so delay in having a bed available in the ED correlates to extended ED “door to room.” The hospital-influenced “admit decision to hospital bed,” i.e. hospital inpatient capacity, interval had a correlation to delayed “door to room” time. The other major factor affecting department bed availability was the “total patients per day,” and the correlation to the increasing “door to room” time also supports the effect availability of resources (beds) had on completing patient evaluation. The time that it took for a patient to receive a room appeared more dependent on the system resources, for example, beds in the ED as well as in the hospital, than on the physician.
Footnotes
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- 1.National Hospital Ambulatory Medical Care Survey. 2008 Emergency Department, Summary Table. US department of health and Human Services, Division of Health Care Statistics; [Google Scholar]
- 2.Shute N, Marcus MB. Code Blue Crisis in the Emergency Department. Turning Away Patients. Long Delays. A Surefire Recipe for Disaster. US New & World Report. 2001;131(9):54–61. [PubMed] [Google Scholar]
- 3.Richards JR, Navarro ML, Derlet RW. Survey of Directors of Emergency Departments in California on Overcrowding. West J Emerg Med. 2000;172(6):385–388. doi: 10.1136/ewjm.172.6.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Derlet R, Richards J, Kravitz R. Frequent Overcrowding in U.S. Emergency Departments. Acad Emerg Med. 2001;8(2):151–155. doi: 10.1111/j.1553-2712.2001.tb01280.x. [DOI] [PubMed] [Google Scholar]
- 5.Herring A, Wilper A, Himmelstein DU, et al. Increasing Length of Stay Among Adult Visits to U.S. Emergency Departments, 2001–2005. Acad Emerg Med. 2009;16(7):609–616. doi: 10.1111/j.1553-2712.2009.00428.x. [DOI] [PubMed] [Google Scholar]
- 6.Hoffenberg S, Hill BH, Houry D. Does Sharing Process Differences Reduce Patient Length of Stay in The Emergency Department? Acad Emerg Med. 2001;8(5):578. doi: 10.1067/mem.2001.119426. [DOI] [PubMed] [Google Scholar]
- 7.Kyriacou DN, Ricketts V, Dyne PL, et al. A 5-Year Time Study Analysis of Emergency Department Patient Care Efficiency. Ann Emerg Med. 1999;34(3):326–335. doi: 10.1016/s0196-0644(99)70126-5. [DOI] [PubMed] [Google Scholar]
- 8.Schneider S, Zwemer F, Doniger A, et al. Rochester, New York: A Decade of Emergency Department Overcrowding. Acad Emerg Med. 2001;8(11):1044–1050. doi: 10.1111/j.1553-2712.2001.tb01113.x. [DOI] [PubMed] [Google Scholar]
- 9.Lambe S, Washington DL, Fink A, et al. Trends in the Use and Capacity of California’s Emergency Departments, 1990–1999. Ann Emerg Med. 2002;39(4):389–396. doi: 10.1067/mem.2002.122433. [DOI] [PubMed] [Google Scholar]
- 10.Wuerz RC, Milne LW, Eitel DR, et al. Reliability and Validity of a New Five-Level Triage Instrument. Acad Emerg Med. 2000;7:236.e42. doi: 10.1111/j.1553-2712.2000.tb01066.x. [DOI] [PubMed] [Google Scholar]
- 11.Welch S, Augustine J, Camargo CA, Jr, et al. Emergency Department Performance Measures and Benchmarking Summit. Acad Emerg Med. 2006;13(10):1074–1080. doi: 10.1197/j.aem.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 12.Russ S, Jones I, Aronsky D, et al. Placing Physician Orders at Triage: The Effect on Length of Stay. Ann Emerg Med. 2010;56(1):27–33. doi: 10.1016/j.annemergmed.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Retezar R, Bessman E, Ding R, et al. The Effect of Triage Diagnostic Standing Orders on Emergency Department Treatment Time. Ann Emerg Med. 2010;57(2):89–99.e2. doi: 10.1016/j.annemergmed.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 14.Considine J, Kropman M, Kelly E, et al. Effect of emergency department fast track on emergency department length of stay: a case-control study. Emerg Med J. 2008;25:815–819. doi: 10.1136/emj.2008.057919. [DOI] [PubMed] [Google Scholar]
- 15.Ding R, McCarthy ML, Desmond JS, et al. Characterizing Waiting Room Time, Treatment Time, and Boarding Time in the Emergency Department Using Quantile Regression. Acad Emerg Med. 2010;17(8):813–823. doi: 10.1111/j.1553-2712.2010.00812.x. [DOI] [PubMed] [Google Scholar]
- 16.Asaro PV, Lewis M, Boxerman SB. The Impact of Input and Output Factors on Emergency Department Throughput. Acad Emerg Med. 2007;14(3):235–242. doi: 10.1197/j.aem.2006.10.104. [DOI] [PubMed] [Google Scholar]
- 17.Institute of Medicine of the National Academics. The Future of Emergency Care in the United States Health System, Brief Report. June. 2006. [DOI] [PubMed] [Google Scholar]
- 18.McCarthy ML, Zeger SL, Ding R, et al. Crowding Delays Treatment and Lengthens Emergency Department Length of Stay, Even Among High-Acuity Patients. Ann Emerg Med. 2009;54(4):492–503. doi: 10.1016/j.annemergmed.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 19.Bagust A, Place M, Posnett JW. Dynamics of bed use in accommodating emergency admissions: stochastic simulation model. BMJ. 1999;319(7203):155–158. doi: 10.1136/bmj.319.7203.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schull MJ, Szalai J, Schwartz B. Emergency Department Overcrowding Following Systematic Hospital Restructuring: Trends at Twenty Hospitals over Ten Years. Acad Emerg Med. 2001;8(11):1037–1043. doi: 10.1111/j.1553-2712.2001.tb01112.x. [DOI] [PubMed] [Google Scholar]
- 21.Vicellio A, Santora C, Singer AJ, et al. The Association Between Transfer of Emergency Department Boarders to Inpatient Hallways and Mortality: A 4-Year Experience. Ann Emerg Med. 2009;54(4):487–491. doi: 10.1016/j.annemergmed.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 22.Rathlev NK, Chessare J, Olshaker J, et al. Time Series Analysis of Variables Associated With Daily Mean Emergency Department Length of Stay. Ann Emerg Med. 2007;49(3):265–271. doi: 10.1016/j.annemergmed.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 23.Lucas R, Farley H, Twanmoh J, et al. Emergency Department Patient Flow: The Influence of Hospital Census Variables on Emergency Department Length of Stay. Acad Emerg Med. 2009;16(7):597–602. doi: 10.1111/j.1553-2712.2009.00397.x. [DOI] [PubMed] [Google Scholar]