Abstract
Objective
Changes in adolescent interpersonal behavior before and after an acute course of psychotherapy were investigated as outcomes and mediators of remission status in a previously described treatment study of depressed adolescents. Maternal depressive symptoms were examined as moderators of the association between psychotherapy condition and changes in adolescents’ interpersonal behavior.
Method
Adolescents (n = 63, mean age = 15.6 years, 77.8% female, 84.1% Caucasian) engaged in videotaped interactions with their mothers before randomization to cognitive behavior therapy (CBT), systemic behavior family therapy (SBFT), or nondirective supportive therapy (NST), and after 12–16 weeks of treatment. Adolescent involvement, problem solving and dyadic conflict were examined.
Results
Improvements in adolescent problem solving were significantly associated with CBT and SBFT. Maternal depressive symptoms moderated the effect of CBT, but not SBFT, on adolescents’ problem solving; adolescents experienced increases in problem solving only when their mothers had low or moderate levels of depressive symptoms. Improvements in adolescents’ problem solving were associated with higher rates of remission across treatment conditions, but there were no significant indirect effects of SBFT on remission status through problem solving. Exploratory analyses revealed a significant indirect effect of CBT on remission status through changes in adolescent problem solving, but only when maternal depressive symptoms at study entry were low.
Conclusions
Findings provide preliminary support for problem solving as an active treatment component of structured psychotherapies for depressed adolescents and suggest one Pathway by which maternal depression may disrupt treatment efficacy for depressed adolescents treated with CBT.
Keywords: Adolescents, Depression, Psychotherapy, Parent-child Interactions
Depressed children and adolescents often have discordant parent-child relationships, marked by high rates of conflict, hostility, rejection, low support and cohesion, and poor communication (Birmaher et al., 2004b; Sheeber, Hops, & Davis, 2001) that may persist after recovery from acute depressive episodes (Sheeber, Hops, Alpert, Davis, & Andrews, 1997). As such, maladaptive family interactions have been postulated to be one of the mechanisms by which depression develops and is maintained in at-risk children and adolescents (Goodman & Gotlib, 1999; Nomura, Wickramaratne, Warner, Mufson & Weissman, 2002). Studies on depressed youths find high levels of impairment in family functioning to be associated with the severity of children’s depressive symptoms, including irritability, low motivation, and social withdrawal (Birmaher et al., 2004a). More recent studies suggest that discordant interactions in the families of depressed youths may be stable and less influenced by the presence or absence of depressive symptoms in youths. Repeated measures of mother-child interactions in a small group of youth whose index episode of depression either remitted or persisted suggest that many aspects of mother-child interactions do not change when children are no longer symptomatic (Dietz et al., 2008a). Similarly, the frequency of mothers’ critical comments about their adolescents did not differ between currently depressed or remitted youth (Silk et al., 2009). Very few empirical studies have examined mother-child interactions in depressed youth longitudinally, and none to date have examined changes in parent-child interactions before and after a course of treatment for adolescent depression. Hence, one of the primary goals of this study is to explore whether certain aspects of adolescent interpersonal behavior observed in interactions with their mothers change over a course of psychotherapy, and if these changes are associated with specific treatment approaches.
Maternal depression has been consistently found to moderate clinical outcomes in treatment studies of adolescent depression, with high maternal depressive symptoms associated with reduced efficacy of cognitive behavior therapy (CBT) on adolescent depression (Brent et al., 1998b; Garber et al., 2009). However, the Pathways by which maternal depression may reduce treatment efficacy for depressed adolescents remain unclear. Problematic mother-child relationships have been suspected to mediate the association between maternal depression and depressed adolescents’ diminished response to psychotherapy (Asarnow et al., 2009; Birmaher et al., 2000; Feeny et al., 2009). Maternal depression is associated with conflict in both marital and mother-child relationships (Goodman & Gotlib, 1999), as well as lower shared positivity and higher disengagement in mothers’ interactions with depressed adolescents (Dietz, et al., 2008a). Maternal depression may sustain negative mother-child interactions that contribute to adolescent depressive symptoms (Hammen, Shih, & Brennan, 2004; Shelton & Harold, 2008) and may impair the adaptation and generalization of effective cognitive and interpersonal skills that are often taught in empirically supported psychotherapies for depression (Brent, Holder, & Kolko, 1998a; Garber, et al., 2009). Depressed mothers may present as less responsive and less skilled social partners to youth who are learning to engage, negotiate, and communicate their needs in relationships. Mothers who have difficulty engaging in positive social relationships and flexible social problem solving may model and reinforce maladaptive interpersonal interactions. Therefore, another goal of this study was to explore the role of maternal depression as a moderator of treatment and changes in adolescents’ interpersonal behavior with their mothers.
The current study investigated changes in adolescents’ interpersonal behavior during mother-child interactions in a previously described sample of depressed adolescents who were randomized to receive one of three psychosocial treatments (Brent et al., 1997): CBT, systemic behavior family therapy (SBFT), and nondirective supportive therapy (NST). Using an intent-to-treat sample, Brent and colleagues (1997) found that depressed adolescents who received CBT were less likely to have met criteria for a diagnosis of MDD at the end of treatment compared with adolescents’ receiving NST, and had a higher rate of remission compared to depressed adolescents receiving SBFT or NST. Subsequent analyses identified comorbid anxiety, hopelessness, cognitive distortion, and later age of onset as predictors of worse outcomes in the sample aggregated across treatments (Brent et al., 1998b).
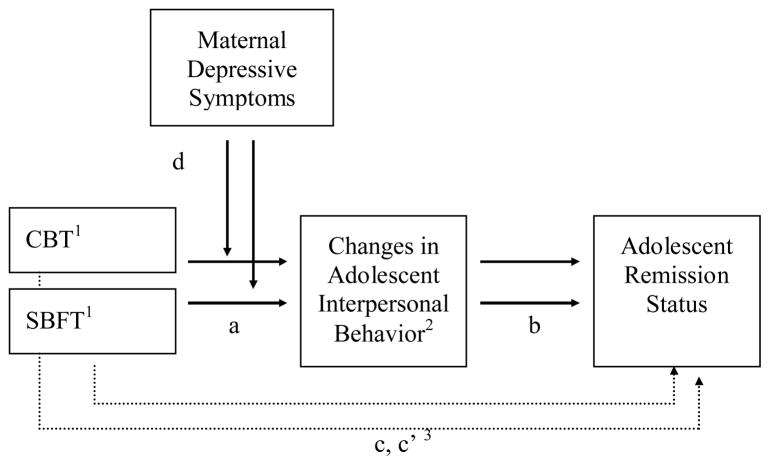
The first aim of this paper was to test a model outlining associations between treatment conditions, change in adolescent interpersonal behavior across treatment duration, and adolescent remission status at post-treatment (see Figure 1). We hypothesized that adolescents’ involvement and problem-solving would significantly increase and dyadic conflict would decrease in the CBT and SBFT conditions (Path a). We also hypothesized that adolescents’ involvement and problem solving would be positively correlated with adolescent remission status, and that dyadic conflict would be negatively associated with post-treatment remission status (Path b). Lastly, we hypothesized that the structured psychotherapies, CBT and SBFT, would be associated with post-treatment adolescent remission status as compared to NST (Path c). The second aim of this paper was to test for indirect effects of treatment group on remission status through changes in observed adolescent interpersonal behaviors. We hypothesized that changes in each of the observed adolescent interpersonal behaviors (involvement, problem solving, dyadic conflict) would have significant indirect effects on the association between structured psychotherapies and adolescents’ remission status (Path c′). Exploratory analyses, employing a moderated mediation paradigm (MacKinnon & Luecken, 2008), were conducted to determine whether or not hypothesized indirect effects of treatment group on remission status through adolescents interpersonal behavior would be moderated by maternal depression (Path d). Because of the small sample size and limited statistical power in this sample, these exploratory analyses were conducted with the goal of clarifying hypotheses for future studies.
Figure 1.
An illustration of planned analyses for hypotheses testing. 1 Each structured psychotherapy is represented by a dummy-coded variables: a) CBT or (b) SBFT, compared to those adolescent who received NST. 2 Three observed indices of adolescents’ interpersonal behavior were assessed during interactions with mothers before and after treatment: adolescent involvement, adolescent problem solving, and dyadic conflict. Changes in adolescents’ interpersonal behavior were estimated by controlling for pre-treatment behavior in regression models. 3 Path c represents the association between each structured psychotherapy and adolescent remission status at post treatment; Path c′ represents the indirect effects of each structured psychotherapy on adolescent remission status through changes in each adolescent interpersonal behavior (involvement, problem solving, dyadic conflict).
Method
Detailed descriptions of the study design and sample have been provided in previous communications (Brent, et al., 1997; Kolko, Brent, Baugher, Bridge, & Birmaher, 2000). Key study features are reviewed briefly to provide information related to the aims of this paper.
Participants
Adolescents enrolled in this clinical trial (n = 107) were between the ages of 13–18, met criteria for major depressive disorder (MDD) on the DSM-III-R (American Psychiatric Association, 1987) as measured by the Schedule for Affective Disorders and Schizophrenia for School-Age Children – Present Version (Chambers et al., 1985), and reported clinically significant depressive symptoms (≥ 13) on the Beck Depression Inventory (BDI). Exclusion criteria included a history of or concurrent psychosis, bipolar disorder, obsessive-compulsive disorder, eating disorder, substance abuse disorder in past 6 months, recent physical or sexual abuse, pregnancy, or chronic medical illness. The study was approved by the IRB at the University of Pittsburgh and conducted in accordance with ethical standards in the treatment of human subjects as outlined by the American Psychological Association. All adolescents provided informed assent for participation in this study and parents gave informed consent.
The present study was comprised of 63 adolescents who finished a 12-week course of psychosocial treatment (CBT = 25, SBFT = 20, and NST = 18) and completed both the observed parent-child interaction protocol at pre- and post-treatment. This sample of adolescents did not differ from the originally recruited sample by demographic factors, including age, race, gender, family composition, depression severity at pre- and post-treatment, by recruitment type (clinical referral or advertisement), or by treatment modality. However, the adolescents included the present study completed significantly more sessions (mean number of sessions (SD) = 13.6 (1.3)) than those not included in the study (mean number of sessions (SD) = 8.2 (4.9)), F (1, 105) = 68.52, p = .000). They were also more likely to have a comorbid anxiety disorder at pre-treatment (14.3%) compared to adolescents not included in study (0%), Fisher’s Exact Test, p = .01. Although they did not differ from adolescents who did not participate in this study on post-treatment depressive diagnosis, 87.3% of adolescents included in this study did not meet diagnostic criteria for depression at post-treatment.
Treatment Protocol
Treatment consisted of 12–16 weekly sessions of CBT, SBFT, or NST delivered by experienced therapists (see Brent, et al., 1997). The CBT protocol was derived from Beck’s treatment model (Beck, Rush, Shaw, & Emery, 1979) and contributed to later CBT protocols for adolescent depression more recently reported in the literature (Brent et al., 2008; March et al., 2004). This intervention focused heavily on cognitive restructuring, but utilized both behavioral activation and taught problem solving skills on a case-by-case basis (see review by Weersing, Rozenman & Gonzalez, 2009). SBFT combined aspects of both Functional Family Therapy (FFT) (Alexander & Parsons, 1973), intended to clarify concerns and identify dysfunctional patterns of family interaction and a behavioral family systems approach (Robin & Foster, 1989), aimed at teaching communication and problem-solving skills to reduce familial conflict. NST protocol was based on Client Centered Therapy (Rogers, 1951) and adapted from models of supportive therapy used in clinical trials with adults (Lerner & Clum, 1990). NST focused on providing support, aiding the adolescent in affect identification and expression of feelings, and discussing patient-initiated options for addressing problems. NST therapists relied on the techniques of accurate empathy and reflexive listening, and refrained from giving advice, setting limits, or teaching specific skills. Expert ratings of videotaped sessions demonstrated that the 3 treatments were delivered with fidelity and were distinct from each other (Brent et al., 1997). Adolescents were removed from treatment at week 6 if they continued to meet criteria for major depression or failed to improve based upon self-reported measures of depression severity.
Instruments
Adolescents’ Depression Diagnosis
Adolescents’ diagnosis of Major Depressive Disorder (MDD) after treatment was assessed using the Schedule for Affective Disorders and Schizophrenia for School-Age Children Present Episode Version (K-SADS-P) (Chambers, et al., 1985), with both the adolescent and parent(s) serving as informants. To meet diagnostic criteria for MDD (0 = absent, 1 = present), adolescents endorsed at least 5 depressive symptoms that persisted for at least a two week period and interfered with their global functioning.
Adolescents Depressive Symptoms
The Beck Depression Inventory (BDI) (Beck, Epstein, Brown & Steer, 1988), a 21-item self-report questionnaire, indexed adolescents’ weekly depressive symptoms during treatment, with higher scores suggesting higher depression severity.
Adolescent Remission Status
Adolescent remission status was informed by post-treatment diagnoses of Major Depressive Disorder (MDD) and adolescents’ weekly self-report of depressive symptoms. Remission status (0 = nonremitted; 1 = remitted) was defined as adolescents’ not meeting diagnostic criteria for MDD at the end of treatment (as defined by K-SADS-P), and the average total score for the last 3 BDI reports < 9. Remission status as defined for this paper was similar to how remission was defined in the parent paper (e.g., absence of MDD diagnosis and 3 consecutive weeks with a BDI<9), r = 0.85, p < .001. We modified the criteria slightly in order to accommodate adolescents who had 2 out of 3 BDIs at the end of treatment (n = 6) and to more closely link post-treatment diagnosis and adolescent report of depressive symptoms at the end of treatment.
Maternal Depressive Symptoms
The Beck Depression Inventory (BDI) (Beck, et al., 1988), a 21-item self-report questionnaire, indexed maternal depressive symptoms prior to adolescents’ start of psychosocial treatment.
Mother-Adolescent Interactions
Ten-minute mother-adolescent interactions were videotaped before and after treatment for the purposes of evaluating changes in adolescent interpersonal behavior. Each dyad was asked to discuss two previously reported issues that currently caused conflict in their relationship. A well-validated, global coding system (Hetherington, Hagan, & Eisenberg, 1992) was employed to obtain 12 observational measures of affect and behavior for adolescents (see Supplemental Materials 1). Each of these variables was rated on a 1–5 Likert scale, with higher numbers indicating traits or behaviors more characteristic (occurs with frequency and/or intensity) of the adolescent in the videotaped interaction.
Videotaped parent-adolescent interactions were coded after the treatment study was completed. Coders were blinded to treatment groups and to the pre- or post-sessions for a given dyad. To minimize halo effects, pre- and post-treatment videotapes were not coded during the same session. Reliability was established on approximately 20% of the coded videotapes between a criterion and secondary coder. Satisfactory inter-rater reliability was determined by intra-class correlations and reduced the number of observational measures to 9 (ICC range: 0.68–0.85, see Supplemental Materials 1).
Of these 9 coded behaviors, two adolescent behaviors were examined in the course of this study: 1) Involvement, the degree to which adolescents initiated ideas about subjects discussed, solicited the other’s point of view to encourage dyadic participation, responded to other’s questions or ideas, or suggested new topics to further elicit discussion of related topics. 2) Problem Solving, the degree to which adolescents willingly negotiated or compromised on their own position in order to resolve the issue being discussed in an appropriate and plausible manner. In addition, the degree of 3) Dyadic Conflict, aversive communication (name calling, swearing, mocking, non-constructive criticism, yelling, verbal threats) and/or behavior (withdrawing from or ending the interaction) that escalates negative affect and feedback between adolescent and mother, was coded for each dyad. Inter-class correlations to assess reliability between raters was satisfactory (ICC for adolescent involvement = 0.70; ICC for adolescent problem solving = 0.68; ICC for dyadic conflict = 0.79). See Supplemental Materials 2 for correlations among behavior codes.
The variables investigated were based upon their overlap with components of the structured therapies (involvement, problem solving) and the empirical literature on adolescent depression and family functioning (dyadic conflict). Adolescent assertiveness was strongly correlated with involvement, and was not examined because of its specificity to CBT rather than SBFT. Indices of adolescent hostility, coercion, and antisocial behavior were not examined because they are more likely associated with adolescent externalizing disorders. The remaining factors (warmth, prosocial behavior) did not appear to map as well onto the putative mechanisms of structured therapies for reducing adolescent depression.
Potential Covariates
The following questionnaires were examined as potential covariates as they were previously identified as moderators of treatment outcomes in the parent study (Brent et al., 1998b): The Beck Hopelessness Scale (BHS) (Beck, Weissman, Lester, & Trexler, 1974), a 20-item self-report questionnaire, was used to assess the degree of hopelessness in adolescents before treatment. The Children’s Negative Cognitive Error Questionnaire (CNCEQ) (Leitenberg, Yost, & Carroll-Wilson, 1986), a 24-item self-report, assessed adolescents’ cognitive distortions, such as catastrophizing, personalization, overgeneralization, and selective abstraction. The Conflict Behavior Questionnaire, Parent and Child versions (CBQ-P/C) (Robin & Weiss, 1980) is a 20-item questionnaire designed to measure conflict and negative communication within the mother-adolescent relationship as perceived by both the adolescent and mother. Socioeconomic status (SES) was measured using the Hollingshead Four-Factor Index (Hollingshead, 1975), with lower numbers indicating higher social status. In addition, adolescents and parents reported on other demographic variables, such as age, sex, minority status, and family composition.
Data Analysis Plan
First, the demographic characteristics of the CBT, SBFT, and NST treatment groups were compared for equivalence using analysis of variance (ANOVA), chi-square (χ2), or Pearson’s correlations as appropriate. All post-hoc tests included Least Significant Difference (LSD) corrections. Pearson’s correlations and ANVOA were used to assess relationships between potential covariates and post-treatment adolescent remission status.
Second, multiple linear regressions were used to test the effects of treatment condition on changes in observed indices of adolescents’ interpersonal behavior during mother-adolescent interactions (see Figure 1, Path a). Two dummy coded variables (Cohen, Cohen, West, & Aiken, 2003) were used to compare the effects of treatment condition, specifically in adolescents who received (a) CBT or (b) SBFT, compared to those adolescent who received NST. Third, logistic regressions were conducted to determine whether a significant relationship between changes in observed indices of adolescent behavior over time was associated with adolescents’ remission status (see Figure 1, Path b). Fourth, logistic regression analyses were conducted to determine whether CBT or SBFT were associated with adolescent remission status (Figure 1, Path c). After testing these 3 Pathways, the indirect effects of treatment condition on remission status through changes in adolescent interpersonal behavior were assessed (Figure 1, Path c′). Indirect effects were tested using the PROCESS macro for SPSS (Hayes, 2012) and according to guidelines for mediation (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002).
Next, we tested the hypotheses that maternal depressive symptoms moderated the relationship between treatment condition and changes in adolescents’ interpersonal behavior during mother-adolescent interactions (see Figure 1, Path d). Maternal BDI was centered in order to reduce nonessential multicollinearity (Aiken & West, 1991, Chapter 3). Two interaction terms were calculated, the products of maternal depressive symptoms and each of the dummy-coded variables representing the CBT and SBFT groups, and entered into step 2 of the regression model. All steps to test and probe statistical interactions were conducted using Aiken & West (1991, pp. 12–13) guidelines. Significant interactions were then probed by estimating the simple slopes of the corresponding paths at high maternal BDI (+1 SD from the mean) and low maternal BDI (−1 SD from the mean).
Lastly, analyses were conducted to investigate moderated mediation for significant interactions detected between maternal depression and treatment group. Moderated mediation was examined using Mplus version 6.12 because of its ability to model multiple related dummy variable predictors and associated interaction terms, and because it provides bootstrapping capability while accommodating tests of indirect effects with dichotomous outcome variables. Moderated mediation analyses tested the significance of indirect effects of treatment condition on adolescent’s remission status through the changes in observed indices of adolescent interpersonal behavior different levels of the moderator (i.e., maternal depressive symptoms). Maximum likelihood estimation was used to test for moderated mediation and the significance of each indirect effect was determined using bias-corrected bootstrapping to define the 95% confidence interval. Bootstrapping the indirect effects is recommended particularly when sample size is small (n < 500) and when the model contains dichotomous variables (MacKinnon, Warsi, & Dwyer, 1995; Shrout & Bolger, 2002).
Results
Preliminary Analyses
Preliminary analyses confirmed the comparability of baseline demographic and clinical characteristics across the CBT, SBFT, and NST treatment conditions (see Table 1). Adolescents’ pre-treatment hopelessness scores (ηp2 = 0.23, p = 0.05) were significantly associated with post-treatment remission status and was therefore included as a covariate in analyses testing Paths b, c′, and moderated mediation. Adolescents’ self-reports of cognitive distortions, maternal BDI scores before adolescents’ treatment, and history of abuse were not significantly associated with adolescents’ post-treatment remission status and were not included as covariates in subsequent analyses.
Table 1.
Demographic Characteristics (Mean ± SD)
| CBT (n = 25) | SBFT (n = 20) | NST (n = 18) | Statistic | |
|---|---|---|---|---|
| Age (years) | 15.6 ± 1.3 | 15.5 ± 1.4 | 15.6 ± 1.3 | F (2, 60) = 0.03 |
| Sex, % female | 76.0% | 75.0% | 83.3% | χ2 (df = 2, n = 63) = 0.46 |
| Minority status, % | 24.0% | 10.0% | 11.1% | χ2 (df = 2, n = 63) = 2.06 |
| SES (Hollingshead) | 38.7 ± 11.6 | 41.1 ± 10.3 | 38.9 ± 18.1 | F (2, 59) = 0.20 |
| Two-parent family, % yes | 52.0% | 40.0% | 55.6% | χ2 (df = 2, n = 63) = 1.05 |
| Comorbid Disruptive Behavior Disorder, % | 16.0% | 15.0% | 33.3% | χ2 (df = 2, n = 63) = 2.49 |
| Comorbid Anxiety Disorder, % | 24.0% | 5.0% | 11.1% | χ2 (df = 2, n = 63) = 3.48 |
| History of Abuse, % | 24.0% | 15.0% | 16.7% | χ2 (df = 2, n = 63) = 0.68 |
| Sessions Completed | 13.6 ± 1.4 | 13.4 ± 1.1 | 13.8 ± 1.5 | F (2, 60) = 0.48 |
| Adolescent BDI (pre-treatment) | 24.6 ± 8.6 | 22.7 ± 7.7 | 24.4 ± 7.0 | F (2, 60) = 0.39 |
| Maternal BDI (pre-treatment) | 13.1 ± 10.4 | 10.6 ± 6.5 | 12.7 ± 10.5 | F (2, 60) = 0.45 |
| Hopelessness (BHS) | 11.8 ± 5.9 | 9.7 ± 5.1 | 12.0 ± 5.6 | F (2, 57) = 1.02 |
| Mother-adolescent Conflict (CBQ), adolescent report | 8.8 ± 6.4 | 12.3 ± 5.3 | 8.5 ± 6.0 | F (2, 57) = 2.41 |
| Cognitive Distortions (CNCEQ) | 79.0 ± 17.8 | 82.5 ± 18.0 | 76.6 ± 21.7 | F (2, 57) = 0.45 |
| Adolescent Involvement (pre-treatment) | 3.3 ± 0.08 | 3.1 ± 0.6 | 3.4 ± 0.7 | F (2, 60) = 0.79 |
| Adolescent Problem Solving (pre-treatment) | 3.2 ± 1.3 | 3.0 ± 1.0 | 3.3 ± 1.1 | F (2, 60) = 0.31 |
| Dyadic Conflict (pre-treatment) | 2.6 ± 1.2 | 2.1 ± 1.0 | 2.6 ± 0.9 | F (2, 60) = 1.44 |
| Adolescent Diagnosis of MDD (post-treatment) | 8.0% | 15.0% | 16.7% | χ2 (df = 2, n = 63) = 0.85 |
| Adolescent Remission Status (post-treatment) | 80.0% | 50.0% | 50.0% | χ2 (df = 2, n = 63) = 5.76† |
Note: Means with different superscripts are significantly different
p < 0.10
Effects of Treatment Condition on Changes in Observed Adolescent Interpersonal Behavior during Mother-Adolescent Interactions (see Figure 1, Path a)
Linear regressions were conducted to determine whether treatment type was associated with changes in adolescent involvement, problem solving, or dyadic conflict over time. In each model, the outcome measure was the observed adolescent behavior at post-treatment. The predictor variables were two dummy coded variables for treatment group (CBT and SBFT) and one covariate, the observed adolescent behavior at pre-treatment. The effects of pre-treatment variables were included to isolate the change in mother-adolescent interaction variables at post-treatment or to, in effect, create change scores. Results indicated that CBT (B = 0.41, CI = .29 – 1.67, t-value = 2.85, p = 0.006) and SBFT (B = 0.30, CI = .02 – 1.47, t-value = 2.07, p = 0.04) were each significantly associated with increases in adolescent problem solving across treatment. As there were no significant associations between treatment group and changes in adolescents’ involvement or dyadic conflict, subsequent analyses were limited to adolescent problem solving.
Changes in Adolescent Problem Solving and Adolescent Remission Status (Figure 1, Path b)
Adolescents’ post-treatment remission status was regressed on changes in adolescent problem solving. Treatment group (dummy codes), pre-treatment adolescent BDI, hopelessness, and pre-treatment adolescent problem solving scores were entered as step 1 and post-treatment adolescent problem solving scores were entered as step 2 of the regression model. Changes in adolescent problem solving were significantly associated with adolescents’ post-treatment remission status (Wald z = 6.11, p = 0.01). Higher ratings of adolescent problem solving were associated with higher rates of remission in adolescents after treatment.
Association Between Treatment Condition and Adolescent Remission Status (Figure 1, Path c)
Logistic regression was used to examine the relationship between treatment condition and adolescent post-treatment remission status. Treatment group (dummy codes) was the independent variable, and adolescent post-treatment remission status was the dependent variable. A significant association was found for CBT and remission status (Wald z = 4.64, p = 0.03), but not for SBFT and remission status (Wald z = 0.00, p = 0.99).
Testing Indirect Effects of Changes in Adolescent Problem Solving on the Association between Treatment Condition and Adolescent Remission Status (Figure 1, Path c′)
Indirect effects in the CBT and SBFT conditions were analyzed separately. In the CBT model, the association between CBT and adolescent problem solving (Path a, B = 1.01, p = .005) was significant as was the association between changes in adolescent problem solving and remission status (Path b, B = .64, p = .05). However the indirect effect was not significant within a 95% CI. These analyses were repeated for the SBFT group despite the lack of a significant Path c between SBFT and adolescent remission status to confirm no significant indirect effect of SBFT on remission status through change in adolescent problem solving on. In the final regression model, the association between SBFT and changes in adolescent problem solving remained significant (Path a, B = .90, p = .02) as did the association between changes in adolescent problem solving and remission status (Path b, B = .64, p = .05). However, the indirect effect was not significant within a 95% confidence interval (CI).
Maternal Depressive Symptoms as Moderators of Treatment Condition on Adolescent Problem Solving (Figure 1, Path d)
Next, maternal depressive symptoms were tested as moderators of the associations between treatment condition and changes in adolescent problem solving across the course of treatment. Treatment group (dummy coded), maternal depressive symptoms, and pre-treatment adolescent problem-solving were entered into step 1 of the linear regression. Two interaction terms, one for CBT x maternal depressive symptoms and one for SBFT x maternal depressive symptoms, were included in step 2 of the model. Results yielded a significant interaction between CBT and maternal depressive symptoms predicting changes in adolescent problem solving (see Table 2). Post-hoc analyses were conducted to probe the significant interaction between CBT and maternal depressive symptoms on changes in adolescent problem solving by estimating the simple slopes of the moderator at low, medium, and high levels as outlined by Aiken and West (1991, pp. 12–13). Regression models were repeated conducted using these transformed variables (and interaction terms between CBT group status and each of the transformed variables). Simple slope analyses indicated that the relationship between CBT and changes in adolescent problem solving was strong and significant only when mothers had low (B = 0.69, CI = 0.34 – 1.25, t = 3.51, p < 0.001) or moderate depressive symptoms (B = 0.42, CI = 0.16 – 0.81, t = 3.02, p < 0.001). When maternal depressive symptoms were high, there was no significant relationship between CBT and changes in adolescent problem solving (B = 0.16, CI = −0.24 – 0.61, t = 0.87, p = 0.39).
Table 2.
Regression of Adolescent Problem Solving on Treatment Group by Maternal Depressive Symptoms.
| Standardized B | Confidence Interval (95%) | t | p | |
|---|---|---|---|---|
| Step one: | ||||
| CBT | 0.42 | 0.16 – 0.81 | 3.02 | 0.00 |
| SBFT | 0.29 | 0.01 – 0.69 | 2.03 | 0.05 |
| Adolescent Problem Solving (pre-treatment) | 0.24 | −0.00 – 0.50 | 2.00 | 0.05 |
| Maternal BDI (pre-treatment) | 0.02 | −0.29 – 0.34 | 0.15 | 0.88 |
| Step two: | ||||
| CBT x Maternal BDI (Path d) | −0.28 | −0.60 – −0.01 | −2.07 | 0.04 |
| SBFT x Maternal BDI (Path d) | −0.23 | −0.73 – 0.07 | −1.63 | 0.11 |
Note: Cognitive behavior therapy (CBT) and systemic behavior family therapy (SBFT) were coded such that 0 = no and 1 = yes. BDI = Beck Depression Inventory.
Moderated Mediation
Because a significant interaction between CBT and maternal depressive symptoms predicting changes in adolescent problem solving, moderated mediation was tested. The mediated effect was calculated using the simple slope parameter estimates of maternal depressive symptoms (high, moderate, and low) previously obtained from moderator analyses. Results are presented in Table 3. Changes in adolescents’ problem solving significantly mediated the relationship between CBT and remission status when maternal depressive symptoms at study entry were low or moderate. Changes in adolescents’ problem solving skills did not significantly mediate the relationship between CBT and remission status for adolescents whose mothers endorsed high depressive symptoms at study entry.
Table 3.
Indirect Effects of changes in adolescents’ problem solving on the relationship between CBT and adolescent remission status at high, medium, and low levels of maternal depression.
| B | SE | p | |
|---|---|---|---|
| Path a | 1.79 | 0.57 | 0.002 |
| Path d | −0.06 | 0.03 | 0.03 |
| Path b | 0.10 | 0.05 | 0.05 |
| Path c | 0.19 | 0.14 | 0.18 |
| Indirect Effects | Confidence Interval (95%) | ||
| Low Maternal Depressive Symptoms | 0.17 | 0.10 | 0.02 – 0.43 |
| Moderate Maternal Depressive Symptoms | 0.12 | 0.07 | 0.01 – 0.30 |
| High Maternal Depressive Symptoms | 0.05 | 0.05 | −0.009 – 0.19 |
Note: Dummy coded SBFT variable and related interaction terms were included in statistical models to control for the effects of SBFT on changes in adolescent problem solving and remission status; results are not presented for the SBFT condition as maternal depressive symptoms did not moderate the association between SBFT and changes in adolescent’ problem solving across treatment. Path a: association between CBT and changes in adolescent problem solving. Path d: association of CBT x maternal depressive symptoms on changes in adolescent problem solving. Path b: association between changes in adolescent problem solving and remission status. Path c: association between CBT and adolescent remission status
Discussion
Observed incidents of adolescent problem solving in interactions with mothers increased over the course of treatment for depression; however, increases in problem solving were specific to the structured treatment conditions of CBT and SBFT. Maternal depressive symptoms at baseline significantly moderated the relationship between CBT and changes in adolescent problem solving, but not for SBFT. Whereas depressed adolescents in the CBT group with mothers endorsing lower depressive symptoms evidenced increased problem-solving after treatment, higher maternal depressive symptoms at the time of study entry disrupted expected increases in problem solving for depressed adolescents receiving CBT. Although increased problem-solving was associated with adolescents’ remission status post-treatment, adolescent problem solving did not mediate the association between SBFT and adolescent remission status at post-treatment. Exploratory analyses utilizing a moderated mediation design indicated a significant Pathway: changes in adolescent problem solving mediated the effect of CBT on adolescent remission status depending upon the severity of maternal depressive symptoms at study entry, but not when maternal depressive symptoms at study entry were high.
The specificity of increased problem solving in the structured psychotherapies of CBT and SBFT is consistent with theoretical underpinnings and putative active components of each treatment for decreasing depressive symptoms. The problem solving component in Brent and colleagues’ CBT protocol (Brent et al., 1997) focused on increasing cognitive flexibility and systematically assessing the outcomes before engaging in problem focused action, whereas problem solving in the SBFT protocol focused on negotiation and compromise in order to reduce family stressors and conflict that may maintain adolescents’ depressive symptoms. Both modalities were associated with increases in adolescent problem solving from pre- to post-treatment. In turn, increases in adolescent problem solving were also associated with higher rates of remission at post-treatment. Ultimately, a causal relationship between increased problem solving skills and higher rates of adolescent remission from depression cannot be established from this paper. The bi-directional relationship between changes in adolescent problem solving and remission from depression also raises the possibility that changes in adolescents’ depressive diagnosis over treatment may mediate the changes observed in adolescent problem solving. However, this alternative model was not supported by supplemental analyses conducted on this sample (see Supplemental Materials 3).
Maternal depressive symptoms at study entry significantly moderated the relationship between CBT and changes in adolescent problem solving, as depressed adolescents in the CBT group evidenced increased problem-solving after treatment only when mothers’ depressive symptoms at study entry were low or moderate. This paper is among the first to explore how maternal depressive symptoms may disrupt the relationship between CBT and favorable treatment outcomes in depressed adolescents. Depressed adolescents with depressed mothers may be less able to adopt new strategies for interpersonal problem solving problem solving or may not be able to model more effective problem solving in interactions with their mothers (Hammen, Shih, Altman, & Brennan, 2003; Sheeber, Allen, Davis, & Sorensen, 2000). Still, it is important to underscore that that maternal depression did not directly moderate changes in problem solving in relation to remission status. Unlike other studies that have found maternal BDI to moderate the efficacy of CBT, the current study found that improved problem solving may be a path to remission for youth whose mothers have low symptoms of depression. Hence, there may be other path(s) to remission for depressed youth with mothers with high BDI scores.
These findings may inform future studies that seek to optimize treatment by matching interventions to individual patient characteristics of depressed youths. It is noteworthy that maternal depression did not moderate the effects of SBFT on increases in adolescents’ problem solving across treatment. One possible explanation for this finding is that the interpersonal problem solving utilized in SBFT was more robust than the problem solving module in CBT that was used on an as-needed basis, as changes in adolescent problem solving in the SBFT group occurred regardless of the severity of maternal depression, while in the CBT group problem solving was only increased when mothers were not more severely depressed. This explanation supports the broader effectiveness of the family-based treatment, particularly for adolescents whose mothers were depressed. A competing explanation is that maternal depressive symptoms may moderate the effects of SBFT on changes in adolescents’ problem solving, but low statistical power rendered us unable to find a significant interaction (p = .11). Indeed, the magnitude of the effect for the interaction between SBFT and maternal BDI is very similar to the effect for the CBT by maternal BDI interaction. Future studies are necessary determine if maternal depression uncouples adolescent problem solving in structured psychotherapies.
SBFT did not indirectly affect remission status through changes in adolescents’ problem solving. Indirect effects of changes in adolescent problem solving may not have been significant because of the low statistical power given the sample size and a weak association between SBFT and adolescent remission status. While SBFT was associated with improved problem solving in depressed adolescents, the 12–16 week time-limited treatment might not have been sufficient for a complete remission of adolescents’ depressive symptoms. Despite no differences in the number of weeks that adolescents in the CBT or SBFT groups attended treatment, the positive effects of SBFT on adolescents’ remission from depression may be expected to occur after improvements in family communication and problem solving skills.
Finally, it is important to underscore that problem solving is not the only pathway by which adolescents’ depressive symptoms may decrease. Although not significant, there were trends for increases in adolescents’ involvement in both the CBT and SBFT groups, suggesting that interpersonal involvement may warrant further exploration in future studies with sufficient statistical power. Significant changes in dyadic conflict were not related to treatment condition or remission status in the present study; however, the use of videotaping during mother-adolescent interactions may have inhibited more frequent or intense conflict between dyads, and may have yielded conservative estimates of dyadic conflict. Adolescents receiving NST also evidenced an increase in remission over the course of treatment (see Brent et al., 1997), despite the decline in interpersonal problem solving observed in the NST group from pre- to post-treatment. As such, there also needs to be a continued examination of different mechanisms, such as nonspecific factors related to a strong therapeutic alliance that may facilitate a decrease in adolescents’ depressive symptoms in supportive and client-centered treatments modalities.
There are several limitations of the current study. These findings can only be considered preliminary since there was only a small subset of adolescents across treatment conditions that had both pre-treatment and post-treatment mother-adolescent interaction data. The possibility of Type I error is strong; these results would not be statistically significant if a Bonferroni correction was applied for multiple comparisons. These results are heavily dependent on future studies confirming that problem-solving is indeed a pivotal construct, and not the result of chance when analyzing a series of different outcome measures. The limited statistical power in this study may have also obscured significant differences between this subsample of adolescents and those who did not completed the videotaped mother-adolescent interaction tasks before and after treatment, or differences between adolescents who completed treatment compared to those who did not. Because of issues of low statistical power, we were careful to avoid over-modeling data because of limited statistical power in this study in order to ensure the validity of our results. Findings from moderated mediation analyses can only be considered exploratory due to low statistical power and because of the proposed mediator, adolescent problem solving, and the dependent variable, remission status, were measured at the same time. Hence, although our results support hypotheses that high levels of maternal depressive symptoms may uncouple the efficacy of CBT for adolescent depression through disrupting improvements in problem solving, this hypothesis must be subsequently investigated in future studies.
Further limitations of this study include a homogenous sample of adolescents, an exclusive focus on mother-adolescent interactions, and clinical response of participants. As the majority of this sample was Caucasian, the pattern of findings described in the current study may not characterize interactions between mothers and depressed adolescents in racial and ethnic minority groups. Similarly, it may be the case that quantifying adolescents’ problem solving skills from dyadic interactions with their mothers may not generalize to their level of social competence in problem solving in relationships with peers or other adults. As fathers were not included in problem-solving interactions with adolescents, these findings may not generalize across parents. It is also important to underscore that adolescents whose depression did not improve were removed from the study after the 6th week of treatment, and findings from this study are specific to depressed adolescents who respond to psychosocial treatments. Finally, the decline in observed interpersonal problem solving in the NST group may have magnified the improvements in problem solving for adolescents in the CBT and SBFT groups, insofar that had adolescent problem solving remained stable for the NST group increases for the two structured psychotherapy groups may not have been statistically significant.
Problem solving training for depressed adolescents may be one approach to maximize efficacious treatment outcomes by delivering an ‘active component’ of CBT at a concentrated dose and within a shorter time frame (Weersing et al., 2009). Several treatment studies utilizing CBT for adolescent depression have found positive associations between frequent use of problem solving training and treatment response (Becker-Weidman, Jacobs, Reinecke, Silva, & March, 2010; Kennard et al., 2009). Preliminary data provide support for the effectiveness of a brief CBT protocol to treat internalizing disorders in youths in primary care that includes use of social problem-solving skills for treating depression and anxiety disorders in youths (Weersing, Gonzalez, Campo, & Lucas, 2008). Future research must be conducted on the efficacy of problem solving as a ‘stand alone’ treatment for depression in adolescents, in addition to investigating problem solving as a mediator of treatment outcomes in CBT.
Results from this study also support a growing body of empirical studies that have found reducing maternal depression to have positive effects on children’s internalizing symptoms (Pilowsky, et al., 2008; Swartz, et al., 2008; Weissman, et al., 2006). Addressing maternal depression and its affect on children and adolescents remains a key challenge for clinicians who treat depressed youth. Integrative or concurrent treatments for depression may reduce barriers for treatment for depressed mothers of youth presenting with a psychiatric disorders. Future treatment development may need to explore integrative treatments for both depressed youths and mothers that focus on improving interpersonal processes as a means of symptom reduction, including interpersonal problem solving (Dietz, Mufson, Irvine, & Brent, 2008b).
Supplementary Material
Acknowledgments
This research was supported in part by grants from the National Institute of Mental Health (MH 46500, David A. Brent, P.I.; MH 079353, Laura J. Dietz, P.I.).
References
- Aiken L, West S. Multiple Regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Alexander JF, Parsons BV. Short-term behavioral intervention with delinquent families: impact on family process and recidivism. Journal of Abnormal Psychology. 1973;81(3):219–225. doi: 10.1037/h0034537. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Emslie G, Clarke G, Wagner KD, Spirito A, Vitiello B, Brent D. Treatment of selective serotonin reuptake inhibitor-resistant depression in adolescents: predictors and moderators of treatment response. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48(3):330–339. doi: 10.1097/CHI.0b013e3181977476.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3. Washington, DC: Author; 1987. rev. [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting & Clinical Psychology. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York, NY: Guilford Press; 1979. [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. Journal of Consulting & Clinical Psychology. 1974;42(6):861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Becker-Weidman EG, Jacobs RH, Reinecke MA, Silva SG, March JS. Social problem-solving among adolescents treated for depression. Behavior Research & Therapy. 2010;48(1):11–18. doi: 10.1080/15374416.2010.486318.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Kolko D, Baugher M, Bridge J, Holder D, Ulloa RE. Clinical outcome after short-term psychotherapy for adolescents with major depressive disorder. Archives of General Psychiatry. 2000;57(1):29–36. doi: 10.1001/archpsyc.57.1.29. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Bridge JA, Williamson DE, Brent DA, Dahl RE, Axelson DA, Ryan ND. Psychosocial functioning in youths at high risk to develop major depressive disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2004a;43(7):839–846. doi: 10.1097/01.chi.0000128787.88201.1b. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Williamson DE, Dahl RE, Axelson DA, Kaufman J, Dorn LD, Ryan ND. Clinical presentation and course of depression in youth: does onset in childhood differ from onset in adolescence? Journal of the American Academy of Child & Adolescent Psychiatry. 2004b;43(1):63–70. doi: 10.1097/00004583-200401000-00015. [DOI] [PubMed] [Google Scholar]
- Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, Zelazny J. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. Journal of the American Medical Association. 2008;299(8):901–913. doi: 10.1001/jama.299.8.901.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Holder D, Kolko D. Treatment for adolescent depression. Harvard Mental Health Letter. 1998a;15(2):7. [PubMed] [Google Scholar]
- Brent DA, Holder D, Kolko D, Birmaher B, Baugher M, Roth C, Johnson BA. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Archives of General Psychiatry. 1997;54(9):877–885. doi: 10.1001/archpsyc.1997.01830210125017. [DOI] [PubMed] [Google Scholar]
- Brent DA, Kolko DJ, Birmaher B, Baugher M, Bridge J, Roth C, Holder D. Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. Journal of the American Academy of Child & Adolescent Psychiatry. 1998b;37(9):906–914. doi: 10.1097/00004583-199809000-00010. [DOI] [PubMed] [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M. The assessment of affective disorders in children and adolescents by semistructured interview. Test-retest reliability of the schedule for affective disorders and schizophrenia for school-age children, present episode version. Archives of General Psychiatry. 1985;42(7):696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West S, Aiken L. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Mahwah, NJ: Lawrence Erlbaum Associates; 2003. [Google Scholar]
- Dietz LJ, Birmaher B, Williamson DE, Silk JS, Dahl RE, Axelson DA, Ryan ND. Mother-child interactions in depressed children and children at high risk and low risk for future depression. Journal of the American Academy of Child & Adolescent Psychiatry. 2008a;47(5):574–582. doi: 10.1097/CHI.0b013e3181676595.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz LJ, Mufson L, Irvine H, Brent DA. Family Based Interpersonal Psychotherapy (FB-IPT) for Depressed Preadolescents: An Open Treatment Trial. Early Intervention in Psychiatry. 2008b;2:154–161. doi: 10.1111/j.1751-7893.2008.00077.x.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeny NC, Silva SG, Reinecke MA, McNulty S, Findling RL, Rohde P, March JS. An exploratory analysis of the impact of family functioning on treatment for depression in adolescents. Journal of Clinical Child & Adolescent Psychology. 2009;38(6):814–825. doi: 10.1080/15374410903297148.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Clarke GN, Weersing VR, Beardslee WR, Brent DA, Gladstone TR, Iyengar S. Prevention of depression in at-risk adolescents: a randomized controlled trial. Journal of the American Medical Association. 2009;301(21):2215–2224. doi: 10.1001/jama.2009.788.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychoPathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106(3):458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Hammen C, Shih J, Altman T, Brennan PA. Interpersonal impairment and the prediction of depressive symptoms in adolescent children of depressed and nondepressed mothers. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(5):571–577. doi: 10.1097/01.CHI.0000046829.95464.E5. [DOI] [PubMed] [Google Scholar]
- Hammen C, Shih JH, Brennan PA. Intergenerational transmission of depression: test of an interpersonal stress model in a community sample. Journal of Consulting & Clinical Psychology. 2004;72(3):511–522. doi: 10.1037/0022-006X.72.3.511. [DOI] [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper] 2012 Retrieved from http://www.afhayes.com/public/process2012.pdf.
- Hetherington EM, Hagan MS, Eisenberg M. Family Interaction coding system. 1992. (Unpublished Manuscript) [Google Scholar]
- Hollingshead A. Four factor index of social status. Yale University; New Haven, CT: 1975. Unpublished Manuscript. [Google Scholar]
- Kennard BD, Clarke GN, Weersing VR, Asarnow JR, Shamseddeen W, Porta G, Brent DA. Effective components of TORDIA cognitive-behavioral therapy for adolescent depression: preliminary findings. Journal of Consulting & Clinical Psychology. 2009;77(6):1033–1041. doi: 10.1037/a0017411.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolko DJ, Brent DA, Baugher M, Bridge J, Birmaher B. Cognitive and family therapies for adolescent depression: treatment specificity, mediation, and moderation. Journal of Consulting & Clinical Psychology. 2000;68(4):603–614. [PubMed] [Google Scholar]
- Leitenberg H, Yost LW, Carroll-Wilson M. Negative cognitive errors in children: questionnaire development, normative data, and comparisons between children with and without self-reported symptoms of depression, low self-esteem, and evaluation anxiety. Journal of Consulting & Clinical Psychology. 1986;54(4):528–536. doi: 10.1037//0022-006x.54.4.528. [DOI] [PubMed] [Google Scholar]
- Lerner M, Clum G. Treatment of suicide ideators: A problem-solving approach. Behavioral Therapy. 1990;21:403–411. [Google Scholar]
- MacKinnon DP, Luecken LJ. How and for whom? Mediation and moderation in health psychology. Health Psychology. 2008;27(2 Suppl):S99–S100. doi: 10.1037/0278-6133.27.2(Suppl.).S99.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Warsi G, Dwyer JH. A simulation study of mediated effect measures. Multivariate Behavioral Research. 1995;30:41–62. doi: 10.1207/s15327906mbr3001_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, Severe J. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. Journal of the American Medical Association. 2004;292(7):807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- Nomura Y, Wickramaratne PJ, Warner V, Mufson L, Weissman MM. Family discord, parental depression, and psychoPathology in offspring: ten-year follow-up. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41(4):402–409. doi: 10.1097/00004583-200204000-00012. [DOI] [PubMed] [Google Scholar]
- Pilowsky DJ, Wickramaratne P, Talati A, Tang M, Hughes CW, Garber J, Weissman MM. Children of depressed mothers 1 year after the initiation of maternal treatment: findings from the STAR*D-Child Study. American Journal of Psychiatry. 2008;165(9):1136–1147. doi: 10.1176/appi.ajp.2008.07081286.. [DOI] [PubMed] [Google Scholar]
- Robin A, Foster S. Negotiating Parent-Adolescent Conflict: A Behavioral Family Systems Approach. New York, NY: Guilford Press; 1989. [Google Scholar]
- Robin AL, Weiss JG. Criterion-related validity of behavioral and self-report measures of problem-solving communication skills in distressed and non-distressed parent-adolescent dyads. Behavioral Assessment. 1980;2:339–352. [Google Scholar]
- Rogers CR. Client-centered Therapy: Its Current Practice, Implications and Theory. London: Constable; 1951. [Google Scholar]
- Sheeber L, Allen N, Davis B, Sorensen E. Regulation of negative affect during mother-child problem-solving interactions: adolescent depressive status and family processes. Journal of Abnormal Child Psychology. 2000;28(5):467–479. doi: 10.1023/a:1005135706799. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Alpert A, Davis B, Andrews J. Family support and conflict: prospective relations to adolescent depression. Journal of Abnormal Child Psychology. 1997;25(4):333–344. doi: 10.1023/a:1025768504415. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Davis B. Family processes in adolescent depression. Clinical Child & Family Psychology Review. 2001;4(1):19–35. doi: 10.1023/a:1009524626436. [DOI] [PubMed] [Google Scholar]
- Shelton KH, Harold GT. Interparental conflict, negative parenting, and children’s adjustment: bridging links between parents’ depression and children’s psychological distress. Journal of Family Psychology. 2008;22(5):712–724. doi: 10.1037/a0013515.. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Silk JS, Ziegler ML, Whalen DJ, Dahl RE, Ryan ND, Dietz LJ, Williamson DE. Expressed emotion in mothers of currently depressed, remitted, high-risk, and low-risk youth: links to child depression status and longitudinal course. Journal of Clinical Child & Adolescent Psychology. 2009;38(1):36–47. doi: 10.1080/15374410802575339.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz HA, Frank E, Zuckoff A, Cyranowski JM, Houck PR, Cheng Y, Shear MK. Brief interpersonal psychotherapy for depressed mothers whose children are receiving psychiatric treatment. American Journal of Psychiatry. 2008;165(9):1155–1162. doi: 10.1176/appi.ajp.2008.07081339.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weersing VR, Gonzalez A, Campo J, Lucas A. Brief behavioral therapy for pediatric anxiety and depression: Piloting an integrated treatment approach. Cognitive and Behavioral Practice. 2008;15:126–139. [Google Scholar]
- Weersing VR, Rozenman M, Gonzalez A. Core components of therapy in youth: do we know what to disseminate? Behavior Modification. 2009;33(1):24–47. doi: 10.1177/0145445508322629.. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. American Journal of Psychiatry. 2006;163(6):1001–1008. doi: 10.1176/ajp.2006.163.6.1001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.