Abstract
Purpose of review
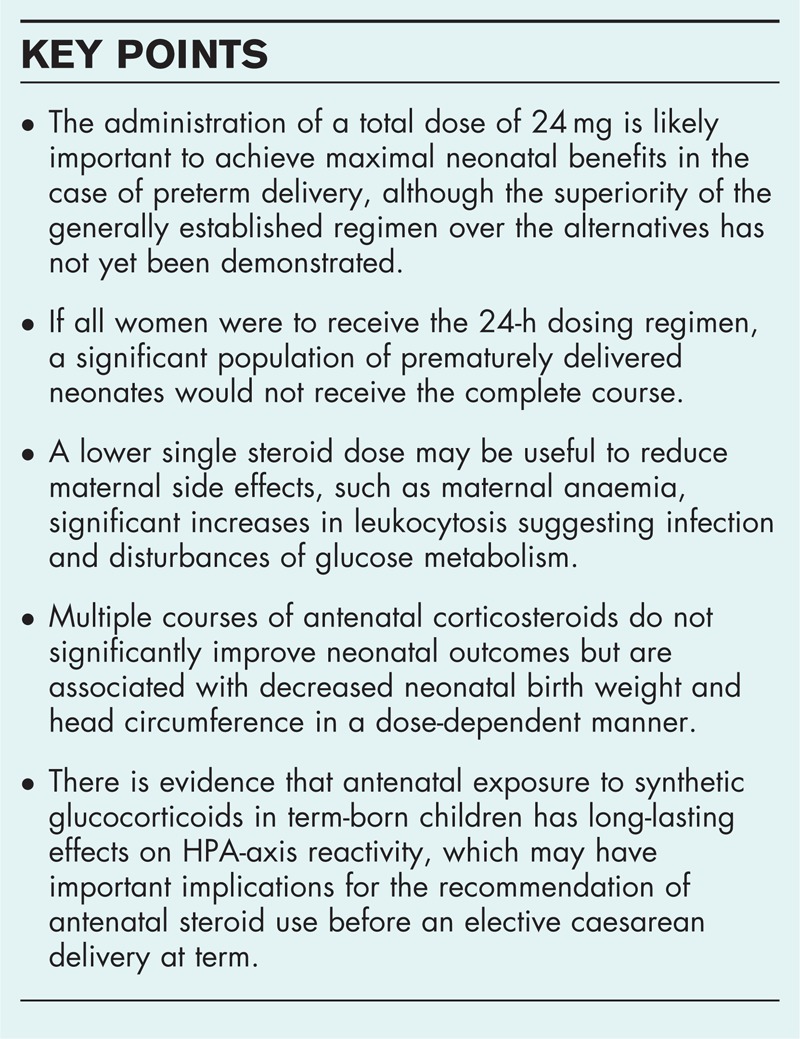
The beneficial effects of antenatal steroids in women at risk of preterm birth are evident. A dose of 24 mg appears sufficient, but there are insufficient data to recommend betamethasone or dexamethasone, a single steroid dose, the optimal interval between doses and repeated courses, the gestational age at which treatment is beneficial and the long-term effects of steroid treatment. This review addresses these aspects of antenatal steroid treatment.
Recent findings
Although the 12-h and 24-h dosing intervals are equivalent with respect to prevention of respiratory distress syndrome, the former enables the completion of treatment in 50% more neonates delivered prematurely. Reducing the single steroid dose in patients at risk for premature birth reduces the associated maternal side effects. An inverse relationship has been demonstrated between the number of corticosteroid courses and foetal growth. The reduced size of exposed foetuses has been attributed to birth at earlier gestational ages and decreased foetal growth. Evidence suggests that antenatal exposure to synthetic glucocorticoids in term-born children has long-lasting effects, which may have important implications in the recommendation of steroids before elective caesarean at term.
Summary
The short-term and long-term effects of the dosage regimen on the pregnant mother and foetus remain unclear.
Keywords: antenatal steroids, dosage regimen, preterm delivery
INTRODUCTION
Prenatal administration of synthetic corticosteroids has been the standard procedure in cases of preterm delivery since 1972, when Liggins and Howie [1] demonstrated that steroid treatment has beneficial effects on the incidence of respiratory distress syndrome (RDS) and neonatal mortality associated with premature birth before 34 weeks’ gestation. A Cochrane Database review published in 2006 summarized 21 studies including 3885 mothers and 4269 infants and confirmed significant reductions in the risks of mortality, RDS and intraventricular haemorrhage (IVH) in preterm infants of 31, 44 and 46%, respectively, after a single course of steroids [2]. Steroids given prenatally also likely decrease the risks of necrotizing enterocolitis (NEC), neonatal ICU (NICU) admission and infection in newborns during the first 48 h of life, as well as the need for respiratory support. Antenatal steroids have not been reported to affect birth weight, delay foetal central nervous system development or increase the risk of maternal death, intra-amniotic infection or puerperal sepsis [2].
Neonatal respiratory outcomes differ among ethnic groups independent of birth weight and gestational age [3]. Haas et al. [4▪▪] showed that genetic polymorphisms in maternal and foetal genotypes for drug-metabolizing enzymes and steroid pathway genes were independently associated with neonatal RDS after treatment with betamethasone for preterm labour. The respiratory outcome severity, including bronchopulmonary dysplasia (BPD) and the need for respiratory support or surfactant use, may be associated with single maternal and foetal nucleotide polymorphisms in key betamethasone pathways [5▪▪].
Box 1.
no caption available
The mechanism of steroid action is complex and affects not only foetal lung maturation [6,7] but also regulation of foetal growth, organ system maturation and the functions of the immune system and sympathetic nervous system [8]. Alteration of the hypothalamic-pituitary-adrenocortical (HPA) axis is a primary consequence observed in the offspring [9]. Steroids play important roles in foetal brain development, altering neuronal migration, synaptic plasticity and neurotransmitter activity [10]. Synthetic corticosteroids given prenatally are not readily metabolized by placental 11β-hydroxysteroid dehydrogenase type 2 (11β-HSD2) and cross the placenta more easily; their influence on the foetal brain may be more pronounced than natural glucocorticoids [11]. Ma et al.[12▪] showed increased expression of 11β-HSD2 in pregnant women with diet-treated GDM, which may limit excessive exposure of the foetus to glucocorticoids.
In 68% of cases, steroid administration transiently decreases vascular resistance in the placental vessels, and the effects last up to 3 days [13]. Clinically, a transient reduction in foetal movements is observed [14]. Foetal exposure to betamethasone also reduces foetal heart rate variability and breathing activity and increases foetal quiescence [15].
Although the effects of antenatal corticosteroids on lung maturation appear to be dose dependent, the biological effects and optimal dosage regimen of antenatal glucocorticoids remain under investigation. The short-term and long-term effects on other systems, particularly the central nervous system, and neurodevelopmental outcomes after different doses and repeat courses require further research. The type of steroid, the dosage and the timing of exposure determine the magnitude of the effects of antenatal steroid treatment on the foetus and mother.
STEROID TYPES
According to the current standard of practice, women at risk of preterm delivery at 24–34 weeks’ gestation receive either a single course of betamethasone intramuscularly in two 12-mg doses at a 24-h interval or dexamethasone in four 6-mg doses at 12-h intervals [16,17]. Although dexamethasone is characterized by a greater affinity for glucocorticoid receptors, betamethasone has a longer half-life [18]. Dexamethasone and betamethasone similarly reduce the risk of perinatal death and alter biophysical activity, although dexamethasone more effectively decreases the incidence of IVH [18]. However, betamethasone is less frequently associated with adverse neurological outcomes [19]. Unlike betamethasone acetate, Jobe et al.[20] showed that a single dose of betamethasone phosphate did not induce foetal lung maturation in sheep. To maintain maximal occupancy of glucocorticoid receptors in tissues, a 1 : 1 mixture of betamethasone phosphate and betamethasone acetate is optimal. The current data are insufficient to recommend one steroid over the other, although a recent study by Remesal et al.[21] suggests that betamethasone might be a better choice than dexamethasone due to stronger inhibition of the expression of phospholipase A2 through the reduction of tumour necrosis factor α in the lungs of newborn rats.
DOSAGE REGIMEN
The guideline-recommended regimen (two 12-mg doses separated by 24 h) was developed to mimic the natural secretion of steroid hormones in preterm infants, which allows for 75% saturation of steroid receptors in foetal tissues [22]. The 24-h dosage interval was selected arbitrarily [18]. Prior to the second dose, the cord blood levels of betamethasone decrease to those observed in untreated children [23]. The more frequent administration of 12 mg or lower doses may allow the steroids to reach the foetus in a nearly constant and even manner [24▪▪]. The total dose of 24 mg was based on animal studies and is sufficient to achieve the steroid concentrations observed in infants after birth during normal physiological stress [25]. Giamfi et al.[26] showed that maternal serum and cord blood betamethasone concentrations did not differ between twin and singleton pregnancies.
The superiority of the generally established regimen over the alternatives has not been demonstrated. Pharmacokinetic data show that betamethasone levels in maternal blood reach the lowest level by 12 h postadministration [23]. Khandelwal et al.[24▪▪] conducted a randomized, noninferiority open trial comparing the effects of two betamethasone regimens: 12 mg over 12-h versus 24-h dosing intervals at 23–34 weeks’ gestation. There were no differences in the RDS incidence, although an increased NEC incidence was observed with 12-h dosing (P = 0.03). If all the women had received the 24-h dosing schedule, approximately 12% of the neonates would not have received the complete course before delivery. In maternal serum, betamethasone levels decreased by more than 50% within 6 h after administration [23]. Our study compared the effects of two betamethasone dosage regimens: six 4-mg doses at 8-h intervals versus two 12-mg doses at a 24-h interval [27▪▪]. The incidences of moderate or severe RDS, IVH and NEC, neonatal infection and anaemia did not differ between groups. Only mild RDS occurred more often in the 4-mg dose group (17.8 versus 15.3%; P = 0.055). The higher single steroid dose most commonly caused maternal anaemia and a significant increase in leukocytosis. The administration of a total dose of 24 mg is most likely the most important for maximal neonatal benefits, but a lower single steroid dose may be useful to reduce maternal side effects, including those in patients with prepregnancy diabetes [28,29].
DURATION OF STEROID ACTION
There are two important aspects concerning the duration of steroid action: the interval between the administration and the start of protection from neonatal complications and the duration of the positive effect. Throughout treatment, foetal serum betamethasone levels are approximately one-third of maternal levels [23]. Hormones are eliminated from the maternal and foetal circulation after 48 h, and the clinical benefit of these compounds is greatly reduced after 7 days [30]. The optimum benefits of glucocorticoid use are achieved 24 h after treatment initiation [16]. Antenatal steroids are most effective when the delivery occurs within 7 days after dose completion, when the reduction in the RDS risk is nearly 50% [2]. Antenatal steroids can prevent RDS for up to 14 days, and there is no linear association between the treatment-to-delivery interval and RDS occurrence [30,31].
EXPOSURE TIME
The efficacy of antenatal steroid treatment depends on gestational age. Mori et al.[32] estimated the effects of steroids in 11 067 children born at 22–33 weeks’ gestation. Antenatal steroids reduced the RDS risk by 9% in the entire cohort, but the effect was significant in infants born at 24–29 weeks’ gestation, reducing the RDS incidence by nearly 20%. Similarly, steroid treatment significantly reduced the risk of IVH in neonates born at 24–29 weeks’ gestation. In a randomized study of 320 patients, Porto et al.[33] demonstrated that steroid administration at gestational weeks 34–36 did not reduce the RDS incidence in newborn infants. Recently, in neonates born at gestational ages of 34 weeks or later, Kamath-Rayne et al.[34▪] confirmed that antenatal corticosteroid treatment following the determination of foetal lung immaturity did not reduce respiratory morbidity. Similar results were shown by Yinon et al.[35▪], who found no differences in RDS incidence between late premature infants treated with steroids and untreated infants, although the neonates given steroids prenatally less frequently presented composite respiratory morbidity (8.4 versus 21%; P = 0.02) or required ventilator support (8.4 versus 20%; P = 0.03). The Royal College of Obstetricians and Gynaecologists recommends a single course of steroids in cases of elective caesarean section prior to 39 weeks’ gestation [16]. Stutchfield et al.[36] analysed the course of the neonatal period for 998 infants delivered by caesarean after 37 weeks’ gestation; steroids were given to 503 women prior to caesarean delivery. NICU admission due to respiratory distress was necessary in 35 children (0.051% with steroids versus 0.024% untreated). To prevent the admission of one neonate to a special care unit, more than 400 children were required to receive unnecessary steroids.
PARTIAL COURSE OF STEROIDS
There is evidence that incomplete treatment with betamethasone or dexamethasone provides some benefits in terms of decreasing morbidity [25]. The smaller benefits attributed to incomplete steroid courses could be due to inadequate doses and shorter durations of foetal exposure. Chien et al.[37] presented data concerning antenatal steroid administration to 11 440 infants in Canada. Only 30% of children completed the antenatal steroid course. Infants who received a complete steroid course exhibited a significant reduction in RDS risk when born before 24 weeks’ or at 24–34 weeks’ gestation. A partial steroid treatment course reduced the incidence of IVH (grades III and IV) and mortality among infants born at 24–35 weeks’ gestation but had no significant effect on RDS. The incidence of NEC was similar in infants receiving a partial or complete course of steroids. Similarly, an analysis by Wong et al.[38] confirmed that hospital mortality was significantly worse without steroids (30 versus 20%; P < 0.001) in extremely premature neonates. Those with no steroid coverage were more likely to have NEC and Grade 3 or 4 IVH.
MULTIPLE STEROID DOSES
According to the American College of Obstetricians and Gynecologists (ACOG), a repeated course of steroids is acceptable if previous treatment was completed over 14 days prior, but only before 34 weeks’ gestation [17]. According to British recommendations, antenatal steroid treatment may be repeated before 34 weeks’ gestation if the first dose was completed 7 days prior and before 26 weeks’ gestation [16]. Crowther et al.[39] summarized the results of eight studies and 3206 children concerning repeat steroid treatment after a 7-day interval. RDS was observed slightly more rarely [relative risk 0.83; 95% confidence interval (CI) 0.75–0.91]. Garite et al.[40] reported a significantly lower risk of neonatal composite morbidity only in infants born 2–7 days after a repeated standard course of betamethasone for deliveries prior to 34 weeks’ gestation (39.3 versus 69.8%; P = 0.035).
Exposure to multiple doses is associated with more profound consequences. Kanagawa et al.[41] compared the effects of repeated doses of dexamethasone on neurogenesis in neonatal rats and showed significant dose-dependent decreases in the number of bromodeoxyuridine-labelled cells in the cortex and the subgranular and subventricular zones. In humans, French et al.[42] reported that serial steroid courses between 24 and 33 weeks’ gestation decreased birth weight and head circumference by 9 and 4%, respectively. A smaller head at birth might be an effect of decreased neurogenesis. Repeated corticosteroid courses were associated with increased rates of aggressive, destructive, distractible and hyperkinetic behaviour at the ages 3 and 6 years [43]. The MACS (Multiple Courses of Antenatal Corticosteroids for Preterm Birth) trial, which included 1858 women at 25–32 weeks’ gestation who did not deliver within 14–21 days after an initial course, showed that multiple antenatal corticosteroid courses (every 14 days) did not improve neonatal outcomes, RDS, BPD, IVH (grades III and IV), cystic periventricular leukomalacia (PVL) or NEC [44]. According to the secondary analysis of the MACS trial, repeated corticosteroid courses were associated with decreased neonatal birth weight (–33.50 g; P = 0.045), length (–0.339 cm, P = 0.019) and head circumference (–0.296 cm, P < 0.001) [45▪▪]. There was a trend towards an incremental decrease in birth weight, length and head circumference for each additional course of antenatal corticosteroids. According to the results of the ACTORDS (Antenatal Collaborative Trial of Repeat Doses of Prenatal Steroids) trial, infants exposed to weekly doses of repeat antenatal corticosteroids presented postnatal growth acceleration 3–5 weeks after birth, which is similar to the catch-up growth observed in intrauterine growth restricted infants [46▪]. Compared with a single course of antenatal glucocorticoids, exposure to repeated doses of antenatal betamethasone was not associated with adverse effects on lung function or altered bone mass in early school-age children [47,48]. However, multiple steroid cycles may cause adrenal insufficiency or osteoporosis in mothers [49].
LONG-TERM EFFECTS OF ANTENATAL STEROIDS
Animal and human data strongly suggest that steroids given prenatally influence and programme the HPA axis, with consequences in the postnatal period [50,51]. Acute suppression of foetal cortisol synthesis and an increase in cortisol bioactivity occur in response to synthetic steroids given prenatally [52]. The suppression of endogenous cortisol production persists in preterm infants and returns to normal after the first week of life [52]. Although baseline levels of cortisol normalize, suppression of the cortisol response to painful stimuli persists even at 4–6 weeks postbirth in premature infants [53,54]. Among healthy full-term infants given steroids prenatally, a pronounced cortisol response to painful stimuli is observed despite normal baseline levels [55]. In a cross-sectional study, Alexander et al.[56▪▪] assessed cortisol secretion patterns in response to a standardized laboratory stressor in 209 6 to 11-year-old children born at term and exposed to antenatal steroids, and they demonstrated significantly increased cortisol reactivity compared with controls (P < 0.001). This finding was independent of the specific synthetic glucocorticoid used and was more pronounced in girls. Erni et al.[57▪] examined psychobiological stress reactivity to a standardized psychosocial stress test in 115 healthy children at 10 years of age and found that it differed in those exposed to prenatal steroids. Animal studies have shown that exposure to elevated glucocorticoid levels during pregnancy is associated with adult-onset diseases, including elevated blood pressure, impaired cardiac and vascular function and altered metabolic function [8].
CONCLUSION
A total dose of 24 mg of betamethasone or dexamethasone appears to be sufficient to achieve the steroid concentrations observed in infants after birth during normal physiological stress. A dosage interval of 24 h for betamethasone administration was selected arbitrarily. The administration of 12 mg of betamethasone at shorter intervals may allow more children to be treated with a complete steroid course. A lower single dose of 6 or even 4 mg appears to be equally effective for the foetus as the standard 12-mg dose and is less toxic to the mother; it may therefore be useful for reducing maternal side effects. Multiple pregnancies do not require dose increases over 24 mg due to similar maternal serum and cord blood concentrations of betamethasone in twin and singleton pregnancies. The short-term and long-term effects of the dosage regimen on both the pregnant mother and the foetus require further investigation.
Acknowledgements
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Liggins GC, Howie RN. A controlled trial of antepartum glucocorticoid treatment for the prevention of respiratory distress syndrome in premature infants. Pediatrics 1972; 50:515–525 [PubMed] [Google Scholar]
- 2.Roberts D, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 2006; CD004454 [DOI] [PubMed] [Google Scholar]
- 3.Frisbie WP, Song SE, Powers DA, Street JA. The increasing disparity in infant mortality: respiratory distress syndrome and other causes. Demography 2004; 41:773–800 [DOI] [PubMed] [Google Scholar]
- 4▪▪.Haas DM, Lehmann AS, Skaar T, et al. The impact of drug metabolizing enzyme polymorphisms on outcomes after antenatal corticosteroid use. Am J Obstet Gynecol 2012; 206:447 e17–e24 [DOI] [PMC free article] [PubMed] [Google Scholar]; This study aimed to explain the differences in the development of RDS seen in preterm neonates despite antenatal steroid treatment. This study showed that genetic polymorphisms in both the maternal and foetal genotypes for drug-metabolizing enzymes (CYP3A5 and CYP3A7) and for steroid pathway genes (adenyl cyclase 9) were associated with the development of RDS.
- 5▪▪.Haas DM, Dantzer J, Lehmann AS, et al. The impact of glucocorticoid polymorphisms on markers of neonatal respiratory disease after antenatal betamethasone administration. Am J Obstet Gynecol 2013; 208:215 e1–e6 [DOI] [PMC free article] [PubMed] [Google Scholar]; This study indicates that single maternal and foetal single nucleotide polymorphisms in key betamethasone pathways may be associated with the severity of respiratory outcomes, such as BPD and the need for respiratory support or surfactant use.
- 6.Ballard PL, Ballard RA. Scientific basis and therapeutic regimens for use of antenatal glucocorticoids. Am J Obstet Gynecol 1995; 173:254–262 [DOI] [PubMed] [Google Scholar]
- 7.Claessens SEF, Belanoff JK, Kanatsou S, et al. Acute effects of neonatal dexamethasone treatment on proliferation and astrocyte immunoreactivity in hippocampus and corpus callosum: towards a rescue strategy. Brain Res 2012; 1482:1–12 [DOI] [PubMed] [Google Scholar]
- 8.Singh RR, Cuffe JS, Moritz KM. Short- and long-term effects of exposure to natural and synthetic glucocorticoids during development. Clin Exp Pharmacol Physiol 2012; 39:979–989 [DOI] [PubMed] [Google Scholar]
- 9.Waffarn F, Davis EP. Effects of antenatal corticosteroids on the hypothalamic-pituitary-adrenocortical axis of the fetus and newborn: experimental findings and clinical considerations. Am J Obstet Gynecol 2012; 207:446–454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weinstock M. The long-term behavioural consequences of prenatal stress. Neurosci Biobehav Rev 2008; 32:1073–1086 [DOI] [PubMed] [Google Scholar]
- 11.Brown RW, Diaz R, Robson AC, et al. The ontogeny of 11(-hydroksysteroid dehydrogenase type 2 and mineralicortocoid receptor gene expression reveal intricate control of glucocorticoid action in development. Endocrinology 1996; 137:794–797 [DOI] [PubMed] [Google Scholar]
- 12▪.Ma R, Liu J, Wu L, et al. Differential expression of placental 11beta-hydroxysteroid dehydrogenases in pregnant women with diet-treated gestational diabetes mellitus. Steroids 2012; 77:798–805 [DOI] [PubMed] [Google Scholar]; This study showed the differential expression of 11β-HSD1 and 11β-HSD2 in pregnant women with diet-treated GDM, which may be the mechanism that limits excessive foetal exposure to glucocorticoids. This may imply that pregnant women with GDM should be advised carefully with respect to diet.
- 13.Wallace EM, Baker LS. Effect of antenatal betamethasone administration on placental vascular resistance. Lancet 1999; 353:1404–1407 [DOI] [PubMed] [Google Scholar]
- 14.Abbasalizadeh S, Pharabar ZN, Abbasalizadeh F, et al. Efficacy of betamethasone and fetal motion and biophysical profile and amniotic fluid index in preterm fetuses. Pak J Biol Sci 2013; 16:1569–1573 [DOI] [PubMed] [Google Scholar]
- 15.Mulder EJH, Koenen SV, Blom I, Visser GHA. The effects of antenatal betamethasone administration on fetal heart rate and behaviour depend on gestational age. Early Hum Dev 2004; 76:65–77 [DOI] [PubMed] [Google Scholar]
- 16.Royal College of Obstetricians and Gynaecologists. RCOG, Green-top Guideline No. 7. Antenatal corticosteroids to reduce neonatal morbidity and mortality. London:2010 [DOI] [PubMed] [Google Scholar]
- 17.ACOG Committee on Obstetric Practice ACOG Committee Opinion No. 475: antenatal corticosteroid therapy for fetal maturation. Obstet Gynecol 2011; 177:422–424 [DOI] [PubMed] [Google Scholar]
- 18.Brownfoot FC, Crowther CA, Middleton P. Different corticosteroids and regimens for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 2008; CD006764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee BH, Stoll BJ, McDonald SA, Higgins RD. Neurodevelopmental outcomes of extremely low birth weight infants exposed prenatally to dexamethasone versus betamethasone. National Institute of Child Health and Human Development Neonatal Research Network. Pediatrics 2008; 21:289–296 [DOI] [PubMed] [Google Scholar]
- 20.Jobe AH, Nitsos I, Pillow JJ, et al. Betamethasone dose and formulation for induced lung maturation in fetal sheep. Am J Obstet Gynecol 2009; 201:611.e1–e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Remesal A, San Feliciano L, De Luca D, et al. Effect of antenatal corticosteroids in activity and expression of secretory phospholipase A2 and TNF alfa in lung of newborn rats. Arch Dis Child 2012; 97:A118 [Google Scholar]
- 22.Collaborative Group on Antenatal Steroid Therapy Effect of antenatal dexamethasone administration on the prevention of respiratory distress syndrome. Am J Obstet Gynecol 1981; 141:276–287 [PubMed] [Google Scholar]
- 23.Ballard PL, Granberg P, Ballard RA. Glucocorticoid level in maternal and cord serum after perinatal betamethasone therapy to prevent respiratory distress syndrome. J Clin Invest 1975; 56:1548–1554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24▪▪.Khandelwal M, Chang E, Hansen C, et al. Betamethasone dosing interval: 12 or 24 h apart? A randomized, noninferiority open trial. Am J Obstet Gynecol 2012; 206:201–211 [DOI] [PubMed] [Google Scholar]; This is a randomized study showing that the 12-h dosing regimen is equivalent to the 24-h dosing interval for the prevention of RDS. The 12-h interval enables the complete course of steroid treatment in 50% more neonates delivered prematurely.
- 25.Elimian A, Figureoa R, Spitzer AR, et al. Antenatal corticosteroids: are incomplete courses beneficial? Obstet Gynecol 2003; 102:352–355 [DOI] [PubMed] [Google Scholar]
- 26.Giamfi C, Mele L, Wagner RJ, et al. The effect of plurality and obesity on betamethasone concentrations in women at risk for preterm delivery. Am J Obstet Gynecol 2010; 203:219.e1–e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27▪▪.Romejko-Wolniewicz E, Oleszczuk L, Zaręba-Szczudlik J, Czajkowski K. Dosage regimen of antenatal steroids prior to preterm delivery and effects on maternal and neonatal outcomes. J Matern Fetal Neonatal Med 2013; 26:237–241 [DOI] [PubMed] [Google Scholar]; This study showed that the incidences of moderate or severe RDS, IVH and NEC are similar for a single steroid dose of 4 mg administered six times in 8-h intervals and a standard single 12 mg steroid dose given at 24-h intervals. The higher single steroid dose was more likely to cause maternal side effects.
- 28.Ogawa M, Matsuda Y, Kobayashi A, et al. Ritodrine should be carefully administered during antenatal glucocorticoid therapy even in nondiabetic pregnancies. ISRN Obstet Gynecol 2013; 2013:120735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu JY, Liang Z, Chai Y, et al. Changes in maternal glucose metabolism after the administration of dexamethasone for fetal lung development. Int J Endocrinol 2012; 2012:652806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilms FF, Vis JY, Pattinaja DAPM, et al. Relationship between the time interval from antenatal corticosteroid administration until preterm birth and the occurrence of respiratory morbidity. Am J Obstet Gynecol 2011; 205:49.e1–e7 [DOI] [PubMed] [Google Scholar]
- 31.Ring AM, Garland JS, Stafeil BR, et al. The effect of a prolonged time interval between antenatal corticosteroid administration and delivery on outcomes in preterm neonates: a cohort study. Am J Obstet Gynecol 2007; 196:457 e1-457.e6 [DOI] [PubMed] [Google Scholar]
- 32.Mori R, Kusuda S, Fujimura M. Antenatal corticosteroids promote survival of extremely preterm infants born at 22 to 23 weeks of gestation. J Pediatr 2011; 159:110–114 [DOI] [PubMed] [Google Scholar]
- 33.Porto AM, Coutinho IC, Correia JB, Amorim MM. Effectiveness of antenatal corticosteroids in reducing respiratory disorders in late preterm infants: randomised clinical trial. BMJ 2011; 342:d1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34▪.Kamath-Rayne BD, DeFranco EA, Marcotte MP. Antenatal steroids for treatment of fetal lung immaturity after 34 weeks of gestation: an evaluation of neonatal outcomes. Obstet Gynecol 2012; 119:909–916 [DOI] [PMC free article] [PubMed] [Google Scholar]; This study confirmed that antenatal corticosteroid treatment following the determination of foetal lung immaturity did not reduce respiratory morbidity.
- 35▪.Yinon Y, Haas J, Mazaki-Tovi S, et al. Should patients with documented fetal lung immaturity after 34 weeks of gestation be treated with steroids? Am J Obstet Gynecol 2012; 207:222 e1–e4 [DOI] [PubMed] [Google Scholar]; This study also found no differences in RDS incidence between late premature infants treated with steroids and untreated infants.
- 36.Stutchfield P, Whitaker R, Russell I. Antenatal betamethasone and incidence of neonatal respiratory distress after elective cesarean section: pragmatic randomised trial. BMJ 2005; 331:662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chien LY, Ohlsson A, Seshia MMK, Boulton J. Variations in antenatal corticosteroid therapy: a persistent problem despite 30 years of evidence. Obstet Gynecol 2002; 99:401–408 [DOI] [PubMed] [Google Scholar]
- 38.Wong D, Abdel-Latif ME, Kent AL. Differences in mortality/morbidity with a complete course of antenatal steroids compared to an incomplete/no course in extremely premature neonates. Archiv Dis Child 2012; 97: A348–A349 [Google Scholar]
- 39.Crowther CA, McKinlay CJD, Middleton P, Harding JE. Repeat doses of prenatal corticosteroids for women at risk of preterm birth for improving neonatal health outcomes. Cochrane Database Syst Rev 2011; CD003935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Garite TJ, Kurtzman J, Maurel K, Clark R. Impact of a ‘rescue course’ of antenatal corticosteroids: a multicenter randomized placebo-controlled trial. Am J Obstet Gynecol 2009; 200:248.e1–e9 [DOI] [PubMed] [Google Scholar]
- 41.Kanagawa T, Tomimatsu T, Hayashi S, et al. The effects of repeated corticosteroid administration on the neurogenesis in the neonatal rat. Am J Obstet Gynecol 2006; 194:231–238 [DOI] [PubMed] [Google Scholar]
- 42.French NP, Hagan R, Evans SF, et al. Repeated antenatal corticosteroids: size at birth and subsequent development. Am J Obstet Gynecol 1999; 180:114–121 [DOI] [PubMed] [Google Scholar]
- 43.French NP, Hagan R, Evans SF, et al. Repeated antenatal corticosteroids: effects on cerebral palsy and childhood behavior. Am J Obstet Gynecol 2004; 190:588–595 [DOI] [PubMed] [Google Scholar]
- 44.Murphy KE, Hannah ME, Willan AR, et al. Multiple courses of antenatal corticosteroids for preterm birth (MACS): a randomised controlled trial. Lancet 2008; 372:2143–2151 [DOI] [PubMed] [Google Scholar]
- 45▪▪.Murphy KE, Willan AR, Hannah ME, et al. Effect of antenatal corticosteroids on fetal growth and gestational age at birth. Obstet Gynecol 2012; 119:917–923 [DOI] [PubMed] [Google Scholar]; This is a secondary analysis of the effect of multiple courses of antenatal corticosteroids on foetal size at birth. The reduction in size of the exposed foetuses was attributed not only to being born at an earlier gestational age but also to decreased foetal growth. A dose–response relationship was demonstrated between the number of corticosteroid courses and a decrease in foetal growth, which may implicate corticosteroid use in growth restriction.
- 46▪.Battin M, Bevan C, Harding J. Growth in the neonatal period after repeat courses of antenatal corticosteroids: data from the ACTORDS randomised trial. Arch Dis Child Fetal Neonatal Ed 2012; 97:F99–F105 [DOI] [PubMed] [Google Scholar]; This study demonstrates that babies exposed to repeated weekly doses of antenatal corticosteroids present postnatal growth acceleration 3–5 weeks after birth, similar to the catch-up growth of intrauterine growth restricted babies.
- 47.McKinlay CJD, Harding JE, Ashwood PJ, et al. Effect of repeat antenatal betamethasone on childhood lung function: a randomized controlled trial (actords). J Paediatrics Child Health 2013; 49:92–93 [Google Scholar]
- 48.McKinlay CJD, Cutfield WS, Battin MR, et al. Repeat antenatal betamethasone does not affect bone mass at early school-age: a randomised controlled trial (actords). J Paediatrics Child Health 2013; 49: 49 [Google Scholar]
- 49.Helal KJ, Gordon MC, Lightner CR, Barth WH. Adrenal suppression induced by betamethasone in women at risk for premature delivery. Obstet Gynecol 2000; 96:287–290 [DOI] [PubMed] [Google Scholar]
- 50.Sandman CA, Davis EP. Gestational stress influences cognition and behavior. Future Neurol 2010; 5:675–690 [Google Scholar]
- 51.Harris A, Seckl J. Glucocorticoids, prenatal stress and the programming of disease. Horm Behav 2011; 59:279–289 [DOI] [PubMed] [Google Scholar]
- 52.Nykanen P, Ralvio T, Heinonen K, et al. Circulating glucocorticoid bioactivity and serum cortisol concentration in premature infants: the influence of exogenous glucocorticoids and clinical factors. Eur J Endocrinol 2007; 156:577–583 [DOI] [PubMed] [Google Scholar]
- 53.Davis EP, Townsend EL, Gunnar MR, et al. Effects of prenatal betamethasone exposure on regulation of stress physiology in healthy premature infants. Psychoneuroendocrinology 2004; 29:1028–1036 [DOI] [PubMed] [Google Scholar]
- 54.Schaffer L, Luzi F, Burkhardt T, et al. Antenatal betamethasone administration alters stress physiology in healthy neonates. Obstet Gynecol 2009; 113:1082–1088 [DOI] [PubMed] [Google Scholar]
- 55.Davis EP, Walfarn F, Sandman CA. Prenatal treatment with glucocorticoids sensitizes the HPA axis response to stress among full-term infants. Dev Psychobiol 2011; 53:175–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56▪▪.Alexander N, Rosenlocher F, Stalder T, et al. Impact of antenatal synthetic glucocorticoid exposure on endocrine stress reactivity in term-born children. J Clin Endocrinol Metab 2012; 97:3538–3544 [DOI] [PubMed] [Google Scholar]; This study provided the first evidence for long-lasting effects of antenatal synthetic glucocorticoids exposure on HPA-axis reactivity in term-born children. These findings may have important implications for recommendations of the antenatal use of steroids, especially before elective caesarean sections and repeated doses.
- 57▪.Erni K, Shaqiri-Emini L, La Marca R, et al. Psychobiological effects of prenatal glucocorticoid exposure in 10-year-old-children. Front Psychiatry 2012; 3:104. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study found changed psychobiological stress reactivity in a standardized psychosocial stress test at the age of 10 in children who have been exposed to prenatal maternal glucocorticoids.


