Abstract
BACKGROUND AND OBJECTIVES:
Inpatient pediatric mental health is a priority topic for national quality measurement and improvement, but nationally representative data on the patients admitted or their diagnoses are lacking. Our objectives were: to describe pediatric mental health hospitalizations at general medical facilities admitting children nationally; to assess which pediatric mental health diagnoses are frequent and costly at these hospitals; and to examine whether the most frequent diagnoses are similar to those at free-standing children’s hospitals.
METHODS:
We examined all discharges in 2009 for patients aged 3 to 20 years in the nationally representative Kids’ Inpatient Database (KID) and in the Pediatric Health Information System (free-standing children’s hospitals). Main outcomes were frequency of International Classification of Diseases, Ninth Revision, Clinical Modification–defined mental health diagnostic groupings (primary and nonprimary diagnosis) and, using KID, resource utilization (defined by diagnostic grouping aggregate annual charges).
RESULTS:
Nearly 10% of pediatric hospitalizations nationally were for a primary mental health diagnosis, compared with 3% of hospitalizations at free-standing children’s hospitals. Predictors of hospitalizations for a primary mental health problem were older age, male gender, white race, and insurance type. Nationally, the most frequent and costly primary mental health diagnoses were depression (44.1% of all mental health admissions; $1.33 billion), bipolar disorder (18.1%; $702 million), and psychosis (12.1%; $540 million).
CONCLUSIONS:
We identified the child mental health inpatient diagnoses with the highest frequency and highest costs as depression, bipolar disorder, and psychosis, with substance abuse an important comorbid diagnosis. These diagnoses can be used as priority conditions for pediatric mental health inpatient quality measurement.
Keywords: pediatric hospitalization, child mental health, depression, bipolar disorder, psychosis, costs
What’s Known on This Subject:
The pediatric mental health burden is substantial, with >4 million children meeting criteria for a mental health disorder. Mental health is a key priority for national pediatric inpatient quality measures, but little is known about admitted patients and their diagnoses.
What This Study Adds:
Nationally, nearly 10% of hospitalizations in children >3 years are for primary mental health diagnoses. The most common and costly are depression, bipolar disorder, and psychosis. Fewer free-standing children’s hospitalizations (3%) were for mental health admissions, although diagnostic distributions were similar.
The burden of pediatric mental health disorders is significant. An estimated 20% of children and adolescents in the United States meet diagnostic criteria for a mental health disorder,1–3 and inpatient and outpatient costs of treating these children are estimated at $247 billion annually.2,3 This burden is growing; inpatient admissions for mental health problems among youth increased 24% from 2007 to 2010,4 and hospitalizations among youth for mood disorders increased 80% from 1997 to 2010.5 In response, recent federal health policies have identified child mental health as a target area for quality improvement.6,7 The Child Health Insurance Program Reauthorization Act Pediatric Quality Measures Program named inpatient mental health as a priority for quality measurement,8 making optimizing care for these children a national goal.
The National Quality Forum, a multistakeholder body that endorses quality measures for national use, uses a strategy that identifies “high impact” inpatient conditions (eg, common and costly) as a way to prioritize diagnoses for national inpatient quality measures.9 Although there is a rich literature on pediatric mental health care outpatient utilization and there are statewide data for 2 states on predictors of inpatient use among publicly insured children,10,11 no studies have examined which specific inpatient mental health diagnoses are the most common or the most costly, and there are no nationally representative descriptions of pediatric mental health hospitalizations.
Nonpsychiatric medical inpatient facilities for children in the United States (the intended targets for national quality measurement) can be categorized into 2 major hospital types: (1) hospitals that serve adults and admit children (henceforth referred to as “general hospitals”) and (2) tertiary care referral hospitals that serve as regional centers for complex, chronically ill children. The tertiary care hospitals serve a smaller but substantial proportion of pediatric patients nationally.12 Patients are generally sicker than those in general hospitals and have higher risks of adverse outcomes and decreased quality of life due to complex chronic illnesses.13,14 Little is known about the differences between the 2 types of pediatric hospitals in the mental health diagnoses they care for, which may differ given the differences in their medical diagnoses. To measure and improve the quality of inpatient pediatric mental health care, it is important to understand the national landscape of all hospitals admitting children as well as to explore how the patient population in tertiary care centers might differ from the national group.
We accomplished these objectives in the current study by using data from a nationally representative sample of US pediatric hospital discharges to (1) estimate the proportion of hospitalizations for a primary mental health diagnosis, (2) examine how mental health hospitalizations vary by child demographic and hospital characteristics, and (3) prioritize diagnoses for quality measure development, using frequency of hospitalizations and aggregated total charges as markers of high impact.9 By using data from a large sample of free-standing children’s hospital discharges, which are all tertiary care hospitals, we also assessed the most common mental health diagnoses in these hospitals compared with hospitals nationally.
Methods
Data Sources
We used the nationally representative Kids’ Inpatient Database (KID) 2009 from the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project (HCUP).15 The 2009 KID contains administrative data on pediatric discharges for patients 0 to 20 years of age from 4121 hospitals in 44 states. The database includes free-standing children’s hospitals and does not include stand-alone psychiatric hospitals. Annual data are gathered every 3 years; 2009 is the most recent. The KID randomly samples 10% of newborn discharges from every participating hospital and 80% of all other pediatric discharges. The stratified sampling frame has been previously described, with HCUP providing sampling weights to create nationally representative statistics.15
To assess hospitalizations in pediatric tertiary care referral hospitals, we used the 2009 Pediatric Health Information System (PHIS) Inpatient database. PHIS is the largest database of free-standing children’s hospitals, which are all tertiary care referral centers. The PHIS includes all discharges from 43 free-standing children’s hospitals in 25 states. In the past 5 years, >130 peer-reviewed publications have used this database to study national inpatient pediatric care delivery.16–21 We chose not to use the KID for analysis of patterns in free-standing children’s hospitals because it has a 9% missing rate for hospital type.
In both data sources, the administrative data include demographic characteristics, procedures, and diagnoses in an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) format. Each record represents a single discharge, so patients may contribute >1 record. Discharge diagnoses are designated as primary or nonprimary, with up to 24 (KID) or 40 (PHIS) fields available for nonprimary diagnoses. Discharge documentation for hospital billing is used to designate the primary discharge diagnosis.
Patients
We analyzed hospital discharge abstracts for patients aged 3 to 20 years. Patients discharged with a mental health diagnosis were identified in KID and PHIS by using ICD-9-CM codes. We first examined patients with a primary mental health diagnosis. To assess the burden of specific diagnoses overall in inpatient settings, we also assessed the frequency of hospitalizations by mental health diagnostic groupings for patients with “any” mental health diagnosis, designated as either primary or nonprimary (“comorbid”). Two experienced child mental health clinician-researchers (J.M.M. and B.T.Z.) created 17 general diagnostic category groupings from >200 specific mental health codes from ICD-9-CM. These categories were aligned with disorder classifications from the Diagnostic and Statistical Manual of Mental Disorders (DSM), Fourth Edition (DSM-IV), and reviewed again after the DSM-V release. DSM manuals do not define suicidality as a distinct diagnosis because it is a symptom in several diagnoses, so it was not included as a separate grouping in this coding. See Supplemental Information Table 4 for mental health ICD-9-CM grouping definitions.
Analysis
All analyses using KID data were weighted by using survey weights provided by HCUP.15 All PHIS analyses were unweighted. We calculated summary statistics for age, gender, and insurance status for all admissions in each database to provide a reference description of the patient populations (Supplemental Information Table 5).
Univariate analyses comparing patient and hospital characteristics for mental health and non–mental health pediatric hospitalizations were conducted by using χ2 tests for categorical variables (age group, gender, race, insurance type, and discharge status; and hospital size, owner type, location, and teaching status) and t tests to compare length of stay (LOS) and hospital charges. To be parsimonious, the adjusted multivariate regression model comparing primary mental health to non–mental health hospitalizations only included the patient and hospital characteristics with a univariate analysis P value of <.20. LOS, discharge status, and hospital charges were not included in the multivariate model because these are indicators of resource utilization.
To assess for the most common causes of admission, we assessed the frequency of hospitalizations by mental health diagnostic groupings for 2 groups: patients with a primary mental health diagnosis and patients with any mental health diagnosis (primary or comorbid). We made these assessments separately in the KID and PHIS data sets. We compared the KID and PHIS proportions of patients with specific mental health diagnoses by using Wilcoxon rank sum testing.
To assess national resource utilization for each primary mental health diagnostic grouping, we used KID 2009 to calculate the following for each grouping: mean charges, total aggregate charges, and mean LOS. We used hospital charges (the amount billed by the hospital) rather than costs of the inpatient stay (actual amount paid to the hospital) due to missing cost-to-charge ratios for some children’s hospitals in the KID database. Aggregate hospital charges, referred to as the “total national health care bill,”22 calculated for each diagnostic grouping allow comparison of relative resource utilization across diagnoses.
All analyses used Stata 12 (StataCorp LP, College Station, TX). The University of California, San Francisco, and Seattle Children’s Hospital Institutional Review Boards approved the study.
Results
During the period studied, there were 159 629 hospitalizations with primary mental health diagnoses for children ages 3 to 20 years sampled in the KID database. When sampling weights were applied, these sampled hospitalizations represented 9.6% (n = 228 808) of 3- to 20-year-old pediatric hospitalizations nationally (N = 2 372 385). All remaining results for KID analyses represent survey-weighted analyses. In PHIS free-standing children’s hospitals, 3.3% (n = 12 542) of the hospitalizations for children aged 3 to 20 years (n = 375 844) had a primary mental health diagnosis (Table 1). When examining the proportion of hospitalizations with any mental health diagnosis (either primary or comorbid), the 2 data sources were more similar, with 22% (n = 523 105) of hospitalizations nationally (KID) having any mental health diagnosis and 17.7% (n = 66 660) of hospitalizations from free-standing children’s hospitals (PHIS).
TABLE 1.
Mental Health and Non–Mental Health Pediatric Hospitalizations for 3- to 20-Year-Olds Nationally, 2009
| Mental Health (N = 228 808)a | Non–Mental Health (N = 2 143 578)a | P | |
|---|---|---|---|
| Patient characteristics | |||
| Age group, n (%) | <.001b | ||
| 3–5 years | 1821 (0.8) | 235 784 (11.1) | |
| 6–11 years | 25 546 (11.1) | 374 286 (17.7) | |
| 12–17 years | 118 683 (51.9) | 639 865 (30.3) | |
| 18–20 years | 82 758 (36.2) | 860 456 (40.8) | |
| Male gender, n (%) | 116 632 (51.2) | 747 239 (35.6) | <.001b |
| Race/ethnicity, n (%) | <.001b | ||
| White | 115 445 (63.5) | 900 523 (50.0) | |
| Black | 31 442 (17.3) | 349 590 (19.4) | |
| Hispanic | 20 421 (11.2) | 415 659 (23.1) | |
| Other | 14 589 (8.0) | 137 349 (7.6) | |
| Insurance status, n (%) | <.001b | ||
| Private | 99 985 (43.9) | 851 967 (39.8) | |
| Medicaid | 99 218 (43.6) | 1 074 129 (50.2) | |
| Uninsured | 15 389 (6.8) | 116 080 (5.4) | |
| Other | 13 093 (5.8) | 97 900 (4.6) | |
| LOS, mean (95% CI), d | 7.4 (6.8–8.0) | 3.3 (3.3–3.4) | <.001c |
| Discharge status, n (%) | <.001b | ||
| Routine to home | 207 250 (90.8) | 1 994 276 (93.1) | |
| Short-term hospital transfer | 4221 (1.8) | 31 412 (1.5) | |
| Transfer to other hospital typed | 12 129 (5.3) | 30 222 (1.4) | |
| Home health care | 483 (2.1) | 69 758 (3.3) | |
| Against medical advice | 4131 (1.8) | 10 368 (0.5) | |
| Died | 8 (<0.1) | 6389 (0.3) | |
| Charges, mean (95% CI), $ | 15 540 (14 571–16 508) | 23 768 (22 685–24 852) | <.001c |
| Hospital characteristics, n (%) | |||
| Size | .047b | ||
| Small | 20 500 (9.5) | 225 575 (11.3) | |
| Medium | 45 479 (21.0) | 507 109 (25.4) | |
| Large | 150 535 (69.5) | 1 267 104 (63.4) | |
| Profit status | .71b | ||
| Not-for-profit, public | 29 249 (13.5) | 296 757 (14.8) | |
| Not-for-profit, private | 162 854 (75.2) | 1 467 083 (73.4) | |
| Commercial | 24 411 (11.3) | 235 948 (11.8) | |
| Teaching | 127 253 (58.8) | 1 148 533 (57.4) | .60b |
| Urban | 198 816 (91.8) | 1 761 922 (88.1) | <.001b |
Unweighted visits = 159 629 for mental health visits and 1 610 503 for non–mental health visits.
Determined by using survey-weighted χ2 analyses comparing proportions of visits in each category for mental health visits with non–mental health visits.
Determined by using survey-weighted Student’s t tests comparing the mean values for all mental health visits with mean values for non–mental health visits.
Includes skilled nursing facility, intermediate care facility, or another type of facility.
Characteristics Associated With Mental Health Hospitalizations
In unadjusted analyses of pediatric hospitalizations nationally from KID, hospitalizations with a primary mental health diagnosis were more frequently for older (P < .001), male (P < .001), white non-Hispanic (P < .001), and privately insured (P < .001) patients, compared with hospitalizations with a non–mental health primary diagnosis. Hospitalizations for primary mental health diagnoses had longer LOS (mean: 7.4 vs 3.3 days; P < .001) and lower charges (mean: $15 540 vs $23 768; P < .001) compared with hospitalizations for a non–mental health primary diagnosis. Hospitalizations for mental health primary diagnoses occurred more frequently at urban hospitals and at larger hospitals than hospitalizations for non–mental health primary diagnoses (Table 1). These relationships persisted in adjusted analyses except for the relationship with hospital size, which became non-significant (Table 2).
TABLE 2.
Patient and Hospital Characteristics Associated With a Primary Mental Health Admission Among Hospitalized 3- to 20-Year-Olds Nationally, 2009
| Adjusted Odds Ratio (95% CI) | P | |
|---|---|---|
| Patient characteristics | ||
| Age group | ||
| 3–5 years | Ref | — |
| 6–11 years | 9.7 (8.5–11.2) | <.001 |
| 12–17 years | 30.2 (25.6–35.7) | <.001 |
| 18–20 years | 18.0 (14.9–21.7) | <.001 |
| Male gender | 2.13 (2.03–2.25) | <.001 |
| Race | ||
| White | Ref | — |
| Black | 0.69 (0.61–0.77) | <.001 |
| Hispanic | 0.37 (0.30–0.46) | <.001 |
| Other | 0.86 (0.73–1.01) | .08 |
| Insurance | ||
| Private | Ref | — |
| Medicaid | 1.05 (0.93–1.19) | .42 |
| Uninsured | 1.31 (1.14–1.50) | <.001 |
| Other | 1.32 (1.11–1.58) | .002 |
| Hospital characteristics | ||
| Size | ||
| Small | Ref | — |
| Medium | 1.10 (0.71–1.70) | .68 |
| Large | 1.45 (0.97–2.16) | .07 |
| Urban | 1.78 (1.40–2.27) | <.001 |
P values were obtained by using a logistic regression model including all presented variables. Variables with P values ≥.20 in the univariate analysis were not included in this multivariate model. LOS, discharge status, and charges were not included in the multivariable model because they are markers of utilization rather than explanatory variables for hospitalization with a mental health diagnosis. Ref, reference.
Most Common Mental Health Diagnoses in Pediatric Hospitalizations
Nationally, among hospitalizations with a primary mental health diagnosis in KID, the most common diagnoses were depression (44.1%), bipolar disorder (18.1%), and psychosis (12.1%) (Table 3). Among hospitalizations with a primary mental health diagnosis in free-standing children’s hospitals (PHIS), the most common primary mental health diagnoses were depression (42.2%), externalizing disorder (10.8%), and bipolar disorder (10.6%) (Table 3). The differences between KID and PHIS in the distributions of specific primary mental health diagnoses were statistically significant (P = .002).
TABLE 3.
Most Common Primary and Comorbid Pediatric Mental Health Inpatient Diagnoses in Hospitals Nationally and in Free-standing Children’s Hospitals for 3- to 20-Year-Olds in 2009
| Primary Mental Health Diagnosisa | Any Mental Health Diagnosisb | |||
|---|---|---|---|---|
| Ranking | National Inpatient Hospitals (N = 228 808)c | Children’s Hospitals, Inpatient (N = 12 542) | National Inpatient Hospitals (N = 523 105)c | Children’s Hospitals, Inpatient (N = 66 660) |
| 1 | Depression*: 100 988 (44.1) | Depression*: 5290 (42.2) | Depression: 187 902 (35.9) | Developmental disorder: 21 796 (32.7) |
| 2 | Bipolar disorder*: 41 345 (18.1) | Externalizing disorder: 1351 (10.8) | Substance abuse: 177 680 (34.0) | Depression: 15 936 (23.9) |
| 3 | Psychosis*: 27 589 (12.1) | Bipolar disorder*: 1325 (10.6) | ADHD: 101 658 (19.4) | ADHD: 15 247 (22.9) |
| 4 | Externalizing disorder: 14 087 (6.2) | Anxiety: 971 (7.7) | Anxiety: 90 140 (17.2) | Autism: 7120 (10.7) |
| 5 | Reaction disorder: 11 856 (5.2) | Psychosis*: 823 (6.6) | Bipolar disorder: 79 352 (15.2) | Externalizing disorder: 6509 (9.8) |
| 6 | Anxiety: 9288 (4.1) | Eating disorder: 684 (5.5) | Externalizing disorder: 63 368 (12.1) | Substance abuse: 5918 (8.9) |
| 7 | Substance abuse: 8501 (3.7) | Miscellaneous: 535 (4.3) | Developmental disorder: 61 662 (11.8) | Anxiety: 5326 (8.0) |
| 8 | ADHD: 6920 (3.0) | ADHD: 343 (2.7) | Psychosis: 51 158 (9.8) | Psychosis: 4545 (6.8) |
| 9 | Eating disorder: 2398 (1.1) | Substance abuse: 308 (2.5) | Reaction disorder: 28 030 (5.4) | Bipolar disorder: 4539 (6.8) |
| 10 | Autism: 2353 (1.0) | Autism: 271 (2.2) | Personality disorder: 26 666 (5.1) | Reaction disorder: 3012 (4.5) |
Data are presented as n (%). Conditions shown with an asterisk (*) indicate the most common and costly primary diagnostic groups in the nationally representative KID. “Developmental disorder” includes learning and communication disorders and intellectual disabilities; “Externalizing disorder” includes oppositional defiant disorder, intermittent explosive disorder, impulse control disorder, and conduct disturbance; “Miscellaneous” includes psychogenic pain, postconcussive syndrome, sleep disorders, and tension headaches.
Mental health diagnoses are designated as primary based on physician discharge documentation. Comparison of national KID and free-standing children’s hospitals (PHIS) data sets using Wilcoxon rank sum testing, P = .002.
“Any” mental health diagnosis refers to primary or nonprimary (ie, comorbid) mental health diagnoses. Comparison of national KID and PHIS free-standing children’s hospitals datasets using Wilcoxon rank sum testing, P = .001.
Unweighted observations used for estimation sample of hospitalizations with a primary mental health diagnosis in national visits: 159 629 visits; hospitalizations with primary or comorbid mental health diagnosis nationally: 375 325.
Among hospitalizations with any mental health diagnosis nationally (KID), the most common diagnosis remained depression (35.9%), followed by substance abuse (34.0%) and attention-deficit/hyperactivity disorder (ADHD; 19.4%). Among hospitalizations with any mental health diagnosis in free-standing children’s hospitals, the most common diagnoses were developmental disorder (32.7%), depression (23.9%), and ADHD (22.9%) (P = .001 for differences in distribution of specific diagnoses between KID and PHIS hospitalizations with any mental health diagnosis) (Table 3).
The most substantial differences between hospitals nationally (KID) and free-standing children’s hospitals (PHIS) in regard to which mental health diagnoses were most common were as follows: for hospitalizations with a primary mental health diagnosis, eating disorders were more common in PHIS (5.5% in PHIS versus 1.1% in KID); for hospitalizations with any mental health diagnosis, substance abuse was more common in KID (34.0% in KID versus 8.9% in PHIS) and developmental disorder and autism were more common in PHIS (32.7% in PHIS vs 11.8% in KID for developmental disorder and 10.7% in PHIS vs 5.1% in KID for autism) (Table 3).
Utilization in Primary Mental Health Hospitalizations Nationally
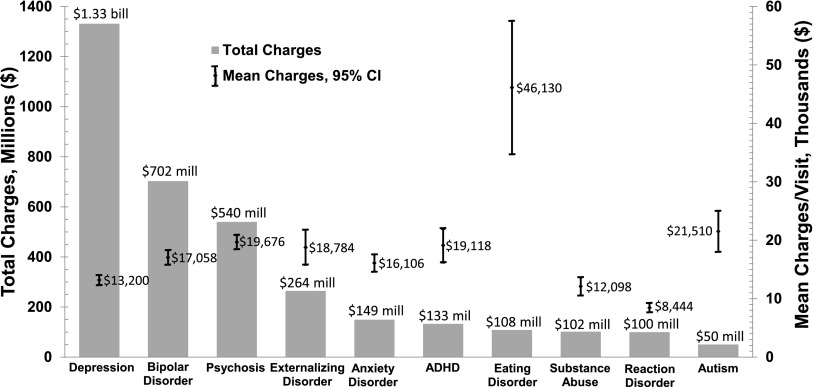
Nationally, mean charges for hospitalizations for a primary mental health diagnosis were $15 540 (95% confidence interval [CI]: $14 571–$16 508). Average LOS was 7.4 days (95% CI: 6.8–8.0 days) compared with 3.3 days (95% CI: 3.3–3.4 days) for hospitalizations without a primary mental health diagnosis (Table 1). Mental health discharges were more likely to be transferred to other institutions (5.3% vs 1.4%) or leave against medical advice (1.8% vs 0.5%; P < .001 for differences across discharge status) (Table 1). Aggregate charges for all hospitalizations nationally with a primary mental health diagnosis were $3.5 billion (6.5% of total charges for all studied mental health and non–mental health hospitalizations). Diagnosis-specific aggregate charges were highest for depression ($1.33 billion), bipolar disorder ($702 million), and psychosis ($540 million). Mean LOS ranged from a low of 3.8 days (95% CI: 3.5–4.1 days) for reaction disorders to a high of 14.3 days (95% CI: 12.3–16.3 days) for eating disorders. Mean LOS for the other groupings ranged from 6.4 to 10.8 days. Diagnosis-specific mean charges were highest for eating disorders ($46 130) (Fig 1).
FIGURE 1.
Resource utilization for the most common primary inpatient mental health diagnoses for 3- to 20-year-olds nationally. bill, billion; mill, million.
Discussion
To our knowledge, this is the first study describing pediatric mental health hospitalizations in a nationally representative sample from all hospitals admitting children and in the regionalized system of free-standing children’s hospitals. We found that mental health hospitalizations are common and costly nationally, with nearly 1 in 10 pediatric admissions having a primary diagnosis of a mental health condition. This finding exceeds national estimates of hospitalizations for asthma (7.1% for 1- to 17-year-olds).23 Aggregate charges for depression alone ($1.33 billion) are comparable to the $1.50 billion in aggregate charges for asthma in 2009.23
Our findings of a substantially lower proportion of mental health hospitalizations in free-standing children’s hospitals (3.3%) compared with hospitals admitting children nationally (9.6%) indicate that general hospitals deliver more inpatient psychiatric services than free-standing children’s hospitals. This difference in mental health care delivery may be because of greater availability of mental health subspecialty services in general hospitals compared with free-standing children’s hospitals, which are often focused on the medical needs of complex chronically ill children24 and may not be licensed for inpatient psychiatric beds. In general hospitals, a higher proportion of mental health hospitalizations were transferred compared with non–mental health hospitalizations, suggesting that some patients may be admitted for medical stabilization and then transferred to other hospitals for psychiatric care. A study of patterns of transfer for mental health emergency department visits at free-standing children’s hospitals might help explain the lower proportion of mental health hospitalizations at free-standing children’s hospitals.
Although the proportion of visits for primary mental health diagnoses is smaller in free-standing children’s hospitals, the finding that the most common primary diagnoses in both systems are the same supports the creation of diagnosis-specific quality measures for all hospitals that admit children. Potential mental health diagnostic priorities, defined as (1) the most common at all hospitals admitting children and at free-standing children’s hospitals and (2) incurring the greatest inpatient expenses nationally, are depression, bipolar disorder, and psychosis. Subsequent delineation of the highest impact, evidence-based processes and outcomes of care within each child mental health diagnosis will guide selection of potential quality measures.
We found that proportions of hospitalizations with any (primary or comorbid) mental health diagnoses were high in both systems (17.1% in free-standing children’s hospitals and 22.0% nationally). This finding suggests that the complex chronically ill children at free-standing children’s hospitals have a relatively high burden of mental health comorbidities, which is consistent with studies in chronically ill pediatric outpatients.25–29 We also found that the most common comorbid mental health diagnoses differed between hospitals nationally and free-standing hospitals. Comorbid developmental disorder and autism were common in free-standing children’s hospitals, suggesting that developmental and behavioral expertise may be a useful resource in these hospitals. Substance abuse was a common comorbidity in hospitals nationally, indicating that substance abuse may be an important focus for quality measurement. Further work assessing how comorbid mental health disorders may complicate the treatment of a child’s primary diagnosis could suggest interventions to improve overall health outcomes.
Eating disorder hospitalizations represent a substantial number of the hospitalizations for primary mental health diagnoses in free-standing hospitals but may be too uncommon nationally to be a high-priority area for quality measurement.9,30 Because of their long LOS and high mean costs, eating disorders could be a focus for quality measurement in tertiary and quaternary care children’s hospitals.
ADHD was a common comorbid diagnosis in both settings (19.4% of hospitalizations with any mental health diagnosis in hospitals nationally and 22.9% in free-standing children’s hospitals). This finding suggests that ADHD may contribute to factors (eg, accidents, medical nonadherence) leading to hospitalization. However, ADHD was an uncommon primary diagnosis and the American Academy of Pediatrics guidelines recommend outpatient primary care management of the disease in a medical home.31 Thus, while maintaining ADHD as a high-priority condition in the outpatient setting may be important,8,32 ADHD may not be a diagnostic priority for quality measurement in the inpatient setting.
We found a greater likelihood of inpatient utilization for primary mental health diagnoses for those of white race compared with those of black race or Hispanic ethnicity. Previous studies of outpatient mental health care have shown that minority children are more likely to be undiagnosed33,34 and that, among children with mental health diagnoses, black and/or Hispanic children are less likely to receive outpatient mental health services.35–39 The increased adjusted likelihood of mental health hospitalization associated with race in the model that includes insurance type (Table 2) indicates that lack of insurance would not completely explain the relationship between race/ethnicity and mental health hospitalizations. Linked outpatient data for these hospital admissions would be helpful in exploring potential reasons for racial/ethnic differences in inpatient utilization.
This study has several limitations. The databases do not include stand-alone psychiatric hospitals, which limits a description of all hospitals delivering pediatric mental health care. Our findings are relevant to primarily medical hospitals admitting a substantial proportion of pediatric patients with mental health diagnoses. PHIS does not include all free-standing children’s hospitals in the country, so it is not nationally representative. However, it is the largest database of free-standing children’s hospitals and captures 16.1% of all pediatric inpatient hospitalizations for 3- to 20-year-olds nationally (Supplemental Information Table 4). We used charges rather than costs due to limited availability of cost-to-charge ratios for the free-standing children’s hospitals. Charges allow an assessment of the relative resource utilization for diagnostic groupings; thus, although not representing absolute cost to the system, they allow relative comparisons of financial impact and are useful for prioritizing specific conditions for quality measurement. In addition, caution is required in applying administrative data findings to individual patients because patients may be counted more than once in these databases. However, administrative data capture the burden to the system, which was the primary research objective. Last, ICD-9-CM codes may be limited in their accuracy for correctly identifying mental health diagnoses40 and may be limited in their sensitivity for identifying all patients with psychiatric diagnoses, if some providers are reluctant to bill for potentially stigmatizing mental health diagnoses. However, in quality measurement, the use of ICD-9-CM codes is currently the most feasible method of patient identification.
Conclusions
Mental health hospitalizations are common in pediatrics and are less common in free-standing children’s hospitals compared with hospitals nationally. Mental health diagnostic priorities for inpatient quality measurement are similar among hospitals nationally and free-standing children’s hospitals. Priorities include depression, bipolar disorder, and psychosis, with substance abuse a potential priority as a comorbid mental health diagnosis. This strategy for prioritization of inpatient diagnoses for quality measurement uses the nationally accepted criterion of high-impact (eg, common or costly) diseases and, specific to pediatrics, focuses on the most common diseases in both tertiary care pediatric referral centers and all hospitals admitting children nationally.
Supplementary Material
Acknowledgments
We thank Dr Lingqi Tang, PhD, for her statistical consultation and Ms Anna Lynn, MPP, for her input on study design and analysis.
Glossary
- ADHD
attention-deficit/hyperactivity disorder
- CI
confidence interval
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- HCUP
Healthcare Cost and Utilization Project
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- KID
Kids’ Inpatient Database
- LOS
length of stay
- PHIS
Pediatric Health Information System
Footnotes
Dr Bardach conceptualized and designed the study, supervised data management, conducted the data analyses, drafted the initial manuscript, and revised the final manuscript as submitted; Dr Coker made substantial contributions to the study conception and design and critically revised the manuscript; Drs Zima and Murphy contributed to the study conception and design and study variable construction and critically revised the manuscript; Dr Knapp contributed to the design, assisted in the initial draft of the manuscript, and revised the article for intellectual content; Dr Edwall contributed to the study design and interpretation of results and reviewed the final manuscript; Drs Richardson and Mangione-Smith contributed to the study design and interpretation of results and critically reviewed and revised the initial manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This study was supported by the Agency for Healthcare Research and Quality (U18 HS020506-03) and the National Institute for Children’s Health and Human Development (K23HD065836), Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Shaffer D, Fisher P, Dulcan MK, et al. The NIMH Diagnostic Interview Schedule for Children version 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA study. Methods for the Epidemiology of Child and Adolescent Mental Disorders Study. J Am Acad Child Adolesc Psychiatry. 1996;35(7):865–877 [DOI] [PubMed] [Google Scholar]
- 2.Costly mental disorders affect millions of us children and teens: News from the centers for disease control and prevention. JAMA. 2013;310(1):23 [Google Scholar]
- 3.Perou R, Bitsko RH, Blumberg SJ, et al. Centers for Disease Control and Prevention . Mental health surveillance among children—United States, 2005-2011. MMWR Surveill Summ. 2013;62(2 suppl 2):1–35 [PubMed] [Google Scholar]
- 4.Health Cost Institute. Children’s Health Care Spending Report: 2007–2010. July 2012. Available at: www.healthcostinstitute.org/files/HCCI_CHCSR20072010.pdf. Accessed May 29, 2013
- 5.Pfuntner A, Wier LM, Stocks C. Most frequent conditions in U.S. hospitals, 2010. Statistical brief no. 148. AHRQ HCUP Statistical Briefs; January 2013. Available at: www.hcup-us.ahrq.gov/reports/statbriefs/sb148.pdf. Accessed May 29, 2013
- 6.Children's Health Insurance Program Reauthorization Act of 2009. Public Law 111-3 (2009) [Google Scholar]
- 7.Patient Protection and Affordable Care Act of 2010. Public Law 111-148 (2010)
- 8.CHIPRA measures by CHIPRA categories: initial core set and PQMP Centers of Excellence measure assignments. 2012;. Available at: www.ahrq.gov/chipra/pqmpmeasures.htm. Accessed May 29, 2013
- 9.National Quality Forum Measure Evaluation Criteria January 2011. Available at: www.qualityforum.org/docs/measure_evaluation_criteria.aspx. Accessed May 29, 2013
- 10.Yampolskaya S, Mowery D, Dollard N. Predictors for readmission into children's inpatient mental health treatment. Community Ment Health J 2013;49(6):781–6 [DOI] [PubMed] [Google Scholar]
- 11.Snowden LR, Masland MC, Libby AM, Wallace N, Fawley K. Racial/ethnic minority children’s use of psychiatric emergency care in California’s Public Mental Health System. Am J Public Health. 2008;98(1):118–124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berry JG, Toomey SL, Zaslavsky AM, et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309(4):372–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wise PH. The rebirth of pediatrics. Pediatrics. 2009;123(1):413–416 [DOI] [PubMed]
- 14.Chamberlain LJ, Chan J, Mahlow P, Huffman LC, Chan K, Wise PH. Variation in specialty care hospitalization for children with chronic conditions in California. Pediatrics. 2010;125(6):1190–1199 [DOI] [PubMed] [Google Scholar]
- 15.Healthcare Cost and Utilization Project (HCUP). Introduction to the HCUP KIDs’ Inpatient database, 2009. Available at: www.hcup-us.ahrq.gov/db/nation/kid/kid_2009_introduction.jsp. Accessed June 11, 2012
- 16.PubMed.gov. Search results: “Pediatric Health Information System”[all fields] AND (“2008/08/08”[PDat]: “2013/08/06”[PDat]). 2013. Available at: www.ncbi.nlm.nih.gov/pubmed/?term=%22Pediatric+Health+Information+System%22%5BAll+Fields%5D+AND+(%222008%2F08%2F08%22%5BPDat%5D+%3A+%222013%2F08%2F06%22%5BPDat%5D). Accessed August 6, 2013
- 17.Florin TA, French B, Zorc JJ, Alpern ER, Shah SS. Variation in emergency department diagnostic testing and disposition outcomes in pneumonia. Pediatrics. 2013;132(2):237–244 [DOI] [PubMed] [Google Scholar]
- 18.Keele L, Keenan HT, Sheetz J, Bratton SL. Differences in characteristics of dying children who receive and do not receive palliative care. Pediatrics. 2013;132(1):72–78 [DOI] [PubMed] [Google Scholar]
- 19.Fieldston ES, Shah SS, Hall M, et al. Resource utilization for observation-status stays at children’s hospitals. Pediatrics. 2013;131(6):1050–1058 [DOI] [PubMed] [Google Scholar]
- 20.Myrvik MP, Burks LM, Hoffman RG, Dasgupta M, Panepinto JA. Mental health disorders influence admission rates for pain in children with sickle cell disease. Pediatr Blood Cancer. 2013;60(7):1211–1214 [DOI] [PubMed] [Google Scholar]
- 21.Stenger MR, Slaughter JL, Kelleher K, et al. Hospital variation in nitric oxide use for premature infants. Pediatrics. 2012;129(4). Available at: www.pediatrics.org/cgi/content/full/129/4/e945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.HCUPnet definitions. 2013. Available at: http://hcupnet.ahrq.gov/HCUPnet.jsp?Id=2F575D0378D24FD8&Form=MAINSEL&JS=Y&Action=%3E%3ENext%3E%3E&HCUPnet%20definitions.x=1. Accessed September 24, 2013
- 23.Agency for Healthcare Research and Quality. HCUPnet, Healthcare Cost and Utilization Project. National statistics on children. 2009. Available at: http://hcupnet.ahrq.gov/HCUPnet.jsp?Id=4578AE155E24E350&Form=SelDB&JS=Y&Action=%3E%3ENext%3E%3E&_DB=NIS09KID. Accessed September 24, 2013
- 24.Wise PH. The transformation of child health in the United States. Health Aff (Millwood). 2004;23(5):9–25 [DOI] [PubMed] [Google Scholar]
- 25.Ji L, Lili S, Jing W, et al. Appearance concern and depression in adolescent girls with systemic lupus erythematous. Clin Rheumatol. 2012;31(12):1671–1675 [DOI] [PubMed] [Google Scholar]
- 26.Grey M, Whittemore R, Tamborlane W. Depression in type 1 diabetes in children: natural history and correlates. J Psychosom Res. 2002;53(4):907–911 [DOI] [PubMed] [Google Scholar]
- 27.Szigethy E, Levy-Warren A, Whitton S, et al. Depressive symptoms and inflammatory bowel disease in children and adolescents: a cross-sectional study. J Pediatr Gastroenterol Nutr. 2004;39(4):395–403 [DOI] [PubMed] [Google Scholar]
- 28.Hood KK, Huestis S, Maher A, Butler D, Volkening L, Laffel LMB. Depressive symptoms in children and adolescents with type 1 diabetes: association with diabetes-specific characteristics. Diabetes Care. 2006;29(6):1389–1391 [DOI] [PubMed] [Google Scholar]
- 29.Tluczek A, Laxova A, Grieve A, et al. Long-term follow-up of cystic fibrosis newborn screening psychosocial functioning of adolescents and young adults [published online ahead of print October 21, 2013 10.1016/j.jcf.2013.10.001]. J Cyst Fibros. [DOI] [PMC free article] [PubMed]
- 30.Bardach NS, Chien AT, Dudley RA. Small numbers limit the use of the inpatient pediatric quality indicators for hospital comparison. Acad Pediatr. 2010;10(4):266–273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wolraich M, Brown L, Brown RT, et al. Subcommittee on Attention-Deficit/Hyperactivity Disorder. Steering Committee on Quality Improvement and Management . ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(5):1007–1022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Medicaid & Medicare Services. 2014 CMS recommended core quality measures. 2013. Available at: www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Recommended_Core_Set.html. Accessed March 8, 2013
- 33.Hacker KA, Penfold R, Arsenault L, Zhang F, Murphy M, Wissow L. Screening for behavioral health issues in children enrolled in Massachusetts Medicaid. Pediatrics 2014;133(1):46–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Howell E, McFeeters J. Children’s mental health care: differences by race/ethnicity in urban/rural areas. J Health Care Poor Underserved. 2008;19(1):237–247 [DOI] [PubMed] [Google Scholar]
- 35.Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: variation by ethnicity and insurance status. Am J Psychiatry. 2002;159(9):1548–1555 [DOI] [PubMed] [Google Scholar]
- 36.Lê Cook B, Barry CL, Busch SH. Racial/ethnic disparity trends in children’s mental health care access and expenditures from 2002 to 2007. Health Serv Res. 2013;48(1):129–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coker TR, Elliott MN, Kataoka S, et al. Racial/ethnic disparities in the mental health care utilization of fifth grade children. Acad Pediatr. 2009;9(2):89–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zimmerman FJ. Social and economic determinants of disparities in professional help-seeking for child mental health problems: evidence from a national sample. Health Serv Res. 2005;40(5 pt 1):1514–1533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Costello EJ, He JP, Sampson NA, Kessler RC, Merikangas KR. Services for adolescents with psychiatric disorders 12-month data from the National Comorbidity Survey-Adolescent [published online ahead of print November 15, 2013 10.1176/appi.ps.201100518]. Psychiatr Serv. [DOI] [PMC free article] [PubMed]
- 40.Rushton JL, Felt BT, Roberts MW. Coding of pediatric behavioral and mental disorders. Pediatrics. 2002;110(1 pt 1):e8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.