Abstract
Diabetes and infections are associated with a high risk of implant failure. However, the effects of such conditions on the electrochemical stability of titanium materials remain unclear. This study evaluated the corrosion behavior of a Ti-6Al-4V alloy, with a smooth surface or conditioned by double-acid-etching, in simulated body fluid with different concentrations of dextrose and lipopolysaccharide. For the electrochemical assay, the open-circuit-potential, electrochemical impedance spectroscopy, and potentiodynamic test were used. The disc surfaces were characterized by scanning electron microscopy and atomic force microscopy. Their surface roughness and Vickers microhardness were also tested. The quantitative data were analyzed by Pearson's correlation and independent t-tests (α = 0.05). In the corrosion parameters, there was a strong lipopolysaccharide correlation with the Ipass (passivation current density), Cdl (double-layer capacitance), and Rp (polarization resistance) values (p<0.05) for the Ti-6Al-4V alloy with surface treatment by double-acid-etching. The combination of dextrose and lipopolysaccharide was correlated with the Icorr (corrosion current density) and Ipass (p<0.05). The acid-treated groups showed a significant increase in Cdl values and reduced Rp values (p<0.05, t-test). According to the topography, there was an increase in surface roughness (R2 = 0.726, p<0.0001 for the smooth surface; R2 = 0.405, p = 0.036 for the double-acid-etching-treated surface). The microhardness of the smooth Ti-6Al-4V alloy decreased (p<0.05) and that of the treated Ti-6Al-4V alloy increased (p<0.0001). Atomic force microscopy showed changes in the microstructure of the Ti-6Al-4V alloy by increasing the surface thickness mainly in the group associated with dextrose and lipopolysaccharide. The combination of dextrose and lipopolysaccharide affected the corrosion behavior of the Ti-6Al-4V alloy surface treated with double-acid-etching. However, no dose-response corrosion behavior could be observed. These results suggest a greater susceptibility to corrosion of titanium implants in diabetic patients with associated infections.
Introduction
Diabetes is a disorder marked by abnormal lipid and glucose metabolism, often with serious complications leading to premature death [1], and it is considered a public health concern worldwide [2]. According to the Centers for Disease Control and Prevention, 10.9 million (26.9%) people aged ≥65 years and 215,000 people younger than 20 years old had diabetes in the United States in 2010, with estimated annual treatment costs of $174 billion [3].
Periodontal diseases such as periodontitis are two and a half times more likely to occur in individuals with diabetes than in those without it [4]. Additionally, diabetes presents a stalemate to patients who undergo treatment with dental implants [5]. Hyperglycemia leads to overproduction of superoxide, which contributes to the pathogenesis of diabetic micro- and macrovascular complications [6]–[8], predisposing to at least a delay in peri-implant bone repair or causing peri-implantitis [7]–[10].
Porphyromonas gingivalis is the most common bacterium contributing to peri-implantitis in partially and completely edentulous patients [11]. P. gingivalis and other Gram-negative bacteria produce lipopolysaccharide (LPS), located in the bacterial cell walls [12], [13], and its presence dictates the prognosis of implant treatment [12]–[15].
Dental implants are composed mainly of titanium (Ti) and feature a strong bond with water or air molecules in the atmosphere, which promotes the immediate formation of a Ti oxide layer on the metal surface. This property creates proper surface energy for osseointegration and corrosion resistance [16], [17]. However, changes in the surrounding oral environment, such as pH and thermal oscillations, and the presence of biofilm, can degrade the oxide layer, allowing for the exchange of Ti ions. This activity contributes to the corrosion process of the implant surface [18]–[20], substantially affecting the mechanical properties and biocompatibility of the implants, resulting in the failure of rehabilitative treatment [21]–[24].
The corrosion resistance of medical and dental Ti implants has been evaluated in vitro in simulated physiological and systemic conditions [21], [23], [25]–[28]. However, few clinical studies have reported on the corrosion of Ti in dentistry. Olmedo et al. [29] reported 2 cases of injury reaction in the peri-implant mucosa, which suggested that it was caused by Ti particles released into the surrounding tissue, resulting in corrosion of the osseointegrated implant surface. In this context, 153 patients rehabilitated with single implants underwent biopsy of the mucosa adjacent to the implant cover screws during the period of osseointegration (4–6 months). In total, 41% of these patients showed Ti particles released from the implant surface, sometimes free or surrounded by macrophages, denoting foreign body reaction with probable metal corrosion [30].
Several mechanical and chemical modifications of dental implant surfaces – such as titanium plasma spray (TPS), hydroxyapatite coating, electrochemical and mechanical polishing, acid etching, aluminum oxide sandblasting, and laser irradiation – have been proposed. These surface treatments have increased the percentage of bone-implant contact, especially in low-bone-density areas, and have accelerated the osseointegration phenomenon [31]–[38].
Therefore, this study investigated the corrosion and microstructure behavior of Ti-6Al-4V alloys as a function of the Ti surface (smooth and modified by treatment with double-acid-etching) in simulated body fluid (SBF) with different dextrose (0 mM, 5 mM, 7.5 mM, and 15 mM) and LPS (0 μg/mL, 0.15 μg/mL, 15 μg/mL, and 150 μg/mL) concentrations, used alone or in combination.
The hypothesis was that the Ti-6Al-4V alloy surface treated with double-acid-etching would generate a corrosion pattern different from that observed in the smooth-surface alloy, both in the combination of dextrose and LPS as well as evaluated separately. Additionally, it was hypothesized that the presence of dextrose and LPS would decrease the corrosion resistance of the Ti-6Al-4V alloy.
Materials and Methods
For the electrochemical test, 96 Ti-6Al-4V alloy discs (15 mm in diameter and 2 mm in thickness) were fabricated. The tested surfaces were detailed as below:
1 - Ti-6Al-4V alloy disc with smooth surface, mimicking implants with machined surface (n = 48); and
2 - Ti-6Al-4V alloy disc modified by treatment with double-acid-etching (n = 48).
Disc preparation
The specimens were divided into 32 groups (n = 3) according to type of surface (smooth or etched with acid), dextrose concentration (0 mM, 5 mM, 7.5 mM, and 15 mM) (Sigma Chemical, St. Louis, MO, USA), and LPS concentration (0 μg/mL, 0.15 μg/mL, 15 μg/mL, and 150 μg/mL) (055: B5, Sigma Chemical) (Table 1). The discs were polished and cleaned by standard metallographic methods [23], [25]. Specimens were polished with sequential sandpaper of 320, 400, 600, and 800 grit (Carbimet 2, Buehler, Lake Bluff, IL, USA) in an automatic polisher (ECOMET 250PRO/AUTOMET 250, Buehler). Subsequently, a polishing cloth (TextMet Polishing Cloth, Buehler), diamond paste (MetaDi 9-micron, Buehler), and lubricant (MetaDi Fluid, Buehler) were used.
Table 1. Groups for testing corrosion in SBF as a function of the concentrations of dextrose (DEX), lipopolysaccharide (LPS), and the association of LPS and dextrose (DEXLPS) (n = 3).
| Surface Types of Discs | Dextrose Concentration (mM) | Concentration of LPS (μg/mL) |
| Smooth | ||
| SBF (control) | 0 | 0 |
| DEX5 | 5 | 0 |
| DEX7.5 | 7.5 | 0 |
| DEX15 | 15 | 0 |
| LPS0.15 | 0 | 0.15 |
| LPS15 | 0 | 15 |
| LPS150 | 0 | 150 |
| DEX5 LPS0.15 | 5 | 0.15 |
| DEX5 LPS15 | 5 | 15 |
| DEX5 LPS150 | 5 | 150 |
| DEX7.5 LPS0.15 | 7.5 | 0.15 |
| DEX7.5 LPS15 | 7.5 | 15 |
| DEX7.5 LPS150 | 7.5 | 150 |
| DEX15 LPS0.15 | 15 | 0.15 |
| DEX15 LPS15 | 15 | 15 |
| DEX15 LPS150 | 15 | 150 |
| Double-acid-etching | ||
| SBF (control) | 0 | 0 |
| DEX5 | 5 | 0 |
| DEX7.5 | 7.5 | 0 |
| DEX15 | 15 | 0 |
| LPS0.15 | 0 | 0.15 |
| LPS15 | 0 | 15 |
| LPS150 | 0 | 150 |
| DEX5 LPS0.15 | 5 | 0.15 |
| DEX5 LPS15 | 5 | 15 |
| DEX5 LPS150 | 5 | 150 |
| DEX7.5 LPS0.15 | 7.5 | 0.15 |
| DEX7.5 LPS15 | 7.5 | 15 |
| DEX7.5 LPS150 | 7.5 | 150 |
| DEX15 LPS0.15 | 15 | 0.15 |
| DEX15 LPS15 | 15 | 15 |
| DEX15 LPS150 | 15 | 150 |
Finally, specimens were mirror-finished with polishing cloth (Chemomet I, Buehler) and colloidal silica (MasterMeD, Buehler). The discs were ultrasonically cleaned with deionized water, de-greased with 70% propanol (Sigma Chemical) for 10 min, and dried with hot air at 250°C. The surface roughness of all samples was determined, to provide standardization in the finishes of the Ti-6Al-4V alloy discs [Roughness average (Ra) of 27.64±7.43 nm].
Dextrose at a concentration of 15 mM was selected as equivalent to 270 mg/dL of blood glucose, commonly found in patients with uncontrolled diabetes or in patients with undiagnosed type II diabetes [39]–[41]. Likewise, for the simulation of diabetes in the initial stages, the concentration of 7.5 mM dextrose was used, which corresponds to 135 mg/dL blood glucose. To simulate healthy patients with blood glucose levels within the normal range, the concentration of 5 mM dextrose was used, corresponding to 90 mg/dL blood glucose. Finally, as a control group, a zero concentration of dextrose was used for comparison among groups. The LPS concentrations (0 μg/mL, 0.15 μg/mL, 15 μg/mL, and 150 μg/mL) were used according to previous studies by Barao et al. [23] and Mathew et al. [42], to simulate the infection process.
Discs with smooth surfaces
After the polishing protocol was applied to the Ti-6Al-4V alloy discs, 48 discs were randomly selected for the test corresponding to the smooth surface.
Surface acid modifications
Forty-eight discs were subjected to surface modification according to market availability. To obtain the treated surface, we chemically treated the smooth discs with double-acid-etching (nitric, sulfuric, and hydrochloric acid), according to company proprietary standards (Military Institute of Engineering - IME, Rio de Janeiro, Brazil).
Electrochemical test
The electrochemical test protocol followed that described previously in the literature [23], [25]. The tests were performed in an electrochemical cell made of polysulfone, which has 4 wells with an electrolyte capacity of 10 mL. All measurements were performed by a standardized method of three-cell electrodes according to the instructions of ASTM International [formerly known as the American Society for Testing and Materials (ASTM) (G61-86 and G31-72)]. A saturated calomel electrode (SCE) was used as the reference electrode (RE), a graphite rod as a counter-electrode (CE), and the exposed surface of the Ti-6Al-4V alloy disc as a working electrode (WE, exposed area of the smooth Ti = 1.77 cm2, and Ti treated with double-acid-etching = 2.62 cm2). A potentiostat (Interface 1000, Gamry Instruments, Warminster, PA, USA) connected to a computer was used to perform the corrosion measurements. A 10-mL quantity of electrolyte solution (SBF with or without dextrose and/or LPS) was used for each corrosion experiment [23], [25], [43]. The electrolyte for simulating blood plasma (SBF) has physiologically characteristic temperatures (37°C) and pH (7.4) [44] to mimic certain clinical conditions.
Initially, the Ti-6Al-4V alloy discs were subjected to a cathodic potential (−0.9 V vs. SCE) for 10 min to ensure the standardization of the oxide layer from the surface thereof. The open circuit potential (OCP) was monitored for a period of 3600 s to evaluate the potential of the material before application of the solution and to stabilize the system. Electrochemical impedance spectroscopy (EIS) was used to investigate the formation and growth of the oxide layer on the Ti surface and the properties of this film (corrosion kinetics). EIS, through the electrochemical process, can be represented by an equivalent electric circuit, and the oxide film properties (capacitance and resistance) were quantified to determine the corrosion process and related corrosion kinetics. The EIS measurements were performed at a frequency range of 100 KHz to 5 mHz, with an AC amplitude curve of 10 mV applied to the electrode at its corrosion potential (Ecorr) [23], [25], [42]. These values were used to determine the real (Z′) and imaginary (Z″) components of impedance, which were plotted in the Bode plot or total impedance (|Z|) and phase angle (theta). Finally, the specimens were anodically polarized from −1.2 V to 1.8 V at a scan rate of 2 mV/s.
The corrosion parameters were obtained by means of potentiodynamic polarization curves. Tafel's method was used to estimate the corrosion rate (corrosion current density - Icorr) and the corrosion potential (Ecorr) of the Ti-6Al-4V alloy. The passivation current density (Ipass) was the amount of current density in the transition between the active and passive regions in the polarization curve of the Ti-6Al-4V alloy. The EIS data were used to model the corrosion process (corrosion kinetics) and to describe the properties of the oxide film formed on the surfaces of the Ti-6Al-4V alloy discs. For this, we used Randle's circuit, in which the polarization resistance is in parallel with the capacitance of the double layer while in series with the resistance of solution (Rsol). Based on such a modeling approach, an electrical circuit can be developed equivalent to the electrochemical reactions at the metal-solution interface. Rsol is the uncompensated electrolyte resistance between the reference and working electrodes; Rp is the polarization resistance or the charge transfer resistance at the interface between the working electrode and the electrolyte, in relation to the corrosion rate reactions at the passive field; and Cdl is the specific double-layer capacitance at the working electrode/electrolyte interface. The capacitance is represented by a constant-phase element (CPE) as an alternative to an ideal capacitance element, owing to the inhomogeneous passive layer at the material surface [25]. For the EIS simulation data (double-layer capacitance - Cdl and polarization resistance - Rp), Gamry Echem Analyst software (Gamry Instruments) was used. A chi-square value (goodness of fit) less than 0.001 was considered to indicate an excellent agreement between the experimental data and the fitted values [45].
Surface characterization
The evaluation of the corroded surfaces plays an important role in our understanding of the mechanisms of degradation. Several techniques for surface characterization were used as described below.
Atomic Force Microscopy
The Ti-6Al-4V alloy discs with a smooth surface and surface-treated by acid-etching were analyzed by atomic force microscopy (AFM) (AFM, Veeco Metrology Inc., Santa Barbara, CA, USA). The images were transported from the microscope to a computer, and in the NanoScope Analysis program (2004 Veeco Instruments Inc., Santa Barbara, CA, USA), the images were initially subjected to filters (lowpass and medium). Images in 3 dimensions (3D) were then obtained, and to facilitate a visual comparative analysis among the groups, a standardized scale of the z-axis was used.
Scanning Electron Microscopy and Energy-dispersive Spectroscopy
Scanning electron microscopy (SEM) (JEOL, model JSM-7401F, Portland, OR, USA) was used to characterize possible irregularities on the surfaces of Ti-6Al-4V alloy discs. Comparisons were made between the images obtained from the Ti surfaces by the pre- and post-corrosion analyses of the tested electrolytes.
In addition, elemental chemical analyses were performed in small volumes, in the order of 1 μm3, through the technique of energy-dispersive spectroscopy (EDS) with a spectrometer. This allows for the simultaneous observation of the entire x-ray spectrum, which permits the rapid quantitative analysis (mapping) of the main elements of the Ti surfaces. Comparisons were made of the chemical composition of the different surfaces analyzed prior to and after the corrosion test.
Analysis of surface roughness
The surface roughness (Ra - arithmetical mean surface roughness) of Ti-6Al-4V alloy was investigated before (baseline) and after the corrosion process by means of a profilometer (Dektak 150-d; Veeco, Plainview, NY, USA). Each specimen was individually placed in the center of the equipment, with the measuring tip of the profilometer on the specimen surface. Three measurements were performed at different areas on each disc (0.25 mm cut-off at a speed of 0.05 mm/s), and the mean value was calculated [46].
Microhardness analysis
The microhardness of the Ti-6Al-4V alloy discs was verified at baseline (before corrosion tests) and after the corrosion tests by means of a microhardness tester (Shimadzu HMV-2000 Micro Hardness Tester, Shimadzu Corporation, Kyoto, Japan). This measurement was performed at room temperature (22±2°C). The applied load was 500 gf for 15 s, and the microhardness was expressed in units of Vickers Hardness (VHN) [47], [48]. The values of Vickers hardness were calculated according to the following formula: VHN 2P = sin (136°/2)/d2, where P = applied load and d = length of the diagonals of indentations. The test was repeated 4 times in 4 randomly distributed points on the surface of each disc. The average of these 4 replicates corresponded to the value of the Vickers microhardness.
Statistical Analysis
Pearson's correlations were used to identify the relationships between the corrosion parameters (Ecorr, Icorr, Ipass, Cdl, and Rp) and the concentrations of LPS or dextrose (used alone or combined). Correlations of roughness and microhardness vs concentrations of LPS or dextrose (used alone or combined) were also investigated.
The independent t-test was used to compare the two Ti surface conditions (smooth or treated with double-acid-etching) for all parameters described above. All tests were conducted with a significance level of 5% (SPSS version 17.0 - Statistical Package for the Social Sciences, Inc., Chicago, IL, USA).
In this study, 3 specimens were used per group, with a power effect of 0.873 (Cohen effect size statistics).
Results
Electrochemical data
The cyclic potentiodynamic polarization curves, the electrochemical data, and EIS can be seen in Figs. 1 to 5. Regions of active-passive transition were observed in the cyclic polarization curves of the Ti-6Al-4V alloys in the control group (SBF) and for all tested groups (Fig 1). A typical passive plateau, which is common in the case of Ti, was evident with both surfaces (smooth and acid). The formation of negative hysteresis was obvious in the curves, as indicated by arrows, which enables us to state that the passive layer formed is strong and uniform, and that Ti in the presence of dextrose and/or LPS is not susceptible to corrosion by pits or cracks.
Figure 1. Representative cyclic potentiodynamic polarization curve of Ti-6Al-4V alloy.
Tests were conducted in simulated body fluid - SBF (control) with different concentrations of dextrose (DEX), lipopolysaccharide (LPS), and combinations of dextrose and lipopolysaccharide (DEXLPS).
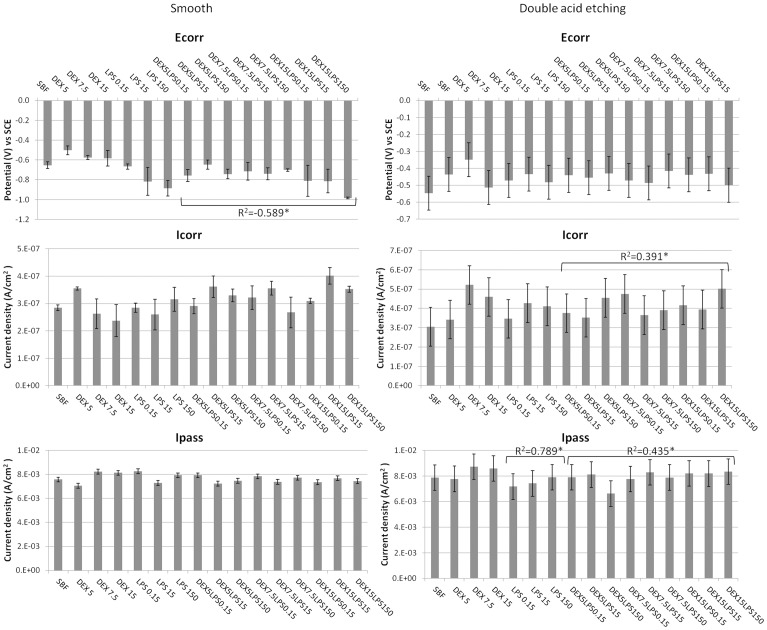
Figure 5. Electrochemical data from the EIS test.
Means and standard deviations of polarization resistance (Rp) and capacitance (Cdl) for the Ti-6Al-4V alloys with a smooth surface and etched with acid in SBF with different concentrations of dextrose (DEX) and lipopolysaccharide (LPS), alone or in combination (DEXLPS). * Denotes significant correlation at the 0.05 level.
For the Ti-6Al-4V alloy with the smooth surface, only the association with dextrose and LPS (DEXLPS) was significantly correlated with some parameter of corrosion. A negative correlation with Ecorr was noted (R2 = -0.589, p<0.001) (Table 2). For the Ti-6Al-4V alloy surface conditioned with double-acid-etching, the presence of dextrose was significantly correlated with Rp (R2 = 0.960, p<0.01) (Table 2). The LPS was correlated with the Ipass (R2 = 0.789, p = 0.011), Cdl (R2 = 0.808, p = 0.008), and Rp (R2 = -0.931, p<0.01) (Table 2). The combination of dextrose and LPS was correlated with Icorr (R2 = 0.391, p = 0.044) and Ipass (R2 = 0.435, p = 0.023) (Table 2).
Table 2. Correlations between parameters of corrosion, roughness, and hardness with concentrations of dextrose (DEX) and lipopolysaccharide (LPS) (used alone or together) for Ti-6Al-4V alloys with smooth surfaces and conditioned with double-acid-etching.
| Smooth | Double-acid-etching | |||||||||||
| Dextrose | LPS | Dextrose+LPS | Dextrose | LPS | Dextrose+LPS | |||||||
| variable | R2 | P | R2 | P | R2 | P | R2 | P | R2 | P | R2 | P |
| Ecorr | −0.479 | 0.192 | −0.615 | 0.078 | −0.589* | 0.001 | 0.639 | 0.064 | −0.246 | 0.523 | −0.121 | 0.547 |
| Icorr | −0.664 | 0.051 | 0.469 | 0.203 | 0.250 | 0.208 | 0.382 | 0.311 | 0.347 | 0.361 | 0.391* | 0.044 |
| Ipass | 0.534 | 0.139 | 0.069 | 0.860 | −0.134 | 0.504 | 0.500 | 0.170 | 0.789* | 0.011 | 0.435* | 0.023 |
| Cdl | 0.070 | 0.858 | 0.477 | 0.194 | 0.008 | 0.967 | −0.172 | 0.658 | 0.808* | 0.008 | 0.104 | 0.605 |
| Rp | −0.557 | 0.119 | 0.224 | 0.562 | 0.217 | 0.277 | 0.960* | 0.0001 | −0.931* | 0.0001 | 0.259 | 0.193 |
| Roughness | 0.0001 | 1.000 | 0.105 | 0.788 | 0.726* | 0.0001 | −0.326 | 0.392 | 0.601 | 0.087 | 0.405* | 0.036 |
| Microhardness | −0.551 | 0.124 | 0.218 | 0.573 | −0.915* | 0.0001 | −0.342 | 0.368 | 0.175 | 0.653 | 0.781* | 0.0001 |
* Correlation is significant at the 0.05 level (2-tailed).
The double-acid-etching surface treatment significantly increased the Icorr values for most groups (p<0.05, t-test) (Table 3, Fig 2). The passivation of the groups treated with double-acid-etching tended to be delayed, a fact evidenced by the values of Ipass. Conversely, the Ecorr values were lower for the Ti-6Al-4V alloys with the smooth surface (Table 3, Fig 2).
Table 3. Comparisons (independent t-test) between the Ti-6Al-4V alloys with smooth surfaces and double-acid-etching parameters for corrosion, roughness, and microhardness.
| Variables | |||||||
| Groups | Ecorr | Icorr | Ipass | Cdl | Rp | Roughness | Microhardness |
| Baseline | - | - | - | - | - | 0.015* | 0.127 |
| SBF (control) | 0.008* | 0.123 | 0.040* | 0.0001* | 0.0001* | 0.0001* | 0.168 |
| DEX5 | 0.083 | 0.161 | 0.105 | 0.0001* | 0.0001* | 0.002* | 0.070 |
| DEX7.5 | 0.002* | 0.004 | 0.162 | 0.0001* | 0.0001* | 0.001* | 0.0001* |
| DEX15 | 0.221 | 0.003* | 0.186 | 0.0001* | 0.0001* | 0.0001* | 0.005* |
| LPS0.15 | 0.019* | 0.022* | 0.024* | 0.0001* | 0.565 | 0.0001* | 0.042* |
| LPS15 | 0.010* | 0.012* | 0.677 | 0.0001* | 0.009* | 0.0001* | 0.259 |
| LPS150 | 0.001* | 0.027* | 0.897 | 0.0001* | 0.0001* | 0.0001* | 0.093 |
| DEX5 LPS0.15 | 0.001* | 0.008* | 0.908 | 0.0001* | 0.0001* | 0.008* | 0.747 |
| DEX5 LPS15 | 0.003* | 0.776 | 0.010* | 0.0001* | 0.003* | 0.001* | 0.391 |
| DEX5 LPS150 | 0.002* | 0.002* | 0.001* | 0.0001* | 0.006* | 0.0001* | 0.161 |
| DEX7.5 LPS0.15 | 0.014* | 0.004* | 0.652 | 0.001* | 0.007* | 0.0001* | 0.023* |
| DEX7.5 LPS15 | 0.003* | 0.726 | 0.029* | 0.0001* | 0.098 | 0.001* | 0.0001* |
| DEX7.5 LPS150 | 0.003* | 0.019* | 0.215 | 0.0001* | 0.001* | 0.0001* | 0.001* |
| DEX15 LPS0.15 | 0.015* | 0.001* | 0.009* | 0.0001* | 0.0001* | 0.0001* | 0.0001* |
| DEX15 LPS15 | 0.006* | 0.725 | 0.010 | 0.0001* | 0.006* | 0.0001* | 0.0001* |
| DEX15 LPS150 | 0.0001* | 0.0001* | 0.007* | 0.0001* | 0.009* | 0.0001* | 0.0001* |
* Significant at the 0.05 level (independent t-–test).
Figure 2. Electrochemical data of cyclic potentiodynamic polarization curve.
Mean and standard deviation of corrosion potential (Ecorr), corrosion current density (Icorr), and the passivation current density (Ipass) for the Ti-6Al-4V alloys with a smooth surface and etched with acid, in SBF with different concentrations of dextrose (DEX) and lipopolysaccharide (LPS), alone or in combination (DEXLPS). * Denotes significant correlation at the 0.05 level.
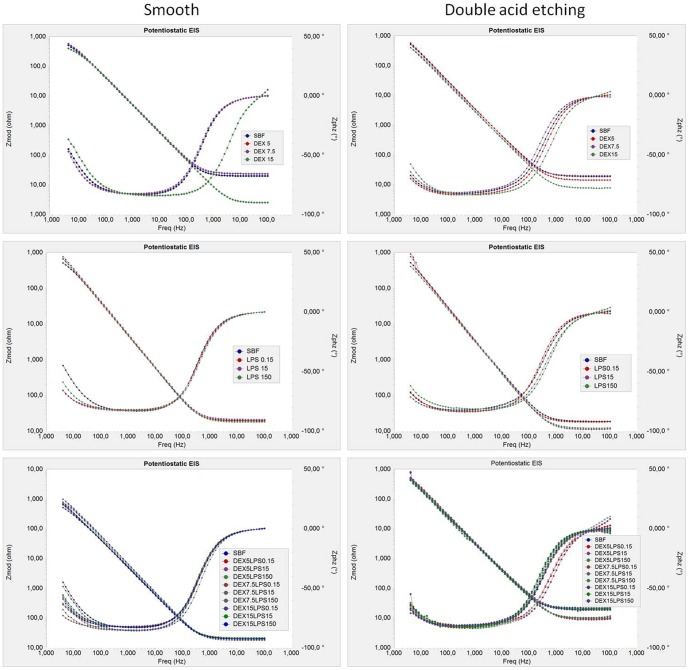
The kinetics of corrosion and passive film formation was demonstrated through the Bode plot (impedance IZI vs frequency; and phase angle vs frequency) (Fig 3). In the phase angle, only a time constant was observed for all groups, which indicates the formation of a compact Ti oxide film, homogeneous and a shield to the metal surface. In high and low frequencies, the overall impedance values were lower in the presence of 15 mM dextrose, for both the smooth-surface acid-treated Ti-6Al-4V alloys. In general, the Nyquist plot (Zimg vs Zreal) (Fig 4) showed that the dextrose and LPS alone or combined decreased the semicircular diameter of the capacitance loop for both Ti-6Al-4V alloy surfaces compared with the control group (SBF). This suggests a lower corrosion resistance of the Ti in these situations. LPS increased the semicircular diameter of the capacitance loop of the smooth Ti-6Al-4V alloy (Fig 4).
Figure 3. Electrochemical impedance spectroscopy (EIS) represented by the Bode plot of the Ti-6Al-4V alloy.
Tests were conducted in simulated body fluid - SBF (control) with different concentrations of dextrose (DEX), lipopolysaccharide (LPS), and combinations of dextrose and lipopolysaccharide (DEXLPS).
Figure 4. Electrochemical impedance spectroscopy (EIS) represented by the Nyquist plot of the Ti-6Al-4V alloy.
Tests were conducted in simulated body fluid - SBF (control) with different concentrations of dextrose (DEX), lipopolysaccharide (LPS), and combinations of dextrose and lipopolysaccharide (DEXLPS).
The type of Ti-6Al-4V alloy surface exerted a strong influence on the corrosion kinetics, as observed in the values of Cdl and Rp. The groups treated with double-acid-etching showed a significant increase in Cdl values and reduced values of Rp (p<0.05, t-test), except for the control group and the dextrose groups, in which the smooth surface produced greater Rp values (Table 3, Fig 5).
Topographic data
The average surface roughness (Ra) and microhardness values are shown in Fig 6. Only the association of dextrose and LPS showed a correlation with the topographic data for both types of Ti-6Al-4V alloy surfaces. A positive correlation with the Ra parameter was noted (R2 = 0.726, p<0.0001 for the smooth Ti; R2 = 0.405, p = 0.036 for the acid Ti). There was a negative correlation for the microhardness data (R2 = −0.915, p<0.0001) in the smooth Ti, while for the Ti with double-acid-etching, a positive correlation was noted (R2 = 0.781, p<0.0001).
Figure 6. Data on surface topography.
Means and standard deviations of surface roughness (Ra) (in nm) and Vickers microhardness for the Ti-6Al-4V alloys with a smooth surface and those etched with acid in SBF with different concentrations of dextrose (DEX) and lipopolysaccharide (LPS), alone or in combination (DEXLPS). * Denotes significant correlation at the 0.05 level.
When the two surface conditions of the Ti-6Al-4V alloy are compared, it can be noted that the double-acid-etching treatment resulted in a significant increase (p<0.05, t-test) in the surface roughness of the material for all groups (Table 3, Fig 6). Overall, the Ti-6Al-4V alloy with a smooth surface showed lower microhardness values when compared with the Ti-6Al-4V surface treated by double-acid-etching (Table 3, Fig 6).
The SEM images of the Ti-6Al-4V alloy with a smooth surface showed no changes in the microstructure of the Ti, except in the dextrose group (at a concentration of 15 mM) associated with LPS (concentrations of 15 and 150 μg/mL), which presented inlays, probably due to the substrates used (dextrose and/or LPS) (Fig 7). For the Ti-6Al-4V alloy treated with double-acid-etching, the comparison between the alloys at baseline and after the corrosion test did not show any change among the groups tested (Fig 8). The smooth Ti-6Al-4V alloy possessed a smooth and fairly flat surface (magnifications of 300× and 10,000×). The white spots identified mainly at the 10,000× magnification are due to the presence of aluminum in the Ti-6Al-4V alloy, confirmed by EDS (Fig 9). The Ti surface treated with acid showed striations on the entire surface, with rough microstructure quite evident. EDS analysis of the elementary chemical composition of the Ti-6Al-4V alloy, in two stages of the experiment (baseline and after the corrosion test), showed no change in the constituents of the Ti-6Al-4V alloy (Fig 9).
Figure 7. Scanning electron microscope images (300× and 10,000×) of the Ti-6Al-4V alloy with smooth surface,
showing the Ti-6Al-4V alloy surface before and after corrosion in SBF (control - Co) with different concentrations of dextrose (DEX) and lipopolysaccharide (LPS), alone or in combination (DEXLPS). WD = 8 mm; 15 Kv.
Figure 8. Scanning electron microscope images (300× and 10,000×) of the Ti-6Al-4V alloy with acid-etched surface,
showing the Ti-6Al-4V alloy surface before and after corrosion in SBF (control - Co) with different concentrations of dextrose (DEX) and lipopolysaccharide (LPS), alone or in combination (DEXLPS). WD = 8 mm; 15 Kv.
Figure 9. Representative energy-dispersive spectroscopy (EDS).
(a) Ti-6Al-4V alloy with smooth surface before corrosion test. (b) Ti-6Al-4V alloy with smooth surface after the corrosion test. (c) Ti-6Al-4V with acid-etched surface before the corrosion test. (d) Ti-6Al-4V with acid-etched surface after the corrosion test.
AFM analysis of the three-dimensional surface of the Ti-6Al-4V alloy demonstrated superficial changes in the material after the corrosion test for both the smooth-surface discs and those conditioned by acid. A greater apparent oxide thickness in the groups associated with dextrose and LPS (DEXLPS) was noted (Figs 10, 11).
Figure 10. 3D AFM images of a Ti-6Al-4V alloy with a smooth surface.
Surfaces were characterized before (baseline) and after corrosion in SBF (control) with different concentrations of dextrose (DEX) and lipopolysaccharide (LPS), alone or in combination (DEXLPS).
Figure 11. 3D AFM images of the Ti-6Al-4V alloy with an acid-etched surface.
Surfaces were characterized before (baseline) and after corrosion in SBF (control) with different concentrations of dextrose (DEX) and lipopolysaccharide (LPS), alone or in association (DEXLPS).
Discussion
The research hypotheses – that (1) the Ti-6Al-4V alloy with the surface treated with double-acid-etching generates a corrosion pattern different from that observed in the smooth surface, and that (2) the presence of LPS and dextrose decreases the corrosion resistance of the Ti-6Al-4V alloy – were partially accepted. The combination of dextrose and LPS negatively affected the electrochemical stability of the Ti-6Al-4V alloy treated with double-acid-etching. Dextrose alone did not impair the corrosion behavior of Ti-6Al-4V alloy for both surface conditions. The Ti-6Al-4V alloy with surface modification by acid etching showed a higher tendency toward corrosion.
Corrosion behavior
In spite of the results obtained by the parameters of corrosion, a significant decrease (more electronegative) in the corrosion potential Ecorr (p<0.01) was noticed on the smooth Ti-6Al-4V alloy when exposed to dextrose and LPS (DEX-LPS). The higher the concentration of the combined DEX-LPS, the lower the corrosion potential of the smooth Ti. The reduced values (more electronegative) of Ecorr suggest that the smooth Ti provides a less stable surface [21], [22] that may be a result of decreased surface passivity. A previous study related the passivity to the thickening of the oxide/hydroxide layer in the titanium/electrolyte interface [21]. The isolated presence of dextrose and LPS alone had no correlation with the Ecorr values of the smooth Ti-6Al-4V alloy at any of the concentrations tested (p>0.05).
Messer et al. [22] evaluated the electrochemical behavior of commercially pure Ti implants (cpTi) in inflammatory and hyperglycemic conditions. The corrosion potential shifted to noble values at high concentrations of dextrose (15 mM) at the same concentration used in this study, as a function of monocyte cultures and blood cells. However, no change in the corrosion rate was found when phosphate-buffered saline (PBS) was used as the medium. Hence it is believed that such inconsistency occurred due to the differences in the electrolyte used. Messer et al. used cultured blood cells and PBS. In the present study, SBF was used, and this medium has a composition similar to that of blood plasma, which may simulate a real clinical situation. Additionally, our tests were conducted over a short term, and Ti-6Al-4V was used instead of cpTi.
The addition of dextrose to the SBF tended to reduce the Rp values for smooth and acid Ti samples. However, the concentration of dextrose was positively correlated to the Rp in the Ti-6Al-4V alloy treated with double-acid-etching (p<0.01). This indicates that the resistance of the material increased with increasing concentrations of dextrose, showing similar Rp values at 15 mM of dextrose concentration when compared with SBF (control), thus protecting the surface of the material. It is believed that the saccharides and proteins on dental implant surfaces can enhance the corrosion resistance of the Ti in accordance with the binding affinity to the specific proteins and cause the release of metal ions from the surface of the material to the peri-implant region [21], [22]. However, the interaction of the metals and proteins, blood cells, and their products to promote corrosion depends on several factors, such as roughness, surface charge, material composition, and the affinity agent molecules of the metal [49], and may even protect the surface of the Ti by protein absorption through the electrolyte [21].
It was noted that the values of capacitance increased and the resistance values decreased with the increased concentration of LPS for Ti-6Al-4V alloys treated with acid (negative action of the LPS on the corrosion kinetics of the acid Ti). Furthermore, there was delayed passivation with the increasing concentration of LPS, due to a positive correlation for the Ipass. Dextrose alone did not cause any effect on the corrosive properties of the Ti-6Al-4V alloy. In contrast, when dextrose was added to LPS (DEXLPS), there was an increase in the rate of corrosion current and less potential for passivation of Ti, confirming the deleterious effect of the LPS on the surface of Ti with acid treatment.
In this context, the action of LPS on the corrosion [23] and tribocorrosion [42] behavior of the Ti was evaluated in vitro. These authors stated that the polysaccharide portion of the LPS can induce the release of Ti ions, proven by the corrosion kinetics, through the values of Cdl and Rp. This probably is due to a greater surface area for electrochemical reactions in the Ti-6Al-4V alloy treated with double-acid-etching. The results of this present study contradict those obtained by Messer et al. [21], who evaluated the Ti surface modified with oxide and phosphate and observed lower corrosion rates due to inflammatory and hyperglycemic conditions (concentration = 1 μg/mL of LPS). It is believed that the concentration of LPS used in the Messer study [21], in simulating the inflammatory effects, was not able to affect the corrosive properties of the Ti. Herein, the concentrations of LPS (15 and 150 μg/mL) mimicked infections, and undoubtedly could cause more harmful effects on the Ti surface. In addition, because the smooth surface had a smaller contact area with the LPS, there was less connection with the polysaccharide portion of the Ti surface. This may have been responsible for the increased Rp values observed on the smooth Ti surface.
The use of LPS at concentrations that mimic infection with the smooth cpTi surface has been verified previously [23]. It was observed that increasing the concentration of LPS caused a significant increase in the rate of corrosion of the cpTi in artificial saliva. This inconsistency with the present study is mainly because simulated body fluid was used as an electrolyte, and the material tested was the Ti-6Al-4V alloy. Therefore, it is clear that the corrosion behavior of the Ti is dependent on the electrolyte and, to a certain extent, on its composition.
Surface Topography
Reports in the literature agree that the corrosion process can increase the surface roughness of Ti [20], [42], [50]. Changes in Ti roughness may imply greater adherence of microorganisms [51]. Additionally, Barao et al. [52] inferred that the corrosion process increased the attachment of P. gingivalis on Ti substrata, increasing the tendency for peri-implantitis [53] and failure of the Ti implant. These findings are in agreement with the results from the current study with respect to the roughness values. In the smooth and treated Ti surfaces, there was a strong positive correlation for the combination of dextrose and LPS (DEXLPS), corroborating the parameters of corrosion.
The increase in Ra values with dextrose and LPS were visually confirmed by the 3D AFM images. This was especially observed in the smooth Ti-6Al-4V alloy by increases in the apparent oxide thickness. SEM images did not show great changes on the Ti-6Al-4V surfaces. Faverani et al. [46] showed that only substantial deterioration can be evidenced on the Ti-6Al-4V alloy surface. Yet, changes in the microstructure of the Ti-6Al-4V alloy in combination with dextrose and LPS were probably due to the impregnation of the substrates used herein.
Analysis of the microhardness data showed a strong negative correlation for the smooth Ti-6Al-4V alloy and a positive correlation for the Ti-6Al-4V alloy treated with acid, in the presence of dextrose combined with LPS. Yang et al. [54] also observed an increase in the microhardness of cpTi with surface treatment when compared with the smooth Ti. The lattice deformation and the solution hardening during surface treatment may be the driving force in such data [55]. Clinically, the surface hardening may be endorsed for load-bearing implants and dental implants [54]. There is still no scientific support to explain why the combination of dextrose and LPS during corrosion increased the surface hardness of the surface-treated group. Therefore, further studies should focus on this topic. It is important to highlight that the greater addition of sugars (i.e., dextrose) and LPS certainly raises the failure rates of dental implants [20], [51], [53] in the clinical setting.
Clinical Implications
The in vitro simulations of this study showed that patients with a combination of hyperglycemia and infections might be more prone to experience implant failure, due to the reduced electrochemical stability of the Ti-6Al-4V alloy. It is noteworthy that it is not only diabetes entails hyperglycemia. Other systemic disorders also cause elevation of blood glucose levels, such as pancreatitis [56], [57], pancreatic cancer [57]–[59], Addison's disease, Cushing's syndrome, and other alterations of the adrenal glands [60]–[62]. Thus, it can be inferred that the blood glucose levels of patients undergoing dental implant procedures should be within normal limits. Furthermore, in view of the increased surface roughness and higher Rp values for the ‘isolated dextrose’ group, the hyperglycemic individuals must have good oral hygiene to reduce local biofilm accumulation.
Limitations and future studies
In this study, the static effects of dextrose, LPS, and the combination of dextrose and LPS in simulated body fluid were investigated. However, it is known that the peri-implant environment is constantly subjected to the action of mechanical oscillations, especially during masticatory load [63], [64]. Thus, as suggested by Mathew et al. [42], future studies evaluating the linking of corrosion and wear (tribocorrosion) are warranted.
Moreover, the occurrence of peri-implantitis, bacteremia, or hyperglycemia in individuals with diabetes may be long-lasting; however, our electrochemical tests were carried out over the short term. Further studies to evaluate the effects of these conditions in the long term (for example, 24 and 48 h after immersion) should be performed.
Conclusions
The combination of dextrose and LPS has a slight influence on the corrosion current density of the Ti-6Al-4V alloy treated with double-acid-etching. However, no dose-response in the corrosion behavior of the Ti-6Al-4V alloy could be observed. The capacitance of the double layer increased with the increased LPS concentration. These results suggest a greater susceptibility of Ti implant corrosion in diabetic patients with associated infections.
Acknowledgments
The authors express their gratitude to the Laboratory of Plasma Technology, especially to Prof. Dr. Nilson Cruz, Sorocaba School of Engineering – Univ. Estadual Paulista (UNESP), for facilitating profilometry; to The Emfils Company, particularly Dr. Fabio Embacher, for providing the Ti-6Al-4V alloy discs; and to Professor Dr. Carlos Nelson Elias of the Military Institute of Engineering, Rio de Janeiro, for performing surface modification on the discs.
Funding Statement
The authors would like to thank Sao Paulo State Research Foundation (FAPESP) for the financial support (#2012/14282-5 and #2011/20021-7). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Udupa A, Nahar P, Shah S, Kshirsagar M, Ghongane B (2013) A comparative study of effects of Omega-3 fatty acids, alpha lipoic acid and vitamin E in Type 2 diabetes mellitus. Ann Med Health Sci Res 3: 442–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. DPTT study group, Engebretson S, Gelato M, Hyman L, Michalowicz BS, et al (2013) Design features of the Diabetes and Periodontal Therapy Trial (DPTT): A multicenter randomized single-masked clinical trial testing the effect of nonsurgical periodontal therapy on glycosylated hemoglobin (HbA1c) levels in subjects with type 2 diabetes and chronic periodontitis. Contemp Clin Trials 36: 515–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Akca K, Sarac E, Baysal U, Fanuscu M, Chang TL, et al. (2007) Micro-morphologic changes around biophysically-stimulated titanium implants in ovariectomized rats. Head Face Med 3: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nelson RG, Shlossman M, Budding LM, Pettitt DJ, Saad MF, et al. (1990) Periodontal disease and NIDDM in Pima Indians. Diabetes Care 13: 836–840. [DOI] [PubMed] [Google Scholar]
- 5. Oates TW, Huynh-Ba G, Vargas A, Alexander P, Feine J (2013) A critical review of diabetes, glycemic control, and dental implant therapy. Clin Oral Implants Res 24: 117–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Manfredi M, McCullough MJ, Vescovi P, Al-Kaarawi ZM, Porter SR (2004) Update on diabetes mellitus and related oral diseases. Oral Dis 10: 187–200. [DOI] [PubMed] [Google Scholar]
- 7. Skamagas M, Breen TL, LeRoith D (2008) Update on diabetes mellitus: prevention, treatment, and association with oral diseases. Oral Dis 14: 105–114. [DOI] [PubMed] [Google Scholar]
- 8. Deshpande K, Jain A, Sharma R, Prashar S, Jain R (2010) Diabetes and periodontitis. J Indian Soc Periodontol 14: 207–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Darnell JA, Saunders MJ (1990) Oral manifestations of the diabetic patient. Tex Dent J 107: 23–27. [PubMed] [Google Scholar]
- 10. Lamey PJ, Darwazeh AM, Frier BM (1992) Oral disorders associated with diabetes mellitus. Diabet Med 9: 410–416. [DOI] [PubMed] [Google Scholar]
- 11. George K, Zafiropoulos GG, Murat Y, Hubertus S, Nisengard RJ (1994) Clinical and microbiological status of osseointegrated implants. J Periodontol 65: 766–770. [DOI] [PubMed] [Google Scholar]
- 12. Knoernschild KL, Bacon WL, Fischman GS, Campbell SD (2001) Effect of pH on endotoxin affinity for metal-ceramic alloys. J Prosthet Dent 86: 644–649. [DOI] [PubMed] [Google Scholar]
- 13. Knoernschild KL, Tompkins GR, Lefebvre CA, Griffiths LL, Schuster GS (1996) Effect of pH on Porphyromonas gingivalis endotoxin affinity for resins. Int J Prosthodont 9: 239–247. [PubMed] [Google Scholar]
- 14. Nelson KE, Fleischmann RD, DeBoy RT, Paulsen IT, Fouts DE, et al. (2003) Complete genome sequence of the oral pathogenic bacterium Porphyromonas gingivalis strain W83. J Bacteriol 185: 5591–5601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Robinson FG, Knoernschild KL, Sterrett JD, Tompkins GR (1996) Porphyromonas gingivalis endotoxin affinity for dental ceramics. J Prosthet Dent 75: 217–227. [DOI] [PubMed] [Google Scholar]
- 16. Cortada M, Giner L, Costa S, Gil FJ, Rodriguez D, et al. (2000) Galvanic corrosion behavior of titanium implants coupled to dental alloys. J Mater Sci Mater Med 11: 287–293. [DOI] [PubMed] [Google Scholar]
- 17. Vieira AC, Ribeiro AR, Rocha LA, Celis JP (2006) Influence of pH and corrosion inhibitors on the tribocorrosion of titanium in artificial saliva. Wear 261: 994–1001. [Google Scholar]
- 18. Nikolopoulou F (2006) Saliva and dental implants. Implant Dent 15: 372–376. [DOI] [PubMed] [Google Scholar]
- 19. Chaturvedi TP (2009) An overview of the corrosion aspect of dental implants (titanium and its alloys). Indian J Dent Res 20: 91–98. [DOI] [PubMed] [Google Scholar]
- 20. Correa CB, Pires JR, Fernandes-Filho RB, Sartori R, Vaz LG (2009) Fatigue and fluoride corrosion on Streptococcus mutans adherence to titanium-based implant/component surfaces. J Prosthodont 18: 382–387. [DOI] [PubMed] [Google Scholar]
- 21. Messer RL, Seta F, Mickalonis J, Brown Y, Lewis JB, et al. (2010) Corrosion of phosphate-enriched titanium oxide surface dental implants (TiUnite) under in vitro inflammatory and hyperglycemic conditions. J Biomed Mater Res B Appl Biomater 92: 525–534. [DOI] [PubMed] [Google Scholar]
- 22. Messer RL, Tackas G, Mickalonis J, Brown Y, Lewis JB, et al. (2009) Corrosion of machined titanium dental implants under inflammatory conditions. J Biomed Mater Res B Appl Biomater 88: 474–481. [DOI] [PubMed] [Google Scholar]
- 23. Barao VA, Mathew MT, Assuncao WG, Yuan JC, Wimmer MA, et al. (2011) The role of lipopolysaccharide on the electrochemical behavior of titanium. J Dent Res 90: 613–618. [DOI] [PubMed] [Google Scholar]
- 24. Gittens RA, Olivares-Navarrete R, Tannenbaum R, Boyan BD, Schwartz Z (2011) Electrical implications of corrosion for osseointegration of titanium implants. J Dent Res 90: 1389–1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Barao VA, Mathew MT, Assuncao WG, Yuan JC, Wimmer MA, et al. (2012) Stability of cp-Ti and Ti-6Al-4V alloy for dental implants as a function of saliva pH – an electrochemical study. Clin Oral Implants Res 23: 1055–1062. [DOI] [PubMed] [Google Scholar]
- 26. Zhoua LY, Mitsuo N, Toshikazu A, Hisao F, Todaa H (2007) Corrosion resistance and biocompatibility of Ti-Ta alloys for biomedical applications. Materials 48: 380–384. [Google Scholar]
- 27. Oliveira NT, Guastaldi AC (2009) Electrochemical stability and corrosion resistance of Ti-Mo alloys for biomedical applications. Acta Biomater 5: 399–405. [DOI] [PubMed] [Google Scholar]
- 28. Mareci D, Chelariu R, Gordin DM, Ungureanu G, Gloriant T (2009) Comparative corrosion study of Ti-Ta alloys for dental applications. Acta Biomater 5: 3625–3639. [DOI] [PubMed] [Google Scholar]
- 29. Olmedo DG, Paparella ML, Brandizzi D, Cabrini RL (2010) Reactive lesions of peri-implant mucosa associated with titanium dental implants: a report of 2 cases. Int J Oral Maxillofac Surg 39: 503–507. [DOI] [PubMed] [Google Scholar]
- 30. Olmedo DG, Paparella ML, Spielberg M, Brandizzi D, Guglielmotti MB, et al. (2012) Oral mucosa tissue response to titanium cover screws. J Periodontol 83: 973–980. [DOI] [PubMed] [Google Scholar]
- 31. Trisi P, Lazzara R, Rebaudi A, Rao W, Testori T, et al. (2003) Bone-implant contact on machined and dual acid-etched surfaces after 2 months of healing in the human maxilla. J Periodontol 74: 945–956. [DOI] [PubMed] [Google Scholar]
- 32. Xavier SP, Carvalho PS, Beloti MM, Rosa AL (2003) Response of rat bone marrow cells to commercially pure titanium submitted to different surface treatments. J Dent 31: 173–180. [DOI] [PubMed] [Google Scholar]
- 33. Buser D, Broggini N, Wieland M, Schenk RK, Denzer AJ, et al. (2004) Enhanced bone apposition to a chemically modified SLA titanium surface. J Dent Res 83: 529–533. [DOI] [PubMed] [Google Scholar]
- 34. Tavares MG, de Oliveira PT, Nanci A, Hawthorne AC, Rosa AL, et al. (2007) Treatment of a commercial, machined surface titanium implant with H2SO4/H2O2 enhances contact osteogenesis. Clin Oral Implants Res 18: 452–458. [DOI] [PubMed] [Google Scholar]
- 35. Pai PS, Mathew MT, Stack MM, Rocha LA (2008) Some thoughts on neural network modelling of microabrasion-corrosion processes. Tribology International 41: 672–681. [Google Scholar]
- 36. Lin A, Wang CJ, Kelly J, Gubbi P, Nishimura I (2009) The role of titanium implant surface modification with hydroxyapatite nanoparticles in progressive early bone-implant fixation in vivo. Int J Oral Maxillofac Implants 24: 808–816. [PubMed] [Google Scholar]
- 37. Wennerberg A, Albrektsson T (2009) Effects of titanium surface topography on bone integration: a systematic review. Clin Oral Implants Res 20 Suppl 4 172–184. [DOI] [PubMed] [Google Scholar]
- 38. Gotfredsen K, Berglundh T, Lindhe J (2001) Bone reactions adjacent to titanium implants subjected to static load of different duration. A study in the dog (III). Clin Oral Implants Res 12: 552–558. [DOI] [PubMed] [Google Scholar]
- 39. Klokkevold PR, Han TJ (2007) How do smoking, diabetes, and periodontitis affect outcomes of implant treatment? Int J Oral Maxillofac Implants 22 Suppl: 173–202. [PubMed] [Google Scholar]
- 40. Tawil G, Younan R, Azar P, Sleilati G (2008) Conventional and advanced implant treatment in the type II diabetic patient: surgical protocol and long-term clinical results. Int J Oral Maxillofac Implants 23: 744–752. [PubMed] [Google Scholar]
- 41.Tamam E, Turkyilmaz I (2012) Effects of pH and elevated glucose levels on the electrochemical behaviour of dental implants. J Oral Implantol In-Press. doi: http://dx.doi.org/10.1563/AAID-JOI-D-11-00083.1. [DOI] [PubMed]
- 42. Mathew MT, Barao VA, Yuan JC, Assuncao WG, Sukotjo C, et al. (2012) What is the role of lipopolysaccharide on the tribocorrosive behavior of titanium? J Mech Behav Biomed Mater 8: 71–85. [DOI] [PubMed] [Google Scholar]
- 43. Barao VA, Mathew MT, Yuan JC, Knoernschild KL, Assuncao WG, et al. (2013) Influence of corrosion on lipopolysaccharide affinity for two different titanium materials. J Prosthet Dent 110: 462–470. [DOI] [PubMed] [Google Scholar]
- 44. Abe Y, Kokubo T, Yamamuro T (1990) Apatite coating on ceramics, metals and polymers utilizing a biological process. J Mater Sci Mater Med 1: 233–238. [Google Scholar]
- 45. Zhang SM, Qiu J, Tian F, Guo XK, Zhang FQ, et al. (2013) Corrosion behavior of pure titanium in the presence of Actinomyces naeslundii . J Mater Sci Mater Med 24: 1229–1237. [DOI] [PubMed] [Google Scholar]
- 46. Faverani LP, Barao VA, Ramalho-Ferreira G, Ferreira MB, Garcia-Junior IR, et al. (2014) Effect of bleaching agents and soft drink on titanium surface topography. J Biomed Mater Res B Appl Biomater 102: 22–30. [DOI] [PubMed] [Google Scholar]
- 47. Al Jabbari Y, Fournelle R, Ziebert G, Toth J, Iacopino A (2008) Mechanical behavior and failure analysis of prosthetic retaining screws after long-term use in vivo. Part 2: Metallurgical and microhardness analysis. J Prosthodont 17: 181–191. [DOI] [PubMed] [Google Scholar]
- 48. Assuncao WG, Jorge JR, Dos Santos PH, Barao VA, Gomes EA, et al. (2011) The effect of mechanical cycling and different misfit levels on Vicker's [sic] microhardness of retention screws for single implant-supported prostheses. J Prosthodont 20: 523–527. [DOI] [PubMed] [Google Scholar]
- 49. Bundy KJ (1994) Corrosion and other electrochemical aspects of biomaterials. Crit Rev Biomed Eng 22: 139–251. [PubMed] [Google Scholar]
- 50. Mabilleau G, Bourdon S, Joly-Guillou ML, Filmon R, Basle MF, et al. (2006) Influence of fluoride, hydrogen peroxide and lactic acid on the corrosion resistance of commercially pure titanium. Acta Biomater 2: 121–129. [DOI] [PubMed] [Google Scholar]
- 51. Morgan TD, Wilson M (2001) The effects of surface roughness and type of denture acrylic on biofilm formation by Streptococcus oralis in a constant depth film fermentor. J Appl Microbiol 91: 47–53. [DOI] [PubMed] [Google Scholar]
- 52.Barao VA, Yoon CJ, Mathew MT, Yuan JC, Wu CD, et al. (2014) Attachment of Porphyromonas gingivalis to corroded commercially pure titanium and titanium-aluminum-vanadium alloy. J Periodontol (in press). [DOI] [PubMed]
- 53. Bollen CM, Papaioanno W, Van Eldere J, Schepers E, Quirynen M, et al. (1996) The influence of abutment surface roughness on plaque accumulation and peri-implant mucositis. Clin Oral Implants Res 7: 201–211. [DOI] [PubMed] [Google Scholar]
- 54. Yang CH, Wang YT, Tsai WF, Ai CF, Lin MC, et al. (2011) Effect of oxygen plasma immersion ion implantation treatment on corrosion resistance and cell adhesion of titanium surface. Clin Oral Implants Res 22: 1426–1432. [DOI] [PubMed] [Google Scholar]
- 55. Li JL, Sun MR, Ma XX, Tang GZ (2006) Structure and tribological performance of modified layer on Ti6Al4V alloy by plasma-based ion implantation with oxygen. Wear 261: 1247–1252. [Google Scholar]
- 56.Affronti J (2011) Chronic pancreatitis and exocrine insufficiency. Prim Care 38: 515–537; ix. [DOI] [PubMed]
- 57. Li B, Luo C, Chowdhury S, Gao ZH, Liu JL (2013) Parp1 deficient mice are protected from streptozotocin-induced diabetes but not caerulein-induced pancreatitis, independent of the induction of Reg family genes. Regul Pept 186C: 83–91. [DOI] [PubMed] [Google Scholar]
- 58. Hwang AL, Haynes K, Hwang WT, Yang YX (2013) Metformin and survival in pancreatic cancer: a retrospective cohort study. Pancreas 42: 1054–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Savari O, Zielinski MC, Wang X, Misawa R, Millis JM, et al. (2013) Distinct function of the head region of human pancreas in the pathogenesis of diabetes. Islets 5: 226–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Baker P, Fain P, Kahles H, Yu L, Hutton J, et al. (2012) Genetic determinants of 21-hydroxylase autoantibodies amongst patients of the Type 1 Diabetes Genetics Consortium. J Clin Endocrinol Metab 97: E1573–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Colucci R, Jimenez RE, Farrar W, Malgor R, Kohn L, et al. (2012) Coexistence of Cushing syndrome from functional adrenal adenoma and Addison disease from immune-mediated adrenalitis. J Am Osteopath Assoc 112: 374–379. [PubMed] [Google Scholar]
- 62. Meyer G, Hackemann A, Penna-Martinez M, Badenhoop K (2013) What affects the quality of life in autoimmune Addison's disease? Horm Metab Res 45: 92–95. [DOI] [PubMed] [Google Scholar]
- 63. Tada S, Stegaroiu R, Kitamura E, Miyakawa O, Kusakari H (2003) Influence of implant design and bone quality on stress/strain distribution in bone around implants: a 3-dimensional finite element analysis. Int J Oral Maxillofac Implants 18: 357–368. [PubMed] [Google Scholar]
- 64. Winter W, Klein D, Karl M (2013) Effect of model parameters on finite element analysis of micromotions in implant dentistry. J Oral Implantol 39: 23–29. [DOI] [PubMed] [Google Scholar]